To the Editor,
Measles and influenza are acute viral, airborne, vaccine-preventable diseases (as COVID-19) that still represent a major public health concern (1, 2). Indeed, despite the availability of safety and effective vaccines, vaccination coverage for both influenza and measles is below the recommended threshold, causing high diseases’ burden and recurrent epidemics. Moreover, there is an elimination plan for measles and influenza share a similar symptomatology with COVID-19. Lastly, for both diseases there are efficient surveillance systems available in Europe. Because of all the above-mentioned aspects, we analyzed the number of cases of measles and influenza positivity retrieved from the Surveillance Atlas of Infectious Diseases tool freely available from the European Centre for Disease Prevention and Control (ECDC) website (https://www.ecdc.europa.eu/en/surveillance-atlas-infectious-diseases), in order to assess any differences in time. For the current investigation, the study period ranged between 1st January 2017 and 31st December 2020 for measles and between first week of 2017 and nineth week of 2021 for influenza. Data from European Union (EU) countries were analysed for measles. Whereas, for influenza, data from United Kingdom were also available. For the five countries (Italy, France, Romania, Greece and Germany) with the highest number of measles cases registered during the last 4 years, the related linear regression equations and the R-squared were calculated. The mean incidences of measles cases were calculated.
Figure 1 shows the European epidemic curve of measles, for the period 2017-2020. Data are shown on a monthly bases for each of the included European countries. Until March 2020, surveillance data confirms the classical cyclical pattern of measles spread, with the highest number of measles cases, registered in the bimester March-April. The remaining months show a relatively low and constant number of cases (approximately one hundred). This classical pattern was not confirmed in 2020, when the number of cases dramatically dropped down. Indeed, from March 2020 many European countries reported zero measles cases. Similar results are also reported for influenza. Figure 2 shows the well-known seasonality pattern of influenza according to which infections starts to increase from November (usually the 47th week of the year) reaching the epidemic peak in February (third week) of the following year. This expected trend was not observed in 2020-2021 when the epidemic curve was flattened. The average incidence of cases in Europe with regard to measles (Figure 3) has a maximum value in 2019 (37.51 cases per million inhabitants) and a minimum value in 2020 (4.24 cases per million inhabitants). Figure 4 shows an important reduction of measles cases in the 5 countries with the highest number of cases registered between 2017 and 2019. The linear regression equations representing these 5 curves have a negative angular coefficient, confirming the impressive cases reduction. In the same direction data collected using the INFLUNET surveillance system (Italian system for influenza), according to which in 2020-2021 there were 1.49 cases per 1.000 inhabitants of influenza like cases, however, none of the samples were flu positive(3).
Figure 1.

Trend in the number of measles cases in European countries from January 2017 to December 2020
Figure 2.

Flu positivity in Europe from first week of 2017 to nineth week of 2021
Figure 3.
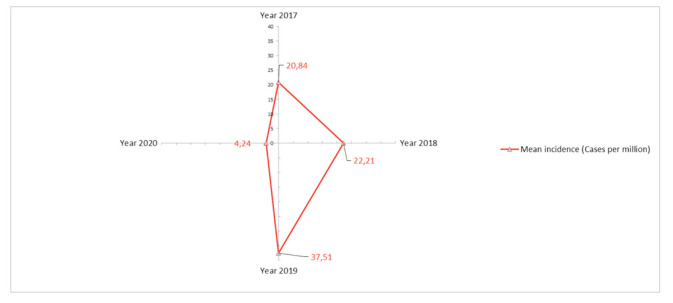
Mean incidence of measles cases in Europe in the 2017-2020 study period.
Figure 4.

Comparison between the 5 Countries with the most cases in the last 4 years of the study period and related linear regression equations.
Based on our data we can speculate that containment measures adopted to prevent COVID-19 spread strongly prevented also other airborne diseases, since the epidemic trend usually observed was not confirmed in 2020-2021. Someone can argue that this reduction is instead due to under-notification. This can be a concurrent event, particularly considering the overload on the whole health care system due to COVID-19(4). However, for both the diseases all the European countries registered a significant and concordant trend reduction. Lastly, we can also speculate that wearing facing mask, frequently washing hands and keep the social distance were much more effective in preventive other infectious diseases compared to COVID-19. This aspect stresses the high transmission rate of COVID-19, probably higher compared to what estimated, especially considering that the estimated basic reproduction rate (R0) of measles is 14, six-time higher compared to COVID-19(5). This data also confirms the importance of a timely massive vaccination campaign for COVID-19 in order to significantly reduce the virus circulation.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- Gianfredi V, Moretti M, Fusco Moffa I. Burden of measles using disability-adjusted life years, Umbria 2013-2018. Acta Biomed. 2020;91(3-S):48–54. doi: 10.23750/abm.v91i3-S.9412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianfredi V, Santangelo OE, Provenzano S. Correlation between flu and Wikipedia’s pages visualization. Acta Biomed. 2021;92(1):e2021056. doi: 10.23750/abm.v92i1.9790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sistema di Sorveglianza Integrata dell’Influenza - Istituto Superiore di Sanità. Rapporto INFLUNET. Aggiornamento del 25 marzo 2021 Rome2021 [Available from: https://w3.iss.it/site/RMI/influnet/pagine/rapportoInflunet.aspx. [Google Scholar]
- Signorelli C, Odone A, Gianfredi V, Bossi E, Bucci D, Oradini-Alacreu A, et al. COVID-19 mortality rate in nine high-income metropolitan regions. Acta Biomed. 2020;91(9-S):7–18. doi: 10.23750/abm.v91i9-S.10134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Gayle AA, Wilder-Smith A, Rocklov J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020;27(2) doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]


