Abstract
Background
The influence of a high sugar diet on colorectal cancer (CRC) survival is unclear.
Methods
Among 1463 stage I–III CRC patients from the Nurses’ Health Study and Health Professionals Follow-up Study, we estimated hazard ratios (HRs) and 95% confidence intervals (CIs) for CRC-specific and all-cause mortality in relation to intake of post-diagnosis sugar-sweetened beverages (SSB), artificially sweetened beverages (ASB), fruit juice, fructose and other sugars.
Results
Over a median 8.0 years, 781 cases died (173 CRC-specific deaths). Multivariable-adjusted HRs for post-diagnosis intake and CRC-specific mortality were 1.21 (95% CI: 0.87–1.68) per 1 serving SSBs per day (serving/day) and 1.24 (95% CI: 0.95–1.63) per 20 grams fructose per day. Significant positive associations for CRC-specific mortality were primarily observed ≤5 years from diagnosis (HR per 1 serving/day of SSBs = 1.59, 95% CI: 1.06–2.38). Significant inverse associations were observed between ASBs and CRC-specific and all-cause mortality (HR for ≥5 versus <1 serving/week = 0.44, 95% CI: 0.26–0.75 and 0.70, 95% CI: 0.55–0.89, respectively).
Conclusions
Higher post-diagnosis intake of SSBs and sugars may be associated with higher CRC-specific mortality, but only up to 5 years from diagnosis, when more deaths were due to CRC. The inverse association between ASBs and CRC-specific mortality warrants further examination.
Subject terms: Epidemiology, Cancer epidemiology, Colorectal cancer, Nutrition
Background
Substantial evidence supports a link between positive energy balance and hyperinsulinemia and colorectal cancer (CRC) development and progression [1]. Obesity, physical inactivity [2] and type 2 diabetes mellitus [3], which influence insulin levels, are established risk factors for CRC incidence. However, the role of these and other risk factors related to metabolic syndrome and CRC survival are not as well understood. A few recent studies suggest that obesity [4], physical inactivity [5], Western dietary pattern (characterised by high intake of red and processed meat, high-fat dairy and refined grains) [6, 7], and high dietary glycemic load and insulin score [8, 9], may be associated with poorer survival in CRC patients. While there is limited prior literature examining the role of sugar-sweetened beverages (SSB) and sugar intake in CRC survival, a few studies have observed associations between post-diagnosis dietary patterns, in which SSBs were a component of the pattern, and CRC survival [6, 7]. Furthermore, cancer survivors are at an increased risk of other chronic conditions [10], for which SSB and sugar consumption may also be relevant [11]. One recent study found that higher post-diagnosis SSB intake was associated with higher colon cancer recurrence and mortality, but this study lacked information on dietary intake before diagnosis [12].
SSBs are the largest source of added sugar in the U.S. diet and the biggest single source of energy intake [13]. SSBs are mostly sweetened with high fructose corn syrup (typically 45% glucose and 55% fructose) or sucrose (table sugar), which is composed of half fructose and half glucose [13]. Dietary recommendations for cancer prevention, such as those published by the World Cancer Research Fund/American Institute for Cancer Research, include limiting SSB and sugar intake [2]. However, the role of SSBs and sugar intake in cancer survival remains unclear.
To address this gap in knowledge, we prospectively examined the association between SSBs, artificially sweetened beverages (ASBs), and fruit juice consumption, as well as total fructose, glucose, sucrose and added sugar intake after CRC diagnosis with CRC-specific and all-cause mortality, with adjustment for pre-diagnosis intake, in two large prospective cohort studies, the Nurses’ Health Study (NHS) and the Health Professionals Follow-up Study (HPFS). As ASBs are often consumed as a no-calorie alternative to SSBs [14], and a recent study found that higher ASB intake was associated with lower colon cancer recurrence and mortality [15], we also examined ASB intake as an exposure. To account for the differences between fructose and glucose metabolism, associations were studied separately by intake of each type of sugar [16, 17].
Methods
Study population
The NHS is a prospective cohort study established in 1976 when 121,700 U.S. female nurses 30–55 years of age responded to a mailed questionnaire about lifestyle factors and medical histories [18]. The HPFS is a prospective cohort study established in 1986 of 51,529 male health professionals 40–75 years of age who similarly responded to a questionnaire [19]. In both cohorts follow-up questionnaires have been sent to participants every 2 years thereafter. The cumulative follow-up rates have been greater than 90% for both cohorts. The study protocol was approved by the institutional review boards of the Brigham and Women’s Hospital and Harvard T.H. Chan School of Public Health, and those of participating registries as required.
Ascertainment of CRC diagnosis and death
Our study population consisted of participants who had no history of cancer at study enrollment and were later diagnosed with stage I to III CRC from 1984–2010 for NHS and 1990–2010 for HPFS. On each biennial questionnaire, participants were asked to report any CRC diagnosis. When a CRC diagnosis was reported, permission was sought to obtain medical records. Study physicians blinded to exposure data reviewed all records to confirm the diagnosis. Stage of disease, grade of tumour differentiation, treatment, year of diagnosis and primary tumour location were recorded. Deaths were mostly reported by family members, the postal service and by searching the National Death Index. For non-responders, the National Death Index was searched to discover deaths and ascertain any CRC diagnosis that contributed to death or was a secondary diagnosis. Next-of-kin were contacted and provided informed consent to review medical records. For all deaths, cause of death was assigned by study physicians blinded to exposure data based on medical record and/or death certificate review. More than 96% of deaths have been identified through these methods [20].
Assessment of dietary intake
Dietary intake was assessed via validated self-administered semi-quantitative food frequency questionnaire (FFQ) in 1980, 1984, 1986 and every four years after for NHS and every four years beginning in 1986 for HPFS (NHS: total of 9 FFQ cycles and HPFS: total of 7 FFQ cycles).
Participants were asked how often, on average, in the previous year they consumed a standard unit or portion size of each food or beverage. SSBs included colas, other carbonated beverages, and other non-carbonated drinks (fruit punches, lemonades or other fruit drinks) that were sugar-sweetened, while ASBs included carbonated and non-carbonated low calorie or diet beverages. Other SSB items, such as sugar-sweetened or flavored milk, did not contribute to our definition of SSBs as they were infrequently consumed in this population based on pilot studies [21]. Fruit juice included orange, apple, grapefruit, and other juices. Total fructose and glucose included intake of each respective sugar plus half the intake of sucrose. Added sugar included sugars added to prepared or processed items but not naturally occurring sugars [22]. Total energy intake was calculated by summing the caloric values from all food and beverage items on the FFQ. Nutrient intakes were adjusted for total energy intake using the residual method [23]. For more detail on diet assessment, please refer to the Supplemental Methods.
To capture long-term dietary intake before CRC diagnosis, we calculated a cumulative average of intake for all FFQs up to four years before the date of diagnosis. Cumulative averaging can dampen variation due to both measurement error and true changes in diet over time [21]. The first dietary assessment collected between 6 months and 4 years after CRC diagnosis was used to define post-diagnosis intake to avoid assessment during the period of active treatment immediately following diagnosis.
Non-dietary covariate assessment
Information was collected on body mass index (BMI), physical activity, smoking history, history of diabetes, regular use of aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) and post-menopausal hormone use (among women) from questionnaires corresponding to the time of the post-diagnosis dietary assessment. Weight change around the time of CRC diagnosis was calculated based on the weight reported on the first biennial questionnaires immediately before and after the CRC diagnosis.
Statistical analysis
Cases without a valid FFQ within 4 years of diagnosis, those with missing data for pre-diagnosis or post-diagnosis sugar intake, and stage IV CRC were excluded from our analysis (see Supplemental Fig. 1). We computed person-years of follow-up beginning from the return of the first post-diagnosis dietary assessment to death or the end of the follow-up period (June 1, 2014 for NHS and January 31, 2014 for HPFS), whichever occurred first. Time since diagnosis was used as the time scale accounting for left truncation due to differences in the timing of the post-diagnosis assessment. The analyses included three outcomes: (1) death from CRC was the primary endpoint with deaths from other causes censored, (2) death from any cause and (3) death due to causes other than CRC as the secondary endpoints. For analyses with other (non-CRC related) mortality as the endpoint, deaths due to CRC were censored. Cox proportional hazards regression models were used to calculate hazard ratios (HRs) of death and 95% confidence intervals (CIs) for the seven exposures. Post-diagnosis SSBs, fruit juice, total fructose, total glucose, sucrose, and added sugar were modeled as continuous variables as 1 serving per day (serving/day) for the beverages and 20 grams per day (grams/day) for the sugars. Restricted cubic spline analyses indicated that associations were consistent with linearity (P for linearity > 0.05) for all exposures except post-diagnosis ASBs [24]. Therefore, post-diagnosis ASB intake was examined as a categorical variable (<1, 1–4, and ≥5 servings/week).
The models were initially adjusted for age groups at diagnosis (<60, 60–64, 65–69, 70–74 and ≥75 years), sex (women/men) and cancer stage (I, II, III and unspecified) as stratification factors, with additional adjustment for age at diagnosis (continuous). The multivariable models included the following additional covariates: year of diagnosis (continuous), tumour grade of differentiation (1–3 and unspecified), subsite (proximal colon, distal colon, rectum and unspecified), history of diabetes (yes/no) and post-diagnosis alcohol consumption (<0.15, 0.15–1.9, 2.0–7.4, ≥7.5 grams/day), pack-years of smoking (0, 1–15, 16–25, 26–45, >45), BMI (<23, 23–24.9, 25–27.4, 27.5–29.9, ≥30 kg/m2), physical activity (women: <5, 5–11.4, 11.5–21.9, ≥22 MET-hours/week; men: <7, 7–14.9, 15–24.9, ≥25 MET-hours/week), regular use of aspirin or NSAIDs (≥2 tablets/week, yes/no), consumption of, folate, calcium, vitamin D, red and processed meat and total energy intake (sex-specific quartiles), and, in women only, chemotherapy use (yes/no, available in women only) and post-menopausal hormone use (pre-menopausal, never, past, current users). This model also included adjustment for the cumulative average of pre-diagnosis intake of the respective post-diagnosis beverage or sugar (<1, 1–4, ≥5 servings/week for SSBs and ASBs; <1, 1–4, 5–7 servings/week, >1 serving/day for fruit juice; sex-specific quartiles for sugar variables). Post- and pre-diagnosis SSB and ASB intakes were mutually adjusted for each other (<1, 1–4, ≥5 servings/week), and the sugar intakes were additionally adjusted for post-diagnosis fruit and vegetable consumption (sex-specific quartiles). In separate analyses, we additionally adjusted the multivariable models for the Alternative Healthy Eating Index 2010 (AHEI-2010, excluding the SSB and juice component; sex-specific quartiles), which awards points for foods and macronutrients associated with reduced chronic disease risk [25], but adjustment for AHEI-2010 had minimal impact on the results and was not included in the final model. All statistical tests were two-sided with P < 0.05 considered statistically significant, and were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). For more detail on the statistical analysis, please refer to the Supplemental Methods.
Results
Among 1463 stage I–III CRC cases included in the analyses (Supplemental Fig. 1), 781 deaths were documented of which 173 were CRC-specific deaths (median 8.0 years follow-up). Other major causes of death were cardiovascular disease (n = 141) and other cancers (n = 115). The overall 5-year survival rates were 93% (95% CI: 90–95%) for stage I, 89% (95% CI: 86–92%) for stage II, and 80% (95% CI: 75–84%) for stage III CRC. Approximately 13% of participants consumed ≥5 servings of SSBs per week and 6% consumed SSBs more than once per day after diagnosis. On average, post-diagnosis added sugar intake from all dietary sources on the FFQ accounted for 10% (interquartile range: 7–13%) of total energy intake. Participants with higher post-diagnosis SSB intake tended to be less physically active, had lower alcohol consumption, and higher intake of total fructose, total glucose, sucrose and added sugar (Table 1). Tumour characteristics did not appear to vary by post-diagnosis SSB intake. Post-diagnosis intakes of each type of sugar were strongly correlated with each other (range of Spearman correlation coefficient r = 0.65–0.98; Supplemental Table 1), and moderately correlated with post-diagnosis SSB intake (r = 0.45–0.58). Pre- and post-diagnosis intake of each exposure were also moderately correlated, ranging from r = 0.39 for pre- and post-diagnosis SSBs to 0.58 for pre- and post-diagnosis ASBs.
Table 1.
Characteristics of colorectal cancer patients after diagnosis and tumour characteristics at diagnosis according to post-diagnosis intake of sugar-sweetened beverages in the Nurses’ Health Study and the Health Professionals Follow-up Study (n = 1463)a.
| Sugar-sweetened beverage intake, servings | |||
|---|---|---|---|
| <1/week | 1–4/week | ≥5/week | |
| (n = 864) | (n = 415) | (n = 184) | |
| Female, % | 72 | 60 | 71 |
| Age at diagnosis, yrs | 69.1 (8.6) | 67.9 (8.9) | 67.4 (9.0) |
| Food and nutrient intakeb | |||
| SSB intake, servings/d | 0.0 (0.0) | 0.3 (0.2) | 1.3 (0.7) |
| ASB intake, servings/d | 0.5 (0.8) | 0.3 (0.5) | 0.2 (0.5) |
| Fruit juice intake, servings/d | 0.8 (0.7) | 1.0 (0.9) | 1.1 (0.9) |
| Total fructose intake, g/d | 39.6 (12.8) | 47.0 (12.5) | 60.5 (15.2) |
| Total glucose intake, g/d | 38.8 (12.2) | 46.0 (12.1) | 58.9 (14.7) |
| Sucrose intake, g/d | 36.9 (13.9) | 45.2 (13.5) | 59.9 (20.5) |
| Added sugar intake, g/d | 35.8 (16.5) | 50.7 (17.8) | 78.1 (26.2) |
| Alcohol, g/d | 7.7 (12.5) | 6.7 (10.7) | 4.9 (9.7) |
| Folate, mcg/d | 708.3 (355.2) | 667.8 (309.9) | 613.9 (307.1) |
| Calcium, mg/d | 1255.5 (587.4) | 1134.1 (509.5) | 1049.7 (501.2) |
| Vitamin D, IU/d | 562.2 (408.9) | 518.3 (365.4) | 493.3 (435.3) |
| Total energy intake, kcal/d | 1685.9 (542.3) | 1858.1 (547.5) | 2024.5 (586.8) |
| AHEI-2010 | 57.0 (11.4) | 53.6 (10.2) | 47.0 (9.1) |
| Body mass index, kg/m2 | 26.5 (4.9) | 25.8 (4.5) | 26.4 (5.3) |
| Physical activity, MET-h/wk | 18.8 (24.1) | 18.2 (21.8) | 15.4 (19.9) |
| Pack-years of smoking | 16.0 (22.1) | 15.3 (20.4) | 18.3 (25.6) |
| Current smokers, % | 5 | 7 | 6 |
| Regular aspirin use, %c | 34 | 38 | 32 |
| Stage, % | |||
| I | 33 | 33 | 28 |
| II | 32 | 26 | 34 |
| III | 23 | 28 | 24 |
| Unspecified | 12 | 13 | 14 |
| Grade of differentiation, % | |||
| Well | 13 | 16 | 18 |
| Moderate | 59 | 58 | 53 |
| Poor/Undifferentiated | 14 | 12 | 15 |
| Unspecified | 14 | 14 | 14 |
| Cancer subsite, % | |||
| Proximal colon | 44 | 41 | 43 |
| Distal colon | 31 | 32 | 30 |
| Rectum | 21 | 22 | 22 |
| Unspecified | 5 | 5 | 5 |
SSB sugar-sweetened beverages, ASB artificially sweetened beverages, MET metabolic equivalent, AHEI. Alternative Healthy Eating Index.
aMeans (SD) are presented for continuous variables. All variables other than age at diagnosis are age standardised.
bNutrients are energy-adjusted.
cRegular use defined as ≥2 standard (325-mg) tablets of aspirin per week.
CRC-specific mortality
In the fully adjusted model (which included pre-diagnosis intake), the HR for CRC-specific mortality per 1 serving/day increase was 1.21 (95% CI: 0.87–1.68) for post-diagnosis SSB and 1.11 (95% CI: 0.91–1.36) for post-diagnosis fruit juice (Table 2). In the fully adjusted model, the HR per 20 grams/day total fructose intake was 1.24 (95% CI: 0.95–1.63), but results did not reach statistical significance (P-value = 0.12). Results for post-diagnosis total glucose, sucrose and added sugar intake were similar, with HRs for CRC-specific mortality ranging between 1.14 (added sugar) and 1.24 (glucose), and P-values between 0.11 and 0.14. On the other hand, higher post-diagnosis ASB intake was associated with lower CRC-specific mortality, particularly after adjustment for pre-diagnosis ASB intake (HR comparing ≥5 versus <1 serving/week: 0.44, 95% CI: 0.26–0.75, fully adjusted model).
Table 2.
Hazard ratios (HR) and 95% confidence intervals (CI) of colorectal-cancer (CRC)-specific mortality, other mortality (deaths due to causes other than CRC), and all-cause mortality according to post-diagnosisa beverage and sugar intake among CRC patients in the Nurses’ Health Study and Health Professionals Follow-up Study (n = 1463).
| No. of person-years | No. of deaths | Age, sex, stage-adjusted HR (95% CI)b | P-value | Multivariable-adjusted HR (95% CI)c | P-value | |
|---|---|---|---|---|---|---|
| Post-diagnosis beverage intake, per 1 serving/dayd | ||||||
| Sugar-sweetened beverages | ||||||
| CRC-specific mortality | 14,618 | 173 | 1.30 (0.98–1.72) | 0.066 | 1.21 (0.87–1.68) | 0.249 |
| Other (non-CRC) mortality | 608 | 1.05 (0.87–1.26) | 0.597 | 1.04 (0.85–1.29) | 0.682 | |
| All-cause mortality | 781 | 1.12 (0.96–1.30) | 0.161 | 1.11 (0.94–1.32) | 0.237 | |
| Artificially sweetened beverages | ||||||
| CRC-specific mortality | 14,618 | 173 | 0.61 (0.40–0.94) | 0.025 | 0.44 (0.26–0.75) | 0.002 |
| Other (non-CRC) mortality | 608 | 1.08 (0.86–1.35) | 0.507 | 0.79 (0.59–1.04) | 0.096 | |
| All-cause mortality | 781 | 0.95 (0.78–1.16) | 0.602 | 0.70 (0.55–0.89) | 0.004 | |
| Fruit juice | ||||||
| CRC-specific mortality | 14,618 | 173 | 1.11 (0.93–1.32) | 0.242 | 1.11 (0.91–1.36) | 0.304 |
| Other (non-CRC) mortality | 608 | 0.95 (0.85–1.05) | 0.306 | 1.03 (0.92–1.16) | 0.584 | |
| All-cause mortality | 781 | 0.99 (0.90–1.08) | 0.776 | 1.04 (0.94–1.15) | 0.406 | |
| Post-diagnosis sugar intake, per 20 g/day | ||||||
| Total fructose | ||||||
| CRC-specific mortality | 14,618 | 173 | 1.17 (0.95–1.43) | 0.148 | 1.24 (0.95–1.63) | 0.120 |
| Other (non-CRC) mortality | 608 | 0.88 (0.78–1.00) | 0.050 | 1.17 (1.00–1.36) | 0.049 | |
| All-cause mortality | 781 | 0.95 (0.85–1.05) | 0.302 | 1.18 (1.04–1.35) | 0.014 | |
| Total glucose | ||||||
| CRC-specific mortality | 14,618 | 173 | 1.17 (0.94–1.45) | 0.173 | 1.24 (0.93–1.64) | 0.140 |
| Other (non-CRC) mortality | 608 | 0.87 (0.77–1.00) | 0.046 | 1.17 (1.00–1.37) | 0.052 | |
| All-cause mortality | 781 | 0.94 (0.84–1.05) | 0.265 | 1.17 (1.03–1.34) | 0.020 | |
| Sucrose | ||||||
| CRC-specific mortality | 14,618 | 173 | 1.16 (0.96–1.39) | 0.117 | 1.21 (0.96–1.53) | 0.111 |
| Other (non-CRC) mortality | 608 | 0.93 (0.83–1.04) | 0.227 | 1.11 (0.97–1.26) | 0.128 | |
| All-cause mortality | 781 | 0.99 (0.90–1.09) | 0.766 | 1.12 (1.00–1.25) | 0.055 | |
| Added sugar | ||||||
| CRC-specific mortality | 14,618 | 173 | 1.10 (0.96–1.26) | 0.178 | 1.14 (0.96–1.36) | 0.132 |
| Other (non-CRC) mortality | 608 | 0.95 (0.88–1.03) | 0.218 | 1.02 (0.93–1.12) | 0.668 | |
| All-cause mortality | 781 | 0.99 (0.92–1.06) | 0.674 | 1.04 (0.95–1.13) | 0.400 | |
aPost-diagnosis intake was assessed at least 6 months but no more than 4 years after diagnosis.
bCox proportional hazards regression model adjusted for age groups at diagnosis (<60, 60–64, 65–69, 70–74 and ≥75 years), sex (women/men) and cancer stage (I, II, III and unspecified) as stratification factors, with additional adjustment for age at diagnosis (continuous).
cFurther adjusted for year of diagnosis (continuous), tumour grade of differentiation (1–3 and unspecified), subsite (proximal colon, distal colon, rectum and unspecified), history of diabetes (yes/no), pre-diagnosis intake of the respective beverage or sugar variable (<1, 1–4, ≥5 servings/week for sugar-sweetened and artificially sweetened beverages; <1, 1–4, 5–7 servings/week, >1 serving/day for fruit juice; sex-specific quartiles for sugar variables) and post-diagnosis alcohol consumption (<0.15, 0.15–1.9, 2.0–7.4, ≥7.5 grams/day), pack-years of smoking (0, 1–15, 16–25, 26–45, >45), BMI (<23, 23–24.9, 25–27.4, 27.5–29.9, ≥30 kg/m2), physical activity (women: <5, 5–11.4, 11.5–21.9, ≥22 MET-hours/week; men: <7, 7–14.9, 15–24.9, ≥25 MET-hours/week), regular use of aspirin or NSAIDs (≥2 tablets/week, yes/no), consumption of folate, calcium, vitamin D, red and processed meat and total energy intake (sex-specific quartiles), and, in women only, chemotherapy use (yes/no, available in women only) and post-menopausal hormone use (pre-menopausal, never, past, current users). Post- and pre-diagnosis sugar-sweetened beverage and artificially sweetened beverage intakes were mutually adjusted for each other (<1, 1–4, ≥5 servings/week), and the sugar intakes were additionally adjusted for post-diagnosis fruit and vegetable consumption (sex-specific quartiles).
dA continuous measure of intake was used for all except for artificially sweetened beverages in which categories of intake were used (<1, 1–4, ≥5 servings/week), with the HR for ≥5 servings/week compared to <1 serving/week (reference group) shown in the table.
All-cause and other (non-CRC) mortality
The fully adjusted multivariable HR per 1 serving/day of post-diagnosis SSBs was 1.11 (95% CI: 0.94–1.32) for all-cause mortality. Post-diagnosis fruit juice intake was not associated with all-cause or non-CRC mortality. However, for post-diagnosis ASB intake, HR comparing ≥5 versus <1 servings/week for all-cause mortality was 0.70 (95% CI: 0.55–0.89) which was similar, albeit weaker, to what was found for CRC-specific mortality. While there was no association between post-diagnosis total fructose or glucose intake with all-cause mortality in the age, sex and stage-adjusted model, these exposures were statistically significantly associated with worse prognosis in the fully adjusted models. No single covariate explained the difference in results between the simple and fully adjusted model by itself (data not shown). For all-cause mortality, the multivariable HR per 20-gram/day increment of post-diagnosis intake was 1.18 (95% CI: 1.04–1.35, P-value = 0.014) for total fructose, 1.17 (95% CI: 1.03–1.34, P-value = 0.02) for total glucose and 1.12 (95% CI 1.00–1.25, P-value = 0.06) for sucrose. While the HRs for each specific type of sugar and non-CRC mortality were comparable to those observed for all-cause mortality, none of these associations reached statistical significance.
Sensitivity analyses
Results remained materially similar in sensitivity analyses excluding participants with a history of diabetes, participants with FFQ assessment less than 1 year after diagnosis, and the first year of follow-up, though the sample size was diminished (data not shown). Results with and without adjustment for BMI were similar, and additional adjustment for weight change around the time of CRC diagnosis did not change results either (data not shown). As we only had treatment information for women, we reran analyses with and without adjustment for treatment in models restricted to women, and results were similar. Associations between added sugar intake and mortality were also similar when we defined post-diagnosis added sugar intake as percent of total energy intake per day (data not shown). When we examined sugar intake as categorical variables, HRs for CRC-specific, non-CRC and all-cause, mortality findings were generally similar to those presented in Table 2, however with the exception of post-diagnosis total fructose and glucose intake and all-cause mortality, associations did not reach statistical significance. Notably, the number of CRC deaths were low in each category and confidence intervals were also wide (Supplemental Table 2). Similarly, while the sample size was limited for the analysis of joint categories of low and high pre- and post-diagnosis intake, non-significant positive associations with CRC-specific mortality were observed for the joint categories where post-diagnosis SSB intake was high, while inverse associations were observed for the joint categories where post-diagnosis ASB intake was high, compared to the category with both low pre- and post-diagnosis intake at each time point for each respective beverage (Supplemental table 3).
Subgroup analyses
We explored whether the associations differed by subgroups of clinical and lifestyle factors. No significant interactions were observed by sex, pre-diagnosis intake, post-diagnosis physical activity or post-diagnosis alcohol consumption (Supplemental table 4). Associations between post-diagnosis intake of each type of sugar and mortality were stronger among patients with lower post-diagnosis BMI (<25 kg/m2), but a statistically significant interaction between post-diagnosis intake and BMI was not observed. Positive associations between post-diagnosis intake of SSBs, fruit juice, and each of the sugars and CRC-specific mortality were primarily seen in stage III patients, with HRs ranging from 1.21 for 1 serving/day of post-diagnosis fruit juice to 1.67 for 20 grams/day of post-diagnosis total fructose intake; though there were no statistically significant interactions by stage (P for interaction ranged between 0.62 for post-diagnosis SSBs to 0.07 for post-diagnosis total fructose).
Time since diagnosis
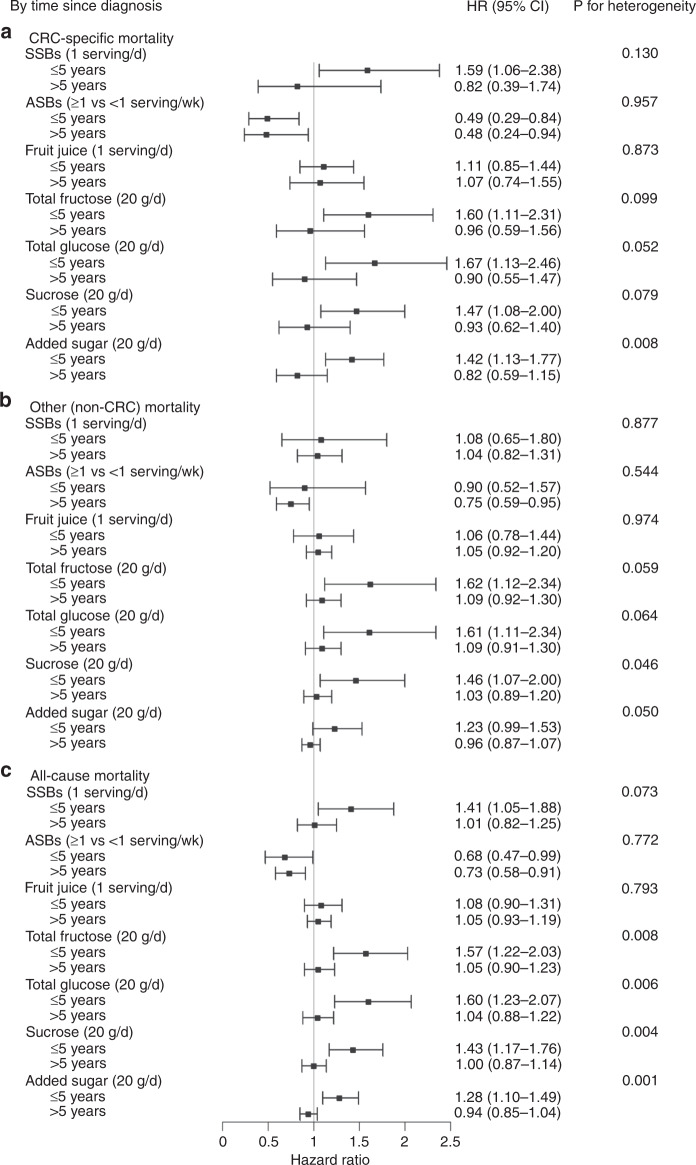
We also examined associations by follow-up time since diagnosis (≤5 and >5 years). 54% of all CRC-specific deaths occurred within the first 5 years after diagnosis and 52% of total deaths identified ≤5 years post-diagnosis were CRC-specific deaths while only 13% were CRC-specific deaths >5 years post-diagnosis. The multivariable HR for CRC-specific mortality per 1 serving/day increase in post-diagnosis SSB intake was 1.59 (95% CI: 1.06–2.38) for ≤5 years and 0.82 (95% CI: 0.39–1.74) for >5 years post-diagnosis (P for heterogeneity = 0.13; Fig. 1, Supplemental table 4). A similar pattern by time since diagnosis was observed for post-diagnosis total fructose, glucose, sucrose and added sugar intake and CRC-specific mortality. HRs for CRC-specific mortality per 20 grams/day of post-diagnosis intake ranged from 1.42 for added sugar to 1.67 for total glucose for ≤5 years, and 0.82 for added sugar to 0.96 for total fructose for >5 years from diagnosis; though P for heterogeneity was >0.05 for all except post-diagnosis added sugar (P for heterogeneity = 0.01). Inverse associations for post-diagnosis ASB intake and CRC-specific mortality were observed regardless of time since diagnosis.
Fig. 1. Associations between post-diagnosis intake and mortality by follow-up time since diagnosis.
Post-diagnosis sugar-sweetened beverage (SSBs), artificially sweetened beverages (ASBs), fruit juice and sugar intake and A colorectal-cancer (CRC)-specific mortality, B other mortality (deaths due to causes other than CRC) and C all-cause mortality by follow-up time since diagnosis (≤5 year [median = 5.0 years, range: 0.8–5.0 years] and >5 years [median = 12.9 years, range: 5.1–29.9 years]). The forest plot shows the hazard ratios (HR) and 95% confidence intervals (CI) per 1 serving per day of SSBs and fruit juice, ≥1 compared to <1 serving/week of ASBs and per 20 g per day for each type of sugar. HRs are adjusted for the same covariates as in Table 2. P-values for heterogeneity by time were evaluated using the Q-test statistic.
Discussion
In this prospective study of stage I–III CRC patients, we observed positive associations between post-diagnosis total fructose and glucose intake and all-cause mortality which was independent of pre-diagnosis intake. After limiting follow-up to the first 5 years after CRC diagnosis, when a greater proportion of deaths were due to CRC, we found significant positive associations between post-diagnosis SSB and sugar and CRC-specific and all-cause mortality. Post-diagnosis intake of SSBs and sugars were not statistically significantly associated with CRC-specific or all-cause mortality >5 years after diagnosis. Furthermore, a statistically significant inverse association was seen between post-diagnosis ASBs and CRC-specific and all-cause mortality regardless of time from diagnosis.
SSB and sugar intake have been explored in relation to CRC incidence previously. In a pooled analysis of 13 prospective studies, no association was observed between intake of 550 grams/day (~>18 ounces/day) of sugar-sweetened carbonated soft drinks versus none and colon cancer incidence [26]. In a previous analysis in NHS and HPFS, higher risk of CRC was observed with higher fructose and sucrose intake in men, but not women, and the association was stronger among overweight men [27]. In contrast, a meta-analysis of six studies did not observe an association between fructose and sucrose intake and risk of CRC [28].
There is limited prior literature examining SSB and sugar intake with CRC survival. A few studies have observed positive associations between post-diagnosis dietary patterns, which included SSBs as a component, and CRC survival [6, 7]. In the Cancer and Leukemia Group B (CALGB) 89803 trial, a cohort of stage III colon cancer patients, SSB consumption was positively associated with colon cancer recurrence and mortality, but only among patients who consumed ≥2 servings/day compared to those with <2 servings/month [12]. Due to limited numbers of patients with ≥2 servings/day of SSBs, we were unable to assess this intake level in our cohorts. In our study, only 13% of cases reported SSB consumption ≥5 servings/week. Compared to adults in the National Health and Nutrition Examination Survey 2011–2012 [29], added sugar consumption was lower in our participants. On average, U.S. adults consumed about 14% of their total energy from added sugar versus 10% in our study, and notably, more than 75% of our participants consumed <14% of total energy from added sugars. Hence, we had a restricted range of sugar intake which may have limited our ability to detect associations with higher levels of SSB consumption and added sugar intake.
In the CALGB cohort, higher post-diagnosis total fructose intake was significantly associated with worse recurrence-free but not disease-free or overall survival. In that study, higher glycemic load and total carbohydrate intake had the strongest positive associations with mortality [8]. A higher post-diagnosis insulin score has previously been associated with increased CRC-specific and all-cause mortality in the NHS and HPFS [9]. Yet, SSBs and sugars are only one component of total carbohydrate intake, and other macronutrients, such as protein and fat, can also induce insulin secretion [30]. Our analyses were adjusted for fruit and vegetable intake, a natural source of sugar, thus post-diagnosis total fructose intake could be interpreted as fructose from sources other than fruits and vegetables. Fruits and vegetables provide beneficial micronutrients and fiber, which could offset the possible negative effects of sugar. Added sugars in beverages and ultra-processed foods, on the other hand, do not induce satiety, which promotes overconsumption, leading to obesity and insulin resistance [31]. Our findings suggested that positive associations between post-diagnosis intake of sugar and mortality may be stronger among patients with lower post-diagnosis BMI (<25 kg/m2); however, P for interaction did not reach statistical significance. Given that BMI is an inaccurate measure for visceral obesity and skeletal muscle mass, and the controversies surrounding the role of obesity in CRC survival (“obesity paradox”) [32], these results need to be interpreted with caution. Nonetheless, adjustment for BMI or weight change (pre versus post-diagnosis weight) did not change our results materially.
When limiting follow-up to the first 5 years after diagnosis, we found significant positive associations between post-diagnosis intake of SSBs, total fructose, glucose, sucrose and added sugar with CRC-specific and all-cause mortality. The majority of CRC deaths occurred within the first 5 years after diagnosis, and half of all deaths in the first 5 years were CRC-specific deaths compared to 13% after 5 years from diagnosis. While these results suggest that the exposure-survival relationship may be strongest during this time that is most critical for the biological history of CRC progression and survival [33], another possible explanation for the lack of association among people surviving >5 years post-diagnosis may be the lower number of CRC-specific deaths in that group.
A possible mechanism underlying the positive association between post-diagnosis SSB and sugar intake and mortality may be through alterations to the insulin-like growth factor axes [1]. Obesity [4], low physical activity [2, 5], and high glycemic load [8, 28] are all associated with insulin resistance and have been linked to both CRC incidence and survival. Insulin stimulates cell proliferation and colon carcinogenesis in studies of colon cancer cell lines and animal models [34, 35]. However, while we adjusted for pre-diagnosis intake in our multivariable analyses, the possibility that insulin resistance prior to diagnosis may have contributed to more aggressive cancers cannot be excluded. Inflammation is also hypothesised as a possible mechanism for CRC survival. In one study, C-reactive protein, a general marker of inflammation, was positively associated with CRC-specific and all-cause mortality [36]. Added sugar, particularly in the form of SSBs, contributes to inflammation [11]. In the HPFS, SSB consumption was associated with an increased risk of plasma concentrations of inflammatory cytokines [37].
In human and animal feeding studies, higher fructose intake contributed to insulin resistance, impaired glucose tolerance, and hyperinsulinemia [38, 39]. Fructose was also positively associated with plasma C-peptide levels, a marker of insulin resistance in a previous analysis in the NHS [40], and higher pre-diagnosis C-peptide plasma levels were associated with almost a doubling of all-cause mortality among non-metastatic CRC patients in the NHS and HPFS [41]. Furthermore, unlike glucose, fructose is metabolised predominantly in the liver and higher fructose intake can alter hepatic insulin and lipid metabolism [16, 17]. Fructose intake has also been linked to non-alcoholic fatty liver disease (NAFLD) [42], the most common chronic liver disease worldwide [43], which can increase inflammatory processes and alter the liver immune microenvironment [44]. Correspondingly, most CRC deaths are caused by liver metastases [45], and deaths caused by liver metastases in early stage patients treated with resection and chemotherapy are probably due to progression of liver micro-metastases undetected at the time of diagnosis [46]. Taken together, while the mechanisms remain unclear, it is possible that an unfavourable liver microenvironment may at least in part contribute to the initiation and progression of liver metastases; [45] however, more research into a potential role of NAFLD and its effect on the liver microenvironment and metastasis is needed before any conclusions can be drawn. Interestingly, in a cross-sectional analysis in the Framingham cohorts, higher SSB but not diet soda intake was associated with higher risk of fatty liver disease [47].
In addition to CRC-related deaths, higher consumption of fructose and SSBs is also associated with weight gain, type 2 diabetes, and cardiovascular disease, which could explain the positive association with non-CRC-related and all-cause mortality in our analyses [11]. Higher cardiovascular disease-specific and overall mortality has been observed among participants with high added sugar, SSB, and total fructose intake when compared to those with low intake [48–50].
We cannot explain the significant inverse association we observed for post-diagnosis ASB consumption and CRC-specific mortality. First, we cannot exclude the possibility of a chance finding. Second, while replacement or substitution of SSBs with ASBs possibly resulting in more favourable insulin and lipid profiles may be one possible explanation, inverse associations were still observed after adjusting for both pre- and post-diagnosis SSB intake. Results also remained similar after further adjustment for a composite diet quality score, the AHEI-2010, suggesting that associations may not be driven by an overall healthier diet pattern. Finally, different artificial sweeteners (e.g. saccharin versus. aspartame) have distinct chemical characteristics and properties, further hampering interpretation of our findings [51]. Interestingly, the CALGB cohort, to our knowledge the only other study that has examined post-diagnosis ASB consumption and mortality, also reported lower cancer recurrence or mortality with higher post-diagnosis ASB consumption among stage III colon cancer patients [15]. While pre-diagnosis ASB intake was not adjusted for in the CALGB study, adjustment for pre-diagnosis intake strengthened the inverse association for post-diagnosis ASB intake and mortality in our study.
Strengths of our study include the prospective study design with detailed collection of post-diagnosis dietary intake and other covariate information, as well as pre-diagnosis intake data. Our study had several limitations worth noting. First, although our FFQs are well validated [52–55], exposure misclassification is still possible as dietary intakes are self-reported. However, findings from our cohorts on diet and CRC are similar to those observed in other cohorts [2], and we also used cumulative updated intake which better represents long-term intake over time. Moreover, dietary information was collected prospectively and any misclassification of exposure would likely have biased findings towards the null. Second, consumption of SSBs and sugars was low in our participants, thus we could not assess these associations at higher consumption levels. Third, we were neither able to differentiate between the various types of artificial sweeteners, nor could we account for total consumption of artificial sweeteners in the diet from all sources. Fourth, we also lacked detailed information on treatment; however, most patients were diagnosed with stage I or II disease, in which surgery alone would generally be standard of care. Although differences in the use of adjuvant chemotherapy is possible, we adjusted for stage of disease and year of diagnosis, a proxy for differences in standard chemotherapy treatments over the study period. Fifth, we also cannot exclude the possibility of residual or unmeasured confounding. However, we adjusted for prognostic factors and various lifestyle and dietary factors including major CRC risk factors. Finally, for subgroup analyses, statistical power was limited, as the number of CRC-specific deaths was relatively small.
In conclusion, higher post-diagnosis total fructose and glucose intake was associated with higher all-cause mortality in stage I to III CRC patients. We also observed positive associations between post-diagnosis SSBs and sugars and CRC-specific mortality, but only up to 5 years after diagnosis, when more deaths were due to CRC. Our results warrant further examination into the role of sugar, SSBs and ASBs in CRC survival.
Supplementary information
Acknowledgements
We would like to thank the participants and staff of the Nurses’ Health Study and the Health Professionals Follow-up Study for their valuable contributions as well as the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, WY. We assume full responsibility for analyses and interpretation of these data. An earlier draft of this paper has been deposited in the Digital Access to Scholarship at Harvard repository [56].
Author contributions
ESZ, SAS-W, MW, MJS, ELG and KW contributed to the study concept and design. MJS and ELG contributed to the data acquisition and analysis. ESZ conducted the statistical analysis. ESZ, KW and ELG drafted the initial manuscript. All authors contributed to the data interpretation and provided critical revisions of the final manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Institutes of Health grants UM1 CA186107, U01 CA167552, P01 CA87969, P50 CA127003, R35 CA197735 and P01 CA 55075, as well as R35 CA253185 to ATC, R01 CA205406 to KN, R03 CA197879 to KW, R21 CA222940 to KW, R21 CA230873 to KW and SO. ESZ was supported in part by National Institutes of Health training grants T32 CA009001, R25 CA098566 and T32 HL125232. JAM is supported by the Douglas Gray Woodruff Chair fund, the Guo Shu Shi Fund, Anonymous Family Fund for Innovations in Colorectal Cancer and the Karen Guo Colon Cancer Research Fund. ATC is a Stuart and Suzanne Steele MGH Research Scholar. KN is supported in part by the Project P Fund. This study was also funded in part by a grant from the American Institute for Cancer Research to KW. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data availability
Further information including the procedures to obtain and access data from the Nurses’ Health Studies and Health Professionals Follow-up Study is described at https://www.nurseshealthstudy.org/researchers (contact email: nhsaccess@channing.harvard.edu) and https://sites.sph.harvard.edu/hpfs/for-collaborators/.
Competing interests
CSF reports consulting role for Amylin Pharmaceuticals, Astra-Zeneca, Bain Capital, CytomX Therapeutics, Daiichi-Sankyo, Eli Lilly, Entrinsic Health, Evolveimmune Therapeutics, Genentech, Merck, Taiho and Unum Therapeutics. He also serves as a Director for CytomX Therapeutics and owns unexercised stock options for CytomX and Entrinsic Health. He is a co-Founder of Evolveimmune Therapeutics and has equity in this private company. He had provided expert testimony for Amylin Pharmaceuticals and Eli Lilly. CSF is now an employee of Genentech and Roche. JAM received institutional research funding from Boston Biomedical and has served as an advisor/consultant to Ignyta, Taiho and Cota; though this study was not funded by any of these commercial entities. ATC has received consulting fees from Bayer Pharma AG, Pfizer Inc, and Boehringer Ingelheim for work unrelated to this manuscript. He has also served as an investigator on a trial funded by Zoe Global Ltd. KN has received institutional research funding from Pharmavite, Evergrande Group, Janssen and Revolution Medicines. She has also served on an advisory board for Seattle Genetics, Array Biopharma and BiomX, and has served as a consultant to X-Biotix Therapeutics. The remaining authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the institutional review boards of the Brigham and Women’s Hospital and Harvard T.H. Chan School of Public Health, and those of participating registries as required. Return of questionnaires was considered to imply informed consent. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Edward L. Giovannucci, Kana Wu.
Supplementary information
The online version contains supplementary material available at 10.1038/s41416-021-01487-7.
References
- 1.Davies M, Gupta S, Goldspink G, Winslet M. The insulin-like growth factor system and colorectal cancer: clinical and experimental evidence. Int J Colorectal Dis. 2006;21:201–8. doi: 10.1007/s00384-005-0776-8. [DOI] [PubMed] [Google Scholar]
- 2.World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. Continuous Update Project Expert Report. 2018. dietandcancerreport.org.
- 3.Larsson SC, Orsini N, Wolk A. Diabetes mellitus and risk of colorectal cancer: a meta-analysis. J Natl Cancer Inst. 2005;97:1679–87. doi: 10.1093/jnci/dji375. [DOI] [PubMed] [Google Scholar]
- 4.Lee J, Meyerhardt JA, Giovannucci E, Jeon JY. Association between body mass index and prognosis of colorectal cancer: a meta-analysis of prospective cohort studies. PLoS ONE. 2015;10:e0120706. doi: 10.1371/journal.pone.0120706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmid D, Leitzmann MF. Association between physical activity and mortality among breast cancer and colorectal cancer survivors: a systematic review and meta-analysis. Ann Oncol. 2014;25:1293–311. doi: 10.1093/annonc/mdu012. [DOI] [PubMed] [Google Scholar]
- 6.Fung TT, Kashambwa R, Sato K, Chiuve SE, Fuchs CS, Wu K, et al. Post diagnosis diet quality and colorectal cancer survival in women. PLoS ONE. 2014;9:e115377. doi: 10.1371/journal.pone.0115377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meyerhardt JA, Niedzwiecki D, Hollis D, Saltz LB, Hu FB, Mayer RJ, et al. Association of dietary patterns with cancer recurrence and survival in patients with stage III colon cancer. JAMA. 2007;298:754–64. doi: 10.1001/jama.298.7.754. [DOI] [PubMed] [Google Scholar]
- 8.Meyerhardt JA, Sato K, Niedzwiecki D, Ye C, Saltz LB, Mayer RJ, et al. Dietary glycemic load and cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Natl Cancer Inst. 2012;104:1702–11. doi: 10.1093/jnci/djs399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yuan C, Bao Y, Sato K, Nimptsch K, Song M, Brand-Miller JC, et al. Influence of dietary insulin scores on survival in colorectal cancer patients. Br J Cancer. 2017;117:1079–87. doi: 10.1038/bjc.2017.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones LW, Demark-Wahnefried W. Diet, exercise, and complementary therapies after primary treatment for cancer. Lancet Oncol. 2006;7:1017–26. doi: 10.1016/S1470-2045(06)70976-7. [DOI] [PubMed] [Google Scholar]
- 11.Malik VS, Hu FB. Fructose and cardiometabolic health: what the evidence from sugar-sweetened beverages tells us. J Am Coll Cardiol. 2015;66:1615–24. doi: 10.1016/j.jacc.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fuchs MA, Sato K, Niedzwiecki D, Ye X, Saltz LB, Mayer RJ, et al. Sugar-sweetened beverage intake and cancer recurrence and survival in CALGB 89803 (Alliance) PLoS ONE. 2014;9:e99816. doi: 10.1371/journal.pone.0099816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev. 2013;14:606–19. doi: 10.1111/obr.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fakhouri THI, Kit BK, Ogden CL. Consumption of diet drinks in the United States, 2009‒2010. NCHS data brief, no 109. Hyattsville, MD: National Center for Health Statistics. 2012. [PubMed]
- 15.Guercio BJ, Zhang S, Niedzwiecki D, Li Y, Babic A, Morales-Oyarvide V, et al. Associations of artificially sweetened beverage intake with disease recurrence and mortality in stage III colon cancer: Results from CALGB 89803 (Alliance) PLoS ONE. 2018;13:e0199244. doi: 10.1371/journal.pone.0199244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ludwig DS. Examining the health effects of fructose. JAMA. 2013;310:33–34. doi: 10.1001/jama.2013.6562. [DOI] [PubMed] [Google Scholar]
- 17.Softic S, Cohen DE, Kahn CR. Role of dietary fructose and hepatic de novo lipogenesis in fatty liver disease. Dig Dis Sci. 2016;61:1282–93. doi: 10.1007/s10620-016-4054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Women’s Health. 1997;6:49–62. doi: 10.1089/jwh.1997.6.49. [DOI] [PubMed] [Google Scholar]
- 19.Rimm EB, Giovannucci EL, Willett WC, Colditz GA, Ascherio A, Rosner B, et al. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet. 1991;338:464–8. doi: 10.1016/0140-6736(91)90542-W. [DOI] [PubMed] [Google Scholar]
- 20.Stampfer MJ, Willett WC, Speizer FE, Dysert DC, Lipnick R, Rosner B, et al. Test of the National Death Index. Am J Epidemiol. 1984;119:837–9. doi: 10.1093/oxfordjournals.aje.a113804. [DOI] [PubMed] [Google Scholar]
- 21.Willet W. Nutritional Epidemiology. 3rd edn. New York: Oxford University Press; 2012.
- 22.Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120:1011–20. doi: 10.1161/CIRCULATIONAHA.109.192627. [DOI] [PubMed] [Google Scholar]
- 23.Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65:1220S–1228S. doi: 10.1093/ajcn/65.4.1220S. [DOI] [PubMed] [Google Scholar]
- 24.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 25.McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76:1261–71. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X, Albanes D, Beeson WL, van den Brandt PA, Buring JE, Flood A, et al. Risk of colon cancer and coffee, tea, and sugar-sweetened soft drink intake: pooled analysis of prospective cohort studies. J Natl Cancer Inst. 2010;102:771–83. doi: 10.1093/jnci/djq107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Michaud DS, Fuchs CS, Liu S, Willett WC, Colditz GA, Giovannucci E. Dietary glycemic load, carbohydrate, sugar, and colorectal cancer risk in men and women. Cancer Epidemiol Biomark Prev. 2005;14:138–47. doi: 10.1158/1055-9965.EPI-05-0428. [DOI] [PubMed] [Google Scholar]
- 28.Aune D, Chan DS, Lau R, Vieira R, Greenwood DC, Kampman E, et al. Carbohydrates, glycemic index, glycemic load, and colorectal cancer risk: a systematic review and meta-analysis of cohort studies. Cancer Causes Control. 2012;23:521–35. doi: 10.1007/s10552-012-9918-9. [DOI] [PubMed] [Google Scholar]
- 29.Powell ES, Smith-Taillie LP, Popkin BM. Added sugars intake across the distribution of US children and adult consumers: 1977-2012. J Acad Nutr Diet. 2016;116:1543–50 e1541. doi: 10.1016/j.jand.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holt SH, Miller JC, Petocz P. An insulin index of foods: the insulin demand generated by 1000-kJ portions of common foods. Am J Clin Nutr. 1997;66:1264–76. doi: 10.1093/ajcn/66.5.1264. [DOI] [PubMed] [Google Scholar]
- 31.Willett WC, Ludwig DS. Science souring on sugar. BMJ. 2013;346:e8077. doi: 10.1136/bmj.e8077. [DOI] [PubMed] [Google Scholar]
- 32.Caan BJ, Meyerhardt JA, Kroenke CH, Alexeeff S, Xiao J, Weltzien E, et al. Explaining the obesity paradox: the association between body composition and colorectal cancer survival (C-SCANS Study) Cancer Epidemiol Biomark Prev. 2017;26:1008–15. doi: 10.1158/1055-9965.EPI-17-0200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Noone A. M, Howlader N, Krapcho M, Miller D, Brest A, Yu M, et al. (eds). SEER Cancer Statistics Review, 1975-2015 (based on November 2017 SEER data submission). Bethesda: National Cancer Institute; 2018.
- 34.Tran TT, Medline A, Bruce WR. Insulin promotion of colon tumors in rats. Cancer Epidemiol Biomark Prev. 1996;5:1013–5. [PubMed] [Google Scholar]
- 35.Sun J, Jin T. Both Wnt and mTOR signaling pathways are involved in insulin-stimulated proto-oncogene expression in intestinal cells. Cell Signal. 2008;20:219–29. doi: 10.1016/j.cellsig.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 36.Cooney RV, Chai W, Franke AA, Wilkens LR, Kolonel LN, Le Marchand, L. C-reactive protein, lipid-soluble micronutrients, and survival in colorectal cancer patients. Cancer Epidemiol Biomark Prev. 2013;22:1278–88. [DOI] [PMC free article] [PubMed]
- 37.de Koning L, Malik VS, Kellogg MD, Rimm EB, Willett WC, Hu FB. Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men. Circulation. 2012;125:1735–41. doi: 10.1161/CIRCULATIONAHA.111.067017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thorburn AW, Storlien LH, Jenkins AB, Khouri S, Kraegen EW. Fructose-induced in vivo insulin resistance and elevated plasma triglyceride levels in rats. Am J Clin Nutr. 1989;49:1155–63. doi: 10.1093/ajcn/49.6.1155. [DOI] [PubMed] [Google Scholar]
- 39.Beck-Nielsen H, Pedersen O, Lindskov HO. Impaired cellular insulin binding and insulin sensitivity induced by high-fructose feeding in normal subjects. Am J Clin Nutr. 1980;33:273–8. doi: 10.1093/ajcn/33.2.273. [DOI] [PubMed] [Google Scholar]
- 40.Wu T, Giovannucci E, Pischon T, Hankinson SE, Ma J, Rifai N, et al. Fructose, glycemic load, and quantity and quality of carbohydrate in relation to plasma C-peptide concentrations in US women. Am J Clin Nutr. 2004;80:1043–9. doi: 10.1093/ajcn/80.4.1043. [DOI] [PubMed] [Google Scholar]
- 41.Wolpin BM, Meyerhardt JA, Chan AT, Ng K, Chan JA, Wu K, et al. Insulin, the insulin-like growth factor axis, and mortality in patients with nonmetastatic colorectal cancer. J Clin Oncol. 2009;27:176–85. doi: 10.1200/JCO.2008.17.9945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jensen T, Abdelmalek MF, Sullivan S, Nadeau KJ, Green M, Roncal C, et al. Fructose and sugar: a major mediator of non-alcoholic fatty liver disease. J Hepatol. 2018;68:1063–75. doi: 10.1016/j.jhep.2018.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Perumpail BJ, Khan MA, Yoo ER, Cholankeril G, Kim D, Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol. 2017;23:8263–76. doi: 10.3748/wjg.v23.i47.8263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Agosti P, Sabba C, Mazzocca A. Emerging metabolic risk factors in hepatocellular carcinoma and their influence on the liver microenvironment. Biochim Biophys Acta Mol Basis Dis. 2018;1864:607–17. doi: 10.1016/j.bbadis.2017.11.026. [DOI] [PubMed] [Google Scholar]
- 45.Langley RR, Fidler IJ. The seed and soil hypothesis revisited-the role of tumor-stroma interactions in metastasis to different organs. Int J Cancer. 2011;128:2527–35. doi: 10.1002/ijc.26031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Andre N, Schmiegel W. Chemoradiotherapy for colorectal cancer. Gut. 2005;54:1194–202. doi: 10.1136/gut.2004.062745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ma J, Fox CS, Jacques PF, Speliotes EK, Hoffmann U, Smith CE, et al. Sugar-sweetened beverage, diet soda, and fatty liver disease in the Framingham Heart Study cohorts. J Hepatol. 2015;63:462–9. doi: 10.1016/j.jhep.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med. 2014;174:516–24. doi: 10.1001/jamainternmed.2013.13563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tasevska N, Park Y, Jiao L, Hollenbeck A, Subar AF, Potischman N. Sugars and risk of mortality in the NIH-AARP Diet and Health Study. Am J Clin Nutr. 2014;99:1077–88. doi: 10.3945/ajcn.113.069369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Malik VS, Li Y, Pan A, De Koning L, Schernhammer E, Willett WC, et al. Long-term consumption of sugar-sweetened and artificially sweetened beverages and risk of mortality in US adults. Circulation. 2019;139:2113–25. doi: 10.1161/CIRCULATIONAHA.118.037401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pearlman M, Obert J, Casey L. The association between artificial sweeteners and obesity. Curr Gastroenterol Rep. 2017;19:64. doi: 10.1007/s11894-017-0602-9. [DOI] [PubMed] [Google Scholar]
- 52.Feskanich D, Rimm EB, Giovannucci EL, Colditz GA, Stampfer MJ, Litin LB, et al. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc. 1993;93:790–6. doi: 10.1016/0002-8223(93)91754-E. [DOI] [PubMed] [Google Scholar]
- 53.Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B, et al. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol. 1989;18:858–67. doi: 10.1093/ije/18.4.858. [DOI] [PubMed] [Google Scholar]
- 54.Al-Shaar L, Yuan C, Rosner B, Dean SB, Ivey KL, Clowry CM, et al. Reproducibility and validity of a semi-quantitative food frequency questionnaire in men assessed by multiple methods. Am J Epidemiol. 2020. 10.1093/aje/kwaa280. [DOI] [PMC free article] [PubMed]
- 55.Yuan C, Spiegelman D, Rimm EB, Rosner BA, Stampfer MJ, Barnett JB, et al. Validity of a dietary questionnaire assessed by comparison with multiple weighed dietary records or 24-hour recalls. Am J Epidemiol. 2017;185:570–84. doi: 10.1093/aje/kww104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zoltick ES. Nutritional and lifestyle factors for cancer incidence and survival. 2016. Preprint at http://nrs.harvard.edu/urn-3:HUL.InstRepos:32644537.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Further information including the procedures to obtain and access data from the Nurses’ Health Studies and Health Professionals Follow-up Study is described at https://www.nurseshealthstudy.org/researchers (contact email: nhsaccess@channing.harvard.edu) and https://sites.sph.harvard.edu/hpfs/for-collaborators/.