Abstract
Introduction and importance
Benign fibroblastic proliferation located within the scrotum are uncommon. They are also identified as fibrous pseudotumour and usually arise from the paratesticular region. Their pathogenesis is unknown. These tumours are difficult to diagnose pre-operatively and resemble intra-scrotal malignancy.
Case presentation
We managed a 26-year-old Nigerian man with a five-year history of left sided hemiscrotal swelling. The mass was excised, and histology showed benign fibroblastic proliferation.
Discussion
Most paratesticular tumours are benign. Imaging studies that show the mass as separate from the testis, normal levels of tumour markers and clinical features not suggestive of malignancy make the case for organ-sparing mass excision, in the treatment of paratesticular fibrous pseudotumour, very strong.
Conclusion
Intra-scrotal benign fibrous proliferation is a challenge to diagnose pre-operatively but excision of this benign mass without an orchidectomy is practicable when pre-operative assessment suggests a benign disease.
Keywords: Benign fibroblastic proliferation, Inflammatory pseudotumour, Scrotal swelling, Rare tumour, Fibroma, Case report
Highlights
-
•
Paratesticular fibrous pseudotumours are benign and uncommon.
-
•
Pre-operative diagnosis of these tumours is difficult, and they resemble intra-scrotal malignancy.
-
•
Many cases are diagnosed post-operatively from orchidectomy specimen.
-
•
Organ-sparing mass excision is practicable with appropriate pre-operative evaluation.
1. Introduction
Paratesticular fibrous proliferations are benign and rare. They arise from testicular tunics and in about 85% of the time, they arise from the tunica vaginalis [1]. Occasionally are found to grow into the epididymis and spermatic cord with epididymal involvement being less than 10% [2]. The tunica albuginea may also be a site of origin [1]. Various names have been used for this lesion such as inflammatory pseudotumour, inflammatory myofibroblastic tumour, fibroma and proliferative funiculitis The third decade of life is when they usually occur but other age groups may also be affected [3], [4]. The clinical picture mimics malignancy hence diagnosis is usually made post-operatively from an orchidectomy specimen [5]. This work has been reported in line with the SCARE 2020 criteria [6].
2. Case presentation
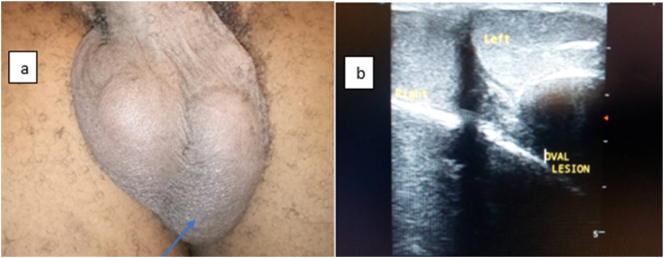
A 26-year-old man presented at our Urology clinic with a five- year history of progressive left hemiscrotal swelling. The swelling was not painful, there was no history of lower urinary tract symptoms, drenching night sweats, cough, weight loss or fever. Physical examination revealed a non-tender, hard left hemiscrotal mass about 4 cm × 2 cm around the lower pole of the ipsilateral testis (Fig. 1a). The mass could not be felt distinctly from the testis. The right testis felt normal in size and consistency. There were no abnormal findings on abdominal and inguinal examination. A clinical diagnosis of a left intra-scrotal calcification was made. Ultrasound of the scrotum showed a solitary lesion floating within the left hemiscrotum not attached to the testis, measuring 2.9 cm × 2.3 cm × 2.0 cm (Fig. 1b). It was of reduced echogenicity in comparison to the ipsilateral testis. The mass was intact and had a uniform outline. The right and left testes appeared normal. Differential diagnosis were fibroma and supernumerary testis. The patient had normal complete blood count. Serum β- human chorionic gonadotrophin, α-fetoprotein and blood chemistry was within normal limits. At operation the mass which was found to arise from the tunica vaginalis was excised (Fig. 2). The patient had an uneventful post-operative recovery and was discharged home.
Fig. 1.
a: pre-operative picture with arrow pointing to the left hemiscrotal mass and b: Scrotal ultrasound showing left hemiscrotal mass as oval lesion.
Fig. 2.
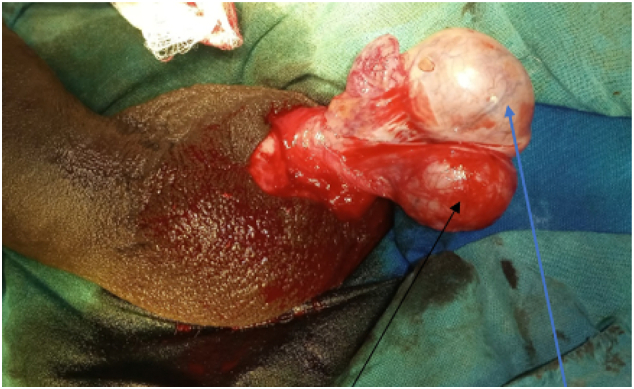
Intra-operative picture with blue arrow pointing to the left testis and black arrow pointing to the left hemiscrotal mass. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Pathology report: Gross specimen was a piece of hard greyish white tissue measuring 3 cm × 2.5 cm × 2 cm. Cut section showed greyish white surfaces. Microscopic examination showed predominant interlacing fascicles of fibroblast and collagen. There were foci containing small sized blood vessels and infiltrates of mononuclear inflammatory cells were seen (Fig. 3).
Fig. 3.
a: Photomicrograph shows predominantly interlacing fascicles of fibroblast and collagen. Foci containing small sized blood vessels and infiltrates of mononuclear inflammatory cells are seen (Haematoxylin and Eosin stain at ×10 magnification), b: Immunohistochemistry photomicrograph showing tumour cells that are negative for cytoplasmic expression of Smooth muscle actin filament. The benign vascular channels are however positive (SMA X10), c: Photomicrograph showing immunuhistologically negative cytoplasmic expression of Desmin filament (Desmin × 10) and d: Photomicrograph showing focal immunohistological expression of S100 (S100 × 10).
Immunohistochemistry showed tumour cells negative for smooth muscle actin (SMA). Desmin was negative with S100 being focally positive. The final histologic diagnosis was Benign fibroblastic proliferation.
3. Discussion
Paratesticular fibrous pseudotumour was first described by Balloch in 1904 [7]. Fibrous pseudotumour account for about 6% of paratesticular tumours [3], [4].
The aetiology of this rare tumour is still unclear but is generally considered to be a benign reactive proliferation of inflammatory and fibrous tissue probably in response to trauma, infection or inflammation [8].
Pre-operative diagnosis is challenging as the lesion tends to mimic malignancy. However, unlike testicular tumours of which about 95% are malignant, most paratesticular tumours are benign [9]. Hence, it is prudent to consider a benign disease process when imaging studies such as ultrasound suggest a lesion that is separate from the testis as in the index case. Furthermore, normal levels of tumour markers point more towards a benign condition. The presentation at 5 years of this slow growing swelling in an otherwise fit man with no other symptoms made a benign condition very likely.
Organ sparing surgeries may be impossible in cases where imaging is unable to show a separation between the testis and the lesion. This is especially the case in fibromatous periorchitis, a variety of benign fibrous proliferation, in which there is diffuse proliferative testicular encasement [10], [11]. Scrotal exploration with frozen section biopsy has been advocated as the best option by Tobias-machado et al. [12] to save the testis. However, in their case report a radical orchidectomy was eventually done as the frozen section result was unable to ascertain if the tumour was a fibroma or a low grade fibrosarcomma. Furthermore, the studies in support of frozen section to prevent radical orchidectomy are sparse [1].
4. Conclusion
Intra-scrotal fibrous pseudotumor though challenging to diagnose pre-operatively is amenable to simple excision when pre-operative assessment suggests a benign disease.
Funding
This research did not receive any grant from funding agencies in the public, commercial or not-for-profit sectors.
Ethical approval
Ethical approval was obtained for this research.
Human Research and Ethics Committee, Federal Teaching Hospital Ido-Ekiti, Nigeria. Potocol no. ERC/2021/05/25/549A.
Consent
Written and informed consent obtained from patient.
Author contribution
PAE: Wrote manuscript and did literature search.
OO: Handled histopathological diagnosis and photomicrographs.
AIO: Contributed to manuscript write-up and literature search.
CCA: Handled radiological diagnosis and images.
OAO: Proof- read and approved final version of manuscript.
All authors have read and approved the manuscript.
Research registration
N/A
Guarantor
Peter Amenaghawon EGHAREVBA, Urologist, Fellow of West African College of Surgeons, Urology Unit, Department of Surgery, FETHI, Ekiti State, Nigeria.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors declare no conflict of interest regarding this article.
Acknowledgements
Department of Surgery, Federal Teaching Hospital Ido-Ekiti, Ekiti State, Nigeria.
Contributor Information
P.A. Egharevba, Email: peteregharevba@yahoo.com.
O. Omoseebi, Email: omoseebidipo@yahoo.com.
A.I. Okunlola, Email: okunlolaai@abuad.edu.ng.
C.C. Achebe, Email: achikky@yahoo.com.
O.A. Omisanjo, Email: sanjofunmi@yahoo.com.
References
- 1.Kodama H., Hatakeyama S., Matsumoto T., Tanaka T., Horiguchi H., Kubota Y. A case of fibrous pseudotumor in the scrotum: challenge for diagnosis and testicular preservation. Case Rep. Urol. 2018 Jan;17(2018) doi: 10.1155/2018/6904827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khallouk A., Ahallal Y., Tazi E., Tazi M.F., Elfassi M.J., Farih M.H. Benign paratesticular fibrous pseudotumor with malignant clinical features. Rev. Urol. 2011;13(4):e203–e205. [PMC free article] [PubMed] [Google Scholar]
- 3.Singh J., Hafiz A., Rasool M., Singh H., Sharma S., Bashir S. Fibrous pseudotumor of paratestis mimicking a testicular tumor. Open Pathol. J. 2014 Jun;13(8):1–3. [Google Scholar]
- 4.Ugras S., Yesil C. Fibrous pseudotumors of tunica albuginea, tunica vaginalis and epididymis: report of two cases. Cancer Epidemiol. 2009 Jul 1;33(1):69–71. doi: 10.1016/j.canep.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Sönmez K., Türkyilmaz Z., Boyacioğlu M., Edali M.N., Özen O., Başaklar A.C. Diffuse fibrous proliferation of tunica vaginalis associated with testicular infarction: a case report. J. Pediatr. Surg. 2001 Jul 1;36(7):1057–1058. doi: 10.1053/jpsu.2001.24745. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2020 Dec;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Balloch E.A.I.X. Fibromata of the tunica vaginalis. Ann. Surg. 1904 Mar;39(3):396–402. doi: 10.1097/00000658-190403000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones M.A., Young R.H., Scully R.E. Benign fibromatous tumors of the testis and paratesticular region: a report of 9 cases with a proposed classification of fibromatous tumors and tumor-like lesions. Am. J. Surg. Pathol. 1997 Mar;31(3):296–305. doi: 10.1097/00000478-199703000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Başal Ş., Malkoç E., Aydur E., Yıldırım İ., Kibar Y., Kurt B. Fibrous pseudotumors of the testis: the balance between sparing the testis and preoperative diagnostic difficulty. Turk. J. Urol. 2014 Sep;40(3):125–129. doi: 10.5152/tud.2014.21284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mutreja D., Murali M., Arya A. Pseudotumors of paratesticular region mimicking malignancy. Arch. Int. Surg. 2013 Jan 1;3(1):70. [Google Scholar]
- 11.White W.M., Hilsenbeck J., Waters W.B. Fibromatous periorchitis of testis. Urology. 2006 Mar 1;67(3) doi: 10.1016/j.urology.2005.09.048. 623.e15 623.e16. [DOI] [PubMed] [Google Scholar]
- 12.Tobias-machado M., Neto A.C.L., Simardi L.H., Borrelli M., Wroclawski E.R. Fibrous pseudotumor of tunica vaginalis and epididymis. Urology. 2000 Oct 1;56(4):670–672. doi: 10.1016/s0090-4295(00)00736-6. [DOI] [PubMed] [Google Scholar]