Abstract
Objective:
To evaluate how the SARS-COV2 is able to affect the nervous system, the main neurological manifestation, and the treatment used, including neurorehabilitation.
Methods:
Studies performed during the current year that fulfilled inclusion criteria were selected from PubMed, Scopus, Cochrane, and Web of Sciences databases. The search combined the terms “Covid 19,” “rehabilitation/treatment,” and “neurological complications.”
Results:
The exact route by which SARS-CoV-2 can penetrate the CNS is still unknown, although a possible retrograde transynaptic pathway from peripheral nerve endings, and/or through the olfactory bulb, have been suggested. An early management of COVID-19 by a multiprofessional team is fundamental to avoid long term sequaele. Rehabilitation is recommended to improve respiratory and cardiac function, as well as to avoid long term neurological complications.
Conclusions:
As no specific conclusions in term of prognosis and treatment could be done, research and consensus paper are needed to provide NeuroCovid patients with the best treatment options, including neurorehabilitation. (www.actabiomedica.it)
Keywords: COVID-19, neurocovid, pandemic, neurological complications
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), originating from Wuhan, is spreading around the world and the outbreak continues to escalate since December 2019. On 30 January 2020, COVID-19 was registered as the sixth Public Health Emergency of International Concern (PHEIC) by the World Health Organization (WHO), which was socially declared as a pandemic on 11 March 2020( 1-3). At the end of January 2020, the infection spread all over Italy, but with high infection rates and mortality in the northern part, especially in Lombardy, the most industrialized and polluted region of the country. It is noteworthy that an association between severe viral respiratory disease and air pollution has been described (4).
SARS-CoV-2 is a beta-coronavirus with an average incubation period of 3-7 days (with a maximum of 14 days). COVID-19 is highly contagious with a wide spectrum of clinical manifestations, typically involving the respiratory system (5-7), although many patients can be totally asymptomatic. Several risk factors are associated with the complications of COVID-19, and these include older age (>65), chronic respiratory diseases, cardiovascular diseases, hypertension, diabetes, and obesity. So far, males are registered to be infected with a higher prevalence compared to females and the reason is yet undiscovered (8, 9).
SARS-CoV-2 is transmitted either via airborne small droplets (aerosols) that disperse one or two metres when speaking or coughing, or direct contact with infected nasal secretions, or by fomites (contaminated objects) (10). It has been suggested that SARS-CoV-2 binds by glycoproteins expressed on its surface to the receptor of the angiotensin-converting enzyme 2 (hACE2) (11), which is distributed in the respiratory tract epithelium, lung parenchyma and other areas, such as the gastrointestinal tract, endothelial cells, among others (12). In addition to ACE2 receptor, SARS-CoV-2 uses the serine protease type II transmembrane serine protease for spike protein priming (13,14). Then, patients with COVID-19 present symptoms that include fever, shortness of breath, cough, sore throat, nasal congestion, dizziness, chills, muscle ache, arthralgia, weakness, fatigue or myalgia, chest tightness, excessive mucus production with expectoration, hemoptysis, and dyspnea (15-21). Severe or fatal complications include pneumonia, type I respiratory failure, sepsis, metabolic acidosis, septic shock, arrhythmia, acute cardiac injury, heart failure, acute kidney injury, bleeding, or hypoxic encephalopathy (22-25).
Growing evidence is demonstrating the involvement, both directly and indirectly, of the nervous system by the SARS-COV-2.
Aim of this review is to evaluate how the SARS-COV2 is able to affect the nervous system, the main neurological manifestation, and the treatment used, including neurorehabilitation.
Search Strategy
Studies were identified by an online search of Scopus, PubMed, Web of Science, and Cochrane databases. The search combined the following terms: ‘‘CoVID19’’[MeSH Terms] OR ‘‘neurological’’[All Fields] AND ‘‘complications’’[All Fields] OR ‘‘neurological complications’’ [All Fields] AND ‘‘COVID-19 neurorehabilitation’’ [MeSH Terms] AND/OR ‘‘pathogenesis’’ [All Fields] AND ‘‘rehabilitation’’ [All Fields] OR‘‘COVID19 pathogenesis and treatment ’’ [All Fields]. Studies met specified selection criteria and were published in the current year (January-November 2020). We selected only texts in English and removed duplicates. All articles were evaluated according to the title, abstract, and text. We included studies that examined pathogenesis and treatment, including rehabilitation in patients with Neurocovid. A total of. . . articles were eventually selected for inclusion (see Figure 1) and the main findings on clinical manifestation reported and table 1.
Figure 1.
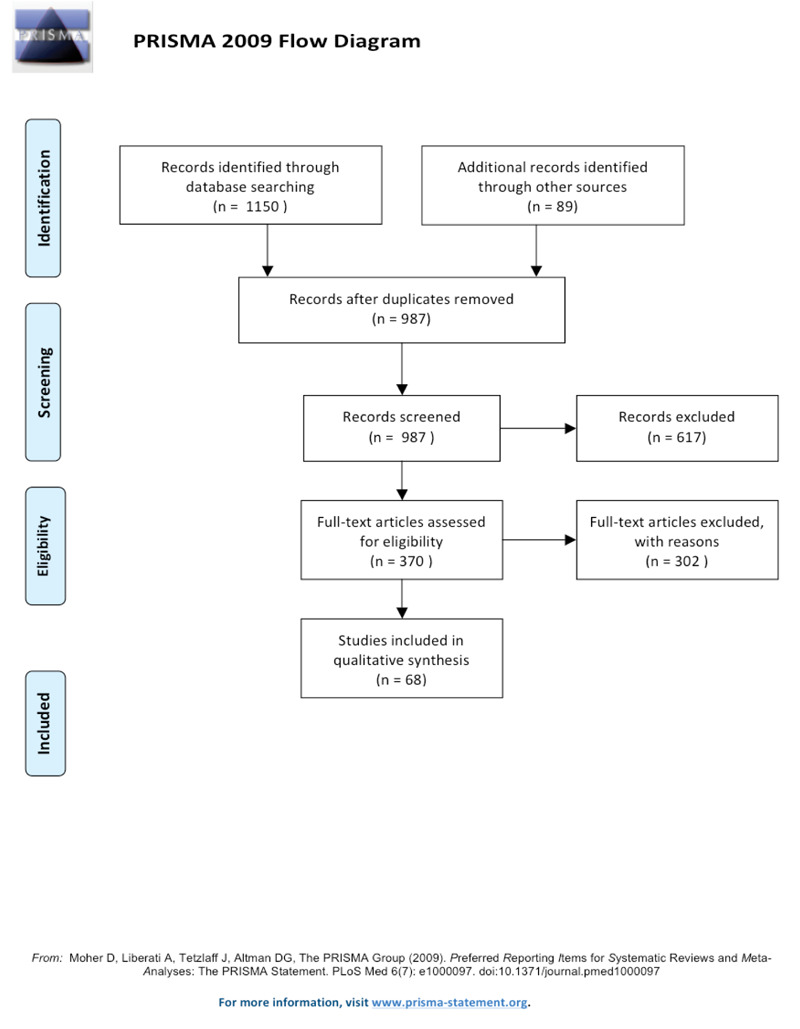
Shows the flow diagram of the study selection.
Table 1.
COVID-19–related complications in the nervous system
| Complication | Clinical manifestations | Auxiliary examination | Physio-pathogenesis | References |
| Viral meningitis/encephalitis | Headache Altered mental status, meningeal irritation signs |
CSF: positive PCR assay for SARS-CoV-2 Increased lymphocytes and proteins MRI: FLAIR hyperintensity EEG: slowing |
unclear may be edema secondary to inflammatory injury versus direct viral infection |
75 80-86 |
|
Acute disseminated
encephalomyelitis (ADEM) |
Multifocal deficits | MRI: FLAIR hyperintensity, multifocal demyelinating lesions Autopsy: ADEM-like appearance in the subcortical white matter |
clusters of macrophages, axonal injury | 87-89 |
|
Acute necrotizing encephalopathy
(ANE) |
Altered mental status | CT: hypoattenuation MRI: T2 FLAIR hyperintensity with internal hemorrhage |
cytokine release syndrome | 90-91 |
| Cerebrovascular disease | Sensory or motor dysfunction | CT/MRI: ischemic or hemorrhagic change | Increased blood pressure thrombocytopenia coagulation disorders cytokine release syndrome hypoxia |
38-39 47-49 52-56; 67-79 |
| Epilepsy | Seizures | CSF: negative PCR assay for SARS-CoV-2 EEG: semirhythmic, irregular, high-amplitude delta waves |
unknown | 95-96 |
| Acute myelitis | Flaccid paralysis, hypesthesia Urinary and bowel dysfunction |
MRI: T2 hyperintensity | unclear | 97-98 |
| Hyposmia and hypogeusia | Loss of a sense of smell and taste | Questionnaire-based survey Cross-sectional study |
transneural penetration through the olfactory bulb, or the penetration through the angiotensin converting enzyme 2 receptor, widely expressed on the epithelial cells of the mucosa of the oral cavity. | 57-61 |
| Guillain-Barré syndrome (GBS) | Flaccid paralysis | CSF: negative PCR assay for SARS-CoV-2 MRI: enhancement of affected nerve roots EMG: decreased recruitment |
Cytokine storm hyperinflammation | 50-51 99-105 |
| Miller Fisher syndrome (MSF) and polyneuritis cranialis | Ophthalmoplegia, ataxia, and areflexia | MRI: relative enlargement, T2 hyperintensity, and enhancement of the affected CN Anti-GD1b antibody positive |
Cytokine storm hyperinflammation | 106-109 |
| Cognitive dysfunction | Memory and executive Function deficits | No information | direct viral involvement of the CNS effect of hypoxemia. |
110-111 |
| Psychiatric dysfunction | depression, fear and anger post-traumatic stress disorder delirium |
No information | prolonged ventilation, use of sedatives, prone positioning, human isolation extended time away from social contacts |
114-115 |
| Other complications have been descrbed secondary to COVID treatment |
neurocognitive impairment neuropathic neuropsychiatric sequelae, retinopathy
ataxia, seizures, limbic encephalitis |
No information | Combined drugs effect | 116-125 |
COVID-19, coronavirus disease; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; CSF, cerebrospinal fluid; CT, computed tomography; MRI, magnetic resonance imaging; PCR, polymerase chain reaction; EEG, electroencephalography; EMG, electromyography.
Pathogenesis and neurovirulence properties of SARS-CoV-2
Coronaviruses belong to the family Coronaviridae which consists of four genera: alpha-, beta-, delta- and gamma-coronavirus (26). Human coronaviruses 229E, OC43, NL63 and HKU1 are endemic worldwide, and are responsible for 15-30% of upper respiratory tract infections, oto-rhinitis, laryngitis and pharyngitis. Sometimes, they can cause more serious infections, such as bronchitis, bronchiolitis, exacerbation of asthma or SARS.
Respiratory viruses can penetrate the central nervous system (CNS) (neuroinvasion), affect both neurons and glial cells (a property known as neurotropism), and induce various neurological pathologies (neurovirulence) (27). The exact route by which SARS-CoV-2 can penetrate the CNS is still unknown (26). Li et al. suggest a possible retrograde transynaptic pathway from peripheral nerve endings, through the mechanoreceptors and chemoreceptors located in the lungs and respiratory tract that transmitted to the nucleus of the solitary tract. On the other hand, SARS-CoV infection has shown to cause neuronal death in ACE2 transgenic mice (28), entering the CNS through the olfactory bulb, and spreading transneuronally to other regions of the brain. Indeed, it has been demonstrated that the human coronaviruses OC43 is neuroinvasive spreading from the olfactory bulb to the brain stem and spinal cord, by the axonal transport system as a means of neuron-to-neuron propagation (27), causing flaccid paralysis and demyelination in animal models (29-32). Regulation of the ACE2-R is another valid route to facilitate cell invasion by SARSCoV-2 and its rapid replication (28). Indeed, the high expression of ACE2-R on the endothelial cells of the blood-brain barrier allows a rapid viral binding and facilitates viral entry into the CNS by damaging vasculature (33-35). When invading the cerebral vascular endothelium, the virus reduces the functionality of the ACE2-R causing an elevation of cerebral blood pressure and, as a consequence, blood vessel rupture leading to massive intracerebral bleeding (36), although thromboembolic events may worsen the clinical picture. This could be the reason why patients taking ACE inhibitors as well as those with comorbidity, especially hypertension and diabetes, are exposed to a major risk of COVID-19 infectious and complications (37).
Another mechanism of damage is the generation of a global systemic inflammatory response (SIRS), producing increased levels of interleukin (IL)-6, IL-12, IL-15, and tumor necrosis factor alpha (TNF-α). This activates glial cells and produces a massive pro-inflammatory CNS state, leading to severe hypoxia and, consequently, cerebral vasodilation, cerebral edema and ischemia (38, 39).
What is more, the virus has been found in the brain stem (26,40), involving the nuclei that regulate the respiratory rhythm. In details, the chemoreceptors that detect changes in the concentrations of CO2 and O2 send the information through the nucleus of the solitary fascicle to the central regulation of breathing. Changes in these mechanisms lead to an increase or decrease in respiratory strength (41,42). In this way, stem nuclei have connections with the respiratory system, and the entry of the coronavirus into this structure could lead to death also by affecting these neuronal groups (42).
On the other hand, the virus could directly damage CNS causing viral encephalitis and/or immune-mediated diseases (43). Finally, it could not be excluded that, the SARS-CoV-2 could be latent in the CNS for a long time and might lately reappear with neurological diseases, as demonstrated for other coronaviruses (i.e. HCoV-229E and HCoV-OC43) that have been detected after a long period in various neurological diseases in humans, including multiple sclerosis (MS) (31).
Clinical manifestation of Neurocovid
The incidence of neurological complications from SARS-CoV-2 is unknown. Necropsy studies have shown the presence of cerebral oedema and neuronal degeneration in deceased patients with COVID-19 (44), suggesting an encephalopathy (45), likely due to toxic and metabolic causes and the effect of hypoxia or drugs or subclinical crises. In a first report, 86 (36.4%) out of 214 hospitalized patients with severe infection in three hospitals of Wuhan reported neurological manifestation (46). Since then, there has been growing evidence on the fact that the virus may cause numerous neurological manifestations, such as encephalopathy (47), limbic and brainstem encephalitis (48, 49), Guillain-Barrè syndrome (50-51) and stroke (52-56). These manifestations may reflect either direct viral infection or dysregulation of the immune response, potentially leading to hyper-inflammation processes and dysfunction of the coagulation system.
Early neurological symptoms of COVID19 infection
Headache is the first most common symptom described in people with COVID-19. In a study of more than 1,000 patients, 13.6% reported mild headaches (15% of those with severe disease), 15% of patients reported myalgia, 13.7% had elevated levels of creatine kinase (19% in severe cases), with two cases of rhabdomyolysis (0.2%)(57).
Olfactory and taste disorders can be the initial neurological symptoms described in such patients. Nevertheless, these patients are classified as asymptomatic or pauci-symptomatic compared to patients with severe respiratory symptoms that, usually, did not report hypogeusia and hyposmia. The underlying pathogenetic mechanism that could explain the taste and olfactory disorders in SARS-CoV-2 infection are either a transneural penetration through the olfactory bulb (28), or the penetration through the ACE-R (58). Then, hyposmia and hypogeusia are considered as a possible early stage of the disease (59), and could represent a clinical screening tool to further orientate testing of pauci-symptomatic individuals (60). The prevalence of olfactory disorders in an Italian survey was described as 20% (61).
Patients with a more severe COVID-19 symptomatology are likely to have other neurologic symptoms, such as acute cerebrovascular diseases, impaired consciousness, and skeletal muscle injury.
Acute neurological complications associated to COVID19 Cerebrovascular diseases
Li et al., in a sample of 221 patients, found that 6% developed severe neurological diseases, such as ischaemic and haemorrhagic stroke, as well as cerebral vein thrombosis, with a significant proportion died as a result (62). Males are at a higher risk for stroke (62 %), with a median age of stroke onset of 63 years. Notably, a large amount of the cases present important vascular risk factors, especially hypertension and diabetes mellitus (63-66). Therefore, COVID-19 could be considered as a “stroke-trigger” with a 7.6-fold increase in the odds of cerebrovascular complications, as compared to influenza (67). Usually the onset of stroke delayed about 10 days after patients developed symptoms of COVID-19, including respiratory symptoms and fever (68,69). On the other hand, young-onset cases of stroke, without risk factors and comorbidities, are frequently related to large-vessel occlusion and occur before the onset of COVID-19 symptoms (70-72). Indeed, patients with COVID-19 appear to be particularly prone to large vessel occlusion or multi-territory involvement or involvement of otherwise uncommonly affected vessels (73-75), including for example the occlusion of the pericallosal artery (73), or the presence of multiple focal stenoses in the V4 segment of the vertebral artery (74). Then, a “protected code stroke” is necessary to be soon adopted in this frail population (76).
The pathogenesis could be explained by the binding of the SARS-CoV-2 to ACE2-R in endothelial cells increasing blood pressure which, together with the presence of thrombocytopenia and coagulation disorders, such as increased levels of D-dimers, prolonged prothrombin time and disseminated intravascular coagulation (77,78), can contribute to the increased risk of both ischaemic and haemorrhagic stroke. Other pathogenic mechanisms include the cytokine release syndrome: the virus infection predispose the patients to a systemic coagulopathy due to increased levels of fibrinogen (94%), platelet (62%) and D-dimer (100%), as well as IL-6 (100%), as a results of the excessive inflammatory state (79).
Meningoencephalitis
On March 4, 2020, the Beijing Ditan Hospital reported the first case of viral encephalitis related to the SARS-CoV-2 (80). A second case of meningoencephalitis was described in a 24 year-old Japanese male with the SARS-CoV-2 RNA detected only in the cerebrospinal fluid (CSF), and MRI hyperintense areas in the right lateral ventricle, the mesial region of the temporal lobe and the hippocampus (81). Further patients have been more recently reported from Strasbourg, France: agitation and corticospinal tract signs were present in 69% and 67% of the patients, respectively(82).
The pathophysiology is unclear but may be related to either the edema secondary to the inflammatory injury or a direct viral infection of the CNS (75).
In Japan, it has been described the first patient who was sent to the emergency department because of a convulsion accompanied by unconsciousness and who was subsequently diagnosed with aseptic encephalitis with the SARS-CoV-2 RNA detected in the CSF (83). Similarly, in Los Angeles, a young woman with COVID-19 showed symptoms of meningoencephalitis without respiratory failure, and SARS-CoV-2 was found to be positive in the CSF by reverse transcription–polymerase chain reaction (PCR) (84). In addition, two patients with acute meningoencephalitis associated to SARS-CoV-2 infection were reported in Switzerland, and a case of rhombencephalitis was reported as a rare complication of acute COVID-19 infection in the United Kingdom (85,86).
Acute disseminated encephalomyelitis (ADEM)
As far as we know, only three cases of ADEM associated to COVID-19 infection have been described: 1) A 40-year old woman with diffuse hyperintensities in the subcortical and deep white matter (87); 2) a 51-year-old woman who developed a coma and impaired unilateral oculocephalic response weeks after a SARS-CoV-2 infection with radiological evidence of ADEM (88); and 3) the autopsy of a 71-year-old patient diagnosed with COVID-19 showed scattered clusters of macrophages, axonal injury, and a perivascular ADEM-like appearance in the subcortical white matter (89). As for other viruses, an immunomediated reaction has been postulated to expalin the disease.
Acute Necrotizing Encephalopathy (ANE)
ANE is a rare complication recently described in patients with COVID-19 (90,91), although the disease was also described in other viral infections, including influenza. The pathogenesis is related to the cytokine release syndrome, a well-known manifestation of COVID-19. Typical MRI findings include hyperintense lesions and hemorrhage in the thalamus, brainstem, cerebellum, and cerebral white matter (92). In such a severe complication, a treatment with intravenous immunoglobulin (IVIG) and steroids can be attempted (93).
Epilepsy
Epileptic seizures are pissible complications of COVID-19. Indeed, new-onset seizures in critically ill patients with COVID-19 should be considered as acute symptomatic seizures and the treating physician should try to determine the etiology of the seizure and manage the cause immediately and appropriately (94). Interestingly, a focal status epilepticus as the onset of COVID-19 in the context of a predisposing but well-controlled SARS-CoV-2 related postencephalitic epilepsy has been reported (94). On the other hand, a man without any history of epilepsy developing multiple episodes of seizures after infection with SARS-CoV-2 was also reported (95). In addition, an infant with both COVID-19 and rhinovirus infections presented with a few seizures, although no changes were observed at the EEG (96).
Subacute Neurological Manifestations
Myelitis
Several cases of acute trasverse myelitis have been reported after COVID-19 infection. Among them: i) a 66-year-old man presented with acute flaccid paralysis of bilateral lower limbs and urinary and bowel incontinencedue to a multifocal transverse myelitis (87); ii) a 60-year-old man developed progressive weakness of the lower limbs, bladder dysfunction, hypoesthesia below the T9 level and a moderate spastic paraparesis due to a hyperintensity lesion of the thoracic spinal cord (97); iii) a 69-yearold woman was diagnosed with acute necrotizing myelitis based on the clinical symptoms and MRI manifestations (98).
Guillain-Barre syndrome (GBS)
Cases of Guillain-Barre syndrome (GBS) as significant neurological sequelae of SARS-CoV-2 have been reported (99,100). Among the published cases, there is a considerable variability in the onset of features of GBS and the typical respiratory symptoms. Generally, flaccid tetraparesis or tetraplegia evolved over a period of 36 hours to 4 days. The interval between the onset of symptoms of Covid-19 and the first symptoms of Guillain–Barré syndrome (GBS) ranged from 5 to 14 days, in line with the well-known “post-infectious” presentation of GBS. However, some GBS cases presented either as the same time as the symptoms of SARS-CoV-2 or before the COVID-19 onset (99). Then, Zhao et al. proposed a so-called “para-infectious” profile pattern when GBS occurs at the same time of an acute episode of infection (99), explaining some of the early onset cases of GBS with early significant respiratory involvement or in the absence of a history of any other plausible infection known to cause GBS. The pathogenesis of GBS and SARS-CoV-2 infection could be explained by the presence of antibodies against the surface glycoproteins of the pathogen, which also respond to similar native protein structures found in the surface of neurones leading (100-102). Other possible theories include the “macrophage activation syndrome,” also known as cytokine storm, with the subsequent “hyperinflammation” (103).
Another important point is the differentiation of GBS from critical illness polyneuropathy and myopathy, in patients with SARS-CoV-2, who have prolonged admission to intensive care (104,105).
Miller Fisher Syndrome and polyneuritis cranialis, which are variants of GBS causing cranial nerve and pharyngeal and facial weakness, have also been described as related to COVID-19 (106-108). An Italian multicentre retrospective/prospective study evaluating the neurologic manifestations of the hospitalized patients with COVID-19 found that the involvement of the CNS had a poor prognosis (109).
Chronic and Secondary Neurological Complications
More and more patients that recover from COVID-19 may complain of lasting neurological sequelae that may have been overlooked at the time of acute illness. Some patients after COVID-19 infection may develop a cognitive decline, including memory and executive function deficits. Moreover, older patients with a more severe disease course can also have confusion and apraxia/ataxia (110) due to a direct viral involvement of the CNS (111) or the effect of hypoxemia. Post-extubation dysphagia has been reported in 3% to 62% of patients requiring mechanical ventilation for ARDS (112,113). The pathophysiological mechanisms of dysphagia could be related to mechanical causes, diminished proprioception, laryngeal injury and peripheral or CNS damage.
Moreover, depression, fear and anger as well as post-traumatic stress disorder have been described as psychiatric problems during the SARS epidemic, for patients, relatives and healthcare workers. The further elements of prolonged ventilation, use of sedatives, prone positioning, human isolation, and extended time away from social contacts may contribute to these and other psychiatric problem, including severe delirium (114,115).
Other complications have been described secondary to COVID treatment. Many of the medications for SARS-COV2 infection (azithromycin, corticosteroids, biologic agents as tocilizumab, antivirals as remdesivir, ribavirin, lopinavir/ritonavir, favipiravir, or antimalarials as hydroxychloroquine and chloroquine) have significant drug interactions and side effects. Lopinavir/ritonavir and azithromycin interact with many common medications in patients with prior strokes including antihypertensives, antiplatelets, statins, and anticoagulants (116-118). These also carry an increased long-term risk of neurocognitive impairment (118-121). Ribavirin and interferon alpha may have both neuropathic and neuropsychiatric sequelae, while interferon caries a risk of retinopathy.122,123 Similarly, antimalarials also carry the risk of neuropsychiatric side effects and less commonly ataxia, seizures, and limbic encephalitis (124). Effects of remdesivir are still under investigation (125).
Treatment options: focus on rehabilitation
With the recent COVID-19 outbreak, there is a crucial need to understand the neurotropic potential of the COVID-19 virus to prioritize and individualize the treatment protocols based on the severity of the disease and predominant organ involvement. By now, no specific therapies are available, and the main measures are represented by prevention, isolation and social distancing, hygienic handwashing measures, and the use of masks.
Thousands of clinical trial results and articles have published in this process to provide treatment methods for the disease (126-128). According to level 1 evidence, the most effective SARS-Co-V-2 pharmacologic treatments include remdesivir for mild to severe disease, and a triple regimen therapy consisting of lopinavir-ritonavir, ribavirin and interferon beta-1b for mild to moderate disease. Also, dexamethasone significantly reduced mortality in those requiring respiratory support. Convalescent plasma from blood donors with anti-SARS-CoV-2 antibodies may benefit patients with COVID-19 by providing immediate passive immunity via transfusion, or when used to manufacture hyperimmune immunoglobulin preparations. Nonetheless, optimal product characteristics, volume of transfusion, and timing of administration, as well as real efficacy, remain to be determined (128).
Moreover, several vaccines for COVID-19 are in clinical trials (NCT04398147; NCT04456595; NCT04466085; NCT04368728) (129), and others under administration in many countries, including Italy (here starting from December 27).
About non pharmacological therapies, early rehabilitation plays an important role in neurological sequelae preventing complications on the respiratory system, restoring respiratory and physical independence, promoting weaning from mechanical ventilation, maintaining and improving the virus-damaged system functions, in order to improve prognosis, quality of life, and facilitates the return to daily activities and work (130,131). Therefore, it is necessary a staging based on the disease severity and organ involvement by SARS-CoV-2 to decide if aggressive or conventional treatment modalities has to be accomplish. However, clinicians are particularly cautious about risks associated with early intervention of rehabilitative techniques, holding a conservative attitude. Then, the extraordinary measures to prevent the spread of this disease urgently imposed a new organization of all ward included rehabilitation (132). By now, there is no evidence for early rehabilitation treatment of COVID-19, a lack of experience in acute management of COVID-19 patients, and the absence of guidelines recommendations.
To this end, a recent EAN expert consensus statement for the management of patients with neurological diseases during the COVID-19 pandemic have been recently published to guide harmonization of highquality healthcare across Europe in the face of current challenges (133).
Moreover, an expert panel with early experience managing patients with COVID-19 outlines the clear need for rehabilitation intervention in both the acute and post-acute phases of the disease (134). Some physicians are in the opinion that the current treatment plan should not allow physical therapists to provide treatment to COVID-19 patients in ICU, as this may increase the risk of cross infection, and that management of these patients should focus only on life support, antiviral therapy, and hormone therapy. It is believed that early rehabilitation will interfere with the clinical treatment, increase patient oxygen consumption, and may not cause any benefit, leading to the current situation where most critically ill patients are not offered the opportunity of early rehabilitative intervention. On the contrary, early rehabilitation of critically ill patients with COVID-19 is believed of some help when performing such an intervention on cognitive status, respiratory function, cardiovascular function, and musculoskeletal function (135).
Indeed, to manage the three major areas, i.e. positioning, early mobilization, and respiratory management, patients present a better prognosis, as per exercise capacity, muscle strength, and walking ability at discharge, as well as reductions in the duration of mechanical ventilation, length of the ICU stay, and length of hospital stay.
The new frontiers of rehabilitation, namely telemedicine, offer the opportunity to follow a rehabilitation program to those who are in hospitals lacking of rehab services or at home. In particular, “telemental health” is a new frontier of providing mental health assessment and treatment at a distance (136,137). Despite the distance, the tool could allow to perform psychology session on-time by creating and maintaining a psychologist/patient trusted relationship (136,137). A motor program with scheduled exercise could be also provided to the patients and virtual physical training program could be followed by several cross-platform tools. Although the initial doubtfully in this new kind of approach, the “cyberhealth psychotherapy” can encourage the patient to be more compliant with the rehabilitation daily schedule and motivated to recover their functions (138). Therefore, a multidisciplinary team is critical to achieve successfully the rehabilitation outcome and an early rehabilitation has become an indispensable part of multidisciplinary management of the critically ill patients. Even recent guidelines on pulmonary rehabilitation community-dwelling state that COVID-19 patients could be managed with telehealth programs to deliver the required rehabilitation input in the form of tele-rehabilitation (139).
In order to ensure that post-discharged COVID-19 patients were appropriately monitored and provided with the required input, a proposed pathway by the Hull University Teaching Hospital NHS Trust was developed. The care pathway aimed to evaluate the post recovery type of rehabilitation and the clinical needs of patients following infection with the SARS-Cov-2 virus in order to set in a multidisciplinary tele-rehabilitation component (139-142).
Cardiac and respiratory long-term complications are frequent after Covid-19, and they should be properly treated, as they can affect also the nervous system. Moreover, patients following stroke or other neurological complications may have cardiorespiratory failure, and thus they should be provided with respiratory rehabilitation, besides neurorehab. Curci et al. showed that post-acute COVID-19 patients suffered from dyspnoea and shortness of breath even for minimal activities, affecting motor rehabilitation (136). Nonetheless, patients with COVID-19 do not present only with respiratory and cardiological dysfunctions, but also with nutritional, internal and neurological injuries, accompanied by motor complications cognitive impairment, critical-illness–related myopathy and neuropathy, dysphagia, joint stiffness and pain, and psychiatric problems (anxiety, depression, fear and anger as well as post-traumatic stress disorder) caused by both prolonged immobilization and cerebral hypoxemia (111, 143-147). As a consequence, a multidisciplinary approach is fundamental to properly manage these frail patients.
In stroke patients with COVID-19, a longer period of immobility is known to delay functional recovery. Thus, the reduced assistance from physical and occupational therapists due to COVID-19 infection could be bypassed by facilitating devices of neurorehabilitation. Prospective techniques can be used to stimulate neurorestoration and maintain muscle strength and required minimal supervision (148). For example, transcutaneous electrical stimulation (TENS) devices of sensory and peripheral nerves improves early poststroke lower-extremity impairment and late motor function (149), improves the flaccid limb (150), and prevents post-stroke spasticity in lower limbs (151) as well as improves hand dexterity in patients with moderate to severe hemiparesis (152). Another simple, effective and feasible method could be the Mirror Therapy (MT) (153), using a mirror that is positioned between the affected and unaffected limbs reflecting the movement of an unaffected limb and giving the illusion of movement of the affected limb. This process facilitates the mirror neurons involved in imitative learning through interaction with the neural motor area (154, 155).
In patients with stroke, virtual reality (VR) can be used to improve upper limb function, gait and balance, global motor function, and cognitive function in patients with stroke (156-158). Also, serious exergamings have proven effective as an adjunct therapy to traditional treatment, especially in improving dynamic balance (158). However, for patients who are recommended to continue motor rehabilitation at home with adapted physical therapy, a supervision of self-managed home rehabilitation is necessary to avoid lacks compliance and abandonment daily exercise compromising a successful recovery (160). Home management of stroke patients is particularly important during pandemics, in order to avoid contagion.
The Italian Health system and the Lombardy region, in order to treat the overall COVID-19 complications established a unique COVID-19 Disease Unit at the San Raffaele Hospital, Milan, Italy (144,161). Three different types of rehabilitation were organised: 1) a high-complexity rehabilitation treating neurological disorders, such as post-stroke, traumatic brain injury, or spinal cord injury; 2) a medium-complexity rehabilitation treating cardiological, orthopaedic and post-infectious patients; and 3) a low-complexity rehabilitation treating chronic conditions (162). Therefore, the organization of COVID-19 rehabilitation units as an integral part of the therapeutic process is fundamental to cope with specific needs of this new clinical entity, not previously provided (163). Consequently, as proportion of patients with COVID-19–related disability could be rapidly grow, a prompt response from physical medicine and rehabilitation specialists is crucial to reduce disability and help re-establish and optimize the function of the acute hospital setting (146). It has been suggested that Rehabilitation Units should constitute an intermediary stage between ICU and discharge and should be prepared to ensure a proper management for patients with COVID-19- related disabilities, including the Post Intensive Care Syndrome (169-174).
Finally, when general condition of post-Covid patients is favourable, advanced treatment, including robotics with or without VR, could be take into consideration, given the efficacy in different neurological diseases (169-174).
Conclusions
COVID-19 primarily affects the respiratory and cardiovascular system. However, neurological involvement is not uncommon and, in some cases, can even precede the respiratory symptoms or may be the only symptoms in COVID-19 patients. The pathogenesis of CNS infection is likely related to the direct effect of the virus on the endothelium and the inflammatory cascade activation after COVID-19 increasing the risk of stroke, but many indirect mechanisms should be taken into consideration. The rapid spread of the COVID-19 pandemic will probably modify the organization and functioning of the healthcare services, including the rehabilitation treatments. However, this kind of treatment represents one of the fundamental field to better recover from critical and long-term COVID-19 consequences. Nonetheless, as no specific conclusions in term of prognosis and treatment could be done, research and consensus paper are needed to provide NeuroCovid patients with the best treatment options, including neurorehabilitation.
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- World Health Organization (WHO) WHO: Geneva, Switzerland; 2005. Statement on the Second Meeting of the International Health Regulations Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV) Available online: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-secondmeetingof-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-ofnovelcoronavirus-(2019-ncov) [Google Scholar]
- World Health Organisation. WHO: Geneva, Switzerland; 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19–11. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19; 11-March-2020. [Google Scholar]
- www.salute.gov.it; accessed on December, 19, 2020. [Google Scholar]
- Raciti L, Calabrò RS. Can volcanic trace elements facilitate Covid-19 diffusion? A hypothesis stemming from the Mount Etna area, Sicily. Med Hypotheses. 2020;144:110058. doi: 10.1016/j.mehy.2020.110058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishiura H, Kobayashi T, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020;94:154–155. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishiura H, Jung SM, Linton C, et al. The Extent of Transmission of Novel Coronavirus in Wuhan, China, 2020. J Clin Med. 2020;9:330. doi: 10.3390/jcm9020330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park M, Cook A, Lim JT, Sun Y, Dickens B. A Systematic Review of COVID-19 Epidemiology Based on Current Evidence. J Clin Med. 2020;9:967. doi: 10.3390/jcm9040967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li LQ, Huang T, Wang YQ, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92:577–583. doi: 10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang F, Deng L, Zhang L, Cai Y, Cheung CW, Xia ZY. Review of the Clinical Characteristics of Coronavirus Disease 2019 (COVID-19) J Gen Intern Med. 2020;35:1545–1549. doi: 10.1007/s11606-020-05762-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020; Mar 17 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Moore MJ, Vasilieva N, et al. Angiotensin-converting enzyme 2: a functional receptor for SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin Med (Lond) 2020;20:124–7. doi: 10.7861/clinmed.2019-coron. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glowacka I, Bertram S, Muller MA, et al. Evidence that TMPRSS2 activates the severe acute respiratory syndrome coronavirus spike protein for membrane fusion and reduces viral control by the humoral immune response. J Virol. 2011;85(9):4122–4134. doi: 10.1128/JVI.02232-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei S, Jiang F, Su W, Chen C, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J, Tong Z, Guan X, Du B, Qiu H. Clinical Characteristics of Patients Who Died of Coronavirus Disease 2019 in China. JAMA Netw Open. 2020;3:e205619. doi: 10.1001/jamanetworkopen.2020.5619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Chen X, Lu Y, Chen F, Zhang W. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci Trends. 2020;14:64–68. doi: 10.5582/bst.2020.01030. [DOI] [PubMed] [Google Scholar]
- Kim ES, Chin BS, Kang CK, et al. Clinical Course and Outcomes of Patients with Severe Acute Respiratory Syndrome Coronavirus2 Infection: A Preliminary Report of the First 28 Patients from the Korean Cohort Study on COVID-19. J Korean Med Sci. 2020;35:e142. doi: 10.3346/jkms.2020.35.e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishiura H, Kobayashi T, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020;94:154–155. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu L, Wang B, Yuan T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infect. 2020;80:656–665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (nCoV) Infection Is Suspected. Available online: https://www.who.int/publications-detail/clinicalmanagement-of-severeacute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected (accessed on 17 March 2020) [Google Scholar]
- Li JY, You Z, Wang Q, Zhou ZJ, Qiu Y, Luo R, Ge XY. The epidemic of 2019-novel-coronavirus (2019-nCoV) pneumonia and insights for emerging infectious diseases in the future. Microbes Infect. 2020;22:80–85. doi: 10.1016/j.micinf.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmy YA, Fawzy M, Elaswad A, Sobieh A, Kenney SP, Shehata AA. The COVID-19 Pandemic: A Comprehensive Review of Taxonomy, Genetics, Epidemiology, Diagnosis, Treatment, and Control. J Clin Med. 2020;9:1225. doi: 10.3390/jcm9041225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17:181–92. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desforges M, Le Coupanec A, Dubeau P, et al. Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses. 2019:12. doi: 10.3390/v12010014. pii: E14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82:7264–75. doi: 10.1128/JVI.00737-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbour N, Cote G, Lachance C, Tardieu M, Cashman NR, Talbot PJ. Acute and persistent infection of human neural cell lines by human coronavirus OC43. J Virol. 1999;73:3338–50. doi: 10.1128/jvi.73.4.3338-3350.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbour N, Ekande S, Cote G, et al. Persistent infection of human oligodendrocytic and neuroglial cell lines by human coronavirus 229E. J Virol. 1999;73:3326–7. doi: 10.1128/jvi.73.4.3326-3337.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbour N, Day R, Newcombe J, Talbot PJ. Neuroinvasion by human respiratory coronaviruses. J Virol. 2000;4:8913–21. doi: 10.1128/jvi.74.19.8913-8921.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brison E, Jacomy H, Desforges M, Talbot PJ. Glutamate excitotoxicity is involved in the induction of paralysis in mice after infection by a human coronavirus with a single point mutation in its spike protein. J Virol. 2011;85:12464–73. doi: 10.1128/JVI.05576-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: Tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11:995–8. doi: 10.1021/acschemneuro.0c00122. [DOI] [PubMed] [Google Scholar]
- Baig AM. Updates on what ACS reported: emerging evidences of COVID-19 with nervous system involvement. ACS Chem Nerosci. 2020 doi: 10.1021/acschemneuro.0c00181. doi.org/10.1021/ acschemsneuro.0c00181 April. [DOI] [PubMed] [Google Scholar]
- Fu Y, Cheng Y, Wu Y. Understanding SARS-CoV-2-mediated inflammatory responses: from mechanisms to potential therapeutic tools. Virol Sin. 2020 doi: 10.1007/s12250-020-00207-4. https://doi.org/10.1007/s12250-020-00207-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karimi N, Rouhani N. COVID 19 and intra cerebral hemorrhage: causative or coincidental. New Microb New Infect. [Internet] 2020:100669. doi: 10.1016/j.nmni.2020.100669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.03.031. https://doi.org/10.1016/j.bbi. 2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-a n update on the status. Mil Med Res. 2020;7(1) doi: 10.1186/s40779-020-00240-0. doi.org/10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé M, Le Coupanec A, Wong AHM, Rini JM, Desforges M, Talbot PJ. Axonal transport enables neuron-to-neuron propagation of human coronavirus OC43. J Virol. 2018;92(17) doi: 10.1128/JVI.00404-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nogués MA, Benarroch E. Respiratory control disorders and respiratory motor unit. Neurol Argent. 2011;3:167–175. [Google Scholar]
- Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may be at least partially responsible for the respiratory failure of COVID-19 patients. J Med Virol. 2020;2:0–2. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L, Zhang M, Wang J, Gao J. Sars-Cov-2: Underestimated damage to nervous system Travel Med Infect Dis. 2020:101642. doi: 10.1016/j.tmaid.2020.101642. doi: 10.1016/j.tmaid.2020.101642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z, Shi L, Wang Y, et al. Pathological fi ndings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delorme C, Paccoud O, Kas A, et al. CoCo-Neurosciences study group and COVID SMIT PSL study group. COVID-19-related encephalopathy: a case series with brain FDG-positron-emission tomography/computed tomography findings. Eur J Neurol. 2020;27(12):2651–2657. doi: 10.1111/ene.14478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambreanu L, Lightbody S, Bhandari M, et al. A case of limbic encephalitis associated with asymptomatic COVID-19 infection. J Neurol Neurosurg Psychiatry. 2020;91(11):1229–1230. doi: 10.1136/jnnp-2020-323839. [DOI] [PubMed] [Google Scholar]
- Khoo A, McLoughlin B, Cheema S, et al. Postinfectious brainstem encephalitis associated with SARS-CoV-2. J Neurol Neurosurg Psychiatry. 2020;91(9):1013–1014. doi: 10.1136/jnnp-2020-323816. [DOI] [PubMed] [Google Scholar]
- Gigli GL, Bax F, Marini A, et al. Guillain-Barré syndrome in the COVID-19 era: just an occasional cluster? J Neurol. 2020 doi: 10.1007/s00415-020-09911-3. doi: 10.1007/s00415-020-09911-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gigli GL, Vogrig A, Nilo A, et al. HLA and immunological features of SARS-CoV-2-induced Guillain-Barré syndrome. Neurol Sci. 2020;41(12):3391–3394. doi: 10.1007/s10072-020-04787-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morassi M, Bagatto D, Cobelli M, et al. Stroke in patients with SARS-CoV-2 infection: case series. J Neurol. 2020;267(8):2185–2192. doi: 10.1007/s00415-020-09885-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogrig A, Bagatto D, Gigli GL, et al. Causality in COVID-19-associated stroke: a uniform case definition for use in clinical research. J Neurol. 2020 doi: 10.1007/s00415-020-10103-2. doi: 10.1007/s00415-020-10103-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyrouti R, Adams ME, Benjamin L, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry. 2020;91(8):889–891. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxley TJ, Mocco J, Majidi S, et al. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N Engl J Med. 2020;382(20):e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Fernández F, Sandoval Valencia H, Barbella-Aponte RA, et al. Cerebrovascular disease in patients with COVID-19: neuroimaging, histological and clinical description. Brain. 2020;143(10):3089–3103. doi: 10.1093/brain/awaa239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin M, Tong Q. Rhabdomyolysis as potential late complication associated with 2019 novel coronavirus disease. Emerg Infect Dis. 2020;26(7):1618–1620. doi: 10.3201/eid2607.200445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacomelli A, Pezzati L, Conti F, et al. Selfreported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: a cross-sectional study. Clin Infect Dis. 2020;71:889–90. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filatov A, Sharma P, Hindi F, Espinosa PS. Neurological complications of coronavirus disease (COVID-19): encephalopathy. Cureus. 2020;12(3):e7352. doi: 10.7759/cureus.7352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis. 2020;71(15):889–890. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Li M, Wang M, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc Neurol. 2020;5(3):279–284. doi: 10.1136/svn-2020-000431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benussi A, Premi E, Pilotto A, et al. Effects of COVID-19 outbreak on stroke admissions in Brescia, Lombardy, Italy. Eur J Neurol. 2021;28(1):e4–e5. doi: 10.1111/ene.14505. [DOI] [PubMed] [Google Scholar]
- Lee MH, Perl DP, Nair G, et al. Microvascular Injury in the Brains of Patients with Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMc2033369. 10.1056/NEJMc2033369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan YK, Goh C, Leow AST, et al. COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J Thromb Thrombolysis. 2020;50(3):587–595. doi: 10.1007/s11239-020-02228-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridman S, Bres Bullrich M, Jimenez-Ruiz A, et al. Stroke risk, phenotypes, and death in COVID-19: Systematic review and newly reported cases. Neurology. 2020;95(24):e3373–e3385. doi: 10.1212/WNL.0000000000010851. [DOI] [PubMed] [Google Scholar]
- Merkler AE, Parikh NS, Mir S, et al. Risk of Ischemic Stroke in Patients With Coronavirus Disease 2019 (COVID-19) vs Patients With Influenza. JAMA Neurol. 2020;77(11):1–7. doi: 10.1001/jamaneurol.2020.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellul MA, Benjamin L, Singh B, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19(9):767–783. doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan YK, Goh C, Leow AST, et al. COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J Thromb Thrombolysis. 2020;50(3):587–595. doi: 10.1007/s11239-020-02228-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxley TJ, Mocco J, Majidi S, et al. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N Engl J Med. 2020;382(20):e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji XY, Ma Y, Shi NN, et al. Clinical characteristics and treatment outcome of COVID-19 patients with stroke in China: A multicenter retrospective study. Phytomedicine. 2020;81:153433. doi: 10.1016/j.phymed.2020.153433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fifi JT, Mocco J. COVID-19 related stroke in young individuals. Lancet Neurol. 2020;19:713–715. doi: 10.1016/S1474-4422(20)30272-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17:181–92. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye M, Ren Y, Lv T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav Immun. 2020;88:945–6. doi: 10.1016/j.bbi.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriguchi T, Harii N, Goto J, et al. A first case of meningitis/encephalitis associated with SARS-coronavirus-2. Int J Infect Dis. 2020;94:55–8. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Pinto T, Luna-Rodríguez A, Moreno-Estébanez A, Agirre-Beitia G, Rodríguez-Antigüedad A, Ruiz-Lopez M. Emergency room neurology in times of COVID-19: malignant ischemic stroke and SARS-COV2 infection. Eur J Neurol. 2020 doi: 10.1111/ene.14286. https://doi.org/10.1111/ene.14286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connors J, Levy J. Thromboinflammation and hypercoagulability of COVID-19. J Thromb Haemost. 2020;18(7):1559–1561. doi: 10.1111/jth.14849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.03.031. doi: https://doi.org/10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriguchi T, Harii N, Goto J, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARSCoV-2 infection. N Engl J Med. 2020;382(23):2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duong L, Xu P, Liu A. Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in downtown los angeles, early April 2020. Brain Behav Immun. 2020;87:33. doi: 10.1016/j.bbi.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang YH, Jiang D, Huang JT. SARS-CoV-2 detected in cerebrospinal fluid by PCR in a case of COVID-19 encephalitis. Brain Behav Immun. 2020;87:149. doi: 10.1016/j.bbi.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M, et al. Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection. Eur J Neurol. 2020 doi: 10.1111/ene.14298. doi: 10.1111/ene.14298 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong PF, Craik S, Newman P, Makan A, Srinivasan K, Crawford E, et al. Lessons of the month 1: a case of rhombencephalitis as a rare complication of acute COVID-19 infection. Clin Med. 2020;20:293–4. doi: 10.7861/clinmed.2020-0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow CCN, Magnussen J, Ip J, Su Y. Acute transverse myelitis in COVID-19 infection. BMJ Case Rep. 2020;13(8):e236720. doi: 10.1136/bcr-2020-236720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons T, Banks S, Bae C, Gelber J, Alahmadi H, Tichauer M. COVID-19-associated acute disseminated encephalomyelitis (ADEM) J Neurol. 2020;267:2799–802. doi: 10.1007/s00415-020-09951-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichard RR, Kashani KB, Boire NA, Constantopoulos E, Guo Y, Lucchinetti CF. Neuropathology of COVID-19: a spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology. Acta Neuropathol. 2020;140:1–6. doi: 10.1007/s00401-020-02166-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: Imaging Features. Radiology. 2020;296(2):E119–E120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon L, Varley J, Gontsarova A, et al. COVID-19-related acute necrotizing encephalopathy with brain stem involvement in a patient with aplastic anemia. Neurol Neuroimmunol Neuroinflamm. 2020;7(5):e789. doi: 10.1212/NXI.0000000000000789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong A, Simon E, Zimmerman R, Wang H, Toh C, Ng S. Acute necrotizing encephalopathy of childhood: correlation of MR findings and clinical outcome. Am J Neuroradiol. 2006;27(9):1919–23. [PMC free article] [PubMed] [Google Scholar]
- Alsolami A, Shiley K. Successful treatment of influenza-associated acute necrotizing encephalitis in an adult using high-dose oseltamivir and methylprednisolone: case report. Open Forum Infect Dis. 2017;4(3):145. doi: 10.1093/ofid/ofx145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emami A, Fadakar N, Akbari A, et al. Seizure in patients with COVID-19. Neurol Sci. 2020;41(11):3057–3061. doi: 10.1007/s10072-020-04731-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohal S, Mossammat M. COVID-19 presenting with seizures. IDCases. 2020;20:e00782. doi: 10.1016/j.idcr.2020.e00782. doi: 10.1016/j.idcr.2020.e00782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugue R, Cay-Martínez KC, Thakur KT, Garcia JA, Chauhan LV, Williams SH, et al. Neurologic manifestations in an infant with COVID-19. Neurology. 2020;94:1100–2. doi: 10.1212/WNL.0000000000009653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munz M, Wessendorf S, Koretsis G, et al. Acute transverse myelitis after COVID-19 pneumonia. J Neurol. 2020;267:2196–7. doi: 10.1007/s00415-020-09934-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotoca J, Rodríguez-Álvarez Y. COVID-19-associated acute necrotizing myelitis. Neurol Neuroimmunol Neuroinflamm. 2020;7:e803. doi: 10.1212/NXI.0000000000000803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H, Shen D, Zhou H, Liu J, Chen S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19(5):383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottaviani D, Boso F, Tranquillini E, et al. Early Guillain-Barré syndrome in coronavirus disease 2019 (COVID-19): a case report from an Italian COVID-hospital. Neurol Sci. 2020;41(6):1351–1354. doi: 10.1007/s10072-020-04449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao-Lormeau VM, Blake A, Mons S, et al. Guillain-Barré syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet. 2016;387(10027):1531–1539. doi: 10.1016/S0140-6736(16)00562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virani A, Rabold E, Hanson T, Haag A, Elrufay R, Cheema T. Guillain-Barré Syndrome associated with SARS-CoV-2 infection. IDCases. 2020;20:e00771. doi: 10.1016/j.idcr.2020.e00771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGonagle D, Sharif K, O’Regan A, Bridgewood C. The role of cytokines including Interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev. 2020;19(6):102537. doi: 10.1016/j.autrev.2020.102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toscano G, Palmerini F, Ravaglia S, et al. Guillain-Barré Syndrome Associated with SARS-CoV-2. N Engl J Med. 2020;382(26):2574–2576. doi: 10.1056/NEJMc2009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittaker A, Anson M, Harky A. Neurological Manifestations of COVID-19: A systematic review and current update. Acta Neurol Scand. 2020;142(1):14–22. doi: 10.1111/ane.13266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutiérrez-Ortiz C, Méndez A, Rodrigo-Rey S, et al. Miller Fisher Syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020 doi: 10.1212/WNL.0000000000009619. doi: 10.1212/WNL.0000000000009619. [DOI] [PubMed] [Google Scholar]
- Lantos JE, Strauss SB, Lin E. COVID-19-associated miller fisher syndrome: MRI findings. AJNR Am J Neuroradiol. 2020;41:1184–6. doi: 10.3174/ajnr.A6609. doi: 10.3174/ajnr.A6609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutiérrez-Ortiz C, Méndez-Guerrero A, Rodrigo-Rey S, San Pedro-Murillo E, Bermejo-Guerrero L, Gordo-Mañas R, et al. Miller fisher syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020;95:e601–5. doi: 10.1212/WNL.0000000000009619. doi: 10.1212/WNL.0000000000009619. [DOI] [PubMed] [Google Scholar]
- Ferrarese C, Silani V, Priori A, et al. An Italian multicenter retrospective-prospective observational study on neurological manifestations of COVID-19 (NEUROCOVID) Neurol Sci. 2020;41(6):1355–1359. doi: 10.1007/s10072-020-04450-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filatov A, Sharma P, Hindi F, Espinosa PS. Neurological complications of Coronavirus Disease (COVID-19): encephalopathy. Cureus. 2020 doi: 10.7759/cureus.7352. cited 2020 Apr 1; available from: https://www.cureus.com/articles/29414-neurological-complications-of-coronavirus-disease-covid-19-encephalopathy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y-C, Bai W-Z, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.25728. http://dx.doi.org/10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodsky MB, Huang M, Shanholtz C, et al. Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors. A 5-year longitudinal study. Ann Am Thorac Soc. 2017;14:376–83. doi: 10.1513/AnnalsATS.201606-455OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T, Lu H, Zhang W. Clinical observation and management of COVID-19 patients. Emerg Microbes Infect. 2020;9:687–90. doi: 10.1080/22221751.2020.1741327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34–9. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611–27. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfiky AA. Anti-HCV, nucleotide inhibitors, repurposing against COVID-19. Life Sci. 2020;248 doi: 10.1016/j.lfs.2020.117477. https://doi.org/10.1016/j.lfs.2020.117477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez S, Long B, Koyfman A, Liang SY. Coronavirus disease (COVID-19): a primer for emergency physicians. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.03.036. doi.org/10.1016/j. ajem.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38:1504–7. doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharyya A, Kumar S, Sarma P, et al. Safety and efficacy of lopinavir/ritonavir combination in COVID-19: A systematic review, meta-analysis, and meta-regression analysis. Indian J Pharmacol. 2020;52(4):313–323. doi: 10.4103/ijp.IJP_627_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younis NK, Zareef RO, Al Hassan SN, Bitar F, Eid AH, Arabi M. Hydroxychloroquine in COVID-19 Patients: Pros and Cons. Front Pharmacol. 2020;11:597985. doi: 10.3389/fphar.2020.597985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pistell PJ, Gupta S, Knight AG, et al. Metabolic and neurologic consequences of chronic lopinavir/ritonavir administration to C57BL/6 mice. Antiviral Res. 2010;88(3):334–42. doi: 10.1016/j.antiviral.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleijfer S, Bannink M, Van Gool AR, Kruit WHJ, Stoter G. Side effects of interferon-α therapy. Pharm World Sci. 2005;27(6):423–31. doi: 10.1007/s11096-005-1319-7. [DOI] [PubMed] [Google Scholar]
- Russo MW, Fried MW. Side effects of therapy for chronic hepatitis C. Gastroenterology. 2003;124(6):1711–9. doi: 10.1016/s0016-5085(03)00394-9. [DOI] [PubMed] [Google Scholar]
- Maxwell NM, Nevin RL, Stahl S, et al. Prolonged neuropsychiatric effects following management of chloroquine intoxication with psychotropic polypharmacy. Clin Case Reports. 2015;3(6):379–87. doi: 10.1002/ccr3.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020 doi: 10.1016/S0140-6736(20)31022-9. doi.org/10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020;323(18):1824–1836. doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- Baroutjian A, Sanchez C, Boneva D, McKenney M, Elkbuli A. SARS-CoV-2 pharmacologic therapies and their safety/effectiveness according to level of evidence. Am J Emerg Med. 2020;38(11):2405–2415. doi: 10.1016/j.ajem.2020.08.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood EM, Estcourt LJ, McQuilten Z. How should we use convalescent plasma therapies for COVID-19? Blood. 2020 doi: 10.1182/blood.2020008903. doi: 10.1182/blood.2020008903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y, Dai T, Wei Y, Zhang L, Zheng M, Zhou F. A systematic review of SARS-CoV-2 vaccine candidates. Signal Transduct Target Ther. 2020;5(1):237. doi: 10.1038/s41392-020-00352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Ding Y, Li X, Yang L, Zhang W, Kang W. Fatal aspergillosis in a patient with SARS who was treated with corticosteroids. N Engl J Med. 2003;349:507–8. doi: 10.1056/NEJM200307313490519. [DOI] [PubMed] [Google Scholar]
- Sosnowski K, Lin F, Mitchell ML, White H. Early rehabilitation in the intensive care unit: an integrative literature review. Aust Crit Care. 2015;28(4):216–225. doi: 10.1016/j.aucc.2015.05.002. [DOI] [PubMed] [Google Scholar]
- Carda S, Invernizzi M, Bavikatte G, et al. The role of physical and rehabilitation medicine in the COVID-19 pandemic: The clinician’s view. Ann Phys Rehabil Med. 2020;63(6):554–556. doi: 10.1016/j.rehab.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Oertzen TJ, Macerollo A, Leone MA, et al. EANcore COVID-19 task force. EAN consensus statement for management of patients with neurological diseases during the COVID-19 pandemic. Eur J Neurol. 2021;28(1):7–14. doi: 10.1111/ene.14521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonter SJ, Alter K, Bartels MN, et al. What Now for Rehabilitation Specialists? Coronavirus Disease 2019 Questions and Answers. Arch Phys Med Rehabil. 2020;101(12):2233–2242. doi: 10.1016/j.apmr.2020.09.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SY, Kumble S, Patel B, et al. Managing the Rehabilitation Wave: Rehabilitation Services for COVID-19 Survivors. Arch Phys Med Rehabil. 2020;101(12):2243–2249. doi: 10.1016/j.apmr.2020.09.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curci C, Pisano F, Bonacci E, et al. Early rehabilitation in post-acute COVID-19 patients: data from an Italian COVID-19 rehabilitation unit and proposal of a treatment protocol. A cross-sectional study. Eur J Phys Rehabil Med. 2020 doi: 10.23736/S1973-9087.20.06339-X. doi:10.23736/S1973-9087.20.06339-X. [DOI] [PubMed] [Google Scholar]
- Maresca G, De Cola MC, Caliri S, et al. Moving towards novel multidisciplinary approaches for improving elderly quality of life: The emerging role of telemedicine in Sicily. J Tel Telecare. 2018 doi: 10.1177/1357633X17753057. 1357633X17753057. [DOI] [PubMed] [Google Scholar]
- Maresca G, Maggio MG, De Luca R, et al. Tele-Neuro-Rehabilitation in Italy: State of the Art and Future Perspectives. Front Neurol. 2020;11:563375. doi: 10.3389/fneur.2020.563375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salawu A, Green A, Crooks MG, Brixey N, Ross DH, Sivan M. A Proposal for Multidisciplinary Tele-Rehabilitation in the Assessment and Rehabilitation of COVID-19 Survivors. Int J Environ Res Public Health. 2020;17(13):4890. doi: 10.3390/ijerph17134890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS England Clinical guide for the management of surge during the coronavirus pandemic: Rapid learning. 2020 Available online: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0167-specialty-guide-surge-based-on-current-hospital-experience-v2.pdf. [Google Scholar]
- De Cola MC, De Luca R, Bramanti A, Bertè F, Bramanti P, Calabrò RS. Tele-health services for the elderly: a novel southern Italy family needs-oriented model. J Tel Telecare. 2016;22(6):356–362. doi: 10.1177/1357633X15604290. [DOI] [PubMed] [Google Scholar]
- Pedretti. Monaldi Arch Chest Dis. 2018 [Google Scholar]
- Kemps HMC, Brouwers RWM, Cramer MJ, et al. Recommendations on how to provide cardiac rehabilitation services during the COVID-19 pandemic. Neth Heart J. 2020 doi: 10.1007/s12471-020-01474-2. https://doi.org/10.1007/s12471-020-01474-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugliera L, Spina A, Castellazzi P, et al. Nutritional management of COVID-19 patients in a rehabilitation unit. Eur J Clin Nutrit. 2020:1–4. doi: 10.1038/s41430-020-0664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugliera L, Spina A, Castellazzi P, et al. Rehabilitation of COVID-19 patients. J Rehabil Med. 2020;52:jrm00046. doi: 10.2340/16501977-2678. [DOI] [PubMed] [Google Scholar]
- Smith SR, Jenq G, Claflin T, Magnant C, Haig AJ, Hurvitz E. Proposed workflow for rehabilitation in a field hospital setting during the COVID-19 pandemic. PMR. 2020 doi: 10.1002/pmrj.12405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carda S, Invernizzi M, Bavikatte G, et al. The role of physical and rehabilitation medicine in the COVID-19 pandemic: The clinician’s view. Ann Phys Rehabil Med. 2020 doi: 10.1016/j.rehab.2020.04.001. doi:10.1016/j.rehab.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang CC, Chao JK, Wang ML, et al. Care for Patients with Stroke During the COVID-19 Pandemic: Physical Therapy and Rehabilitation Suggestions for Preventing Secondary Stroke. J Stroke Cerebrovasc Dis. 2020;29(11):105182. doi: 10.1016/j.jstrokecerebrovasdis.2020.105182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharififar S, Shuster JJ, Bishop MD. Adding electrical stimulation during standard rehabilitation after stroke to improve motor function. a systematic review and metaanalysis. Ann Phys Rehabil Med. 2018;61(5):339–344. doi: 10.1016/j.rehab.2018.06.005. [DOI] [PubMed] [Google Scholar]
- Nasuelli NA, Pettinaroli R, Godi L, et al. Critical illness neuro-myopathy (CINM) and focal amyotrophy in intensive care unit (ICU) patients with SARS-CoV-2: a case series. Neurol Sci. 2020:1–3. doi: 10.1007/s10072-020-04820-9. doi: 10.1007/s10072-020-04820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood A, Veluswamy SK, Hombali A, Mullick A N M, Solomon JM. Effect of transcutaneous electrical nerve stimulation on spasticity in adults with stroke: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2019;100(4):751–768. doi: 10.1016/j.apmr.2018.10.016. [DOI] [PubMed] [Google Scholar]
- Liu H, Au-Yeung SSY. Corticomotor excitability effects of peripheral nerve electrical stimulation to the paretic arm in stroke. Am J Phys Med Rehabil. 2017;96(10):687–693. doi: 10.1097/PHM.0000000000000748. [DOI] [PubMed] [Google Scholar]
- Gandhi DB, Sterba A, Khatter H, Pandian JD. Mirror therapy in stroke rehabilitation: current perspectives. Ther Clin Risk Manage. 2020;16:75–85. doi: 10.2147/TCRM.S206883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho D, Teixeira S, Lucas M, et al. The mirror neuron system in post-stroke rehabilitation. Int Arch Med. 2013;6(1):41. doi: 10.1186/1755-7682-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thieme H, Morkisch N, Mehrholz J, et al. Mirror therapy for improving motor function after stroke. Cochrane Database Syst Rev. 2018;7:Cd008449. doi: 10.1002/14651858.CD008449.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- In T, Lee K, Song C. Virtual Reality Reflection Therapy Improves Balance and Gait in Patients with Chronic Stroke: Randomized Controlled Trials. Med Sci Monit: Int Med J Exp Clin Res. 2016;22:4046–4053. doi: 10.12659/MSM.898157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekbib DB, Han J, Zhang L, et al. Virtual reality therapy for upper limb rehabilitation in patients with stroke: a meta-analysis of randomized clinical trials. Brain Inj. 2020;34(4):456–465. doi: 10.1080/02699052.2020.1725126. [DOI] [PubMed] [Google Scholar]
- Laver KE, Lange B, George S, Deutsch JE, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017;11:Cd008349. doi: 10.1002/14651858.CD008349.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karasu AU, Batur EB, Karatas GK. Effectiveness of Wiibased rehabilitation in stroke: a randomized controlled study. J Rehabil Med. 2018;50(5):406–412. doi: 10.2340/16501977-2331. [DOI] [PubMed] [Google Scholar]
- Zedda A, Gusai E, Caruso M, et al. DoMoMEA: a Home-Based Telerehabilitation System for Stroke Patients. Annu Int Conf IEEE Eng Med Biol Soc. 2020;2020:5773–5776. doi: 10.1109/EMBC44109.2020.9175742. [DOI] [PubMed] [Google Scholar]
- Li J. Rehabilitation management of patients with COVID-19. Lessons learned from the first experiences in China. Eur J Phys Rehabil Med. 2020 doi: 10.23736/S1973-9087.20.06292-9. PMID: 32329589. [DOI] [PubMed] [Google Scholar]
- Wainwright TW, Low M. Beyond acute care: why collaborative self-management should be an essential part of rehabilitation pathways for COVID-19 patients. J Rehabil Med. 2020;52:jrm00055. doi: 10.2340/16501977-2685. [DOI] [PubMed] [Google Scholar]
- Iannaccone S, Alemanno F, Houdayer E, et al. COVID-19 rehabilitation units are twice as expensive as regular rehabilitation units. J Rehabil Med. 2020;52(6):jrm00073. doi: 10.2340/16501977-2704. [DOI] [PubMed] [Google Scholar]
- Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID-19 infection. Am J Phys Med Rehabil. 2020;99:470–474. doi: 10.1097/PHM.0000000000001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiekens C, Boldrini P, Andreoli A, et al. Rehabilitation and respiratory management in the acute and early post-acute phase. “Instant paper from the field” on rehabilitation answers to the Covid-19 emergency. Eur J Phys Rehabil Med. 2020 doi: 10.23736/S1973-9087.20.06305-4. doi: 10.23736/S1973-9087.20.06305-4. [DOI] [PubMed] [Google Scholar]
- Levy J, Léotard A, Lawrence C, et al. A model for a ventilator-weaning and early rehabilitation unit to deal with post-ICU impairments with severe COVID-19. Ann Phys Rehabil Med. 2020 doi: 10.1016/j.rehab.2020.04.002. doi: 10.1016/j.rehab.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao HM, Xie YX, Wang C. Recommendations for respiratory rehabilitation in adults with COVID-19. Chin Med J (Engl) 2020 doi: 10.1097/CM9.0000000000000848. doi: 10.1097/CM9.0000000000000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stam HJ, Stucki G, Bickenbach J. Covid-19 and Post Intensive Care Syndrome: A Call for Action. J Rehabil Med. 2020;52(4):jrm00044. doi: 10.2340/16501977-2677. doi: 10.2340/16501977-2677. [DOI] [PubMed] [Google Scholar]
- Wang YL, Zhu FZ, Zeng L, et al. Guideline for diagnosis and treatment of spine trauma in the epidemic of COVID-19. Chin J Traumatol. 2020:S1008–1275. doi: 10.1016/j.cjtee.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrò RS, Naro A, Russo M, et al. The role of virtual reality in improving motor performance as revealed by EEG: a randomized clinical trial. J Neuroeng Rehabil. 2017;14(1):53. doi: 10.1186/s12984-017-0268-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni MF, Melegari C, De Cola MC, Bramanti A, Bramanti P, Calabrò RS. What does best evidence tell us about robotic gait rehabilitation in stroke patients: A systematic review and meta-analysis. J Clin Neurosci. 2018;48:11–17. doi: 10.1016/j.jocn.2017.10.048. [DOI] [PubMed] [Google Scholar]
- Maggio MG, Torrisi M, Buda A, et al. Effects of robotic neurorehabilitation through lokomat plus virtual reality on cognitive function in patients with traumatic brain injury: A retrospective case-control study. Int J Neurosci. 2019 doi: 10.1080/00207454.2019.1664519. doi: 10.1080/00207454.2019.1664519. [DOI] [PubMed] [Google Scholar]
- Portaro S, Russo M, Bramanti A, et al. The role of robotic gait training and tDCS in Friedrich ataxia rehabilitation: A case report. Medicine (Baltimore) 2019;98(8):e14447. doi: 10.1097/MD.0000000000014447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straudi S, Benedetti MG, Venturini E, Manca M, Foti C, Basaglia N. Does robot-assisted gait training ameliorate gait abnormalities in multiple sclerosis? A pilot randomized-control trial. NeuroRehabilitation. 2013;33(4):555–63. doi: 10.3233/NRE-130990. [DOI] [PubMed] [Google Scholar]


