Abstract
Background and aim of the work:
Proximal humeral fractures incidence in the elderly population is increasing. Treatment management is complicated by fracture complexity and patients’ comorbidities. The aim of our prospective study is the outcome evaluation of the role of minimally invasive plate osteosynthesis (MIPO) for elderly patients with a 3- or 4-parts proximal humeral fractures having an intact medial wall.
Methods:
N=45 patients were selected using inclusion criteria (>75yo, unilateral 3- or 4-parts proximal humeral fracture and with a surgical indication). We analyzed n=42 fractures treated with MIPO (3 patients had been reversed to ORIF and arthroplasty intraoperatively): n=20 4-parts fractures and n=22 were 3-parts. Of the 42 operated patients 17 identified as male and 25 as female (mean age 84yo). A trans-deltoid approach has been used with minimal surgical exposure and tissue damage to preserve the local tissue for early shoulder mobilization.
Results:
At follow-up, the DASH recorded mean value was 72, while the Constant mean score was 68. Complications have been recorded in 23,8% of patients with 4-parts fractures having the highest complication frequency. Mean shoulder joint ROM was recorded: anterior elevation 75°, lateral elevation 80°, abduction 90°, intra-rotation 50°, extra-rotation 25°. The following factors were identified influencing the outcome: >8mm calcar fragment, head valgus impaction and periosteal medial hinge preservation.
Conclusions:
The increase in population longevity matches the increase in complex humeral fracture frequency. We strongly for management consensus for proximal humerus fracture, in a similar way as for neck femoral fractures. MIPO is excellent in reducing soft tissue damage and complications for elderly patients with limited functional demand. (www.actabiomedica.it)
Keywords: minimally invasive plate osteosynthesis, proximal humeral fracture, elderly population, medial hinge
Introduction
Humeral fractures represent around 7% of all fractures; of those around 4% involve the proximal part of the humerus with an incidence of 48-142 cases every 100000 people; In the elderly proximal humeral fractures are the third most common fracture (after femoral and wrist fractures respectively) with 2:1 female-to-male ratio (1). The predominance in the female population over 60 years could be explained by the higher prevalence Osteoporosis (i.e. it is estimated that around 50% of patients over 85 years old reported at least once-a-year fall, with women 2 times more frequently than men (1)). Moreover, fractures of the proximal humerus are extremely invalidating as patients are likely to suffer other pathologies that influence fracture management and treatment.
In the next future, the increased incidence of this type of fracture is expected to match the increased longevity rates and, compared to posterior data, we can already observe a rise in proximal humeral fracture incidence (1). Palvanen et al. estimated a 3-fold increase in proximal humeral fractures in the next 3 decades (2).
In the United States alone 275.000 proximal humeral fractures are estimated by 2030, with a growing incidence of 50% in 15 years when compared to data collected in 2008 (graph 1) (2).
Graph 1:

Estimated growing incidence of proximal humeral fractures in the United States in the next 30 years (Solberg et al.)
According to Cornell (3), roughly 80% of proximal humeral fractures are stable, 2-parts fractures with minimal or no displacement that can be treated conservatively with optimal results. However the growing frequency of unstable proximal humeral fractures open a debate over the efficiency of surgical treatment: the future perspective is taking into consideration the plethora of comorbidities and problems of each patient to correctly manage the trauma and its healthcare costs, similarly to the consensus established for neck femoral fractures.
There are no universally accepted guidelines or a univocal treatment for proximal humeral fractures as every clinical case stands on its own: especially in the aged population comorbidities and functional demand have both a strong influence on clinical management. Just “treating” the fracture is simply not enough: the orthopedic surgeon must have a 360-degree global consideration of the patients: age, bone mineral density, comorbidities and functional demand of the affected limb. Proximal humeral epiphyseal fractures can be classified according to the Neer, AO and Hertel classification systems. The advantage of the Neer classification lies in its homogenous subdivisions leading to a rapid and practical management guide (4), making it the most used classification system:
proximal humeral fractures are classified as displaced if any of the fragments has a > 45° angulation or a separation of > 1cm, dividing them into 6 classes. Our study intends to prospectively evaluate the role of minimally invasive plate osteosynthesis for elderly patients with 3 and 4-parts proximal humeral fractures with an intact medial wall (so with minimal varus/valgus head impaction) using a trans-deltoid approach and preserving the local bioenvironment of the medial compartment of the shoulder.
The rationale is fracture reduction and functional recovery by minimizing the risks of the surgical treatment, ensuring the preservation of the local bone biology with a minimally invasive approach. This includes borderline cases where shoulder arthroplasty is indicated but the general health conditions halt from more invasive procedures. The principle of mini-invasive surgery is obtaining the best results with minimal impaction on functional structures (5). Minimally invasive procedures have the benefit to reduce surgical exposition, infectious risk and blood supply, soft tissues and skin damage.
The LCP (locking compression plate) technique is based on the decreased friction between the plate and the bone surface to enhance subchondral bone-screws interface stability. Numerous divergent and convergent multidirectional screws can be utilized to augment the osteosynthesis angular stabilization to reduce pain and enhance the postoperative outcome (6).
Materials and methods
From February 2019 to February 2020 n=45 patients were included in the study. Inclusions criteria were: a) age > 75 years old; b) 3 or 4-parts proximal humerus fracture C) surgical indication. Also, exclusion criteria identified were: a) age <75 years; b) conservative treatments; c) surgical indications for treatments other than MIPO; d) open fractures. Intraoperatively the surgical indication for 3 patients has changed: 2 underwent an ORIF procedure and 1 a reverse shoulder arthroplasty. None of our patients were treated conservatively or with an external fixator. In total n=42 patients were treated with MIPO (table 1): 16 GmbH plates (DePuy Synthes®, Solothurn, Switzerland, and 26 PHILOS plats (DePuy Synthes®, Solothurn, Switzerland). Patients have been divided by self-identified gender (17 males and 25 female) and by fracture type (20 4-part fractures and 22 3-parts fractures). The mean age was 84 years (75-94), the dominant side is the right one, involved in 80% of cases. The injury mechanism was a fall from standing height for 41 patients, a traffic accident in 3 patients and a fall from the top of the stairs for 1 patient. Clinical and radiographic follow-ups have been planned at 3, 6, and 12 months after surgery with a median follow-up time of 9 months. The average time between the traumatic episode and the surgical treatment was 2.6 days (2-6 days). Arthroplasty is a possible treatment for proximal humeral fracture but we have decided to exclude it due to the high frequency of comorbidities in our cohort (e.g. diabetes, obesity, etc.)
Table 1.
Patients divided by type of fracture, calcar and impaction angle
| 3 fragments | 4 fragments | |
| Calcar >8mm | 5 | 8 |
| Calcar < 8mm | 7 | 13 |
| Valgus angulation | 15 | 12 |
| Varus angulation | 7 | 8 |
All patients have been clinically and radiographically using XR and CT image modalities evaluated pre- and intraoperatively (to ensure correct arm positioning) and at follow-ups (7). X-ray views have been taken according to trauma x-ray series theorized by Neer: an anteroposterior (AP) view, a lateral scapular view (also known as Y scapular) and an axillary view in the supine position, when feasible (figure 4). The AP glenoid view has been used to evaluate any varus/valgus shift of the surgical neck and of the tuberosities. As the scapula lies obliquely over the thoracic wall, x-ray beans must be inclined by 40°. The axillary view gives information for any eventual displacement of the humeral tuberosities; it can be obtained by using a Velpeau view: the patient is seated and lies 45° backward. It is fundamental to evaluate the humeral head angular displacement, tuberosities dislocation and the length of the intact metaphyseal segment and bone healing (8). Two parameters are crucial: the humeral head-shaft angulation (HSA), measured from the crossing of 1) a line tangent to the shoulder articular surface and 2) a line parallel to the humeral shaft axis; the HSA is directly correlated to the medial hinge integrity. The second parameter is the height of the humeral head (HHH), directly correlated to the (absolute or relative) upward displacement of the lesser trochanter, measured as the vertical distance between the greater trochanter and a line tangent to the highest point of the humeral head. Preoperative measurements are compared at follow-ups: an HSA > 120° and a decrease by 10° are considered negative prognostic factors (6)(8).
Figure 4.
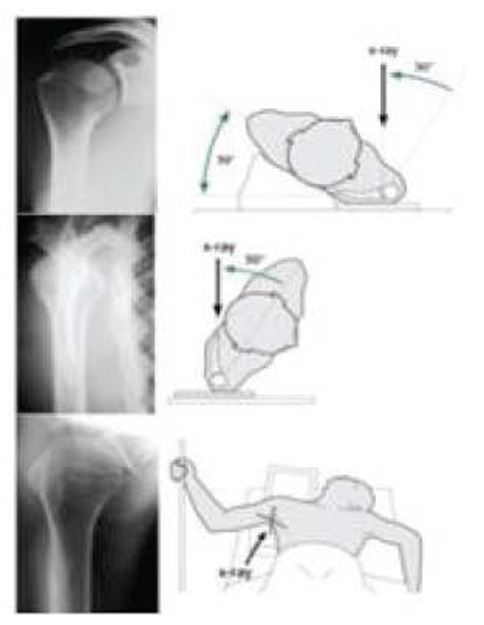
AP, lateral and axillary view
Figure 1.

Neer Classification, 1970
Figure 2.

The AO/OTA Classification
Figure 3.

The Hertel classification
Other negative predictive factors are: humeral head varus/valgus rotation, greater trochanter displacement >8mm relative to the anatomical neck superior margin, glenohumeral luxation, comminution and humeral head splitting.
High-quality axial CT series with 2 mm section are used to identify humeral head displacement degree or fragments number; surgical treatment is indicated if there is a >= 1 cm displacement. When compared to XR, CT could provide more valuable information regarding any fracture of the surgical neck or the tuberosities, fragments displacement (especially in the posterior compartment for comminuted fractures), any involvement of the articular surface (e.g. Hill-Sachs lesion and inverse Hill-Sachs), inveterate luxation and fractures of the anterior glenoid labrum (e.g. Bankart lesion and inverse Bankart). CT spiral 3D reconstructions can be useful in preoperative planning. MRI could evaluate the rotator’s cuff and its ligaments, including the glenoid labrum and shoulder soft tissues (9). However, most 3- or 4-parts comminuted fractures are evaluated at best only intraoperatively.
First, we divided proximal humeral fracture cases admitted in the ER in minimally displaced and displaced fractures, using XR and CT and the Neer Classification (figure 5). Also Hertel et al. stated that the most relevant predictors factors for ischemia in intracapsular fractures treated with osteosynthesis are: the calcar length, the medial hinge integrity and some specific fracture types (10). The periosteal posteromedial hinge evaluation was not always possible using standard XR or CT images. We evaluated it indirectly by measuring the cervico-diaphyseal angle that has been described as a second-level prognostic factor by Hertel: this is a good index of periosteal integrity if increased (e.g. increased valgus) as demonstrated by Solberg et al. and Hardeman et al. (Figure 6) (8)(11). Similarly, preoperative assessment of any articular surface fracture and/or a second head fracture line are equally important (12)(13). Bone quality estimation is indispensable for internal fixation: in XR images, osteoporosis is identified as hypodense areas in the humeral head, tuberosity comminution and a poor diaphyseal cortex-medullary index (14).
Figure 5.

4-parts proximal epiphyseal fracture: preoperative XR (left) and CT images (right).
Figure 6.

the cervico-diaphyseal angle
Not reducible luxation, humeral head comminution on the frontal plane and patients unfitted for operative treatment have been excluded from our study. We included 3- and 4-parts fractures patients with a cervico-diaphyseal angle (valgus impaction) compatible with an intact posteromedial periosteum. The medial hinge has been evaluated in relation to the cervico-diaphyseal angle during preoperative imaging analysis and was an exclusion criteria if considered not sufficiently intact (e.g. head varus impactation >10°).
The operative treatment chosen was minimally invasive plate osteosynthesis for a total of 42 fractures analyzed (table 1): 16 GmbH plates (DePuy Synthes®, Solothurn, Switzerland and 26 PHILOS plats (DePuy Synthes®, Solothurn, Switzerland) (figure 8). Patients have been divided by self-identified gender (17 males and 25 female) and by fracture type (20 4-part fractures and 22 3-parts fractures). The mean age was 84 years (75-94), the dominant side is the right one, involved in 80% of cases.
Figure 8.

4-parts proximal epiphyseal fracture: preoperative XR (left) and CT images (right).
Clinical and radiographic follow-ups have been planned at 3, 6 and 12 months after surgery with a median follow-up time of 9 months (figure 9). The DASH (Disabilities of the Arm, Shoulder and Hand) Score and Constant Score were used for patients’ outcome evaluation.
Figure 9.

1-year follow-up postoperative x-rays
Surgical technique
The surgical target was to create minimal surgical exposure and tissue damage rather than achieving an optimal anatomic reduction while preserving the local tissue biological environment for an early mobilization of the affected arm.
Sufficient space for the image intensifier and for the mobility of the affected upper limb in all planes must be planned during patient positioning. All patients have been placed in a beach-chair position (30°-60°) under general anesthesia and interscalenic nerve block.
We performed a trans-deltoid approach in all patients; an incision was made at the III anterolateral portion of the deltoid muscle as we identified the deltoid raphe between the anterior and middle third of the deltoid (figure 7). Once the anterolateral acromial border was identified, we split the muscle to reach the articular surface. A second distal incision was made around 4 cm down the first one to preserve the axillary nerve, previously identified below the deltoid. Also, to avoid any subcutaneous adherences, incisions are made away from the axillary region. The benefits of this surgical technique are: reducing surgical exposure and infectious risk and protecting the periosteum around the fracture site to reduce bio-local damage and increase aesthetic satisfaction (15)(16). First the head is reduced: the fundamental step is to align the head; then we proceeded with fracture fixation. The fundamental step is to align the head to the shaft. Surgical wound closure should be as linear as possible to reduce poorly aesthetical scars as in “S” shaped incisions. Once identified, the Cephalic vein should be displaced medially or laterally or immediately plugged. A better surgical exposure is achieved by making a 1 cm incision in the fibrous zone of the anterior V of the deltoid about 1 cm from its insertion, having care of suturing it back after fixation.
Figure 7.

The trans-deltoid approach
Surgical instruments used in mini-invasive percutaneous LCP procedure include soft tissue retractors of variable sizes, bending pliers, bending irons and various others.
For impacted fractures: if the medial wall is intact, reduction can be achieved by simply placing instrument(s) among the trochanters and pushing the head superolateral border upwards. The medial periosteum acts as a barrier for head medial displacement. The humeral head valgus angulation is considered satisfying only once anatomic reduction is obtained. For not-impacted fractures: any loss of integrity of the medial periosteum causes humeral head instability and lateral dislocation; placing an instrument on the medial wall is needed to preserve it and prevent head medial dislocation and valgus angulation (17)(18). Post-operative care included temporary immobilization with braces and immediate active assisted shoulder exercises if pain allowed. Most patients started standard active and resistive mobilization at 6-weeks follow-ups.
Results
At follow-ups patients showed a high satisfaction regarding their quality of life. When measuring patients’ outcome the DASH recorded mean value was 72, while the Constant mean score was 68. The highest scores were recorded in patients with 3-parts fractures (graph 2). Intraoperatively 2 patients have been shifted to an open reduction external fixation (ORIF) procedure; for 1 patient we decided to perform an arthroplasty due to reduction failure; for 12 patients we used bone grafts and for 21 patients screws were adopted to fixate the greater tuberosity (graph 3). Complications have been recorded in 10 out of 42 patients (23,8%): among those (graph 4): 1 avascolar necrosis; 4 varus displacement cases with loss of stability with greater trochanter displacement (varus collapse); 3 cases of screws piercing the articular joint; 2 impingement cases due to plate position. No infections nor axillary nerve palsy were documented. Proximal humeral 4-parts fractures have registered the highest number of complications (graph 5). Surgical treatment evaluation is in line with similar results published in the literature for studies with a younger mean age. Shoulder joint mobility was recorded showing the following mean values: anterior elevation 75°, lateral elevation 80°, abduction 90°, intra-rotation 50°, extra-rotation 25°, with a decent degree of satisfaction in >80% of patients. We could not analyze work-related satisfaction as most patients were unemployed or retired. The outcome has been influenced by: >8mm calcar fragment, head valgus impaction and periosteal medial hinge preservation. fracture comminution did not influence the outcome. Four-parts fractures with an intact medial hinge and a perioperative >8mm calcar fragment have shown better results when compared to 3-parts fractures (graph 6). The preservation of the calcar and the medial hinge have positively influenced the outcome by giving physical support on the medial side and increasing the bone-plate stability. The 2 groups complication mean values have been statistically compared at follow-up, showing significant results. Also, we subdivided patients in 2 groups based on calcar integrity and its length, excluding any comminution (graph 7). Group I (n=15, 8 3-parts and 5 4-parts fractures) had a >8mm calcar fragment: n=15 (8 3-parts and 5 4-parts fractures). Group II had a <8mm calcar fragment (n=22: 7 3-parts and 13 4-parts fractures). 4-parts fractures with a calcar fragment less than 8 mm had the worst outcome overall.
Graph 2:

Outcome DASH and Constant scores for 3- and 4-parts fractures.
Graph 3:

Intraoperative modifications
Graph 4:

Complication recorded (%)
Graph 5:
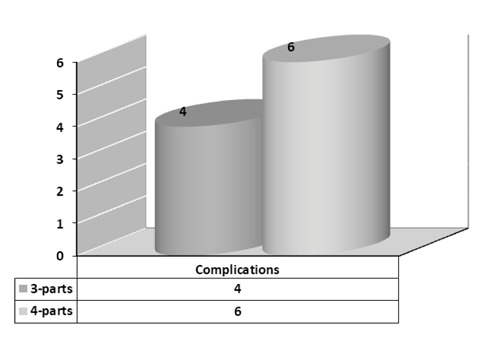
Complications recorded (n) in 3- and 4-parts fractures
Graph 6:

Complications in patients with a <8 mm and > 8 mm calcar fragments (n)
Graph 7:

Outcome comparison of 3- and 4-parts fractures
Discussion
Three and four parts proximal humerus fractures treatment is a high debated topic (techniques (19). Numerous studies have been published in the literature but no guidelines have been universally validated yet. Each clinical case stands on its own, especially regarding elderly people with plenty of comorbidities that impact healing. Fracture treatment management is influenced by patients’ global health status and their functional demand. Bone quality, rotator’s cuff integrity and local vascularization also guide treatment. We identified both local and general clinical issues. Quite often orthopedics must opt for a nonoperative treatment out of necessity due to co-morbidities trying to achieve the best trade-off between benefits and risks. Recently MIPO has been found a valid alternative (20). A meta-analysis by Li et al. comparing ORIF and MIPO outcomes for proximal humeral fractures in 1060 patients with lower mean age compared to our study; MIPO was found superior to ORIF when comparing postoperative pain total operative time, quantity of blood loss, union time, and Constant scores (21). The MIPO minimal incision and preservation of the local bone and soft tissue (i.e. the deltoid muscle) environment lead to a rapid ROM recovery (22). Early rehabilitation is fundamental for measuring patient’s outcome and is directly related to the fracture pattern: the integrity and reduction of the greater and the lesser tubercles are important factors for shoulder’s stability (23). Due to limited tissue exposure, MIPO has a lower incidence in avascular necrosis and infection and increase recovery time and early motion, when compared to ORFI using a deltopectoral approach (24). External fixators could be a valid alternative for elderly patients with osteoporosis and comorbidities as it is a mini-invasive surgery preserving soft tissues (25). Local bone issues are osteoporosis and the local humeral head bone stock that can reduce the stability of the bone-plate system Barlow et al. described the use of elastic Kirschner wires in distraction/compression to obtain optimal results (26). Those studies focus on the medial wall integrity rather than on fracture comminution as highlighted by Solberg et al. (8): this study analyzes osteosynthesis complications for fractures with a valgus/varus angulation fractures and 2 other radiographical factors that negatively influenced the outcome: humeral head angulation direction and the calcar length; the best results were recorded in the group where the calcar was at least >2mm intact, independently from the Neer classification. Similarly, Gardner et al. highlight the importance of the medial wall integrity to achieve a good prognosis in plate osteosynthesis (27). XR detected calcar comminution has been found as a negative prognostic factor by Osterhoff et al. (28).
In addition, the number of drilled holes in the humeral head has been considered a negative prognostic factor. A study by Konrad et al. with 187 patients treated with plate osteosynthesis has pointed out how all 25 complications recorded were caused by iatrogenic factors (e.g. screws piercing into the articular joint or unjustified multiple screws perforations) (29). Those data display the link between good surgical results and the surgeon’s experience. Similarly, a retrospective study by Touloupakis et al. using PHILOS plates shows how MIPO can be a valid alternative for intramedullary nailing having similar infection, nonunion and nerve injury rates (30). The Axillary, Musculocutaneous and Radial nerve can be damaged during MIPO with some authors highlighting a lower incidence of iatrogenic radial nerve injury when comparing MIPO to other surgical techniques (19)(21)(30). If the incision is prolonged distally, the radial nerve can be protected if the arm is placed in 90° abduction and the forearm in full supination (31). The axillary could be protected by limiting the incision 5 cm distal to the tip of the acromion and protected using the index finger when placing the plaque (32)(33). Compared to ORIF, MIPO has a longer radiation time (21). Osteosynthesis is superior for functional outcome in 3- and 4-parts displaced proximal humeral fractures in the aged population compared to non-operative treatment. This has been presented by two randomized studies by Olerud and Zito recording follow-ups data at 2 and 5 years showing increased quality of life in surgically treated patients (34). A study by Kim et al. has proven the benefit of autologous bone graft (taken from the contralateral iliac wing) associated with LCP for giving mechanical support and biological stimuli for four-parts fractures healing (35). Our experience demonstrates how minimally invasive osteosynthesis is positively correlated to anatomic reduction and fixation stability, leading to an optimal functional outcome to give back independence to patients, as demonstrated by Constant scores. We recorded around 5% of osteonecrosis cases, in line with literature results (20). Regarding complex proximal humeral fractures we strongly suggest MIPO, if there are no indications for arthroplasty (e.g. comminution of the articular surface, not-reducible tuberosities, etc.), to achieve a better outcome and quality of life and a lowering of healthcare costs and surgical risks, even in borderline patients with a compromised clinical picture and limited management options.
Conclusions
Management of 3- and 4-parts proximal humeral fractures in the elderly is still not clear. Due to the increase in longevity, we want to push the debate towards establishing guidelines similar to what has been done for neck femoral fractures.
The focus of treatment management must be the patient instead of the fracture itself by including patients’ comorbidities and functional demand evaluation. Prior a meticulous preoperative planning evaluation, an acceptable compromise is opting for a mini-vasive operative treatment with MIPO plates in order to secure a satisfying clinical outcome and functional demand while lowering local and global health risks. Postoperative results are rewarding for fractures with an intact calcar and medial hinge, independently from fracture comminution. Orthopedics can expect to successfully treat proximal humeral fractures in the elderly population using ORIF and bone grafts.
Abbreviations:
- MIPO:
minimally invasive plate osteosynthesis
- LCP:
locking compression plate
- HAS:
humeral head-shaft angulation
- HHH:
height of the humeral head
- ROM:
range of motion
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Maier D, Jäger M, Strohm PC. Südkamp NP. Treatment of proximal humeral fractures - a review of current concepts enlightened by basic principles. Acta Chir Orthop Traumatol Cech. 2012;79(4):307–16. Review. PubMed PMID: 22980928. [PubMed] [Google Scholar]
- Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006 Jan;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. PubMed PMID: 16394745. [DOI] [PubMed] [Google Scholar]
- Cornell CN, Ayalon O. Evidence for success with locking plates for fragility fractures. HSS J. 2011 Jul;7(2):164–9. doi: 10.1007/s11420-010-9194-8. doi: 10.1007/s11420-010-9194-8. Epub 2011 Feb 1. PubMed PMID: 22754418; PubMed Central PMCID: PMC3145849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neer CS., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. Sep 1970;52(6):1077–89. [PubMed] [Google Scholar]
- Burkhart KJ, Dietz SO, Bastian L, Thelen U, Hoffmann R, Müller LP. The treatment of proximal humeral fracture in adults. Dtsch Arztebl Int. 2013 Sep;110(35-36):591–7. doi: 10.3238/arztebl.2013.0591. doi: 10.3238/arztebl.2013.0591. Epub 2013 Sep 2. Review. PubMed PMID: 24078839; PubMed Central PMCID: PMC3785018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003 Nov;34(Suppl 2):B63–76. doi: 10.1016/j.injury.2003.09.026. Review. PubMed PMID: 14580987. [DOI] [PubMed] [Google Scholar]
- Bai L, Fu ZG, Wang TB, Chen JH, Zhang PX, Zhang DY, Jiang BG. Radiological evaluation of reduction loss in unstable proximal humeral fractures treated with locking plates. Orthop Traumatol Surg Res. 2014 May;100(3):271–4. doi: 10.1016/j.otsr.2013.12.024. doi: 10.1016/j.otsr.2013.12.024. Epub 2014 Apr 4. PubMed PMID: 24709305. [DOI] [PubMed] [Google Scholar]
- Solberg BD, Moon CN, Franco DP. Paiement GD. Locked plating of 3-and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009 Feb;23(2):113–9. doi: 10.1097/BOT.0b013e31819344bf. doi: 10.1097/BOT.0b013e31819344bf. PubMed PMID: 19169103. [DOI] [PubMed] [Google Scholar]
- Kilcoyne RF, Shuman WP, Matsen FA 3rd, Morris M. Rockwood CA. The Neer classification of displaced proximal humeral fractures: spectrum of findings on plain radiographs and CT scans. AJR Am J Roentgenol. 1990 May;154(5):1029–33. doi: 10.2214/ajr.154.5.2108538. PubMed PMID: 2108538. [DOI] [PubMed] [Google Scholar]
- Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004 Jul-Aug;13(4):427–33. doi: 10.1016/j.jse.2004.01.034. PubMed PMID: 15220884. [DOI] [PubMed] [Google Scholar]
- Hardeman F, Bollars P, Donnelly M, Bellemans J, Nijs S. Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury. 2012 Feb;43(2):153–8. doi: 10.1016/j.injury.2011.04.003. doi: 10.1016/j.injury.2011.04.003. Epub 2011 May 12. PubMed PMID: 21570073. [DOI] [PubMed] [Google Scholar]
- Resch H, Hubner C, Schwaiger R. Minimally invasive reduction and osteosynthesis of articular fractures of the humeral head. Injury. 2001;32(Suppl. 1):SA25–32. doi: 10.1016/s0020-1383(01)00058-4. [DOI] [PubMed] [Google Scholar]
- Hertel R. Fractures of the proximal humerus in osteoporotic bone. Osteoporos Int. 2005;16(Suppl. 2):S65–72. doi: 10.1007/s00198-004-1714-2. [DOI] [PubMed] [Google Scholar]
- Tingart MJ, Apreleva M, von Stechow D, Zurakowski D, Warner JJ. The cortical thickness of the proximal humeral diaphysis predicts bone mineral density of the proximal humerus. J Bone Joint Surg Br. 2003;85(4):611–7. doi: 10.1302/0301-620x.85b4.12843. [DOI] [PubMed] [Google Scholar]
- Hepp P, Theopold J, Voigt C, Engel T, Josten C, Lill H. The surgical approach for locking plate osteosynthesis of displaced proximal humeral fractures influences the functional outcome. J Shoulder Elbow Surg. 2008 Jan-Feb;17(1):21–8. doi: 10.1016/j.jse.2007.03.029. Epub 2007 Nov 1. PubMed PMID: 17936024. [DOI] [PubMed] [Google Scholar]
- Lill H, Hepp P, Rose T, Ko¨nig K, Josten C. The angle stable lockingproximal-humerus-plate (LPHP) for proximal humeral fractures using a small anterior-lateral-deltoid-splitting-approach - technique and first results. Zentralbl Chir. 2004;129:43–8. doi: 10.1055/s-2004-44870. [DOI] [PubMed] [Google Scholar]
- Gregory TM, Vandenbussche E, Augereau B. Surgical treatment of three and four-part proximal humeral fractures. Orthop Traumatol Surg Res. 2013 Feb;99(1 Suppl):S197–207. doi: 10.1016/j.otsr.2012.12.006. doi: 10.1016/j.otsr.2012.12.006. Epub 2013 Jan 16. Review. PubMed PMID: 23333125. [DOI] [PubMed] [Google Scholar]
- Robinson CM, Page RS. Severely impacted valgus proximal humeral fractur es. Results of operative treatment. J Bone Joint Surg. 2003;85-A:1647–55. doi: 10.2106/00004623-200309000-00001. [DOI] [PubMed] [Google Scholar]
- Tetsworth K, et al. Minimally invasive plate osteosynthesis of humeral shaft fractures: current state of the art. J Am Acad Orthop Surg. 2018;26:652–661. doi: 10.5435/JAAOS-D-17-00238. [DOI] [PubMed] [Google Scholar]
- Frima H, Michelitsch C, Beks RB, Houwert RM, Acklin YP, Sommer C. Long-term follow-up after MIPO Philos plating for proximal humerus fractures. Arch Orthop Trauma Surg. 2019;139(2):203–209. doi: 10.1007/s00402-018-3063-1. doi: 10.1007/s00402-018-3063-1. [DOI] [PubMed] [Google Scholar]
- Li F, Liu X, Wang F, et al. Comparison between minimally invasive plate osteosynthesis and open reduction-internal fixation for proximal humeral fractures: a meta-analysis based on 1050 individuals. BMC Musculoskelet Disord. 2019;20(1):550. doi: 10.1186/s12891-019-2936-y. Published 2019 Nov 18. doi: 10.1186/s12891-019-2936-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao L, Yang P, Zhu L. Chen AM. Minimal invasive percutaneous plate osteosynthesis (MIPPO) through deltoid-pectoralis approach for the treatment of elderly proximal humeral fractures. BMC Musculoskelet Disord. 2017;18:187. doi: 10.1186/s12891-017-1538-9. doi: 10.1186/s12891-017-1538-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caforio M, Maniscalco P. The importance of early rehabilitation in proximal humeral fracture: A clinical trial of efficacy and safety of a new endomedullary nail. J Back Musculoskelet Rehabil. 2017;30(2):195–202. doi: 10.3233/BMR-160732. doi: 10.3233/BMR-160732. [DOI] [PubMed] [Google Scholar]
- Alberio RL, Del Re M. Grassi FA. Minimally Invasive Plate Osteosynthesis for Proximal Humerus Fractures: A Retrospective Study Describing Principles and Advantages of the Technique. Adv Orthop. 2018;2018:5904028. doi: 10.1155/2018/5904028. Published 2018 Jun 3. doi: 10.1155/2018/5904028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicenti G, Antonella A, Filipponi M, et al. A comparative retrospective study of locking plate fixation versus a dedicated external fixator of 3-and 4-part proximal humerus fractures: Results after 5 years. Injury. 2019;50(Suppl 2):S80–S88. doi: 10.1016/j.injury.2019.01.051. doi: 10.1016/j.injury.2019.01.051. [DOI] [PubMed] [Google Scholar]
- Barlow JD, Sanchez-Sotelo J, Torchia M. Proximal humerus fractures in the elderly can be reliably fixed with a “hybrid” locked-plating technique. Clin Orthop Relat Res. 2011 Dec;469(12):3281–91. doi: 10.1007/s11999-011-1894-y. doi: 10.1007/s11999-011-1894-y. PubMed PMID: 21479762; PubMed Central PMCID: PMC3210261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner MJ, Lorich DG, Werner CM. Helfet DL. Second-generation concepts for locked plating of proximal humerus fractures. Am J Orthop (Belle Mead NJ) 2007 Sep;36(9):460–5. PubMed PMID: 17948148. [PubMed] [Google Scholar]
- Osterhoff G, Hoch A, Wanner GA, Simmen HP, Werner CM. Calcar comminution as prognostic factor of clinical outcome after locking plate fixation of proximal humeral fractures. Injury. 2012 Oct;43(10):1651–6. doi: 10.1016/j.injury.2012.04.015. doi: 10.1016/j.injury.2012.04.015. Epub 2012 May 12. PubMed PMID: 22579397. [DOI] [PubMed] [Google Scholar]
- Konrad G, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, Luo C, Plecko M, Wendt K, Köstler W, Südkamp N. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J Bone Joint Surg Am. 2010 Mar;92(Suppl 1 Pt 1):85–95. doi: 10.2106/JBJS.I.01462. doi: 10.2106/JBJS.I.01462. PubMed PMID: 20194347. [DOI] [PubMed] [Google Scholar]
- Touloupakis G, Di Giorgio L, Bibiano L, et al. Exploring the difficulties to improve minimally invasive application with long PHILOS plate in multifocal metadiaphyseal fractures of the proximal humerus: analysis of intraoperative procedure and clinical outcomes. Acta Biomed. 2019;89(4):532–539. doi: 10.23750/abm.v89i4.6212. Published 2019 Jan 15. doi: 10.23750/abm.v89i4.6212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005 Apr;36(4):530–8. doi: 10.1016/j.injury.2004.05.036. [DOI] [PubMed] [Google Scholar]
- Ruchholtz S, Hauk C, Lewan U, Franz D, Kühne C, Zettl R. Minimally invasive polyaxial locking plate fixation of proximal humeral fractures: a prospective study. J Trauma. 2011;71:1737–1744. doi: 10.1097/TA.0b013e31823f62e4. [DOI] [PubMed] [Google Scholar]
- Laflamme GY, Rouleau DM, Berry GK, Beaumont PH, Reindl R, Harvey EJ. Percutaneous humeral plating of fractures of the proximal humerus: results of a prospective multicenter clinical trial. J Orthop Trauma. 2008;22:153–158. doi: 10.1097/BOT.0b013e3181694f7d. doi: 10.1097/BOT.0b013e3181694f7d. [DOI] [PubMed] [Google Scholar]
- Olerud P, Ahrengart L, Söderqvist A, Saving J, Tidermark J. Quality of life and functional outcome after a 2-part proximal humeral fracture: a prospective cohort study on 50 patients treated with a locking plate. J Shoulder Elbow Surg. 2010 Sep;19(6):814–22. doi: 10.1016/j.jse.2009.11.046. doi: 10.1016/j.jse.2009.11.046. Epub 2010 Mar 19. PubMed PMID: 20303288. [DOI] [PubMed] [Google Scholar]
- Kim SH, Lee YH, Chung SW, Shin SH, Jang WY, Gong HS, Baek GH. Outcomes for four-part proximal humerus fractures treated with a locking compression plate and an autologous iliac bone impaction graft. Injury. 2012 Oct;43(10):1724–31. doi: 10.1016/j.injury.2012.06.029. doi: 10.1016/j.injury.2012.06.029. Epub 2012 Jul 20. PubMed PMID: 22819250. [DOI] [PubMed] [Google Scholar]


