Abstract
Background:
Over the last 20 years, the incidence of pediatric femoral shaft fractures was increased, due to changes in the children’s daily activities. The healing times are different according to the chosen treatment and to other factors such as age, type of fracture, the involvement of the soft tissues, and concomitance with other injuries. The Bisaccia and Meccariello technique (Intramedullary titanium nail Osteosynthesis Linked External-fixator -IOLE) was born to prevent rotationally and lengthening malunion or nonunion in the treatment of pediatric femoral shaft fractures.
Hypotheis:
The aim or the objective of this paper is to compare the IOLE with the two most used methods for the treatment of femoral fractures in children.
Methods:
From 2000 to 2016, 58 pediatric patients with femoral shaft fractures were surgically treated and enrolled in the study. The ranged age of the patients was between 3 and 15 years. Twenty-two patients were treated with endomedullary titanium nails (TEN), 22 with external axial or modular external fixators and 14 patients treated with IOLE technique. The IOLE technique, in brief, is the hybridization of titanium intramedullary nails with a modular external fixator. It is divided into three phases, the first revenue given the length of the femur with the external fixator; the second, the rotations are dominated by the elastic nails; and the third finally they are hybridized on the external fixator. Comparing the three groups, radiographic images were taken to assess fracture reduction and consolidation.
Results:
At the final follow-up, statistically significant differences in not weight-bearing times were found in favor of the IOLE group. There were no statistical differences between three groups in terms of significant rotation defects, angulation, growth, and/or nonunion.
Conclusions:
The Bisaccia- Meccariello technique (IOLE) showed to lead to healing the pediatric femoral shaft fracture of the femur but allows an early weight-bearing to these patients and normal life like that.
Keywords: External fixator, Femoral fractures, Pediatric fractures, TEN
Introduction
Pediatric femoral shaft fractures are the most frequent lesions treated by the orthopedic surgeon (1, 2). They represent about 1–2% of all bone lesions in children (3). They are a big challenge for the orthopedic surgeon because the different ages of pediatrics are associated with a difference in bone healing and bone deformity remodeling(3-6). Closed reduction with hip spica application, delayed hip spica following traction, elastic intramedullary nailing(Fig. 1), open or bridge plating (BP) and external fixators(Fig. 2) are the major methods of treatment of these fractures(7). There is still no consensus regarding the age between 6 and 14; many surgeons prefer to use intramedullary flexible nails in closed fractures or external fixation in open fractures (3,5). Some authors propose elastic nails supplemented with an external fixator for the initial 4 weeks after surgical, can maintain the length as well as alignment till union (7). Our study aims to compare a new concept and Surgical Technique(Fig. 3) “Intramedullary titanium nail Osteosynthesis Linked External-fixator (IOLE)” and the two most used surgical treatment external fixation(EF) and titanium elastic nail (TEN) for pediatric’s femoral shaft fracture.
Fig. 1:
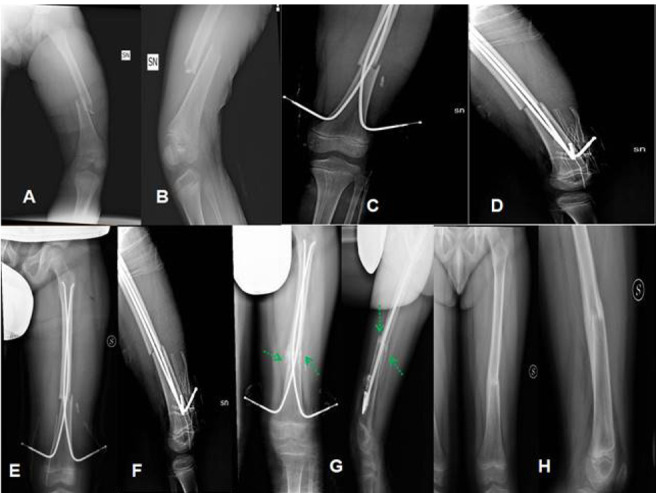
9-year-old child fell from the scooter, diaphyseal fracture of the left femur 33.A3 according to AO (Fig. 1 A and B). Emergency treatment with two Eiffel Tower TENs (Fig. 1 C and D). Radiographic control after 1 month of plaster immobilization after surgical intervention does not callus bone (Fig. 1 E and F). X-ray inspection (Fig. 1G) 3 months after surgery, bone Callus formation (green arrows). Radiographic check at 2 months after the removal of the wires, 115 days after the operation (Fig. 1H).
Fig. 2:
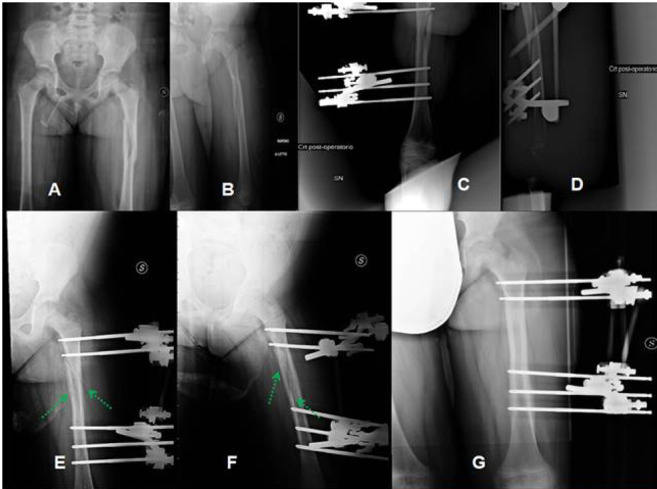
A 6-year-old girl, obese, fallen from a bicycle, reports a fracture of type 33.B2 according to AO (Fig. 2 A and B). Rx Control after surgery with External Fixation (Fig. 2 C and D). A l RX 1 month after surgery (Fig. 2 E and F) good bone callus formation (green arrows). Figure 2G shows the complete healing and restitutio ad integrum of the biomechanical and anatomic axis of the femur.
Fig. 3:
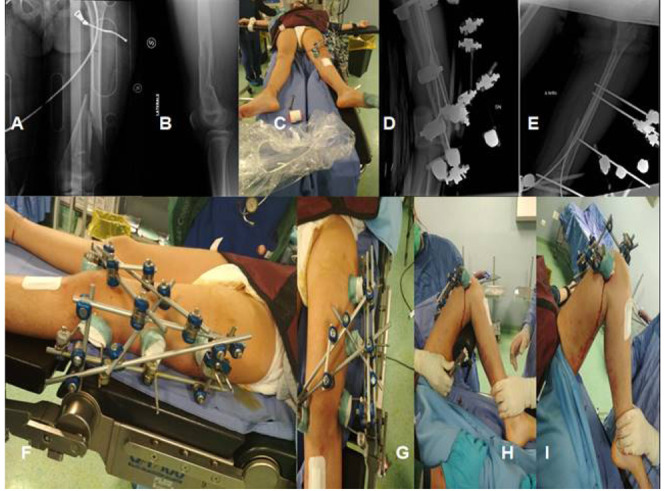
12-year-old girl, car accident, fracture 33.C3 according to AO (Fig. 3 A and B). Photo of the patient treated with IOLE technique on the operating table (Fig. 3C). Postoperative RX Control (Fig. 3 D and E). Plant details (Fig. 3 F and G) showing the hybridization of TENs with the Hoffman II® external fixator. The Fig. 3G and 3H show the possibility of moving the knee passively without problems.
Materials and Methods
From a total of 117 patients, we included 58 pediatric patients with femoral shaft fractures after using the following exclusion criteria: hematological or oncological patients; acute or chronicle local and systemic infections; previous lower limb trauma; bilateral lower injures; nerve injuries; vessels injuries; not 3.2 fracture according to AO (8); age under 6 yeard old or over 14 years old; plate or cast treatment, bone metabolism diseases, mental or neurologic disorder.
All fractures were classified according to AO classification (8). The enrolled patients were described in Table 1; We divided the 58 patients into three groups: 22 patients treated with TEN; 22 patients treated with EF and 14 patients treated with IOLE.
Tab. 1:
Description of the three populations.
| Description of population | TEN | EF | IOLE |
| Number of Patients | 22 | 22 | 14 |
| Average of age (SD) | 7.23 (±0.63) | 9.37(±0.57) | 11.54(±1.32) |
| Range of age | 6-14 | 6-14 | 6-14 |
| Gender Ratio (m:f) | 1.2(12:10) | 1.2(12:10) | 1.28(9:7) |
| Type of Accident | Bike: 6(27.27%) Skate: 8(36.37%) Care Accident: 1(4.54%) Inflatable: 3 (13.64%) Trampolines: 3(13.64%) Domestic Violence: 1(4.54%) |
Bike: 6(27.27%) Skate: 8(36.37%) Care Accident: 1(4.54%) Inflatable: 3 (13.64%) Trampolines: 3(13.64%) Domestic Violence: 1(4.54%) |
Bike: 4 (28.57%) Skate: 4 (28.57%) Care Accident: 2(14.28%) Inflatable: 2 (14.18%) Trampolines: 1(7.15%) Domestic Violence: 1(7.15%) |
| Femoral Shaft Fractures According AO[8] | A1: 2(9.09%) A2:2(9.09%) A3:5(22.73%) B1:2(9.09%) B2:2(9.09%) B3:2(09.09%) C1:3(13.64%) C2:2(9.09%) C3:2(9.09%) |
A1: 2(9.09%) A2:2(9.09%) A3:5(22.73%) B1:2(9.09%) B2:2(9.09%) B3:2(13.64%) C1:3(9.09%) C2:2(9.09%) C3:2(9.09%) |
A1: 2(14.28%) A2:2(14.28%) A3:1(7.15%) B1:2(14.25%) B2:1(7.15%) B3:2(14.28%) C1:1(7.15%) C2:1(7.15%) C3:2(14.28%) |
| Injured Upper Limb Side | Right: 10(45.46%) Left: 12(54.54%) |
Right: 12(54.54%) Left: 10(45.46%) |
Right: 4(28.57%) Left: 10(71.43%) |
| Average Non Union Scoring System(SD) | 3.34(±0.74) | 3.67(±0.79) | 5.5(±1.23) |
| Range Non Union Scoring system | 1-15 | 1-15 | 1-15 |
All the parents of the patients were informed clearly and comprehensively of the type of treatment (See IOLE Operative Surgical Technique) and other possible surgical and conservative alternatives. Patients were treated according to the ethical standards of the Helsinki Declaration and were invited to read, understand, and sign the informed consent form.
All patients underwent the same rehabilitation protocol (see rehabilitation protocol). To study the bone healing on radiographs, we used the Non-Union Scoring System (NUSS) in retrospective mode (Table 1) (9).
The criteria to evaluate the patient’s groups during the follow-up were: the mean follows up; the duration of surgery; Pain visual analogic score (VAS) was collected the same day that the X-rays were taken(10); objective quality of life and the hip function measured by the modified Harris Hip Score (HHS)(11), the subjective quality of life and the knee function measured by Knee Society Score (KSS)(12). The quality of life measured by the Pediatric Quality of Life Inventory (PedsQL) 4.0(13). The bone healing and femoral alignment were measured using X-rays. Bone union was measured using the radiographic union score as described by Litrenta et al (14). The intermediate evaluation endpoints were: post-operative, 1 month, 3 months, 6 months from the surgery. The final evaluation endpoint was set at 12 months after surgery.
Statistical Analysis
Descriptive statistics were used to summarize the characteristics of the study group and subgroups, including means and standard deviations of all continuous variables. The t-test was used to compare continuous outcomes. The Chi-square test or Fisher’s exact test (in subgroups smaller than 10 patients) were used to compare categorical variables. The statistical significance was defined as P < 0.05. We used Pearson correlation coefficient (r) was used to compare the predictive score of outcomes and quality of life. Mean ages (and their range) of the patients were rounded at the closest year. The predictive score of outcomes and quality of life and their ranges were approximated at the first decimal while at the second decimal was approximated Pearson correlation coefficient (r).
Cohen's kappa coefficient (κ) is a statistic that measures inter-rater agreement for qualitative (categorical) items. We through this parameter we calculated the concordance between different qualitative values of the outcomes and the bone healing, the anatomical and biomechanical axis of the humerus from the radiological point of view.
IOLE Surgical Technique
The patient is placed supine on a transparent radio bed with the knee flexed at 20 ° with a support under the popliteal cord (Fig. 3H). For first we implant the two TENs were implanted Eiffel’s tower starting from 1 cm above the physis of the medial femoral epicondyle and then the lateral one always at 1 cm from the lateral epicondyle (Fig 3 E, F, and G). Both wires must exceed 10 cm from the fracture site and at least 1 cm be anchored to the small trochanter (Fig 3 D and F). After, all patients were treated with the Stryker™ Hoffman II® modular fixator, with the configuration of two proximal and one in the middle and one distal parallel to the physiological and supracondylar physis(Fig 3 E, F, and G), reduced and stabilized the fracture in three dimensions with the external fixator, After doing this the two wires are hybridized to the external fixator with two Fiches-Bar clamps and the knee flexion test with(Fig. 3H) or without(Fig. 3I) subplot thickness(Fig. 4).
Fig. 4:
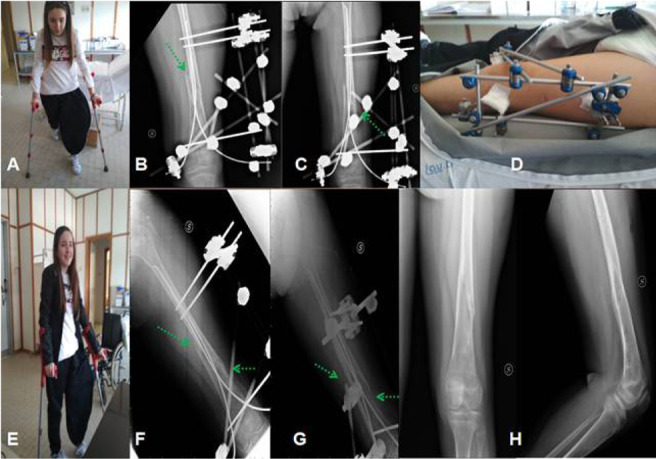
Image 4A shows the patient starting loading at 4 weeks, while radiographic images 4B and 4C show the initial presence of bone callus (green arrows). Image 4 D shows the removal of the neutralization bars and middle screw to allow system derigidification and total load already from the 5th week. Photo 4E shows the patient with a total load of 3 months, the radiographs show the presence of the abbonant callus bone (Fig. 4F and 4G). The hardware was removed 125 days after surgery, photo 4H shows healing 12 months after surgery.
Rehabilitation Protocol
The purpose of our protocol is to provide the clinician with an orientation of the postoperative course of rehabilitation, to rationalize and to have the whole patient population conform to a single physiotherapy program.
Week 1-3
During the first three postoperative weeks, the patients wore a resin cast from the lesser trochanter to the foot in TEN group with Knee flexed at 20 degrees. EF and IOLE groups sudden start the flexion of from 0° to 90° and 10% of weight body bearing.
Week 4-6
After the first three weeks, the patient received a weight-bearing.
- Week 4: partial weight-bearing, up to 10%, and ROM’s hip and knee 0°-90°.
- Week 5: partial weight-bearing, up to 20%, and ROM’s hip and knee 0°-100°.
- Week 6: partial weight-bearing, up to 35%, and ROM’s hip and knee 0°-105°.
Strengthening Program
Single plane active ROM hip and knee flexion-extension, isometric work.
Week 7-11
- Week 7: partial weight-bearing, up to 40%, and hip and knee’s full ROM
- Week 8: partial weight-bearing, up to 50%, and hip and knee’s full ROM
- Week 9: partial weight-bearing, up to 70%, and hip and knee’s full ROM
- Week 10: partial weight-bearing, up to 80%, and hip and knee’s full ROM
- Week 11: partial weight-bearing, up to 85%, and hip and knee’s full ROM
Full range of motion of the hip and knee;
If at 8 weeks post-operatively the patient has a significant range of motion deficits, the therapist may consider more aggressive management after consultation with the referring surgeon.
Strengthening Program
A progressive active-resistance exercise program for hip and knee flexion-extension, isometric work.
Week 12 until the hardware removal
The patient may initiate a lower extremity weight training until the hardware removal.
Strengthening program
Initiation of endurance program that simulates desired work activities/requirements.
Stimulation of hip and knee range of motion, strength, and coordination.
Results
The mean of follow-up was 14.26 (±0.46; range 12–24) months for TEN while 14.23 (±0.51; range 12–24) months for EF and 14.18 (±0.39; range 12–24) months for IOLE, p>0.05.
The surgery duration was an average of 36.8 (±12.4; range 12-65) minutes in TEN while 38.9 (±13.7; range 15-63) minutes for EF and 41.9 (±13.7; range 36-71) minutes for IOLE, p>0.05.
The average time of bone healing was 138.7 (±15.7; 62-156) days after the surgery in TEN while 139.8 (±14.4; 72 -152) days for EF and 127.8(±15.7; 68-152) for IOLE, p>0.05.
An average day of the bone healing the RUSH was 25.9 (±2.8; range 23.8-30) point in TEN while 26.6 (±2.7; range 24.6-30) in EF and 28.2 (±1.5; range 27.4-30) for IOLE, p<0.05 for IOLE.
At the average day of the bone healing the VAS was of 0.6 (±0.1; range 0-2) point in TEN while 0.7 (±0.1; range 0-2) in EF while 0.8(±0.2; range 0-2) for IOLE, p>0.05
We found that on an average day of bone healing the regression between RUSH and VAS scores showed a p value of 0.059 in TEN while p= 0.061 in EF and p=0.072 in IOLE, p>0.05.
The average time of hardware removal was 158.7 (±15.7; 82-176) days after the surgery in TEN while 159.8 (±14.4; 92 -172) days for EF and 147.8(±15.7; 88-172) for IOLE, p>0.05.
In comparing the complications of the three populations, we only did find a statistically significant difference: in malalignment varus/valgus; antecurvatus/recurvatus; and total complications for IOLE group. IOLE group had fewer complications than the other two groups (Table 2).
Tab. 2:
In comparing the results of the three populations, we only did find a statistically significant difference(*) in mal alignment and in total complication for IOLE.
| Complicarions | TEN | EF | IOLE | P Value |
| Loss of distal Locking | 0 | 0 | 0 | P=1 |
| Breakage or mobilization of Hardaware Orthopedics Device | 0 | 0 | 0 | P=1 |
| Blood Loss >2.5 gr/dl Hb | 2(9.09%)* | 2(09.09%)* | 1(7.15%) | P>0.05 |
| Mal Aligment Varus/Valgus>15° | 1(4.54%) | 1(4.54%) | 0* | P<0.05 |
| Mal Aligment in Pro Curvatus/Retrocurvatus <15° | 1(4.54%) | 1(4.54%) | 0* | P<0.05 |
| Rotational Union | 1(4.54%) | 0 | 0 | P=1 |
| Eterometria (<2cm) | 3(13.64%) | 3(13.64%) | 2(14.28%) | P>0.05 |
| Skin Infection | 1(4.54%) | 2(9.09%) | 1(7.15%) | P=1 |
| Deep Infection | 0 | 0 | 0 | P=1 |
| Pain Insertion Site | 1(4.54%) | 0 | 0 | P>0.05 |
| Total | 10(45.46%) | 9(40.9%) | 4(28.57%)* | P<0.05 |
In the three groups, patients demonstrated wound healing within 15 days after the remotion of the hardware.
At the Trend of Harris Hip Score (HHS) before and at 1 year after the second stage revision surgery event. There was not a statistically differences at before the trauma and evaluative endpoint. The Ten groups have the worst outcomesat the first and the third months after surgery, (p<0.05).
The trend of Knee Society Score (KSS) before and at 1 year after the second stage revision surgery event. There was not a statistically differences at before the trauma and evaluative endpoint. The Ten groups have the worst outcomes at the first and the third months after surgery, (p<0.05).
The trend of Subjective quality of life measured by Pediatric Quality of Life Inventory (PedsQL) 4.0 before the trauma and at 1 year after the surgery. There were no statistical differences(p>0.05) before the trauma and evaluative endpoint. The Ten groups have the worst outcomes at the first and the third months after surgery, (p<0.05). The worst results were due to the psychological and scholar subgroups.
The Average Correlation clinical-radiographic results and patients outcomes were high according to Cohen κ: 0,830618182± 0,082479for Ten while 0,828416875±0,098097 for EF and 0,882465± 0,07896 for IOLE there were statistical differences between the two groups, p<0.05 for IOLE.
Discussion
Fractures of the pediatric age have a high remodeling capacity and therefore usually have a good prognosis. The treatment of these fractures in children and adolescents depends on various factors including age and weight, fracture characteristics, surgeon preferences, social situation and compliance of the family and any comorbidities (15). The goal of treatment is to restore the normal functionality of the limb in the shortest possible time; the most frequent complications are nonunion, malunion, stiffness in the knee, and refracture (16).
The different treatment options include spica cast, synthesis with TEN, synthesis with plate, external fixation and synthesis with intramedullary rigid nails; each of these treatment methods with its own advantages and disadvantages (15).
Historically these fractures have been treated conservatively in younger children (5-10 years), however, spica casting treatment had many disadvantages including loss of reduction, skin lesions, and nerve palsies. In addition, spica casting was found to have longer healing times, a higher rate of malunion, higher hospital costs, as well as a slower return to normal life. For this reason, the surgical treatment of these fractures in children over 5 years of age has seen a 2-fold increase over the past 20 years. Flynn (17) in a study of 86 patients between 6 and 12 years of age confused the treatment with spica cast and the synthesis with ten obtaining significantly better results in terms of shortening, fracture angle and healing time in patients treated with ten.
Nowadays, fractures of the femoral shaft in children under 5 years are treated with spica casting and in children over 12 years with rigid intramedullary nailing; therefore, the problem of which is the best treatment option arises in the age group between 5 and 12 years, where there is currently no consensus on which is the best treatment.
The reduction and immobilization of these fractures with a cast spica is currently the gold standard in patients aged up to 5 years. The main disadvantages of this method are a shortening of the unacceptable limb (greater than 25 mm), and an angle beyond the acceptable limits. As regards the acceptable angle in patients up to 2 years of age, an angle of up to 30 ° is accepted in both the sagittal and coronal plane, between 2 and 5 years an angle of <20 ° on the sagittal plane and <15 ° on the Coronal plane, between 5 and 10 years an angle <10 ° on the coronal plane and <15 ° on the sagittal plane is acceptable. (18,19); in cases where the angle is not acceptable, it is necessary to remake a plaster by changing the alignment or switch to another synthesis technique such as tens, plate synthesis or external fixation (20).
Problems with TENS are: pain at insertion site near the knee in up to 40% of patients; increased rate of complications in patients 11 years or up or > 50 kg; malunion increased rates with comminuted, shortened, or very proximal/distal fractures(3).
Problems with EF are more complications than internal fixation; pin tract infections are frequent; higher rates of delayed union, nonunion and malunion; and increased risk of refracture (1.5-21%) after removal of fixator especially with varus malunion (3).
Synthesis with TEN is the most used treatment method in children aged between 6 and 15 years. In this age group, it is important that the patient can move the limb freely for the duration of the treatment. Furthermore, the early return of the child to his social environment is very important in terms of psychosocial development. In the TEN surgical technique, described by the “Nancy team”, the nail is chosen by measuring 40% of the narrowest diameter of the femoral canal. From a biomechanical point of view, TEN is a stable elastic intramedullary nail which is based on the principle of three-point fixation resisting the distraction and compression forces. The main disadvantage of TENs is that a plaster must be applied, and immediate loading cannot be granted. (21,22).
Among the disadvantages of this technique, we must consider a high learning curve, a prolonged exposure to X-rays for both the patient and the surgeon, the need for a second intervention for the removal of the TENs, and sometimes the need for a second method additional stabilization, especially in fractures of the distal femur. Rapp (23), in a study of 112 Tens cases, in 13 cases had to modify the synthesis or add an external fixator for problems of insufficient stability of the synthesis
Synthesis with plate is another treatment option for this type of fracture, but is rarely used due to the risk of infection, delayed union and non-union; moreover, extensive tissue dissection is required, and a second surgery is always required to remove it. Furthermore, it very often gives rise to a substantial scar which can be a problem in some children. (25,26).
Regarding external fixation, previous studies report various complications related to its use including delayed or non-union, refracture, deep pin tract infection (27,28,29). However, improvements in the technique of external fixation have allowed to minimize these complications, including Hydroxyapatite-coated half pins, reducing the risk of thermal necrosis with pre-drill, with the use of oral antibiotics to reduce the risk of infection, with the possibility of dynamizing the fixator (30).
Generally, external fixation has the advantage of very limited soft tissue dissection, small scars, relatively short surgical time and early mobilization and are associated with a low rate of major complications (31). Besides, external fixation does not increase periosteal damage and the fracture hematoma remains intact. Therefore, this method does not interfere with the bone healing process, in which the large sub periosteal hematoma and the abundant thickness of the periosteum play an important role, contributing to a rapid healing of the fracture (32,33).
In this study we revised 58 patients with a diaphyseal femoral fracture in retrospective way, the treatment of fracture: TENS, F.E., or IOLE is dependent on different factors, such as the age of the patient, the type of fracture, the compliance of the patient and the family, the general clinical conditions.
We did not find statistically significant differences between the three techniques as regards the duration of the surgery and the average time of bone healing, however the IOLE technique proved superior in terms of fracture alignment and early weigh bearing.
The advantage of the IOLE technique is to associate the biomechanics of TENs that resist well to bending forces, however they do not oppose rotational forces equally well, to external fixation which instead allows to control very well the rotational and shear forces.
Besides, by combining the two synthesis techniques, we allowed the children partial load starting from the first post-operative day, with less hospitalization time, early recovery of muscle strength and proprioception, faster recovery to daily life.
In conclusion, in our opinion, the Bisaccia and Meccariello (IOLE) technique, if well used and well indicated, allows an early weigh bearing of the operated limb, with a lower risk of malunion without an increase in other complications. The main limitation of our study is the limited number of patients; further research is needed to confirm the advantage of this technique.
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Flynn John M, Schwend Richard M. Management of pediatric femoral shaft fractures. J Am Acad Orthop Surg. 2004;12:347–359. doi: 10.5435/00124635-200409000-00009. [DOI] [PubMed] [Google Scholar]
- Petković L, Djan I, Gajdobranski D, Marić D, Petković M. Pediatric femur fractures, epidemiology and treatment. Vojnosanit Pregl. 2011;68(1):9–14. doi: 10.2298/vsp1101009p. [DOI] [PubMed] [Google Scholar]
- Rollo G, Guida P, Bisaccia M, et al. TEN versus external fixator in the management of pediatric diaphyseal femoral fractures: evaluation of the outcomes. Eur J Orthop Surg Traumatol. 2018;28(7):1421–1428. doi: 10.1007/s00590-018-2201-3. doi: 10.1007/s00590-018-2201-3. [DOI] [PubMed] [Google Scholar]
- Kong H, Sabharwal S. External fixation for closed pediatric femoral shaft fractures: where are we now? Clin Orthop Relat Res. 2014;472(12):3814–3822. doi: 10.1007/s11999-014-3554-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berne D, Mary P, Damsin JP, Filipe G. Femoral shaft fracture in children: treatment with early spica cast. Rev Chir Orthop Reparatrice Appar Mot. 2003;89(7):599–604. [PubMed] [Google Scholar]
- Kosuge D, Barry M. Changing trends in the management of children’s fractures. Bone Joint J. 2015;97-B(4):442–448. doi: 10.1302/0301-620X.97B4.34723. [DOI] [PubMed] [Google Scholar]
- Dey S, Mishra K, Nagda TV, Dhamele J, Rathod C, Dey D. Titanium Elastic Nailing with Temporary External Fixator versus Bridge Plating in Comminuted Pediatric Femoral Shaft Fractures: A Comparative Study. Indian J Orthop. 2018;52(5):507–512. doi: 10.4103/ortho.IJOrtho_304_17. doi: 10.4103/ortho.IJOrtho_304_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slongo TF, Audigé L AO Pediatric Classification Group. Fracture and dislocation classification compendium for children: the AO pediatric comprehensive classification of long bone fractures (PCCF) J Orthop Trauma. 2007;21(10 Suppl):S135–60. doi: 10.1097/00005131-200711101-00020. [DOI] [PubMed] [Google Scholar]
- Calori GM, Colombo M, Mazza EL, Mazzola S, Malagoli E, Marelli N, Corradi A. Validation of the Non-Union Scoring System in 300 long bone non-unions. Injury. 2014;45(Suppl 6):S93–7. doi: 10.1016/j.injury.2014.10.030. doi: 10.1016/j.injury.2014.10.030. [DOI] [PubMed] [Google Scholar]
- Maiettini D, Bisaccia M, Caraffa A, et al. Feasibility and Value of Radiographic Union Score Hip Fracture after Treatment with Intramedullary Nail of Stable Hip Fractures. Acta Inform Med. 2016;24(6):394–396. doi: 10.5455/aim.2016.24.394-396. doi: 10.5455/aim.2016.24.394-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d’Entremont AG, Cooper AP, Johari A, Mulpuri K. What clinimetric evidence exists for using hip-specific patient-reported outcome measures in pediatric hip impingement? Clin Orthop Relat Res. 2015;473(4):1361–7. doi: 10.1007/s11999-014-4027-6. doi: 10.1007/s11999-014-4027-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su Y, Nan G. ORIF with percutaneous cross pinning via the posterior approach for paediatric widely displaced supracondylar femoral fractures. Injur. 2016;47(6):1242–7. doi: 10.1016/j.injury.2016.02.024. doi: 10.1016/j.injury.2016.02.024. [DOI] [PubMed] [Google Scholar]
- Hullmann SE, Ryan JL, Ramsey RR, Chaney JM, Mullins LL. Measures of general pediatric quality of life: Child Health Questionnaire (CHQ), DISABKIDS Chronic Generic Measure (DCGM), KINDL-R, Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales, and Quality of My Life Questionnaire (QoML) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S420–30. doi: 10.1002/acr.20637. doi: 10.1002/acr.20637. [DOI] [PubMed] [Google Scholar]
- Litrenta J, Tornetta P 3rd, Mehta S, et al. Determination of radiographic healing: an assessment of consistency using RUST and modified RUST in metadiaphyseal fractures. J Orthop Trauma. 2015;29(11):516–20. doi: 10.1097/BOT.0000000000000390. doi: 10.1097/BOT.0000000000000390. [DOI] [PubMed] [Google Scholar]
- Naranje SM, Stewart MG, Kelly DM, Jones TL, Spence DD, Warner WC Jr, Beaty JH, Sawyer JR. Changes in the Treatment of Pediatric Femoral Fractures: 15-Year Trends From United States Kids’ Inpatient Database (KID) 1997 to 2012. J Pediatr Orthop. 2016;36(7):e81–5. doi: 10.1097/BPO.0000000000000633. doi: 10.1097/BPO.0000000000000633. [DOI] [PubMed] [Google Scholar]
- Sigrist EJ, George NE, Koder AM, Gwam CU, Etcheson JI, Herman MJ. Treatment of Closed Femoral Shaft Fractures in Children Aged 6 to 10. J Pediatr Orthop. 2019;39(5):e355–e359. doi: 10.1097/BPO.0000000000001310. doi: 10.1097/BPO.0000000000001310. [DOI] [PubMed] [Google Scholar]
- Flynn JM, Luedtke LM, Ganley TJ, et al. Comparison of titanium elastic nails with traction and a spica cast to treat femoral fractures in children. J Bone Joint Surg Am. 2004 Apr;86-A(4):770–7. doi: 10.2106/00004623-200404000-00015. [DOI] [PubMed] [Google Scholar]
- Sargent MC. Single-Leg Spica Cast Application for Treatment of Pediatric Femoral Fracture. JBJS Essent Surg Tech. 2017 Sep 13;7(3):e26. doi: 10.2106/JBJS.ST.15.00070. doi: 10.2106/JBJS.ST.15.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alluri RK, Sabour A, Heckmann N, Hatch GF, Vanden Berg C. Increasing Rate of Surgical Fixation in Four-and Five-year-old Children With Femoral Shaft Fractures. J Am Acad Orthop Surg. 2019 Jan 1;27(1):e24–e32. doi: 10.5435/JAAOS-D-17-00064. doi: 10.5435/JAAOS-D-17-00064. [DOI] [PubMed] [Google Scholar]
- Rickert KD, Hosseinzadeh P, Edmonds EW. What’s New in Pediatric Orthopaedic Trauma: The Lower Extremity. J Pediatr Orthop. 2018;38(8):e434–e439. doi: 10.1097/BPO.0000000000001209. doi: 10.1097/BPO.0000000000001209. [DOI] [PubMed] [Google Scholar]
- Ligier JN, Metaizeau JP, Prévot J, Lascombes P. Elastic stable intramedullary nailing of femoral shaft fractures in children. J Bone Joint Surg Br. 1988 Jan;70(1):74–7. doi: 10.1302/0301-620X.70B1.3339064. [DOI] [PubMed] [Google Scholar]
- Imam MA, Negida AS, Elgebaly A, et al. Titanium Elastic Nails Versus Spica Cast in Pediatric Femoral Shaft Fractures: A Systematic Review and Meta-analysis of 1012 Patients. Arch Bone Jt Surg. 2018;6(3):176–188. [PMC free article] [PubMed] [Google Scholar]
- Rapp M, Kaiser MM, Grauel F, Gielok C, Illing P. Femoral shaft fractures in young children (<5 years of age): operative and non-operative treatments in clinical practice. Eur J Trauma Emerg Surg. 2016;42(6):719–724. doi: 10.1007/s00068-015-0570-4. [DOI] [PubMed] [Google Scholar]
- Sink EL, Gralla J, Repine M. Complications of pediatric femur fractures treated with titanium elastic nails: a comparison of fracture types. J Pediatr Orthop. 2005;25(5):577–80. doi: 10.1097/01.bpo.0000164872.44195.4f. [DOI] [PubMed] [Google Scholar]
- Brousil J, Hunter JB. Femoral fractures in children. Curr Opin Pediatr. 2013;25(1):52–7. doi: 10.1097/MOP.0b013e32835c20e0. doi: 10.1097/MOP.0b013 e32835c20e0. [DOI] [PubMed] [Google Scholar]
- Caird MS, Mueller KA, Puryear A, Farley FA. Compression plating of pediatric femoral shaft fractures. J Pediatr Orthop. 2003;23(4):448–52. [PubMed] [Google Scholar]
- de Sanctis N, Gambardella A, Pempinello C, Mallano P, Della Corte S. The use of external fixators in femur fractures in children. J Pediatr Orthop. 1996;16(5):613–20. doi: 10.1097/00004694-199609000-00013. [DOI] [PubMed] [Google Scholar]
- Blasier RD, Aronson J, Tursky EA. External fixation of pediatric femur fractures. J Pediatr Orthop. 1997;17(3):342–6. [PubMed] [Google Scholar]
- Hinton RY, Lincoln A, Crockett MM, Sponseller P, Smith G. Fractures of the femoral shaft in children. Incidence, mechanisms, and sociodemographic risk factors. J Bone Joint Surg Am. 1999;81(4):500–9. doi: 10.2106/00004623-199904000-00007. [DOI] [PubMed] [Google Scholar]
- Sabharwal S, Kishan S, Behrens F. Principles of external fixation of the femur. Am J Orthop (Belle Mead NJ) 2005;34(5):218–23. [PubMed] [Google Scholar]
- Zhang YT, Jin D, Niu J, Li ZJ, Fu S, Zou ZL. A meta-analysis of external fixation andflexible intramedullary nails for femoral fractures in children. Acta Orthop Belg. 2016;82(4):673–680. [PubMed] [Google Scholar]
- Guo YC, Feng GM, Xing GW, et al. A meta-analysis of flexible intramedullary nailing versus external fixation for pediatric femoral shaft fractures. J Pediatr Orthop B. 2016;25(5):466–70. doi: 10.1097/BPB.0000000000000336. doi: 10.1097/BPB.0000000000000336. [DOI] [PubMed] [Google Scholar]
- Wani MM, Rashid M, Dar RA, et al. Use of external fixator versus flexible intramedullary nailing in closed pediatric femur fractures: comparing results using data from two cohort studies. Eur J Orthop Surg Traumatol. 2016;26(2):223–30. doi: 10.1007/s00590-015-1737-8. doi: 10.1007/s00590-015-1737-8. [DOI] [PubMed] [Google Scholar]


