Abstract
Introduction
Rabies is a fatal zoonotic infectious disease that poses a serious threat to public health in China. Since 2005, a National Animal Rabies Surveillance System has been operating to understand the rabies situation in animals in China with a view to control and eventually eliminate dog-mediated human rabies.
Methods
From 2010, the brain tissues of dogs, livestock, and wild animals showing rabies-like clinical signs were collected and tested by the National Reference Laboratory (NRL) for Animal Rabies to analyze the epidemiological characteristics of rabies, including animal species, geographic distribution, and transmission sources. Over the same period, clinically suspected animal rabies cases were collected by Animal Disease Control Centers through the National Animal Disease Monitoring Information Platform (NADMIP) and then reported in the Veterinary Bulletin.
Results
During 2010–2020, 170 of 212 suspected animal rabies cases were submitted to and confirmed by NRL as rabies virus-positive. Of these confirmed cases dogs, especially free-roaming and ownerless dogs in rural areas, were major transmission hosts (71/170). A total of 51 infected dogs attacked humans with 45 biting more than one person. The dog cases were reported all year round, but with significantly more in spring and summer. The majority of livestock rabies cases (70/80) being caused by rabid wild foxes in Xinjiang and Inner Mongolia revealed that foxes play a pivotal role in animal rabies epizootics in the north and northwest of the country.
Conclusion
Dogs were the main transmission sources of rabies in China, and along with the recent increase of rabies in foxes and other wildlife, presented an increasing threat to livestock and public health.
Keywords: Animal, Rabies, Epidemics, Rabies Virus
INTRODUCTION
Rabies is a zoonotic disease caused by rabies virus (RABV) and rabies-related lyssaviruses (1). It is a serious public concern in China with the majority of human rabies cases caused by rabid dogs (2). Since 2005, to understand the epidemiology of animal rabies and to establish a comprehensive control strategy, animal rabies surveillance throughout the country has been implemented under the National Animal Rabies Prevention and Control Plan by the Ministry of Agriculture and Rural Affairs of China (MARA) (3). According to the Rabies Surveillance Plan, animal rabies surveillance must be conducted across the country to identify the major transmitters, their geographical distribution, and roles in transmission of rabies to human and domestic animals. Through the National Animal Disease Monitoring Information Platform (NADMIP), details of suspected animal rabies cases based on clinical signs have been collected and reported to the China Animal Disease Control Center by provincial and municipality Animal Disease Control Centers, and then published in the Veterinary Bulletin, an official journal of MARA for the dissemination of monthly information on animal infectious diseases in China since 2010 ( http://www.moa.gov.cn/zwllm/tzgg/gb/sygb/). Most of these suspected cases were diagnosed by clinical observation and investigation, with only a small part being subjected to brain tissue collection for laboratory diagnosis in National Reference Laboratory (NRL). Here, only evidence-based data have been used for analyzing the epidemiological characteristics of animal rabies in China.
METHODS
According to the Rabies Surveillance Plan, brain tissues of rabies-suspected animals (dogs behaving abnormally or biting humans, livestock showing rabies-like clinical signs, dead foxes, wolves, and raccoon dogs) with background information submitted to NRL by provincial and municipality Animal Disease Control Centers (CADCs) as well as Forestry and Grassland Administrations of China, were examined by the direct fluorescent antibody test (DFA) using fluorescein isothiocyanate (FITC)-conjugated anti-rabies monoclonal antibody (Fujirebio Diagnostics Inc., USA) (4). Concurrently, information on suspected animal rabies based on clinical observation and investigation was collected by provincial CADCs, reported through NADMIP to the National CADC, and published monthly in the Veterinary Bulletin.
RESULTS
Over the period 2010 to 2020, brain tissues (80.2%, 170/212) of suspected animal rabies cases submitted from 16 provincial-level administrative divisions (PLADs) to NRL were confirmed to be rabies positive by DFA (Table 1). Over the same period, the Veterinary Bulletin reported 1,132 suspected rabies deaths (Figure 1), showing a trend similar to that of the laboratory-confirmed findings (Figure 2). The data showed a rapid increase of animal rabies in 2020.
Table 1. The ratios of confirmed animal rabies cases in China, 2010–2020.
| Item | IM | CQ | SH | XJ | SX | ZJ | GD | TJ | HeN | GS | HLJ | JS | SN | GX | HN | JX |
| Note: ratios=positive samples/total samples submitted.
–: No sample submitted. Abbreviations: IM=Inner Mongolia Autonomous Region; CQ=Chongqing Municipality; SH=Shanghai Municipality; XJ=Xinjiang Uyghur Autonomous Region; SX=Shanxi Province; ZJ=Zhejiang Province; GD=Guangdong Province; TJ=Tianjin Municipality; HeN=Henan Province; GS=Gansu Province; HLJ=Heilongjiang Province; JS=Jiangsu Province; SN=Shaanxi Province; GX=Guangxi Zhuang Autonomous; HN=Hainan Province; JX=Jiangxi Province. | ||||||||||||||||
| 2010 | – | 3/3 | 3/4 | – | 6/6 | – | – | – | – | – | – | – | – | – | – | – |
| 2011 | – | 6/6 | 1/2 | – | 1/1 | – | – | – | – | – | – | – | – | – | – | – |
| 2012 | – | 2/3 | – | – | 1/1 | – | – | – | – | – | – | – | – | – | – | – |
| 2013 | 3/3 | 3/3 | 1/1 | 2/3 | 1/1 | – | 0/1 | – | – | – | – | – | – | – | – | – |
| 2014 | 8/12 | 2/4 | 1/2 | 4/6 | 1/1 | – | – | 1/1 | – | 1/1 | – | – | – | – | – | – |
| 2015 | 2/2 | 5/6 | – | 2/2 | 2/2 | – | – | – | 1/1 | – | – | – | – | 0/2 | 0/1 | – |
| 2016 | 4/4 | – | 2/2 | 1/1 | – | 2/2 | 1/1 | – | – | 0/1 | 1/2 | – | 0/1 | – | – | – |
| 2017 | 3/4 | 4/4 | – | 2/2 | – | – | 1/1 | 1/1 | – | – | – | – | – | – | – | – |
| 2018 | 4/4 | 0/1 | 1/1 | 0/1 | – | 1/3 | – | – | 1/1 | – | – | 1/1 | 0/1 | – | – | – |
| 2019 | 3/4 | – | 9/10 | 1/1 | – | 0/5 | – | – | – | – | – | – | – | – | – | 0/1 |
| 2020 | 59/64 | – | 5/6 | – | – | 0/1 | – | – | – | – | – | – | – | – | – | – |
| Positive rate | (86/97) | (25/30) | (23/28) | (12/16) | (12/12) | (3/11) | (2/3) | (2/2) | (2/2) | (1/2) | (1/2) | (1/1) | (0/2) | (0/2) | (0/1) | (0/1) |
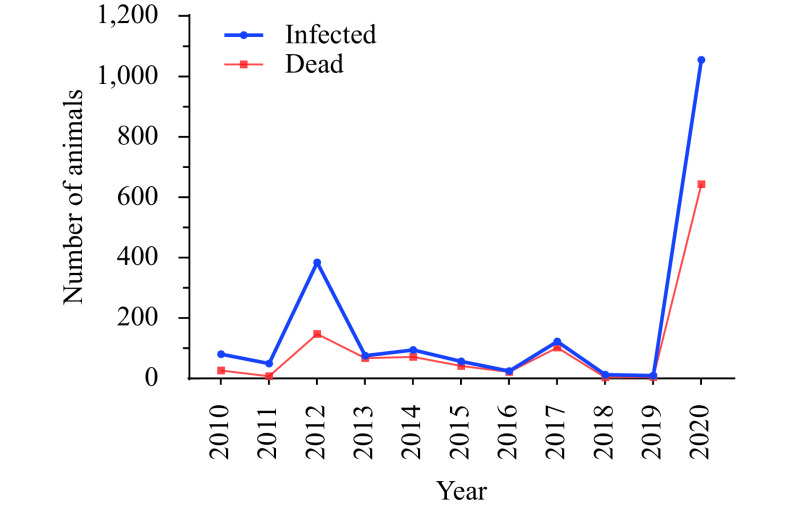
Figure 1.
Domestic animal rabies cases reported in the Veterinary Bulletin, 2010–2020.
Note: The domestic animal species include dogs and livestock.
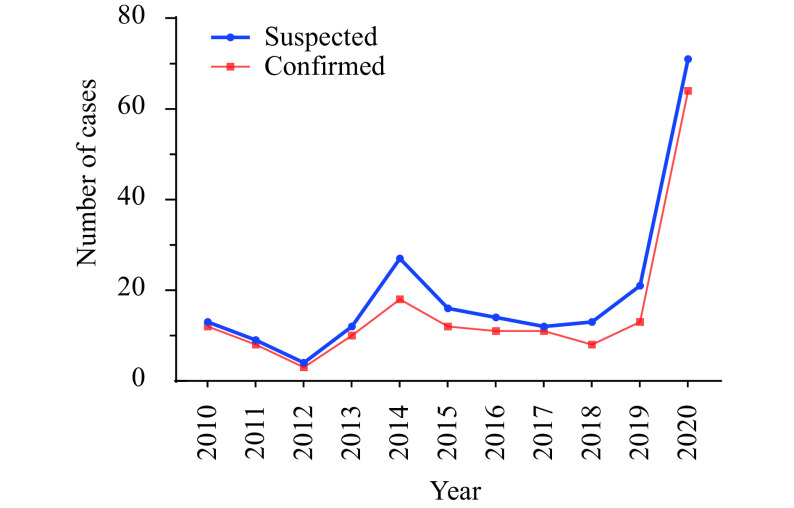
Figure 2.
Confirmed animal rabies cases in China, 2010–2020, reported by the National Reference Laboratory.
Among the positive cases, dogs were the main rabid animals, accounting for 41.8% of total cases (71/170), followed by cattle (28.2%, 48/170), sheep (13.5%, 23/170), foxes (Vulpes vulpes) (9.4%, 16/170), camels (4.1%, 7/170), badgers (Meles leucurus) (1.2%, 2/170), a raccoon dog (Nyctereutes procyonoides) (0.6%, 1/170), a horse (0.6%, 1/170), and a donkey (0.6%, 1/170).
Further analysis showed that infected dogs, and especially those that were free-roaming or stray, were major transmission sources in rural areas (45/71). The ratio of rural dogs to urban dogs was 1.7 (45∶26). Of the 51 rabid dogs that attacked people, 45 (88.2%) bit more than one person, with one even biting 63. All victims received timely post-exposure prophylaxis (PEP). The number of animal rabies cases varied seasonally, with higher incidences in spring (28) and summer (20) than in autumn (15) and winter (8).
Yearly numbers of infected and dead animal rabies cases reported in the Veterinary Bulletin varied, but with a marked increase in both during 2020 (Figure 1). There was a high correlation with increases in confirmed rabies cases reported by Changchun Veterinary Research Institute (CVRI). According to CVRI surveillance, the majority of livestock rabies cases (70/80) were caused by rabid wild foxes, which served as a major transmission source and reservoir in Xinjiang Uygur and Inner Mongolia autonomous regions. Rabies in badgers and a raccoon dog were also confirmed in Inner Mongolia Autonomous Region in 2020, revealing the diversity of animal reservoirs.
DISCUSSION
Reported human rabies cases in China have steadily declined from 3,300 in 2007 to 202 in 2020 (5), benefiting from improvements in the governmental supervision system as well as the ready availability of PEP (6). Nevertheless, animal rabies continues to expand geographically over the country, and emerging and reemerging cases have been reported over the last decade in previously rabies-free or low-incidence regions such as Heilongjiang, Xinjiang, Inner Mongolia, Tibet, and Qinghai PLADs and Taiwan, China (7-9). Even though animal rabies is spreading, however, the reported animal cases were still less than the number of reported human cases, likely due to inadequate surveillance and a lack of awareness of reporting and laboratory procedures. Animal rabies cases were therefore likely to have been underestimated. Evidence for this was provided by the numbers of reported cases of laboratory-confirmed animal rabies (Figure 2 and Table 1), which were much lower than those reported in the Veterinary Bulletin (Figure 1); i.e., the majority of suspected animal rabies cases in China were not diagnosed in laboratories. However, the fact that the rabies positive detection rate in suspected cases was generally high, as shown in Table 1 and Figure 2, indicating that clinical judgement on rabies based on nervous system symptoms and aggressiveness of suspected animals was acceptable in the absence of laboratory methods, and therefore can be used to predict animal rabies status.
Our results have also revealed that rabid dogs, particularly from rural areas, continue to be the main sources of transmission of rabies virus in China. In addition, dogs showing strange behavior or biting more than one person (mostly free-roaming or stray) were usually confirmed as being rabid. There being no effective management of the health of free-roaming and stray dogs, it is difficult to implement dog vaccination in rural areas (6). To date, cat rabies has not been reported nor identified during our surveillance. This may be due to cats exploiting a rather solitary existence, resulting in cats not playing a significant role in rabies transmission as reported in a previous study (10).
The data reveal a remarkable increase in 2020 (Figures 1–2), which has been ascribed to increasing numbers of cases of rabies in livestock in Inner Mongolia (Table 1) since it was first confirmed there in 2013 in wild foxes (8). Since then, animal rabies has been increasing in Inner Mongolia Autonomous Region with cases in 25 livestock (cattle, sheep, and camels) diagnosed between 2013 and 2018 (11). This trend continued in 2020 with 59 laboratory-confirmed cases by NRL and 597 clinically-judged cases in Inner Mongolia Autonomous Region published in the Veterinary Bulletin. Our previous study showed a spillover of fox RABV strains to other rabies transmitters such as dogs, badgers, and raccoon dogs, with the field RABVs in Inner Mongolia Autonomous Region showing a broad genetic diversity and with fox-origin variants closely related to strains circulating in Xinjiang Uyghur Autonomous Region and the surrounding countries including Mongolia and Russia (11). A case of fox-mediated human rabies was confirmed in Xinjiang Uyghur Autonomous Region in 2016 (12). These observations not only demonstrated the spillover of wildlife RABVs into dogs in the past decade but have also indicated that the risk of spillover is increasing and threatening public health in northwestern China.
In addition to terrestrial animals, a bat (Murina leucogaster) harboring Irkut virus was confirmed in Jilin in 2012 (13). This was the first bat-borne lyssavirus identified in China, suggesting that public warnings regarding bat bites should be increased.
This study was subject to some limitations. Although national surveillance systems for animal rabies have been established in China, the animal rabies case reporting is not comprehensive. The reported and confirmed dog rabies cases in this study were far below the human cases, especially in high incidence provinces of human rabies. The infrequent information sharing between the human and animal health sectors was identified as major gap. Cross-department cooperation should be enhanced. Furthermore, the national reference laboratory is responsible for diagnosis of animal rabies at the national level; however, the laboratory diagnostic capacity of most provincial CADCs remains weak.
MARA has made substantial progress in dog rabies control in last decade. A National Medium- and Long-term Plan for Animal Epidemic Prevention and Control (2012–2020) was issued by the General Office of the State Council in 2012 (14). To implement this plan, MARA has published every year since 2005 a National Animal Disease Surveillance and Epidemiological Survey, which includes animal rabies surveillance across the country. In addition, the National Animal Rabies Prevention and Control Plan (2017–2020) implemented by MARA in 2017 further strengthens prevention and control strategy (15). Nevertheless, there remain major challenges for China to achieve the goal of eliminating dog-mediated human rabies by 2030. Compulsory dog vaccination covering the entire country must be initiated in a multiple-sector based collaborative manner, including participation of the public.
Contributor Information
Zhanying Kou, Email: syggwsc@126.com.
Changchun Tu, Email: changchun_tu@hotmail.com.
References
- 1.Miao FM, Li N, Yang JJ, Chen T, Liu Y, Zhang SF, et al Neglected challenges in the control of animal rabies in China. One Health. 2021;12:100212. doi: 10.1016/j.onehlt.2021.100212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tao XY, Liu SQ, Zhu WY, Rayner S Rabies surveillance and control in China over the last twenty years. Biosaf Health. 2021;3(3):142–7. doi: 10.1016/j.bsheal.2020.11.004. [DOI] [Google Scholar]
- 3.Tu CC, Feng Y, Wang YY Animal rabies in the People’s Republic of China. Rev Sci Tech. 2018;37(2):519–28. doi: 10.20506/rst.37.2.2820. [DOI] [PubMed] [Google Scholar]
- 4.Rupprecht CE, Fooks AR, Abela-Ridder B. Laboratory techniques in rabies volume 1. 5th ed. Geneva: World Health Organization. 2018; p. 29−108. https://www.who.int/publications/i/item/9789241515153.
- 5.National Health Commission of the People’s Republic of China. General Situation of National Legal Infectious Diseases, 2020. http://www.nhc.gov.cn/jkj/s3578/202103/f1a448b7df7d4760976fea6d55834966.shtml. [2021-3-12]. (In Chinese).
- 6.Yin WW, Dong J, Tu CC, Edwards J, Guo FS, Zhou H, et al Challenges and needs for China to eliminate rabies. Infect Dis Poverty. 2013;2(1):23. doi: 10.1186/2049-9957-2-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tao XY, Li ML, Wang Q, Baima C, Hong M, Li W, et al The reemergence of human rabies and emergence of an Indian subcontinent lineage in Tibet, China. PLoS Negl Trop Dis. 2019;13(1):e0007036. doi: 10.1371/journal.pntd.0007036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feng Y, Wang W, Guo J, Alatengheli, Li Y, Yang G, et al Disease outbreaks caused by steppe-type rabies viruses in China. Epidemiol Infect. 2015;143(6):1287–91. doi: 10.1017/S0950268814001952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiou HY, Hsieh CH, Jeng CR, Chan FT, Wang HY, Pang VF Molecular characterization of cryptically circulating rabies virus from ferret badgers, Taiwan. Emerg Infect Dis. 2014;20(5):790–8. doi: 10.3201/eid2005.131389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baer GM The natural history of rabies: volume I, 2nd ed. New York: Academic Press. 1975;:139–55. doi: 10.1016/C2012-0-01433-0. [DOI] [Google Scholar]
- 11.Feng Y, Wang YY, Xu WD, Tu ZZ, Liu TF, Huo MH, et al Animal rabies surveillance, China, 2004–2018. Emerg Infect Dis. 2020;26(12):2825–34. doi: 10.3201/eid2612.200303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taxitiemuer A, Tuerdi G, Zhang Y, Wushouer F, Tao XY, Talipu J, et al An investigation of the first case of human rabies caused by a fox in China in May 2016. Biomed Environ Sci. 2017;30(11):825–8. doi: 10.3967/bes2017.110. [DOI] [PubMed] [Google Scholar]
- 13.Liu Y, Chen Q, Zhang F, Zhang SF, Li N, Lian H, et al Evaluation of rabies biologics against Irkut virus isolated in China. J Clin Microbiol, 2013;51(11):3499–504. doi: 10.1128/JCM.01565-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.General Office of the State Council. National medium- and long-term plan for animal epidemic prevention and control (2012–2020). 2012. http://www.gov.cn/xxgk/pub/govpublic/mrlm/201205/t20120525_65163.html. [2012-5-20]. (In Chinese).
- 15.Ministry of Agriculture and Rural Affairs of the People’s Republic of China. National animal rabies prevention and control plan (2017–2020). 2017. http://www.xmsyj.moa.gov.cn/zcjd/201904/t20190429_6287267.htm. [2017-6-16]. (In Chinese).