Abstract
Prevalence of child marriage has remained high in many parts of Africa despite its multisectoral adverse effect. As it is now being suggested to have intergeneration impact, we examined if marriage at or after 18th birthday is associated with the risk of anaemia among under‐five children. Cross‐sectional data from Demographic and Health Surveys (DHS) conducted between 2010 and 2018 in 15 African countries as of August 2020 were used. Maternal age of marriage was defined as when they started living with their husband or partner. Children with haemoglobin level below 11.0 g/dl after adjustment for altitude were categorised to be anaemic. The study involved a multivariable logistic regression analysis of 17,033 children data born by women between the childbearing ages. About 65% of under‐five children in Sub‐Saharan Africa (SSA) were anaemic, ranging from 40% in Rwanda to 82% in Mali. Girl child marriage ranged from 40% in South Africa to 97% in Niger with an average of about 60%. We observed a significant reduction (20%) in the risk of anaemia among under‐five children when their mothers married after at or after their 18th birthday. Country‐specific analysis showed that increased risk of anaemia was strongly associated with early marriage in Côte d'Ivoire and Mozambique. This study contributed to the growing evidence that maternal age of marriage might have an intergenerational impact. Maternal marriage at or after their 18th birthday reduces the risk of anaemia among under‐five children in Africa. Interventions aimed at tackling anaemia in Africa should capture and affect household socioeconomic risks and children's exposures.
Keywords: anaemic, demographic health survey, girl child marriage, Sub‐Saharan Africa, under‐five mortality
Key messages.
There is growing evidence on intergenerational impact of child marriage.
The risk of anaemia among under‐five children was reduced by 16% when their mothers married at or after 18th birthday.
Child characteristic seems to have a stronger effect on the relationship. Under‐five risk of anaemia among those with mother that married early (before 18 years) was significant in Congo and Mozambique.
Beyond policy formulation and implementations targeted at high‐risk children at risk of anaemia, social problem like early marriage should be incorporated and tackle for effective and contextual solutions.
An evidenced‐based advocacy, highlighting the multiple and intergenerational impact of early marriage, should be used as tool to policymakers and community gate‐keeps in order to reduce it prevalence and impact.
1. INTRODUCTION
The unacceptably high prevalence of child marriage in more than 100 countries is well known, despite the numerous attention child marriage has received from the United Nations (UN), other international and governmental agencies since 1940s (Loaiza & Fund, 2012). One of the setbacks probably faced was the loosely defined minimum age requirement for child marriage. However, at the convention of Right of the Child held in 1987, female in formal union before the age of 18 years was recognised as child marriage (United Nation, 1989). Across all regions where this is largely practised, it is far more prevalent among girls than boys, thus reflect and justified the heightened emphasis on resolving girl child marriage at a global stage.
Girl child marriage is an ancient practice, as old as marriage institution, it cut across most cultures of the world and it is still prevalent in many countries till now (UNICEF, 2005). About 700 million currently married women entered into marriage before they were 18 years old; globally, about 39,000 girl child marriage occurs per day (Fund U. N. I. C. E, 2014). Report from some researchers and development experts has argued that despite the decline in rate in past decades, the world is seeing the greatest number of girl child bride and more are at increased risk (Fund U. N. I. C. E, 2014; Loaiza & Fund, 2012). Nevertheless, the rapid growth in population and the availability of more accurate data from recent surveys, especially in low‐ and middle‐income countries (LMICS) where these practices are pervasive (Loaiza & Fund, 2012; Nour, 2009), could be responsible for this increase.
The highest number of girl child marriage is found in South Asia; however, the higher proportion and rate is in Africa (Efevbera et al., 2019; Fund U. N. I. C. E, 2014). More recent estimates revealed that 18 of the 20 countries with the highest prevalence are in Sub‐Saharan Africa (SSA). It has also been projected that the continent will account for highest prevalence at the instance of its current population growth (Fund U. N. I. C. E, 2014; Nour, 2006). Meanwhile, girl child marriage is usually a product of deprived and unequal society, especially where gender inequalities and patriarchal norms are prevalent. More importantly, girl child marriage perpetuates vicious cycles of poverty, illiteracy, violence against women and ultimately adverse health outcomes (Dahl, 2010; Nour, 2006; Wodon et al., 2017; Yaya et al., 2019).
Being the focus of several international and funding agencies, girl child marriage and its impact are well researched. Findings from these studies have shown that it is well associated with increased family planning needs and fertility, poor utilisation of maternal and child health services and exposure to intimate partner violence and mental health (Efevbera et al., 2019; Kidman, 2016; Yaya et al., 2019). In addition to the direct associations with women's outcomes, which are usually long term in most cases, evidence on the intergenerational impact of girl child marriage is increasingly being recognised and mentioned in recent the literature (Parsons et al., 2015; Sekhri & Debnath, 2014).
Meanwhile, poor nutrition remains a big public health and development concern in developing countries. Anaemia has been recognised as the most prevailing nutritional disorder across the world, and it affects children and women more (Bailey et al., 2015; WHO, 2019). About 40% of children are estimated to be anaemic globally, and more than 65% of under‐five children in Africa are anaemic (Parbey et al., 2019; Stevens et al., 2013). The impact of this alone on health outcome in the continent cannot be overemphasised, especially in its contribution to under‐five morbidity. Medically, iron deficiency has been identified as the major cause of anaemia in developing countries, including Africa (Simo et al., 2020; WHO, 2019). Women's experiences such as menstruation and pregnancy already expose them to this disorder if not properly managed (Yaya et al., 2021; Solovyova et al., 2018). Other maternal and household socioeconomic characteristics such as illiteracy, lack of access to family planning, clean drinking water, hygiene and poverty have also been linked to risk of anaemia (Hakizimana et al., 2019; Moschovis et al., 2018). Girls who married before their 18th birthday are far more exposed to these risk factors as they are expected to step into adult roles when they ought to be learning and being catered for (UNICEF, 2019).
Applying the WHO's social determinant of health framework to the risk of anaemia in under‐five children as our outcome of interest, that girl child marriage cut across the three core domains of this framework (Benach et al., 2010). The practice of girl child marriage varies widely across developing countries today with huge resistance in ‘cultural and societal’ settings where it is perceived normal even by parents. It is also common in poorer households, hence used as means to strengthen family economic life. Finally, circumstances that affect their psychosocial and behavioural factors are linked to risk of anaemia and low the utilisation of reproductive, maternal and child health services (Seth et al., 2018; Wahyudi et al., 2019). Previous studies, though scanty, have established the existence of a relationship between maternal early marriage and health outcomes in their newborn.
In this study, we hypothesised that girl child marriage is one of the key determinants of the unacceptably high prevalence of anaemia among under‐five children, not just among newborns (Finlay et al., 2011). However, we were more interested in exploring if and the extent to which maternal marriage after their 18th birthday is associated with the risk of anaemia in the women's under‐five offspring. Due to diverse methodologies and challenges associated with missing data in surveys because blood sample is required, multi‐country analysis and comparison are scarce. In this study, we pooled data from 15 SSA countries to explore the potential association between girl child marriage and risk of anaemia among under‐five children when the child's maternal, and household factors were controlled simultaneously. Finally, we also examined different age categories of girl child marriage and its modulating effect on children's anaemic status.
2. MATERIALS AND METHODS
2.1. Data source
Data from the most recent Demographic and Health Surveys (DHS) between 2010 and 2018 were used; 15 SSA countries were involved in this study based on data availability for the outcome and key determinant variables. DHS is a multi‐country survey that involves data collection every 5 years using similar multi‐stratification cluster sampling approaches across all the countries. Data collection is done via face‐to‐face interviews of women from randomly selected households in clusters, and birth history for 5 years before the surveys year was collected from the women. Other procedures used in data collection have been published elsewhere (Rutstein & Rojas, 2006).
In this study, we used children as our unit of analysis based on the outcome variables. DHS provide a rich source of data on demographic, environmental, socioeconomic, nutritional and other health indicators at individual levels and suitable for multi‐country comparison. The 17,033 datasets from 15 SSA countries were pooled and included in our analysis. We restricted our analysis to children whose mothers were 15–24 years at the time of the survey. DHS collect data every 5 years on five previous births; therefore, older women at the time of the survey, even when they married early, would not have been able to record the birth history of their children birthed after the fifth year. More importantly, we were more interested in young mothers because of its prevalence in this group (Nour, 2006; Paul et al., 2019). The outcome variable, anaemic status, involves a random selection of under‐five children, and then blood samples were taken and assessed for their anaemic level. Therefore, we had missing data more than 10%, in the pooled dataset. Nevertheless, this type of missing data, missing at random (MAR), allows the prediction of missing values from respondents with complete values (Jakobsen et al., 2017). Therefore, we applied multiple imputation techniques to treat the missing data to prevent underestimation or overestimation in our result.
2.2. Measures
2.2.1. Anaemia
Anaemia among under‐five children is the outcome variable in this study. It was assessed using the haemoglobin level in the blood of under‐five years children after adjusting for altitude. A binary outcome was computed, following WHO's recommendation (Khusun et al., 1999; Marn & Critchley, 2016), children with haemoglobin levels below 11.0 g/dl were coded as ‘1’ and ‘0’ otherwise.
2.2.2. Girl child marriage
The main exposure of interest in this study is girl child marriage. DHS data contain information on the marital status of women and when they started living with their partner if currently married (ager and specific date). Mothers below 18 years old at first marriage were coded ‘0’, and those that married after their 18th birthday were coded as ‘1’. To test for early marital age differences, we further categories the former (<14, 14–15 and16–17 years) and compared with those that married on or after their 18th birthday.
2.2.3. Other measures
We included and controlled for various but relevant of demographic and socio‐economic variables selected based on previous and relevant studies. We removed highly correlated variables such as pregnancy intention instead of mother's anaemic status after multicollinearity test was performed. Child variables included are child's age in month (1–11, 24–25, 36‐47, 48–59), number antenatal visits (ANC) and birth weight at birth (<2500 as underweight, 2500–3500 kg as normal and >3500 kg as obese). The household variables are family structure (monogamy, polygynous and single mother) and household wealth index (poor, average and rich). Maternal characteristics included in the analysis were family planning need, mother education level, number of living children alive, mother's body mass index (BMI) (<18.5 as thin, 18.5–24.9 as normal and >25 as obese) and mother's anaemic status.
2.3. Statistical analysis
We weighted the data for each country to ensure that the data are representative and generalisability of findings. We conducted weighted descriptive analysis involving all the variables included in this study. We presented the overall estimates for each variable and stratified by children's anaemia status and finally. The descriptive test of association was assessed using Pearson's χ 2. Due to the multilevel nature of DHS survey design, we employed complex design tools, ‘svy’ command and survey package in Stata and R, respectively. The association between maternal age of marriage and risk of anaemia in their children was assessed by conducting a series of multivariable logistic regression involving four models. Model I contains child variables alone, Model II contained household‐level variables, Model III contained mother characteristic, and Model IV involved all the significant variables from all the models, simultaneously control for each other. The same model pattern was repeated for the analysis to test for the very early marital ages analysis. Finally, we computed country‐specific risk difference of the association between girl child marriage and risk of anaemia among under‐five children when all the determinants were adjusted for. We further used a map to visualise these risk difference. All analyses were using STATA, version 16 and R version 3.7.
2.4. Ethical consideration
Ethical permissions were not required for this study because we used DHS dataset, which is already publicly available.
3. RESULTS
3.1. Descriptive statistics
Data of 17,033 children born to young women between age 15 and 24 years from 15 SSA countries were used for this study. The prevalence of girl child marriage and anaemia varies among the 15 included countries, the former from 45.8% in South Africa to 90.1% in Niger with an average of about 69.5% and the later ranging from 61.6% in Uganda to 84.5% in Mali with 72.3% on the average (Table 1). Countries such as Niger, Mali and Sierra Leone showed high prevalence (above 70%) of anaemia and child marriage. Figure 1 showed the percentage distribution of anaemia across the 15 SSA countries.
TABLE 1.
Description of DHS data by countries, survey year, weighted percentage of child marriage and anaemia (with confidence interval)
| Country | Total | Child marriage (%) | Anaemic (%) |
|---|---|---|---|
| Burundi | 982 | 45.76 [41.45–50.14] | 66.67 [61.59–72.21] |
| DR Congo | 1854 | 68.87 [65.38–72.16] | 64.60 [57.96–57.96] |
| Côte d'Ivoire | 797 | 71.4 [64.78–77.21] | 79.29 [69.07‐]89.39 |
| Gabon | 1239 | 61.4 [54.41–67.95] | 67.51 [58.99–76.03] |
| Gambia | 994 | 64.47 [59.26–69.36] | 69.27 [61.33–77.34] |
| Ghana | 453 | 57.37 [50.59–63.88] | 73.55 [63.34–83.53] |
| Guinea | 789 | 81.53 [78.0–84.59] | 78.45 [71.23–85.55] |
| Malawi | 1654 | 64.54 [61.18–67.76] | 67.24 [61.79–72.75] |
| Mali | 1063 | 77.33 [73.54–80.72] | 84.56 [75.88–93.23] |
| Mozambique | 1450 | 68.88 [65.1–72.38] | 70.98 [65.00–77.02] |
| 65.95Niger | 1425 | 90.10 [87.86–92] | 65.95 [59.79–72.20] |
| Nigeria | 2092 | 74.63 [71.85–77.23] | 73.62 [68.64–78.60] |
| 73.99Sierra Leone | 1346 | 74.4 [70.58–77.88] | 73.99 [65.38–82.69] |
| 61.59Togo | 585 | 52.0 [46.0–58.05] | 75.66 [67.78–83.71] |
| Uganda | 1174 | 58.87 [54.54–63.06] | 61.59 [55.40–67.86] |
Abbreviation: DHS, Demographic and Health Surveys.
FIGURE 1.
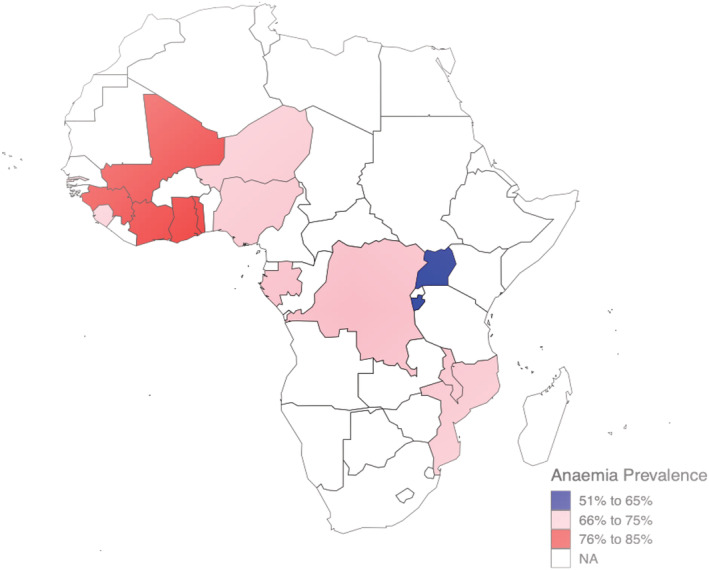
Map showing the distribution of anaemia across the 15 Sub‐Saharan Africa (SSA) countries
As shown in Table 2, more of the children were born into monogyny amily structure (69.4) and live mostly in urban residence (70.9%). About 37.5% of them were born by mothers who had family planning, 29.2% of the mother had a minimum of secondary school education and 31.8% resides in rich households. Also, 52.7% of children were in 2‐ to 3‐year age category, 56.1% had at least four ANC visits in their pregnancies, 55.1% had high weight at birth and mothers had normal BMI between 18.5 and 24.918.5 kg/m2. The χ 2 analysis, which was conducted to examine the significant distribution of anaemia, showed that about 70% of the under‐five children from 15 SSA were anaemic 33.6% of anaemic under‐five children had mothers who married at or after their 18th year birthday. Also, 49.7% of female children, 36.5% of those that had normal weight at birth, children whose ages are between 3 and 5 years (10.2%), with high birth weight (56.3%) and whose mother had at least four ANC visits (54.8%) were anaemic. On the other hand, children in polygynous family structure (13.9%), in urban residence (72.2%), whose mother had no family planning need (38.1%), no education (36.3%) and children that grew up in households in poor quartile (36.2%) had a higher percentage of anaemia.
TABLE 2.
Descriptive statistics with the pooled sample of 17,033 children aged 0–59 months in Africa
| Independent variable | Overall | Not anaemic | Anaemic | p test |
|---|---|---|---|---|
| N | 17,033 | 4602 | 12,032 | |
| Age of marriage (≥18 [%]) | 4613 (30.5) | 1377 (33.5) | 3149 (29.6) | <0.001 |
| Iron supplement = 1 (%) | 3084 (18.1) | 841 (18.3) | 2164 (18.0) | 0.681 |
| Family structure (%) | <0.001 | |||
| Mono union | 11,463 (69.4) | 3177 (71.5) | 8027 (68.6) | |
| Poly union | 2178 (13.2) | 472 (10.6) | 1628 (13.9) | |
| Single mom | 2882 (17.4) | 793 (17.9) | 2040 (17.4) | |
| Residence = Urban (%) | 12,083 (70.9) | 3136 (68.1) | 8688 (72.2) | <0.001 |
| Family planning = 1 (%) | 6394 (37.5) | 1624 (35.3) | 4581 (38.1) | 0.001 |
| Maternal education (%) | <0.001 | |||
| No education | 5823 (34.2) | 1240 (26.9) | 4366 (36.3) | |
| Primary education | 6240 (36.6) | 1841 (40.0) | 4309 (35.8) | |
| Secondary and higher | 4966 (29.2) | 1521 (33.1) | 3356 (27.9) | |
| Maternal currently working (%) | 10,941 (64.2) | 3057 (66.4) | 7746 (64.4) | 0.014 |
| Wealth index (%) | <0.001 | |||
| Poor | 5818 (34.2) | 1334 (29.0) | 4361 (36.2) | |
| Average | 5793 (34.0) | 1588 (34.5) | 4089 (34.0) | |
| Rich | 5422 (31.8) | 1680 (36.5) | 3582 (29.8) | |
| Child age (%) | <0.001 | |||
| 0–11 | 2868 (16.8) | 503 (10.9) | 2257 (18.8) | |
| 24–35 | 8983 (52.7) | 2174 (47.2) | 6630 (55.1) | |
| 36–47 | 3001 (17.6) | 1014 (22.0) | 1918 (15.9) | |
| 48–59 | 2181 (12.8) | 911 (19.8) | 1227 (10.2) | |
| Gender = female (%) | 8571 (50.3) | 2393 (52.0) | 5979 (49.7) | 0.008 |
| ANC visits, ≥4 visits (%) | 6649 (56.1) | 1673 (59.1) | 4803 (54.8) | <0.001 |
| Maternal BMI (%) | <0.001 | |||
| Thin | 1696 (10.0) | 400 (8.7) | 1261 (10.5) | |
| Normal | 12,866 (75.8) | 3431 (74.8) | 9220 (76.9) | |
| Obese | 2405 (14.2) | 755 (16.5) | 1501 (12.5) | |
| Parity (%) | <0.001 | |||
| At least one | 9741 (41.1) | 1731 (37.6) | 4943 (41.1) | |
| Two to four | 13,754 (58.0) | 2819 (61.3) | 6982 (58.0) | |
| Multi (≥5) | 229 (1.0) | 52 (1.1) | 107 (0.9) | |
| Maternal is anaemic (%) | 8700 (52.0) | 2836 (62.3) | 5736 (48.2) | <0.001 |
| Birth weight (%) | <0.001 | |||
| Low birthweight | 1236 (7.3) | 348 (7.6) | 866 (7.2) | |
| Normal birthweight | 6415 (37.7) | 1881 (40.9) | 4392 (36.5) | |
| High birthweight | 9376 (55.1) | 2372 (51.6) | 6769 (56.3) | |
| Age of marriage (≥18 years [%]) | 4613 (30.5) | 1377 (33.5) | 3149 (29.6) | <0.001 |
| Iron supplement = 1 (%) | 3084 (18.1) | 841 (18.3) | 2164 (18.0) | 0.681 |
| Family structure (%) | <0.001 | |||
| Monogamy union | 11,463 (69.4) | 3177 (71.5) | 8027 (68.6) | |
| Polygany union | 2178 (13.2) | 472 (10.6) | 1628 (13.9) | |
| Single mom | 2882 (17.4) | 793 (17.9) | 2040 (17.4) | |
| Residence = Urban (%) | 12,083 (70.9) | 3136 (68.1) | 8688 (72.2) | <0.001 |
| Family planning = 1 (%) | 6394 (37.5) | 1624 (35.3) | 4581 (38.1) | 0.001 |
| Maternal education (%) | <0.001 | |||
| No education | 5823 (34.2) | 1240 (26.9) | 4366 (36.3) | |
| Primary education | 6240 (36.6) | 1841 (40.0) | 4309 (35.8) | |
| Secondary and higher | 4966 (29.2) | 1521 (33.1) | 3356 (27.9) | |
| Maternal currently working (%) | 10,941 (64.2) | 3057 (66.4) | 7746 (64.4) | 0.014 |
| Wealth index (%) | <0.001 | |||
| Poor | 5818 (34.2) | 1334 (29.0) | 4361 (36.2) | |
| Average | 5793 (34.0) | 1588 (34.5) | 4089 (34.0) | |
| Rich | 5422 (31.8) | 1680 (36.5) | 3582 (29.8) | |
| Child age in month (%) | <0.001 | |||
| 0–11 | 2868 (16.8) | 503 (10.9) | 2257 (18.8) | |
| 24–35 | 8983 (52.7) | 2174 (47.2) | 6630 (55.1) | |
| 36–47 | 3001 (17.6) | 1014 (22.0) | 1918 (15.9) | |
| 48–59 | 2181 (12.8) | 911 (19.8) | 1227 (10.2) | |
| Gender = female (%) | 8571 (50.3) | 2393 (52.0) | 5979 (49.7) | 0.008 |
| ANC visits, ≥4 visits (%) | 6649 (56.1) | 1673 (59.1) | 4803 (54.8) | <0.001 |
| Maternal BMI (%) | <0.001 | |||
| Thin | 1696 (10.0) | 400 (8.7) | 1261 (10.5) | |
| Normal | 12,866 (75.8) | 3431 (74.8) | 9220 (76.9) | |
| Obese | 2405 (14.2) | 755 (16.5) | 1501 (12.5) | |
| Parity (%) | <0.001 | |||
| At least one | 9741 (41.1) | 1731 (37.6) | 4943 (41.1) | |
| Two to four | 13,754 (58.0) | 2819 (61.3) | 6982 (58.0) | |
| Multi (≥5) | 229 (1.0) | 52 (1.1) | 107 (0.9) | |
| Maternal is anaemic (%) | 8700 (52.0) | 2836 (62.3) | 5736 (48.2) | <0.001 |
| Birth weight (%) | <0.001 | |||
| Low birthweight | 1236 (7.3) | 348 (7.6) | 866 (7.2) | |
| Normal birthweight | 6415 (37.7) | 1881 (40.9) | 4392 (36.5) | |
| High birthweight | 9376 (55.1) | 2372 (51.6) | 6769 (56.3) |
Abbreviations: ANC, antenata visit; parity, number of times a woman has given birth to a fetus with a gestational age of 24 weeks and more; BMI, body mass index—a measure that uses your height and weight.
3.2. Association between girl child marriage and risk of anaemia among under‐five children
The results from the multivariable regression examined the association between maternal age marriage at or after their 18th birthday and the risk of anaemia as presented in Table 3. In Model I, which is unadjusted, the risk anaemia among under‐five children was significantly associated with maternal marriage age at or after their 18th birthday 0.80 [0.75–0.85]. When child characteristics and exposures were adjusted for in Model II, the risk anaemia among under‐five children 0.76 [0.70–0.83] was significantly reduced by 24% among those whose mother married at or after their 18th birthday in comparison with those that their mothers married before their 18th birthday. In Model III, when the other mother's characteristics (access to family planning, maternal education, BMI and if a mother is working or not) were adjusted for, the risk of anaemia among under‐five children was significantly reduced only by 13% among children whose mother married at or after their 18th birthday. Model IV when household characteristics (family structure and wealth index) were controlled for, 17% significant reduction in the risk of anaemia was observed.
TABLE 3.
Results from multi‐variable regression on maternal age of marriage and the risk of anaemia among under‐five children
| Predicators | Model 1: Unadjusted | Adjusted for child characteristics | Adjusted for maternal characteristics | Adjusted for SES | Final model |
|---|---|---|---|---|---|
| Odds ratios [CI] | Odds ratios [CI] | Odds ratios [CI] | Odds ratios [CI] | Odds ratios [CI] | |
| Age of marriage (≥18) | 0.83 [0.75–0.91] *** | 0.80 [0.73–0.88] *** | 0.89 [0.81–0.98]* | 0.89 [0.81–0.98] * | 0.88 [0.80–0.97]* |
| Iron supplement (1) | 1.04 [0.92–1.18] | ||||
| Child's age | |||||
| 24–35 | 0.64 [0.56–0.73]*** | 0.64 [0.56–0.73]*** | |||
| 36–47 | 0.39 [0.34–0.46]*** | 0.38 [0.33–0.45]*** | |||
| 48–59 | 0.27 [0.23–0.31]*** | 0.26 [0.22–0.31]*** | |||
| Gender (female) | 0.96 [0.89–1.04] | ||||
| ANC visits (≥4 visits) | 0.91 [0.84–1.00]* | 1.00 [0.91–1.09] | |||
| Birth weight | |||||
| Normal birthweight | 0.95 [0.79–1.14] | 0.97 [0.80–1.18] | |||
| High birthweight | 1.23 [1.02–1.47]* | 1.09 [0.90–1.32] | |||
| Unmet family planning | 0.96 [0.87–1.05] | ||||
| Parity | |||||
| Two to four | 0.80[0.73–0.87] *** | 0.98 [0.88–1.08] | |||
| Multi (≥5) | 0.61[0.38–0.98] * | 0.74 [0.46–1.18] | |||
| Maternal education (no education as ref) | |||||
| Primary | 0.71 [0.63–0.79]*** | 0.74 [0.66–0.83]*** | |||
| Secondary and higher | 0.62 [0.55–0.69]*** | 0.69 [0.60–0.78]*** | |||
| Mother currently working | 0.92 [0.84–1.01] | 0.89 [0.81–0.98]* | |||
| Body mass index (thin as ref) | |||||
| Normal | 0.98 [0.84–1.14] | 1.04 [0.89–1.21] | |||
| Obese | 0.75 [0.63–0.89]** | 0.88 [0.73–1.05] | |||
| Maternal is anaemic | 0.58 [0.53–0.63]*** | 0.57 [0.52–0.63]*** | |||
| Family structure (single as ref) | |||||
| Poly union | 1.24 [1.08–1.42]** | 1.18 [1.02–1.36]* | |||
| Single mom | 1.11 [0.99–1.25] | 1.09 [0.96–1.23] | |||
| Residence (rural) | 0.95 [0.84–1.08] | ||||
| Wealth index (poor as ref) | |||||
| Poly union | 0.75 [0.67–0.84]*** | 0.80 [0.71–0.89]*** | |||
| Single mom | 0.60 [0.52–0.69]*** | 0.70 [0.62–0.79]*** | |||
| Observations | 17,033 | 17,033 | 17,033 | 17,033 | 17,033 |
Abbreviations: ANC, antenata visit; BMI, body mass index—a measure that uses your height and weight; CI, confidence interval; parity, number of times a woman has given birth to a fetus with a gestational age of 24 weeks and more.
p < 0.05.
p < 0.01.
p < 0.001.
In the final model, when all the significant variables from individual models were simultaneously adjusted for, 14% reduction in risk of anaemia was observed among under‐five children whose mothers married after 18th birthday when compared with those with mothers married before 18th birthday. Overall, growing up in polygynous family structure seems to have the strongest positive impact on the risk of anaemia among under‐five children 1.43 [1.23–1.67]; it significantly increases the risk by 43%. We also observed that as under‐five children increase in age, the risk of anaemia reduces; the strongest reduction was observed at age 3–5 (about 76% reduction). Normal birthweight compared with low birth weight, being born to a single mother compared with monogyny family structure, access to family planning, and rural residence was not significantly associated with risk of anaemia.
The result from the different age of marriage categories showed that maternal marriage between 14 and 15 and 16–17 years was not significantly associated with risk of anaemia when compared with marriage below 14 years. However, maternal marriage at or after 18‐year birthday was significantly associated with a 19% reduction in risk of anaemia among under‐five children (see supporting information). Finally, in the individual meta‐analysis conducted, the overall risk of anaemia among children whose mother married before their 18th birthday was significantly increased by 7% (Figure 2). The country‐specific risk of anaemia showed that 14 of the 15 SSA countries showed an increased risk of anaemia among children whose mother married before age 18; however, this was only significant in Côte d'Ivoire and Mozambique (83% and 52% increased risk).
FIGURE 2.
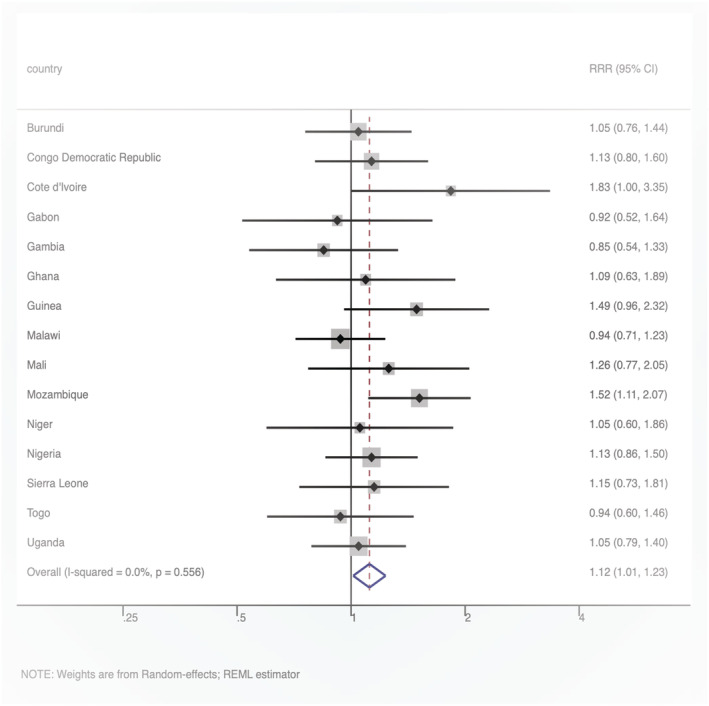
Forest plot showing country‐specific associations between anaemia in under‐five and girl child marriage
4. DISCUSSION
This study explored the possible association between maternal age of marriage and the anaemia status of children under‐five years of age. We explored how child, maternal and household characteristics shaped this relationship with a special interest in what extent does maternal marriage at or after 18th birthday suggest protective role on risk of anaemia among under‐five children in SSA countries. Based on our analysis with the different categories in the age of marriage, we also conducted a country‐specific analysis to highlight part of Africa countries where marriage before age 18 is associated with risk of anaemia among under‐five children. We found compelling evidence that maternal marriage at or after their 18th birthday significantly reduces the risk of anaemia among under‐fives with highest impact in Côte d'Ivoire and Mozambique.
Descriptively, countries such as Niger, Mali and Sierra Leone had higher prevalence of anaemia, above 70% in both outcomes. A similar pattern in the prevalence of anaemia and girl child marriage has been confirmed in previous studies, especially with the lower prevalence in Burundi when compared with other African countries (Fund U. N. I. C. E, 2014; Moschovis et al., 2018). However, our study showed higher figures in the prevalence of anaemia, about 45.7% anaemia prevalence in Rwanda as against the 34.0% reported in a most recent study by Moschovis et al. (2018). The notable differences were the survey year (5‐year difference), and our measure of anaemia was adjusted for altitude. A similar increase in anaemia when altitude is being adjusted for has been reported, and more importantly, this disparity highlights the importance of accurate assessment of anaemia in research according to the WHO standard—which recommends adjustment to altitude for comparable analyses (Accinelli & Leon‐Abarca, 2020; Smith et al., 2010). In addition, because the data used for our study are more recent than the data used by Moschovis et al., we can suggest that the prevalence of anaemia might have increased in countries like Burundi.
By applying the average estimate of anaemia found in our study (69.1%) to the UN's Population Division estimate of under‐five children population in SSA, which is 157.4 million (Moschovis et al., 2018), it will imply that about 108.6 million under‐five children are anaemic in SSA. Following WHO's guidelines, iron supplementation is strongly recommended for children from 6 month old to tackle anaemia in regions with highly prevalent like Africa. However, identifying the risk factors will provide more proactive approaches for preventive and promotive interventions against the unacceptably high prevalence of anaemia in SSA.
Across all our models, when household, mother and child's characteristics were individually and simultaneously adjusted for, we found that the maternal age of marriage was significantly associated with the risk of anaemia among under‐five children. Maternal marriage after 18th birthday reduces the risk of anaemia among under‐five children by 16%. Our result mirrored findings from previous and similar studies; girl child marriage has been linked with other nutritional and anthropometric outcomes such as stunting, underweight and wasting. From our extensive literature research, Paul et al. (2019) were the only ones that had explored similar association using Indian National Family Health Survey (NFHS). Although they were focused on if girl child marriage exposes under‐five children to risk of anaemia, our findings were largely consistent with this study. They reported 8% increased risk of anaemia among under‐five children whose mother married before their 18th birthday.
These findings do not necessarily mean that under‐five children whose mothers married before and after their 18th birthday are automatically prone and provide protection against anaemia, respectively. As suggested in the literature, there are different pathways through which this can occur and some of them are inter‐related. For example, it is well established that young married women are less likely to have completed secondary school education before 18 years in most developing countries as they had to drop out of school when they become pregnant and permanent termination of their education (HRW, 2018; Paul, 2020). This alone will lead to a cascade of experiences and exposures such as unemployment, lack of financial independence, low decision‐making power and poverty, which breed poor nutritional optional and health services. All these exposures, through various interactions at individual and community levels, are enough to expose their under‐five to anaemia. Based on recent estimate and projections, about 50 million girl child marriage could be prevented in if all girls finished secondary school (Save the Children [STC], 2018). This also corroborates the finding from our study as we found that maternal secondary school education reduces the risk of anaemia by 38% under‐five children.
Findings from our study also revealed how child, maternal and household characteristics shape the association between under‐five risk of anaemia and maternal age of marriage. Child's characteristics seem to have the strongest modulating effect; when they were adjusted for, 24% reduction in risk of anaemia was observed among under‐five whose mother married at or after their 18th birthday. However, child age and gender were the only significant characteristics in the final model. The increased need for iron at the first 2 years of life and early introduction of iron‐rich food after weaning has been suggested as the possible reason for the difference in risk of anaemia across the age streams (Domello et al., 2002; McCarthy et al., 2018). Policy options to tackling anaemia in Africa might be more effective if high‐risk children—born by under‐age mother, less than 2 years and males under‐five children, should be prioritised. Previous studies have shown similar findings, and these have been suggested for policy implications in some developed countries. An example is the iron supplement for children under two years as suggested by international agencies (WHO, 2016).
When the household characteristics were adjusted for, the association between risk of anaemia and child marriage was significantly modulated, although in lesser degree when compared with other models. When adjusted for, 17% reduction in risk of anaemia was observed among under‐five whose mother married at or after their 18th birthday. Being born into wealthy households was significantly associated with reduced risk of anaemia by 3%; however, children born into polygynous union were at increased risk of anaemia even when their mother married at the normal age (18 years and above). This probably suggests how these household factors highlighted above influence nutritional and health outcomes. Desai's 1995 dilution of resources has been used to explain this possible linkage of polygynous union with poor health outcome of mother and child (Smith‐Greenaway & Trinitapoli, 2014). Previous studies have shown that polygyny does not only reflect household characteristics but also a common feature society with high gender inequality and strong patriarchal system.
Finally, when maternal risk factors were controlled, the risk of anaemia among under‐five children was reduced only by 13% when compared with the odd ratio of unadjusted relationship. This contrasts the 24% and 16% reduction observed when children's and household characteristics were adjusted for. Already, previous studies have reported prevalence of iron deficiency and body mass depletion in girl child bride and adolescent pregnancy; this might suggest one of the pathways through which the risk of anaemia among under‐five is related to the maternal age of marriage (Alquaiz et al., 2013; McLean et al., 2009; Paul et al., 2019). The concept of the vicious cycle could also be used to explain this in relation to other characteristics. This concept explains how negative series of events such as girl child marriage, in this case, build up and continually reinforce other risk factors. Maternal characteristics and exposures will likely be at the centre point of this cycle as they are shaped by household and societal factors themselves, and they also influence children's condition of birth and living experiences individually.
In our analysis with different age categories, risk of anaemia among under‐five children whose mother married before 14 in comparison with those that married between 14 and 15 years was not different, probably because they experience a similar risk. The difference in risk of anaemia was evident from age 18 years; when maternal marriage is at least 18 years, the risk of anaemia among under five is significantly reduced by 21%, almost double when their mothers married between age 16 and 17 years. This finding alone further reinforces the safest and maybe most healthy age of marriage for women, and especially in African countries (Efevbera et al., 2019; Kidman, 2017; Paul, 2020). Also, our findings from our country‐specific analysis revealed that the risk of anaemia among under‐five children whose mother married too early (before age 18) was highly significant in Côte d'Ivoire and Mozambique. Along with other innovative effective targeted at high‐risk mother and children, these countries should probably be prioritised by international agencies as part of initiatives to tackle child marriage and relevant health outcomes.
4.1. Strengths and limitations
This study involves a large dataset including 17,033 women–child pairs from 15 SSA countries. There were missing data points as expected in anaemia research using survey data; however, we were able to apply multiple imputations to deal with missing data problem. In addition, the DHS data are usually nationally representative and use the same data collection procedure; therefore, findings from this study can be generalised. The main limitation of our study is that care has to be taken while interpreting our findings as association do not mean causality because the DHS is a cross‐sessional study. The survey used was from different years; nonetheless, we controlled for year of survey variable along with a host of other key determinants. Finally, we recognise that environmental factors are related to anaemia among under‐five children; also, more factors indicating child's diet might have increased robustness of the models. However, they were neither not available at individual levels nor not consistent across the DHS data used for this study.
5. CONCLUSIONS
This study established that there is an association between maternal girl's child marriage and risk of anaemia among under‐five children in SSA, suggesting that marriage at or after 18th birthday is strongly associated with the risk factor of anaemia among under‐five children, suggesting a protective role. We also found that children and household characteristics seem to have more impact on the relationship than the maternal characteristics. We found a significant association between girl child marriage and the risk of anaemia Mozambique and Côte d'Ivoire. Although iron supplement remains the major strategy to tackle anaemia prevalence in most developing countries, it is also necessary to remember that access to these supplementations is not likely to be readily available for young girls who married too early. They are more likely to lack education to understand the use and importance of these supplements or lack the decision‐making power and sometimes finances to access them. Although policies to make iron supplement free might remove these barriers, policies that will address girl child marriage, like boosting girl child educational attainment, will be more effective and yield result that could turn the tide of the vicious cycles set in motion girl child marriage. We also believe that our findings can inform the development of simple policy tools for relevant policymakers and more importantly, community gatekeepers, where the practice of girl child marriage is usually deeply rooted in culture and predominant religion.
CONFLICTS OF INTEREST
The authors declare that they have no competing interest.
CONTRIBUTIONS
SY contributed to the study design and conceptualization. SY and SA reviewed the literature performed the analysis and drafted the first draft of this manuscript. SAA provided technical support and critically reviewed the manuscript for its intellectual content. SY had final responsibility to submit for publication. All authors read and amended drafts of the paper and approved the final version.
Supporting information
Table S1. Multi‐variable regression on maternal age of marriage (in different categories) and the risk of anaemia among under‐five children
ACKNOWLEDGEMENTS
The authors thank the MEASURE DHS project for their support and for free access to the original data. The authors received no specific funding for this work.
Anjorin, S., & Yaya, S. (2021). Anaemia among under‐five children: Is maternal marriage at 18th birthday and above protective? Evidence from 15 countries in Sub‐Saharan Africa. Maternal & Child Nutrition, 17(4), e13226. 10.1111/mcn.13226
DATA AVAILABILITY STATEMENT
Data for this study were sourced from Demographic and Health surveys (DHS) and available online (http://dhsprogram.com/data/available-datasets.cfm).
REFERENCES
- Accinelli, R. A., & Leon‐Abarca, J. A. (2020). Age and altitude of residence determine anemia prevalence in Peruvian 6 to 35 months old children. PLoS ONE, 15(1), e0226846. 10.1371/journal.pone.0226846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alquaiz, A. M., Gad Mohamed, A., Khoja, T. A. M., Alsharif, A., Shaikh, S. A., Al Mane, H., Aldiris, A., Kazi, A., & Hammad, D. (2013). Prevalence of anemia and associated factors in child bearing age women in Riyadh, Saudi Arabia. Journal of Nutrition and Metabolism, 2013, 1–7. 10.1155/2013/636585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey, R. L., West, K. P.Jr., & Black, R. E. (2015). the epidemiology of global micronutrient deficiencies. Annals of Nutrition and Metabolism, 66(Suppl. 2), 22–33. 10.1159/000371618 [DOI] [PubMed] [Google Scholar]
- Benach, J., Friel, S., Houweling, T., Labonte, R., Muntaner, C., Schrecker, T., & Simpson, S. (2010). A conceptual framework for action on the social determinants of health. Geneva: World Health Organization. [Google Scholar]
- Dahl, G. B. (2010). Early teen marriage and future poverty. Demography, 47(3), 689–718. 10.1353/dem.0.0120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domello, M., Hernell, O., & Domellöf, M. (2002). Iron‐deiciency anaemia during the first two years of life iron‐deciency anaemia during the rst two years of life. Scandinavian Journal of Nutrition, 46, 20–30. 10.1080/110264802753704091 [DOI] [Google Scholar]
- Efevbera, Y., Bhabha, J., Farmer, P., & Fink, G. (2019). Girl child marriage, socioeconomic status, and undernutrition: Evidence from 35 countries in Sub‐Saharan Africa. BMC Medicine, 17(1), 55. 10.1186/s12916-019-1279-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay, J. E., Özaltin, E., & Canning, D. (2011). The association of maternal age with infant mortality, child anthropometric failure, diarrhoea and anaemia for first births: Evidence from 55 low‐ and middle‐income countries. BMJ Open, 1(2), e000226. 10.1136/bmjopen-2011-000226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fund, U. N. I. C. E . (2014). Ending child marriage: Progress and prospects. file:///Users/aos/Downloads/Child‐Marriage‐Brochure‐HR_164.pdf
- Hakizimana, D., Nisingizwe, M. P., Logan, J., & Wong, R. (2019). Identifying risk factors of anemia among women of reproductive age in Rwanda—A cross‐sectional study using secondary data from the Rwanda demographic and health survey 2014/2015. BMC Public Health, 19(1), 1662. 10.1186/s12889-019-8019-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- HRW . (2018). Discrimination in education against pregnant girls and adolescent mothers|HRW. Human Health Watch|Leave No Girl Behind Africa. https://www.hrw.org/report/2018/06/14/leave-no-girl-behind-africa/discrimination-education-against-pregnant-girls-and
- Jakobsen, J. C., Gluud, C., Wetterslev, J., & Winkel, P. (2017). When and how should multiple imputation be used for handling missing data in randomised clinical trials—A practical guide with flowcharts. BMC Medical Research Methodology, 17(1), 162. 10.1186/s12874-017-0442-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khusun, H., Ray, Y., Schultink, W., & Dillon, D. H. S. (1999). World health organization hemoglobin cut‐off points for the detection of anemia are valid for an Indonesian population. Journal of Nutrition, 129(9), 1669–1674. 10.1093/jn/129.9.1669 [DOI] [PubMed] [Google Scholar]
- Kidman, R. (2016). Child marriage and intimate partner violence: A comparative study of 34 countries. International Journal of Epidemiology, 46(2), dyw225. 10.1093/ije/dyw225 [DOI] [PubMed] [Google Scholar]
- Kidman, R. (2017). Child marriage and intimate partner violence: A comparative study of 34 countries. International Journal of Epidemiology, 46(2), 662–675. 10.1093/ije/dyw225 [DOI] [PubMed] [Google Scholar]
- Loaiza, E., & Fund, S. W. (2012). Marrying too young. End child marriage. In UNFPA. https://www.unfpa.org/sites/default/files/pub-pdf/MarryingTooYoung.pdf
- Marn, H., & Critchley, J. A. (2016). Accuracy of the WHO Haemoglobin Colour Scale for the diagnosis of anaemia in primary health care settings in low‐income countries: A systematic review and meta‐analysis. The Lancet Global Health, 4(4), e251–e265. 10.1016/S2214-109X(16)00005-X [DOI] [PubMed] [Google Scholar]
- McCarthy, E. K., ní Chaoimh, C., Kenny, L. C., Hourihane, J. O., Irvine, A. D., Murray, D. M., & Kiely, M. E. (2018). Iron status, body size, and growth in the first 2 years of life. Maternal & Child Nutrition, 14(1), e12458. 10.1111/mcn.12458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean, E., Cogswell, M., Egli, I., Wojdyla, D., & De Benoist, B. (2009). Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993–2005. Public Health Nutrition, 12(4), 444–454. 10.1017/S1368980008002401 [DOI] [PubMed] [Google Scholar]
- Moschovis, P. P., Wiens, M. O., Arlington, L., Antsygina, O., Hayden, D., Dzik, W., Kiwanuka, J. P., Christiani, D. C., & Hibberd, P. L. (2018). Individual, maternal and household risk factors for anaemia among young children in sub‐Saharan Africa: A cross‐sectional study. BMJ Open, 8(5), 19654. 10.1136/bmjopen-2017-019654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nour, N. M. (2006). Health consequences of child marriage in Africa. Emerging Infectious Diseases, 12(11), 1644–1649. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3372345/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nour, N. M. (2009). Child marriage: A silent health and human rights issue. Reviews in Obstetrics and Gynecology, 2(1), 51–56. https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2672998/ [PMC free article] [PubMed] [Google Scholar]
- Parbey, P. A., Tarkang, E., Manu, E., Amu, H., Ayanore, M. A., Aku, F. Y., Ziema, S. A., Bosoka, S. A., Adjuik, M., & Kweku, M. (2019). risk factors of anaemia among children under five years in the Hohoe Municipality, Ghana: A case control study. Anemia, 2019, 1–9. 10.1155/2019/2139717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons, J., Edmeades, J., Kes, A., Petroni, S., Sexton, M., & Wodon, Q. (2015). Economic impacts of child marriage: A review of the literature. Review of Faith and International Affairs, 13(3), 12–22. 10.1080/15570274.2015.1075757 [DOI] [Google Scholar]
- Paul, P. (2020). Child marriage among girls in India: Prevalence, trends and socio‐economic correlates. Indian Journal of Human Development, 14(2), 304–319. 10.1177/0973703020950263 [DOI] [Google Scholar]
- Paul, P., Chouhan, P., & Zaveri, A. (2019). Impact of child marriage on nutritional status and anaemia of children under 5 years of age: Empirical evidence from India. Public Health, 177, 95–101. 10.1016/j.puhe.2019.08.008 [DOI] [PubMed] [Google Scholar]
- Rutstein, S. O. G., & Rojas, M. C. S. (2006). Guide to DHS statistics.
- Sekhri, S., & Debnath, S. (2014). Intergenerational consequences of early age marriages of girls: Effect on children's human capital. Journal of Development Studies, 50(12), 1670–1686. 10.1080/00220388.2014.936397 [DOI] [Google Scholar]
- Seth, R., Bose, V., Qaiyum, Y., Chandrashekhar, R., Kansal, S., Taneja, I., & Seth, T. (2018). Social determinants of child marriage in rural india. The Ochsner Journal, 18(4), 390–394. 10.31486/toj.18.0104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simo, L. P., Agbor, V. N., Agborndip, E., Sone, D., Ekaney, M., Mbeng, E. N., Linonge Etombi, C., Neba, K. N., Kemah, B.‐L. A., Mbanya, D., Valirie, D., & Agbor, N. (2020). Prevalence and determinants of anaemia in children aged 6–59 months in Africa: A protocol for systematic review and meta‐analysis. BMJ Open, 10, 32042. 10.1136/bmjopen-2019-032042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, J. L., Johnston, N. P., Dearden, K. A., Eggett, D. L., & Campbell, A. K. (2010). The impact of altitude and diet on anemia in school‐aged children in Lago San Pablo, Ecuador. ICAN: Infant, Child, & Adolescent Nutrition, 2(5), 288–293. 10.1177/1941406410383013 [DOI] [Google Scholar]
- Smith‐Greenaway, E., & Trinitapoli, J. (2014). Polygynous contexts, family structure, and infant mortality in sub‐Saharan Africa. Demography, 51(2), 341–366. 10.1007/s13524-013-0262-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solovyova, A. V., Gace, V., Ermolenko, K. S., & Khorolskiy, V. A. (2018). Anemia in women of reproductive age. In Current Topics in Anemia. InTech. 10.5772/intechopen.71520 [DOI] [Google Scholar]
- STC . (2018). International day of the girl: If all girls completed secondary school, more than 50 million child marriages could be prevented|Save the Children International. Save the Children. https://www.savethechildren.net/news/international-day-girl-if-all-girls-completed-secondary-school-more-50-million-child-marriages#_ednref1
- Stevens, G. A., Finucane, M. M., De‐Regil, L. M., Paciorek, C. J., Flaxman, S. R., Branca, F., Peña‐Rosas, J. P., Bhutta, Z. A., & Ezzati, M. (2013). Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non‐pregnant women for 1995–2011: A systematic analysis of population‐representative data. The Lancet Global Health, 1(1), e16–e25. 10.1016/S2214-109X(13)70001-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2005). Early marriage: A harmful traditional practice. https://www.unicef.org/publications/files/Early_Marriage_12.lo.pdf
- UNICEF . (2019). Fast facts: 10 facts illustrating why we must #EndChildMarriage. UNICEF. https://www.unicef.org/press-releases/fast-facts-10-facts-illustrating-why-we-must-endchildmarriage
- United Nation . (1989). United nations treaty collection. https://treaties.un.org/pages/ViewDetails.aspx?src=IND&mtdsg_no=IV-11&chapter=4&lang=en
- Wahyudi, T., Hasanbasri, M., Kusnanto, H., & Hakimi, M. (2019). Social determinants of health of child marriage (analysis of IFLS 2000, 2007, 2014). Jurnal Kesehatan Masyarakat, 15(1), 62–68. 10.15294/kemas.v15i1.16514 [DOI] [Google Scholar]
- WHO . (2016). Daily iron supplementation in infant and children guideline. https://apps.who.int/iris/bitstream/handle/10665/204712/9789241549523_eng.pdf
- WHO . (2019). WHO|Micronutrient deficiencies. World Health Organisation. http://www.who.int/nutrition/topics/ida/en/
- Wodon, Q., Male, C., Nayihouba, A., Onagoruwa, A., Savadogo, A., Yedan, A., Edmeades, J., Kes, A., John, N., Murithi, L., Steinhaus, M., Petroni, S., Nayihouba, A., Onagoruwa, A., Savadogo, A., Yedan, A., Edmeades, J., Kes, A., John, N., … Petroni, S. (2017). Economic impacts of child marriage: Global synthesis report. www.costsofchildmarriage.org.
- Yaya, S., Anjorin, S. S., & Adedini, S. A. (2021). Disparities in pregnancy‐related deaths: Spatial and Bayesian network analyses of maternal mortality ratio in 54 African countries. BMJ Global Health, 6(1). 10.1136/bmjgh-2020-004233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaya, S., Odusina, E. K., & Bishwajit, G. (2019). Prevalence of child marriage and its impact on fertility outcomes in 34 sub‐Saharan African countries. BMC International Health and Human Rights, 19(1), 33. 10.1186/s12914-019-0219-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Multi‐variable regression on maternal age of marriage (in different categories) and the risk of anaemia among under‐five children
Data Availability Statement
Data for this study were sourced from Demographic and Health surveys (DHS) and available online (http://dhsprogram.com/data/available-datasets.cfm).


