Abstract
Background
The senses serve as the crucial interface between the individual and the environment. They are subject to aging and disease processes.
Methods
This review is based on pertinent publications retrieved by a selective search in the Medline and Cochrane Library databases.
Results
Approximately 40% of persons aged 70 to 79 manifest dysfunction in at least one, and more than 25% in multiple senses. Sensory changes are accompanied by diverse comorbidities which depend on the particular sense(s) affected. The presence of sensory deficits is associated with an increased risk of developing dementia (OR: 1.49 [95% confidence interval: 1.12; 1.98] for dysfunction in a single sensory modality, 2.85 [1.88; 4.30] for dysfunction in three or more sensory modalities). The risk of developing depressive symptoms is elevated as well (OR 3.36 [2.28; 4.96]). The individual’s ability to cope with the demands of everyday life is largely determined by the ability to carry out multisensory integration, in which the perceptions of the different senses are bound together. This function itself is subject to age-related changes that can be either adaptive or maladaptive; it can, therefore, serve as an indicator for pathological aging processes.
Conclusion
Sensory dysfunction in old age should be detected as early as possible. This implies the need for close collaboration of all of the involved disciplines. It would be desirable to develop sensory screening tests as well as a procedure for testing multisensory integration in routine clinical practice.
Sensory perception, whether normal or impaired, has an enormous impact on our lives. The elderly often suffer a marked decline in one or more sensory systems. Most studies on this subject to date have focused on only one sensory system per study (e1). It has been determined, however, that 39.2% of persons aged 70 to 79 have an objectively demonstrable functional impairment in a single sensory modality, 20.1% in two, and approximately 6% in three or four modalities (e2).
Learning objectives
This article is intended to enable the reader to:
Sensation in old age.
Approximately 40% of persons aged 70 to 79 have an objectively demonstrable functional impairment in a single sensory modality, and more than 25% in multiple modalities.
know the basic changes to which each sensory modality is subject in old age,
gain an overview of current scientific evidence on the effects of sensory impairment in old age, and
understand how central integration of the different sensory modalities is affected by normal and pathological aging processes.
Hearing impairment
Hearing impairment.
From age 60 onward, the auditory threshold rises, particularly at high frequencies. Hearing impairment is often recognized late or else accepted as a supposedly inevitable part of aging.
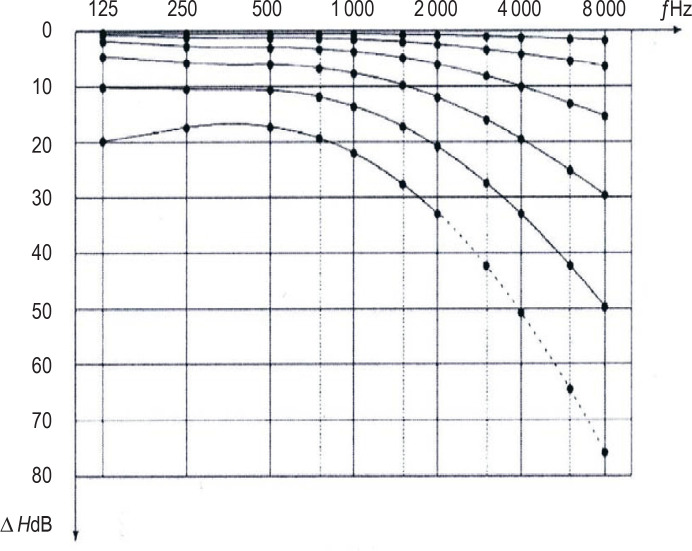
Even in otologically healthy persons, the auditory threshold rises by an average of 1 dB per year from age 60 onward (figure 1) (e3). Hearing impairment as defined by the WHO criteria is present in 20.3% of persons in their seventh decade, 42.2% of persons in their eighth, and 71.5% of persons aged 80 and above (e4). Elderly persons often do not notice their hearing impairment until long after its onset, or else accept it as a supposedly inevitable part of aging (e5, e6). As a result, even though good treatment options are available (e7, e8), hearing aids are worn by only 5.8% of hearing-impaired persons in Germany who are in their seventh decade, and by 32.6% of hearing-impaired 80-year-olds (e4). There are similar estimates from the USA and Sweden with respect to the provision of cochlear implants (e9, e10).
Figure 1.
Median values of expected changes of the auditory threshold in dB (Δ HdB) for otologically normal men as a function of frequency, f, and of age (the curves, from above downward, are for 30-, 40-, 50-, 60-, 70-, and 80-year-old men), according to DIN EN ISO 7029: 2014. Reproduced with permission from the German Institute for Standardization (DIN).
Hearing loss is associated with a variety of diseases. Above all, the relation between hearing loss and cognitive impairment has been the object of numerous studies. As early as 2011, a longitudinal study revealed that the risk of dementia appearing within 11.9 years is elevated by a factor of 1.89 (95% confidence interval: [1.00; 3.58]) in persons with mild hearing impairment, threefold [1.43; 6.30] in persons with moderate hearing impairment, and by a factor of 4.94 [1.09; 22.40] in persons with severe hearing impairment (e11). This was confirmed in a recent meta-analysis of 36 studies. A mild, but statistically significant correlation was found between age-associated hearing impairment and dysfunction in multiple cognitive domains (global cognition: r = -0.15 [-0.18; -0.11]). The odds ratio (OR) for incident dementia among persons with hearing loss is 2.42 [1.24; 4.72] in cross-sectional studies and 1.28 [1.02; 1.59] in longitudinal studies (1). Similarly, a longitudinal study based on data from over 150,000 insurees of the AOK health insurance carrier in Germany aged 65 and above revealed an elevated risk of dementia in persons with bilateral hearing impairment (hazard ratio [HR] = 1.43, p < 0.01) (e12).
It is still unclear how hearing impairment and cognitive changes influence each other (e13, e14). Various hypotheses are under discussion, but none of them have yet been definitively confirmed by scientific evidence:
an underlying pathological change affecting both the ascending auditory pathway and the multimodal cortex
a decline of cognitive resources because of primary, longstanding impoverishment of auditory stimulation
overloading of cognitive reserves by the increased effort required for useful hearing under difficult acoustic circumstances
damage to the medial portion of the temporal lobe, which is affected in early-stage Alzheimer’s disease and is also responsible for so-called auditory cognition, resulting in simultaneous impairment of cognitive function as well as hearing and/or auditory processing (2, 3).
Cognitive impairment due to hearing loss.
The relation between hearing loss and cognitive impairment has been the object of numerous studies. An elevated risk for the development of dementia has been demonstrated.
No data on the temporal course of the appearance of these sensory and cognitive changes are yet available that would support inferences about causation (e15). The mechanisms underlying these changes are the crucial determinants of whether auditory rehabilitation in middle age, in the form of a hearing aid or cochlear implant, might be able to prevent cognitive decline and dementia in old age, as postulated by Livingstone (4). While a few non-randomized studies have revealed improvement in various cognitive domains 6 and 12 months after cochlear implantation, the evidence remains insufficient (5, e16, e17). Prospective, clinically controlled longitudinal trials are hard to conduct for both ethical and practical reasons, not least because middle-aged persons are often reluctant to accept hearing aids (e18). Initial multicenter trials have begun; their results are pending (6).
Cochlear implants and cognitive decline in old age.
It is unclear whether auditory rehabilitation in middle age in the form of a cochlear implant might be able to prevent global cognitive decline in old age. A few studies have revealed improvement in various cognitive domains. The state of the evidence is not yet conclusive.
In persons already suffering from Alzheimer dementia (AD), wearing a hearing aid for 6 months seems not to cause any significant change in cognitive function, according to the findings of an initial randomized and placebo-controlled trial carried out on 38 patients with AD aged 68 and above (e19). An intervention of this type might, however, lower the probability of a transition from mild cognitive impairment (MCI) to dementia, as suggested by a recent retrospective data analysis based on subjective assessments of hearing status (HR 0.73 [0.61; 0.89]) (e20).
Moreover, hearing impairment is associated with a higher frequency of mental symptoms and illnesses (e21). For instance, women aged 60 to 69 with an untreated hearing impairment suffer more frequently from social isolation: the odds ratio (OR) rises by 3.49 [1.91; 6.39] per 25 dB worsening of hearing, averaged over the range 500–4000 Hz (e22). Hearing impairment is also associated with depression: the relative risk of depression is 1.41 [1.26; 1.58] five years after the onset of a hearing impairment, and 6.88 [4.62; 9.14] at 10 years (e23). According to a meta-analysis of 35 studies, a significant association of hearing impairment with depression has been revealed both by cross-sectional studies (OR: 1.54 [1.31; 1.80]) and by longitudinal studies (OR: 1.39 [1.16; 1.67]) (7). It remains unknown whether this is due to behavioral changes alone or to structural changes in the limbic system as well (8).
Elderly persons with at least 25 dB of hearing loss also have a 1.4-fold [1,3; 1,5] elevation of the risk of falling (e24). This association was recently confirmed in a meta-analysis of four studies, after adjustment for other risk factors (OR: 1.72 [1.07; 2.37]) (9).
Impairment of balance
The elderly often suffer from impaired balance because of multifactorial deficits in vestibular, proprioceptive, visual, and somatosensory function (e25). Many age-dependent degenerative changes have been demonstrated in the vestibular system at the cellular and neuronal level, but these often cannot be correlated with clinical manifestations, because the physiology of the central vestibular system is complex (10). The clinical relevance of physiological aging processes in this sensory system is, therefore, difficult to determine.
Mental illness.
Persons with hearing impairment suffer more frequently from social isolation or depression.
When interpreting data on the prevalence of age-associated impairment of balance, one must bear in mind that the common lay term “dizziness” can refer both to apparent relative motion of the subject and the environment (i.e., true vertigo) and, more broadly, to an unsystematic feeling of unsteadiness. Data on the prevalence of balance disturbances are mainly derived from questionnaires and may not differentiate between these two senses of the word. A study by Gassmann revealed an increasing prevalence of impaired balance with increasing age (27% in persons aged 65 to 70, 54% in persons aged 90 and above) (11). Women have a higher prevalence of impaired balance than men (at age 70, 36% vs. 29%; at age 90, 51% vs. 45%).
The frequency distribution of diagnosed causes of impaired balance is highly dependent on the particular medical specialty performing the diagnostic assessment (e26). An interdisciplinary approach and thorough history-taking are thus very important. The patient should be asked about the nature and duration of the difficulty with balance, precipitating factors, accompanying symptoms and concomitant illnesses, and medication use, as well as about any falls that may have occurred and any further risk factors for falling that may be present.
In the elderly, dizziness as a symptom is a major risk factor for falling (e27). A recent meta-analysis determined that, in the presence of dizziness, the relative risk of falling is 1.32 [1.10; 1.59] (13). Moreover, dizziness is also associated with elevated mortality after risk adjustment (adjusted OR: 1.7 [1.36; 2.18]) (e28).
With regard to peripheral vestibular disturbances, bilateral vestibulopathy should be considered as a possible cause in any patient with chronically impaired balance. The typical clinical manifestation is movement-dependent unsteadiness that worsens in darkness and when the patient walks on an uneven surface. A cause can be identified in only 49% of cases (e.g., vestibulotoxic drugs, bilateral Ménière’s disease) (e29). The term “presbyvestibulopathy” refers to bilateral mild reduction of vestibular function, as determined by objective measurement. Further diagnostic criteria for it include age 60 or above, unsteadiness, gait impairment, chronic dizziness, and recurrent falls that are not explained by another disorder (14). The recommended treatment is daily balance training, particularly with rotation of the head in all three axes, in order to train the vestibulo-ocular reflex (level I evidence) (e30), supplemented by fall prevention under physiotherapeutic guidance (15). A combination of balance, strength, and gait training can lower the risk of falling by 23 % (level I evidence) (e31).
Visual impairment
Impairment of balance.
The elderly often suffer from impaired balance because of multifactorial deficits in vestibular, proprioceptive, visual, and somatosensory function. Impaired balance is a major risk factor for falling in old age.
Visual disturbances become more common in old age. The prevalence of visual impairment and blindness in Germany is 0.4% overall (431.5 per 100 000 persons), 0.7% (735.4/100 000) in persons aged 65 to 74, and 2.4% (2391.4/100 000) in persons aged 75 and above (16). The most common causes of blindness in Germany are associated with aging, namely, age-associated macular degeneration (AMD) and glaucoma (e32).
In contrast to diseases such as AMD, the normal, continuous aging processes of the various tissue systems of the eye have only mild symptoms at first. Contrast perception declines slowly, as does the ability to adapt to different lighting conditions. Physiological changes of the lens play a major role at first; the declining accommodation ability of the lens from age 45 onward (presbyopia) is due to structural changes of the lens itself, its zonular fibers (suspensory apparatus), the ciliary muscle tendons, and the ciliary muscle (e33). Presbyopia can be corrected with spectacles, multifocal contact lenses, or microsurgically implanted intraocular lenses of various types (17). There are nonetheless more than 800 million persons around the world with inadequate access (or none at all) to presbyopia correction. This constitutes a major socioeconomic problem, particularly in rural areas (18).
Progressive destabilization of lens proteins in old age leads to turbidity of the lens and ultimately to a pathological cataract (19). Depending on the morphology of the turbidity/opacification, the symptoms may consist of lessened contrast sensitivity, increased sensitivity to glare, and/or impaired visual acuity (20). Cataract is the main preventable cause of blindness around the world (e34).
Presbyopia.
Presbyopia is the normal decline with aging in the ability of the pupil to accommodate. Eyeglasses are the most important optical aid for the correction of presbyopia.
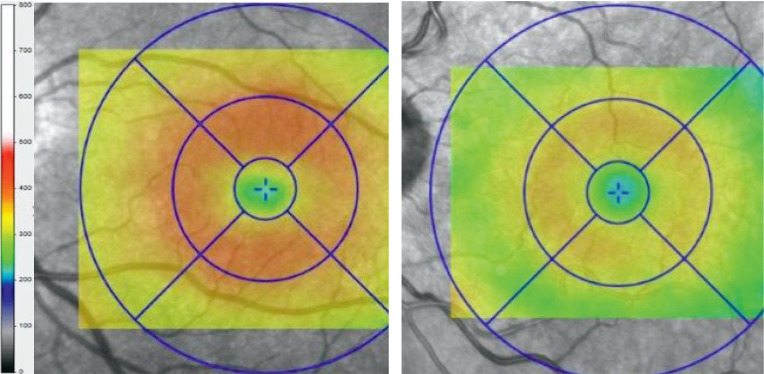
There are various reasons for the lessened central visual acuity and impaired vision in dim light that accompany normal aging. The pupils become narrower, allowing less light to reach the retina (19). The retinal ganglion-cell layer in the macular region becomes approximately 3% thinner with each additional decade of life (figure 2) (20). The number of rod cells, which are responsible for vision in dim light, also diminishes between the ages of 60 and 70 (21). Adaptation to darkness becomes harder as the amount of the photopigment rhodopsin in the photoreceptors lessens and phototransduction processes for rod-cell regeneration become slower. Thus, the normal switching from cone to rod vision in dim light is slowed. Lastly, transport processes for vitamin A, a necessary component of the visual cycle, are impaired by changes in the retinal pigment epithelium (RPE), by the accumulation of extracellular materials between Bruch’s membrane and the RPE (drusen), and by thickening of Bruch’s membrane itself. This can be a transitional stage to the development of diseases of old age, such as age-associated macular degeneration (AMD) (e35).
Figure 2.
Figure 2: Normal age-related changes in the thickness (µm) of all retinal layers at the macula are illustrated here with optical coherence tomographic findings from a 12-year-old boy (left) compared to those of a 68-year-old man (right).
In general, elderly persons with impaired vision suffer more often from cognitive impairment (relative risk [RR]: 1.47 [1.36; 1.60]) and dementia (RR 1.35 [1.28; 1.41]) (22). Visual acuity often improves markedly after cataract surgery in elderly persons with cognitive impairment, who often have very advanced lenticular opacification. The visual improvement may also have a beneficial effect on cognition.
Impairment of smell
Anosmia, i.e., the total lack of olfactory perception, affects 3.6% of the general population (23, e36). It has wide-ranging consequences for the perception of dangers in everyday life (smoke, poisonous substances). 45% of persons with anosmia, but only 19% of persons with a normal sense of smell, report having had accidents of types that may have to do with olfactory perception (e37). Moreover, the inability to smell the aroma of food may impair the enjoyment of eating and the rewarding character of the eating experience (e38). A depressive mood disturbance is found in approximately one-third of patients with impaired olfaction (24, e39), and most suffer from a lowered quality of life.
Loss of visual acuity.
Reasons for the lessened central visual acuity and impaired vision in dim light that accompany normal aging include narrowing of the pupils, loss of retinal ganglion cells, and changes in the number of rods and in their metabolism.
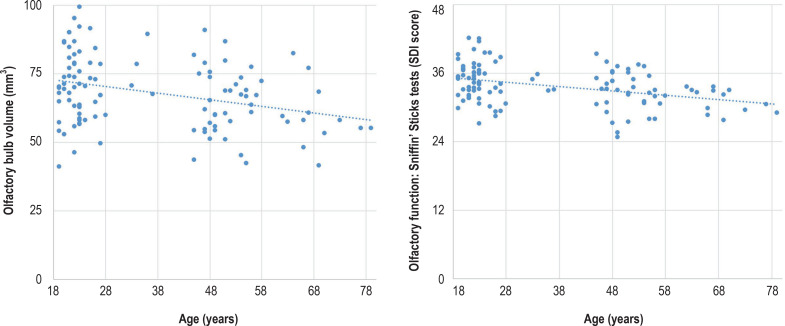
The sense of smell declines with age and is practically absent in at least one-third of persons aged 80 and above (25, e40). The loss of smell apparently reflects the summed effect of changes at various levels of olfactory perception (26). The olfactory epithelium can regenerate itself, but this ability declines over a lifetime (e41, e42). The olfactory bulb also possesses plasticity (e43, e44), which can be seen in imaging studies as a change of volume (figure 3) (e45). The mean volume of the olfactory bulb is 71.6 mm3 in persons under age 40 and 59.6 mm3 in persons over age 60 (27). The activation of the brain by odors declines as well, mainly in the secondary olfactory cortex (e46).
Figure 3.
Age-dependence of olfaction. Right: olfactory function as measured by Sniffin’ Sticks tests (SDI score). Left: olfactory bulb volume as a structural correlate in healthy subjects. (Modified from Buschhüter 2008)
Various methods are available for the assessment of olfactory function. Self-assessment of the general ability to smell is erroneous in approximately one-third of cases (e47). For clinical olfactory testing, Sniffin’ Sticks can be used as a screening test (e48) or for more detailed testing (e49). If the ability to tell odors apart and the perceptory threshold for odors are affected to varying extents, the cause probably lies in a disturbance at either the central nervous or the peripheral nasal level (e50, e51); a variety of treatments are available (23, e52). In persons with age-associated impairment of smell, the plasticity of the olfactory system can be stimulated by regular smell training. In one study carried out on 91 healthy subjects, improvement was seen in 20% of the smell-training group and in 10% of the control group (e53).
Impairment of smell.
The sense of smell declines with age through the summed effect of changes at various levels of olfactory perception.
At any age, olfactory disturbances of unclear cause may be an early symptom of a neurodegenerative diseases such as idiopathic Parkinson syndrome (IPS). Although unexplained olfactory loss has a positive predictive value of only 0.09, olfactory testing may be helpful in the differential diagnosis of IPS (28). Moreover, up to 94% of patients with manifest IPS have impaired olfaction (e54), which suggests that reconsideration of the diagnosis of IPS may be advisable in patients with a normal sense of smell.
Impairment of taste
Impaired gustatory perception (sweet, sour, salty, bitter, umami) affects approximately 5% of the population (e55). It may be idiopathic, or else due to a reduced number of papillae in the mouth, altered production and composition of the saliva, or impaired central nervous processing (e56, e57). Moreover, a declining sense of smell leads indirectly to lessened reinforcement of gustatory function (e58). Hardly any treatment is available for impaired taste (e59).
Somatosensory impairment
Assessment of the sense of smell.
Methods such as the Sniffin’ Stick test can be used for screening or for more detailed testing of olfactory function.
The somatosensory system, with its component modalities (exteroception, proprioception, interoception), is responsible from intrauterine development onward for both active (haptic) and passive (tactile) somatic sensation. Somatosensory performance varies greatly between individuals and changes over the course of any single individual’s lifetime as well (29– 31) (e60).
From age 20 onward, the quality of perception of tactile stimuli at the fingertips declines by approximately 1% per year. This is due not only to an age-dependent loss of Meissner and Merkel receptors, but also to a loss of neurons (e61). The perception of passively applied, high-frequency (>100 Hz) vibratory stimuli worsens with age, while that of lower-frequency vibratory stimuli (< 40 Hz) remains unimpaired even in old age. The decline of perception of high-frequency vibratory stimuli is thought to be due to structural changes in the Pacinian corpuscles (32, e62, e63).
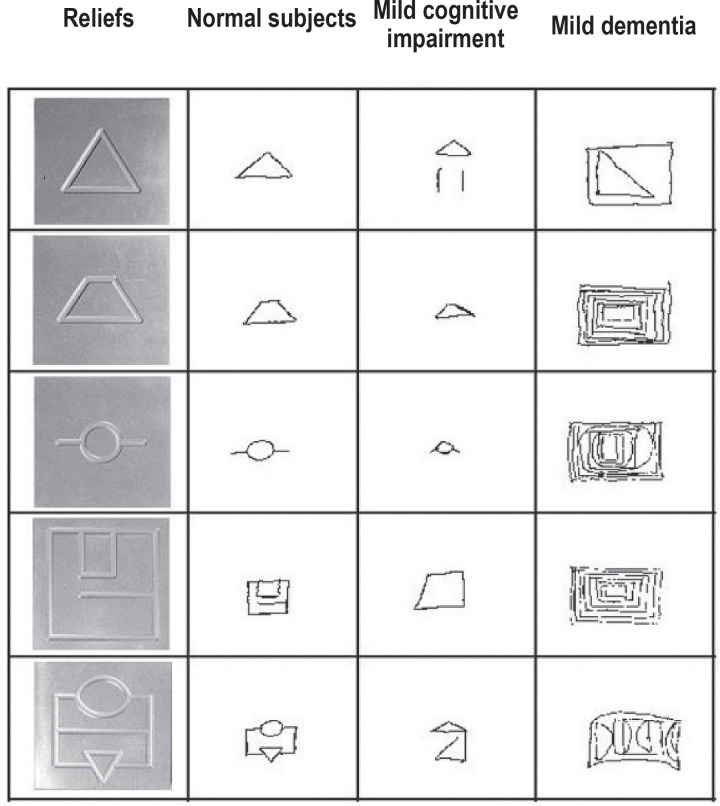
The active, haptic capacity to recognize objects regularly declines in old age, but later than passive, tactile somatosensory perception. The decline of active, haptic ability is more closely correlated with cognitive changes than with the declining number of somatosensory receptors in old age (figure 4) (e64, e65). The age-related decline of proprioceptive ability is often associated with impaired balance; the degree of resulting functional impairment depends on the individual’s prior motor experience and level of physical activity (e66, e67). Nonetheless, as all somatosensory dimensions are trainable even in old age, proprioceptive training can help lower the frequency of falls in elderly patients (e68, e69).
Figure 4.
Drawings made after haptic object recognition of real bas-reliefs by normal subjects and by patients with mild cognitive impairment and mild dementia (mean age, 78 years). The bas-reliefs (13 × 3 cm) contained abstract patterns with a trace width and trace depth of 5mm. The task was to feel each bas-relief with the eyes closed and then draw them with the eyes open (from: Grunwald 2002).
There are also changes in some aspects of intero-ception from age 50 onward. Painful visceral stimuli are processed less adequately; nonetheless, the elderly complain of pain more commonly than younger persons. This is thought to be the result of summation effects due to pain located at multiple bodily sites simultaneously in old age, as well as to a decline of inhibitory mechanisms and a stronger emotional-motivational component (e70).
Despite the decline of somatosensory function, the elderly have an unchanged need for bodily social interaction. Studies have shown a positive effect of social physical contact on perceived loneliness (e71, e72), depression, and anxiety, as well as improved food intake and diminution of aggressive and agitated behaviors in persons with dementia (33, e73, e74).
Interactions between the sensory systems
Impairment of taste.
Potential causes of impaired gustatory perception include:
a reduced number of papillae in the mouth
altered production and composition of the saliva
impaired central nervous processing
The consequences of sensory impairment are more severe if multiple sensory systems are affected. The degree of sensory impairment, as measured with the Global Sensory Impairment Index, is significantly correlated with activities of daily living (OR 1.26 [1.10; 1.46]), physical mobility (OR 1.32 [1.17; 1.50]), and 5-year mortality (OR 1.45 [1.19; 1.76]) (e1). Moreover, the OR for the appearance of dementia is 1.49 [1.12; 1.98] with functional impairment in a single sensory modality, 1.91 [1.39; 2.63] with impairment in two, and 2.85 [1.88; 4.30] with impairment in three or more modalities (e2). The simultaneous dysfunction of multiple sensory systems is associated with poorer physical performance ability (e75), and the risk of developing depression is elevated by a factor of 3.36 [2.28; 4.96] if three or more sensory systems are impaired (34).
Somatosensory impairment.
The decline of active, haptic ability is correlated with cognitive changes and with impaired balance. Proprioceptive training can lessen the frequency of falls.
These effects can be well explained as being due to altered multisensory integration (MSI). As part of everyday life, the brain has the task of generating a single, holistic perception out of the voluminous data that are conveyed to it uninterruptedly by the various sensory systems, in all of their differing and more or less correlated temporal, spatial, textual, and semantic aspects. These data must be matched to each other in such a way as to give the individual a maximally realistic picture of the environment, so that his or her ensuing behavior will be situationally appropriate, with the lowest possible chance of bringing harm. It is presumed that, in order to carry out this enormously complex integrative task, the brain performs the equivalent of computing Bayesian probabilities (35, e76). Bayes’s Theorem enables the continuous computation of a posteriori probabilities of hypotheses, as in the following example from the visual domain: the hypothesis “The two headlights that I see coming my way in the dark as I drive down this wet road belong to a car that is coming toward me” has an a priori probability (derived from pre-existing knowledge about approaching headlights in comparable situations) that can be corrected for current circumstances (e.g., a dirty windshield).
MSI can improve the perceptions of our senses adaptively, or else it can have maladaptive effects, causing perceptual illusions. The precise mechanisms are imperfectly known to date (36, 37, e76). Imaging studies and neurophysiological studies provide evidence that the capacity for MSI not only remains intact over an individual’s lifetime but actually improves, mainly in the processing of congruent stimuli (37, e77, e78). Thus, MSI may be able to compensate for age-associated impairment of particular peripheral sensory functions (e79). On the other hand, some aspects of MSI seem to worsen with age, with adverse consequences for everyday life. For instance, impaired visuo-somatosensory integration has been found to be associated with poorer balance (p < 0.05) and an elevated risk of falling (HR : 0.24, p = 0.01) (38). The extent of impairment of MSI may also be an early indicator of pathological aging processes (e80, 36).
The interaction of multiple sensory systems.
Changes in multisensory integration can lead to impairment in many areas of life.
It is only in the last few years that multisensory integration has attracted increased scientific attention (e81). In view of the functional importance of MSI, the changes and adaptations in this capability over an individual’s lifetime, and, especially, its susceptibility to impairment by age-associated neurological diseases, it appears important that testing procedures for MSI should be developed for use in the routine clinical evaluation of elderly patients in particular (36, e80). The essential prerequisite is an intensive collaboration of geriatrics with the other relevant specialties in both the clinical and the scientific domain.
Overview
Impairments in single sensory systems have far-reaching consequences for the individual. These are even more marked when multiple sensory systems are affected. The multisensory integration of sensory perceptions plays a crucial role in enabling elderly persons to continue going about their everyday activities. In the future, early detection of sensory impairments in the elderly would be a desirable component of preventive medical check-ups, as it might help lessen severe long-term consequences. Moreover, multimodal therapeutic approaches might help slow aging processes by stimulating the plasticity of the brain (e81, e82).
Overview
The multisensory integration of sensory perceptions plays a crucial role in enabling elderly persons to continue going about their everyday activities.
Further information on CME.
Participation in the CME certification program is possible only via the Internet: cme.aerzteblatt.de. The submission deadline is 25.07.2022. Submissions by letter, email, or fax cannot be considered.
The completion time for all newly started CME units is 12 months. The results can be accessed 4 weeks following the start of the CME unit. Please note the respective submission deadline at: cme.aerzteblatt.de.
This article has been certified by the North Rhine Academy for Continuing Medical Education. CME points can be managed using the “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be stated during registration on www.aerzteblatt.de (“Mein DÄ”) or entered in “Meine Daten,” and consent must be given for results to be communicated. The 15-digit EFN can be found on the CME card (8027XXXXXXXXXXX).
Participation is possible at cme.aerzteblatt.de. The submission deadline is 25 July 2022.
Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
What is found in approximately one-third of all patients with an impaired sense of smell?
a depressive mood disturbance
a fatigue syndrome
a hyperactivity syndrome
Asperger syndrome
a bipolar disorder
Question 2
What is the explanation for reduced perception of passively applied vibratory stimuli?
structural changes in the Pacinian corpuscles
degeneration of sensory areas in the cerebral cortex
hypertrophy of the granular layer
increased subcutaneous fat
structural changes in the Ruffini bodies
Question 3
According to an epidemiological study, what is the prevalence of hearing impairment (as defined by the WHO criteria) among persons aged 70 to 79 in Germany?
15.6%
20.3%
29.9%
42.2%
71.5%
Question 4
What is meant by the term “multisensory integration”?
The ability to generate an overall impression from sensory perceptions in different modalities.
The selective processing of, at most, three sensory stimuli.
The integration of visual and auditory information, with simultaneous suppression of tactile stimuli.
The simultaneous processing of vestibular, interoceptive, and exteroceptive information.
Primary perception of the stimulus that is strongest at present.
Question 5
According to a longitudinal study from 2011, by what factor is the risk of developing dementia in 11.9 years elevated in the presence of high-grade hearing impairment?
1.89
3.56
4.94
5.73
10.32
Question 6
What type of training is recommended for patients with gait insecurity, gait disturbance, chronic dizziness, and repeated falls without any other identifiable, treatable cause?
mild aerobic interval training
simple balance exercises with the eyes closed
progressive muscle relaxation according to Jacobson
balance training with head rotation in three axes
hypnotherapy and isometric training
Question 7
What is the main preventable cause of blindness around the world?
glaucoma
diabetic retinopathy
age-associated macular degeneration
cataract
vitamin A deficiency
Question 8
What is the physiological cause of slowed light/dark adaptation in old age?
atrophy of the zonular fibers
thickening of the cornea
opacification of the lens
lowered rhodopsin concentration in the rods
thinning of Bruch’s membrane
Question 9
What is often associated with an age-associated decline of proprioceptive ability?
impaired balance
reduced visual acuity
the onset of malignant disease
reduced need for physical interaction with others
lessened perception of tactile stimuli in central areas of the body
Question 10
What percentage of persons in the general population suffer from anosmia?
0.6%
1.6%
2.6%
3.6%
4.6%
► Participation is only possible online: cme.aerzteblatt.de
Acknowledgments
Translated from the original German by Ethan Taub, M.D:
Footnotes
Conflict of interest statement
Prof. Völter has received reimbursement of scientific meeting participation fees and accommodation expenses, as well as honoraria for preparing continuing medical education events and funding for a research project that she initiated, from MED-EL.
PD Thomas has received reimbursement of scientific meeting participation fees and travel expenses from MED-EL. From the same company, he has received honoraria for preparing continuing medical education events, as well as payment for carrying out clinical trials.
Rainer Guthoff has received lecture honoraria from Hoffmann La Roche AG and reimbursement of scientific meeting participation fees and travel expenses from Bayer AG and DORC GmbH. He has received payment for carrying out clinical trials from Bayer AG, Novartis Pharma, Hoffmann La Roche AG, and Samsung.
Prof. Hummel has received funding for a research project that he initiated from Smell and Taste, Geneva, and from Sony and Takasago.
The remaining authors state that they have no conflict of interest.
References
- 1.Loughrey DG, Kelly ME, Kelley GA, Brennan S, Lawlor BA. Association of age-related hearing loss with cognitive function, cognitive impairment, and dementia: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2018;144:115–126. doi: 10.1001/jamaoto.2017.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griffiths TD, Lad M, Kumar S, et al. How can hearing loss cause dementia? Neuron. 2020;108:401–412. doi: 10.1016/j.neuron.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson JCS, Marshall CR, Weil RS, Bamiou D-E, Hardy CJD, Warren JD. Hearing and dementia: from ears to brain. Brain. 2021;144:391–401. doi: 10.1093/brain/awaa429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–446. doi: 10.1016/S0140-6736(20)30367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dawes P. Hearing interventions to prevent dementia. HNO. 2019;67:165–167. doi: 10.1007/s00106-019-0617-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deal JA, Goman AM, Albert MS, et al. Hearing treatment for reducing cognitive decline: design and methods of the aging and cognitive health evaluation in elders randomized controlled trial. Alzheimers ¬Dement (N Y) 2018;4:499–507. doi: 10.1016/j.trci.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lawrence BJ, Jayakody DMP, Bennett RJ, Eikelboom RH, Gasson N, Friedland PL. Hearing loss and depression in older adults: a systematic review and meta-analysis. Gerontologist. 2020;60:e137–e154. doi: 10.1093/geront/gnz009. [DOI] [PubMed] [Google Scholar]
- 8.Rutherford BR, Brewster K, Golub JS, Kim AH, Roose SP. Sensation and psychiatry: linking age-related hearing loss to late-life depression and cognitive decline. Am J Psychiatry. 2018;175:215–224. doi: 10.1176/appi.ajp.2017.17040423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jiam NTL, Li C, Agrawal Y. Hearing loss and falls: a systematic review and metaanalysis. Laryngoscope. 2016;126:2587–2596. doi: 10.1002/lary.25927. [DOI] [PubMed] [Google Scholar]
- 10.Zalewski, Christopher K. Aging of the human vestibular system. Semin Hear. 2015;26 doi: 10.1055/s-0035-1555120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gassmann KG, Rupprecht R. Dizziness in an older community dwelling population: a multifactorial syndrome. J Nutr Health Aging. 2009;13:278–282. doi: 10.1007/s12603-009-0073-2. [DOI] [PubMed] [Google Scholar]
- 12.Jönsson R, Sixt E, Landahl S, Rosenhall U. Prevalence of dizziness and vertigo in an urban elderly population. J Vestib Res. 2004;14:47–52. [PubMed] [Google Scholar]
- 13.Jehu DA, Davis JC, Falck RS, et al. Risk factors for recurrent falls in older adults: a systematic review with meta-analysis. Maturitas. 20211;44:23–28. doi: 10.1016/j.maturitas.2020.10.021. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal Y, van de Berg R, Wuyts F, et al. Presbyvestibulopathy: diagnostic criteria consensus document of the Classification Committee of the Bárány Society. J ¬Vestib Res. 2019;29:161–170. doi: 10.3233/VES-190672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strupp M, Dlugaiczyk J, Ertl-Wagner BB, Rujescu D, Westhofen M, Dieterich M. Vestibular disorders: diagnosis, new classification and treatment. Dtsch Arztebl Int. 2020;117:300–310. doi: 10.3238/arztebl.2020.0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolfram C, Pfeiffer N. Blindness and low vision in Germany 1993-2009. Ophthalmic Epidemiol. 2012;19:3–7. doi: 10.3109/09286586.2011.628136. [DOI] [PubMed] [Google Scholar]
- 17.Charman WN. Developments in the correction of presbyopia II: surgical ¬approaches. Ophthalmic Physiol Opt. 2014;34:397–426. doi: 10.1111/opo.12129. [DOI] [PubMed] [Google Scholar]
- 18.Global Blindness Division. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–e160. doi: 10.1016/S2214-109X(20)30489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Owsley C. Vision and aging. Annu Rev Vis Sci. 2016;2:255–271. doi: 10.1146/annurev-vision-111815-114550. [DOI] [PubMed] [Google Scholar]
- 20.Chauhan BC, Vianna JR, Sharpe GP, et al. Differential effects of aging in the ¬macular retinal layers, neuroretinal rim, and peripapillary retinal nerve fiber layer. Ophthalmol. 2020;127:177–185. doi: 10.1016/j.ophtha.2019.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Girard B, Chouard B, Levy P, Luquel L, Seux ML, Drunat O. Modifications des troubles du comportement après l’opération de la cataracte chez les patients Alzheimer [Neuropsychological benefit of cataract surgery among sight impaired Alzheimer‘s patient] J Fr Ophtalmol. 2016;39:675–686. doi: 10.1016/j.jfo.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 22.Shang X, Zhu Z, Wang W, Ha J, He M. The association between vision impairment and incidence of dementia and cognitive impairment: a systematic review and meta-analysis. Ophthalmol. 2021;161 doi: 10.1016/j.ophtha.2020.12.029. [DOI] [PubMed] [Google Scholar]
- 23.Hummel T, Whitcroft KL, Andrews P, et al. Position paper on olfactory dysfunction. Rhinol Suppl. 2017;54:1–30. doi: 10.4193/Rhino16.248. [DOI] [PubMed] [Google Scholar]
- 24.Croy I, Symmank A, Schellong J, et al. Olfaction as a marker for depression in ¬humans. J Affec Disord. 2014;160:80–86. doi: 10.1016/j.jad.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 25.Doty RL. Age-related deficits in taste and smell. Otolaryngol Clin North Am. 2018;51:815–825. doi: 10.1016/j.otc.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 26.Manzini I, Frasnelli J, Croy I. How we smell and what it means to us: basic principles of the sense of smell. HNO. 2014;62:846–852. doi: 10.1007/s00106-014-2925-2. [DOI] [PubMed] [Google Scholar]
- 27.Buschhüter D, Smitka M, Puschmann S, et al. Correlation between olfactory bulb volume and olfactory function. Neuroimage. 2008;42:498–502. doi: 10.1016/j.neuroimage.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 28.Haehner A, Masala C, Walter S, Reichmann H, Hummel T. Incidence of Parkinson’s disease in a large patient cohort with idiopathic smell and taste loss. J Neurol. 2019;266:339–345. doi: 10.1007/s00415-018-9135-x. [DOI] [PubMed] [Google Scholar]
- 29.Grunwald M, Busse F, Hensel A. Theta-power differences in patients with mild ¬cognitive impairment under rest condition and during haptic tasks. Alzheimer Dis Assoc Disord. 2002;16:40–48. doi: 10.1097/00002093-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 30.McIntyre S, Nagi SS, McGlone F, Olausson H. The effects of ageing on tactile function in humans. Neuroscience. 2021;464:53–58. doi: 10.1016/j.neuroscience.2021.02.015. [DOI] [PubMed] [Google Scholar]
- 31.García-Piqueras J, García-Mesa Y, Cárcaba L, et al. Ageing of the somatosensory system at the periphery: age-related changes in cutaneous mechanoreceptors. J Anat. 2019;234:839–852. doi: 10.1111/joa.12983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lindholm E, Löndahl M, Fagher K, Apelqvist J, Dahlin LB. Strong association ¬between vibration perception thresholds at low frequencies (4 and 8 Hz), ¬neuropathic symptoms and diabetic foot ulcers. PLoS One. 2019;14 doi: 10.1371/journal.pone.0212921. e0212921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim EJ, Buschmann MT. The effect of expressive physical touch on patients with dementia. Int J Nurs Stud. 1999;36:235–243. doi: 10.1016/s0020-7489(99)00019-x. [DOI] [PubMed] [Google Scholar]
- 34.Liljas AEM, Jones A, Cadar D, Steptoe A, Lassale C. Association of multisensory impairment with quality of life and depression in english older adults. JAMA ¬Otolaryngol Head Neck Surg. 2020;146:278–285. doi: 10.1001/jamaoto.2019.4470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones SA, Noppeney U. Ageing and multisensory integration: A review of the ¬evidence, and a computational perspective. Cortex. 2021;138:1–23. doi: 10.1016/j.cortex.2021.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Dieuleveult AL de, Siemonsma PC, van Erp JBF, Brouwer A-M. Effects of aging in multisensory integration: a systematic review. Front Aging Neurosci. 2017;9 doi: 10.3389/fnagi.2017.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Misselhorn J, Göschl F, Higgen FL, Hummel FC, Gerloff C, Engel AK. Sensory capability and information integration independently explain the cognitive status of healthy older adults. Sci Rep. 2020;10:1–18. doi: 10.1038/s41598-020-80069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahoney JR, Cotton K, Verghese J. Multisensory integration predicts balance and falls in older adults. J Gerontol A Biol Sci Med Sci. 2019;74:1429–1435. doi: 10.1093/gerona/gly245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Pinto JM, Wroblewski KE, Huisingh-Scheetz M, et al. Global sensory impairment predicts morbidity and mortality in older U.S. adults. J Am Geriatr Soc. 2017;65:2587–2595. doi: 10.1111/jgs.15031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Brenowitz WD, Kaup AR, Lin FR, Yaffe K. Multiple sensory impairment is associated with increased risk of dementia among black and white older adults. J Gerontol A Biol Sci Med Sci. 2019;74:890–896. doi: 10.1093/gerona/gly264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E3.Fischer N, Weber B, Riechelmann H. Presbyakusis- Altersschwerhörigkeit. Laryngo-Rhino-Otol. 2016;95:497–510. doi: 10.1055/s-0042-106918. [DOI] [PubMed] [Google Scholar]
- E4.Gablenz P von, Holube I. Prevalence of hearing impairment in northwestern Germany. Results of an epidemiological study on hearing status (HORSTAT) HNO. 2015;63:195–214. doi: 10.1007/s00106-014-2949-7. [DOI] [PubMed] [Google Scholar]
- E5.Ramage-Morin PL, Banks R, Pineault D, Atrach M. Unperceived hearing loss among Canadians aged 40 to 79. Health Rep. 2019;30:11–20. doi: 10.25318/82-003-x201900800002-eng. [DOI] [PubMed] [Google Scholar]
- E6.D‘Haese PSC, Bodt M de, van Rompaey V, van de Heyning P. Awareness of hearing loss in older adults: results of a survey conducted in 500 subjects across 5 European countries as a basis for an online awareness campaign. Inquiry. 2018;55 doi: 10.1177/0046958018759421. 46958018759421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E7.Dazert S, Thomas JP, Loth A, Zahnert T, Stöver T. Cochlear implantation. Dtsch Arztebl Int. 2020;117:690–700. doi: 10.3238/arztebl.2020.0690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E8.Löhler J, Cebulla M, Shehata-Dieler W, Volkenstein S, Völter C, Walther LE. Hearing impairment in old age: detection, treatment, and associated risks. Dtsch Arztebl Int. 2019;116 doi: 10.3238/arztebl.2019.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E9.Sorkin DL, Buchman CA. Cochlear implant access in six developed countries. Otol Neurotol. 2016;37:e161–e164. doi: 10.1097/MAO.0000000000000946. [DOI] [PubMed] [Google Scholar]
- E10.Turunen-Taheri SK, Edén M, Hellström S, Carlsson P-I. Rehabilitation of adult patients with severe-to-profound hearing impairment-why not cochlear implants? Acta Otolaryngol. 2019;139:604–611. doi: 10.1080/00016489.2019.1607976. [DOI] [PubMed] [Google Scholar]
- E11.Lin FR, Metter EJ, O‘Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. Arch Neurol. 2011;68:214–220. doi: 10.1001/archneurol.2010.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E12.Fritze T, Teipel S, Óvári A, Kilimann I, Witt G, Doblhammer G. Hearing impairment affects dementia incidence. An analysis based on longitudinal health claims data in Germany. PLoS One. 2016;11 doi: 10.1371/journal.pone.0156876. e0156876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E13.Wayne RV, Johnsrude IS. A review of causal mechanisms underlying the link between age-related hearing loss and cognitive decline. Ageing Res Rev. 2015;23:154–166. doi: 10.1016/j.arr.2015.06.002. [DOI] [PubMed] [Google Scholar]
- E14.Uchida Y, Sugiura S, Nishita Y, Saji N, Sone M, Ueda H. Age-related hearing loss and cognitive decline - The potential mechanisms ¬linking the two. Auris Nasus Larynx. 2019;46:1–9. doi: 10.1016/j.anl.2018.08.010. [DOI] [PubMed] [Google Scholar]
- E15.Sardone R, Battista P, Panza F, et al. The age-related central ¬auditory processing disorder: Silent impairment of the cognitive ear. Front Neurosci. 2019;13 doi: 10.3389/fnins.2019.00619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E16.Völter C, Götze L, Haubitz I, Müther J, Dazert S, Thomas JP. Impact of cochlear implantation on neurocognitive subdomains in adult cochlear implant recipients. Audiol Neurootol. 2021:1–10. doi: 10.1159/000510855. [DOI] [PubMed] [Google Scholar]
- E17.Mosnier I, Bebear J-P, Marx M, et al. Improvement of cognitive function after cochlear implantation in elderly patients. JAMA Otolaryngol Head Neck Surg. 2015;141:442–450. doi: 10.1001/jamaoto.2015.129. [DOI] [PubMed] [Google Scholar]
- E18.McCormack A, Fortnum H. Why do people fitted with hearing aids not wear them? Int J Audiol. 2013;52:360–368. doi: 10.3109/14992027.2013.769066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E19.Nguyen M-F, Bonnefoy M, Adrait A, et al. Efficacy of hearing aids on the cognitive status of patients with Alzheimer’s disease and hearing loss: a multicenter controlled randomized trial. J Alzheimers Dis. 2017;58:123–137. doi: 10.3233/JAD-160793. [DOI] [PubMed] [Google Scholar]
- E20.Bucholc M, McClean PL, Bauermeister S, et al. Association of the use of hearing aids with the conversion from mild cognitive impairment to dementia and progression of dementia: A longitudinal retrospective study. Alzheimers Dement (N Y) 2021;7 doi: 10.1002/trc2.12122. e12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E21.Brüggemann P, Szczepek AJ, Klee K, Gräbel S, Mazurek B, Olze H. In patients undergoing cochlear implantation, psychological burden affects tinnitus and the overall outcome of auditory rehabilitation. Front Hum Neurosci. 2017;11 doi: 10.3389/fnhum.2017.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E22.Mick P, Kawachi I, Lin FR. The association between hearing loss and social isolation in older adults. Otolaryngol Head Neck Surg. 2014;150:378–384. doi: 10.1177/0194599813518021. [DOI] [PubMed] [Google Scholar]
- E23.Deal JA, Reed NS, Kravetz AD, et al. Incident hearing loss and comorbidity: a longitudinal administrative claims study. JAMA Otolaryngol Head Neck Surg. 2019;145:36–43. doi: 10.1001/jamaoto.2018.2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E24.Lin FR, Ferrucci L. Hearing loss and falls among older adults in the United States. Arch Intern Med. 2012;172:369–371. doi: 10.1001/archinternmed.2011.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E25.Kristinsdottir EK, Jarnlo GB, Magnusson M. Aberrations in postural control, vibration sensation and some vestibular findings in healthy 64-92-year-old subjects. Scand J Rehabi Med. 1997;29:257–265. [PubMed] [Google Scholar]
- E26.Parker IG, Hartel G, Paratz J, Choy NL, Rahmann A. A systematic review of the reported proportions of diagnoses for dizziness and vertigo. Otol Neurotol. 2019;40:6–15. doi: 10.1097/MAO.0000000000002044. [DOI] [PubMed] [Google Scholar]
- E27.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75:51–61. doi: 10.1016/j.maturitas.2013.02.009. [DOI] [PubMed] [Google Scholar]
- E28.Corrales CE, Bhattacharyya N. Dizziness and death: an imbalance in mortality. Laryngoscope. 2016;126:2134–2136. doi: 10.1002/lary.25902. [DOI] [PubMed] [Google Scholar]
- E29.Zingler VC, Cnyrim C, Jahn K, et al. Causative factors and epidemiology of bilateral vestibulopathy in 255 patients. Ann Neurol. 2007;61:524–532. doi: 10.1002/ana.21105. [DOI] [PubMed] [Google Scholar]
- E30.Hall CD, Herdman SJ, Whitney SL, et al. Vestibular rehabilitation for peripheral vestibular hypofunction: an evidence-based clinical practice guideline: from the American Physical Therapy Association Neurology Section. J Neurol Phys Ther. 2016;40:124–155. doi: 10.1097/NPT.0000000000000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E31.Sherrington C, Fairhall N, Wallbank G, et al. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med. 2020;54:885–891. doi: 10.1136/bjsports-2019-101512. [DOI] [PubMed] [Google Scholar]
- E32.Finger RP, Bertram B, Wolfram C, Holz FG. Blindness and visual impairment in Germany—a slight fall in prevalence. Dtsch Arztebl Int. 2012;109:484–489. doi: 10.3238/arztebl.2012.0484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E33.Donaldson PJ, Grey AC, Heilman BM, Lim JC, Vaghefi E. The physiological optics of the lens. Prog Retin Eye Res. 2017;56:e1–e24. doi: 10.1016/j.preteyeres.2016.09.002. [DOI] [PubMed] [Google Scholar]
- E34.Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125:1492–1499. doi: 10.1016/j.ophtha.2018.04.013. [DOI] [PubMed] [Google Scholar]
- E35.Stahl A. The diagnosis and treatment of age-related macular ¬degeneration. Dtsch Arztebl Int. 2020;117 doi: 10.3238/arztebl.2020.0513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E36.Vennemann MM, Hummel T, Berger K. The association between smoking and smell and taste impairment in the general population. J Neurol. 2008;255:1121–1126. doi: 10.1007/s00415-008-0807-9. [DOI] [PubMed] [Google Scholar]
- E37.Santos DV, Reiter ER, DiNardo LJ, Costanzo RM. Hazardous events associated with impaired olfactory function. Arch Otolaryngol Head Neck Surg. 2004;130:317–319. doi: 10.1001/archotol.130.3.317. [DOI] [PubMed] [Google Scholar]
- E38.Oleszkiewicz A, Schriever VA, Croy I, Hähner A, Hummel T. Updated Sniffin’Sticks normative data based on an extended sample of 9139 subjects. Eur Arch Otorhinolaryngol. 2019;276:719–728. doi: 10.1007/s00405-018-5248-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E39.Eliyan Y, Wroblewski KE, McClintock MK, Pinto JM. Olfactory dysfunction predicts the development of depression in older US adults. Chem Senses. 2021 doi: 10.1093/chemse/bjaa075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E40.Hüttenbrink K-B, Hummel T, Berg D, Gasser T, Hähner A. Olfactory dysfunction: common in later life and early warning of ¬neurodegenerative disease. Dtsch Arztebl Int. 2013;110 doi: 10.3238/arztebl.2013.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E41.Schwob JE. Neural regeneration and the peripheral olfactory system. Anant Rec. 2002;269:33–49. doi: 10.1002/ar.10047. [DOI] [PubMed] [Google Scholar]
- E42.Durante MA, Kurtenbach S, Sargi ZB, et al. Single-cell analysis of olfactory neurogenesis and differentiation in adult humans. Nat Neurosci. 2020;23:323–326. doi: 10.1038/s41593-020-0587-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E43.Bergmann O, Liebl J, Bernard S, et al. The age of olfactory bulb neurons in humans. Neuron. 2012;74:634–639. doi: 10.1016/j.neuron.2012.03.030. [DOI] [PubMed] [Google Scholar]
- E44.Lötsch J, Schaeffeler E, Mittelbronn M, et al. Functional genomics suggest neurogenesis in the adult human olfactory bulb. Brain Struct Funct. 2014;219:1991–2000. doi: 10.1007/s00429-013-0618-3. [DOI] [PubMed] [Google Scholar]
- E45.Gudziol V, Buschhüter D, Abolmaali N, Gerber J, Rombaux P, Hummel T. Increasing olfactory bulb volume due to treatment of chronic rhinosinusitis—a longitudinal study. Brain. 2009;132:3096–3101. doi: 10.1093/brain/awp243. [DOI] [PubMed] [Google Scholar]
- E46.Yousem DM, Maldjian JA, Hummel T, et al. The effect of age on odor-stimulated functional MR imaging. AJNR Am J Neuroradiol. 1999;20:600–608. [PMC free article] [PubMed] [Google Scholar]
- E47.Lötsch J, Hummel T. Clinical usefulness of self-rated olfactory ¬performance—a data science-based assessment of 6000 patients. Chemical Senses. 2019;44:357–364. doi: 10.1093/chemse/bjz029. [DOI] [PubMed] [Google Scholar]
- E48.Hummel T, Rosenheim K, Konnerth C-G, Kobal G. Screening of olfactory function with a four-minute odor identification test: reliability, normative data, and investigations in patients with olfactory loss. Ann Otol Rhinol Laryngol. 2001;110:976–981. doi: 10.1177/000348940111001015. [DOI] [PubMed] [Google Scholar]
- E49.Oleszkiewicz A, Park D, Resler K, et al. Quality of life in patients with olfactory loss is better predicted by flavor identification than by orthonasal olfactory function. Chemical Senses. 2019;44:371–377. doi: 10.1093/chemse/bjz027. [DOI] [PubMed] [Google Scholar]
- E50.Whitcroft KL, Cuevas M, Haehner A, Hummel T. Patterns of olfactory impairment reflect underlying disease etiology. Laryngoscope. 2017;127:291–295. doi: 10.1002/lary.26229. [DOI] [PubMed] [Google Scholar]
- E51.Liu B, Luo Z, Pinto JM, et al. Relationship between poor olfaction and mortality among community-dwelling older adults: A cohort study. Ann Intern Med. 2019;170:673–681. doi: 10.7326/M18-0775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E52.Mainland JD, Barlow LA, Munger SD, et al. Identifying treatments for taste and smell disorders: gaps and opportunities. Chemical Senses. 2020;45:493–502. doi: 10.1093/chemse/bjaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E53.Wegener B-A, Croy I, Hähner A, Hummel T. Olfactory training with older people. Int J Geriatr Psychiatry. 2018;33:212–220. doi: 10.1002/gps.4725. [DOI] [PubMed] [Google Scholar]
- E54.Haehner A, Boesveldt S, Berendse HW, et al. Prevalence of smell loss in Parkinson‘s disease—a multicenter study. Parkinsonism ¬Relat Disord. 2009;15:490–494. doi: 10.1016/j.parkreldis.2008.12.005. [DOI] [PubMed] [Google Scholar]
- E55.Welge-Lüssen A, Dörig P, Wolfensberger M, Krone F, Hummel T. A study about the frequency of taste disorders. J Neurol. 2011;258:386–392. doi: 10.1007/s00415-010-5763-5. [DOI] [PubMed] [Google Scholar]
- E56.Fark T, Hummel C, Hähner A, Nin T, Hummel T. Characteristics of taste disorders. Eur Arch Otorhinolaryngol. 2013;270:1855–1860. doi: 10.1007/s00405-012-2310-2. [DOI] [PubMed] [Google Scholar]
- E57.Ogawa T, Annear MJ, Ikebe K, Maeda Y. Taste-related sensations in old age. J Oral Rehabil. 2017;44:626–635. doi: 10.1111/joor.12502. [DOI] [PubMed] [Google Scholar]
- E58.Mojet J, Heidema J, Christ-Hazelhof E. Taste perception with age: generic or specific losses in supra-threshold intensities of five taste qualities? Chemical Senses. 2003;28:397–413. doi: 10.1093/chemse/28.5.397. [DOI] [PubMed] [Google Scholar]
- E59.Landis BN, Just T. Schmeckstörungen. HNO. 2009:95–106. [Google Scholar]
- E60.Wickremaratchi MM, Llewelyn JG. Effects of ageing on touch. Postgrad Med J. 2006;82:301–304. doi: 10.1136/pgmj.2005.039651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E61.Libouton X, Barbier O, Plaghki L, Thonnard J-L. Tactile roughness discrimination threshold is unrelated to tactile spatial acuity. Behav Brain Res. 2010;208:473–478. doi: 10.1016/j.bbr.2009.12.017. [DOI] [PubMed] [Google Scholar]
- E62.Perry SD. Evaluation of age-related plantar-surface insensitivity and onset age of advanced insensitivity in older adults using vibratory and touch sensation tests. Neurosci Lett. 2006;392:62–67. doi: 10.1016/j.neulet.2005.08.060. [DOI] [PubMed] [Google Scholar]
- E63.Peters RM, McKeown MD, Carpenter MG, Inglis JT. Losing touch: age-related changes in plantar skin sensitivity, lower limb cutaneous reflex strength, and postural stability in older adults. J Neurophysiol. 2016;116:1848–1858. doi: 10.1152/jn.00339.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E64.Grunwald M, Busse F, Hensel A, et al. Theta-power differences in patients with mild cognitive impairment under rest condition and during haptic tasks. Alzheimer Dis Assoc Disord. 2002;16:40–48. doi: 10.1097/00002093-200201000-00006. [DOI] [PubMed] [Google Scholar]
- E65.Kleinman JM, Brodzinsky DM. Haptic exploration in young, middle-aged, and elderly adults. J Gerontol. 1978;33:521–527. doi: 10.1093/geronj/33.4.521. [DOI] [PubMed] [Google Scholar]
- E66.Adamo DE, Martin BJ, Brown SH. Age-related differences in upper limb proprioceptive acuity. Percept Mot Skills. 2007;104:1297–1309. doi: 10.2466/pms.104.4.1297-1309. [DOI] [PubMed] [Google Scholar]
- E67.Kalisch T, Kattenstroth J-C, Kowalewski R, Tegenthoff M, Dinse HR. Cognitive and tactile factors affecting human haptic performance in later life. PLoS One. 2012;7 doi: 10.1371/journal.pone.0030420. e30420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E68.Pickard CM, Sullivan PE, Allison GT, Singer KP. Is there a difference in hip joint position sense between young and older groups? J Gerontol A Biol Sci Med Sci. 2003;58:631–635. doi: 10.1093/gerona/58.7.m631. [DOI] [PubMed] [Google Scholar]
- E69.Ribeiro F, Oliveira J. Aging effects on joint proprioception: the role of physical activity in proprioception preservation. European Review of Aging and Physical Activity. 2007;4:71–76. [Google Scholar]
- E70.Müller S, Winkelmann C, Grunwald M. Haptik im Gesundheitsberuf - Relevanz für Physiotherapeuten, Ergotherapeuten und Pflegeberufe. Berlin, Heidelberg: Springer (in press) [Google Scholar]
- E71.Playfair C. Human relationships: an exploration of loneliness and touch. Br J Nurs. 2010;19:122–126. doi: 10.12968/bjon.2010.19.2.46301. [DOI] [PubMed] [Google Scholar]
- E72.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172:1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E73.Hogstel MO. Older widowers: a small group with special needs. Geriatr Nurs. 1985;6:24–26. doi: 10.1016/s0197-4572(85)80104-x. [DOI] [PubMed] [Google Scholar]
- E74.Gleeson M, Timmins F. The use of touch to enhance nursing care of older person in long-term mental health care facilities. J Psychiatr Ment Health Nurs. 2004;11:541–545. doi: 10.1111/j.1365-2850.2004.00757.x. [DOI] [PubMed] [Google Scholar]
- E75.Gadkaree SK, Sun DQ, Li C, et al. Does sensory function decline independently or concomitantly with age? Data from the Baltimore longitudinal study of aging. J Aging Res. 2016;2016 doi: 10.1155/2016/1865038. 1865038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E76.Noppeney U, Jones SA, Rohe T, Ferrari A. See what you hear-how the brain forms representations across the senses. Neuroforum. 2018;24:A169–A181. [Google Scholar]
- E77.Parker JL, Robinson CW. Changes in multisensory integration across the life span. Psychol Aging. 2018;33:545–558. doi: 10.1037/pag0000244. [DOI] [PubMed] [Google Scholar]
- E78.Freiherr J, Lundström JN, Habel U, Reetz K. Multisensory integration mechanisms during aging. Front Hum Neurosci. 2013;7 doi: 10.3389/fnhum.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E79.Higgen FL, Heine C, Krawinkel L, et al. Crossmodal congruency enhances performance of healthy older adults in visual-tactile pattern matching. Front Aging Neurosci. 2020;12 doi: 10.3389/fnagi.2020.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E80.Murray MM, Eardley AF, Edginton T, Oyekan R, Smyth E, Matusz PJ. Sensory dominance and multisensory integration as screening tools in aging. Sci Rep. 2018;8:1–11. doi: 10.1038/s41598-018-27288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E81.Stein BE, Stanford TR, Rowland BA. Multisensory integration and the Society for Neuroscience: then and now. J Neurosci. 2020;40:3–11. doi: 10.1523/JNEUROSCI.0737-19.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E82.Leon M, Woo C. Environmental enrichment and successful aging. Front Behav Neurosci. 2018;12 doi: 10.3389/fnbeh.2018.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]