Abstract
Ensuring diets of children aged 6–23 months meet recommended guidance is crucial for growth and development and for the prevention of malnutrition including stunting, wasting and micronutrient deficiencies. Despite some improvement, indicators related to undernutrition and overnutrition fall short of global targets in the Middle East and North Africa (MENA) region that consist of low‐ and middle‐income countries witnessing political and social changes and a nutrition transition. This research aims at reviewing the situation related to the diets of children aged 6–23 months in five selected countries in the MENA region, examining factors affecting complementary feeding and providing recommendations for guiding effective strategies to improve it. The study triangulated data on complementary feeding status and predictors from semistructured interviews with 30 key informants, and multivariable analysis of household surveys in Egypt, Jordan, Lebanon, State of Palestine and Sudan including data on refugees in Lebanon and Jordan. There remain considerable gaps in complementary feeding differing noticeably among geographic areas. Findings from qualitative and quantitative analyses showed that maternal factors, including maternal education and age, household level factors such as paternal education and wealth, community‐level factors (culture and geographic location), and utilization of health services, were associated with minimum dietary diversity (MDD), minimum meal frequency (MMF) and minimum acceptable diet (MAD) at varied levels in the five countries. Interventions to improve complementary feeding practices should include actions tailored to the needs of the population at multiple levels including at the caregiver's level, household, service use, community and policy level.
Keywords: complementary feeding, DHS, Egypt, infant and young child feeding, Jordan, Lebanon, MICS, mixed methods research, multilevel model, predictors, State of Palestine, Sudan
Key messages
Complementary feeding practices among children aged 6–23 months in five countries of the MENA region do not meet recommendations with lowest rates in Sudan and among Syrian refugees in Lebanon.
The most consistent predictors of complementary feeding across all countries are at the maternal and household level including maternal education and wealth quintiles.
At the community level and within countries, there are significant differences in complementary feeding indicators.
Where data exist for two countries, utilization of antenatal care and receiving vitamin A supplementation were among the health services utilization factors associated with complementary feeding indicators.
Factors at the policy level need further investigation.
1. INTRODUCTION
Optimal nutrition during the first 1000 days between conception and a child's second birthday is vital for children to reach their full growth and development potential and can protect from adverse health outcomes in later life (Adair et al., 2013; Wrottesley et al., 2016). The World Health Organization (WHO) and the United Nations International Children's Fund (UNICEF) recommend exclusive breastfeeding for the first 6 months of age, after which the introduction of adequate and age appropriate complementary food, with continued breastfeeding up to the age of 2 years and beyond are advised (WHO & UNICEF, 2003). Ensuring recommended complementary feeding (CF) practices requires that infants and young children have age appropriate food consistency, variety and frequency (WHO, UNICEF, & USAID, 2008).
The lack of compliance with these recommendations along with increased susceptibility to infection during the period between 6 and 23 months of age has been associated with poor health and nutrition outcomes. These can include overnutrition and/or undernutrition as well as infant and young child mortality with effects mediated by poor nutrition (Bhutta et al., 2013; Danaei et al., 2016).
The Middle East and North Africa (MENA) region includes low‐ and middle‐income countries, several of which are facing humanitarian emergencies from natural disasters and/or conflict. The region, which includes countries that are extremely diverse in their culture and political stability, has witnessed significant social, economic and political changes impacting the lifestyle and health of populations (WHO, 2019). Shifts in diets and lifestyles have led to a nutrition transition characterized by a reliance on high‐energy, nutrient‐poor diets while at the same time there is a threat of food insecurity, undernutrition and micronutrient deficiencies (FAO et al., 2020; Ghattas et al., 2020; Nasreddine et al., 2018).
Regardless of the stage of the nutrition transition of the varying countries of the region, children remain the most vulnerable to malnutrition in all its forms including stunting, wasting, anaemia, other micronutrient deficiencies, overweight, and obesity. Similar to the situation at the global level (Development Initiatives, 2020), progress in nutrition indicators in this region has been slow with inequities between and within countries. It is estimated that the regional average prevalence of stunting and wasting are 15% and 8%, respectively, whereas the regional average prevalence of overweight and obesity in children under 5 years is 11% (United Nations Children’s Fund, Division of Data Research and Policy, 2019).
A recent regional analysis highlighted the double burden of malnutrition and the prevalence of both overnutrition (overweight) and undernutrition (stunting) in under‐5 year olds in the region (Ghattas et al., 2020). This double burden has been reported to occur both within countries as well as within households. In Egypt, the prevalence of households where a child is stunted and the mother is overweight has been reported to exceed 10%, and this has been linked to low diet diversity and increased consumption of sugary snacks (Aitsi‐Selmi, 2015). In the Gaza Strip, 16% of households were found to include an overweight mother and an underweight child (El Kishawi et al., 2016). Infant and young child feeding (IYCF) indicators have also shown little improvements in the region where only 38% of children aged 6–23 months have adequate diet diversity and 21% only meet the minimum acceptable diet (MAD) (United Nations Children’s Fund, Division of Data Research and Policy, 2019).
Considering the multitude of adverse nutritional status outcomes in children and the lack of analysis on predictors of IYCF practices in the region, a better understanding of practices and factors that affect child feeding is important to identify entry points for the improvement of infant and young children's diets and nutrition. In 2018, and in order to address gaps in nutrition, UNICEF MENA Regional Office (MENARO) prioritized support to countries in the region by accelerating interventions aimed at improving the diets of young children to reduce stunting. Simultaneously, UNICEF launched a new framework for CF programming, which aims at improving CF by adopting a systems approach (UNICF, 2020). The first element for the action framework includes conducting a situation analysis to understand the status and drivers of young children's diets.
The objectives of this study are to:
Review the situation related to CF practices including indicators of CF such as minimum diet diversity (MDD), minimum meal frequency, and minimum adequate diet in five selected countries of the MENA region [Egypt, Jordan, Lebanon, State of Palestine (SoP) and Sudan].
Examine the factors associated with appropriate CF at the individual, household, service utilization, community and policy level among children aged 6–23 months in the five selected countries using qualitative as well as nationally representative data.
Provide recommendations to guide the development of effective strategies and programmatic activities that optimize CF in the MENA region.
2. METHODS
2.1. Selected country populations
We focused on five countries in the MENA region: Egypt, Jordan, Lebanon, State of Palestine (SoP) and Sudan to examine diets of children aged 6–23 months. These countries were selected as they provide variability in terms of geographic subregion, income levels, exposure to emergency/conflict and stage of the nutrition transition. Sudan represents a low‐income country in North Africa as well as a complex emergency context. Egypt, Jordan, Lebanon and SoP are middle‐income countries in the early stages of the nutrition transition. Jordan and Lebanon both host a large number of refugees including Syrians and Palestinians. Appendix A presents nutrition status indicators in the five selected countries.
2.2. Overall study design
An exploratory approach was used in which information was collected from various sources and triangulated, where applicable, to create a comprehensive view of the situation related to CF practices and their predictors in the five countries. This study therefore combined stakeholder perspectives through key‐informant interviews and a secondary analysis of data on CF indicators and their predictors from household surveys. It was guided by existing frameworks including the UNICEF framework for malnutrition (UNICEF, 1990), the UNICEF Programming Guidance (UNICEF, 2020), the socioecological model (CDC, 2016) and the nurturing care framework (WHO, 2018). Accordingly, when exploring factors associated with CF practices, these were grouped into child level, individual level, household, community, health service utlisation and policy level (the latter only for qualitative interviews).
2.3. Qualitative interviews
Semistructured interviews with key informants were conducted in all five countries. Interviews served as a tool to collect information on perceptions around the diets of children 6–23 months of age, factors affecting feeding practices and existing relevant policies.
Semistructured interviews were conducted (either face to face or via Skype) with a convenient sample of key informants identified from Ministries of Health, UN agencies and non‐governmental organizations (NGOs) holding key positions with engagement in nutrition and IYCF in the country (Table 1).
TABLE 1.
Interviews conducted and household surveys used
| Country | Number of individuals interviewed | Datasets | Population groups/datasets |
|---|---|---|---|
| Egypt |
2 MoH representatives 3 UN representatives 1 NGO representative |
DHS 2014 | 1. Nationals in Egypt |
| Jordan |
1 MoH representative 2 UN representatives |
DHS 2017/2018 |
2. Nationals in Jordan 3. Syrian refugees in Jordan (SRJ) |
| Lebanon |
3 MoH representatives 2 UN representatives 3 NGO representatives |
UNICEF Baseline Survey 2016 |
4. Nationals in Lebanon 5. Syrian refugees in Lebanon (SRL) 6. Palestinian refugees in Lebanon (PRL) 7. Palestinians coming from Syria in Lebanon (PRSL) |
| Sudan |
5 MoH representatives 2 UN representatives 3 NGO representatives |
MICS 2014 | 8. Nationals in Sudan |
| SoP |
1 MoH representative 1 UN representative 1 NGO representative |
MICS 2014 | 9. Nationals in SoP |
| Total | 30 |
Invitations were sent to key informants requesting participation in the study and explaining the objectives through a participant information sheet. Interviews were conducted in Arabic or English by bilingual researchers. Interviews were recorded and transcribed into English for analysis. Thematic analysis was adopted, which consisted of (a) familiarization with the information collected, (b) data coding and indexing of information, (c) grouping and categorizing by themes, (d) labelling and (e) writing of the results. Key‐informant perceptions on predictors of CF were grouped under three categories showing the strength of the factors perceived to affect CF practices (Table 2).
TABLE 2.
Perceived predictors of complementary feeding practices and alignment with results from national household surveys (where applicable)
| Factor/qualitative interview themes | Egypt | Jordan | SoP | Sudan | Lebanon | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Perceptionc | In line with multivariable analysis?a | Perceptionc | In line with multivariable analysis?a | Perceptionc | In line with multivariable analysis?a | Perceptionc | In line with multivariable analysis?a | Perceptionc | In line with multivariable analysis?a | ||
| Lack of awareness among mothers | +++ | Data not available for MMD, MMF and MAD | +++ | Data not available for MMD, MMF and MAD | ++ | Data not available for MMD, MMF and MAD | +++ | Data not available for MMD, MMF and MAD | ++ | Data not available for MMD, MMF and MAD | |
| Maternal level | Nutritional status of mother | — | n/ab | ++ | n/ab | — | n/ab | — | n/ab | — | n/ab |
| Educational status of mother | + | Higher maternal education significantly associated with better MDD, MMF and MAD | ++ | Higher maternal education significantly associated with better MDD, MMF and MAD except amongst SRJ | — | Higher maternal education was significantly associated with better MDD, MMF and MAD | ++ | Higher maternal education significantly associated with better MDD, MMF and MAD | — | Higher maternal education not significantly associated with feeding indicators | |
| Early marriage/ young mother | + | Higher maternal age was significantly associated with better MDD and MMF | — | Higher maternal age was significantly associated with better MDD | — | Higher maternal age was significantly associated with better MDD | +++ | Higher maternal age was significantly associated with better MDD | — | Maternal age was not significantly associated with feeding indicators | |
| Household level | Influence of mother in law, mother, father, other family members or caretakers | +++ |
Higher paternal education significantly associated with higher MMF |
+++ |
Higher paternal education significantly associated with higher MDD and MAD. |
+++ | Higher paternal education significantly associated with higher MDD and MAD. | +++ | Higher paternal education significantly associated with higher MDD and MAD. | +++ | Higher paternal education was not significantly associated with higher MDD and MAD. |
| Households where the husband or someone else decides on access to health care did not have lower odds of feeding indicators | Households where the husband or someone else decides on access to health care had lower odds of feeding indicators amongst SRJ | Households where the husband or someone else decides on access to healthcare did not have lower odds of feeding indicators | Households where the husband or someone else decides on access to health care did not have lower odds of feeding indicators | Households where the husband or someone else decides on access to health care did not have lower odds of feeding indicators | |||||||
| Poverty affecting access to food—high cost of fruits and vegetables | +++ | Higher wealth quintile significantly positively associated with all CF indicators | ++ | Higher wealth quintile significantly positively associated with higher MAD | +++ | Higher wealth quintile significantly positively associated with all CF indicators | +++ | Higher wealth quintile significantly positively associated with all CF indicators | + | Data not available | |
| Water pollution and other WASH factors | — | Having piped water not significantly associated with meeting MMF | — | Having piped water significantly associated with meeting MMF | + | Having piped water not significantly associated with meeting MMF | +++ | Having piped water not significantly associated with meeting MMF | ++ | Having piped water significantly associated with meeting MMF | |
| Community level | Cultural beliefs, traditions, habits and peer pressure | +++ | Data not available | +++ | Data not available | ++ | Data not available | +++ | Data not available | ++ | Data not available |
| Health service utilization | Utilization of health care (presence and quality of counselling including breastfeeding counselling) | ++ | Utilization of antenatal care significantly associated with higher MDD and meeting MMF | ++ | Utilization of antenatal care not significantly associated with feeding indicators | ++ | Utilization of antenatal care not significantly associated with feeding indicators | ++ | Utilization of antenatal care significantly associated with MDD | ++ | Data not available |
| Policy level | Country policies related to marketing of BMS and maternity protection | — | Data not available | — | Data not available | — | Data not available | — | Data not available | + | Data not available |
Similar colour between ‘perception’ and ‘in line with multivariable analysis’ indicates aligned results between qualitative interviews and multivariable analysis.
Nutritional status was part of bivariate not multivariable analysis.
Strength of perception.
Strong perceived relation with CF practices (mentioned by many/most informants).
Medium perceived relation with CF practices (mentioned by some informants).
Weak perceived relation with CF practices (rarely mentioned).
Not mentioned or not perceived as a factor.
2.4. Quantitative analysis of household surveys
We analysed data from nationally representative household surveys in the five selected countries: Egypt (2014), Jordan (2017–2018), Lebanon (2016), SoP (2014) and Sudan (2015) (Table 1). We retrieved the most recent Multiple Indicator Cluster Survey (MICS) or Demographic Household Survey (DHS) from each country. For Lebanon, a recent MICS—like survey conducted by UNICEF (referred to as the UNICEF Baseline Survey)—was used (Table 1). MICS and DHS surveys are nationally representative household surveys that include household and individual level data. The surveys all used a multistage stratified cluster sampling design. In Jordan and Lebanon, refugee populations were treated as separate subpopulations with different sampling frames, and data were therefore presented separately. In total, nine data sets were analysed including Egypt, Jordan, Syrian refugees in Jordan (SRJ), SoP, Sudan, Lebanon, Palestinian refugees in Lebanon (PRL), Palestinian refugees from Syria living in Lebanon (PRSL) and Syrian refugees in Lebanon (SRL) (Table 1).
2.4.1. Data accessibility statement
DHS data sets for Egypt and Jordan are derived from https://dhsprogram.com. MICS data sets for Sudan and SoP are derived from http://mics.unicef.org. The UNICEF Baseline survey data set for Lebanon was requested from UNICEF Lebanon. Data requests for this survey need to be addressed to UNICEF Lebanon.
2.5. CF indicators and predictor variables
The three main CF indicators used are MDD, minimum meal frequency (MMF) and MAD based on the WHO indicators for assessing IYCF practices (WHO, 2010) and relevant subsequent reports (UNICEF, WHO, FANTA, USAID, 2017). See Appendix B for definitions of the indicators.
For each of the household surveys, potential predictor variables were selected based on the literature and frameworks (CDC, 2016; UNICEF, 1990, 2020; WHO, 2018) in addition to findings from key‐informant interviews when data were available. At the child level, the following characteristics were included: child gender, child age and diarrheal illness. At the maternal level, maternal age, education and whether the mother is working were included. At the household level, we considered paternal education, health care decision, sex of head of household, wealth quintiles, water and sanitation characteristics and number of children under 5. At the health service utilization level, antenatal clinic visits and vitamin A supplementation were included to describe utilization of maternal child nutrition services.
Some variables were missing from certain household surveys and were therefore excluded from the analysis (see Appendix C for a list of indicators available per country).
2.6. Statistical analysis
The prevalence of CF practices for 6‐ to 23‐month‐old children was estimated for each country and subpopulation and adjusted for sampling weights. CF indicators were disaggregated by age (6–8, 9–11, 12–17 and 18–23 months), breastfeeding status and subnational geographic region. The association between various potential correlates and CF indicators (MDD, MMF and MAD) was examined. Variables that were associated with CF in bivariate analysis with a p value less than 0.20 were included in the multivariable logistic regression model. We present the data in different multivariable logistic regression models, focusing on child level, mother level, household level, health service utilization level and community level predictors. Multicollinearity was tested in the multivariable model. To avoid collinearity, variance inflation factors (VIFs) analysis was conducted on predictor variables. In the final models, none of the predictor variable had a VIFs greater than five. All models were adjusted for the complex sampling design and household clustering of children. Values of p < 0.05 were considered significant for all tests. Analyses were conducted on Stata 15.0 (StataCorp, College Station, TX, USA). To visualize the prevalence of CF indicators in different governorates and examine community level CF, we used online ArcGIS.
2.7. Ethical considerations
Ethical approval was granted from the UNICEF Ethics Review Board.
3. RESULTS
3.1. CF practices
Survey data and qualitative interviews showed that diets of infants and young children in the CF period in the MENA region did not fully meet recommendations.
Data from the analysis of the household surveys are presented in Figure 1 and show suboptimal feeding practices in all five countries including refugee population groups in Jordan and Lebanon. The lowest proportion of children meeting the MDD was found in Sudan (24%) and among SRL (22%). Higher proportions of children met MDD in PRL (42%) with the highest proportion meeting MDD in SoP (almost 50%). For all countries, MDD was less than 50%. Findings were similar for the overall quality of the diet as illustrated by MAD, whereby lowest proportions were seen in Lebanon and SRL (both 13%) and highest in the SoP (35%). Again, the proportion of children aged 6–23 months meeting MAD did not reach 50% in any of the countries.
FIGURE 1.
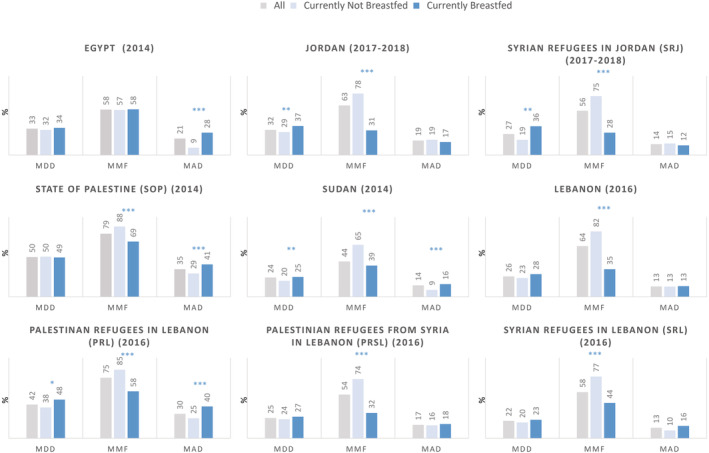
Complementary feeding indicators in five countries in the MENA region (children aged 6–23 months) (*p < 0.05, **p < 0.01 and ***p < 0.001). MAD, minimum acceptable diet; MDD, minimum dietary diversity; MMF, minimum meal frequency
Despite availability of fruits and vegetables and a diverse array of foods in the Middle‐Eastern diet, qualitative data highlighted that interviewees perceived that diets of infants and young children in the CF period were not diverse.
There are poor feeding habits practiced by mothers … lack of variety… although our food is rich in nutrients (MoH representative—Lebanon)
Interviewees highlighted that some children were fed foods that may not be age appropriate (such as raw meat). The consistency of the food provided may also be inappropriate, with some children fed a full liquid diet using infant feeding bottles on one end or others receiving full solid food as first foods. Foods may be introduced before the recommended age of 6 months or much later.
The bottle is the way to go, if the child has the bottle the mother is free. But the food will be blended (MoH representative—SoP)
Infants who are breastfed had better or similar MDD as nonbreastfed infants in all countries (Figure 1): the difference was significant in Jordan, Sudan, SRJ and PRSL. Similarly, infants who are breastfed had better or similar MAD in all countries, with significantly better MAD in Egypt, Lebanon, SoP, Sudan and among refugees. These findings were expected as both MDD and MAD scores account for breast milk. On the other hand, there was an inverse association with MMF in Egypt, SoP, Sudan and among PRL and PRSL.
3.2. Predictors of CF practices
Predictors of CF practices were examined at various levels including at the individual (maternal and child), household, community, health service (utilization) and policy levels by triangulating data obtained from the key‐informant interviews (Table 2) and the adjusted odds ratio (OR) for predictors of CF indicators in the multivariable multilevel models (Table 3).
TABLE 3.
Perceived predictors of complementary feeding practices and alignment with results from national household surveys (where applicable)
| Egypt (2014) | Jordan (2017–2018) | State of Palestine (SoP) (2014) | Sudan (2014) | Lebanon (2016) | Palestinian refugees in Lebanon (PRL) (2016) | Palestinian refugees from Syria in Lebanon (PRSL) (2016) | Syrian refugees in Lebanon (SRL) (2016) | Syrian refugees in Jordan (SRJ) (2017–2018) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MDD (No/Yes) | OR | (95%CI) | p value | OR | (95%CI) | p value | OR | (95%CI) | p value | OR | (95%CI) | p value | OR | (95%CI) | p value | OR | (95%CI) | p value | OR | (95%CI) | p value | OR | (95%CI) | p value | OR | (95%CI) | p value | |
| Child characteristics | N | 5100 | 2387 | 2325 | 4009 | 1247 | 483 | 224 | 530 | 488 | ||||||||||||||||||
| Child gender | ||||||||||||||||||||||||||||
| Female | 1.01 | [0.88, 1.17] | 0.81 | [0.62, 1.06] | 0.87 | [0.73, 1.04] | 0.98 | [0.81, 1.19] | 0.47 | [0.23, 0.97] | 0.94 | [0.64, 1.38] | 0.94 | [0.50, 1.77] | 0.70 | [0.41, 1.20] | 1.31 | [0.66, 2.60] | ||||||||||
| Child age | ||||||||||||||||||||||||||||
| 9–11 months | 2.76 | [2.07, 3.66] | *** | 2.17 | [1.25, 3.78] | ** | 2.56 | [1.86, 3.54] | *** | 3.35 | [2.25, 4.99] | *** | 1.21 | [0.27, 5.45] | 4.14 | [1.70, 10.08] | ** | 5.88 | [1.38, 25.06] | * | 12.66 | [1.89, 84.74] | ** | 2.36 | [0.59, 9.44] | |||
| 12–17 months | 4.46 | [3.47, 5.74] | *** | 3.53 | [2.15, 5.79] | *** | 4.11 | [3.11, 5.43] | *** | 4.21 | [2.94, 6.02] | *** | 5.42 | [1.91, 15.32] | ** | 5.45 | [2.45, 12.14] | *** | 4.09 | [1.11, 14.98] | * | 29.12 | [5.65, 150.02] | *** | 3.52 | [0.98, 12.62] | ||
| 18–23 months | 5.15 | [4.02, 6.61] | *** | 4.56 | [2.78, 7.48] | *** | 4.59 | [3.48, 6.06] | *** | 3.86 | [2.70, 5.51] | *** | 3.28 | [1.25, 8.63] | * | 6.92 | [3.10, 15.45] | *** | 7.37 | [1.97, 27.51] | ** | 23.73 | [4.57, 123.27] | *** | 2.77 | [0.75, 10.28] | ||
| Illness (diarrhoea) | ||||||||||||||||||||||||||||
| Yes | 0.78 | [0.65, 0.93] | ** | 1.14 | [0.80, 1.63] | 0.73 | [0.58, 0.92] | ** | 0.97 | [0.80, 1.18] | 0.79 | [0.28, 2.24] | 0.53 | [0.33, 0.84] | ** | 0.75 | [0.34, 1.65] | 0.38 | [0.15, 0.98] | 1.51 | [0.64, 3.58] | |||||||
| Maternal characteristics | N | 5131 | 2394 | 2322 | 4017 | 1238 | 478 | 222 | 523 | 490 | ||||||||||||||||||
| Maternal age | 1.02 | [1, 1.03] | * | 1.05 | [1.03, 1.08] | *** | 1.03 | [1.02, 1.05] | *** | 1.02 | [1.00, 1.03] | * | 1.00 | [0.95, 1.06] | 0.99 | [0.96, 1.02] | 1.01 | [0.96, 1.06] | 1.03 | [0.98, 1.08] | 1.00 | [0.95, 1.05] | ||||||
| Maternal education | ||||||||||||||||||||||||||||
| Secondary | 1.24 | [1.04, 1.48] | * | 3.05 | [1.60, 5.82] | ** | 1.45 | [1.16, 1.81] | ** | 3.25 | [2.53, 4.16] | *** | 2.00 | [0.75, 5.32] | 1.66 | [1.04, 2.65] | * | 1.35 | [0.57, 3.18] | 0.94 | [0.52, 1.68] | 1.71 | [0.77, 3.81] | |||||
| Higher | 1.37 | [1.09, 1.71] | ** | 2.54 | [1.31, 4.92] | ** | 2.50 | [2.01, 3.1] | *** | 3.96 | [2.83, 5.54] | *** | 2.27 | [0.81, 6.31] | 1.93 | [0.95, 3.89] | 2.02 | [0.52, 7.78] | ||||||||||
| Mother working (yes) | 1.18 | [0.94, 1.46] | 0.65 | [0.40, 1.06] | 0.84 | [0.26, 2.64] | ||||||||||||||||||||||
| Household characteristics | N | 4742 | 2249 | 2288 | 2398 | 1206 | 461 | 195 | 481 | 452 | ||||||||||||||||||
| Paternal education | ||||||||||||||||||||||||||||
| Secondary | 1.19 | [0.99, 1.43] | 1.98 | [1.16, 3.38] | * | 1.12 | [0.90, 1.38] | 1.53 | [1.16, 2.01] | ** | 0.83 | [0.38, 1.80] | 1.27 | [0.84, 1.94] | 0.72 | [0.34, 1.51] | 0.99 | [0.53, 1.87] | 1.02 | [0.49, 2.10] | ||||||||
| Higher | 1.10 | [0.86, 1.4] | 2.24 | [1.25, 4.04] | ** | 1.47 | [1.18, 1.83] | *** | 1.70 | [1.15, 2.50] | ** | 1.04 | [0.38, 2.87] | 2.08 | [0.97, 4.47] | 0.85 | [0.18, 3.99] | 1.55 | [0.32, 7.60] | 1.57 | [0.56, 4.36] | |||||||
| Health care decision | ||||||||||||||||||||||||||||
| Respondent & Husband/partner/someone else | 1.14 | [0.93, 1.41] | 1.15 | [0.81, 1.64] | 0.30 | [0.14, 0.63] | ** | |||||||||||||||||||||
| Husband/partner/someone else | 0.92 | [0.71, 1.19] | 1.02 | [0.59, 1.77] | 0.10 | [0.03, 0.30] | *** | |||||||||||||||||||||
| Sex of head of household | ||||||||||||||||||||||||||||
| Female | 0.60 | [0.36, 1.02] | 2.41 | [0.57, 10.14] | 0.81 | [0.37, 1.78] | 1.05 | [0.38, 2.84] | 0.10 | [0.01, 0.99] | 2.03 | [0.52, 7.92] | 1.35 | [0.41, 4.47] | 0.55 | [0.16, 1.83] | 0.49 | [0.16, 1.56] | ||||||||||
| Wealth quintiles | ||||||||||||||||||||||||||||
| Poorer | 1.21 | [0.95, 1.54] | 0.96 | [0.64, 1.44] | 1.26 | [0.96, 1.67] | 1.42 | [0.83, 2.42] | 1.02 | [0.32, 3.26] | ||||||||||||||||||
| Middle | 1.24 | [0.97, 1.58] | 1.46 | [0.98, 2.18] | 2.21 | [1.52, 3.22] | *** | 2.08 | [1.28, 3.35] | ** | 0.61 | [0.19, 2.02] | ||||||||||||||||
| Richer | 1.27 | [1.00, 1.62] | * | 1.09 | [0.71, 1.66] | 2.67 | [1.79, 3.98] | *** | 3.02 | [1.90, 4.78] | *** | 1.01 | [0.36, 2.80] | |||||||||||||||
| Richest | 1.40 | [1.09, 1.79] | ** | 0.91 | [0.56, 1.47] | 3.21 | [2.11, 4.89] | *** | 5.56 | [3.39, 9.14] | *** | 1.06 | [0.34, 3.28] | |||||||||||||||
| Sharing toilet (yes) | 0.95 | [0.55, 1.42] | 0.83 | [0.34, 2.02] | 0.70 | [0.36, 1.34] | 0.79 | [0.59, 1.04] | 2.40 | [0.48, 11.94] | 1.54 | [0.39, 6.03] | 1.55 | [0.69, 3.50] | 2.04 | [1.1, 3.78] | * | 1.09 | [0.47, 2.5] | |||||||||
| Water piped (yes) | 1.11 | [0.86, 1.47] | 0.87 | [0.65, 1.15] | 1.36 | [0.99, 1.86] | 1.21 | [0.91, 1.61] | 0.91 | [0.44, 1.92] | 0.97 | [0.61, 1.55] | 0.98 | [0.34, 2.86] | 1.15 | [0.60, 2.20] | 0.53 | [0.27, 1.03] | ||||||||||
| Number of children under 5 | 0.94 | [0.84, 1.04] | 0.76 | [0.61, 0.95] | * | 0.94 | [0.84, 1.04] | 1.04 | [0.89, 1.22] | 1.33 | [0.87, 2.03] | 0.83 | [0.61, 1.13] | 0.73 | [0.52, 1.04] | 0.98 | [0.73, 1.32] | 0.69 | [0.48, 1.00] | * | ||||||||
| Utilization of health services | N | 5035 | 2122 | 2296 | 319 | 431 | ||||||||||||||||||||||
| Antenatal clinic visits 4 times or more | 1.21 | [1.00, 1.48] | * | 0.84 | [0.51, 1.40] | 1.47 | [0.87, 2.48] | 1.51 | [1.2, 1.91] | *** | 1.76 | [0.47, 6.65] | ||||||||||||||||
| Received vit A supplementation in past 6 months | 1.54 | [1.30, 1.83] | *** | 1.90 | [1.40, 2.59] | *** | 2.28 | [1.02, 5.06] | * | |||||||||||||||||||
| MMF (no/yes) | ||||||||||||||||||||||||||||
| Child characteristics | N | 5087 | 2327 | 2317 | 3849 | 1245 | 482 | 224 | 529 | 463 | ||||||||||||||||||
| Child gender | ||||||||||||||||||||||||||||
| Female | 0.88 | [0.77, 1.00] | 0.95 | [0.74, 1.22] | 0.99 | [0.80, 1.21] | 1.00 | [0.84, 1.19] | 1.04 | [0.57, 1.92] | 1.03 | [0.67, 1.59] | 1.07 | [0.62, 1.84] | 1.38 | [0.89, 2.12] | 1.02 | [0.57, 1.83] | ||||||||||
| Child age | ||||||||||||||||||||||||||||
| 9–11 months | 0.69 | [0.55, 0.86] | ** | 0.97 | [0.63, 1.48] | 0.78 | [0.56, 1.08] | 0.87 | [0.65, 1.17] | 1.08 | [0.45, 2.62] | 1.50 | [0.68, 3.35] | 1.31 | [0.48, 3.61] | 1.13 | [0.51, 2.48] | 0.93 | [0.33, 2.59] | |||||||||
| 12–17 months | 0.88 | [0.72, 1.06] | 1.59 | [1.09, 2.32] | * | 1.37 | [1.02, 1.85] | * | 1.18 | [0.92, 1.52] | 1.50 | [0.66, 3.42] | 1.43 | [0.75, 2.72] | 1.56 | [0.72, 3.38] | 2.52 | [1.29, 4.92] | ** | 1.20 | [0.53, 2.69] | |||||||
| 18–23 months | 0.92 | [0.76, 1.11] | 1.73 | [1.20, 2.50] | ** | 1.71 | [1.26, 2.31] | ** | 1.47 | [1.13, 1.91] | ** | 2.36 | [1.21, 4.58] | * | 2.47 | [1.27, 4.80] | ** | 1.91 | [0.82, 4.43] | 2.80 | [1.42, 5.53] | ** | 1.27 | [0.56, 2.88] | ||||
| Illness (diarrhoea) | ||||||||||||||||||||||||||||
| Yes | 0.84 | [0.72, 0.99] | * | 1.46 | [1.02, 2.1] | * | 0.88 | [0.68, 1.15] | 0.72 | [0.60, 0.87] | ** | 0.55 | [0.21, 1.04] | 0.53 | [0.33, 0.86] | * | 1.48 | [0.78, 2.80] | 1.08 | [0.60, 1.93] | 0.83 | [0.38, 1.80] | ||||||
| Maternal characteristics | N | 5117 | 2334 | 2314 | 3856 | 1236 | 477 | 222 | 522 | 465 | ||||||||||||||||||
| Maternal age | 1.01 | [1.00, 1.03] | * | 1.01 | [0.99, 1.03] | 1.01 | [0.99, 1.03] | 1.01 | [0.99, 1.02] | 1.05 | [1.00, 1.10] | 0.97 | [0.94, 1.01] | 1.00 | [0.95, 1.04] | 0.98 | [0.95, 1.01] | 0.99 | [0.94, 1.03] | |||||||||
| Maternal education | ||||||||||||||||||||||||||||
| Secondary | 1.36 | [1.16, 1.6] | *** | 1.87 | [1.05, 3.36] | * | 1.34 | [1.03, 1.74] | * | 1.43 | [1.14, 1.81] | ** | 1.03 | [0.44, 2.39] | 1.34 | [0.80, 2.25] | 2.37 | [1.17, 4.82] | * | 0.86 | [0.56, 1.31] | 1.17 | [0.56, 2.46] | |||||
| Higher | 1.69 | [1.36, 2.1] | *** | 2.20 | [1.21, 3.98] | ** | 1.94 | [1.48, 2.53] | *** | 1.87 | [1.31, 2.67] | ** | 1.05 | [0.43, 2.59] | 2.35 | [0.97, 5.64] | 0.38 | [0.12, 1.20] | ||||||||||
| Mother working (yes) | 1.07 | [0.86, 1.34] | 1.78 | [1.10, 2.88] | * | 0.66 | [0.23, 1.88] | |||||||||||||||||||||
| Household characteristics | N | 4727 | 2194 | 2280 | 2302 | 1205 | 460 | 195 | 481 | 431 | ||||||||||||||||||
| Paternal education | ||||||||||||||||||||||||||||
| Secondary | 1.16 | [0.98, 1.37] | 1.43 | [0.84, 2.44] | 1.11 | [0.86, 1.42] | 1.10 | [0.83, 1.45] | 1.66 | [0.89, 3.09] | 1.22 | [0.76, 1.95] | 1.98 | [1.02, 3.83] | * | 1.04 | [0.65, 1.65] | 1.37 | [0.69, 2.70] | |||||||||
| Higher | 1.33 | [1.05, 1.67] | * | 1.45 | [0.81, 2.59] | 1.62 | [1.23, 2.12] | ** | 1.23 | [0.82, 1.83] | 1.18 | [0.52, 2.65] | 4.09 | [1.16, 14.46] | * | 2.02 | [0.50, 8.18] | 0.20 | [0.05, 0.85] | * | 0.46 | [0.15, 1.41] | ||||||
| Health care decision | ||||||||||||||||||||||||||||
| Respondent & Husband/partner/someone else | 0.93 | [0.76, 1.14] | 0.82 | [0.58, 1.14] | 0.83 | [0.69, 2.70] | ||||||||||||||||||||||
| Husband/partner/someone else | 0.79 | [0.62, 1.01] | 0.62 | [0.37, 1.05] | 0.99 | [0.15, 1.41] | ||||||||||||||||||||||
| Sex of head of household | ||||||||||||||||||||||||||||
| Female | 0.98 | [0.62, 1.54] | 1.42 | [0.34, 5.97] | 2.41 | [0.72, 8.06] | 0.52 | [0.22, 1.19] | 0.49 | [0.06, 3.96] | 1.30 | [0.26, 6.54] | 0.65 | [0.22, 1.90] | 0.72 | [0.24, 2.16] | 1.08 | [0.40, 2.90] | ||||||||||
| Wealth quintiles | ||||||||||||||||||||||||||||
| Poorer | 1.29 | [1.03, 1.61] | * | 0.77 | [0.53, 1.11] | 1.30 | [0.93, 1.81] | 0.93 | [0.62, 1.41] | 0.39 | [0.13, 1.13] | |||||||||||||||||
| Middle | 1.46 | [1.17, 1.82] | ** | 1.27 | [0.85, 1.88] | 1.28 | [0.80, 2.06] | 1.54 | [1.04, 2.28] | * | 1.28 | [0.46, 3.57] | ||||||||||||||||
| Richer | 1.46 | [1.17, 1.82] | ** | 1.01 | [0.67, 1.51] | 2.11 | [1.27, 3.48] | ** | 1.42 | [0.96, 2.10] | 0.37 | [0.15, 0.90] | * | |||||||||||||||
| Richest | 1.64 | [1.30, 2.07] | *** | 1.02 | [0.65, 1.61] | 1.90 | [1.14, 3.19] | * | 1.55 | [1.00, 2.4] | * | 0.86 | [0.29,2.56] | |||||||||||||||
| Sharing toilet (yes) | 0.72 | [0.47, 1.11] | 0.92 | [0.36, 2.35] | 1.03 | [0.47, 2.23] | 1.05 | [0.80, 1.38] | 0.81 | [0.18, 3.67] | 2.07 | [0.29, 14.71] | 0.63 | [0.30, 1.31] | 1.64 | [0.95, 2.82] | 1.45 | [0.78, 2.71] | ||||||||||
| Water piped (yes) | 0.80 | [0.62, 1.02] | 1.34 | [1.01, 1.76] | * | 1.23 | [0.82, 1.83] | 0.96 | [0.72, 1.28] | 2.58 | [1.44, 4.64] | ** | 1.86 | [1.12, 3.07] | * | 0.83 | [0.34, 1.99] | 1.21 | [0.75, 1.95] | 0.99 | [0.53, 1.81] | |||||||
| Number of children under 5 | 0.84 | [0.76, 0.92] | *** | 0.80 | [0.66, 0.98] | 0.96 | [0.84, 1.09] | 0.93 | [0.80, 1.09] | 0.74 | [0.50, 1.09] | 0.74 | [0.52, 1.05] | 0.96 | [0.67, 1.37] | 0.83 | [0.64, 1.08] | 0.89 | [0.65, 1.21] | |||||||||
| Utilization of health services | N | 5024 | 2064 | 2288 | 3064 | 407 | ||||||||||||||||||||||
| Antenatal clinic visits four times or more | 1.29 | [1.08, 1.54] | ** | 1.25 | [0.77, 2.03] | 1.30 | [0.71, 2.35] | 1.09 | [0.89, 1.34] | 1.07 | [0.42, 2.73] | |||||||||||||||||
| Received vit A supplementation in past 6 months | 1.29 | [1.09, 1.53] | ** | 1.59 | [1.16, 2.18] | ** | 1.48 | [0.71, 3.08] | ||||||||||||||||||||
| MAD | ||||||||||||||||||||||||||||
| Child characteristics | N | 5084 | 2326 | 2317 | 3849 | 1245 | 482 | 224 | 529 | 463 | ||||||||||||||||||
| Child gender | ||||||||||||||||||||||||||||
| Female | 0.99 | [0.84, 1.16] | 0.77 | [0.55, 1.08] | 0.80 | [0.67, 0.95] | * | 0.95 | [0.76, 1.20] | 0.63 | [0.31, 1.29] | 1.25 | [0.83, 1.88] | 0.54 | [0.26, 1.15] | 0.67 | [0.34, 1.32] | 3.04 | [1.27, 7.26] | * | ||||||||
| Child age | ||||||||||||||||||||||||||||
| 9–11 months | 2.02 | [1.50, 2.70] | *** | 1.85 | [0.87, 3.95] | 1.78 | [1.27, 2.49] | ** | 2.56 | [1.61, 4.06] | *** | 0.30 | [0.08, 1.15] | 2.71 | [1.05, 7.01] | * | 4.23 | [0.74, 24.28] | 16.52 | [1.59, 172.10] | * | 1.28 | [0.15, 11.09] | |||||
| 12–17 months | 2.63 | [2.03, 3.41] | *** | 3.50 | [1.79, 6.83] | *** | 2.69 | [2.02, 3.58] | *** | 3.09 | [2.03, 4.72] | *** | 2.10 | [0.73, 6.02] | 3.67 | [1.58, 8.56] | ** | 3.91 | [0.82, 18.51] | 63.62 | [8.29, 488.50] | *** | 4.06 | [0.92, 17.82] | ||||
| 18–23 months | 1.70 | [1.31, 2.22] | *** | 5.69 | [2.92, 11.06] | *** | 2.03 | [1.53, 2.70] | *** | 2.68 | [1.76, 4.06] | *** | 3.29 | [1.15, 9.37] | * | 4.27 | [1.83, 9.94] | ** | 5.68 | [1.23, 26.14] | * | 56.64 | [7.34, 437.12] | *** | 2.25 | [0.46,11.02] | ||
| Illness (diarrhoea) | ||||||||||||||||||||||||||||
| Yes | 0.73 | [0.60, 0.90] | ** | 1.74 | [1.13, 2.67] | 0.65 | [0.51, 0.83] | *** | 0.74 | [0.58, 0.94] | 0.38 | [0.15, 0.95] | * | 0.64 | [0.39, 1.05] | 0.70 | [0.29, 1.69] | 0.16 | [0.05, 0.55] | ** | 1.31 | [0.32,5.36] | ||||||
| Maternal characteristics | N | 5114 | 2333 | 2314 | 3856 | 1236 | 477 | 222 | 522 | 465 | ||||||||||||||||||
| Maternal age | 1.01 | [1.00, 1.03] | 1.04 | [1.01, 1.07] | ** | 1.03 | [1.02, 1.05] | *** | 1.01 | [0.99, 1.02] | 1.04 | [0.97, 1.11] | 1.00 | [0.97, 1.03] | 1.03 | [0.97, 1.09] | 1.01 | [0.97, 1.06] | 0.95 | [0.89, 1.01] | ||||||||
| Maternal education | ||||||||||||||||||||||||||||
| Secondary | 1.07 | [0.87, 1.30] | 2.73 | [1.12, 6.67] | * | 1.46 | [1.14, 1.86] | ** | 2.60 | [1.97, 3.44] | *** | 1.29 | [0.51, 3.27] | 1.54 | [0.93, 2.55] | 1.66 | [0.58, 4.72] | 0.90 | [0.45, 1.78] | 1.95 | [0.65, 5.88] | |||||||
| Higher | 1.30 | [1.01, 1.67] | * | 2.54 | [1.01, 6.36] | * | 2.48 | [1.97, 3.12] | *** | 3.77 | [2.55, 5.56] | *** | 1.93 | [0.69, 5.39] | 1.80 | [0.86, 3.77] | 0.36 | [0.07, 1.81] | ||||||||||
| Mother working (yes) | 1.04 | [0.81, 1.33] | 1.06 | [0.61, 1.85] | 1.47 | [0.20, 10.75] | ||||||||||||||||||||||
| Household characteristics | N | 4727 | 2193 | 2280 | 2302 | 1205 | 460 | 195 | 481 | 431 | ||||||||||||||||||
| Paternal education | ||||||||||||||||||||||||||||
| Secondary | 1.06 | [0.86, 1.30] | 1.76 | [0.88, 3.50] | 1.24 | [0.99, 1.56] | 1.47 | [1.08, 1.99] | * | 1.23 | [0.50, 2.98] | 1.14 | [0.73, 1.79] | 1.05 | [0.45, 2.49] | 1.07 | [0.50, 2.29] | 1.40 | [0.48, 4.06] | |||||||||
| Higher | 1.09 | [0.83, 1.43] | 2.57 | [1.21, 5.43] | * | 1.94 | [1.55, 2.42] | *** | 1.68 | [1.10, 2.58] | * | 1.11 | [0.31, 3.96] | 2.39 | [1.10, 5.21] | * | 1.87 | [0.38, 9.23] | 0.72 | [0.11, 4.84] | 0.88 | [0.21, 3.62] | ||||||
| Health care decision | ||||||||||||||||||||||||||||
| Respondent & Husband/partner/someone else | 1.14 | [0.90, 1.45] | 1.12 | [0.73, 1.72] | 0.26 | [0.09, 0.74] | * | |||||||||||||||||||||
| Husband/partner/someone else | 0.86 | [0.64, 1.16] | 0.53 | [0.24, 1.14] | 0.07 | [0.02, 0.29] | *** | |||||||||||||||||||||
| Sex of head of household | ||||||||||||||||||||||||||||
| Female | 0.59 | [0.31, 1.10] | 1.33 | [0.16, 11.23] | 0.80 | [0.36, 1.76] | 0.61 | [0.10, 3.8] | 0.18 | [0.02, 1.96] | 0.67 | [0.13, 3.47] | 1.60 | [0.48, 5.32] | 0.47 | [0.16, 1.39] | 1.16 | [0.29,4.68] | ||||||||||
| Wealth quintiles | ||||||||||||||||||||||||||||
| Poorer | 1.13 | [0.85, 1.50] | 0.84 | [0.49, 1.43] | 1.18 | [0.87, 1.60] | 1.45 | [0.69, 3.06] | 1.04 | [0.21, 5.13] | ||||||||||||||||||
| Middle | 1.24 | [0.94, 1.64] | 1.72 | [1.05, 2.80] | * | 1.59 | [1.07, 2.36] | * | 2.21 | [1.12, 4.34] | * | 1.47 | [0.28, 7.55] | |||||||||||||||
| Richer | 1.24 | [0.94, 1.63] | 1.08 | [0.63, 1.86] | 2.23 | [1.47, 3.38] | *** | 3.12 | [1.67, 5.83] | *** | 0.75 | [0.18, 3.17] | ||||||||||||||||
| Richest | 1.42 | [1.07, 1.89] | * | 1.05 | [0.58, 1.89] | 2.63 | [1.72, 4.02] | *** | 4.88 | [2.58, 9.23] | *** | 1.14 | [0.20, 6.58] | |||||||||||||||
| Sharing toilet (yes) | 0.92 | [0.51, 1.66] | 0.43 | [0.17, 1.10] | 0.61 | [0.27, 1.34] | 0.78 | [0.56, 1.09] | 0.74 | [0.17, 3.08] | 1.29 | [0.30, 5.51] | 1.35 | [0.56, 3.29] | 2.11 | [1.01, 4.39] | * | 1.70 | [0.62, 4.61] | |||||||||
| Water piped (yes) | 0.86 | [0.64, 1.16] | 0.75 | [0.52, 1.08] | 1.18 | [0.86, 1.62] | 1.31 | [0.98, 1.74] | 2.20 | [1.08, 4.50] | * | 1.00 | [0.60, 1.65] | 1.11 | [0.34, 3.68] | 1.51 | [0.60, 3.78] | 0.70 | [0.26, 1.88] | |||||||||
| Number of children under 5 | 1.01 | [0.9, 1.14] | 0.76 | [0.56, 1.02] | 0.90 | [0.81, 1.00] | * | 1.04 | [0.87, 1.24] | 1.11 | [0.61, 2.03] | 0.92 | [0.67, 1.28] | 0.73 | [0.47, 1.12] | 0.99 | [0.67, 1.45] | 0.76 | [0.44, 1.29] | |||||||||
| Utilization of health services | N | 5021 | 2063 | 2288 | 3064 | 407 | ||||||||||||||||||||||
| Antenatal clinic visits four times or more | 1.23 | [0.98, 1.54] | 0.91 | [0.46, 1.80] | 1.33 | [0.76, 2.34] | 1.24 | [0.94, 1.65] | 1.01 | [0.20, 5.16] | ||||||||||||||||||
| Received vit A supplementation in past 6 months | 1.47 | [1.21, 1.77] | *** | 2.00 | [1.37, 2.90] | *** | 6.16 | [2.32, 16.33] | *** | |||||||||||||||||||
Note: Grey cells indicate data not available.
p < 0.05.
p < 0.01.
p < 0.001.
3.3. Factors at the individual level
In the multivariable child level model, gender of the child was not associated with poor CF practices, whereas child age was significantly associated with all three CF indicators. Compared with children aged 6–8 months, older children were significantly more likely to meet the minimum CF indicators (Table 3).
Children whose mothers reported diarrheal illness in the child in the 2 weeks prior to the surveys were associated with lower odds of meeting all minimum CF indicators in Egypt (OR = 0.78 for MDD, OR = 0.84 for MMF, and OR = 0.73 for MAD), MMF in Sudan (OR = 0.72), and among PRL (OR = 0.53), and MAD in various settings (Table 3).
Although key informants did not report on any child level factors, maternal factors were perceived to affect CF practices, and these were mostly in line with data from household surveys (Table 2).
In the maternal level multivariable model, higher maternal education was significantly associated with better MDD, MMF and MAD indicators in all countries except for Lebanon and among refugees (PRL, PRSL, SRL and SRJ) (Table 3). In Jordan only, we noted an association between working mothers and higher MMF (OR = 1.78) (Table 3). There was no association in Egypt, and data on mother's work status were not available in Lebanon, SoP or Sudan.
Higher maternal age was significantly associated with meeting MDD in Egypt (OR = 1.02), Jordan (OR = 1.05), SoP (OR = 1.03) and Sudan (OR = 1.02) but not in Lebanon or among refugees (PRL, PRSL, SRL and SRJ) (Table 3). This is aligned with interviewees' reports (Table 2) that younger mothers lacked the experience and relied on their own mothers and mothers‐in‐law who themselves did not have the appropriate knowledge related to CF. Yet, quantitatively, age at first marriage was not associated with any CF indicator (data not shown), despite interviewees relating early marriage to a mother's educational status and awareness about care for children including nutrition. Particularly in Sudan, there was a strong perceived relation between early marriage/young mothers and CF practices (Table 2). Maternal knowledge and awareness was perceived to be a factor driven by several other existing factors such as social support systems and available health and nutrition services. Interviewees highlighted the role of mothers and their knowledge in shaping a child's diet. There was a strong perceived relation in almost all countries (Table 2).
The main cause of poor complementary feeding is really the lack of knowledge amongst mothers (MoH representative—Jordan)
3.4. Factors at the household level
In the multivariable household level model, paternal education, health care decision, sex of head of household, wealth quintiles, sharing toilet, piped water supply and number of children under 5 were included as predictors of CF. Children whose father had secondary or higher education as compared with primary were associated with higher odds of meeting MDD (in Jordan OR = 2.24, SoP OR = 1.47 and Sudan OR = 1.70), MMF (in Egypt OR = 1.33, SoP OR = 1.62 and PRL OR = 4.09) and MAD (in Jordan OR = 2.57, SoP OR = 1.94, Sudan OR = 1.68 and PRL OR = 2.39). Data on decision making were available in Egypt and Jordan, and we note that children living in households where the husband or someone else decides on access to health care had lower odds of meeting MDD and MAD indicators among SRJ (Table 3). Qualitatively, grandmothers, mothers‐in‐law, fathers, sisters and other caregivers were all mentioned by key informants as affecting feeding practices and maternal choice when it comes to providing food for infants and young children. There was a strong perceived relation in all countries (Table 2).
There is prevalent wrong information that is linked to poor habits … it comes from the traditional way of thinking … and the power of the “teta” [grandmother] and mother‐in‐law. Even if the mother is educated (MoH representative—Egypt)
In Lebanon, the role of the ‘house maid’ was emphasized as affecting feeding practices where mothers relied on the helper to feed the baby. Often from a different nationality, the latter would feed the child according to her own culture.
Higher wealth quintile was significantly positively associated with meeting all CF indicators in most countries (except for MMF and MDD in Jordan). Data were not available in Lebanon (Table 3). The strength of the association varied between countries with the strongest associations found in SoP (OR = 3.21) and Sudan (OR = 5.56). In the latter countries, interviewees emphasized that food security and socio‐economic status were key determinants of feeding practices. The high cost of fruits and vegetables and families' limited access to healthier options were perceived as affecting the choice of families and mothers in terms of what to feed their infants (Table 2—strong perceived relation with CF in Egypt, Sop and Sudan).
Various fruits and vegetables are available for consumption, but food diversity for infants and children is not part of [our] feeding culture. The fruits and vegetables that are grown are often sold (NGO representative—Sudan)
Fruits and vegetables have high prices—1 kg of Tomato is 10 gneh [Egyptian pounds] and vegetables are seasonal—the problem is with access to fruits and vegetables (NGO representative—Egypt)
In Jordan and Lebanon, socio‐economic status and cost of food were perceived to be less important (Table 2) while acknowledging that in some pockets and areas within the countries, these factors continue to play a role.
Having piped water was only significantly associated with meeting MMF in Jordan (OR = 1.34), Lebanon (OR = 2.58), and among PRL (OR = 1.86), and MAD in Lebanon (OR = 2.20) (Table 3). Although the role of water pollution in feeding practices was mainly mentioned in Lebanon, water quality was reported to be an issue in SoP and Sudan (Table 2). Key informants highlighted that often the lack of clean water affects the choice of the food and makes it difficult for families to clean the food before giving it to children.
3.5. Factors at the community level
Regional analyses within countries representing multiple communities and cultures showed intracountry inequities in the percentage of children aged 6–23 months who achieved CF indicators (Figure 2). For example, in Egypt, children in Upper Egypt had significantly lower CF indicators (MDD 31%, MMF 52% and MAD 20%) than children in the urban governorate (MDD 36%, MMF 67% and MAD 26%). In SoP, the percentage of children achieving MDD (57%) and MAD (40%) in the West Bank was significantly higher than in Gaza (MDD 42% and MAD 29%). In Sudan, children in Sinnar, Kassala, Kordofan and Darfur had significantly lower MDD (26%, 23%, 21% and 12%, respectively) than children in Merowe (42%). In Lebanon, children in South/Nabatieh had significantly lower MDD (16%) than those in Beirut/Mount Lebanon (32%). Similarly, qualitative data showed that feeding practices differ starkly by geographical or administrative regions and by urban/rural location. There are prevalent cultural and geographic disparities leading to diversity in practices with suboptimal practices more prevalent in rural areas. In Egypt and Sudan, this difference was highlighted further, and reference was made to tribal communities that have very specific cultural practices and may lack the appropriate knowledge. Different population groups were described to have distinct practices that affect CF practices, specifically those in urban areas. There was a strong perceived relation between cultural beliefs and traditions with CF practices (Table 2).
FIGURE 2.
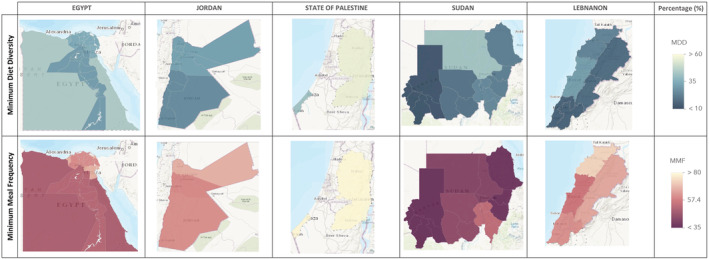
Percentage of children aged 6–23 months that achieve MDD and MMF at different subregional levels in Egypt, Jordan, SoP, Sudan and Lebanon. Darker colours represent lower percentage of children meeting MDD and MMF scores reflecting poorer feeding practices. MDD, minimum dietary diversity; MMF, minimum meal frequency
Sudan is extremely diverse in terms of culture and situation. There are pockets that are completely isolated from the rest of the country. (UN agency representative—Sudan)
3.6. Factors at the health service level (utilization)
In the multivariable heath utilization level model, antenatal clinic visits (four times or more) and receipt of vitamin A supplementation in the past 6 months were used as predictors of CF to reflect on utilization of health care. Where data were available (Egypt, Jordan and SRJ), vitamin A supplementation was significantly associated with meeting all three CF indicators (Table 3).
Utilization of antenatal care was significantly positively associated with MDD in Egypt (OR = 1.21) and Sudan (OR = 1.51) (Table 3). Adequate pre‐ and post‐natal counselling and education on breastfeeding was perceived by interviewees to impact CF practices as the latter are often dictated by the breastfeeding journey in the first 6 months of life (Table 2—medium perceived relation in all countries).
It starts with problems with breastfeeding and mothers have difficulties with breastfeeding … She starts introducing food, and the problem of … solid food persists until 5 years. (NGO representative—Sudan)
3.7. Factors at the policy level
This level was only analysed qualitatively. Qualitative data showed gaps in programmes and policies supporting CF including lack of human resources equipped to provide adequate counselling, lack of public awareness, limited access to counselling services and gaps in policy implementation. These were thought to play a role in improving knowledge and awareness of mothers and therefore affecting feeding choices and care practices. Particularly, in Lebanon and SoP, gaps in implementation of policies related to the marketing of breast milk substitutes (BMS) and maternity protection were perceived to affect feeding practices (Table 2).
4. DISCUSSION
We examined CF practices and their predictors using key informant interviews and nationally representative data in five countries in the MENA region in addition to refugee populations in Jordan and Lebanon.
Overall, results show that CF practices in the five selected countries do not meet the recommendations with the percentage of children meeting their MDD ranging from 22% among SRL to almost 50% in SoP. For most countries, these are first time measurements of CF indicators, and therefore, trend analysis was not possible. The only previous data available was for Jordan showing no improvement in CF indicators (Department of Statistics [Jordan] and ICF International, 2012). These results highlight the need for interventions to improve CF practices in the countries under study. The analysis of correlates of CF indicators can inform the targeting of such interventions.
Data from both the qualitative and the quantitative components of this study show that most factors that predict CF practices were at the individual, household and health service utilization levels. These findings are also aligned with evidence from other regions (Abdurahman et al., 2019; Dhami et al., 2019; Senarath et al., 2012).
We found the youngest children (aged 6–8 months) to have significantly lower CF indicators than older children in line with other studies indicating the older the child, the better the feeding indicators (Na, Aguayo, Arimond, Dahal, et al., 2018; Na, Aguayo, Arimond, Narayan, et al., 2018) and recommending the potential need to prioritize young children who are at higher risk of not being fed appropriately. It is likely that cultural beliefs relating to appropriateness of introduction of different types of foods at different ages play a role in the delayed introduction of a more diverse diet in this region (Issaka et al., 2015; Manikam, Prasad, et al., 2018; Manikam, Sharmila, et al., 2018). Cultural factors are also likely to influence what children are fed when ill. Diarrheal illness was found to be a predictor of lower CF indicators among nationals in Egypt, Jordan, Lebanon and SoP but not for PRSL and SRJ. Possible explanations include that refugee populations benefit from various health promotion activities and access to assistance including primary care (Akik et al., 2019).
There also appears to be a role for breastfeeding in determining CF indicators. We found breastfed infants to have significantly higher MDD in Jordan, Sudan and among SRJ compared with nonbreastfed. Bortolini et al. (2019) showed that in Brazil, breastfed infants were almost five times more likely to have a diverse diet and 19% less likely to consume foods rich in sugar fat, and salt than nonbreastfed infants. At the same time, our findings showed that breastfed infants seem to have significantly lower MMF than nonbreastfed infants in all countries including refugees except for Egypt. This can possibly be because breastfed infants feed frequently on the breast. Despite this difference in MMF, breastfed infants continued to show significantly higher MAD in Egypt, SoP and Sudan and among PRL and PRSL indicating that MMF did not have a great effect on the overall quality of the diet among breastfed.
At the maternal level, education was found to predict the diets of infants and young children aged 6–23 months in all countries except for Lebanon and most refugee populations. Although key informant interviews did not specify educational attainment as a factor, awareness was highlighted as a significant contributing factor. Other studies found similar results in relation to maternal education and child feeding practices both in the region and globally (Abdurahman et al., 2019; El‐Gilany & Abdel‐Hady, 2014; El Shafei & Labib, 2014; Issaka et al., 2015; Kandeel et al., 2018; Manikam et al., 2017; Manikam, Prasad, et al., 2018; Manikam, Sharmila, et al., 2018; Musmar & Qanadeelu, 2012; Na, Aguayo, Arimond, Dahal, et al., 2018; Na, Aguayo, Arimond, Narayan, et al., 2018; Reinbott & Jordan, 2016). For example, in Egypt, maternal education was significantly associated with early introduction of solids (El Shafei & Labib, 2014) as well as prelacteal feeds (El‐Gilany & Abdel‐Hady, 2014). Age of the mother was also found to be a determining factor. In India, Dhami et al. (2019) found that children of mothers aged 35–49 years had higher odds of meeting MDD than younger mothers. It is therefore important to direct awareness and education programmes towards less educated and young mothers to improve CF practices.
At household level, the influence of household members, specifically mothers and mothers in law, and husbands were highlighted in interviews and data from the household surveys. The role of paternal education in child feeding is consistent with other similar studies (Abdurahman et al., 2019; Manikam, Sharmila, et al., 2018; Na, Aguayo, Arimond, Mustaphi, et al., 2018). At the same time, children in households where the husband or someone else other than the mother decides on access to health care had lower indicators in populations where these data were available is also consistent with other studies (Temesgen et al., 2018). The influence of household members on feeding practices has been confirmed in a KAP study in Egypt showing older people were considered the main source of knowledge on child care, especially grandmothers, and their knowledge is greatly respected (UNICEF & MoHP, 2019). Similarly, in Sudan, grandmothers were reported to be the major influencers for decisions on feeding, and other relatives were an important source of information for CF. Although feeding practices mainly depend on the mother, programmes that adopt innovative approaches to engage key influencers such as fathers and grandmothers may play an important role in improving CF practices (Dinga et al., 2018; Mukuria et al., 2016).
Poverty, food insecurity and socio‐economic status are major predictors for CF as highlighted by key informants and confirmed by the quantitative analysis and the literature (Dhami et al., 2019; Na, Aguayo, Arimond, Narayan, et al., 2018; Reinbott & Jordan, 2016). Data were not available for Lebanon; however, for all other countries, it is apparent that there is a need to improve the livelihood and the living conditions of vulnerable and at‐risk families thus contributing to improving the diets of infants and young children. The rise in cost of fruits and vegetables has been reported to affect household access to food and purchasing power (Kavle et al., 2015). Specifically, it was reported that maternal food choice is driven by affordability as well as food preferences and perceived appropriateness of food for consumption during a certain stage (pregnancy for example) (Kavle et al., 2018). An individual study in Egypt showed that in rural areas, farm households purchase most of their foods rather than consume what they produce and given the high cost of fruits, vegetables and meat, they end up consuming lower nutritional value items (El‐Enbaby et al., 2019). One indicator of socio‐economic status includes access to water and quality of sanitation. In Lebanon and Jordan specifically, having piped water positively predicted MMF showing the poor living conditions can also contribute to poor feeding.
For predictors of CF at the community level, we considered geographical location to be a proxy of different cultural beliefs and practices and found significant variability in feeding practices by geography. The analysis of household surveys showed that remote and rural areas, where most traditional and tribal communities reside and where, as indicated by key informants, it is likely that most myths and misconceptions prevail, had significantly lower CF indicators. Practices in urban areas, namely, the capital, were in most cases better. For each of these areas and within each country, there is a need for tailored interventions that tackle prevailing ill practices related to feeding of infants and young children aged 6–23 months.
When examining predictors at the health service, utilization of antenatal care and breastfeeding counselling were found to predict CF practices in Egypt and Sudan. No survey data were available for Lebanon, yet qualitative data showed that access to counselling and education was perceived to be a contributing factor in all countries. Similar findings were reported in other countries. In Ethiopia, a systematic review showed that the presence of antenatal care follow‐up during pregnancy was significantly associated with child dietary diversity (Temesgen et al., 2018). In Burkina Faso, a facility‐based counselling programme had a positive impact on CF practices (Manikam et al. (2017). Breastfeeding issues were also perceived as contributing to poorer CF practices. In Egypt, Kavle et al. (2015) showed that prelacteal feeding is an entry point to the early introduction of junk foods and is a traditional remedy for perceived insufficient breast milk (Kavle et al., 2015). Also, in rural Egypt, lactation problems were significantly correlated with early introduction of solids (Kavle et al., 2015). There is therefore a need for programmes that integrate counselling for both breastfeeding and CF for mothers and caregivers in order to address IYCF comprehensively.
At the policy level, there was not enough variability in policy provisions between countries to explain CF practices. The only country that had fully enacted the Code of Marketing of Breastmilk Substitutes (WHO, 1981) was Lebanon, although feeding indicators in Lebanon were the poorest. This may be partially attributed to the poor implementation of the Code (Akik et al., 2017). Similarly, only Jordan has fully achieved the WHO recommendations for restricting marketing of foods and non‐alcoholic beverages to children. There is therefore a need to ensure that plans and policies specifically related to diets of infants and young children aged 6–23 months are well developed, implemented, monitored and evaluated to contribute to improving CF practices.
The main implications of this study relate to the need for supporting programmatic and policy interventions to improve CF practices in the selected countries. Interventions should address gaps in predictors of CF including behaviour change interventions and education for mothers, improving access to counselling on breastfeeding and CF, social support and access to food, and policy change.
4.1. Strengths and limitations
The study is the first to provide a comprehensive analysis of CF indicators and their predictors in the region. In particular, the study combines both qualitative and quantitative data providing richness to the findings by triangulating both sources of information where available. The multivariable analysis of household surveys included information not only related to nationals but also relevant to refugee populations. The advantage of using MICS and DHS data sets includes the comparability across countries using the same survey and a standard methodology of data collection of country representative data. However, our analysis is limited by the cross‐sectional nature of the data and thus our inability to determine cause and effect and look at time trends. Another limitation is the lack of data on other possible predictors of CF for example: antenatal care and wealth indicators were not available for Lebanon. A key limitation in the triangulation of qualitative and quantitative results is that we were unable to triangulate factors mentioned by key informants that were not measured by the surveys (such as at the policy level) (Table 2).
5. CONCLUSION
In conclusion, this assessment revealed that poor CF practices are affecting more than half of the infants and young children aged 6–23 months in five countries of the MENA region. Factors affecting feeding practices include those related to maternal education and wealth as well as cultural and geographic factors that need to be addressed. There is a need to improve programmatic interventions providing mothers and families with children under 2 years of age with access to education, social support, and counselling on IYCF including breastfeeding and CF.
CONFLICTS OF INTEREST
The authors declare no conflict of interest. The authors alone are responsible for the views expressed in this publication, and they do not necessarily represent the decisions, policy or views of UNICEF.
CONTRIBUTIONS
LSB conceptualized study design, conducted qualitative data collection and analysis and prepared first draft of the manuscript. VT provided technical support on study design and contributed to manuscript review. CA provided technical support on study design, analysis of qualitative data and contributed to interpretation, and manuscript review. ZJ conducted the quantitative analysis of household surveys and contributed to interpretation and manuscript review. HG provided technical support on study design and analysis and contributed to interpretation, and manuscript review.
ACKNOWLDGMENTS
This work was commissioned by UNICEF Regional Office for the Middle East and North Africa with support from UNICEF/HQ. The authors wish to thank Aashima Garg, Jessica White and Kendra Siekmans Nutrition Specialists from UNICEF/HQ along with Nadine Nasser and Sarah Zahr, who helped with data extraction and analysis and Elsie Abou Diwan who conducted key informant interviews in Sudan.
APPENDIX A.
TABLE A1.
Nutritional status indicators for each of the five countries
| Indicator data source (years) | Egypt (LMIC) DHS (2014) | Jordan (UMIC) DHS (2017) | SoP (LMIC) MICS (2014) | Sudan (LMIC) MICS (2014) | Lebanon (UMIC) UNICEF Baseline Survey 2016 |
|---|---|---|---|---|---|
| Low birth weight | 15.5% | 16.7% | 8.3% | 32.3% | 9.5% |
| Stunting | 21.0% | 7.7% | 7.4% | 38.2% | N/A |
| Wasting | 8.0% | 2.4% | 1.2% | 16.3% | N/A |
| Overweight | 14.9% | 4.4% | 8.2% | 3.0% | N/A |
| Anaemia | 27.2% | 32.0% | N/A | N/A | N/A |
Abbreviations: LMIC, low‐ and middle‐income country; UMIC, upper middle‐income country.
APPENDIX B.
TABLE B1.
Definitions of complementary feeding indicators
| Complementary feeding indicators | 6–8 months | 9–23 months |
|---|---|---|
| Minimum dietary diversity | Number of children who received food from a ≥ 5 out of 8 food groups in the past day (UNICEF et al., 2017) | |
| Minimum meal frequency | ||
| Breastfed | Number of children who received solid, semi‐solid or soft foods ≥2 times during the past day. | Number of children who received solid, semi‐solid or soft foods ≥3 times during the past day. |
| Not breastfed | Number of children who received solid, semi‐solid or soft foods and milk feeds b ≥ 4 times during the past day. | Number of children who received solid, semi‐solid or soft foods and milk feeds b ≥ 4 times during the past day. |
| Minimum acceptable diet | ||
| Breastfed | Number of children who received food from a ≥ 5 out of 8 food groups AND who received solid, semi‐solid, or soft foods ≥2 times during the past day. | Number of children who received food from a ≥ 5 out of 8 food groups AND who received solid, semi‐solid, or soft foods ≥3 times during the past day. |
| Not breastfed | Number of children who received food from c ≥ 5 out of 8 food groups AND milk feed b ≥ 2, AND who received solid, semi‐solid, or soft foods and milk feed b ≥ 4 times during the past day. | Number of children who received food from c ≥ 5 out of 8 food groups AND milk feed b ≥ 2, AND who received solid, semi‐solid, or soft foods and milk feed b ≥ 4 times during the past day. |
Note: Table adapted from Na, Aguayo, Arimond, Dahal, et al. (2018), World Health Organization (2021).
Food group score is calculated based on consumption of eight food groups, breastmilk, grains, roots and tubers, legumes nuts, dairy products, flesh foods, eggs, vitamin A‐rich fruits and vegetables, and other fruits and vegetables.
Milk feeds are consumption of infant formula, milk such as tinned, powdered or fresh animal milk, and yogurt.
For this food group, score is calculated based on consumption of six food groups, excluding dairy products.
APPENDIX C.
TABLE C1.
List of indicators and descriptive table of subjects' characteristics
| Egypt | Jordan | State of Palestine (SoP) | Sudan | Lebanon | PRL | PRS | SRL | SRJ | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | 2014 | 2017–2018 | 2014 | 2014 | 2016 | 2016 | 2016 | 2016 | 2017–2018 | |
| Child characteristics | N | 5,205 | 2,441 | 2,326 | 4,064 | 1,252 | 484 | 224 | 532 | 500 |
| Child gender (%) | ||||||||||
| Male | 52.4 | 53.9 | 51.7 | 51.4 | 55.6 | 51.9 | 52.7 | 56.1 | 49.6 | |
| Female | 47.6 | 46.1 | 48.3 | 48.6 | 44.4 | 48.1 | 47.3 | 43.9 | 50.4 | |
| N | 5205 | 2441 | 2326 | 4064 | 1252 | 484 | 224 | 532 | 500 | |
| Child age (%) | ||||||||||
| 6–8 months | 19.2 | 17.9 | 18.8 | 19.8 | 16.8 | 13.7 | 17.8 | 13.6 | 18.7 | |
| 9–11 months | 17.0 | 18.4 | 15.6 | 15.3 | 17.2 | 16.8 | 12.2 | 15.0 | 17.7 | |
| 12–17 months | 31.7 | 30.1 | 33.1 | 36.1 | 38.9 | 35.5 | 39.9 | 35.0 | 32.9 | |
| 18–23 months | 32.2 | 33.6 | 32.5 | 28.8 | 27.1 | 34.0 | 30.1 | 36.4 | 30.8 | |
| N | 5106 | 2390 | 2326 | 4032 | 1247 | 483 | 224 | 530 | 488 | |
| Child had diarrhoea symptoms in the past 2 weeks (%) | 22.6 | 16.1 | 18.9 | 39.0 | 23.2 | 23.5 | 28.5 | 16.2 | 15.5 | |
| Maternal characteristics | N | 5205 | 2441 | 2323 | 4045 | 1240 | 479 | 222 | 523 | 500 |
| Maternal age (mean ± SE) | 28.5 ± 0.0 | 30.9 ± 0.1 | 29.2 ± 0.1 | 29.9 ± 0.1 | 29.6 ± 0.1 | 30.3 ± 0.1 | 28.6 ± 0.2 | 28.1 ± 0.1 | 28.2 ± 0.2 | |
| N | 5205 | 2441 | 2326 | 4061 | 1250 | 483 | 224 | 532 | 500 | |
| Maternal education (%) | ||||||||||
| Basic/intermediate | 23.4 | 3.8 | 27.3 | 74.2 | 27.6 | 24.2 | 20.3 | 60.4 | 71.6 | |
| Secondary | 59.0 | 50.4 | 34.5 | 17.8 | 47.4 | 65.4 | 74.5 | 36.6 | 20.8 | |
| Higher | 17.6 | 45.8 | 38.1 | 8.0 | 25.0 | 10.4 | 5.2 | 3.1 | 7.6 | |
| N | 5205 | 2434 | 500 | |||||||
| Mother working (%) | ||||||||||
| Yes | 12.4 | 13.1 | 1.9 | |||||||
| No | 87.6 | 86.9 | 98.1 | |||||||
| Household characteristics | N | 5204 | 2422 | 2294 | 3548 | 1209 | 461 | 195 | 481 | 495 |
| Paternal education (%) | ||||||||||
| Basic/intermediate | 23.6 | 6.6 | 38.2 | 71.8 | 41.8 | 36.4 | 28.7 | 62.1 | 33.9 | |
| Secondary | 58.7 | 59.7 | 30.3 | 20.9 | 36.6 | 56.4 | 66.5 | 35.6 | 55.8 | |
| Higher | 17.7 | 33.7 | 31.4 | 7.3 | 21.5 | 7.2 | 4.8 | 2.3 | 10.3 | |
| N | 5137 | 2423 | 496 | |||||||
| Women own health care decision (%) | ||||||||||
| Respondent alone | 14.4 | 22.2 | 28.1 | |||||||
| Respondent & husband/partner/someone else | 67.0 | 69.2 | 54.5 | |||||||
| Husband/partner/someone else | 18.6 | 8.6 | 17.4 | |||||||
| N | 5205 | 2441 | 2326 | 4064 | 1252 | 484 | 224 | 532 | 500 | |
| Sex of head of household (%) | ||||||||||
| Male | 96.2 | 97.5 | 97.6 | 91.1 | 98.0 | 95.7 | 83.9 | 87.4 | 89.8 | |
| Female | 3.8 | 2.5 | 2.4 | 8.9 | 2.0 | 4.3 | 16.1 | 12.6 | 10.2 | |
| N | 4873 | 2304 | 2326 | 4041 | 467 | |||||
| Wealth quintiles (%) | ||||||||||
| Poorest | 18.2 | 20.0 | 25.5 | 19.5 | 18.3 | |||||
| Poorer | 19.3 | 21.0 | 19.2 | 18.0 | 18.1 | |||||
| Middle | 19.3 | 18.7 | 19.8 | 21.1 | 23.7 | |||||
| Richer | 21.8 | 20.4 | 20.1 | 21.1 | 18.6 | |||||
| Richest | 21.4 | 19.9 | 15.4 | 20.4 | 21.4 | |||||
| N | 4878 | 2304 | 2320 | 2772 | 1249 | 484 | 224 | 532 | 467 | |
| Sharing toilet (%) | 2.4 | 2.0 | 1.9 | 25.4 | 1.8 | 3.2 | 21.4 | 18.2 | 11.5 | |
| N | 4882 | 2304 | 2326 | 4058 | 1252 | 484 | 224 | 532 | 467 | |
| Water piped (%) | 90.2 | 51.5 | 52.6 | 33.4 | 40.4 | 24.3 | 13.0 | 35.4 | 48.0 | |
| N | 5205.0 | 2441.0 | 2326.0 | 4064.0 | 1252.0 | 484.0 | 224.0 | 532.0 | 500.0 | |
| Number of children under 5 (mean ± SE) | 1.68 ± 0.01 | 1.68 ± 0.01 | 1.97 ± 0.01 | 1.92 ± 0.01 | 1.57 ± 0.01 | 1.61 ± 0.02 | 1.81 ± 0.03 | 1.92 ± 0.02 | 2.15 ± 0.03 | |
| Utilization of health services | N | 5186 | 2189 | 2297 | 3205 | 447 | ||||
| Antenatal clinic visits four times or more (%) | 84.1 | 93.4 | 96.9 | 65.5 | 88.6 | |||||
| N | 5059 | 2363 | 483 | |||||||
| Received Vit. A supplementation in past 6 months (%) | 79.8 | 71.6 | 74.3 | |||||||
Shaker‐Berbari, L., Qahoush Tyler, V., Akik, C., Jamaluddine, Z., & Ghattas, H. (2021). Predictors of complementary feeding practices among children aged 6–23 months in five countries in the Middle East and North Africa region. Maternal & Child Nutrition, 17(4), e13223. 10.1111/mcn.13223
Contributor Information
Linda Shaker‐Berbari, Email: linda.shaker.berbari@gmail.com.
Chaza Akik, Email: ca36@aub.edu.lb.
Hala Ghattas, Email: hg15@au.edu.lb.
REFERENCES
- Abdurahman, A. A., Chaka, E. E., Bule, M. H., & Niaz, K. (2019). Magnitude and determinants of complementary feeding practices in Ethiopia: A systematic review and meta‐analysis. Heliyon, 5(7), e01865. 10.1016/j.heliyon.2019.e01865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adair, L. S., Fall, C. H., Osmond, C., Stein, A. D., Martorell, R., Ramirez‐Zea, M., Sachdev, H. S., Dahly, D. L., Bas, I., Norris, S. A., & Micklesfield, L. (2013). Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: Findings from five birth cohort studies. The Lancet, 382(9891), 525–534. 10.1016/S0140-6736(13)60103-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aitsi‐Selmi, A. (2015). Households with a stunted child and obese mother: Trends and child feeding practices in a middle‐income country, 1992‐2008. Maternal & Child Health Journal, 19(6), 1284–1291. 10.1007/s10995-014-1634-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akik, C., Ghattas, H., Filteau, S., & Knai, C. (2017). Barriers to breastfeeding in Lebanon: A policy analysis. Journal of Public Health Policy, 38(3), 314–326. [DOI] [PubMed] [Google Scholar]
- Akik, C., Ghattas, H., Mesmar, S., Rabkin, M., El‐Sadr, W. M., & Fouad, F. M. (2019). Host country responses to non‐communicable diseases amongst Syrian refugees: A review. Conflict and Health, 13(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta, Z. A., Das, J. K., Rizvi, A., Gaffey, M. F., Walker, N., Horton, S., Webb, P., Lartey, A., Black, R. E., Group, T. L., & Maternal and Child Nutrition Study Group . (2013). Evidence‐based interventions for improvement of maternal and child nutrition: What can be done and at what cost? The Lancet, 382(9890), 452–477. 10.1016/S0140-6736(13)60996-4 [DOI] [PubMed] [Google Scholar]
- Bortolini, G. A., Giugliani, E. R. J., Gubert, M. B., & Santos, L. M. P. (2019). Breastfeeding is associated with children's dietary diversity in Brazil. Ciência & Saúde Coletiva, 24, 4345–4354. 10.1590/1413-812320182411.29312017 [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention (CDC) . (2016). The social ecological model: A framework for prevention. [online] Available at: http://www.cdc.gov/violenceprevention/overview/socialecologicalmodel
- Danaei, G., Andrews, K. G., Sudfeld, C. R., Fink, G., McCoy, D. C., Peet, E., Sania, A., Smith Fawzi, M. C., Ezzati, M., & Fawzi, W. W. (2016). Risk factors for childhood stunting in 137 developing countries: A comparative risk assessment analysis at global, regional, and country levels. PLoS Medicine, 13(11), e1002164. 10.1371/journal.pmed.1002164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Statistics [Jordan] and ICF International . (2012). Jordan population and family health survey 2012. Calverton, Maryland, USA: Department of Statistics and ICF International. [Google Scholar]
- Development Initiatives . (2020). 2020 global nutrition report: Action on equity to end malnutrition. Bristol, UK: Development Initiatives. [Google Scholar]
- Dhami, M. V., Ogbo, F. A., Osuagwu, U. L., & Agho, K. E. (2019). Prevalence and factors associated with complementary feeding practices among children aged 6–23 months in India: A regional analysis. BMC Public Health, 19(1), 1034. 10.1186/s12889-019-7360-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinga, L. A., Kiage, B. N., & Kyallo, F. M. (2018). Effect of paternal education about complementary feeding of infants in Kisumu county, Kenya. African Journal of Food, Agriculture, Nutrition and Development, 18(3), 13702–13716. [Google Scholar]
- El Kishawi, R. R., Soo, K. L., Abed, Y. A., & Wan Muda, W. A. (2016). Prevalence and associated factors for dual form of malnutrition in mother‐child pairs at the same household in the Gaza Strip‐Palestine. PLoS ONE [Electronic Resource], 11(3), e0151494. 10.1371/journal.pone.0151494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Shafei, A. M., & Labib, J. R. (2014). Determinants of exclusive breastfeeding and introduction of complementary foods in rural Egyptian communities. Global Journal of Health Science, 6(4), 236–244. 10.5539/gjhs.v6n4p236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El‐Enbaby, H., Ecker, O., Figueroa, J. L., Leroy, J. L., & Breisinger, C. (2019). Characteristics of smallholder farm households in Upper Egypt: Implications for nutrition‐sensitive agricultural interventions (Vol. 20). Intl Food Policy Res Inst. [Google Scholar]
- El‐Gilany, A. H., & Abdel‐Hady, D. M. (2014). Newborn first feed and prelacteal feeds in Mansoura, Egypt. BioMed Research International, 2014, 258470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO , IFAD , UNICEF , WFP , & WHO . (2020). The State of Food Security and Nutrition in the World 2020. Transforming food systems for affordable healthy diets. Rome, FAO. 10.4060/ca9692en [DOI]
- Ghattas, H., Acharya, Y., Jamaluddine, Z., Assi, M., El Asmar, K., & Jones, A. D. (2020. Apr). Child‐level double burden of malnutrition in the MENA and LAC regions: Prevalence and social determinants. Maternal & Child Nutrition, 16(2), e12923. 10.1111/mcn.12923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Issaka, A. I., Agho, K. E., Burns, P., Page, A., & Dibley, M. J. (2015). Determinants of inadequate complementary feeding practices among children aged 6–23 months in Ghana. Public Health Nutrition, 18(4), 669–678. 10.1017/S1368980014000834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandeel, W. A., Rabah, T. M., Zeid, D. A., El‐Din, E. M. S., Metwally, A. M., Shaalan, A., El Etreby, L. A., & Shaaban, S. Y. (2018). Determinants of exclusive breastfeeding in a sample of Egyptian infants. Open Access Macedonian Journal of Medical Sciences, 6(10), 1818–1823. 10.3889/oamjms.2018.359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavle, J. A., El‐Zanaty, F., Landry, M., & Galloway, R. (2015). The rise in stunting in relation to avian influenza and food consumption patterns in Lower Egypt in comparison to Upper Egypt: Results from 2005 and 2008 Demographic and Health Surveys. BMC Public Health, 15, 285. 10.1186/s12889-015-1627-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavle, J. A., Mehanna, S., Khan, G., Hassan, M., Saleh, G., & Engmann, C. (2018). Program considerations for integration of nutrition and family planning: Beliefs around maternal diet and breastfeeding within the context of the nutrition transition in Egypt. Maternal & Child Nutrition, 14(1), e12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manikam, L., Prasad, A., Dharmaratnam, A., Moen, C., Robinson, A., Light, A., Ahmed, S., Lingam, R., & Lakhanpaul, M. (2018). Systematic review of infant and young child complementary feeding practices in South Asian families: The India perspective. Public Health Nutrition, 21(4), 637–654. 10.1017/S136898001700297X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manikam, L., Robinson, A., Kuah, J. Y., Vaidya, H. J., Alexander, E. C., Miller, G. W., Singh, K. K., Dawe, V., Ahmed, S., Lingam, R., & Lakhanpaul, M. (2017). A systematic review of complementary feeding practices in South Asian infants and young children: The Bangladesh perspective. BMC Nutrition, 3(1), 56. 10.1186/s40795-017-0176-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manikam, L., Sharmila, A., Dharmaratnam, A., Alexander, E. C., Kuah, J. Y., Prasad, A., Ahmed, S., Lingam, R., & Lakhanpaul, M. (2018). Systematic review of infant and young child complementary feeding practices in South Asian families: The Pakistan perspective. Public Health Nutrition, 21(4), 655–668. 10.1017/S1368980017002956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukuria, A. G., Martin, S. L., Egondi, T., Bingham, A., & Thuita, F. M. (2016). Role of social support in improving infant feeding practices in western Kenya: A quasi‐experimental study. Global Health: Science and Practice, 4(1), 55–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musmar, S. G., & Qanadeelu, S. (2012). Breastfeeding patterns among Palestinian infants in the first 6 months in Nablus refugee camps: Cross‐sectional study. Journal of Human Lactation, 28(2), 196–202. 10.1177/0890334411432715 [DOI] [PubMed] [Google Scholar]
- Na, M., Aguayo, V. M., Arimond, M., Dahal, P., Lamichhane, B., Pokharel, R., Chitekwe, S., & Stewart, C. P. (2018). Trends and predictors of appropriate complementary feeding practices in Nepal: An analysis of national household survey data collected between 2001 and 2014. Maternal & Child Nutrition, 14, e12564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na, M., Aguayo, V. M., Arimond, M., Mustaphi, P., & Stewart, C. P. (2018). Predictors of complementary feeding practices in Afghanistan: Analysis of the 2015 Demographic and Health Survey. Maternal & Child Nutrition, 14, e12696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na, M., Aguayo, V. M., Arimond, M., Narayan, A., & Stewart, C. P. (2018). Stagnating trends in complementary feeding practices in Bangladesh: An analysis of national surveys from 2004‐2014. Maternal & Child Nutrition, 14, e12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasreddine, L., Ayoub, J. J., & Al Jawaldeh, A. (2018). Review of the nutrition situation in the Eastern Mediterranean Region. Eastern Mediterranean Health Journal, 24(1), 77–91. 10.26719/2018.24.1.77 [DOI] [PubMed] [Google Scholar]
- Reinbott, A., & Jordan, I. (2016). Determinants of child malnutrition and infant and young child feeding approaches in Cambodia. In Hidden Hunger (Vol. 115) (pp. 61–67). Chicago: Karger Publishers. [DOI] [PubMed] [Google Scholar]
- Senarath, U., Agho, K. E., Akram, D. E. S., Godakandage, S. S., Hazir, T., Jayawickrama, H., Joshi, N., Kabir, I., Khanam, M., Patel, A., Pusdekar, Y., Roy, S. K., Siriwardena, I., Tiwari, K., & Dibley, M. J. (2012). Comparisons of complementary feeding indicators and associated factors in children aged 6–23 months across five South Asian countries. Maternal & Child Nutrition, 8, 89–106. 10.1111/j.1740-8709.2011.00370.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temesgen, H., Negesse, A., Woyraw, W., & Mekonnen, N. (2018). Dietary diversity feeding practice and its associated factors among children age 6–23 months in Ethiopia from 2011 up to 2018: A systematic review and meta‐analysis. Italian Journal of Pediatrics, 44(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2020). UNICEF Programming guidance. Improving young children's diets during the complementary feeding period.
- UNICEF and MoHP . (2019). Knowledge, attitude and practices study of current practice and beliefs related to breast feeding, nutrition and weaning in five governorates.
- UNICEF , WHO , FANTA , USAID . (2017). MEETING REPORT on reconsidering, refining, and extending the World Health Organization infant and young child feeding indicators.
- United Nations Children's Fund (UNICEF) . (1990). Strategy for improved nutrition of children and women in developing countries. New York: NY, UNICEF. [DOI] [PubMed] [Google Scholar]
- United Nations Children's Fund, Division of Data Research and Policy . (2019). Global UNICEF Global Databases: Infant and young child. Minimum acceptable diet, Minimum diet diversity, Minimum meal frequency, New York.
- World Health Organization (WHO) . (2019). Strategy on nutrition for the Eastern Mediterranean Region 2020–2030. https://applications.emro.who.int/docs/9789290222996-eng.pdf?ua=1&ua=1
- World Health Organization . (2010). Indicators for assessing infant and young child feeding practices: Part 2: Measurement.
- World Health Organization (WHO) . (1981). International code of marketing of breast‐milk substitutes. Geneva.
- World Health Organization (WHO) . (2018). Nurturing care for early childhood development: A framework for helping children survive and thrive to transform health and human potential.
- World Health Organization (WHO) , & UNICEF . (2003). Global strategy for infant and young child feeding.
- World Health Organization (WHO) , United Nations Children's Fund (UNICEF) , & USAID . (2008). Indicators for assessing infant and young child feeding practices. Geneva: World Health Organization. [Google Scholar]
- World Health Organization (WHO) (2021). Indicators for assessing infant and young child feeding practices: Definitions and measurement methods, [Google Scholar]
- Wrottesley, S. V., Lamper, C., & Pisa, P. T. (2016). Review of the importance of nutrition during the first 1000 days: Maternal nutritional status and its associations with fetal growth and birth, neonatal and infant outcomes among African women. Journal of Developmental Origins of Health and Disease, 7(2), 144–162. 10.1017/S2040174415001439 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
DHS data sets for Egypt and Jordan are derived from https://dhsprogram.com. MICS data sets for Sudan and SoP are derived from http://mics.unicef.org. The UNICEF Baseline survey data set for Lebanon was requested from UNICEF Lebanon. Data requests for this survey need to be addressed to UNICEF Lebanon.


