Abstract
Background
The global burden of poor maternal, neonatal, and child health (MNCH) accounts for more than a quarter of healthy years of life lost worldwide. Targeted client communication (TCC) via mobile devices (MD) (TCCMD) may be a useful strategy to improve MNCH.
Objectives
To assess the effects of TCC via MD on health behaviour, service use, health, and well‐being for MNCH.
Search methods
In July/August 2017, we searched five databases including The Cochrane Central Register of Controlled Trials, MEDLINE and Embase. We also searched two trial registries. A search update was carried out in July 2019 and potentially relevant studies are awaiting classification.
Selection criteria
We included randomised controlled trials that assessed TCC via MD to improve MNCH behaviour, service use, health, and well‐being. Eligible comparators were usual care/no intervention, non‐digital TCC, and digital non‐targeted client communication.
Data collection and analysis
We used standard methodological procedures recommended by Cochrane, although data extraction and risk of bias assessments were carried out by one person only and cross‐checked by a second.
Main results
We included 27 trials (17,463 participants). Trial populations were: pregnant and postpartum women (11 trials conducted in low‐, middle‐ or high‐income countries (LMHIC); pregnant and postpartum women living with HIV (three trials carried out in one lower middle‐income country); and parents of children under the age of five years (13 trials conducted in LMHIC). Most interventions (18) were delivered via text messages alone, one was delivered through voice calls only, and the rest were delivered through combinations of different communication channels, such as multimedia messages and voice calls.
Pregnant and postpartum women
TCCMD versus standard care
For behaviours, TCCMD may increase exclusive breastfeeding in settings where rates of exclusive breastfeeding are less common (risk ratio (RR) 1.30, 95% confidence intervals (CI) 1.06 to 1.59; low‐certainty evidence), but have little or no effect in settings where almost all women breastfeed (low‐certainty evidence). For use of health services, TCCMD may increase antenatal appointment attendance (odds ratio (OR) 1.54, 95% CI 0.80 to 2.96; low‐certainty evidence); however, the CI encompasses both benefit and harm. The intervention may increase skilled attendants at birth in settings where a lack of skilled attendants at birth is common (though this differed by urban/rural residence), but may make no difference in settings where almost all women already have a skilled attendant at birth (OR 1.00, 95% CI 0.34 to 2.94; low‐certainty evidence). There were uncertain effects on maternal and neonatal mortality and morbidity because the certainty of the evidence was assessed as very low.
TCCMD versus non‐digital TCC (e.g. pamphlets)
TCCMD may have little or no effect on exclusive breastfeeding (RR 0.92, 95% CI 0.79 to 1.07; low‐certainty evidence). TCCMD may reduce 'any maternal health problem' (RR 0.19, 95% CI 0.04 to 0.79) and 'any newborn health problem' (RR 0.52, 95% CI 0.25 to 1.06) reported up to 10 days postpartum (low‐certainty evidence), though the CI for the latter includes benefit and harm. The effect on health service use is unknown due to a lack of studies.
TCCMD versus digital non‐targeted communication
No studies reported behavioural, health, or well‐being outcomes for this comparison. For use of health services, there are uncertain effects for the presence of a skilled attendant at birth due to very low‐certainty evidence, and the intervention may make little or no difference to attendance for antenatal influenza vaccination (RR 1.05, 95% CI 0.71 to 1.58), though the CI encompasses both benefit and harm (low‐certainty evidence).
Pregnant and postpartum women living with HIV
TCCMD versus standard care
For behaviours, TCCMD may make little or no difference to maternal and infant adherence to antiretroviral (ARV) therapy (low‐certainty evidence). For health service use, TCC mobile telephone reminders may increase use of antenatal care slightly (mean difference (MD) 1.5, 95% CI –0.36 to 3.36; low‐certainty evidence). The effect on the proportion of births occurring in a health facility is uncertain due to very low‐certainty evidence. For health and well‐being outcomes, there was an uncertain intervention effect on neonatal death or stillbirth, and infant HIV due to very low‐certainty evidence. No studies reported on maternal mortality or morbidity.
TCCMD versus non‐digital TCC
The effect is unknown due to lack of studies reporting this comparison.
TCCMD versus digital non‐targeted communication
TCCMD may increase infant ARV/prevention of mother‐to‐child transmission treatment adherence (RR 1.26, 95% CI 1.07 to 1.48; low‐certainty evidence). The effect on other outcomes is unknown due to lack of studies.
Parents of children aged less than five years
No studies reported on correct treatment, nutritional, or health outcomes.
TCCMD versus standard care
Based on 10 trials, TCCMD may modestly increase health service use (vaccinations and HIV care) (RR 1.21, 95% CI 1.08 to 1.34; low‐certainty evidence); however, the effect estimates varied widely between studies.
TCCMD versus non‐digital TCC
TCCMD may increase attendance for vaccinations (RR 1.13, 95% CI 1.00 to 1.28; low‐certainty evidence), and may make little or no difference to oral hygiene practices (low‐certainty evidence).
TCCMD versus digital non‐targeted communication
TCCMD may reduce attendance for vaccinations, but the CI encompasses both benefit and harm (RR 0.63, 95% CI 0.33 to 1.20; low‐certainty evidence).
No trials in any population reported data on unintended consequences.
Authors' conclusions
The effect of TCCMD for most outcomes is uncertain. There may be improvements for some outcomes using targeted communication but these findings were of low certainty. High‐quality, adequately powered trials and cost‐effectiveness analyses are required to reliably ascertain the effects and relative benefits of TCCMD. Future studies should measure potential unintended consequences, such as partner violence or breaches of confidentiality.
Keywords: Child, Preschool; Female; Humans; Infant; Infant, Newborn; Pregnancy; Breast Feeding; Breast Feeding/statistics & numerical data; Cell Phone; Child Health; Child Health/standards; Child Health/statistics & numerical data; Communication; Delivery, Obstetric; Delivery, Obstetric/standards; Health Behavior; Health Services Needs and Demand; Health Status; HIV Infections; HIV Infections/drug therapy; Infant Health; Infant Health/standards; Infant Health/statistics & numerical data; Maternal Health; Maternal Health/standards; Maternal Health/statistics & numerical data; Medication Adherence; Medication Adherence/statistics & numerical data; Postpartum Period; Prenatal Care; Prenatal Care/statistics & numerical data; Quality Improvement; Randomized Controlled Trials as Topic; Text Messaging
Plain language summary
Communicating to pregnant woman and parents through their mobile devices to improve maternal, neonatal, and child health
Aim of this review
We assessed the effect of sending targeted messages by mobile devices to pregnant women and parents of young children about health and healthcare services.
Key messages
There are gaps in the evidence regarding the effects of targeted messages by mobile devices to pregnant women and parents of young children about health and healthcare services. Some of these messages may improve some people's health and their use of health services, but others may make little or no difference. The existing evidence is mostly of low or very low certainty.
What was studied in the review?
Targeted client communication (TCC) is an intervention in which the health system sends information to particular people, based on their health status or other factors specific to that population group. Common types of TCC are text messages reminding people to attend appointments or that offer healthcare information and support. Our review assessed whether TCC can change pregnant women's and parents' behaviour, health service use, health, and well‐being.
What happens when pregnant women receive targeted messages by mobile device?
Compared to women who get no messages
Women may breastfeed more in settings where exclusive breastfeeding is not common. They may also go to more antenatal care appointments. They may use skilled birth attendants more where this is less common. We do not know if the messages affect women's or babies' health because the certainty of the evidence is very low.
Compared to women who get messages sent in other ways
Women and newborns may have fewer health problems during the first 10 days after birth. The messages may make little or no difference to the number of women who breastfeed. We do not know if they make women use more health services.
Compared to women who get untargeted messages
The messages may make little or no difference to whether women get influenza vaccines during pregnancy. We do not know if the messages affect women's or babies' health or lead women to use skilled birth attendants more because the evidence is lacking or of very low certainty.
What happens when pregnant women living with HIV receive targeted messages by mobile device?
Compared to women who get no messages
Women may go to slightly more antenatal care appointments. We do not know whether the messages lead more women to give birth in a health facility or improve babies' health because the evidence is of very low certainty. The messages may make little or no difference to whether pregnant women and babies follow antiretroviral (ARV) treatment (used to treat HIV) according to plan. We do not know if the messages affect women's health because the evidence is missing.
Compared to women who get messages sent in other ways
We do not know what the effect of these messages is because we lack evidence.
Compared to women who get untargeted messages
More parents may follow their babies' ARV treatment according to plan. We do not know if the messages improve women's or babies' health or their use of services because the evidence is missing.
What happens when parents of young children receive targeted messages by mobile device?
Compared to parents who get no messages
More parents may take their children to healthcare services such as vaccination appointments. But we do not know if the messages improve children's health or their health behaviour because the evidence is missing.
Compared to parents who get messages sent in other ways
Slightly more parents may take their children to vaccination appointments. The messages may make little or no difference to children's toothbrushing habits. We do not know if the messages affect children's health because the evidence is missing.
Compared to parents who get untargeted messages
Fewer parents may take their children to vaccination appointments, but this evidence is mixed. We do not know if the messages affect children's health due to lack of evidence.
How up‐to‐date is this review?
We searched for studies published up to August 2017. We carried out a search update in July 2019 and relevant studies are reported in the 'Characteristics of studies awaiting classification' section.
Summary of findings
Summary of findings 1. Digital targeted client communication via mobile devices compared to standard care or no intervention (pregnant and postpartum women) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to standard care or no intervention (pregnant and postpartum women) for improving maternal, neonatal, and child health | ||||||
| Patient or population: pregnant and postpartum women Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: standard care or no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with standard care | Risk with digital targeted client communication | |||||
|
Health status and well‐being – maternal mortality and morbidity Follow‐up: up to 3 months |
4 RCTs reported on 5 morbidity outcomes and the CIs for most outcomes encompassed both benefit and harm: severe obstetric complications up to 6 weeks postpartum (RR 0.86, 95% CI 0.70 to 1.07); 'any maternal health problem' up to 10 days postpartum (RR 0.50, 95% CI 0.90 to 2.76); breast pain up to 3 months postpartum (RR 0.28, 95% CI 0.09 to 0.80); breast engorgement up to 3 months postpartum (RR 0.58, 95% CI 0.31 to 1.10); number of acute maternal episodes requiring a clinic visit up to 3 months postpartum (MD 0.06, 95% CI –0.19 to 0.31). 1 study also reported on maternal mortality (RR 2.86, 95% CI 0.30 to 27.40), but this study only recorded 5 events. | 3073 (4 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | We are uncertain of the effect of the intervention on maternal mortality and morbidity because the certainty of the evidence was very low. | ||
|
Health status and well‐being – neonatal mortality and morbidity Follow‐up: up to 3 months |
The results of pooled analysis of 3 RCTs for neonatal morbidity and mortality combined was consistent with no effect but CIs encompassed benefit and harm (OR 1.00, 95% CI 0.61 to 1.64). 1 RCT reported that the intervention reduced number of acute neonatal episodes requiring a clinic visit up to 3 months postpartum (MD –0.53, 95% CI –0.92 to –0.14). | 3005 (4 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | We are uncertain of the effect of the intervention on neonatal mortality and morbidity because the certainty of the evidence was very low. | ||
|
Health behaviour change: breastfeeding – exclusive breastfeeding Follow‐up: up to 3 months |
Low‐risk setting | ⊕⊕⊝⊝ Lowa,d | In settings where 100% of women report exclusive breasting, the intervention may make little or no difference to exclusive breastfeeding (though an increase would not be possible). The CI encompasses no effect and harm. The intervention may increase short‐term exclusive breastfeeding in settings where rates of exclusive breastfeeding are lower. |
|||
| 1000 per 1000 | 920 per 1000 (790 to 1000) | RR 0.92 (0.79 to 1.08) | 40 (1 RCT) |
|||
| Moderate‐risk setting | ||||||
| 667 per 1000 | 867 per 1000 (707 to 1000) | RR 1.30 (1.06 to 1.59) | 135 (1 RCT) | |||
|
Service utilisation – attendance at ≥ 4 antenatal care appointments Follow‐up: during antenatal period |
311 per 1000 | 410 per 1000 (265 to 572) | OR 1.54 (0.80 to 2.96) | 2550 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | The intervention may increase attendance for antenatal care appointments, but the CI includes both an increase and a decrease. |
|
Service utilisation: intrapartum care – skilled attendant at birth Follow‐up: at delivery |
Low‐risk setting | ⊕⊕⊝⊝ Lowa,b | The intervention may make little or no difference to the proportion of births occurring with skilled attendance in settings where skilled attendance at is common. In settings where skilled attendance at birth is less common, the intervention may increase the proportion of births occurring with skilled attendance in urban areas. The intervention may slightly reduce skilled attendance in rural settings, but the CI encompasses both benefit and harm. |
|||
| 988 per 1000 | 988 per 1000 (978 to 998) | OR 1.00 (0.34 to 2.94) | 1743 (1 RCT) | |||
| High‐risk setting | ||||||
| Results were presented separately for urban and rural populations. The study reported intervention benefit in urban populations (cluster‐adjusted OR 4.45, 95% CI 1.36 to 14.51), but not in rural populations (cluster adjusted OR 0.83, 95% CI 0.36 to 1.92) | 2550 (1 RCT) | |||||
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence identified. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for risk of bias: all studies had unclear sequence generation or allocation concealment, or both. bDowngraded one level for imprecision: 95% confidence intervals that encompass both harmful and beneficial effects of the intervention. cDowngraded one level due to inconsistency: effect estimates vary in terms of direction and magnitude of effect. dDowngraded one level for imprecision: few events.
Summary of findings 2. Digital targeted client communication via mobile devices compared to non‐digital targeted client communication (pregnant and postpartum women) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to non‐digital targeted client communication (pregnant and postpartum women) for improving maternal, neonatal, and child health | ||||||
| Patient or population: pregnant and postpartum women Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: non‐digital targeted client communication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with non‐digital targeted client communication | Risk with digital targeted client communication | |||||
| Health status and well‐being – maternal mortality and morbidity ('any maternal health problem' up to 10 days postpartum) | 333 per 1000 | 63 per 1000 (13 to 263) | RR 0.19 (0.04 to 0.79) | 59 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | The intervention may reduce the proportion of women reporting a maternal health problem up to 10 days after birth. |
| Health status and well‐being – neonatal mortality and morbidity ('any newborn health problem' up to 10 days postpartum) | 481 per 1000 | 250 per 1000 (120 to 510) | RR 0.52 (0.25 to 1.06) | 59 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | The intervention may reduce the proportion of women reporting a newborn health problem up to 10 days after birth. But the CI includes both an increase and a decrease in reporting. |
| Health behaviour change: breastfeeding (exclusive breastfeeding at 9 weeks) | 1000 per 1000 | 920 per 1000 (790 to 1000) | RR 0.92 (0.79 to 1.07) | 42 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | The intervention may make little or no difference to the proportion who breastfeed exclusively (though an increase would not be possible due to 100% breastfeeding in the control arm). The CI encompasses no beneficial effect and harm. It is possible the effect of the intervention may be different in populations with different levels of baseline risk. |
| Service utilisation – attendance antenatal care appointments | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on attendance for antenatal care is unknown as there was no direct evidence identified. | |
| Service utilisation: intrapartum care – skilled attendant at birth | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on intrapartum care is unknown as there was no direct evidence identified. | |
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence identified. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for risk of bias: unclear risk of bias for allocation concealment and incomplete outcome data. bDowngraded one level for imprecision: few events.
Summary of findings 3. Digital targeted client communication via mobile devices compared to digital non‐targeted client communication (pregnant and postpartum women) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to digital non‐targeted client communication (pregnant and postpartum women) for improving maternal, neonatal, and child health | ||||||
| Patient or population: pregnant and postpartum women Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: digital non‐targeted client communication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with digital non‐targeted communication | Risk with digital targeted client communication | |||||
| Health status and well‐being – maternal mortality and morbidity | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on maternal morbidity and mortality is unknown as there was no direct evidence. | |
| Health status and well‐being – neonatal mortality and morbidity | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on neonatal morbidity and mortality is unknown as there was no direct evidence. | |
| Health behaviour change: breastfeeding | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on breastfeeding is unknown as there was no direct evidence. | |
| Service utilisation – attendance antenatal care appointments (attendance for antenatal influenza vaccination) | 310 per 1000 | 326 per 100 (220 to 490) | RR 1.05 (0.71 to 1.58) | 204 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | The intervention may make little or no difference to attendance for antenatal influenza vaccination, but the CI includes both an increase and a decrease in attendance. |
|
Service utilisation: intrapartum care – skilled attendant at birth Follow‐up: at delivery |
875 per 1000 | 875 per 1000 (604 to 1000) | RR 1.00 (0.69 to 1.45) | 16 (1 RCT) | ⊕⊝⊝⊝ Very lowb,c | We are uncertain of the effect of the intervention on the proportion of women having a skilled attendant at birth because the certainty of the evidence was very low. |
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for imprecision: 95% confidence intervals that encompass a potential harmful effect and a potential beneficial effect of the intervention. bDowngraded one level for risk of bias: trial at unclear risk of bias for several domains. cDowngraded two levels for risk of bias: trial at unclear or high risk of bias across all domains.
Summary of findings 4. Digital targeted client communication via mobile devices compared to standard care or no intervention (pregnant and postpartum women with HIV) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to standard care or no intervention (pregnant and postpartum women with HIV) for improving maternal, neonatal, and child health | ||||||
| Patient or population: pregnant and postpartum women with HIV Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: standard care or no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with standard care | Risk with digital targeted client communication | |||||
| Health status and well‐being: maternal morbidity and mortality combined | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on maternal morbidity and mortality is unknown as there was no direct evidence. | |
|
Health status and well‐being – neonatal morbidity and mortality combined Follow‐up: up to 4 weeks |
32 per 1000 | 36 per 1000 (12 to 105) | RR 1.12 (0.39 to 3.28) | 381 (1 RCT) | ⊕⊕⊝⊝ Lowa |
The intervention may make little or no difference to neonatal mortality and morbidity. However, the CI includes both an increase and a decrease in neonatal mortality and morbidity. |
|
Service utilisation – antenatal care: communications with HCWs Follow‐up: during antenatal period |
Mean number of face‐to‐face or mobile communications with HCW for antenatal care was 6 | Mean number of face‐to‐face or mobile communications with HCW for antenatal care was 7.5 (5.64 to 9.36) | MD 1.50 (–0.36 to 3.36) | 297 (1 RCT) | ⊕⊕⊝⊝ Lowb | The intervention may slightly increase attendance for antenatal care appointments. |
|
Service utilisation – intrapartum care: birth in health facility Follow‐up: at delivery |
600 per 1000 | 510 per 1000 (372to 690) | RR 0.85 (0.62 to 1.15) | 134 (1 RCT) | ⊕⊝⊝⊝ Very lowb,c | We are uncertain of the effect of the intervention on the proportion of women giving birth in a health facility because certainty of the evidence was very low. |
|
Health status and well‐being – neonatal health: infant HIV test positive Follow‐up: 8 weeks postpartum |
13 per 1000 | 7 per 1000 (1 to 33) | RR 0.54 (0.11 to 2.56) | 852 (2 RCTs) | ⊕⊝⊝⊝ Very lowd,e | We are uncertain of the effect of the intervention on the proportion of infants testing positive for HIV because the certainty of the evidence was very low. |
|
Health behaviour change: adherence to ARV therapy Follow‐up: up to 6–8 weeks postpartum |
1 study reported maternal antenatal ARV usage (RR 1.04, 95% CI 0.91 to 1.19), maternal postnatal ARV usage (RR 0.87, 95% CI 0.61 to 1.24), and infant ARV/PMTCT treatment adherence at 6–8 weeks postpartum (RR 1.01, 95% CI 0.98 to 1.04). | 503 (1 RCT) |
⊕⊕⊝⊝ Lowb | The intervention may make little or no difference to maternal and infant ARV treatment adherence. However, the CI includes benefit and harm. | ||
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ARV: antiretroviral; CI: confidence interval; HCW: healthcare worker; MD: mean difference; PMTCT: prevention of mother‐to‐child transmission; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two levels for imprecision: few events and a 95% confidence intervals that encompass a potential large harmful effect and a potential large beneficial effect of the intervention. bDowngraded two levels for risk of bias: more women were newly diagnosed with HIV in the control arm (55% with intervention versus 66% with control; P = 0.015), randomisation procedures and allocation concealment were not described, lack of blinding of participants, and only per‐protocol analysis reported with unexplained dropouts (Kassaye 2016). cDowngraded one level for imprecision: 95% confidence intervals that encompass a harmful effect and a potential beneficial effect of the intervention. dDowngraded one level for risk of bias: for one trial randomisation procedures and allocation concealment were not described, lack of blinding of participants, and only per‐protocol analysis reported with unexplained dropouts. eDowngraded two levels for imprecision: few events and a 95% confidence intervals that encompass a potential large harmful effects and a potential large beneficial effect of the intervention.
Summary of findings 5. Digital targeted client communication via mobile devices compared to non‐digital targeted client communication (pregnant and postpartum women with HIV) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to non‐digital targeted client communication (pregnant and postpartum women with HIV) for improving maternal, neonatal, and child health | ||||||
| Patient or population: pregnant and postpartum women with HIV Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: non‐digital targeted client communication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with non‐digital targeted client communication | Risk with digital targeted client communication | |||||
| Health status and well‐being: maternal morbidity and mortality combined | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on maternal morbidity and mortality is unknown as there was no direct evidence. | |
| Health status and well‐being – neonatal morbidity and mortality combined | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on neonatal morbidity mortality is unknown as there was no direct evidence. | |
| Service utilisation – antenatal care | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on attendance for antenatal care is unknown as there was no direct evidence. | |
| Service utilisation – intrapartum care | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on intrapartum care is unknown as there was no direct evidence. | |
| Health status and well‐being – neonatal health: infant HIV status | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on the proportion of infants testing positive for HIV is unknown as there was no direct evidence. | |
| Health behaviour change: adherence to ARV therapy | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on adherence to ARV therapy is unknown as there was no direct evidence. | |
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ARV: antiretroviral; CI: confidence interval; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
Summary of findings 6. Digital targeted client communication via mobile devices compared to digital non‐targeted client communication (pregnant and postpartum women with HIV) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to digital non‐targeted client communication (pregnant women and postpartum with HIV) for improving maternal, neonatal, and child health | ||||||
| Patient or population: pregnant and postpartum women with HIV Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: digital non‐targeted client communication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with digital non‐targeted client communication | Risk with digital targeted client communication | |||||
| Health status and well‐being – maternal morbidity and mortality combined | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on maternal morbidity and mortality is unknown as there was no direct evidence. | |
| Health status and well‐being – neonatal morbidity and mortality combined | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on neonatal morbidity mortality is unknown as there was no direct evidence. | |
| Service utilisation – antenatal care | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on attendance for antenatal care is unknown as there was no direct evidence. | |
| Service utilisation – intrapartum care | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on intrapartum care is unknown as there was no direct evidence. | |
| Health status and well‐being – neonatal health: infant HIV status | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on the proportion of infants testing positive for HIV is unknown as there was no direct evidence. | |
|
Health behaviour change: adherence to ARV therapy Follow‐up: 6 weeks postpartum |
720 per 1000 | 907 per 1000 (770 to 1000) | RR 1.26 (1.07 to 1.48) | 150 (1 RCT) | ⊕⊕⊝⊝ Lowa | The intervention may increase infant ARV adherence. |
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ARV: antiretroviral; CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded twice for risk of bias: trial at high or unclear risk of bias across all applicable domains.
Summary of findings 7. Digital targeted client communication via mobile devices compared to standard care or no intervention (parents of children aged under five years) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to standard care or no intervention (parents of children aged < 5 years) for improving maternal, neonatal, and child health | ||||||
| Patient or population: parents of children aged < 5 years Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: standard care or no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with standard care | Risk with digital targeted client communication | |||||
| Health status and well‐being – child morbidity and mortality combined | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on child morbidity and mortality is unknown as there was no direct evidence. | |
| Health status and well‐being – child nutritional status | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on child nutritional status is unknown as there was no direct evidence. | |
| Health behaviour change – breastfeeding | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on breastfeeding is unknown as there was no direct evidence. | |
|
Service utilisation – attendance for necessary healthcare (attendance for vaccinations at 6–12 months, attendance at HIV medical appointments) Follow‐up: up to 12 months |
642 per 1000 | 777 per 1000 (693 to 860) | RR 1.21 (1.08 to 1.34) | 5660 (10 RCTs) | ⊕⊕⊝⊝ Lowa,b | The intervention may increase attendance for necessary healthcare. However, the result varied considerably according to whether the healthcare attendance was for vaccinations at 6 months, vaccinations at 12 months, or an HIV medical appointment, and between studies within each of these outcome categories. |
| Health behaviour change – hygiene practices | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on hygiene practices is unknown as there was no direct evidence. | |
| Health behaviour change – correct treatment taken | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on taking correct treatment is unknown as there was no direct evidence. | |
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for risk of bias: most studies at unclear risk of bias for allocation concealment. bDowngraded one level for inconsistency: high statistical heterogeneity (I2 > 90%).
Summary of findings 8. Digital targeted client communication via mobile devices compared to non‐digital targeted client communication (parents of children aged under five years) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to non‐digital targeted client communication (parents of children aged < 5 years) for improving maternal, neonatal, and child health | ||||||
| Patient or population: parents of children aged < 5 years Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: non‐digital targeted client communication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with non‐digital targeted client communication | Risk with digital targeted client communication | |||||
| Health status and well‐being – child morbidity and mortality combined | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on child morbidity and mortality is unknown as there was no direct evidence. | |
| Health status and well‐being – child nutritional status | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on child nutritional status is unknown as there was no direct evidence. | |
| Health behaviour change – breastfeeding | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on breastfeeding is unknown as there was no direct evidence. | |
| Service utilisation – attendance for necessary healthcare (attendance for vaccinations at 14 weeks) | 839 per 1000 | 948 per 1000 (839 to 1000) | RR 1.13 (1.00 to 1.28) | 744 (1 RCT) | ⊕⊕⊝⊝ Lowa | The intervention may slightly increase attendance for vaccinations. However, the CI includes both no increase and a large increase in attendance. |
| Health behaviour change – hygiene practices (oral health in children at 4 weeks, Visible Plaque Index, 0–100%, lower score is better) | Mean score: 35.6 | Mean score: 33.5 (28.06 to 38.94) | MD –2.10 (–7.54 to 3.34) | 143 (1 RCT) | ⊕⊕⊝⊝ Lowb,c | The intervention may make little or no difference to oral hygiene practices. However, the CI includes both benefit and harm. |
| Health behaviour change – correct treatment taken | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on taking correct treatment is unknown as there was no direct evidence. | |
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two levels for risk of bias: study at unclear or high risk of bias across all but one domain. bDowngraded one level for imprecision: confidence interval encompasses both benefit and harm. cDowngraded one level for risk of bias: study at unclear risk of bias for sequence generation and allocation concealment.
Summary of findings 9. Digital targeted client communication via mobile devices compared to digital non‐targeted client communication (parents of children aged under five years) for improving maternal, neonatal, and child health.
| Digital targeted client communication via mobile devices compared to digital non‐targeted client communication (parents of children aged < 5 years) for improving maternal, neonatal, and child health | ||||||
| Patient or population: parents of children aged < 5 years Setting: community and healthcare settings Intervention: digital targeted client communication via mobile devices Comparison: digital non‐targeted client communication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with digital non‐targeted client communication | Risk with digital targeted client communication | |||||
| Health status and well‐being – child morbidity and mortality combined | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on child morbidity and mortality is unknown as there was no direct evidence. | |
| Health status and well‐being – child nutritional status | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on child nutritional status is unknown as there was no direct evidence. | |
| Health behaviour – breastfeeding | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on breastfeeding is unknown as there was no direct evidence. | |
|
Service utilisation – attendance for necessary healthcare – attendance for vaccinations at 6 months Follow‐up: 6 months |
652 per 1000 | 411 per 1000 (215 to 782) | RR 0.63 (0.33 to 1.20) | 40 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | The intervention may reduce attendance for vaccinations, but the CI includes both an increase and a decrease in attendance. |
| Health behaviour change – hygiene practices | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on hygiene practices is unknown as there was no direct evidence. | |
| Health behaviour change – correct treatment taken | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on taking correct treatment is unknown as there was no direct evidence. | |
| Unintended consequences | No studies reported this outcome. | — | (0 studies) | — | The effect of the intervention on unintended consequences is unknown as there was no direct evidence. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for risk of bias: unclear risk of bias for allocation concealment, high risk of bias for incomplete outcome reporting and other bias. bDowngraded one level for imprecision: small number of events and confidence interval encompassing potential harmful effect and potential beneficial effect of the intervention.
Background
Description of the condition
The enormous burden of disease due to poor sexual, reproductive, maternal, newborn, child, and adolescent health (SRMNCAH) renders them urgent global health priorities. In 2016, poor maternal and neonatal health, and communicable and nutritional diseases, which particularly adversely affect children, accounted for more than a quarter of healthy years of life lost worldwide (Hay 2016). Neonatal preterm birth complications, HIV/AIDS, neonatal encephalopathy due to birth asphyxia and trauma, lower respiratory infections, and diarrhoeal diseases were among the 10 leading causes of total years of life lost, with the burden heavily concentrated in children under five years of age (Naghavi 2017). Those living in low‐ and middle‐income countries are disproportionately affected by poor SRMNCAH (Black 2016).
In 2015, an estimated 303,000 women died during and following pregnancy and childbirth, and maternal mortality remains a leading cause of death for adolescent women. The vast majority of these deaths occurred in low‐resource settings, and most could have been prevented (Alkema 2016). Almost three‐quarters of maternal deaths are due to direct obstetric causes, such as haemorrhage, hypertensive disorders, sepsis, abortion, embolism, and complications of labour (Say 2014). The majority of indirect causes of maternal deaths are due to the exacerbation of pre‐existing conditions; with HIV accounting for an estimated 5.5% of global maternal deaths (Say 2014). Intrinsically linked to maternal health, 1.7 million stillbirths occurred in 2016 worldwide, with key causes including pregnancy and childbirth complications, lifestyle factors, diabetes and hypertension, maternal infections, preterm birth, and birth defects (Naghavi 2017; WHO 2017). Furthermore, five million children under the age of five years died in 2016, with almost half of these deaths occurring among newborns. The three leading global causes of death in children aged under five years were lower respiratory infections, neonatal preterm birth complications, and neonatal encephalopathy due to birth asphyxia and trauma (Naghavi 2017). Of those who survive, one‐third of children fail to reach their full physical, cognitive, psychological, or socioemotional potential (or a combination of these) as a result of poverty, poor health and nutrition, insufficient care and stimulation, and other risk factors of importance to early childhood development (Every Women Every Child 2015).
Indicative of the continued global commitment to the survival and well‐being of women and children, the UN Secretary General's Global Strategy for Women's and Children's Health was launched in 2010. In 2015, this was recast as the Global Strategy for Women's, Children's and Adolescents' Health aligning its priorities with the ambitious targets relating to the improvement of sexual, reproductive, maternal, newborn, and child health which feature in the Sustainable Development Goals (UN 2015). In 2011, the World Health Organization (WHO) published its global review of RMNCAH interventions, Essential Interventions, Commodities and Guidelines for Reproductive, Maternal, New‐born and Child Health, with the aim of developing consensus on the content of packages of interventions to address the main causes of maternal, newborn, and child deaths (PMNCH 2011). The health issues targeted by the recommended interventions span adolescence and prepregnancy health (e.g. prevention and management of sexually transmitted infections (STIs) including HIV, family planning, and preconception care); pregnancy (e.g. provision of safe abortion and postabortion care; appropriate antenatal care (ANC) including screening for maternal illness, preventive dietary supplements, and immunisations; prevention of pre‐eclampsia); childbirth (e.g. medical interventions such caesarean section where indicated); maternal postnatal care (e.g. detection and management of sepsis; family planning); newborn postnatal care (e.g. early initiation of exclusive breastfeeding; kangaroo care (prolonged skin‐to‐skin contact between baby and carer); detection and management of infections); and infancy and childhood (e.g. adequate nutrition; prevention and management of illness). However, despite some progress, the burden of poor sexual, reproductive, maternal, newborn, and child health remains substantial. New interventions are urgently needed to support further improvement in SRMNCAH, especially in low‐ and middle‐income countries.
Description of the intervention
Targeted client communication (TCC), also referred to as health promotion messaging or behaviour change communication, is the transmission of targeted health content to a specified population or people within a predefined health or demographic group (WHO 2018). TCC can fall along a continuum of tailored communication, such as individualised or personalised notifications, as well as untailored content which draws on predetermined content developed for the identified population group (Hawkins 2008). In order to define the populations for the TCC, eligible people need to be identified and subscribed into a system that allows the transmission of the health content information. Additionally, the health system initiates the first transmission of information, rather than a client seeking information, as in telemedicine and on‐demand information services. Following this initial communication from the health system to the client, clients may subsequently respond or continue engagement with the health system, also referred to as bidirectional communication. In contrast, non‐targeted client communication (non‐TCC) is the transmission of health promotion content delivered to the general population or an undefined population.
TCC has the potential to improve RMNCAH through targeting knowledge, motivation, and behaviour change in order to increase client demand and utilisation of the essential interventions detailed in the WHO Guidelines for Reproductive, Maternal, New‐born and Child Health described above (PMNCH 2011). For example, for the successful promotion of breastfeeding, TCC may enhance the provision of health system services through the provision of education relating to breastfeeding, providing links to local services, and providing social support.
Mobile devices may be a particularly effective way of delivering TCC. Mobile phone ownership is almost universal in high‐income countries and estimated to have reached over 90% in low‐ and middle‐income countries (ICT 2016). Phones are generally carried wherever people go and can be accessed 24 hours a day. Given their broad reach, mobile devices may provide a cost‐effective mechanism for engaging with target populations and delivering health information relating to SRMNCAH.
How the intervention might work
TCC via mobile devices can be used to target the individual‐level knowledge, attitudes, and behaviours of importance for the prevention and management of health issues, including those relating to the WHO essential interventions for reproductive, maternal, new‐born, and child health (PMNCH 2011). For example, mobile device‐based interventions can (Kaufman 2017):
provide information and education relevant to the health issue being targeted (e.g. information relating to breastfeeding, adequate child nutrition, vaccinations, and the recognition of symptoms of severe childhood infections);
facilitate timely access to health advice and services when required (e.g. by providing details of local healthcare services);
provide reminders (e.g. for HIV medication adherence; for antenatal appointment attendance; for childhood vaccination appointment attendance);
provide social and psychological support for the behaviour change targeted (e.g. through the provision of encouragement and positive reinforcement; and specifically targeting of psychological factors such as lack of motivation and low self‐efficacy).
Why it is important to do this review
Mobile device‐based interventions are of particular interest given their low‐cost and potential for widespread delivery, however, the current evidence base supporting their implementation for the improvement of maternal, newborn, and child health is limited. The most recent reviews concerned with the effectiveness of mobile device‐based interventions for maternal, newborn, or child health have been limited to studies conducted in low/middle‐income countries and have included non‐randomised controlled trials, which are prone to bias (Lee 2016). Broader reviews of randomised controlled trials (RCTs) of digital health interventions for healthcare consumers (e.g. Free 2013a) are in need of updating to consider the more recent emerging evidence in this field. Other reviews of relevance, concerned with preventive healthcare, reminders for appointment attendance, and self‐management of long‐term illnesses have focused specifically on SMS (short message service) and MMS (multimedia message service) mobile phone messaging (de Jongh 2012; Gurol‐Urganci 2013; Vodopivec‐Jamsek 2012), thereby excluding other phone‐based delivery mechanisms, such as voice calls, Interactive Voice Response (IVR), and mobile application delivered instant messages.
This review is one of two linked systematic reviews which were carried out to directly inform WHO guidelines on digital interventions for health system strengthening (WHO 2019). This review focuses on the effectiveness of TCC via mobile devices for maternal, newborn, and child health, and the other review examines the effectiveness of TCC via mobile devices for sexual and reproductive health (Palmer in preparation). Although the potential for mobile and digital technologies is acknowledged, there remains considerable demand from ministries of health, donors, and decision‐makers for evidence‐based guidance on the value of digital tools for improving health. In response to this global need for government decision‐makers, the WHO has developed a guideline on digital interventions for health system strengthening to inform government‐led investments. In combination, the current review, and the linked review focusing on sexual and reproductive health (Palmer in preparation) complement a qualitative evidence synthesis on the use of TCC for RMNCAH (Ames 2019); combined, these reviews aim to provide a comprehensive overview of the impact, acceptability, and implementation considerations for formulating guideline recommendations.
Objectives
The overall aim of this review was to assess the effects of TCC via mobile devices on health behaviour, service use, and health and well‐being for maternal, new‐born and child health. This review focuses on RMNCH priorities in LMIC relating to the WHO essential interventions for reproductive, maternal, new‐born and child health (PMNCH 2011).
Our specific objectives relate to three distinct populations and outcomes relevant to these populations. For each population group outlined below, we sought to determine whether targeted client communication via mobile devices can address challenges related to health and well‐being, health behaviour, and service utilization. Interventions and comparisons are the same throughout.
To assess the effects of TCC via mobile devices on behavioural, health/well‐being, and service utilisation outcomes relevant to maternal and new‐born health among pregnant and postpartum women (up to 6 weeks) and their partners or others who support them.
To assess the effects of TCC via mobile devices on behavioural, health/well‐being, and service utilisation outcomes relevant to maternal and new‐born health among pregnant and postpartum women (up to 6 weeks) living with HIV and their partners or others who support them.
To assess the effects of TCC via mobile devices, delivered to parent and caregivers (i.e. legal guardians, not healthcare professionals) of children under the age of 5 years, on behavioural, health/well‐being, and service utilisation outcomes relevant to child health
Secondary objectives
Had there been sufficient studies we planned to assess whether the effects of targeted client communication accessible via mobile devices differ according to:
Purpose of the intervention (e.g. to remind/recall versus to inform/educate or to support);
Income region (by World Bank income group) (World Bank 2017);
Delivery mechanism (e.g. voice, SMS, interactive voice response).
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs). We included full‐text studies, conference abstracts, and unpublished data irrespective of their publication status and language of publication.
We excluded small‐scale studies which had randomised fewer than 20 participants.
Types of participants
We included trials with the following participants:
pregnant and postpartum women up to six weeks after birth, and their partners or others who supported them (where pregnancy status had not been disaggregated, studies in which at least 70% of women were pregnant or up to six weeks postpartum);
pregnant and postpartum women up to six weeks after birth living with HIV, and their partners or others who supported them (where HIV status had not been disaggregated, studies in which at least 70% of pregnant and postpartum women were living with HIV);
parents and carers of children aged under five years (where age had not been disaggregated, studies in which at least 70% of children were under five years of age).
Types of interventions
We included trials that assessed TCC delivered via mobile devices, where the content of the communication was intended to improve maternal, new‐born, or child health, or a combination of these.
Targeted client communication
By TCC, we mean the transmission of targeted health content to a specified population or people within a predefined health or demographic group. Unless otherwise stated, we use the terms 'clients', 'patients', and 'consumers' to refer to the individuals whose behaviour, health service use, or health and well‐being were being targeted.
We included all of the following:
studies in which the healthcare consumers were the recipients of the transmitted information;
studies in which health content was transmitted from the health system to the client, also referred to as unidirectional communication;
studies in which health content was transmitted from the client to the health system or a health worker, provided that the first communication was initiated by the health system to the client's mobile device. This can occur as bidirectional communication in which clients may respond or exchange with the health system following an initial communication from the health system to the client.
We excluded:
studies in which the communication between the client and health system was first initiated by the client. Studies in which clients initiated contact with providers were included in a separate review on client‐to‐provider telemedicine (Gonçalves‐Bradley 2018);
studies in which health content was transmitted to the general population or an undefined population group;
studies in which the client used fully automated services, including websites, to self‐care or access clinical information;
studies in which TCC was combined with a health worker tool for tracking client's health status, as this combination was included in a separate review (Agarwal 2018).
Mobile device/multimedia delivery of targeted health communication
By mobile devices, we mean mobile phones of any type (but not analogue landline telephones), as well as tablets and personal digital assistants, which facilitate communication via different multimedia channels including SMS, voice calls, IVR, MMS, and smartphone applications (apps) when used for instant messaging purposes.
We included studies that used the following communication channels:
mobile text messaging (including SMS, and unstructured supplementary service data (USSD));
MMS, including video and audiovisual messages;
IVR;
voice calls and call‐backs;
WhatsApp and other instant messaging services (such as Facebook messenger);
apps, only when they provided an instant messaging function to provide TCC.
We excluded studies that use the following communication channels:
web portals, applications, and websites that did not have a targeted communication component to notify clients (i.e. which did not provide an instant messaging function, and thereby provided passive information which relied on clients to actively access);
emails alone;
social media websites such as Facebook, Baidu, Twitter (unless there was explicit mention of the provision of instant messaging services to individuals to provide target client communication).
Mixed modes of delivery
We included studies in which the intervention delivered to mobile devices was the primary intervention component under evaluation.
When considering interventions delivered by multiple modes, we included interventions involving additional components which could have conceivably been delivered by a mobile device (e.g. an intervention delivered by SMS in combination with email, websites, social media) as all of these delivery mechanisms would allow the entire intervention to be received via a mobile device. Interventions including additional components that could not conceivably be delivered by a mobile device were excluded (e.g. an intervention delivered by SMS in combination with face‐to‐face counselling).
Content and purpose of the targeted client communication
We included TCC dealing with the health issues listed below. We derived the list of health issues from two key resources by the WHO on Essential Interventions for RMNCH:
Partnership for Maternal, Newborn & Child Health. 2011. A Global Review of the Key Interventions Related to Reproductive, Maternal, Newborn and Child Health (RMNCH) (PMNCH 2011); and
WHO, Packages of Interventions for Family Planning, Safe Abortion care, Maternal, Newborn and Child Health (WHO 2010).
For pregnant and postpartum women (up to six weeks), interventions could target:
ANC;
birth preparedness;
skilled attendant at birth;
emergency obstetric care;
postpartum care;
kangaroo mother care;
tetanus immunisation;
anaemia prevention and control;
STI testing and treatment in pregnancy;
sexual violence;
malaria prevention and treatment;
smoking cessation during pregnancy;
antiretroviral (ARV) adherence (for pregnant and postpartum women living with HIV);
early infant diagnosis (for pregnant and postpartum women living with HIV);
retention of mother and infant pairs in elimination of mother‐to‐child transmission (eMTCT) care (for pregnant and postpartum women living with HIV).
Parents and other carers of children under five years of age, interventions could target:
postnatal care;
Immunisation;
breastfeeding;
integrated management of newborn and childhood illnesses (IMNCI);
water, sanitation, and hygiene (WASH);
Management of diarrhoeal illnesses, oral rehydration salts (ORS), zinc;
growth monitoring and nutrition;
early infant diagnosis in HIV‐exposed children; ARV therapy for HIV‐exposed and HIV‐infected children;
early childhood development.
Interventions could serve at least one of the following purposes (Kaufman 2017):
to inform and educate identified clients;
to remind and recall identified clients;
to teach skills to identified clients;
to provide support (i.e. for the behaviour change targeted, disease prevention, or health improvement);
facilitate decision‐making;
enable communication.
We have only included health issues that could potentially be addressed through targeted communication to the client, as opposed to those that relate to the provision of clinical care which would be targeted through communication to the healthcare provider. Further details of outcomes that were included can be found below.
Types of comparisons
We included trials with the following comparisons:
targeted communication delivered to the client via mobile device compared with standard care or no intervention;
targeted communication accessible to the client via mobile device compared with targeted, non‐digital communication (e.g. letters, face‐to‐face communication with clients);
targeted communication accessible to the client via mobile devices compared with non‐targeted, digital communication via mobile devices (e.g. digital communications which did not target issues relating to maternal, newborn or child health)
We excluded comparisons of:
one type of targeted communication accessible to the client via mobile devices compared with another type of targeted communication accessible via mobile devices held by the client (e.g. mobile messaging compared with mobile voice);
studies that compare different technical specifications of telecommunication technologies (e.g. different communication channels, software, etc.);
studies comparing TCC via mobile device in addition to another intervention that could not conceivably be delivered by mobile device (e.g. face‐to‐face counselling), compared with TCC via mobile device alone;
studies comparing TCC via mobile device in addition to another intervention that could not conceivably be delivered by mobile device (e.g. face‐to‐face counselling), compared with standard care/no intervention.
Types of outcome measures
The outcome measures extracted were according to the population targeted. Below we present the outcomes relevant for pregnant and postpartum women (up to six weeks) living without HIV and living with HIV and the outcomes extracted for children under the age of five years. We extracted both objectively measured and self‐reported outcomes for all lengths of follow‐up reported.
Where a study reported the same outcome measure for multiple time points, we extracted data for the outcome at the longest follow‐up time point. Where we identified studies that reported multiple outcome measures falling under the same outcome category, we extracted all outcome measures. For example, under the outcome category of 'partner violence', we would have extracted measures of sexual, physical, and emotional violence, to ensure that we were able to reflect different aspects within a single outcome category.
Where we identified studies that reported multiple outcome measures of the same outcome, we applied a set of rules to decide which outcome measure(s) to report in our review in order to avoid over‐representing single trials that reported on multiple measures relating to a single outcome. Where a study reported both dichotomous and continuous measures relating to a single outcome, we applied the following rules to identify one dichotomous outcome measure and one continuous outcome measure to present. The rationale for presenting both a dichotomous and a continuous outcome measure, where available, was because trials may have been underpowered to detect a difference in a clinically important dichotomous outcome (e.g. proportion adherent to medication), but may have power to detect a mean difference (MD) in the equivalent continuous outcome (e.g. MD in number of days covered by medication).
Where objective measurement was possible, we prioritised reporting an objectively measured outcome over a self‐reported outcome measure. For example, had a study included the outcome of STI status, and recorded both biochemically confirmed STI status and self‐reported STI status, we would have reported the biochemically confirmed STI status outcome. For outcomes that had not been directly objectively measured, likely for some health behaviour outcomes, we listed the outcomes of the trial (without considering either effect size or its statistical significance) and two review authors made a decision about which was most 'clinically' important or which was the most appropriate measure of the outcome under focus (or both). For example, in terms in clinical importance, if a study reported the outcome measure of attendance to at least one antenatal appointment and the outcome measure of attendance to all antenatal appointments, we presented the outcome relating to attendance to all antenatal appointments as this likely to have greater clinical impact.
Primary outcomes
Pregnant and postpartum women (living without HIV and living with HIV)
The following outcomes were identified based on the list of health issues that could be targeted by included interventions. As described above, these are based on two key resources by the WHO on Essential Interventions for RMNCH:
the Partnership for Maternal, Newborn & Child Health. 2011. A Global Review of the Key Interventions Related to Reproductive, Maternal, Newborn and Child Health (RMNCH) (PMNCH 2011); and
WHO, Packages of Interventions for Family Planning, Safe Abortion care, Maternal, Newborn and Child Health (WHO 2010).
Health behaviour change
Smoking cessation; b. alcohol consumption; c. adherence to preventive regimens for pre‐eclampsia (calcium, magnesium, low‐dose aspirin); d. adherence to antenatal regimens (e.g. folic acid); e. adherence to preventive/treatment regimens for anaemia (ante‐ and postnatal iron supplements); f. adherence to malaria prevention strategies (insecticide‐treated nets (ITNs), intermittent‐preventive treatment (IPTp) with sulphadoxine‐pyrimethamine (SP)); g. adherence to treatment for treatable infections (e.g. chlamydia, syphilis, mastitis); h. adherence to management strategies for pre‐existing conditions, e.g. diabetes; i. adherence treatment for mental health conditions; j. initiation of kangaroo care; k. initiation of breastfeeding; l. postpartum contraceptive uptake; m. adherence to deworming regimen; n. other lifestyle changes, e.g. exercise, health diet; o. adherence to ARVs (tablet count, prescription data).
Service utilisation
ANC: a. attendance for ANC appointment (e.g. more than one appointment with skilled personnel, more than four appointments with skilled personnel, attendance for vaccinations, attendance for screening, e.g. HIV, syphilis, anaemia, hypertensive disorders, attendance for malaria prevention services e.g. ITNs, IPTp with SP); b. attendance for high‐risk pregnancies (preterm, multiple pregnancies, previous maternal haemorrhage); c. attendance to eMTCT care.
Intrapartum care: a. place of birth (home, hospital); b. skilled attendant at birth.
Postnatal care: a. attendance for postpartum care appointment; b. attendance for information and counselling on nutrition, safe sex, family planning and provision of contraceptive methods; c. attendance to eMTCT care.
Postnatal care (newborn): a. attendance for postpartum care appointment.
Health status and well‐being
Maternal morbidity/mortality (physical): a. STI (any) status; b. HIV status/HIV management (CD4 count, viral load); c. tetanus; d. syphilis; e. anaemia (e.g. haemoglobin, haematocrit, ferritin); d. malaria; e. pre‐eclampsia (blood pressure); f. birth‐related complications (e.g. severe bleeding, receipt of blood transfusion, postdelivery haemoglobin, infection); g. postabortion complications (e.g. incomplete abortion, severe bleeding, infection); h. mastitis; i. maternal mortality (objective and self‐reported measures).
Maternal morbidity (mental): a. depression (validated measure); b. anxiety (validated measure); c. puerperal psychosis.
Neonatal Health: a. gestational age at birth; b. birth weight; c. Apgar score; d. perinatal death; e. neonatal death; d. HIV status.
Partner violence: a. sexual violence; b. physical violence; c. emotional violence (objective, e.g. hospital admissions and self‐report measures).
Well‐being: a. validated measures of health‐related quality of life.
Parents and other carers of children under five years of age
Health behaviour change of parent/carer
Breastfeeding: a. duration of breastfeeding; b. exclusive breastfeeding (among babies under six months of age).
Nutrition: a. introduction of complementary foods (among babies aged six to eight months); b. dietary diversity/adequacy (children aged six to 23 months who received foods from four or more food groups); c. minimum meal frequency; d. consumption of iron‐rich or iron‐fortified foods; e. adherence to vitamin A supplements.
Hygiene practices: a. handwashing; b. general hygiene (e.g. washing kitchen utensils, sterilisation of household goods); c. cord care; d. safe disposal of faeces.
Treatment adherence: a. adherence to ARV in HIV‐exposed and HIV‐positive children; b. adherence to prescribed regimen for other illnesses (e.g. local infections); c. adherence to treatment for malnutrition; d. correct treatment for diarrhoeal disease (e.g. use of ORS, rice water); e. adherence to prescribed regimen for prevention of malaria (ITNs, IPTp with SP).
Service utilisation
a. attendance for vaccinations (including measles/diphtheria/pertussis/tetanus vaccine); b. attendance to healthcare services when child showed symptoms of severe illness (e.g. sepsis); c. antibiotic treatment for pneumonia; d. time to diagnosis of HIV in HIV‐exposed infants.
Health status and well‐being of child
Normal growth: a. weight; b. height; c. body mass index; d. growth trajectories (e.g. stunting).
Nutritional status: a. anaemia; b. vitamin deficiencies.
Disease: a. malaria; b. measles; c. HIV; d. pneumonia; e. diarrhoeal disease; f. tetanus; g. pertussis; h. diphtheria; i. other infections; j. CD4 count, viral load (among children with HIV); k. child mortality.
Cognitive development: a. achievement of developmental milestones.
Secondary outcomes
We extracted the following secondary outcomes for all populations.
Patient/client acceptability and satisfaction with the intervention (among those who received the intervention).
Resource use, including cost to the system (e.g. human resources/time, supplies, and equipment). This measure had to be prespecified and available directly from the main trial report (i.e. we did not search for separate reports on cost‐effectiveness analyses).
Unintended consequences (these could have included: misreading or misinterpretation of data; transmission of inaccurate data; loss of verbal and non‐verbal communication cues, including between provider and client; issues of privacy and disclosure; affecting interpersonal relationships; negative impact on equity; issues with implementation fidelity resulting in an undesirable effect on health outcomes, such as failure or delay in the message delivery that results in missed appointments).
Reporting one or more of the outcome measures listed here in the trial was not an inclusion criterion for the review.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases:
Cochrane Central Register of Controlled Trials (CENTRAL, the Cochrane Library) (August 2017);
MEDLINE (OvidSP) (July 2017);
Embase Classic + Embase (OvidSP) (August 2017);
POPLINE (August 2017);
WHO Global Health Library (August 2017).
Search strategies were tailored according to database requirements. The search strategies for each database are reported in Appendix 1; Appendix 2; Appendix 3; Appendix 4; and Appendix 5. The search strategies were designed to retrieve studies relevant to the two linked reviews: 1. Targeted client communication via mobile devices for improving maternal, neonatal, and child health, and 2. Targeted client communication via mobile devices for improving reproductive and sexual health (Palmer in preparation).
We searched for studies published since 2010. A review entitled "The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: a systematic review" by Free 2013a carried out searches for studies published up to 2010. With the exception of our focus on a narrower range of health issues (sexual, reproductive, maternal, newborn, child health), our inclusion and exclusion criteria were consistent with Free 2013a. Therefore, we included all relevant studies from Free 2013a covering the period up to 2010.
Searches were initially carried out in July/August 2017 and all relevant studies identified up to this date have been reported in this review. Prior to publication, a search update was carried out in July 2019. Relevant studies from the update search were not included in the review but reported in the Characteristics of studies awaiting classification section. The PRISMA diagram in Figure 1 represents the flow of studies up to July 2019.
1.
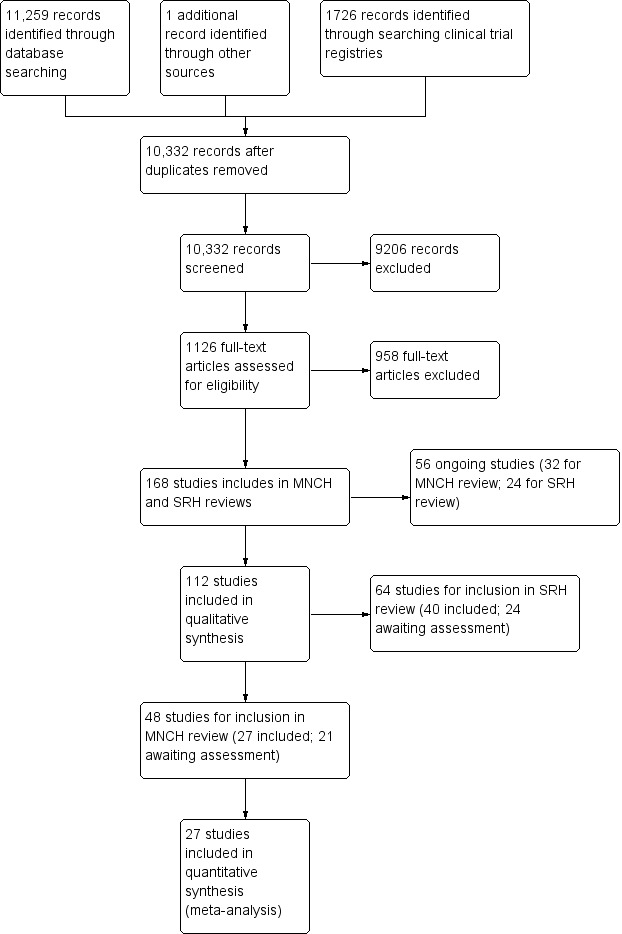
Study flow diagram. MNCH: maternal, neonatal, and child health; SRH: sexual and reproductive health.
Searching other resources
We searched for ongoing trials in the following trial registries:
WHO ICTRP (International Clinical Trials Registry Platform; www.who.int/ictrp) (July 2019; Appendix 6);
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov) (July 2019; Appendix 7).
We also searched Epistemonikos (www.epistemonikos.org/) (July 2019) to identify all relevant systematic reviews and screened them for relevant primary studies. Additionally, WHO issued a call for papers through popular digital health communities of practice such as the Global Digital Health Network and Implementing Best Practices, to identify additional primary studies as well as grey (unpublished) literature.
On completion of screening, we ran a search for all related citations of the included studies, and these citations were screened.
Data collection and analysis
The review was carried out as described in the protocol (Palmer 2018a), with exceptions noted in the Differences between protocol and review section.
Selection of studies
Two review authors independently screened all titles and abstracts identified from searches to determine those which met the inclusion criteria. We retrieved in full text any papers identified as potentially relevant. Two review authors independently screened full‐text articles for inclusion or exclusion, with discrepancies resolved by discussion and by consulting a third review author where necessary. Selected potentially relevant papers excluded from the review at the full‐text stage are listed as excluded studies, with reasons provided in the Characteristics of excluded studies table. We recorded citation details and any available information about ongoing studies (see Characteristics of ongoing studies table). We collated and reported details of duplicate publications, so that each study (rather than each report) was the unit of interest in the review. The screening and selection process is presented in an adapted PRISMA flow chart (Figure 1) (Liberati 2009).
Data extraction and management
One review author extracted data from included studies, and this was cross‐checked by a second review author. Any discrepancies were resolved by discussion until consensus was reached, or through consultation with a third review author where necessary. We developed and piloted a data extraction form using the Cochrane Consumers and Communication Review Group Data Extraction Template (available at: cccrg.cochrane.org/author-resources).
Data extracted included the following items:
methods: study design; total duration of study; study setting; and date of study;
participants: number randomised; number lost to follow‐up/withdrawn; number analysed; mean age; age range; gender; and inclusion criteria and exclusion criteria;
interventions: details of intervention and comparison group conditions (including detail of what 'standard care' included). This included intervention delivery mechanism (e.g. text messages/MMS/apps/combined); how the intervention was developed; if the intervention was personalised; and frequency and duration of intervention receipt;
outcomes: primary and secondary outcomes specified and collected; unintended consequences; and time points reported;
notes: funding for trial and notable conflicts of interest of trial authors.
All extracted data was entered into Review Manager 5 (Review Manager 2014) by one review author, and checked for accuracy against the data extraction sheets by a second review author working independently.
Assessment of risk of bias in included studies
We assessed and reported the methodological risk of bias of included studies in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and the guidelines of the Cochrane Consumers and Communication Review Group (Ryan 2013), which recommends the explicit reporting of the following individual elements for RCTs: random sequence generation; allocation sequence concealment; blinding (participants, personnel); blinding (outcome assessment); completeness of outcome data; selective outcome reporting; and other bias. We considered blinding separately for different outcomes where appropriate (e.g. blinding may have the potential to differently affect subjective versus objective outcome measures). Under 'Other bias', we considered other potential sources of bias such as the presence of baseline imbalances related to the outcome under study, and evidence of contamination. For cluster‐RCTs we also assessed and reported the risk of bias associated with an additional domain: selective recruitment of cluster participants. We judged each item as being at high, low, or unclear risk of bias as set out in the criteria provided by Higgins 2011, and provided a quote from the study report and a justification for our judgement for each item in the 'Risk of bias' table. One review author independently assessed the risk of bias of included studies and a second review author cross‐checked all assessments. Any disagreements were resolved by discussion to reach consensus.
Measures of treatment effect
For individually randomised controlled trials reporting dichotomous outcomes, we analysed data based on the number of events and the number of people assessed in the intervention and comparison groups. We used these to calculate the risk ratio (RR) or odds ratio (OR) and 95% confidence interval (CI). For continuous measures, we analysed data based on the mean, standard deviation (SD) and number of people assessed for both the intervention and comparison groups to calculate mean difference (MD) and 95% CI. If the MD was reported without individual group data, we used this to report the study results. If more than one study measured the same outcome using different tools, we calculated the standardised mean difference (SMD) and 95% CI using the inverse variance method in Review Manager 5 (Review Manager 2014). For cluster RCTs, where the study reported cluster‐adjusted effect estimates (e.g. RR, OR) or counts, these were extracted.
Unit of analysis issues
We included both individually and cluster RCTs. Where cluster‐RCTs were included, in the first instance, we extracted effect estimates that were adjusted for within‐cluster correlation by the study authors. If no adjusted estimates were available in the study report, we derived intracluster correlation coefficients (ICCs) for the outcomes of interest from other included studies or from a paper by Pagel 2011 and calculated adjusted effect estimates prior to meta‐analysis. We calculated a design effect using these ICCs and mean cluster size, which was used to calculate the effective number of events per control/intervention and effective number of participants per control/intervention (for methods see Higgins 2011).
Where we identified multiarm trials with more than one relevant intervention arm but only one control arm, we pooled the intervention arms for a single pair‐wise comparison as recommended by the Cochrane Handbook for Systematic Reviewsof Interventions (Higgins 2011). We excluded intervention arms from multi‐arm trials that were not eligible for inclusion, but listed them in the Characteristics of included studies table.
Dealing with missing data
We planned to contact investigators or study sponsors to obtain missing data where possible (e.g. when a study was identified as abstract only); however, we did not have the resources to do so. Where a study was identified as abstract only (Kamau‐Mbuthia 2013; Kebaya 2014), we searched for associated full reports. We commented on the potential impact of studies that apparently measured outcomes but did not contribute usable data in the Effects of interventions section. Where missing data were considered a potential source of serious bias, we planned to conduct a sensitivity analysis to explore the impact of including such studies in the overall assessment of results.
For participant data, we planned, where possible, to conduct analysis on an intention‐to‐treat basis; otherwise data were analysed as reported. We reported loss to follow‐up and assessed this as a source of potential bias.
Assessment of heterogeneity
We carried out meta‐analyses when we considered it meaningful to do so. In order to be pooled, studies had to have been conducted among the same population (i.e. we did not pool studies across the three distinct populations as defined under Types of participants), targeting and measuring the same outcome, and comparing the intervention with similar control groups conditions (i.e. pooling was carried out separately for the following three comparisons: TCC delivered by mobile device versus 1. standard care or no intervention, 2. non‐digital TCC, or 3. digital non‐targeted communication. We assessed the degree of heterogeneity by visual inspection of forest plots and by examining the Chi2 test for heterogeneity. Heterogeneity was quantified using the I2 statistic and interpreted by considering the size and direction of effects and the strength of the evidence for heterogeneity, based on the P value from the Chi2 test (Higgins 2011). Where heterogeneity was present in pooled effect estimates, we intended to explore possible reasons for variability by conducting our prespecified subgroup analysis; however, there were an insufficient number of studies in the pooled analyses to conduct meaningful subgroup analyses. Where we noted other potential explanations for high heterogeneity (e.g. differing baseline level of risk), and there was a sufficient number of studies, we conducted subgroup analyses to examine these.
Assessment of reporting biases
We assessed reporting bias qualitatively based on the characteristics of the included studies. For example, if only small studies that indicated positive findings were identified for inclusion, or information that we obtained from contacting experts and authors of studies suggested that there were relevant unpublished studies, we would have considered this as potential evidence of publishing bias and would have reported it as so. If we had identified sufficient studies (at least 10) for inclusion in a meta‐analysis, we planned to construct a funnel plot to investigate small‐study effects, which may indicate the presence of publication bias. We also searched for trial registry entries and published protocols of all included studies, and used this to assess the risk of bias due to selective reporting.
Data synthesis
We decided whether to meta‐analyse data based on whether the included trials were similar enough in terms of participants, settings, intervention, comparison, and outcome measures to ensure meaningful conclusions from a statistically pooled result.
For studies which measured the same outcome at different time points, we extracted the outcome measured at the longest follow‐up time point. We had planned to categorise lengths of follow‐up as follows: short‐term follow‐up: less than three months; moderate‐term follow‐up: three to 12 months; long‐term follow‐up: more than 12 months. However, given the limited number of studies with the same aim, comparison, and outcome measure that could be pooled, we decided to pool outcomes across different lengths of follow‐up.
Due to the anticipated variability in the interventions of included studies, we used random‐effects models for meta‐analysis. The primary meta‐analyses included all studies regardless of their score on the risk of bias assessment.
For continuous outcomes, we calculated MDs with 95% CIs. If more than one study measured the same continuous outcome using different tools, we calculated the SMD and 95% CI using the inverse variance method in Review Manager 5 (Review Manager 2014). We calculated RR or OR with 95% Cl for dichotomous outcomes. For cluster‐RCTs that presented adjusted effect estimates (e.g. OR, RR), we combined these estimates with using generic inverse variance random‐effects (Higgins 2011).
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses for the objectively measured outcomes of health status:
income region (by World Bank income group: lower income, lower‐middle income, upper‐middle income, high income) (World Bank 2017);
delivery mechanisms (i.e. mobile phone messaging only, mobile apps only, combined mobile phone messaging and apps, combined apps and other).
However, there was an insufficient number of studies reporting the same health status outcomes to conduct these subgroup analyses.
Sensitivity analysis
We planned to carry out the following sensitivity analyses:
only including studies with low risk of bias on the sequence generation, allocation concealment, and incomplete outcome data domains;
only including studies with objectively measured outcomes.
However, there was only a sufficient number of studies to conduct the first specified sensitivity analysis.
'Summary of findings' table
We prepared 'Summary of findings' tables to present the results of meta‐analyses or narrative synthesis (or both) for the major comparisons of the review, for the following prespecified outcomes.
Pregnant and up to six weeks postpartum women
Maternal morbidity and mortality combined.
Neonatal morbidity and mortality combined.
Breastfeeding.
Attendance for ANC.
Birth in a health facility/occurring with a skilled attendant present.
Unintended consequences.
Pregnant and up to six weeks postpartum women living with HIV
Maternal morbidity and mortality combined.
Neonatal morbidity and mortality combined.
Attendance for ANC (including eMTCT care).
Birth in a health facility.
Unintended consequences.
Neonate HIV status.
Adherence to ARV therapy.
Parents and other carers of children under five years of age
Child morbidity and mortality combined.
Child nutritional status (including anthropometric measures).
Breastfeeding.
Clinic attendance for necessary healthcare (e.g. for vaccinations, care for severe illness, HIV tests)
Hygiene practices (e.g. handwashing).
Correct treatment taken (e.g. correct treatment for diarrhoeal disease, adherence to ARV therapy).
Unintended consequences.
Two review authors independently used the GRADE criteria to assess the certainty of the evidence based on the methods described in Chapter 11 of the Cochrane Handbook for Systematic Reviews of Interventions, using the GRADEprofiler (GRADEpro) software (Schünemann 2011). Where meta‐analyses were not possible, we presented results in a narrative format.
Ensuring relevance to healthcare decisions
The protocol and review received input and feedback from members of the WHO throughout the review process to ensure the relevance of the review for health policy and practice decisions. The review was also refereed by content experts and including a consumer referee as part of the Cochrane Consumers and Communication Group standard editorial processes.
Results
Description of studies
Results of the search
The results of the search are shown in Figure 1. The search of the databases retrieved 11,259 records, with a further 1726 records identified from clinical trial registries, and one additional record from other sources. After deduplication, 10,332 records remained for title and abstract screening, of which 9206 were clearly irrelevant and excluded. We assessed 1126 full‐text articles for eligibility and 168 studies (including 64 ongoing studies) met the inclusion criteria for either this review, or the linked review of TCC via mobile devices for sexual and reproductive health (Palmer in preparation).
For this review, the search identified 48 eligible studies, of which 21 were added to the Characteristics of studies awaiting classification section. A total of 27 studies were included in the synthesis reported below, 11 concerned pregnant and postpartum populations, three related to pregnant and postpartum populations living with HIV, and 13 related to parents of children under the age of five years.
Included studies
The Characteristics of included studies table presents details of the design, methods, participants, intervention, comparison, and outcome measures for the studies included in this review.
Participants and settings
In the 11 studies conducted among pregnant and postpartum populations, the sample size ranged from 68 to 2637, totalling 7626 participants. The three studies concerned with pregnant and postpartum women living with HIV had sample sizes varying from 150 to 550, resulting in 1088 women. All participants were recruited from a mix of community and healthcare settings.
The 13 studies among parents of children aged under five years were conducted with 8749 participants, with sample sizes ranging from 57 to 2054. All trials recruited through healthcare settings or community settings linked with healthcare facilities.
Table 10 presents details of the settings in which each trial was carried out. Of the 11 trials concerned with pregnant and postpartum women, four were conducted in high‐income countries, two in upper middle‐income countries, four in lower middle‐income countries, and one in a low‐income country. All three trials among pregnant and postpartum women living with HIV were carried out in Kenya (a lower middle‐income country). Of the 13 studies targeting parents of children under five years of age, five were conducted in high‐income countries, seven in lower middle‐income countries, and one in a low‐income country.
1. Setting and income group of included studies.
| Study ID | Setting | Country | Income groupa |
| Population: pregnant and post‐partum women | |||
| Evans 2014 | Community | USA | High income |
| Jareethum 2008 | Healthcare | Thailand | Upper middle income |
| Joshi 2015 | Community | India | Lower middle income |
| Kamau‐Mbuthia 2013 | Healthcare | Kenya | Lower middle income |
| Lund 2012 | Healthcare | Tanzania | Low income |
| Maslowsky 2016 | Healthcare and community | Ecuador | Upper middle income |
| McConnell 2016 | Healthcare | Kenya | Lower middle income |
| Moniz 2013 | Community | USA | High income |
| Naughton 2017 | Healthcare | England | High income |
| Omole 2018 | Healthcare | Nigeria | Lower middle income |
| Yudin 2017 | Healthcare | Canada | High income |
| Population: pregnant and post‐partum women living with HIV | |||
| Kassaye 2016 | Healthcare and community | Kenya | Lower middle income |
| Kebaya 2014 | Community | Kenya | Lower middle income |
| Odeny 2014 | Healthcare | Kenya | Lower middle income |
| Population: parents of children under five years | |||
| Ahlers‐Schmidt 2012 | Healthcare | USA | High income |
| Bangure 2015 | Healthcare | Zimbabwe | Low income |
| Bigna 2015 | Healthcare | Cameroon | Lower middle income |
| Brown 2016 | Healthcare and community | Nigeria | Lower middle income |
| Domek 2016 | Healthcare and community | Guatemala | Lower middle income |
| Eze 2015 | Healthcare | Nigeria | Lower middle income |
| Gibson 2017 | Community | Kenya | Lower middle income |
| Haji 2016 | Community | Kenya | Lower middle income |
| Hannan 2016 | Community | USA | High income |
| Hofstetter 2015a | Community | USA | High income |
| Niederhauser 2015 | Healthcare | Hawaii | High income |
| Sharma 2011 | Not reported | India | Lower middle income |
| Stockwell 2015 | Healthcare and community | USA | High income |
aIncome group according to World Bank list of economies, June 2017 (iccmoot.com/wp-content/uploads/2017/07/World-Bank-List-of-Economies.pdf).
Interventions
Details of the interventions are provided in the Characteristics of included studies table and Table 11.
2. Interventions in included studies.
| Study ID | Intervention type | Theory | Phone compatibility | Delivery mechanism | Personalisation | Data security | Assessment of fidelity | |
| Remind/recall | Inform/educate or support | |||||||
| Population: pregnant and post‐partum women | ||||||||
| Evans 2014 | — | Inform/educate or support | Based on: – health belief model – social influence and diffusion of information within a target population – social cognitive theory. | Not reported | Text messages | Messages tailored to date of enrolment and baby's gestational age. Thus, a woman enrolling in her 10 week of pregnancy would begin receiving week 10 messages. | Quote: "Voxiva [commercial company providing texting services] did not have access to any data collected … or any patient information stored at Madigan." | Not reported |
| Jareethum 2008 | — | Inform/educate or support | Not mentioned | Not reported | Text messages; phone call at 32 weeks' gestation | Not reported | Not reported | Not reported |
| Joshi 2015 | — | Inform/educate or support | Not reported | Simple mobile phone (SMS and call functions only) | MMS, including video and audiovisual messages; voice calls | Timed and targeted as per beneficiary's gestational age; sent in a user specified language and time slot. | Not reported | Not reported |
| Kamau‐Mbuthia 2013 | — | Inform/educate or support | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | Not reported | Not reported | Not reported |
| Lund 2012 | Remind/recall | Inform/educate or support | Not mentioned | Simple mobile phone (SMS and call functions only) | Text messages | The content of the messages varied depending on the stage of the pregnancy. Message content provided as simple text in the local language of Swahili. | Not reported | Not reported |
| Maslowsky 2016 | — | Inform/educate or support | Not mentioned | Simple mobile phone (SMS and call functions only); feature phone (can run java apps); smartphones (android, iOS, Symbian) | Voice calls | Each participant also indicated the days of the week and times of day that were best to reach her. | Not reported | All intervention participants completed the 48‐hour postdischarge education session. Only 3 participants called the nurse to ask for additional advice. |
| McConnell 2016 | — | Inform/educate or support | The checklist used by CHWs was developed using international guidelines and academic publications (Table 1, page 3). | Simple mobile phone (SMS and call functions only) | Voice calls | Process was available in English and Kiswahili. | Not reported | Not reported |
| Moniz 2013 | — | Inform/educate or support | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | Not reported | All text messages were sent through a password‐protected online service (www.eztexting.com). | 13/104 received no messages. |
| Naughton 2017 | — | Inform/educate or support | MiQuit objectives are informed by Social Cognitive Theory Perspectives on Change Theory, the Elaboration Likelihood Model of Persuasion and several additional cognitive determinants of quitting smoking in pregnancy. | Simple mobile phone (SMS and call functions only) | Text messages, phone call, email just 4 weeks after randomisation | Tailoring characteristics of the intervention include gestation, motivation to quit, the hardest situation to avoid smoking, cessation self‐efficacy, cigarette dependence and partner's smoking status. Women were encouraged to set and send a quit date to MiQuit to enable them to receive additional support orientated around when their quit attempt begins. | Not reported | Intervention fidelity was high, 98% of MiQuit recipients recalled receiving text message support. |
| Omole 2018 | Remind/recall | Inform/educate or support | Not mentioned | Simple mobile phone (SMS and call functions only) | Text messages | Pregnancy reminders for ANC appointments and health information structured by the age of the pregnancy, delivered once a week, at a time chosen by the participant. | Not reported | 1. Recording of all messages sent by the system and archiving of messages received from registered participants. In addition, the timestamp when the SMS was received and the response given to each SMS received were collected. 2. Periodic contact (based on ANC appointments) with study participants to confirm receipt of messages. 3. All responses to clients' messages were stored in a database. |
| Yudin 2017 | — | Inform/educate or support | The messages were developed using principles from the Health Belief Model of preventive health behaviour. | Simple mobile phone (SMS and call functions only) | Text messages | Not reported | Messages were sent via a password‐protected online service, Memotext (Memotext LLC). | Not reported |
| Population: pregnant and post‐partum women living with HIV | ||||||||
| Kassaye 2016 | Remind/recall | Inform/educate or support | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | Messages targeted based on pregnancy stage. | Not reported | Not reported |
| Kebaya 2014 | Remind/recall | — | Not reported | Simple mobile phone (SMS and call functions only) | Voice calls | Not reported | Not reported | Not reported |
| Odeny 2014 | Remind/recall | Inform/educate or support | Health Belief Model | Simple mobile phone (SMS and call functions only) | Text messages | SMS preferences were recorded by sending a text message from their phone. This message included date of last normal menstrual period and preferred language (English, Kiswahili, or Dholuo). For participants randomised to the intervention, the message also included preferred time for receiving SMS, and preferred name. | Not reported | Not reported |
| Population: parents of children under five years | ||||||||
| Ahlers‐Schmidt 2012 | Remind/recall | — | Not reported | Not reported | Text messages | Not reported | Not reported | Not reported |
| Bangure 2015 | Remind/recall | — | Not reported | Not reported | Text messages | None | Not reported | Not reported |
| Bigna 2015 | Remind/recall | — | Not reported | Simple mobile phone (SMS and call functions only) | Text messages, voice calls | Not reported | Text message did not contain information about the name of the child or adult, or the health status of the child. Name of adult and child not mentioned in phone call. | 57/121 (47%) participants did not receive intervention. |
| Brown 2016 | Remind/recall | Inform/educate or support | Not reported | Simple mobile phone (SMS and call functions only) | Voice calls | None | Not reported | Not reported |
| Domek 2016 | Remind/recall | — | Not reported | Not reported | Text messages | SMS messages were autopopulated with the child's name and the name of the appropriate clinic. | Not reported | Not reported |
| Eze 2015 | Remind/recall | — | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | Each message is tagged with the name of the health facility. No other personalisation reported. | Not reported | No SMS delivery log. Authors stated that "The majority of respondents, [93.1%] accepted the option of being sent reminder messages." Among those who preferred not to be sent SMS reminders, self‐confidence in not forgetting appointments (61%) and the fear of giving out phone numbers (28.8%) were the greatest barriers to mHealth uptake in this study. |
| Gibson 2017 | Remind/recall | — | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | Baby's first name, relevant vaccine name, and relevant district were personalised in the messages. | Not reported | The vast majority of carers reported receiving ≥ 1 SMS reminder or incentive during the study. |
| Haji 2016 | Remind/recall | — | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | Not reported | Not reported | 1488 messages were sent to the participants in the SMS group. |
| Hannan 2016 | Remind/recall | Inform/educate or support | Not reported | Simple mobile phone (SMS and call functions only); feature phone (can run java apps); smartphones (android, iOS, Symbian) | Text messages, voice calls | Not reported | Not reported | 681 mobile phone calls; 630 by NPs to mothers and 51 calls to NPs by mothers. The NPs were contacted via texting 29 times by the mothers. |
| Hofstetter 2015a | Remind/recall | — | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | Messages were sent in either English or Spanish depending on the primary language specified in the electronic health record. | This study utilised a customised text messaging platform integrated with the hospital registration system and its immunisation registry, EzVac. The registration system included demographic and visit data for participants, while the EzVac registry automatically captured from the institution's electronic health record all vaccine doses administered to subjects at the hospital and affiliated clinics. | Of 1254 parents in the text messaging arms who were sent ≥ 1 text message, 7.1% experienced ≥ 1 undelivered message. |
| Niederhauser 2015 | Remind/recall | — | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | The SMS included wording such as: "your baby," "your appointment," "your health care provider." | Not reported | To validate that the participants were receiving the text messages, 10% of the parents were randomly selected to receive phone calls verifying the receiving of the messages. |
| Sharma 2011 | — | Inform/educate or support | Not reported | Simple mobile phone (SMS and call functions only) | Text messages | Messages targeted mothers by saying: "you should," "your child teeth, your child tongue," etc. | Not reported | Not reported |
| Stockwell 2015 | Remind/recall | Inform/educate or support | 5 messages were selected based on previous studies. | Simple mobile phone (SMS and call functions only) | Text messages | SMS were sent in English or Spanish based on the participant's request at enrolment. | Not reported | Although no undeliverable SMS were registered, 1 postintervention survey revealed that some families did not remember receiving SMS. |
ANC: antenatal care; CHW: community healthcare worker; MMS: multimedia service; NP: nurse practitioner; SMS: short message service.
Of the 11 studies conducted among pregnant and postpartum populations, nine evaluated interventions that aimed to provide information, education, or support (Evans 2014; Jareethum 2008; Joshi 2015; Kamau‐Mbuthia 2013; Maslowsky 2016; McConnell 2016; Moniz 2013; Naughton 2017; Yudin 2017), and two interventions also provided reminders alongside information/education or support (Lund 2012; Omole 2018). Six trials delivered the intervention by text messages only (Evans 2014; Kamau‐Mbuthia 2013; Lund 2012; Moniz 2013; Omole 2018; Yudin 2017); two delivered via voice calls only (Maslowsky 2016; McConnell 2016); and the remaining three studies examined interventions delivered by multiple mechanisms, such as text messages, telephone calls, and email (Naughton 2017), texts messages and telephone calls (Jareethum 2008), and multimedia messaging including video and audiovisual messages, combined with voice calls (Joshi 2015). Four studies did not report on personalisation of the intervention (Jareethum 2008; Kamau‐Mbuthia 2013; Moniz 2013; Yudin 2017); and the rest reported some extent of personalisation, such as messaging specific to the baby's gestational age, choice of language in which to receive intervention, and preferred time of receipt of messaging. In eight of the trials among pregnant and postpartum women, the control group received standard care/no intervention, and in two trials the control group received digital non‐targeted communication, both in the form of text messages containing general health information (Moniz 2013; Omole 2018). One trial had two control groups contributing to this review; of which one was standard care, and the other was non‐digital targeted communication (which involved delivering the content of the intervention through home visits by community health workers) (McConnell 2016).
Of the trials conducted among pregnant and postpartum women living with HIV, one tested an intervention providing reminders (Kebaya 2014), and the other two provided information, education, or support alongside reminders (Kassaye 2016; Odeny 2014). One trial delivered the intervention through voice calls (Kebaya 2014), and the other two via text messaging only (Kassaye 2016; Odeny 2014). One trial did not report if the intervention was personalised (Kebaya 2014); one was tailored according to pregnancy stage (Kassaye 2016); and one allowed participants to select their preferred time of receipt of messaging and their preferred name (Odeny 2014). Two of the trials among pregnant and postpartum women living with HIV compared the intervention to a control of standard care/no intervention (Kassaye 2016; Odeny 2014), and, in one trial, the control group received digital non‐targeted communication in the form of standard healthcare text messages (Kebaya 2014).
Most trials among parents of children aged under five years tested interventions providing reminders only, as most of these studies were concerned with efforts to increase attendance for childhood vaccinations (Ahlers‐Schmidt 2012; Bangure 2015; Bigna 2015; Domek 2016; Eze 2015; Gibson 2017; Haji 2016; Hofstetter 2015a; Niederhauser 2015). Three trials evaluated interventions aiming to provide both reminders and education, information, or support (Brown 2016; Hannan 2016; Stockwell 2015); and one provided education, information, or support without reminders (Sharma 2011). Ten interventions were delivered via text messages (Ahlers‐Schmidt 2012; Bangure 2015; Domek 2016; Eze 2015; Gibson 2017; Haji 2016; Hofstetter 2015a; Niederhauser 2015; Sharma 2011; Stockwell 2015), one through voice calls (Brown 2016), and two through a combination of text messages and voice calls (Bigna 2015; Hannan 2016). Four studies did not report on whether the intervention had any degree of personalisation (Ahlers‐Schmidt 2012; Bigna 2015; Haji 2016; Hannan 2016); two studies reported that the intervention was not personalised (Bangure 2015; Brown 2016); and the rest reported at least some degree of personalisation such as use of the child's name or name of clinic at which the appointment was due (or both), and delivery in preferred language. In 10 of the trials among parents of children aged under five years, the control group received standard care or no intervention, in one trial the control received digital non‐targeted communication in the form of text messages about general infant health, without the reminders for vaccination appointments that were received by the intervention group (Niederhauser 2015); and in one trial the control group received non‐digital targeted communication in the form of pamphlets (Sharma 2011). One trial among parents of children had two control groups for the purposes of this review; one received standard care and the other received non‐digital targeted communication in the form of sticker vaccination reminders (Haji 2016).
Outcomes
Health behaviours
Six trials among pregnant and postpartum women reported on at least one health behaviour change outcome. Two trials recorded smoking during pregnancy (Evans 2014; Naughton 2017), one reported on alcohol consumption during pregnancy (Evans 2014), three reported on breastfeeding (Kamau‐Mbuthia 2013; Maslowsky 2016; McConnell 2016), one reported on uptake of postpartum contraception (Maslowsky 2016), and one on adherence to iron/folic acid tablets during the antenatal period (Joshi 2015).
Two of the three trials among pregnant and postpartum women living with HIV reported on behaviour change – one in the form of maternal utilisation and adherence to ARV therapy, infant ARV/PMTCT, and infant HIV testing (Kassaye 2016); and one on recorded adherence to newborn PMTCT treatment (nevirapine prophylaxis) (Kebaya 2014).
Only one of the trials carried out with parents of children aged under five years reported a behaviour change outcome, and this was an indicator of hygiene practices for oral health (the Visible Plaque Index (VPI) in children) (Sharma 2011).
Service utilisation
Seven of the trials among pregnant and postpartum women reported on health service utilisation outcomes: one measured the proportion of women attending more than four ANC appointments (Lund 2012); two measured attendance for antenatal influenza vaccine (Moniz 2013; Yudin 2017); three reported whether birth occurred in a health facility or whether it was attended to by a skilled birth assistant (Joshi 2015; Lund 2012; Omole 2018); and two measured attendance for postpartum care appointments (Maslowsky 2016; McConnell 2016).
All three of the trials among pregnant and postpartum women living with HIV recorded service utilisation outcomes. One recorded the proportion of births occurring in a health facility, ANC, and mean number of face‐to‐face or mobile communications with healthcare workers (Kassaye 2016); two reported attendance for postpartum care visits (Kebaya 2014; Odeny 2014).
Eleven of the trials targeting parents of children aged under five years reported on health service utilisation outcomes, most which related to attendance for childhood vaccinations (Ahlers‐Schmidt 2012; Bangure 2015; Brown 2016; Domek 2016; Eze 2015; Gibson 2017; Haji 2016; Hannan 2016; Hofstetter 2015a; Niederhauser 2015; Stockwell 2015). Two studies reported on other types of health service utilisation – one on attendance to HIV medical appointments (among HIV‐positive and HIV‐exposed infants) (Bigna 2015); and one reported on urgent care seeking (Hannan 2016).
Health and well‐being
Three trials among pregnant and postpartum women measured health and well‐being outcomes. One reported on neonatal diarrhoeal disease and infant growth up to three months postpartum (Kamau‐Mbuthia 2013); one reported on preterm delivery, birthweight, and gestational age at birth (Jareethum 2008); and one trial measured perinatal death and maternal mortality (Lund 2012).
Two of three trials among pregnant and postpartum women living with HIV recorded HIV status of the neonate (Kassaye 2016; Odeny 2014), and one trial reported neonatal deaths/stillbirths (Odeny 2014). None of trials among parents of children aged under five years recorded health and well‐being outcomes.
Unintended consequences
None of the trials carried out among the three populations of interest reported data on unintended consequences or adverse events.
Acceptability
Eight studies among pregnant and postpartum women recorded at least one measure relating to acceptability/satisfaction with the intervention (Jareethum 2008; Joshi 2015; Lund 2012; Maslowsky 2016; Moniz 2013; Naughton 2017; Omole 2018; Yudin 2017), whereas as none of the studies among pregnant and postpartum women living with HIV did so. Of the trials carried out with parents of children aged under five years, six reported on indicators of acceptability/satisfaction with the intervention (Ahlers‐Schmidt 2012; Bangure 2015; Domek 2016; Gibson 2017; Hofstetter 2015a; Stockwell 2015).
Resource use
One trial conducted among pregnant and postpartum women reported on the costs associated with delivering the intervention (Naughton 2017). No trials among pregnant and postpartum women living with HIV reported on the intervention costs. Five of the trials among parents of children aged under five years provided information relating to intervention costs (Bangure 2015; Bigna 2015; Eze 2015; Haji 2016; Hannan 2016).
Funding
Of the trials conducted among pregnant and postpartum women, nine were funded by non‐commercial grants (Evans 2014; Joshi 2015; Kamau‐Mbuthia 2013; Maslowsky 2016; McConnell 2016; Moniz 2013; Naughton 2017; Omole 2018; Yudin 2017), and one did not state the source of funding (Jareethum 2008).
Two of the trials conducted among pregnant and postpartum women living with HIV reported non‐commercial funding sources (Kassaye 2016; Odeny 2014), and one did not report the source of funding (Kebaya 2014).
Most trials conducted among parents of children aged under five years reported non‐commercial funding sources (Ahlers‐Schmidt 2012; Bangure 2015; Bigna 2015; Domek 2016; Gibson 2017; Haji 2016; Hannan 2016; Hofstetter 2015a; Lund 2012; Stockwell 2015), and four of the studies did not report their source of funding (Brown 2016; Eze 2015; Niederhauser 2015; Sharma 2011).
Excluded studies
Following full‐text screening, we excluded 958 articles (Figure 1). The details of relevant excluded trials are provided in the Characteristics of excluded studies table. Reasons for exclusion included not having a randomised controlled design or enrolling an irrelevant population (e.g. parents of older children/adolescents). The most common reasons for exclusion were related to the intervention being evaluated. In some cases, the intervention was not considered to be TCC as per our definition, or the intervention included a digital tracking component, or was used in conjunction with other interventions (e.g. face‐to‐face interventions).
Studies awaiting classification
We updated the search in August 2019, and identified a further 21 studies, which are summarised in the Characteristics of studies awaiting classification table.
Ongoing studies
We identified 32 ongoing studies, which are summarised in the Characteristics of ongoing studies table.
Risk of bias in included studies
Details of the risk of bias assessments for each of the included studies are presented in the 'Risk of bias' tables in the Characteristics of included studies table, and in Figure 2.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Pregnant and postpartum women
One trial demonstrated adequate random sequence generation and allocation concealment, and so was at low risk of bias for both domains (Yudin 2017). Five trials reported adequate random sequence generation and were at low risk of bias on this domain, but did not provide sufficient information on their procedures relating to allocation concealment and therefore were at unclear risk of bias for this domain (Evans 2014; Jareethum 2008; Maslowsky 2016; McConnell 2016; Naughton 2017). One trial was at unclear risk of bias for random sequence generation, and at low risk of bias for allocation concealment (Moniz 2013). Four studies were at unclear risk of bias for both random sequence generation and allocation concealment domains as they provided insufficient information (Joshi 2015; Kamau‐Mbuthia 2013; Lund 2012; Omole 2018).
Pregnant and postpartum women living with HIV
One trial demonstrated adequate random sequence generation and allocation concealment, and so was at low risk of bias for both domains (Odeny 2014). Two studies were at unclear risk of bias for both random sequence generation and allocation concealment domains as they provided insufficient information (Kassaye 2016; Kebaya 2014).
Parents and carers of children aged under five years
Four trials demonstrated adequate random sequence generation and allocation concealment, and so were at low risk of bias for both domains (Bigna 2015; Domek 2016; Gibson 2017; Hofstetter 2015a). Five studies reported adequate random sequence generation and were at low risk of bias on this domain, but did not provide sufficient information on their procedures relating to allocation concealment and therefore were at unclear risk of bias for this domain (Ahlers‐Schmidt 2012; Bangure 2015; Eze 2015; Hannan 2016; Niederhauser 2015). Three studies were at unclear risk of bias for both random sequence generation and allocation concealment domains as they provided insufficient information (Brown 2016; Haji 2016; Sharma 2011), and one study was at unclear risk of bias for random sequence generation, but low risk of bias for allocation concealment (Stockwell 2015).
Blinding
Pregnant and postpartum women
Nine trials were at high risk of bias for the blinding of participants and personnel domain (Evans 2014; Jareethum 2008; Joshi 2015; Kamau‐Mbuthia 2013; Lund 2012; Maslowsky 2016; McConnell 2016; Naughton 2017; Omole 2018). One trial did not provide sufficient information relating to blinding of participants and personnel and so was at unclear risk of bias for this domain (Moniz 2013). One trial was at low risk of bias for blinding of participants and personnel (Yudin 2017). Three studies demonstrated adequate blinding for objective outcomes and were at low risk of bias on this domain (Jareethum 2008; Moniz 2013; Naughton 2017), two studies did not provide adequate information and so were at unclear risk of bias on this domain (Lund 2012; Omole 2018), and six studies did not record objective outcomes (Evans 2014; Joshi 2015; Kamau‐Mbuthia 2013; Maslowsky 2016; McConnell 2016; Yudin 2017). In relation to blinding for subjective outcome assessment, one trial was a low risk of bias (Yudin 2017), two were at unclear risk of bias due to lack of information provided (Moniz 2013; Omole 2018), seven were at high risk of bias (Evans 2014; Jareethum 2008; Joshi 2015; Kamau‐Mbuthia 2013; Maslowsky 2016; McConnell 2016; Naughton 2017), and the remaining study did not record any subjective outcomes (Lund 2012).
Pregnant and postpartum women living with HIV
All three trials were at high risk of bias for the blinding of participants and personnel domain (Kassaye 2016; Kebaya 2014; Odeny 2014).
One study was at high risk of bias for subjective outcome assessment, and did not record any objectively measured outcomes (Kassaye 2016), one provided insufficient information and was considered to be at unclear risk of bias for blinding of both objective and subjective outcomes (Kebaya 2014), and third study was at low risk of bias for blinding of objective outcomes, and did not record any subjective outcomes (Odeny 2014).
Parents of children aged under five years
With the exception on one trial which was at low risk of bias for blinding of participants and personnel (Hofstetter 2015a), all trials among parents of children aged under five years were at high risk of bias for this domain. One study was at low risk of bias for blinding of both objective and subjective outcome assessments (Hofstetter 2015a), one study was at low risk of bias for blinding of objective outcome assessments, and did not record any subjective outcomes (Sharma 2011), one study was at low risk of bias for objective outcomes and unclear risk of bias for subjective outcomes (Gibson 2017), and four studies were at low risk of bias for blinding of objective outcome assessments and high risk of bias for blinding of subjective outcome assessments (Ahlers‐Schmidt 2012; Bigna 2015; Eze 2015; Stockwell 2015). Three studies were at unclear risk of bias for blinding of objective outcome assessment, and high risk of bias for subjective outcome assessment (Bangure 2015; Domek 2016; Niederhauser 2015). One study was at unclear risk of bias for blinding of objective outcomes, and did not record subjective outcomes (Brown 2016); one study did not record objective outcomes, and was at high risk of bias for subjective outcome blinding (Hannan 2016); and one study was at high risk of bias for blinding for both objective and subjective outcome assessment (Haji 2016).
Incomplete outcome data
Pregnant and postpartum women
Four of the trials among pregnant and postpartum women were at low risk of bias for incomplete outcome data (Jareethum 2008; Lund 2012; Moniz 2013; Yudin 2017) and seven were at high or unclear risk of bias for this domain (Evans 2014; Joshi 2015; Kamau‐Mbuthia 2013; Maslowsky 2016; McConnell 2016; Naughton 2017; Omole 2018).
Pregnant and postpartum women living with HIV
For the incomplete outcome data domain, one trial among pregnant and postpartum women living with HIV was at low risk of bias (Odeny 2014), one was at unclear risk of bias (Kebaya 2014), and one was at high risk of bias (Kassaye 2016).
Parents of children aged under five years
Eight of the trials among parents of children aged under five years were at low risk of bias for incomplete outcome data (Ahlers‐Schmidt 2012; Bangure 2015; Bigna 2015; Brown 2016; Domek 2016; Gibson 2017; Hofstetter 2015a; Stockwell 2015), two were at unclear risk of bias (Eze 2015; Haji 2016), and three were at high risk of bias for this domain (Hannan 2016; Niederhauser 2015; Sharma 2011).
Selective reporting
Pregnant and postpartum women
Seven studies were at low risk of bias for the selective outcome reporting domain as their protocols or trial registry entries (or both) could be identified and all expected outcomes were reported (Evans 2014; Jareethum 2008; Lund 2012; McConnell 2016; Moniz 2013; Naughton 2017; Yudin 2017). Two studies were at unclear risk of bias as their protocols could not be identified (Joshi 2015; Maslowsky 2016). Two studies were at high risk of bias on the selective outcome reporting domain due to inconsistencies between the prespecified and actual outcome reporting (Kamau‐Mbuthia 2013; Omole 2018).
Pregnant and postpartum women living with HIV
Two of the trials among pregnant and postpartum women living with HIV were at unclear risk of bias for selective outcome reporting as their protocols could not be identified (Kassaye 2016; Odeny 2014), and one was at high risk of bias due to inconsistency between prespecified and actual outcome reporting (Kebaya 2014).
Parents of children aged under five years
Six studies among parents of children aged under five years were at low risk of bias for the selective outcome reporting domain as their protocols or trial registry entries (or both) could be identified and all expected outcomes were reported (Bangure 2015; Bigna 2015; Domek 2016; Gibson 2017; Haji 2016; Stockwell 2015). Seven studies were at unclear risk of bias as their protocols could not be identified (Ahlers‐Schmidt 2012; Brown 2016; Eze 2015; Hannan 2016; Hofstetter 2015a; Niederhauser 2015; Sharma 2011).
Other potential sources of bias
Pregnant and postpartum women
Four studies were at low risk of bias for the 'other bias' domain (Jareethum 2008; Lund 2012; Maslowsky 2016; Moniz 2013), and seven were at unclear risk of bias (Evans 2014; Joshi 2015; Kamau‐Mbuthia 2013; McConnell 2016; Naughton 2017; Omole 2018; Yudin 2017).
Pregnant and postpartum women living with HIV
For the 'other bias' domain, one trial among pregnant and postpartum women living with HIV was at low risk of bias (Odeny 2014), one was at unclear risk of bias (Kebaya 2014), and one was at high risk of bias as due to important baseline differences between groups (Kassaye 2016).
Parents of children aged under five years
Five of the trials conducted among parents of children aged under five years were at low risk of other bias (Bangure 2015; Gibson 2017; Hofstetter 2015a; Sharma 2011; Stockwell 2015). Five trials were at unclear risk of bias for this domain (Ahlers‐Schmidt 2012; Bigna 2015; Domek 2016; Hannan 2016; Niederhauser 2015). Three trials were at high risk of bias for this domain due to: significant demographic differences between clusters in a clustered RCT (Brown 2016); participants being swapped between the intervention and control group when people who did not own a mobile phone had been allocated to the intervention (Eze 2015); and an issue whereby attending a different facility may results in misclassification of the outcome of vaccination (Haji 2016).
Selective cluster recruitment
Pregnant and postpartum women
Three of the 11 trials conducted among pregnant and postpartum women were cluster RCTs and one was at low risk of bias for the domain of selective cluster recruitment (Lund 2012), one was at unclear risk of bias (Joshi 2015), and one was at high risk of bias due to participant enrolment after cluster allocation had been made (Omole 2018). The remaining trials were individually randomised trials and so were not assessed regarding cluster recruitment.
Pregnant and postpartum women living with HIV
One of the three trials conducted among pregnant and postpartum women living with HIV was a cluster RCT and at unclear risk of bias for the domain of selective cluster recruitment (Kassaye 2016). The other two trials were individually randomised trials and so were not assessed regarding cluster recruitment.
Parents of children aged under five years
Three of the 13 trials conducted among parents of children aged under five years were cluster RCTs. One was at unclear risk of bias for the domain of selective cluster recruitment (Brown 2016), and two were at high risk of bias due to convenient enrolment of participants likely to have taken place after cluster allocation to intervention arms (Haji 2016), and participant enrolment after cluster allocation had been made (Gibson 2017). The remaining trials were individually randomised trials and so were not assessed regarding cluster recruitment.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9
Pregnant and postpartum women
Targeted client communication via mobile devices versus standard care
Table 1 presents the evidence relating to the effect of TCC via mobile devices compared to standard care or no intervention among pregnant and postpartum women for the outcomes of maternal mortality and morbidity, neonatal mortality and morbidity, breastfeeding, attendance for ANC, receipt of intrapartum care, and unintended consequences.
Health behaviour change
There was at best moderate‐certainty evidence relating to the effect of TCC via mobile devices on health behaviours when compared to standard care.
One study carried out in Kenya provided low‐certainty evidence relating to the effect of TCC via mobile devices for the promotion of exclusive breastfeeding in a setting where all women in the control group exclusively breastfed (exclusive breastfeeding at 9 weeks postpartum: RR 0.92, 95% CI 0.79 to 1.08; n = 40; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 1.1) (McConnell 2016). Another study, conducted in Ecuador, which had comparatively lower breastfeeding rates in the standard care arm, suggests that the intervention may increase exclusive breastfeeding at three months postpartum (RR 1.30, 95% CI 1.06 to 1.59; n = 135; low‐certainty evidence – downgraded for risk of bias (unclear risk of bias on the allocation concealment domain and high rates of loss to follow‐up) and imprecision; Analysis 1.1) (Maslowsky 2016). A second RCT in Kenya found that mobile phone‐based support may increase the proportion of postpartum women receiving help with breastfeeding (RR 2.15, 95% CI 1.78 to 2.58; n = 332; low‐certainty evidence – downgraded twice for risk of bias; Analysis 1.2) (Kamau‐Mbuthia 2013).
1.1. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 1: Health behaviour change – exclusive breastfeeding in short term (up to 3 months)
1.2. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 2: Health behaviour change – receiving postpartum help with breastfeeding (3 months postpartum)
One study conducted among women living in rural villages in India demonstrated that voice messages delivered to mobile devices probably increased the proportion of participants who took iron and folate tablets for 100 days during pregnancy (RR 1.71, 95% CI 1.42 to 2.07; n = 908; moderate‐certainty evidence – downgraded once due to unclear risk of bias for random sequence generation and allocation concealment; Analysis 1.3) (Joshi 2015).
1.3. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 3: Health behaviour change – taking iron and folate tablets during pregnancy
We are uncertain about the effects of the intervention on postpartum contraceptive use at three months (study in Ecuador) and at nine weeks postpartum (study in Kenya) because the certainty of the evidence was very low (RR 1.35, 95% CI 0.75 to 2.46; n = 175; downgraded twice for risk of bias and once for imprecision; Analysis 1.4) (Maslowsky 2016; McConnell 2016).
1.4. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 4: Health behaviour change – contraceptive use (3 months postpartum)
Two studies reported on smoking during pregnancy: one UK trial among pregnant women who smoked suggested that the intervention may increase objectively verified continuous abstinence (RR 2.76, 95% CI 0.89 to 8.54; n = 407; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 1.6) (Naughton 2017). One trial in the USA among pregnant women (who were not recruited based on smoking status) suggested that the intervention may reduce the proportion of pregnant women reporting having smoked in the last 30 days (RR 0.43, 95% CI 0.17 to 1.10; n = 459; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 1.5) (Evans 2014). The USA study also found that the intervention may have little or no impact on preventing alcohol consumption during pregnancy (RR 1.00, 95% CI 0.97 to 1.03; n = 459; low‐certainty evidence – due to risk of bias and indirectness based evidence from a single high‐income country; Analysis 1.7) (Evans 2014). However, over 97% of participants across the intervention and control group reported no alcohol consumption at baseline leaving little room for any change to be observed postintervention. The effect of the intervention may be different in populations with different levels of baseline risk.
1.6. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 6: Health behaviour change – smoking cessation (objectively verified continuous abstinence) (36 weeks' gestation)
1.5. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 5: Health behaviour change – smoked in the last 30 days
1.7. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 7: Health behaviour change – no alcohol consumption during pregnancy
Service utilisation
Evidence for whether TCC via mobile devices increased service utilisation was mixed. TCC via mobile devices may have a modest effect on increasing the proportion of women attending four or more antenatal appointments (cluster‐adjusted OR 1.54, 95% CI 0.80 to 2.96; n = 2550; low‐certainty evidence – downgraded due to risk of bias and imprecision, CI encompasses both benefit and harm; Analysis 1.8) (Lund 2012). Based on pooled analyses of this trial and another conducted in Canada, TCC via mobile devices may increase attendance for antenatal vaccinations (influenza and tetanus) (OR 1.36, 95% CI 0.90 to 2.06; n = 714; low‐certainty evidence – downgraded due to risk of bias and imprecision (Analysis 1.9) (Lund 2012; Yudin 2017). The study by Lund 2012 also suggests that TCC via mobile devices may increase antenatal attendance for preventive treatment for malaria (cluster adjusted OR 1.69, 95% CI 0.82 to 3.48; low‐certainty evidence – downgraded for risk of bias and imprecision; Analysis 1.10).
1.8. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 8: Service utilisation – attendance at ≥ 4 antenatal care appointments
1.9. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 9: Service utilisation – attendance for antenatal vaccination
1.10. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 10: Service utilisation – attendance at antenatal preventive treatment for malaria
Two studies examined the effect of TCC via mobile devices on the proportion of births with a skilled attendant present The intervention may make little or no difference in one low‐risk setting where 99% of both the control and intervention group had a skilled attendant at birth (OR 1.00, 95% CI 0.34 to 2.94; n = 1743; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 1.11) (Joshi 2015). The second trial conducted in a high‐risk setting (Tanzanian urban and rural settings where about 50% of all deliveries take place at home with unskilled attendance) found that there may be benefit in urban populations (cluster‐adjusted OR 4.45, 95% CI 1.36 to 14.51; n = 1077), but not rural populations (cluster adjusted OR 0.83, 95% CI 0.36 to 1.92; n = 1473) (low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 1.11) (Lund 2012) (this study only reported effect estimates accounting for clustering separately by urban and rural for this outcome).
1.11. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 11: Service utilisation – skilled attendant at birth
Two studies examined the effect of TCC via mobile devices on utilisation of care for newborns. One trial conducted in Kenya found that the intervention may make little or no difference to care utilisation (RR 0.98, 95% CI 0.87 to 1.11; n = 56; low‐certainty evidence – downgraded for risk of bias and imprecision; Analysis 1.12). However, this was a low‐risk setting where 96% of the control group attended care for their newborn leaving little room for demonstration of an improvement (McConnell 2016). Another trial, conducted in Ecuador – a high risk setting where utilisation of care for newborns was lower (53.3% attendance in the control group) – reported that the intervention may increase the proportion of women attending services for infant care within 10 days of delivery (RR 1.35, 95% CI 1.02 to 1.78; n = 135; low‐certainty evidence – downgraded for risk of bias and imprecision; Analysis 1.12) (Maslowsky 2016). Maslowsky 2016 also reported that "no effect of the intervention on attendance at maternal postpartum visits was observed," without providing data for extraction.
1.12. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 12: Service utilisation – newborn postpartum care
One study in Kenya showed that TCC via mobile device may increase attendance for a postpartum care appointment at 10 days postpartum (RR 1.50, 95% CI 0.30 to 7.52; n = 56; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 1.13), and may have little or no effect on newborn vaccination (pentavalent and polio at up to nine weeks) (RR 1.08, 95% CI 0.89 to 1.32; n = 40; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 1.14) (McConnell 2016).
1.13. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 13: Service utilisation – attendance for postpartum care appointment (mother) (10 days postpartum)
1.14. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 14: Service utilisation – attendance for newborn vaccination
Health status and well‐being
Based on very low‐certainty evidence from one study in Tanzania, we are uncertain as to whether TCC via mobile devices has an effect on maternal mortality (RR 2.86, 95% CI 0.30 to 27.40; n = 2637; downgraded due to risk of bias and twice for imprecision; Analysis 1.15) (Lund 2012). While this effect estimate is large, it is based on very few events (four maternal deaths in the intervention group and one in the control group), and the CI is very wide, consistent with a decrease in mortality as well as a large increase; therefore, we cannot be certain what the effect might be. This study also provided low‐certainty evidence that the intervention may slightly reduce severe obstetric complications up to six weeks postpartum (RR 0.86, 95% CI 0.70 to 1.07; n = 2550; downgraded due to risk of bias and imprecision; Analysis 1.15) (Lund 2012). The trial conducted by McConnell 2016 provided low‐certainty evidence that TCC via mobile devices may reduce the likelihood of reporting having experienced 'any maternal health problem' up to 10 days postpartum (RR 0.50, 95% CI 0.90 to 2.76; n = 56; downgraded due to risk of bias and imprecision; Analysis 1.15). There was low‐certainty evidence that TCC via mobile devices may reduce self‐reported breast pain and breast engorgement up to three months postpartum (pain: RR 0.28, 95% CI 0.09 to 0.80; n = 332; engorgement: RR 0.58, 95% CI 0.31 to 1.10; n = 332; Analysis 1.15) (Kamau‐Mbuthia 2013). There was low‐certainty evidence that the intervention may result in little or no difference to the number of acute maternal episodes requiring a clinic visit up to three months postpartum (MD 0.06, 95% CI –0.19 to 0.31; n = 135; downgraded due to risk of bias and imprecision; Analysis 1.16) (Maslowsky 2016).
1.15. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 15: Health status and well‐being – maternal mortality and morbidity
1.16. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 16: Health status and well‐being – maternal mortality and morbidity
There was very low‐certainty evidence relating to the effect of the intervention on neonatal mortality and morbidity based on three trials (in Tanzania and Kenya) (OR 1.00, 95% CI 0.61 to 1.64; n = 2870; downgraded once due to risk of bias and twice for imprecision; Analysis 1.17) (Kamau‐Mbuthia 2013; Lund 2012; McConnell 2016). There was moderate‐certainty evidence that the intervention may reduce the number of acute neonatal episodes requiring a clinic visit up to three months postpartum (MD –0.53, 95% CI –0.92 to –0.14; n = 135; downgraded due to risk of bias; Analysis 1.18) (Maslowsky 2016). One study reported on the effect of TCC via mobile devices on gestational age at birth and birth weight (gestational age: MD 0.10 weeks, 95% CI –0.45 to 0.65; n = 61; birth weight: MD –173 g, 95% CI –448.87 to 102.87; n = 61; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 1.19) (Jareethum 2008). Two studies conducted in Thailand and Zanzibar reported preterm birth (RR 0.85, 95% CI 0.31 to 2.33; n = 2557; low‐certainty evidence – downgraded due to risk of bias and an imprecise effect estimate, which encompassed both large potential benefit and harm of the intervention; Analysis 1.20) (Jareethum 2008; Lund 2012). A sensitivity analysis was also conducted to examine the effect of excluding the cluster RCT by Lund 2012 from the analysis with preterm birth as the outcome. This resulted in no substantive change in the findings; the point estimate remained in the direction of intervention benefit (RR 0.18, 95% CI 0.01 to 3.64; Analysis 1.21), but the CI was considerably wider, encompassing both benefit and harm.
1.17. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 17: Health status and well‐being – neonatal mortality and morbidity
1.18. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 18: Health status and well‐being – neonatal mortality and morbidity
1.19. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 19: Health status and well‐being – neonatal health
1.20. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 20: Health status and well‐being – preterm birth
1.21. Analysis.

Comparison 1: Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women), Outcome 21: Sensitivity analysis (cluster‐RCTs: health status and well‐being – preterm birth
Targeted client communication via mobile devices versus non‐digital targeted communication
Table 2 presents the evidence relating to the effect of TCC via mobile devices compared to non‐digital targeted communication among pregnant and postpartum women for the outcomes of maternal mortality and morbidity, neonatal mortality and morbidity, breastfeeding, attendance for ANC, receipt of intrapartum care, and unintended consequences.
Health behaviour change
One study conducted in Kenya compared TCC via mobile devices to non‐digital targeted communication (in the form of home visits by community health workers). This provided low‐certainty evidence relating to the effect on exclusive breastfeeding at nine weeks postpartum (RR 0.92, 95% CI 0.79 to 1.07; n = 42; Analysis 2.1; downgraded due to risk of bias and imprecision) (this study reported 100% of participants were breastfeeding in the control arm, so there was no room for benefit to be observed and the effect of the intervention may be different in populations with different levels of baseline risk) (McConnell 2016). The same study also provided low‐certainty evidence for the effect on contraceptive use at nine weeks postpartum (RR 1.45, 95% CI 0.78 to 2.69; n = 42; downgraded due to risk of bias and imprecision; Analysis 2.2) (McConnell 2016).
2.1. Analysis.

Comparison 2: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (pregnant and postpartum women), Outcome 1: Health behaviour change – exclusive breastfeeding (9 weeks postpartum)
2.2. Analysis.

Comparison 2: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (pregnant and postpartum women), Outcome 2: Health behaviour change – contraceptive use (9 weeks postpartum)
Service utilisation
The trial by McConnell 2016 provided moderate‐certainty evidence that the intervention made little or no difference to attendance for newborn care at 10 days postpartum (RR 0.97, 95% CI 0.87 to 1.09; n = 59; downgraded due to risk of bias; Analysis 2.3) or attendance for newborn vaccination at nine weeks (pentavalent and polio vaccine) (RR 1.01, 95% CI 0.88 to 1.16; n = 42; downgraded due to risk of bias; Analysis 2.4). This trial also provided low‐certainty evidence relating to the intervention effect on attendance for a maternal care postpartum appointment (RR 0.56, 95% CI 0.18 to 1.79; n = 59; downgraded due to risk of bias and imprecision; Analysis 2.5) (McConnell 2016).
2.3. Analysis.

Comparison 2: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (pregnant and postpartum women), Outcome 3: Service utilisation – newborn postpartum care (10 days after delivery)
2.4. Analysis.

Comparison 2: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (pregnant and postpartum women), Outcome 4: Service utilisation – attendance for newborn vaccination
2.5. Analysis.

Comparison 2: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (pregnant and postpartum women), Outcome 5: Service utilisation – attendance for postpartum care appointment (mother) (10 days postpartum)
Health status and well‐being
Based on the McConnell 2016 trial, there was low‐certainty evidence that the intervention may reduce 'any maternal health problem' reported up to 10 days postpartum (RR 0.19, 95% CI 0.04 to 0.79; n = 59; Analysis 2.6) and 'any newborn health problem' reported up to 10 days postpartum (RR 0.52, 95% CI 0.25 to 1.06; n = 59; Analysis 2.7). For both outcomes, the certainty of the evidence was downgraded due to risk of bias and imprecision due to the small number of events.
2.6. Analysis.

Comparison 2: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (pregnant and postpartum women), Outcome 6: Health status and well‐being – maternal mortality and morbidity
2.7. Analysis.

Comparison 2: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (pregnant and postpartum women), Outcome 7: Health status and well‐being – neonatal mortality and morbidity
Targeted client communication via mobile devices versus digital non‐targeted communication
Table 3 presents the evidence relating to the effect of TCC via mobile devices compared to digital non‐targeted communication among pregnant and postpartum women for the outcomes of maternal mortality and morbidity, neonatal mortality and morbidity, breastfeeding, attendance for ANC, receipt of intrapartum care, and unintended consequences.
Health behaviour change
No studies reported health behaviour outcomes for the comparison of TCC via mobile devices compared with digital non‐targeted communication.
Service utilisation
Based on one study in the USA comparing TCC via mobile devices with digital non‐targeted communication, there was low‐certainty evidence that the intervention may have little or no effect on attendance for antenatal influenza vaccination (RR 1.05, 95% CI 0.71 to 1.58; n = 204; downgraded due to risk of bias and imprecision; Analysis 3.1) (Moniz 2013). Based on a single study conducted in Nigeria we are uncertain as to whether TCC via mobile devices has an effect on the proportion of births occurring with skilled attendant when compared with digital non‐targeted communication (RR 1.00, 95% CI 0.69 to 1.45; n = 16; very low‐certainty evidence – downgraded twice due to risk of bias and once due to imprecision; Analysis 3.2) (Omole 2018).
3.1. Analysis.

Comparison 3: Digital targeted client communication (TCC) compared to digital non‐targeted client communication (pregnant and postpartum women), Outcome 1: Service utilisation – attendance for antenatal influenza vaccination
3.2. Analysis.

Comparison 3: Digital targeted client communication (TCC) compared to digital non‐targeted client communication (pregnant and postpartum women), Outcome 2: Service utilisation – birth at health facility
Health status and well‐being
No studies reported health status and well‐being outcomes for the comparison of TCC via mobile devices compared with digital non‐targeted communication.
Patient/client acceptability and satisfaction with the intervention
There was generally high rates of satisfaction with the interventions received. One UK trial targeting smoking cessation in pregnancy reported that 61.7% of intervention participants thought the messages were helpful, and 80.8% would recommend the support, while 14.2% reported that the messages were 'annoying' and 13.3% discontinued the support by texting 'STOP' (Naughton 2017). One study in Canada evaluating the effect of text messages aiming to increase influenza vaccine uptake during pregnancy found that 88% of intervention recipients were satisfied with the messages; 81% found the information in the messages useful; 65% thought the messages were appropriately timed; and 60% thought that the number of messages was right (received two messages per week for four weeks) (Yudin 2017). About 99% of intervention recipients in a trial conducted in Nigeria stated that they thought the SMS reminders improved ANC attendance; over 95% stated the messages influenced their decision to deliver in a health facility and to attend a postnatal clinic; 77.8% stated that the messages helped them to complete immunisations and preventive therapy for malaria in pregnancy; and 96.6% agreed that they supported the use of a SMS platform for informing ANC clients about obstetric danger signs (Omole 2018). One trial in India reported that 89.3% of the intervention group were satisfied with the content of the voice messages and 97.4% with animations received (Joshi 2015). One trial among pregnant women in Thailand who received text messages about pregnancy and the early postpartum period reported high levels of satisfaction (a mean score of 9.25, based on a visual analogue scale of 1 to 10 points) (Jareethum 2008). The majority of participants receiving the SMS intervention in one trial conducted Tanzania rated the messages positively. About 59% stated that receiving text messages influenced the number of times they attended ANC and 71% reported that the messages helped them in various areas, including learning about danger signs in pregnancy and feeling that the health system cared for them (Lund 2012). The trial of an intervention delivered through phone calls providing postpartum health education and support in Ecuador reported almost universal satisfaction – 98% of intervention participants agreed that they would like to have access to the service at their next birth, and 100% that they would recommend the service to a friend (Maslowsky 2016). Most recipients of messages communicating the importance of influenza vaccinations during pregnancy along with general health advice (USA) reported that they liked the text messages (90%), found them to be helpful (86%), wanted to receive text messages in the future (82%), and thought they increased their satisfaction with their ANC (80%) (Moniz 2013).
Resource use
Naughton 2017 reported that the total cost of delivering the 'MiQuit' text messaging intervention was GBP 4.62 per participant, and, based on the relevant incremental quit rate estimate of 3.46%, this resulted in an incremental cost per additional quitter of GBP 133.53 (95% CI –395.78 to 843.62).
Unintended consequences
None of the trials among pregnant and postpartum women collected or reported data on unintended consequences.
Equity considerations
The three trials concerned with breastfeeding were conducted in upper‐middle and lower‐middle income countries, and two of which specifically highlighted their inclusion of low‐income participants (Kamau‐Mbuthia 2013; McConnell 2016). Both trials of interventions aiming to reduce harmful behaviour during pregnancy (smoking and alcohol consumption) were conducted in high‐income countries, and it is not possible to assess whether the results are applicable to low‐income settings (Evans 2014; Naughton 2017). The two trials of TCC via mobile devices for promoting attendance for antenatal influenza vaccination were also from high‐income countries: one primarily included unmarried participants with low levels of education (Moniz 2013), while the other study population was made up of mostly married or partnered women with higher levels of education (Yudin 2017); despite the apparent socioeconomic differences in these populations, both studies demonstrated no benefit.
Of note for consideration of issues relating to equity, is that more than half of the trials applied a language‐based criteria in their inclusion/exclusion criteria. Given the nature of the intervention, it is likely that those studies not explicitly stating the need to speak the native language to partake in the study, will have also excluded those lacking such fluency in a particular language. This raises the issue of exclusion of illiterate populations and recent migrants, who are known to be a particularly vulnerable population, but are unable to provide consent to take part in studies that rely on phone‐based communications in a specific language.
Pregnant and postpartum women living with HIV
Targeted client communication via mobile devices versus standard care
Table 4 presents the evidence relating to the effect of TCC via mobile devices compared to standard care or no intervention among pregnant and postpartum women living with HIV for the outcomes of maternal mortality and morbidity, neonatal mortality and morbidity, attendance for ANC (including eMTCT care), receipt of intrapartum care, unintended consequences, neonate HIV status, and adherence to ARV therapy.
Health behaviours
One study reported the effect of TCC via mobile devices on whether mothers took any type of ARVs antenatally and postnatally compared to standard care in Kenya (Kassaye 2016). There was low‐certainty evidence suggesting the intervention may make little or no difference to maternal antenatal ARV usage (RR 1.04, 95% CI 0.91 to 1.19; n = 503; downgraded twice due to risk of bias; Analysis 4.1). The same study also provided very low‐certainty evidence relating to the effect of the intervention on maternal postnatal ARV usage (RR 0.87, 95% CI 0.61 to 1.24; n = 471; downgraded twice for risk of bias and once for imprecision; Analysis 4.2). This study also reported infant ARV/PMTCT treatment adherence as an outcome, providing low‐certainty evidence that the intervention may have little or no effect (RR 1.01, 95% CI 0.98 to 1.04; n = 223; downgraded twice due to risk of bias; Analysis 4.3).
4.1. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 1: Health behaviour change – mother taking any type of antiretroviral (ARV) (34–36 weeks' gestation)
4.2. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 2: Health behaviour change – mother taking any type of ARV (6–8 weeks postpartum)
4.3. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 3: Health behaviour change – infant ARV/prevention of mother‐to‐child transmission treatment adherence (6 weeks postpartum)
Pooled analyses of two studies carried out in Kenya provided low‐certainty evidence that TCC via mobile devices may have little or no effect on increasing rates of infant HIV testing in comparison to standard care (RR 1.04, 95% CI 0.95 to 1.13; n = 838; downgraded twice due to risk of bias; Analysis 4.4) (Kassaye 2016; Odeny 2014). Repeating this analysis excluding the cluster RCT (Kassaye 2016), resulted in very little change from the original pooled estimate (RR 1.08, 95% CI 1.00 to 1.16; n = 378).
4.4. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 4: Health behaviour change – infant HIV tested (6–8 weeks postpartum)
Service utilisation
One trial conducted in Kenya provided very low‐certainty evidence relating to the effect of a text messaging intervention on the proportion of births occurring in health facilities, with CI encompassing both potential intervention benefit and harm (RR 0.85, 95% CI 0. 62 to 1.15; n = 134; downgraded twice due to risk of bias and once due to imprecision; Analysis 4.6) (Kassaye 2016). This trial also provided low‐certainty evidence that the intervention may result in a slight increase in the mean number of face‐to‐face or mobile communications with a healthcare worker during ANC (MD 1.50, 95% CI –0.36 to 3.36; n = 297; downgraded twice due to risk of bias; Analysis 4.7).
4.6. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 6: Service utilisation – intrapartum care: birth in health facility
4.7. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 7: Service utilisation – antenatal care: mean number of face‐to‐face or mobile communications with healthcare workers
One trial carried out among pregnant women living with HIV in Kenya found that a text messaging intervention may increase attendance to appointments for postpartum care (RR 1.66, 95% CI 1.02 to 2.70; n = 381; moderate‐certainty evidence – downgraded due to the low number of events recorded; Analysis 4.5) (Odeny 2014).
4.5. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 5: Service utilisation – postnatal care: attendance at postpartum care appointment (6–8 weeks postpartum)
Health status and well‐being
Based on low‐certainty evidence from a single trial in Kenya, TCC via mobile devices may make little or no difference to neonatal health (RR for neonatal death or stillbirth: 1.12, 95% CI 0.39 to 3.28; n = 381; downgraded twice for imprecision; Analysis 4.8) (Odeny 2014). Given the wide CI consistent with both benefit and harm, there is uncertainty about what the true effect might be. Pooled analyses of two trials in Kenya also provided very low‐certainty evidence, meaning we are uncertain as to whether TCC via mobile devices has an effect on the proportion of infants testing HIV positive (RR 0.54, 95% CI 0.11 to 2.56; n = 852; downgraded one level due to risk of bias and two levels due to imprecision; Analysis 4.9). The CI encompassed both benefit and harm, meaning we are uncertain as to what the true effect might be (Kassaye 2016; Odeny 2014). Repeating this analysis excluding the cluster RCT (Kassaye 2016), resulted in very little change from the original pooled estimate (RR 0.64, 95% CI 0.11 to 3.80; n = 378).
4.8. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 8: Health status and well‐being – neonatal health: neonatal death/stillbirth
4.9. Analysis.

Comparison 4: Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV), Outcome 9: Health status and well‐being – neonatal health: infant HIV test positive (6–8 weeks postpartum)
Targeted client communication via mobile devices versus non‐digital targeted communication
Table 5 presents the evidence relating to the effect of TCC via mobile devices compared to non‐digital targeted communication among pregnant and postpartum women living with HIV for the outcomes of maternal mortality and morbidity, neonatal and morbidity, attendance for ANC (including eMTCT care), receipt of intrapartum care, unintended consequences, neonate HIV status, and adherence to ARV therapy.
Health behaviours
No studies reported health behaviour outcomes for the comparison of TCC via mobile devices compared with non‐digital targeted communication among pregnant and postpartum women living with HIV.
Service utilisation
No studies reported service utilisation outcomes for the comparison of TCC via mobile devices compared with non‐digital targeted communication among pregnant and postpartum women living with HIV.
Health and well‐being
No studies reported health and well‐being outcomes for the comparison of TCC via mobile devices compared with non‐digital targeted communication among pregnant and postpartum women living with HIV.
Targeted client communication via mobile devices versus digital non‐targeted communication
Table 6 presents the evidence relating to the effect of TCC via mobile devices compared to digital non‐targeted communication among pregnant and postpartum women living with HIV for the outcomes of maternal mortality and morbidity combined, neonatal and morbidity combined, attendance for ANC (including eMTCT care), receipt of intrapartum care, unintended consequences, neonate HIV status, and adherence to ARV therapy.
Health behaviour
One trial conducted in Kenya among women living with HIV recruited within 24 hours of birth examined the effect of a two‐weekly phone calls about PMTCT compared with standard healthcare messages. Based on this study, TCC via mobile devices may be beneficial for infant ARV/PMTCT treatment adherence at six weeks postpartum compared with digital non‐targeted communication (RR 1.26, 95% CI 1.07 to 1.48; n = 150; low‐certainty evidence – downgraded twice due to risk of bias with the trial at unclear or high risk of bias across all applicable domains; Analysis 5.1) (Kebaya 2014).
5.1. Analysis.

Comparison 5: Digital targeted client communication (TCC) compared to digital non‐targeted client communication (pregnant women with HIV), Outcome 1: Health behaviour – infant antiretroviral/prevention of mother‐to‐child transmission adherence (6 weeks after delivery)
Service utilisation
One trial provided low‐certainty evidence that the intervention may increase attendance to appointments for postpartum care at 10 weeks (RR 1.86, 95% CI 1.34 to 2.58; n = 150; downgraded twice for risk of bias; Analysis 5.2) (Kebaya 2014).
5.2. Analysis.

Comparison 5: Digital targeted client communication (TCC) compared to digital non‐targeted client communication (pregnant women with HIV), Outcome 2: Service utilisation – postnatal care: attendance at postpartum care appointment (10 weeks postpartum)
Health and well‐being
No studies reported health status and well‐being outcomes for the comparison of TCC via mobile devices compared with digital non‐targeted communication among pregnant and postpartum women living with HIV.
Acceptability
No studies among pregnant and postpartum women living with HIV reported measures of acceptability.
Resource use
No studies among pregnant and postpartum women living with HIV reported on resource use.
Unintended consequences
No studies among pregnant and postpartum women living with HIV reported on unintended consequences or adverse outcomes.
Equity considerations
All three trials were conducted in Kenya (a lower‐middle income country), and it is not possible to assess the applicability of these findings to other settings. One study specifically stated that it excluded women without a phone, who did not receive ANC, and who could not read or did not have someone to read, making it highly likely that particularly vulnerable women were unable to take part in this trial (Odeny 2014). The other two studies provided little information on exclusion criteria, however, all trials recruited from healthcare facilities, meaning that those not accessing care will not have had the opportunity for inclusion.
Parents or carers of children aged less than five years
Targeted client communication via mobile devices versus standard care
Table 7 presents the evidence relating to the effect of TCC via mobile devices compared to standard care or no intervention among parents of children aged under five years for the outcomes of child morbidity and mortality, child nutritional status, breastfeeding, clinic attendance for necessary healthcare, hygiene practices, correct treatment taken, and unintended consequences.
Health behaviours
No studies reported health behaviour outcomes for the comparison of TCC via mobile devices compared with standard care among parents of children under five years of age.
Service utilisation
Overall, for the outcome of attendance to services for necessary health care, we found low‐certainty evidence for a modest intervention benefit based on the pooled results of 10 studies concerned with attendance for childhood vaccinations at six to 12 months and attendance for HIV medical appointments (among HIV‐positive and HIV‐exposed infants) (RR 1.21, 95% CI 1.08 to 1.34; n = 5660; downgraded for risk of bias and inconsistency; Analysis 6.1) (Ahlers‐Schmidt 2012; Bangure 2015; Bigna 2015; Brown 2016; Domek 2016; Gibson 2017; Haji 2016; Hannan 2016; Hofstetter 2015a; Stockwell 2015). Given the very high degree of inconsistency indicated by the I2 value (I2 = 91%), we also present subgroup analyses by type of service and timing of vaccination, described below.
6.1. Analysis.

Comparison 6: Digital targeted client communication (TCC) compared to standard care (parents of children aged under five years), Outcome 1: Attendance for necessary healthcare
Pooled analyses of five studies (conducted in the USA, Zimbabwe, Guatemala, and Kenya) indicated that TCC via mobile devices may result in a slight increase in attendance for vaccinations at six months (RR 1.14, 95% CI 1.01 to 1.28; n = 1586; low‐certainty evidence – downgraded due to risk of bias and inconsistency; Analysis 6.1) (Ahlers‐Schmidt 2012; Bangure 2015; Domek 2016; Haji 2016; Hannan 2016). The I2 value was 63%, with one study reporting an point estimate indicative of reduced vaccination rates in the intervention arm (Ahlers‐Schmidt 2012), and the other four studies reporting effect estimates indicative of benefit. Excluding the cluster RCT (Haji 2016) from this analysis resulted in a negligible change in the pooled effect estimate (RR 1.13, 95% CI 0.96 to 1.32).
Four studies (conducted in Nigeria, Kenya, USA) provided low‐certainty evidence that TCC via mobile devices may increase attendance for vaccinations at 12 months (RR 1.24, 95% CI 1.02 to 1.52; n = 3832) (Brown 2016; Gibson 2017; Hofstetter 2015a; Stockwell 2015) (Analysis 6.1). This body of evidence was downgraded due to risk of bias and inconsistency between individual effect estimates (I2 = 92%), with two trials reporting effect estimates consistent with intervention benefit (Brown 2016; Stockwell 2015), and two trials reporting little or no difference with CI encompassing no effect (Gibson 2017; Hofstetter 2015a). Repeating this analysis without including the cluster RCTs (Brown 2016; Gibson 2017), resulted in little change to the effect estimate, but a widening of the CI (RR 1.28, 95% CI 0.82 to 2.01).
Pooled analyses of four RCTs (conducted in the USA, Nigeria, and Kenya) provided moderate‐certainty evidence that TCC via mobile devices probably has a modest effect on increasing 'timeliness of vaccination' (vaccine receipt within a certain time period) compared with standard care (RR 1.18, 95% CI 1.04 to 1.34; n = 2400; downgraded due to risk of bias; Analysis 6.2) (Ahlers‐Schmidt 2012; Eze 2015; Gibson 2017; Stockwell 2015). Excluding the cluster RCT from this analysis (Gibson 2017) resulted in a negligible change in the pooled effect estimate (RR 1.19, 95% CI 0.96 to 1.46).
6.2. Analysis.

Comparison 6: Digital targeted client communication (TCC) compared to standard care (parents of children aged under five years), Outcome 2: Timeliness of vaccination
One trial indicated that TCC via mobile devices probably increases the attendance of HIV‐positive and HIV‐exposed children to medical appointments in Cameroon (RR 1.63, 95% CI 1.26 to 2.11; n = 242; moderate‐certainty evidence – downgraded due to imprecision given the small number of events; Analysis 6.1) (Bigna 2015).
One study conducted in the USA provided very low‐certainty evidence meaning we are uncertain as to whether the two‐way communication phone and texting intervention had an effect on attendance to the emergency department in the six months after birth (no attendance: RR 1.32, 95% CI 1.03 to 1.70; n = 129; downgraded due to risk of bias, imprecision resulting from a small number of events, and indirectness (a single study conducted in a high‐income country; Analysis 6.3) (Hannan 2016).
6.3. Analysis.

Comparison 6: Digital targeted client communication (TCC) compared to standard care (parents of children aged under five years), Outcome 3: Service utilisation – no emergency department attendance (6 months)
Health and well‐being
No studies reported health and well‐being outcomes for the comparison of TCC via mobile devices compared with standard care among parents of children under five years of age.
Targeted client communication via mobile devices versus non‐digital targeted communication
Table 8 presents the evidence relating to the effect of TCC via mobile devices compared to non‐digital targeted communication among parents of children under five years of age for the outcomes of child morbidity and mortality, child nutritional status, breastfeeding, clinic attendance for necessary healthcare, hygiene practices, correct treatment taken, and unintended consequences.
Health behaviours
One trial carried out in India comparing the effect of providing oral health education via text messages with the provision of the same information via pamphlets suggests that the intervention may have little or no effect on children's oral health at four weeks, measured with the VPI (MD –2.10, 95% CI –7.54 to 3.34; n = 143; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 7.1) (Sharma 2011).
7.1. Analysis.

Comparison 7: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (parents of children aged under five years), Outcome 1: Health behaviour change – oral health in children (Visible Plaque Index, [0–100%], low = good)
Service utilisation
Based on one study, there was low‐certainty evidence that TCC via mobile devices might result in a slight increase in attendance for vaccinations compared with non‐digital targeted communication (in the form of stickers) (RR 1.13, 95% CI 1.00 to 1.28; n = 744; downgraded twice due to risk of bias; Analysis 7.2) (Haji 2016).
7.2. Analysis.

Comparison 7: Digital targeted client communication (TCC) compared to non‐digital targeted client communication (parents of children aged under five years), Outcome 2: Service utilisation – attendance for vaccinations at 14 weeks
Health and well‐being
No studies reported health and well‐being outcomes for the comparison of TCC via mobile device compared with non‐digital targeted communication among parents of children under five years of age.
Targeted client communication via mobile devices versus digital non‐targeted communication
Table 9 presents the evidence relating to the effect of TCC via mobile devices compared to digital non‐targeted communication among parents of children under five years of age for the outcomes of child morbidity and mortality, child nutritional status, breastfeeding, clinic attendance for necessary healthcare, hygiene practices, correct treatment taken, and unintended consequences.
Health behaviour
No studies reported health behaviour outcomes for the comparison of TCC via mobile device compared with digital non‐targeted communication among parents of children under five years of age.
Service utilisation
One trial in Hawaii compared vaccination reminders delivered via SMS with the control arm receiving general health information for their babies. This study found that SMS reminders may reduce attendance for vaccinations at seven months; however, the CI encompassed both benefit and harm (RR 0.63, 95% CI 0.33 to 1.20; n = 40; low‐certainty evidence – downgraded due to risk of bias and imprecision; Analysis 8.1) (Niederhauser 2015).
8.1. Analysis.

Comparison 8: Digital targeted client communication (TCC) compared to digital non‐targeted client communication (parents of children aged under five years), Outcome 1: Service utilisation – attendance for vaccinations at 7 months
Health status and well‐being
No studies reported health status and well‐being outcomes for the comparison of TCC via mobile device compared with digital non‐targeted communication among parents of children under five years of age.
Acceptability and satisfaction
There was generally a high level of acceptability and satisfaction with the interventions assessed among parents of children aged under five years. One trial in the USA of text message reminders for childhood vaccinations interviewed 18/50 participants randomised to the intervention group, all of whom reported that they found the messages 'helpful' or 'somewhat helpful' and that they would be willing to receive text message reminders in the future (Ahlers‐Schmidt 2012). Most (93%) intervention recipients in one trial of SMS immunisation reminders in Zimbabwe perceived the use of SMS as 'very beneficial' (Bangure 2015). One study of SMS vaccination reminders in Guatemala reported that 99.1% of intervention parents agreed that they would be interested in receiving text message reminders in the future and 67.5% said that they would be willing to pay for future SMS reminders (Domek 2016). One study in Kenya reported that 97.5% of participants thought the number of reminders was 'just right' (SMS vaccination reminders were sent three days and the day before each scheduled immunisation visits) (Gibson 2017). Another study involving reminders for the measles, mumps, and rubella (MMR) vaccination in the USA reported that 86.8% of participants liked the messages and 9.3% did not like them (Hofstetter 2015a). Finally another US study reported that nearly all intervention recipients (98.0%) were very satisfied or satisfied with the messages which sought to increase attendance for childhood influenza vaccination (Stockwell 2015).
Resource use
Five studies reported on the resource use of the interventions. One study reported a cost of USD 59.22 for all the messages (n = 1368) (Bangure 2015). Another reported a cost of USD 0.27 per child for the project (Haji 2016). One study reported that the intervention was estimated to save between USD 51,030 and USD 104,277 in healthcare costs (Hannan 2016). Another study did not report the total costs but noted that text messaging was the most efficient intervention when both the direct costs of the intervention and staff working time were considered (Bigna 2015). Only one study reported on a cost‐effectiveness analysis and found that projected cost of using SMS reminders was about 25% what it would cost to use Junior Community Health Extension Workers (CHEWs) for functional home visits in one year (Eze 2015).
Unintended consequences
No studies among parents of children aged under five years reported on unintended consequences.
Equity considerations
The trials targeting childhood immunisations were conducted in a range of high‐, lower‐middle‐, and low‐income countries. Two studies specifically included low‐income families (Hannan 2016; Stockwell 2015), for example, the intervention examined by Hannan 2016 targeted low‐income first‐time mothers. A third study assessing text message reminders for immunisation recruited from two public health clinics in Guatemala City serving a publicly insured and low‐income population (Domek 2016). Of the participants involved in the text messaging trial conducted in Kenya, 77% were unemployed and 49% had only primary level education (Haji 2016).
Sensitivity analyses
We planned to conduct a sensitivity analysis only including studies at low risk of bias (those scored at low risk of bias for the sequence generation, allocation concealment, and incomplete outcome data domains). The following trials had a low risk of bias: Yudin 2017 (pregnant and postpartum women); Odeny 2014 (pregnant and postpartum women living with HIV); and Bigna 2015; Domek 2016; Gibson 2017; Hofstetter 2015a (parents of children aged under five years). Therefore, only the comparison of TCC via mobile devices and standard care for outcome of uptake of childhood vaccinations at 12 months could undergo sensitivity analyses. As reported above, the pooled results of four studies was RR 1.28 (95% CI 0.82 to 2.01) (Brown 2016; Gibson 2017; Hofstetter 2015a; Stockwell 2015). However, when repeating this analysis pooling only the two studies at low risk of bias, the effect estimate was attenuated to RR 1.03 (95% CI 0.98 to 1.09; n = 2802) (Gibson 2017; Hofstetter 2015a).
Studies not contributing usable data
All included studies provided data that could be analysed using meta‐analyses for examining the intervention effect on health behaviour, service utilisation, health and well‐being, or a combination of these, meaning that conclusions relating to effectiveness have been made based on all available data from included studies.
Discussion
Summary of main results
We included 27 studies in our review. For pregnant and postpartum women and parents of children aged under five years, trials were conducted in a range of low‐ to high‐income countries. All trials among pregnant women living with HIV were conducted in one lower‐middle income country.
Pregnant and postpartum women
See Table 1; Table 2; and Table 3.
Targeted client communication delivered by mobile device versus standard care
Women receiving TCC via mobile devices may breastfeed more in settings where breastfeeding is less common. They may go to more ANC appointments, and may use skilled birth attendants more in settings where this is less common. We do not know if TCC via mobile devices affects women's or infant morbidity or mortality because the evidence is of very low certainty.
Targeted client communication via mobile devices compared to non‐digital targeted client communication or digital non‐targeted communication
When compared to non‐digital TCC, TCC via mobile devices may have little or no effect on breastfeeding, and may improve maternal and newborn health. We do not know what the effect is on health service use because the evidence is missing.
We do not know what the effect of TCC via mobile devices is on women's use of a skilled birth attendant when compared to digital non‐targeted communication because the evidence is of very low certainty. TCC via mobile devices may make little or no difference to whether women attendance appointments for vaccination during pregnancy when compared to digital non‐targeted communication. We do not know what the effect of TCC via mobile devices is on women's or babies' morbidity or mortality or breastfeeding when compared to digital non‐targeted communication because the evidence is missing.
The effects of TCC via mobile devices on unintended consequences is unknown due to lack of studies. Only one study reported on resource use associated with the intervention. Satisfaction with the intervention was generally high when assessed, but few studies conducted in low‐income settings reported on measures of satisfaction.
Pregnant and postpartum women living with HIV
See Table 4; Table 5; and Table 6.
Targeted client communication delivered by mobile device versus standard care
Women who receive TCC via mobile devices may go to slightly more ANC appointments. We do not know what the effect of TCC via mobile devices is on whether women give birth in a health facility because the evidence was of very low certainty. We do not know what the effect of TCC via mobile devices is on babies' health or mortality because the evidence is of very low certainty. No studies reported on maternal mortality or morbidity. TCC via mobile devices may make little or no difference to maternal and infant adherence to ARV therapy.
Targeted client communication via mobile devices compared to non‐digital targeted client communication or digital non‐targeted communication
We do not know what the effect of TCC via mobile devices is on women's or babies' health or mortality, use of healthcare services during pregnancy, or whether women use skilled attendants at birth because the evidence is missing. Women who receive TCC via mobile devices may follow their baby's ARV treatment better than women who receive digital non‐targeted communication.
For pregnant and postpartum women living with HIV, we are uncertain of the satisfaction and resource use associated with receiving TCC via mobile devices, or the effects on unintended consequences, due to lack of evidence.
Parents or carers of children aged under five years
See Table 7; Table 8; and Table 9.
Targeted client communication delivered by mobile device versus standard care
We do not know what the effect of parental receipt of TCC via mobile devices is on breastfeeding, children's health or nutrition, whether they received the right treatments, or parents' hygiene practices because the evidence is missing. Parents who receive TCC via mobile devices may take their children to more healthcare services, such as vaccination appointments; however, the results varied widely between studies.
Targeted client communication via mobile devices compared to non‐digital targeted client communication or digital non‐targeted communication
We do not know what the effect of TCC via mobile devices is on breastfeeding, children's health or nutrition, or whether they received the correct treatments, because the evidence in missing. Parents who receive TCC via mobile devices may take their children to more vaccination appointments compared to parents who receive non‐digital targeted communication although the effects vary. There is little or no difference observed between these groups in terms of oral hygiene practices. Parents who receive TCC via mobile devices may take their children to fewer vaccination appointments than parents who receive digital non‐targeted communication, but it is possible that the intervention makes little or no difference.
The effects of TCC via mobile devices on unintended consequences is unknown due to lack of studies. Acceptability and satisfaction with the intervention was high in the six studies that reported these outcomes. Costs were low in the five studies that reported on intervention costs.
Overall completeness and applicability of evidence
This review includes evidence from 27 studies, 11 of which were conducted among pregnant and postpartum women, three among pregnant and postpartum women living with HIV, and 13 among parents of children aged under five years. In collating those trials relating to the same population, employing the same comparison groups, and measuring the same outcomes, these specific bodies of evidence were generally made up of only a small number of studies, thereby limiting the extent to which conclusions can be made.
With the exception of trials among pregnant and postpartum women living with HIV, all of which were carried out in Kenya, there was generally a varied geographical spread for where studies were conducted, with representation of low‐ to high‐income countries. Furthermore, the trials recruited from a mix of community and healthcare settings.
No trials targeted or measured correct treatment of childhood illness or child nutritional outcomes. No trials reported measuring unintended consequences or adverse events. However, HIV and reproduction can be sensitive topics and there is the potential for harm resulting from interventions concerned with these issues. In the accompanying review focusing on reproductive and sexual health, one trial among women living with HIV reported one participant withdrew due to her undisclosed HIV status being compromised (Palmer in preparation).
Quality of the evidence
Using GRADE methodology, we assessed the certainty of the evidence for all outcomes. Among the pregnant and postpartum population, there was low or very low‐certainty evidence relating to the effect of TCC via mobile devices for most outcomes. There was moderate‐certainty evidence for only three outcomes among this population, generally based on the results of a single trial. For pregnant and postpartum women living with HIV, the evidence for all outcomes except one were considered of low or very low certainty. Based on trials conducted among parents of children aged under five years, for most outcomes the evidence was of low or very low certainty. Across all three populations, the most common reasons for downgrading were risk of bias of the studies and imprecision of the effect estimates.
Given the nature of the interventions, participant blinding was generally unfeasible. The trials among pregnant and postpartum women primarily depended on self‐reported outcome measures. Therefore, among these studies there is risk of response bias which could result in an overestimation of intervention benefit. Most trials among parents of children aged under five years concerned with increasing uptake of childhood vaccination were able to use objective outcome measures based on clinic attendance recording systems, meaning that for these studies, having unblinded intervention recipients would be unlikely to bias the effect estimates recorded. Few other trials used objective outcomes, which would be less subject to bias than self‐reported measures.
Potential biases in the review process
There were limited resources to follow‐up with authors of reports that did not provide sufficient information for data extraction/risk of bias assessments. Furthermore, publication bias, whereby trials with positive findings are more likely to be published, may have biased the selection of included studies in this review. However, efforts were made to overcome this through searching clinical trial registries for prospectively registered trials.
Agreements and disagreements with other studies or reviews
As with other communication and behaviour change interventions, a challenge in synthesising the results of TCC interventions delivered by mobile device is the heterogeneity of interventions, ranging from reminders to educational and more complex behaviour change support. As evidenced by the heterogeneity of some pooled estimates in our review and similar reviews (Amankwaa 2018; McFadden 2017), this can result in real differences in effects of interventions even when they use the same delivery mechanisms and target the same outcomes.
There was uncertain evidence relating to the effect of TCC via mobile devices for improving postpartum contraception use. The CI was wide so modest benefits similar to those reported in other Cochrane Reviews of contraception interventions delivered by mobile phone for general populations of women or women postabortion cannot be excluded (Palmer in preparation; Smith 2015).
Our finding that TCC delivered by mobile devices may improve exclusive breastfeeding at three months in settings where exclusive breastfeeding rates are modest is consistent with one Cochrane Review which found that breastfeeding support is effective in increasing exclusive breastfeeding and the duration of breastfeeding. We note, however, that the trial of TCC included in our review was delivered by mobile phone calls and the Cochrane Review found that face‐to‐face support was more effective than telephone support (McFadden 2017).
This review showed TCC delivered by mobile devices may increase abstinence from smoking in pregnancy, but evidence is low certainty. These findings are consistent with the effects of TCC delivered by mobile phone which doubles continuous abstinence from smoking among general populations of smokers willing to make a quit attempt (Free 2011; Palmer 2018b; Whittaker 2016). Effective smoking cessation support delivered by mobile phone includes a range of behavioural change techniques, and the behaviour change techniques found in effective psychosocial support for smoking cessation in pregnant women have also been described (Lorencatto 2012). Since our search was completed, one trial of TCC by mobile phone for smoking cessation in pregnant women compared to digital non‐targeted communication reported an increase in validated no smoking in the last seven days at three months (OR 1.47, 95% CI 1.21 to 1.78) (Abroms 2017a) and one recent systematic review including the Abroms 2017a trial reported an increase in smoking cessation during pregnancy (pooled OR 1.59, 95% CI 1.07 to 2.38) (Griffiths 2018). Our review findings are also consistent with the findings of one systematic review of health education and psychosocial interventions, not specifically delivered by mobile devices, for smoking cessation during pregnancy which found evidence of a beneficial intervention effect (Chamberlain 2017).
Our finding of a lack of effect of TCC via mobile devices for alcohol reduction in pregnancy is consistent with one Cochrane Review of psychological and education interventions for reducing alcohol intake, not specifically delivered by mobile devices, which found no intervention effects for most outcomes (Stade 2009).
The effect of TCC via mobile devices for improving antenatal and postnatal adherence to ARV therapy among women living with HIV was uncertain. The effects on ARV/PMTCT adherence in infants were mixed. One previous Cochrane Review examining text messaging for adherence to ARV therapy in populations of all ages reported evidence of beneficial effects from two trials (Horvath 2012), but further trials of ARV therapy adherence interventions delivered by mobile phone have been published since 2012, with mixed results reported in more recent systematic reviews (Quintana 2018; Shah 2019). One systematic review reported an increase in adherence for adults based on a pooled analysis of interventions delivered by SMS, but uncertain effects of interventions delivered by voice message (Amankwaa 2018).
The finding that TCC via mobile devices may improve service utilisation, such as attendance to antenatal and postnatal care appoints among pregnant and postpartum women, and attendance for infant HIV medical appointments, is in accordance with our findings relating to other populations (Palmer in preparation), and previous research findings that mobile phone‐based reminders improve healthcare appointment attendance (Free 2013b; Gurol‐Urganci 2013).
Some feasibility studies have shown promise for TCC delivered by mobile devices altering nutrition in infants or children (Singh 2014). However, we did not identify any RCTs of nutritional interventions or trials reporting infant or child nutrition outcomes that met our inclusion criteria.
Our findings that TCC via mobile devices among parents of children aged under five years may have modest effects on increasing attendance for childhood immunisations and necessary health care is consistent with the findings of a previous review of mobile phone‐based interventions (Free 2013a), and a Cochrane Review examining face‐to‐face interventions for parents about childhood vaccinations, which also found evidence for small intervention benefits (Kaufman 2018). However, in our review, the effects varied in different studies. This could be due to bias, as both of the trials that found a positive effect were at unclear risk of bias for random sequence generation. It is also possible that there was a ceiling effect in the Gibson 2017 trial due to the high uptake of vaccination in the control arm (82%) leaving less scope for extra improvement to be demonstrated. It may also be that for some vaccinations remembering an appointment is not the main barrier to uptake, so simple reminders would not be expected to improve attendance. The Hofstetter 2015a trial in the USA was targeting MMR, which in the context of vaccine concerns might be intractable to improvement using reminder messages only. Educational messages targeting parental concerns about the MMR vaccine could be more relevant.
Authors' conclusions
Implications for practice.
We cannot make strong recommendations for implementation of targeted client communication (TCC) delivered by mobile devices on the basis of this review as the certainty of the evidence was primarily very low or low.
TCC interventions delivered by mobile devices, such as appointment reminders have already been implemented in many settings. Where healthcare providers and policy makers are considering implementation, we suggest prioritising interventions for which evidence is suggestive of an improvement in outcomes, such as TCC delivered by mobile devices for general populations of pregnant women for antenatal care attendance, skilled attendance at birth, and for childhood vaccinations. However, careful consideration should be given to the costs and resources needed in conjunction with the limited strength of evidence for gains in service use and health behaviours. Few studies in this review reported on costs, but those that did so generally indicated costs to be low. Furthermore, the interventions delivered in trials which observed evidence for a small increase in attendance for vaccinations (parents of children aged under five years) compared to standard care, consisted of simple reminders which may be more straightforward to implement than more complex interventions. The text messaging intervention evaluated by Odeny 2014 consisted of just 14 messages sent to pregnant women living with HIV from 28 weeks' gestation to six weeks postdelivery, but seemed to result in gains in relation to attendance for the postpartum appointment, and infant HIV testing. In other areas of health behaviour change, such as smoking cessation, effective TCC delivered by mobile devices has been shown to be highly cost effective (Guerriero 2013). The majority of TCC interventions in this review were delivered by text message (SMS). The World Health Organization and the International Telecommunication Union have developed guidance on implementing SMS‐based smoking cessation support at scale, and much of this guidance would apply to implementing any SMS health platform (WHO/ITU 2015). Nonetheless, setting up, maintaining and monitoring SMS platforms, and delivery requires resources and incurs ongoing costs, which can represent a considerable burden and challenge in some settings. Furthermore, the findings of one complementary synthesis of qualitative research which explored clients' perceptions and experiences of targeted communication via mobile devices on topics related to reproductive, maternal, newborn, child, and adolescent health (RMNCAH) (Ames 2019), highlights continuing barriers to the widespread implementation of TCC via mobile devices. Despite the high rate of mobile phone ownership globally, use of these devices can still be limited by poor access to mobile networks and the internet, phones breaking, the inability to afford airtime, and the inability to charge the device. Given that there are contexts in which uninterrupted access to mobile devices cannot be guaranteed, it may be premature to roll out TCC via mobile devices if it is at the expense of other channels of communication.
For some outcomes, the findings suggested intervention benefits may be gained only in settings where the behaviour targeted is relatively uncommon and there is greater scope for improvement. For example, while TCC via mobile devices had little or no effect in a low‐risk setting where the majority of births already occurred with a skilled attendant present, there was evidence that the intervention increased skilled birth attendance in a moderate‐risk urban setting where two‐thirds of births occurred with skilled attendance (but not in the rural area included in the same study). Therefore, background levels of health service use and behaviours (and existing health facility infrastructure), should be considered prior to implementation. While the majority of comparisons in the review were between TCC via mobiles devices and standard care/no intervention, consideration should also be given to the apparent lack of intervention benefit when the comparison group is in receipt of something quite similar to the intervention. For example. the trial by Niederhauser 2015 examined the effect of a TCC mobile device‐delivered intervention involving childhood vaccination reminders at four weeks and two weeks prior to the routine vaccination appointments, compared with the control group who received well baby messages. However, the study report states that the participants in both groups were also receiving the "routine reminders that they receive from their healthcare providers," therefore, the finding of no additional benefit of the reminder messaging intervention, and perhaps even a slight negative effect, might be considered unsurprising. This highlights that an understanding of what is delivered as part of existing medical practice, which may vary between contexts, is important to prevent misplaced interventions which result in few or no gains.
Healthcare providers and policy makers should be especially cautious regarding the implementation of interventions specifically targeting pregnant women living with HIV. While the evidence is of low or very low certainty, the confidence intervals around the effect estimates suggest that TCC delivered by mobile devices may have little benefit or no effect. Due to the sensitivity and stigma associated with HIV status, it is essential that such interventions are designed so that content and delivery ensures confidentiality of sensitive material. In contexts where women's access to phones is controlled by others, or where phones are shared, it may not be feasible for content to remain private. In such circumstances it may be better to include HIV‐positive pregnant women in mobile phone interventions for general populations of pregnant women, such as for attendance for antenatal care, rather than targeting them in isolation on the basis of their HIV status. This is consistent with the findings of one synthesis of qualitative research concerned with perceptions and experiences of TCC via mobile devices on topics related to RMNCAH (Ames 2019). Practical considerations for messaging concerned with stigmatised or personal health conditions included the use of neutral language, and tailoring the content, timing, and frequency of the messages (Ames 2019).
No studies across the three populations in this review reported on unintended consequences or adverse events. However, given that reproduction can be a sensitive topic and HIV is subject to considerable stigma, there is the potential for harm resulting from interventions concerned with these issues. For example, in the accompanying review focusing on reproductive and sexual health, a trial among women living with HIV reported that one participant withdrew due to her undisclosed HIV status being compromised. Furthermore, globally one in three women has experienced intimate partner violence in their lifetime and pregnancy is a time when domestic violence can escalate (WHO 2013). There is the potential that TCC on sensitive topics could result in further escalations in abuse for women in abusive relationships. Consequently, those implementing interventions should consider how the risks of such potential unintended consequences can minimised and monitored.
Issues relating to language and literacy have been highlighted in this review as potential barriers in achieving equity of access and benefit from communication‐based interventions. This is also a finding of the qualitative synthesis of clients' perceptions experiences with such interventions (Ames 2019), in which language, literacy, techno‐literacy, or a combination of these were raised as potential limiting factors for accessing these types of interventions. Based on this, some participants reported a preference for voice calls in which they could request clarifying information. Where interventions are being implemented, this should be accompanied by monitoring and evaluation of impact (including both benefits and harms), equity, and associated costs.
Implications for research.
The effect of TCC delivered by mobile devices on health service use (antenatal care, delivery in a health facility) and vaccinations at six and 12 months requires further assessment. The vaccination interventions in this review primarily provided reminders. Further TCC interventions, which also target attitudinal barriers to childhood vaccinations, should be evaluated.
Given the somewhat equivocal evidence relating to the effects of TCC delivered by mobile devices for pregnant women living with HIV, future research should explore whether carefully designed interventions can improve outcomes in this population, and the contexts in which this can occur.
We found no trials of TCC delivered by mobile devices that targeted treatment of childhood illness, and infant and child nutrition. Therefore, research is needed to evaluate whether well‐designed TCC interventions targeting these behaviours can be effective.
Future research should ensure potential unintended consequences and adverse events are considered in the design of the intervention and evaluation, so that risks are minimised and any such events that do occur are adequately captured.
Researchers should ensure that interventions are adequately described in sufficient detail for them to be replicated, for example, with reference to guidance on reporting interventions (Agarwal 2016; Hoffmann 2014).
Both trials and implementation research should evaluate equity in access to, and the effects of, TCC delivered by mobile devices for maternal, neonatal, and child health.
Where interventions have been shown to be effective, cost‐effectiveness analysis of TCC delivered by mobile device for maternal, neonatal, and child health is needed.
Further high‐quality trials are warranted to evaluate the effects of TCC by mobile devices on behaviours such as postpartum contraception use and breastfeeding. Given that lay support is associated with increased exclusive breastfeeding and duration of breastfeeding, trials of lay support for breastfeeding delivered by mobile devices could be considered (McFadden 2017).
History
Review first published: Issue 8, 2020
Notes
The protocol for this review is based on standard text and guidance provided by Cochrane Consumers and Communication (Ryan 2016).
Acknowledgements
We thank the editors and staff of Cochrane Consumers and Communication, particularly Bronwen Merner, Ann Jones, and Rebecca Ryan for their input into the protocol.
We are grateful to the Guideline Development Group and External Review Group of the WHO Guideline on digital interventions for health system strengthening for their constructive feedback in formulating the guiding questions for this systematic review. Cochrane Response, an evidence services unit operated by Cochrane provided screening and data extraction services for this review. This work was funded by the UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored program executed by the World Health Organization (WHO). We thank John Eyers for designing and running the search strategies for this review.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Cell Phones] this term only 535
#2 MeSH descriptor: [Smartphone] this term only 73
#3 MeSH descriptor: [MP3‐Player] this term only 19
#4 MeSH descriptor: [Computers, Handheld] this term only 203
#5 ((cell* or mobile*) near/1 (phone* or telephone* or technolog* or device*)):ti,ab,kw 1601
#6 (handheld or hand‐held):ti,ab,kw 1174
#7 (smartphone* or smart‐phone* or cellphone* or mobiles):ti,ab,kw 749
#8 ((personal near/1 digital) or (PDA near/3 (device* or assistant*)) or "MP3 player*" or "MP4 player*"):ti,ab,kw 188
#9 (samsung or nokia):ti,ab,kw 44
#10 (windows near/3 (mobile* or phone*)):ti,ab,kw 3
#11 android:ti,ab,kw 155
#12 (ipad* or i‐pad* or ipod* or i‐pod* or iphone* or i‐phone*):ti,ab,kw 403
#13 (tablet* near/3 (device* or computer*)):ti,ab,kw 187
#14 MeSH descriptor: [Telemedicine] this term only 1528
#15 MeSH descriptor: [Videoconferencing] this term only 134
#16 MeSH descriptor: [Webcasts as Topic] this term only 16
#17 MeSH descriptor: [Text Messaging] this term only 428
#18 MeSH descriptor: [Telenursing] this term only 25
#19 (mhealth or m‐health or "mobile health" or ehealth or e‐health or "electronic health"):ti,ab,kw 1305
#20 (telemedicine or tele‐medicine or telehealth or tele‐health or telecare or tele‐care or telenursing or tele‐nursing or telepsychiatry or tele‐psychiatry or telemonitor* or tele‐monitor* or teleconsult* or tele‐consult* or telecounsel* or tele‐counsel* or telecoach* or tele‐coach*):ti,ab,kw 3320
#21 (videoconferenc* or video‐conferenc* or webcast* or web‐cast*):ti,ab,kw 418
#22 (((text* or short or voice or multimedia or multi‐media or electronic or instant) near/1 messag*) or "instant messenger") .ti,ab,kw 48
#23 (texting or texted or texter* or ((sms or mms) near (service* or messag*)) or "interactive voice response*" or IVR or "voice call*" or callback* or "voice over internet" or VOIP):ti,ab,kw 1011
#24 (Facebook or Twitter or Whatsapp* or Skyp* or YouTube or "You Tube" or "Google Hangout*"):ti,ab,kw 226
#25 MeSH descriptor: [Mobile Applications] this term only 151
#26 "mobile app*":ti,ab,kw 441
#27 MeSH descriptor: [Social Media] this term only 67
#28 (social near (media or network*)):ti,ab,kw 967
#29 MeSH descriptor: [Reminder Systems] this term only 816
#30 (remind* near/3 (text* or system* or messag*)):ti,ab,kw 1228
#31 MeSH descriptor: [Electronic Mail] this term only 278
#32 ("electronic mail*" or email* or e‐mail or webmail):ti,ab,kw 1778
#33 MeSH descriptor: [Medical Informatics] this term only 76
#34 MeSH descriptor: [Medical Informatics Applications] this term only 28
#35 MeSH descriptor: [Nursing Informatics] this term only 10
#36 MeSH descriptor: [Public Health Informatics] this term only 6
#37 ((medical or clinical or health or healthcare or nurs*) near/3 informatics):ti,ab,kw 265
#38 MeSH descriptor: [Multimedia] this term only 192
#39 MeSH descriptor: [Hypermedia] this term only 8
#40 MeSH descriptor: [Blogging] this term only 14
#41 (multimedia or multi‐media or hypermedia or hyper‐media or blog* or vlog* or weblog* or web‐log*):ti,ab,kw 728
#42 MeSH descriptor: [Interactive Tutorial] this term only 0
#43 MeSH descriptor: [Computer‐Assisted Instruction] this term only 1132
#44 ((interactive or computer‐assisted) near/1 (tutor* or technolog* or learn* or instruct* or software or communication)):ti,ab,kw 1322
#45 {or #1‐#44} 13953
#46 MeSH descriptor: [Family Planning Services] this term only 205
#47 MeSH descriptor: [Contraception] this term only 289
#48 MeSH descriptor: [Reproductive Behavior] this term only 11
#49 MeSH descriptor: [Contraception Behavior] this term only 187
#50 MeSH descriptor: [Contraceptive Agents] explode all trees 2318
#51 MeSH descriptor: [Contraceptive Devices] explode all trees 1411
#52 (condom* or (OC near pill) or ("depot medroxyprogest*" or NET‐EN or "NET EN" or Mesigyna or Cyclofem) or ("intrauterine system" or "intra‐uterine system" or IUS or "intrauterine device*" or "intra‐uterine device*" or IUD*) or (vasectomy or sterilisation or sterilization or (tubal near ligation)) or ((vaginal near ring) or cycletel or cycle‐tel or ((abstain or abstinen*) near/2 (sex* or intercourse)) or "lactational amenorr*")):ti,ab,kw 4178
#53 (contracept* or "family planning" or (birth near (control or regulat* or spacing)) or "planned parenthood" or ((population or fertility) near (regulat* or control))):ti,ab,kw 9149
#54 MeSH descriptor: [Pregnancy in Adolescence] this term only 185
#55 (pregnan* near/2 (adolescen* or teen* or schoolchild*)):ti,ab,kw 1541
#56 MeSH descriptor: [Pregnancy, Unplanned] this term only 73
#57 MeSH descriptor: [Pregnancy, Unwanted] this term only 48
#58 (pregnan* near/3 (prevent* or interrupt* or unplanned or unwanted or mistimed)):ti,ab,kw 2178
#59 MeSH descriptor: [Sexually Transmitted Diseases] explode all trees and with qualifier(s): [Diagnosis ‐ DI, Drug therapy ‐ DT, Epidemiology ‐ EP, Prevention & control ‐ PC, Psychology ‐ PX, Transmission ‐ TM] 8731
#60 ("sexually transmi*" or STI or STIs or STD or STDs or venereal):ti,ab,kw 2535
#61 MeSH descriptor: [HIV Infections] explode all trees and with qualifier(s): [Diagnosis ‐ DI, Drug therapy ‐ DT, Epidemiology ‐ EP, Prevention & control ‐ PC, Psychology ‐ PX, Transmission ‐ TM] 7638
#62 MeSH descriptor: [HIV Seropositivity] this term only and with qualifier(s): [Drug therapy ‐ DT, Epidemiology ‐ EP, Psychology ‐ PX, Transmission ‐ TM] 380
#63 MeSH descriptor: [Anti‐HIV Agents] this term only 2641
#64 MeSH descriptor: [Antiretroviral Therapy, Highly Active] this term only 1246
#65 MeSH descriptor: [Medication Adherence] this term only 1733
#66 (#63 or #64) and #65 191
#67 (hiv or hiv‐1* or hiv‐2* or hiv1 or hiv2 or "human immunodeficiency virus" or "human immunedeficiency virus" or "human immuno‐deficiency virus" or "human immune‐deficiency virus" or ("human immun*" and "deficiency virus") or "acquired immunodeficiency syndrome" or "acquired immunedeficiency syndrome" or "acquired immuno‐deficiency syndrome" or "acquired immune‐deficiency syndrome" or ("acquired immun*" and "deficiency syndrome")):ti,ab,kw 16777
#68 ((antiretroviral* or anti‐retroviral* or ARV*) near/2 (complian* or adheren*)):ti,ab,kw 265
#69 MeSH descriptor: [Infant, Premature] this term only 3279
#70 MeSH descriptor: [Infant, Newborn] this term only 14904
#71 MeSH descriptor: [Infant, Low Birth Weight] this term only 1010
#72 MeSH descriptor: [Infant, Extremely Low Birth Weight] this term only 103
#73 MeSH descriptor: [Infant, Small for Gestational Age] this term only 254
#74 MeSH descriptor: [Infant] this term only 66
#75 MeSH descriptor: [Infant, Very Low Birth Weight] this term only 802
#76 MeSH descriptor: [Infant, Postmature] this term only 6
#77 MeSH descriptor: [Infant, Extremely Premature] this term only 100
#78 MeSH descriptor: [Child] this term only 225
#79 MeSH descriptor: [Child, Preschool] this term only 80
#80 MeSH descriptor: [Adolescent] this term only 91247
#81 {or #69‐#80} and (#63 or #64) 595
#82 ((antiretroviral* or anti‐retroviral* or ARV*) and (infant* or newborn* or neonat* or child* or schoolchild* or adolescen* or teen*)):ti,ab,kw 1265
#83 MeSH descriptor: [Papillomavirus Infections] this term only and with qualifier(s): [Prevention & control ‐ PC] 285
#84 MeSH descriptor: [Papillomavirus Vaccines] this term only and with qualifier(s): [Administration & dosage ‐ AD, Therapeutic use ‐ TU] 213
#85 MeSH descriptor: [Human Papillomavirus Recombinant Vaccine Quadrivalent, Types 6, 11, 16, 18] this term only and with qualifier(s): [Administration & dosage ‐ AD, Therapeutic use ‐ TU] 8
#86 ((hpv or "papilloma virus*" or papillomavirus*) near/2 (vaccinat* or revaccinat* or immuniz* or immunis* or immunother* or inoculat* or innoculat* or prophyla*)):ti,ab,kw 306
#87 MeSH descriptor: [Domestic Violence] this term only 159
#88 MeSH descriptor: [Spouse Abuse] this term only 211
#89 MeSH descriptor: [Intimate Partner Violence] this term only 34
#90 MeSH descriptor: [Rape] this term only 105
#91 (((sexual or domestic or spouse* or "intimate partner") near/3 (violen* or abus*)) or rape):ti,ab,kw 1425
#92 MeSH descriptor: [Puberty] this term only 292
#93 (pubert* or pubescen*):ti,ab,kw 1161
#94 MeSH descriptor: [Menstruation] this term only 467
#95 (menstruat* or menstrual*):ti,ab,kw 5420
#96 MeSH descriptor: [Abortion, Legal] this term only 29
#97 MeSH descriptor: [Abortion, Induced] this term only 936
#98 (abort* or miscarr* or (pregnan* near/2 terminat*)):ti,ab,kw 4659
#99 MeSH descriptor: [Infertility] this term only 430
#100 MeSH descriptor: [Reproductive Techniques, Assisted] this term only 222
#101 MeSH descriptor: [Fertilization in Vitro] this term only 1927
#102 (infertil* or "assisted reproductive technolog*" or "in vitro fertili*" or "in‐vitro fertili*" or IVF):ti,ab,kw 7649
#103 MeSH descriptor: [Sexual Behavior] this term only 1721
#104 MeSH descriptor: [Sex Work] this term only 90
#105 MeSH descriptor: [Safe Sex] this term only 224
#106 MeSH descriptor: [Unsafe Sex] this term only 256
#107 (sex* near (protected or unprotected or safe or unsafe or risk* or behavio*)):ti,ab,kw 7317
#108 MeSH descriptor: [Contact Tracing] this term only 102
#109 MeSH descriptor: [Disease Notification] this term only 24
#110 MeSH descriptor: [Sexual Partners] this term only 542
#111 (#108 or #109) and #110 31
#112 (partner* near/3 (notifi* or tracing or report*)):ti,ab,kw 338
#113 MeSH descriptor: [Prenatal Care] this term only 1322
#114 (((antenatal or ante‐natal or prenatal or pre‐natal or antepartum or ante‐partum) near/3 (care or service* or counsel* or test*)) or (birth near/3 prepar*)):ti,ab,kw 2581
#115 MeSH descriptor: [Maternal Health Services] this term only 232
#116 ((maternal or mother*) near/3 (health or service* or care)):ti,ab,kw 2279
#117 MeSH descriptor: [Reproductive Health] this term only 64
#118 (reproductive near/2 (health or care or service*)):ti,ab,kw 545
#119 MeSH descriptor: [Midwifery] this term only 327
#120 (midwi* or "skilled birth" or "skilled attendan*"):ti,ab,kw 1200
#121 MeSH descriptor: [Obstetric Labor Complications] this term only 472
#122 MeSH descriptor: [Pregnancy Complications] this term only 1493
#123 ((obstetric* or pregnan* or labour or labor or parturition) near/3 (emergenc* or complication*)):ti,ab,kw 5036
#124 MeSH descriptor: [Postnatal Care] this term only 391
#125 MeSH descriptor: [Perinatal Care] this term only 166
#126 MeSH descriptor: [Postpartum Period] this term only 956
#127 ((postnatal or post‐natal or perinatal or peri‐natal or postpartum or post‐partum) near/2 (care or service*)):ti,ab,kw 1204
#128 MeSH descriptor: [Maternal Nutritional Physiological Phenomena] this term only 205
#129 MeSH descriptor: [Prenatal Nutritional Physiological Phenomena] this term only 121
#130 MeSH descriptor: [Breast Feeding] this term only 1632
#131 ("breast feed*" or "breast fed" or breastfeed* or breastfed):ti,ab,kw 3952
#132 MeSH descriptor: [Early Diagnosis] this term only 581
#133 #132 and {or #69‐#77} 27
#134 (early near/1 diagnos* near/2 (infant* or neonat* or newborn*)):ti,ab,kw 48
#135 (diagnos* and (infant* or neonat* or newborn*)):ti,ab,kw 5267
#136 MeSH descriptor: [Infectious Disease Transmission, Vertical] this term only 586
#137 (("mother‐to‐child transmi*" near/3 (prevent* or eliminat*)) or emtct or pmtct or (vertical near transmi*)):ti,ab,kw 835
#138 MeSH descriptor: [Immunization] explode all trees 4855
#139 MeSH descriptor: [Immunization Programs] explode all trees 465
#140 (#138 or #139) and {or #69‐#80} 1539
#141 MeSH descriptor: [Pregnancy] this term only 58
#142 (#138 or #139) and #141 2
#143 ((immuniz* or immunis* or vaccinat*) and (infant* or newborn* or neonat* or child* or adolescen* or teen*)):ti,ab,kw 6911
#144 MeSH descriptor: [Child Health Services] this term only 387
#145 MeSH descriptor: [Maternal‐Child Health Services] explode all trees 11
#146 MeSH descriptor: [Child Nutrition Disorders] explode all trees 149
#147 MeSH descriptor: [Infant Nutrition Disorders] explode all trees 99
#148 MeSH descriptor: [Nutrition Disorders] explode all trees 13509
#149 MeSH descriptor: [Infant] explode all trees 15237
#150 MeSH descriptor: [Child, Preschool] this term only 80
#151 #148 and (#149 or #150) 352
#152 MeSH descriptor: [Delivery of Health Care, Integrated] this term only 359
#153 ((integrat* near/3 ("health care" or healthcare or management or treat* or service*) near/3 (child* or schoolchild* or infant* or neonat* or newborn or adolescen* or teen*)) or IMCI or IMNCI):ti,ab,kw 105
#154 MeSH descriptor: [Guideline Adherence] this term only 999
#155 MeSH descriptor: [Quality Assurance, Health Care] this term only 806
#156 (#154 or #155) and (#149 or #150) 52
#157 ((((guideline* or protocol*) near/3 (adher* or observ*)) or "prescribed care") and (infant* or newborn* or neonat* or child*)):ti,ab,kw 303
#158 MeSH descriptor: [Diarrhea] explode all trees and with qualifier(s): [Diagnosis ‐ DI, Drug therapy ‐ DT, Epidemiology ‐ EP, Prevention & control ‐ PC, Therapy ‐ TH] 1754
#159 #158 and {or #69‐#80} 346
#160 (diarrh* and (infant* or newborn* or neonat* or child* or schoolchild* or adolescen* or teen*)):ti,ab,kw 5413
#161 MeSH descriptor: [Hand Hygiene] this term only 41
#162 MeSH descriptor: [Hand Disinfection] this term only 339
#163 MeSH descriptor: [Water Supply] this term only 163
#164 MeSH descriptor: [Drinking Water] this term only 81
#165 MeSH descriptor: [Sanitation] this term only 62
#166 (handwash* or hand‐wash* or (wash* near/1 hand*) or "hand hygiene" or hand‐hygiene or soap or "water suppl*" or sanitation or sanitary or "drinking water" or "potable water"):ti,ab,kw 1933
#167 MeSH descriptor: [Fluid Therapy] this term only 1536
#168 #167 and {or #69‐#79} 107
#169 ("oral rehydration" near (solution* or salt* or therapy)):ti,ab,kw 587
#170 MeSH descriptor: [Child Development] this term only 1604
#171 MeSH descriptor: [Adolescent Development] this term only 78
#172 ((child* or schoolchild* or adolescen* or teen*) near/2 (develop* or progress*)):ti,ab,kw 4641
#173 MeSH descriptor: [Breast Neoplasms] this term only and with qualifier(s): [Diagnosis ‐ DI, Diagnostic imaging ‐ DG, Prevention & control ‐ PC] 1770
#174 MeSH descriptor: [Breast Neoplasms] this term only 10204
#175 MeSH descriptor: [Mass Screening] this term only 4818
#176 #173 or (#174 and #175) 1866
#177 MeSH descriptor: [Uterine Cervical Neoplasms] this term only and with qualifier(s): [Diagnosis ‐ DI, Diagnostic imaging ‐ DG, Prevention & control ‐ PC] 826
#178 (((breast or cervix or cervical) near (neoplasm* or cancer*)) and (screen* or diagnos*)):ti,ab,kw 6059
#179 MeSH descriptor: [Folic Acid] this term only and with qualifier(s): [Administration & dosage ‐ AD, Therapeutic use ‐ TU] 1046
#180 MeSH descriptor: [Folic Acid Deficiency] this term only and with qualifier(s): [Drug therapy ‐ DT, Prevention & control ‐ PC, Therapy ‐ TH] 51
#181 (folic acid near (fortif* or supplement* or treat* or therap*)):ti,ab,kw 1880
#182 MeSH descriptor: [Sex Education] this term only 242
#183 (sex* near (educat* or "health promot*")):ti,ab,kw 1551
#184 MeSH descriptor: [Pregnancy in Adolescence] this term only 185
#185 MeSH descriptor: [Kangaroo‐Mother Care Method] this term only 42
#186 (kangaroo near/2 (mother* or infant* or care)):ti,ab,kw 242
#187 MeSH descriptor: [Anemia] this term only and with qualifier(s): [Drug therapy ‐ DT, Prevention & control ‐ PC] 1051
#188 MeSH descriptor: [Anemia, Hypochromic] this term only and with qualifier(s): [Drug therapy ‐ DT, Prevention & control ‐ PC] 195
#189 MeSH descriptor: [Anemia, Iron‐Deficiency] this term only and with qualifier(s): [Drug therapy ‐ DT, Prevention & control ‐ PC] 643
#190 MeSH descriptor: [Pregnancy Complications] this term only 1493
#191 (#187 or #188 or #189) and #190 49
#192 ((maternal or mother* or pregnan*) near/2 (nutrition* or folate or folic or iron or anaemi* or anemi*)):ti,ab,kw 1369
#193 MeSH descriptor: [Malaria] this term only and with qualifier(s): [Diagnosis ‐ DI, Drug therapy ‐ DT, Prevention & control ‐ PC] 863
#194 MeSH descriptor: [Malaria, Falciparum] this term only and with qualifier(s): [Diagnosis ‐ DI, Drug therapy ‐ DT, Prevention & control ‐ PC] 1240
#195 MeSH descriptor: [Malaria, Vivax] this term only and with qualifier(s): [Diagnosis ‐ DI, Drug therapy ‐ DT, Prevention & control ‐ PC] 151
#196 MeSH descriptor: [Pregnancy] this term only 58
#197 MeSH descriptor: [Pregnancy Complications, Parasitic] this term only 167
#198 (#193 or #194 or #195) and (#196 or #197) 124
#199 ((malaria* or falciparum or vivax) near/3 (pregnan* or mother* or maternal or postpartum or "post partum")):ti,ab,kw 319
#200 MeSH descriptor: [Smoking Cessation] this term only 3848
#201 #200 and (#196 or #184) 6
#202 (((smoking or smoker* or cigarette or tobacco) near/3 (ceas* or cessation or stop* or discontinu*)) and (pregnan* or maternal or mother*)):ti,ab,kw 479
#203 MeSH descriptor: [Mental Health] this term only 1082
#204 MeSH descriptor: [Mental Disorders] this term only 2830
#205 MeSH descriptor: [Mental Health Services] this term only 727
#206 MeSH descriptor: [Community Mental Health Services] this term only 743
#207 MeSH descriptor: [Maternal Behavior] this term only 253
#208 MeSH descriptor: [Mother‐Child Relations] this term only 704
#209 MeSH descriptor: [Paternal Behavior] explode all trees 28
#210 MeSH descriptor: [Depression, Postpartum] this term only 392
#211 (((mental or behavio*) near/3 (health or disorder*)) or "postpartum depression" or "post‐partum depression" or "postnatal depression" or "post‐natal depression"):ti,ab,kw 25906
#212 {or #46‐#62, #66‐#68, #81‐#107, #111‐#131, #133‐#137, #140, #142‐#147, #151‐#153, #156‐#157, #159‐#166, #168‐#172, #176‐#186, #191‐#192, #198‐#199, #201‐#211} 115974
#213 #45 and #212 Publication Year from 2010 to 2017, in Trials 2150 hits
Appendix 2. Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) search strategy
1 Family Planning Services/ (24014)
2 Contraception/ (18551)
3 Reproductive behavior/ or Contraception behavior/ (8119)
4 exp Contraceptive agents/ (68445)
5 exp Contraceptive Devices/ (23921)
6 (condom* or (OC adj pill) or (depot medroxyprogest* or NET‐EN or NET EN or Mesigyna or Cyclofem) or (intrauterine system or intra‐uterine system or IUS or intrauterine device* or intra‐uterine device* or IUD*) or (vasectomy or sterilisation or sterilization or (tubal adj ligation)) or ((vaginal adj ring) or cycletel or cycle‐tel or ((abstain or abstinen*) adj2 (sex* or intercourse)) or lactational amenorr*)).ti,ab,kw. (55772)
7 (contracept* or family planning or (birth adj (control or regulat* or spacing)) or planned parenthood or ((population or fertility) adj (regulat* or control))).ti,ab,kw. (88295)
8 Pregnancy in Adolescence/ (7481)
9 (pregnan* adj2 (adolescen* or teen* or schoolchild*)).ti,ab,kw. (6460)
10 Pregnancy, unplanned/ or Pregnancy, unwanted/ (3826)
11 (pregnan* adj3 (prevent* or interrupt* or unplanned or unwanted or mistimed)).ti,ab,kw. (12867)
12 exp Sexually Transmitted Diseases/di, dt, ep, pc, px, tm [Diagnosis, Drug Therapy, Epidemiology, Prevention & Control, Psychology, Transmission] (203961)
13 (sexually transmi* or STI or STIs or STD or STDs or venereal).ti,ab,kw. (43434)
14 exp HIV Infections/di, dt, ep, pc, px, tm [Diagnosis, Drug Therapy, Epidemiology, Prevention & Control, Psychology, Transmission] (172773)
15 HIV Seropositivity/dt, ep, pc, px, tm [Drug Therapy, Epidemiology, Prevention & Control, Psychology, Transmission] (8281)
16 (Anti‐HIV Agents/ or Antiretroviral Therapy, Highly Active/) and Medication Adherence/ (1731)
17 (hiv or hiv‐1* or hiv‐2* or hiv1 or hiv2 or human immunodeficiency virus or human immunedeficiency virus or human immuno‐deficiency virus or human immune‐deficiency virus or (human immun* and deficiency virus) or acquired immunodeficiency syndrome or acquired immunedeficiency syndrome or acquired immuno‐deficiency syndrome or acquired immune‐deficiency syndrome or (acquired immun* and deficiency syndrome)).ti,ab,kw. (305680)
18 ((antiretroviral* or anti‐retroviral* or ARV*) adj2 (complian* or adheren*)).ti,ab,kw. (2211)
19 (Anti‐HIV Agents/ or Antiretroviral Therapy, Highly Active/) and (Infant, Premature/ or Infant, Newborn/ or Infant, Low Birth Weight/ or Infant, Extremely Low Birth Weight/ or Infant, Small for Gestational Age/ or Infant/ or Infant, Very Low Birth Weight/ or Infant, Postmature/ or Infant, Extremely Premature/ or Child/ or Child, Preschool/ or Adolescent/) (8416)
20 ((antiretroviral* or anti‐retroviral* or ARV*) and (infant* or newborn* or neonat* or child* or schoolchild* or adolescen* or teen*)).ti,ab,kw. (7849)
21 Papillomavirus Infections/pc [Prevention & Control] (4923)
22 Papillomavirus Vaccines/ad, tu [Administration & Dosage, Therapeutic Use] (3440)
23 Human Papillomavirus Recombinant Vaccine Quadrivalent, Types 6, 11, 16, 18/ad, tu [Administration & Dosage, Therapeutic Use] (66)
24 ((hpv or papilloma virus* or papillomavirus*) adj2 (vaccinat* or revaccinat* or immuniz* or immunis* or immunother* or inoculat* or innoculat* or prophyla*)).ti,ab,kw. (4560)
25 Domestic Violence/ or Spouse Abuse/ or Intimate Partner Violence/ or Rape/ (18904)
26 (((sexual or domestic or spouse* or intimate partner) adj3 (violen* or abus*)) or rape).ti,ab,kw. (29484)
27 Puberty/ (12854)
28 (pubert* or pubescen*).ti,ab,kw. (35751)
29 Menstruation/ (15653)
30 (menstruat* or menstrual*).ti,ab,kw. (46842)
31 Abortion, Legal/ (7401)
32 Abortion, Induced/ (26969)
33 (abort* or miscarr* or (pregnan* adj2 terminat*)).ti,ab,kw. (90766)
34 Infertility/ (13697)
35 Reproductive Techniques, Assisted/ (8232)
36 Fertilization in Vitro/ (29054)
37 (infertil* or assisted reproductive technolog* or in vitro fertili* or in‐vitro fertili* or IVF).ti,ab,kw. (78409)
38 Sexual behavior/ or Sex work/ or Safe sex/ or Unsafe sex/ (59074)
39 (sex* adj (protected or unprotected or safe or unsafe or risk* or behavio*)).ti,ab,kw. (30964)
40 (Contact tracing/ or Disease notification/) and Sexual partners/ (489)
41 (partner* adj3 (notifi* or tracing or report*)).ti,ab,kw. (4218)
42 Prenatal Care/ (24280)
43 (((antenatal or ante‐natal or prenatal or pre‐natal or antepartum or ante‐partum) adj3 (care or service* or counsel* or test*)) or (birth adj3 prepar*)).ti,ab,kw. (24022)
44 Maternal Health Services/ (12560)
45 ((maternal or mother*) adj3 (health or service* or care)).ti,ab,kw. (23733)
46 Reproductive Health/ (2247)
47 (reproductive adj2 (health or care or service*)).ti,ab,kw. (11738)
48 Midwifery/ (17848)
49 (midwi* or skilled birth or skilled attendan*).ti,ab,kw. (21972)
50 Obstetric Labor Complications/ (16678)
51 Pregnancy Complications/ (85905)
52 ((obstetric* or pregnan* or labour or labor or parturition) adj3 (emergenc* or complication*)).ti,ab,kw. (19704)
53 Postnatal Care/ (4878)
54 Perinatal Care/ (3796)
55 Postpartum Period/ (22535)
56 ((postnatal or post‐natal or perinatal or peri‐natal or postpartum or post‐partum) adj2 (care or service*)).ti,ab,kw. (5636)
57 Maternal Nutritional Physiological Phenomena/ (3299)
58 Prenatal Nutritional Physiological Phenomena/ (1591)
59 Breast Feeding/ (34451)
60 (breast feed* or breast fed or breastfeed* or breastfed).ti,ab,kw. (37063)
61 (Infant, Premature/ or Infant, Newborn/ or Infant, Low Birth Weight/ or Infant, Extremely Low Birth Weight/ or Infant, Small for Gestational Age/ or Infant/ or Infant, Very Low Birth Weight/ or Infant, Postmature/ or Infant, Extremely Premature/) and Early Diagnosis/ (2277)
62 (early adj1 diagnos* adj2 (infant* or neonat* or newborn*)).ti,ab,kw. (378)
63 diagnosis.fs. and (infant* or neonat* or newborn*).ti,ab,kw. (84137)
64 *"Infectious Disease Transmission, Vertical"/ (8524)
65 ((mother‐to‐child transmi* adj3 (prevent* or eliminat*)) or emtct or pmtct or (vertical adj transmi*)).ti,ab,kw. (7686)
66 (Immunization/ or Immunization, passive/ or Immunization schedule/ or Immunization, secondary/ or Immunization Programs/ or Vaccination/ or Mass vaccination/) and (Infant, Premature/ or Infant, Newborn/ or Infant, Low Birth Weight/ or Infant, Extremely Low Birth Weight/ or Infant, Small for Gestational Age/ or Infant/ or Infant, Very Low Birth Weight/ or Infant, Postmature/ or Infant, Extremely Premature/ or Child/ or Child, Preschool/ or Adolescent/ or Pregnancy/) (43902)
67 ((immuniz* or immunis* or vaccinat*) and (infant* or newborn* or neonat* or child* or adolescen* or teen*)).ti,ab,kw. (45525)
68 Child health services/ or Maternal‐child health services/ (19947)
69 exp child nutrition disorders/ or exp infant nutrition disorders/ or (exp nutrition disorders/ and (exp Infant/ or Child, Preschool/)) (39850)
70 "Delivery of Health Care, Integrated"/ (10651)
71 ((integrat* adj3 (health care or healthcare or management or treat* or service*) adj3 (child* or schoolchild* or infant* or neonat* or newborn or adolescen* or teen*)) or IMCI or IMNCI).ti,ab,kw. (935)
72 (Guideline Adherence/ or Quality Assurance, Health Care/) and (exp Infant/ or Child, Preschool/) (4112)
73 ((((guideline* or protocol*) adj3 (adher* or observ*)) or "prescribed care") and (infant* or newborn* or neonat* or child*)).ti,ab,kw. (1065)
74 (Diarrhea/di, dt, ep, pc, th, tm or Diarrhea, Infantile/di, dt, ep, pc, th, tm) and (Infant, Premature/ or Infant, Newborn/ or Infant, Low Birth Weight/ or Infant, Extremely Low Birth Weight/ or Infant, Small for Gestational Age/ or Infant/ or Infant, Very Low Birth Weight/ or Infant, Postmature/ or Infant, Extremely Premature/ or Child/ or Child, Preschool/ or Adolescent/) (10212)
75 (diarrh* and (infant* or newborn* or neonat* or child* or schoolchild* or adolescen* or teen*)).ti,ab,kw. (25541)
76 Hand Hygiene/ or Hand Disinfection/ (5743)
77 Water Supply/ (31018)
78 Drinking Water/ (5487)
79 Sanitation/ (6592)
80 (handwash* or hand‐wash* or (wash* adj1 hand*) or hand hygiene or hand‐hygiene or soap or water suppl* or sanitation or sanitary or drinking water or potable water).ti,ab,kw. (79667)
81 Fluid Therapy/ and (Infant, Premature/ or Infant, Newborn/ or Infant, Low Birth Weight/ or Infant, Extremely Low Birth Weight/ or Infant, Small for Gestational Age/ or Infant/ or Infant, Very Low Birth Weight/ or Infant, Postmature/ or Infant, Extremely Premature/ or Child/ or Child, Preschool/) (4522)
82 (oral rehydration adj (solution* or salt* or therapy)).ti,ab,kw. (2174)
83 Child Development/ or Adolescent Development/ (43982)
84 ((child* or schoolchild* or adolescen* or teen*) adj2 (develop* or progress*)).ti,ab,kw. (48454)
85 Breast Neoplasms/di, dg, pc or (Breast Neoplasms/ and Mass Screening/) (60213)
86 Uterine Cervical Neoplasms/di, dg, pc [Diagnosis, Diagnostic Imaging, Prevention & Control] (22572)
87 (((breast or cervix or cervical) adj (neoplasm* or cancer*)) and (screen* or diagnos*)).ti,ab,kw. (70920)
88 Folic Acid/ad, tu, th [Administration & Dosage, Therapeutic Use, Therapy] (8376)
89 Folic Acid Deficiency/dt, pc, th [Drug Therapy, Prevention & Control, Therapy] (806)
90 (folic acid adj (fortif* or supplement* or treat* or therap*)).ti,ab,kw. (3105)
91 Sex Education/ (8484)
92 (sex* adj (educat* or "health promot*")).ti,ab,kw. (8530)
93 Pregnancy in Adolescence/ (7481)
94 Kangaroo‐Mother Care Method/ (224)
95 (kangaroo adj2 (mother or infant or care)).ti,ab,kw. (546)
96 (Anemia/dt, pc or Anemia, Hypochromic/dt, pc or Anemia, Iron‐Deficiency/dt, pc) and Pregnancy/ (1425)
97 ((maternal or mother* or pregnan*) adj2 (nutrition* or folate or folic or iron or anaemi* or anemi*)).ti,ab,kw. (8978)
98 (Malaria/di, dt, pc or Malaria, Falciparum/di, dt, pc or Malaria, Vivax/di, dt, pc) and (Pregnancy/ or Pregnancy Complications, Parasitic/) (2012)
99 ((malaria* or falciparum or vivax) adj3 (pregnan* or mother* or maternal or postpartum or post partum)).ti,ab,kw. (2199)
100 Smoking Cessation/ and (Pregnancy/ or Pregnancy in Adolescence/) (1521)
101 (((smoking or smoker* or cigarette or tobacco) adj3 (ceas* or cessation or stop* or discontinu*)) and (pregnan* or maternal or mother*)).ti,ab,kw. (1903)
102 Mental health/ or Mental disorders/ or Mental health services/ or Community mental health services/ (207284)
103 Maternal behavior/ or Mother‐child relations/ or Parenting/ or Paternal behavior/ (39063)
104 Depression, Postpartum/ (4500)
105 (((mental or behavio*) adj3 (health or disorder*)) or postpartum depression or post‐partum depression).ti,ab,kw. (188278)
106 or/1‐105 (1926054)
107 Cell Phones/ (7081)
108 Smartphone/ (1248)
109 MP3‐Player/ (167)
110 Computers, Handheld/ (3094)
111 ((cell* or mobile*) adj1 (phone* or telephone* or technolog* or device*)).ti,ab,kw. (13097)
112 (handheld or hand‐held).ti,ab,kw. (9948)
113 (smartphone* or smart‐phone* or cellphone* or mobiles).ti,ab,kw. (5528)
114 ((personal adj1 digital) or (PDA adj3 (device* or assistant*)) or MP3 player* or MP4 player*).ti,ab,kw. (1294)
115 (samsung or nokia).ti,ab,kw. (816)
116 (windows adj3 (mobile* or phone*)).ti,ab,kw. (43)
117 android.ti,ab,kw. (1531)
118 (ipad* or i‐pad* or ipod* or i‐pod* or iphone* or i‐phone*).ti,ab,kw. (1959)
119 (tablet* adj3 (device* or computer*)).ti,ab,kw. (995)
120 Telemedicine/ (16715)
121 Videoconferencing/ or Webcasts as topic/ (1495)
122 Text Messaging/ (1659)
123 Telenursing/ (174)
124 (mhealth or m‐health or "mobile health" or ehealth or e‐health or "electronic health").ti,ab,kw. (15415)
125 (telemedicine or tele‐medicine or telehealth or tele‐health or telecare or tele‐care or telenursing or tele‐nursing or telepsychiatry or tele‐psychiatry or telemonitor* or tele‐monitor* or teleconsult* or tele‐consult* or telecounsel* or tele‐counsel* or telecoach* or tele‐coach*).ti,ab,kw. (13879)
126 (videoconferenc* or video‐conferenc* or webcast* or web‐cast*).ti,ab,kw. (2492)
127 (((text* or short or voice or multimedia or multi‐media or electronic or instant) adj1 messag*) or instant messenger).ti,ab,kw. (3426)
128 (texting or texted or texter* or ((sms or mms) adj (service* or messag*)) or interactive voice response* or IVR or voice call* or callback* or voice over internet or VOIP).ti,ab,kw. (2544)
129 (Facebook or Twitter or Whatsapp* or Skyp* or YouTube or "You Tube" or Google Hangout*).ti,ab,kw. (4064)
130 Mobile Applications/ (2240)
131 "mobile app*".ti,ab,kw. (1732)
132 Social Media/ (3805)
133 (social adj (media or network*)).ti,ab,kw. (16003)
134 Reminder Systems/ (3057)
135 (remind* adj3 (text* or system* or messag*)).ti,ab,kw. (1405)
136 Electronic Mail/ (2408)
137 (electronic mail* or email* or e‐mail or webmail).ti,ab,kw. (11435)
138 Medical informatics/ or Medical informatics applications/ (12875)
139 Nursing informatics/ or Public health informatics/ (2467)
140 ((medical or clinical or health or healthcare or nurs*) adj3 informatics).ti,ab,kw. (5003)
141 Multimedia/ (1790)
142 Hypermedia/ (399)
143 Blogging/ (815)
144 (multimedia or multi‐media or hypermedia or hyper‐media or blog* or vlog* or weblog* or web‐log*).ti,ab,kw. (6166)
145 Interactive Tutorial/ (248)
146 Computer‐Assisted Instruction/ (11266)
147 ((interactive or computer‐assisted) adj1 (tutor* or technolog* or learn* or instruct* or software or communication)).ti,ab,kw. (2214)
148 or/107‐147 (133860)
149 randomized controlled trial.pt. (470403)
150 controlled clinical trial.pt. (94471)
151 randomized.ab. (403622)
152 placebo.ab. (189095)
153 drug therapy.fs. (2022689)
154 randomly.ab. (280484)
155 trial.ab. (423499)
156 groups.ab. (1725529)
157 or/149‐156 (4123563)
158 exp animals/ not humans.sh. (4445095)
159 157 not 158 (3560201)
160 106 and 148 and 159 (4615)
161 limit 160 to yr="2010 ‐Current" (3358)
Appendix 3. Embase Classic + Embase (Ovid) search strategy
1 family planning/ (36696)
2 contraception/ (46800)
3 reproductive behavior/ (919)
4 contraceptive behavior/ (2794)
5 exp contraceptive agent/ (150341)
6 exp contraceptive device/ (40749)
7 (condom* or (OC adj pill) or (depot medroxyprogest* or NET‐EN or NET EN or Mesigyna or Cyclofem) or (intrauterine system or intra‐uterine system or IUS or intrauterine device* or intra‐uterine device* or IUD*) or (vasectomy or sterilisation or sterilization or (tubal adj ligation)) or ((vaginal adj ring) or cycletel or cycle‐tel or ((abstain or abstinen*) adj2 (sex* or intercourse)) or lactational amenorr*)).ti,ab,kw. (66547)
8 (contracept* or family planning or (birth adj (control or regulat* or spacing)) or planned parenthood or ((population or fertility) adj (regulat* or control))).ti,ab,kw. (95639)
9 adolescent pregnancy/ (8690)
10 (pregnan* adj2 (adolescen* or teen* or schoolchild*)).ti,ab,kw. (6730)
11 unplanned pregnancy/ (4299)
12 unwanted pregnancy/ (3137)
13 (pregnan* adj3 (prevent* or interrupt* or unplanned or unwanted or mistimed)).ti,ab,kw. (16419)
14 exp sexually transmitted disease/di, dt, ep, pc [Diagnosis, Drug Therapy, Epidemiology, Prevention] (36227)
15 (sexually transmi* or STI or STIs or STD or STDs or venereal).ti,ab,kw. (56299)
16 exp Human immunodeficiency virus infection/di, dt, ep, pc [Diagnosis, Drug Therapy, Epidemiology, Prevention] (161972)
17 (hiv or hiv‐1* or hiv‐2* or hiv1 or hiv2 or human immunodeficiency virus or human immunedeficiency virus or human immuno‐deficiency virus or human immune‐deficiency virus or (human immun* and deficiency virus) or acquired immunodeficiency syndrome or acquired immunedeficiency syndrome or acquired immuno‐deficiency syndrome or acquired immune‐deficiency syndrome or (acquired immun* and deficiency syndrome)).ti,ab,kw. (372022)
18 ((antiretroviral* or anti‐retroviral* or ARV*) adj2 (complian* or adheren*)).ti,ab,kw. (2598)
19 (antiretroviral therapy/ or highly active antiretroviral therapy/) and medication compliance/ (703)
20 (antiretroviral therapy/ or highly active antiretroviral therapy/) and (child/ or infant/ or adolescent/ or newborn/) (4203)
21 ((antiretroviral* or anti‐retroviral* or ARV*) and (infant* or newborn* or neonat* or child* or schoolchild* or adolescen* or teen*)).ti,ab,kw. (10214)
22 papillomavirus infection/pc [Prevention] (2243)
23 Wart virus vaccine/ad, dt [Drug Administration, Drug Therapy] (6083)
24 ((hpv or papilloma virus* or papillomavirus*) adj2 (vaccinat* or revaccinat* or immuniz* or immunis* or immunother* or inoculat* or innoculat* or prophyla*)).ti,ab,kw. (5974)
25 domestic violence/ or battered woman/ or family violence/ or exp partner violence/ (19311)
26 statutory rape/ or acquaintance rape/ or rape/ or marital rape/ (7284)
27 (((sexual or domestic or spouse* or intimate partner) adj3 (violen* or abus*)) or rape).ti,ab,kw. (36302)
28 puberty/ or menarche/ (36986)
29 (pubert* or pubescen*).ti,ab,kw. (50840)
30 menstruation/ (22869)
31 (menstruat* or menstrual*).ti,ab,kw. (62512)
32 abortion/ or imminent abortion/ or recurrent abortion/ or septic abortion/ or spontaneous abortion/ (74082)
33 (abort* or miscarr* or (pregnan* adj2 terminat*)).ti,ab,kw. (120224)
34 infertility/ (38578)
35 infertility therapy/ or in vitro fertilization/ (19053)
36 (infertil* or assisted reproductive technolog* or in vitro fertili* or in‐vitro fertili* or IVF).ti,ab,kw. (116136)
37 sexual behavior/ or adolescent sexual behavior/ or casual sex/ or prostitution/ or exp safe sex/ or sexual practice/ or exp unsafe sex/ (110380)
38 (sex* adj (protected or unprotected or safe or unsafe or risk* or behavio*)).ti,ab,kw. (33582)
39 contact examination/ (3275)
40 (partner* adj3 (notifi* or tracing or report*)).ti,ab,kw. (5304)
41 prenatal care/ or prenatal screening/ (40985)
42 (((antenatal or ante‐natal or prenatal or pre‐natal or antepartum or ante‐partum) adj3 (care or service* or counsel* or test*)) or (birth adj3 prepar*)).ti,ab,kw. (30891)
43 maternal health service/ (467)
44 ((maternal or mother*) adj3 (health or service* or care or welfare)).ti,ab,kw. (28175)
45 reproductive health/ (13171)
46 (reproductive adj2 (health or care or service*)).ti,ab,kw. (15081)
47 midwife/ or nurse midwife/ (28959)
48 (midwi* or skilled birth or skilled attendan*).ti,ab,kw. (24665)
49 labor complication/ (9228)
50 pregnancy complication/ (71410)
51 ((obstetric* or pregnan* or labour or labor or parturition) adj3 (emergenc* or complication*)).ti,ab,kw. (32301)
52 postnatal care/ or newborn care/ (16770)
53 perinatal care/ (13024)
54 maternal care/ or maternal welfare/ (27759)
55 maternal nutrition/ (10080)
56 puerperium/ (37622)
57 ((postnatal or post‐natal or perinatal or peri‐natal or postpartum or post‐partum) adj2 (care or service*)).ti,ab,kw. (7276)
58 breast feeding/ (44726)
59 (breast feed* or breast fed or breastfeed* or breastfed).ti,ab,kw. (45447)
60 early diagnosis/ and (exp infant/ or newborn/) (6264)
61 (early adj1 diagnos* adj2 (infant* or neonat* or newborn*)).ti,ab,kw. (556)
62 diagnosis.fs. and (infant* or neonat* or newborn*).ti,ab,kw. (103847)
63 vertical transmission/ (12794)
64 ((mother‐to‐child transmi* adj3 (prevent* or eliminat*)) or emtct or pmtct or (vertical adj transmi*)).ti,ab,kw. (9842)
65 (immunization/ or mass immunization/ or vaccination/) and (exp infant/ or newborn/ or exp child/ or adolescent/ or pregnancy/) (51587)
66 ((immuniz* or immunis* or vaccinat*) and (infant* or newborn* or neonat* or child* or adolescen* or teen* or pregnan*)).ti,ab,kw. (65983)
67 child health care/ or early childhood intervention/ or maternal child health care/ (37990)
68 exp nutritional disorder/ and (preschool child/ or exp infant/) (58303)
69 integrated health care system/ (9211)
70 ((integrat* adj3 (health care or healthcare or management or treat* or service*) adj3 (child* or schoolchild* or infant* or neonat* or newborn or adolescen* or teen*)) or IMCI or IMNCI).ti,ab,kw. (1093)
71 (protocol compliance/ or health care quality/) and (preschool child/ or exp infant/) (6812)
72 ((((guideline* or protocol*) adj3 (adher* or observ*)) or "prescribed care") and (infant* or newborn* or neonat* or child*)).ti,ab,kw. (1754)
73 infantile diarrhea/di, dm, dt, ep, pc, th [Diagnosis, Disease Management, Drug Therapy, Epidemiology, Prevention, Therapy] (1735)
74 diarrhea/di, dm, dt, ep, pc, th and (exp infant/ or newborn/ or exp child/ or adolescent/ or pregnancy/) (6447)
75 (diarrh* and (infant* or newborn* or neonat* or child* or schoolchild* or adolescen* or teen*)).ti,ab,kw. (33784)
76 hand washing/ or hand disinfection/ (11612)
77 water supply/ (34795)
78 drinking water/ (42849)
79 sanitation/ (13878)
80 (handwash* or hand‐wash* or (wash* adj1 hand*) or hand hygiene or hand‐hygiene or soap or water suppl* or sanitation or sanitary or drinking water or potable water).ti,ab,kw. (106006)
81 oral rehydration therapy/ (2412)
82 (oral rehydration adj (solution* or salt* or therapy)).ti,ab,kw. (2252)
83 child development/ or adolescent development/ (45720)
84 ((child* or schoolchild* or adolescen* or teen*) adj2 (develop* or progress*)).ti,ab,kw. (57900)
85 breast cancer/di, dm, dt, pc [Diagnosis, Disease Management, Drug Therapy, Prevention] (95730)
86 breast cancer/ and cancer screening/ (15585)
87 uterine cervix cancer/di, dm, dt, pc [Diagnosis, Disease Management, Drug Therapy, Prevention] (16909)
88 (((breast or cervix or cervical) adj (neoplasm* or cancer*)) and (screen* or diagnos*)).ti,ab,kw. (110687)
89 folic acid/ad, dt [Drug Administration, Drug Therapy] (11586)
90 folic acid deficiency/dm, dt, pc, th [Disease Management, Drug Therapy, Prevention, Therapy] (1174)
91 (folic acid adj (fortif* or supplement* or treat* or therap*)).ti,ab,kw. (4146)
92 sexual education/ (10956)
93 (sex* adj (educat* or "health promot*")).ti,ab,kw. (8934)
94 kangaroo care/ (720)
95 (kangaroo adj2 (mother or infant or care)).ti,ab,kw. (725)
96 (anemia/dt, pc or iron deficiency anemia/dt, pc) and pregnancy/ (1212)
97 ((maternal or mother* or pregnan*) adj2 (nutrition* or folate or folic or iron or anaemi* or anemi*)).ti,ab,kw. (10422)
98 (malaria/di, dm, dt, pc or malaria, falciparum/di, dm, dt, pc or malaria, vivax/di, dm, dt, pc) and (pregnancy/ or pregnancy complication/) (1493)
99 ((malaria* or falciparum or vivax) adj3 (pregnan* or mother* or maternal or postpartum or post partum)).ti,ab,kw. (2728)
100 smoking cessation/ and (pregnancy/ or adolescent pregnancy/) (1947)
101 (((smoking or smoker* or cigarette or tobacco) adj3 (ceas* or cessation or stop* or discontinu*)) and (pregnan* or maternal or mother*)).ti,ab,kw. (2318)
102 mental health/ or community mental health/ or mental health service/ (156252)
103 maternal behavior/ or parental behavior/ or paternal behavior/ (22837)
104 puerperal depression/ (8364)
105 (((mental or behavio*) adj3 (health or disorder*)) or postpartum depression or post‐partum depression or postnatal depression or post‐natal depression).ti,ab,kw. (246537)
106 or/1‐105 (2439735)
107 mobile phone/ or smartphone/ (16146)
108 mp3 player/ (162)
109 ((cell* or mobile*) adj1 (phone* or telephone* or technolog* or device*)).ti,ab,kw. (16688)
110 (handheld or hand‐held).ti,ab,kw. (13317)
111 (smartphone* or smart‐phone* or cellphone* or mobiles).ti,ab,kw. (7717)
112 ((personal adj1 digital) or (PDA adj3 (device* or assistant*)) or MP3 player* or MP4 player*).ti,ab,kw. (1692)
113 (samsung or nokia).ti,ab,kw. (1456)
114 (windows adj3 (mobile* or phone*)).ti,ab,kw. (67)
115 android.ti,ab,kw. (2452)
116 (ipad* or i‐pad* or ipod* or i‐pod* or iphone* or i‐phone*).ti,ab,kw. (3612)
117 (tablet* adj3 (device* or computer*)).ti,ab,kw. (1571)
118 telemedicine/ or telecardiology/ or teleconsultation/ or teledermatology/ or telediagnosis/ or telemonitoring/ or telepathology/ or telepsychiatry/ or teleradiotherapy/ or telesurgery/ or teletherapy/ (27986)
119 videoconferencing/ or webcast/ (2824)
120 text messaging/ (2877)
121 telenursing/ (203)
122 (mhealth or m‐health or "mobile health" or ehealth or e‐health or "electronic health").ti,ab,kw. (19595)
123 (telemedicine or tele‐medicine or telehealth or tele‐health or telecare or tele‐care or telenursing or tele‐nursing or telepsychiatry or tele‐psychiatry or telemonitor* or tele‐monitor* or teleconsult* or tele‐consult* or telecounsel* or tele‐counsel* or telecoach* or tele‐coach*).ti,ab,kw. (17704)
124 (videoconferenc* or video‐conferenc* or webcast* or web‐cast*).ti,ab,kw. (3335)
125 (((text* or short or voice or multimedia or multi‐media or electronic or instant) adj1 messag*) or instant messenger).ti,ab,kw. (4491)
126 (texting or texted or texter* or ((sms or mms) adj (service* or messag*)) or interactive voice response* or IVR or voice call* or callback* or voice over internet or VOIP).ti,ab,kw. (3560)
127 (Facebook or Twitter or Whatsapp* or Skyp* or YouTube or "You Tube" or Google Hangout*).ti,ab,kw. (5883)
128 mobile application/ (4502)
129 "mobile app*".ti,ab,kw. (2078)
130 social media/ (9110)
131 (social adj (media or network*)).ti,ab,kw. (20813)
132 reminder system/ (2143)
133 (remind* adj3 (text* or system* or messag*)).ti,ab,kw. (1962)
134 e‐mail/ (15606)
135 (electronic mail* or email* or e‐mail or webmail).ti,ab,kw. (23089)
136 medical informatics/ (17801)
137 nursing informatics/ (1286)
138 ((medical or clinical or health or healthcare or nurs*) adj3 informatics).ti,ab,kw. (7055)
139 multimedia/ (3205)
140 hypermedia/ (371)
141 blogging/ (141)
142 (multimedia or multi‐media or hypermedia or hyper‐media or blog* or vlog* or weblog* or web‐log*).ti,ab,kw. (9103)
143 teaching/ (85381)
144 ((interactive or computer‐assisted) adj1 (tutor* or technolog* or learn* or instruct* or software or communication)).ti,ab,kw. (3142)
145 or/107‐144 (260905)
146 106 and 145 (29013)
147 crossover procedure/ (53072)
148 double blind procedure/ (143697)
149 randomized controlled trial/ (465243)
150 single‐blind procedure/ (28784)
151 random$.tw. (1234071)
152 factorial$.tw. (31351)
153 (crossover$ or cross over$ or cross‐over$).tw. (90817)
154 placebo$.tw. (263675)
155 (doubl$ adj blind$).tw. (184763)
156 (singl$ adj blind$).tw. (19947)
157 assign$.tw. (323334)
158 allocat$.tw. (119980)
159 volunteer$.tw. (228637)
160 or/147‐159 (1925757)
161 146 and 160 (4486)
162 limit 161 to yr="2010 ‐Current" (3567)
163 limit 162 to embase (1725)
Appendix 4. POPLINE search strategy
All Fields: ((cell OR cellular OR mobile) AND (phone OR phones OR telephone OR telephones OR technology OR technologies OR device OR devices)) OR smartphone OR smartphones OR smart‐phone OR smart‐phones OR cellphone OR cellphones OR mobiles OR mhealth OR m‐health OR "mobile health" OR ehealth OR e‐health OR "electronic health" OR telemedicine OR tele‐medicine OR telehealth OR tele‐health OR telecare OR tele‐care OR telenursing OR tele‐nursing OR telepsychiatry OR tele‐psychiatry OR telemonitor OR telemonitoring OR tele‐monitor OR tele‐monitoring OR teleconsult OR teleconsulting OR tele‐consult OR tele‐consulting OR telecounsel OR telecounseling OR tele‐counsel OR tele‐counseling OR telecoach OR telecoaching OR tele‐coach OR tele‐coaching OR videoconference OR videoconferences OR videoconferencing OR video‐conference OR video‐conferences OR video‐conferencing OR webcast OR webcasts OR webcasting OR web‐cast OR web‐casts OR web‐casting OR ((text OR texts OR texting OR short OR voice OR multimedia OR multi‐media OR electronic OR instant) AND (message OR messages OR messaging)) OR "instant messenger" OR texting OR texted OR texter OR texters OR ((sms OR mms) AND (service OR services OR message OR messages OR messaging)) OR "interactive voice response" OR "interactive voice responses" OR ivr OR "voice call" OR "voice calls" OR callback OR "voice over internet" OR voip OR "mobile app" OR "mobile apps" OR "mobile application" OR "mobile applications" OR "social media" OR ((medical OR clinical OR health OR healthcare OR nurse OR nurses OR nursing) AND informatics) OR Keyword: × TEXT MESSAGING OR × MOBILE DEVICES OR × INFORMATION COMMUNICATION TECHNOLOGY OR × CELLULAR PHONE
AND
All Fields: (randomised OR randomized OR "randomly allocated" OR "random allocation" OR "controlled trial" OR "control group" OR "control groups" OR trial) OR
Keyword: × QUANTITATIVE RESEARCH OR × QUANTITATIVE EVALUATION OR
× RESEARCH METHODOLOGY OR × CLINICAL TRIALS OR × CONTROL GROUPS ‐ 1006 hits
Appendix 5. WHO Global Health Library search strategy
(tw:(((cell* OR mobile*) AND (phone* OR telephone* OR technolog* OR device*)) OR smartphone* OR smart‐phone* OR cellphone* OR mobiles OR mhealth OR m‐health OR "mobile health" OR ehealth OR e‐health OR "electronic health" OR telemedicine OR tele‐medicine OR telehealth OR tele‐health OR telecare OR tele‐care OR telenursing OR tele‐nursing OR telepsychiatry OR tele‐psychiatry OR telemonitor* OR tele‐monitor* OR teleconsult* OR tele‐consult* OR telecounsel* OR tele‐counsel* OR telecoach* OR tele‐coach* OR videoconferenc* OR video‐conferenc* OR webcast* OR web‐cast* OR ((text* OR short OR voice OR multimedia OR multi‐media OR electronic OR instant) AND messag*) OR "instant messenger" OR texting OR texted OR texter* OR ((sms OR mms) AND (service* OR messag*)) OR "interactive voice response*" OR ivr OR "voice call*" OR callback* OR "voice over internet" OR voip OR "mobile app*" OR (social AND (media OR network*)) OR ((medical OR clinical OR health OR healthcare OR nurs*) AND informatics) )) OR (mh:("Telemedicine" OR "Cell Phones" OR "Internet" OR "Mobile Applications" OR "Medical Informatics" OR "Information Technology" OR "Smartphone")) AND (mh:("Controlled Clinical Trials, Randomized" OR "Controlled Clinical Trials as Topic" OR "Controlled Clinical Trial" OR "Clinical Trial")) OR (tw:(randomised OR randomized OR "randomly allocated" OR "random allocation" OR "controlled trial" OR "control group" OR "control groups" OR trial)) – 1121 hits
Appendix 6. WHO ICTRP search strategy
Search 1:
Title: reproductive health OR maternal health OR child health OR adolescent health OR immunization OR immunisation OR pregnancy
AND
Intervention: mobile device OR mobiles OR smartphone OR phone OR cellphone
Result: 80 hits
Search 2:
Title: mobile device OR mobiles OR smartphone OR phone OR cellphone
AND
Intervention: reproductive health OR maternal health OR child health OR adolescent health
Result: 22 hits
Search 3:
Intervention: sexually transmitted OR HIV OR nutrition OR mental health OR family planning OR contraception OR abortion OR prenatal OR postnatal
AND
Title: mobile device OR mobiles OR smartphone OR phone OR cellphone
Result: 240 hits
Search 4:
Title: mobile device OR mobiles OR smartphone OR phone OR cellphone
AND
Intervention: sexually transmitted OR HIV OR nutrition OR mental health OR family planning OR contraception OR abortion OR prenatal OR postnatal
Result: 101 hits
Search 5:
Title: sexual behavior OR sexual behaviour OR sexual health OR safe sex OR unsafe sex OR sex education OR breastfeeding OR integrated delivery
AND
Intervention: mobile device OR mobiles OR smartphone OR phone OR cellphone
Result: 41 hits
Search 6:
Title: mobile device OR mobiles OR smartphone OR phone OR cellphone
AND
Intervention: sexual behavior OR sexual behaviour OR sexual health OR safe sex OR unsafe sex OR sex education OR breastfeeding OR integrated delivery
Result: 90 hits
Amalgamated Results (duplicates removed): 492 hits
Appendix 7. ClinicalTrials.gov search strategy
Search 1: ("reproductive health" OR "maternal health" OR "child health" OR "adolescent health" OR immunization OR immunisation OR pregnancy) AND ("mobile phone" OR "mobile phones" OR "mobile devices" OR mobiles OR smartphone OR smartphones) | Child, Adult | Studies received on or after 01/01/2000 | Studies updated on or before 08/31/2017 – 275 hits
Search 2: ("sexually transmitted" OR HIV OR nutrition OR "mental health" OR "family planning" OR contraception OR abortion OR prenatal OR postnatal) AND ("mobile phone" OR "mobile phones" OR "mobile devices" OR mobiles OR smartphone OR smartphones ) | Child, Adult | Studies received on or after 01/01/2000 | Studies updated on or before 08/31/2017– 481 hits
Search 3: ("sexual behavior" OR "sexual behaviour" OR "sexual health" OR "safe sex" OR "unsafe sex" OR "sex education" OR breastfeeding OR "integrated delivery") AND ("mobile phone" OR "mobile phones" OR "mobile devices" OR mobiles OR smartphone OR smartphones) | Child, Adult | Studies received on or after 01/01/2000 | Studies updated on or before 08/31/2017 – 180 hits
Data and analyses
Comparison 1. Digital targeted client communication (TCC) compared to standard care (pregnant and postpartum women).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Health behaviour change – exclusive breastfeeding in short term (up to 3 months) | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1.1 Low‐risk setting | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.79, 1.08] |
| 1.1.2 Moderate‐risk setting | 1 | 135 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.06, 1.59] |
| 1.2 Health behaviour change – receiving postpartum help with breastfeeding (3 months postpartum) | 1 | 332 | Risk Ratio (M‐H, Random, 95% CI) | 2.15 [1.79, 2.58] |
| 1.3 Health behaviour change – taking iron and folate tablets during pregnancy | 1 | 908 | Risk Ratio (M‐H, Random, 95% CI) | 1.71 [1.42, 2.07] |
| 1.4 Health behaviour change – contraceptive use (3 months postpartum) | 2 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.75, 2.46] |
| 1.5 Health behaviour change – smoked in the last 30 days | 1 | 459 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.17, 1.10] |
| 1.6 Health behaviour change – smoking cessation (objectively verified continuous abstinence) (36 weeks' gestation) | 1 | 407 | Risk Ratio (M‐H, Random, 95% CI) | 2.76 [0.89, 8.54] |
| 1.7 Health behaviour change – no alcohol consumption during pregnancy | 1 | 459 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.97, 1.03] |
| 1.8 Service utilisation – attendance at ≥ 4 antenatal care appointments | 1 | 2550 | Odds Ratio (IV, Random, 95% CI) | 1.54 [0.80, 2.96] |
| 1.9 Service utilisation – attendance for antenatal vaccination | 2 | 714 | Odds Ratio (IV, Random, 95% CI) | 1.36 [0.90, 2.06] |
| 1.9.1 Influenza vaccine | 1 | 281 | Odds Ratio (IV, Random, 95% CI) | 1.22 [0.73, 2.04] |
| 1.9.2 Tetanus vaccine | 1 | 433 | Odds Ratio (IV, Random, 95% CI) | 1.67 [0.84, 3.33] |
| 1.10 Service utilisation – attendance at antenatal preventive treatment for malaria | 1 | 2550 | Odds Ratio (IV, Random, 95% CI) | 1.69 [0.82, 3.48] |
| 1.11 Service utilisation – skilled attendant at birth | 2 | Odds Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.12 Service utilisation – newborn postpartum care | 2 | 191 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.69, 1.87] |
| 1.12.1 Low‐risk setting | 1 | 56 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.87, 1.11] |
| 1.12.2 High‐risk setting | 1 | 135 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [1.02, 1.78] |
| 1.13 Service utilisation – attendance for postpartum care appointment (mother) (10 days postpartum) | 1 | 56 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.30, 7.52] |
| 1.14 Service utilisation – attendance for newborn vaccination | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.14.1 Pentavalent and polio vaccine at up to 9 weeks | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.89, 1.32] |
| 1.15 Health status and well‐being – maternal mortality and morbidity | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.15.1 Maternal mortality up to 6 weeks postpartum | 1 | 2637 | Risk Ratio (IV, Random, 95% CI) | 2.86 [0.30, 27.40] |
| 1.15.2 Maternal morbidity – severe obstetric complications up to 6 weeks postpartum | 1 | 2550 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.70, 1.07] |
| 1.15.3 Maternal morbidity – any maternal health problem up to 10 days postpartum | 1 | 56 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.09, 2.76] |
| 1.15.4 Maternal morbidity – mastitis: breast pain up to 3 months postpartum | 1 | 332 | Risk Ratio (IV, Random, 95% CI) | 0.28 [0.09, 0.80] |
| 1.15.5 Maternal morbidity – mastitis: breast engorgement up to 3 months postpartum | 1 | 332 | Risk Ratio (IV, Random, 95% CI) | 0.58 [0.31, 1.10] |
| 1.16 Health status and well‐being – maternal mortality and morbidity | 1 | 135 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.19, 0.31] |
| 1.16.1 Acute episodes requiring clinic visit up to 3 months postpartum | 1 | 135 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.19, 0.31] |
| 1.17 Health status and well‐being – neonatal mortality and morbidity | 3 | 2870 | Odds Ratio (IV, Random, 95% CI) | 1.00 [0.61, 1.64] |
| 1.17.1 Neonatal mortality up to 6 weeks after delivery | 1 | 2482 | Odds Ratio (IV, Random, 95% CI) | 0.85 [0.37, 1.95] |
| 1.17.2 Neonatal diarrhoea up to 3 months postpartum | 1 | 332 | Odds Ratio (IV, Random, 95% CI) | 1.05 [0.53, 2.11] |
| 1.17.3 Any newborn health problem reported up to 10 days postpartum | 1 | 56 | Odds Ratio (IV, Random, 95% CI) | 1.27 [0.36, 4.51] |
| 1.18 Health status and well‐being – neonatal mortality and morbidity | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.18.1 Acute episodes requiring clinic visit up to 3 months postpartum | 1 | 135 | Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.92, ‐0.14] |
| 1.19 Health status and well‐being – neonatal health | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.19.1 Gestational age at birth (weeks) | 1 | 61 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.45, 0.65] |
| 1.19.2 Birth weight (g) | 1 | 61 | Mean Difference (IV, Random, 95% CI) | ‐173.00 [‐448.87, 102.87] |
| 1.19.3 Infant weight (kg) at 3 months | 1 | 332 | Mean Difference (IV, Random, 95% CI) | Not estimable |
| 1.19.4 Infant length (cm) at 3 months | 1 | 332 | Mean Difference (IV, Random, 95% CI) | Not estimable |
| 1.20 Health status and well‐being – preterm birth | 2 | 2557 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.31, 2.33] |
| 1.21 Sensitivity analysis (cluster‐RCTs: health status and well‐being – preterm birth | 1 | Risk Ratio (IV, Random, 95% CI) | 0.18 [0.01, 3.64] |
Comparison 2. Digital targeted client communication (TCC) compared to non‐digital targeted client communication (pregnant and postpartum women).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Health behaviour change – exclusive breastfeeding (9 weeks postpartum) | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.79, 1.07] |
| 2.2 Health behaviour change – contraceptive use (9 weeks postpartum) | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [0.78, 2.69] |
| 2.3 Service utilisation – newborn postpartum care (10 days after delivery) | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.09] |
| 2.4 Service utilisation – attendance for newborn vaccination | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.4.1 Pentavalent and polio vaccine at 9 weeks | 1 | 42 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.88, 1.16] |
| 2.5 Service utilisation – attendance for postpartum care appointment (mother) (10 days postpartum) | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.18, 1.79] |
| 2.6 Health status and well‐being – maternal mortality and morbidity | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.6.1 Any maternal health problem reported up to 10 days postpartum | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.04, 0.79] |
| 2.7 Health status and well‐being – neonatal mortality and morbidity | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.7.1 Any newborn health problem reported up to 10 days postpartum | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.25, 1.06] |
Comparison 3. Digital targeted client communication (TCC) compared to digital non‐targeted client communication (pregnant and postpartum women).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Service utilisation – attendance for antenatal influenza vaccination | 1 | 204 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.71, 1.58] |
| 3.2 Service utilisation – birth at health facility | 1 | 16 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.69, 1.45] |
Comparison 4. Digital targeted client communication (TCC) compared to standard care (pregnant women with HIV).
Comparison 5. Digital targeted client communication (TCC) compared to digital non‐targeted client communication (pregnant women with HIV).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Health behaviour – infant antiretroviral/prevention of mother‐to‐child transmission adherence (6 weeks after delivery) | 1 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.07, 1.48] |
| 5.2 Service utilisation – postnatal care: attendance at postpartum care appointment (10 weeks postpartum) | 1 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 1.86 [1.34, 2.58] |
Comparison 6. Digital targeted client communication (TCC) compared to standard care (parents of children aged under five years).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Attendance for necessary healthcare | 10 | 5660 | Risk Ratio (IV, Random, 95% CI) | 1.21 [1.08, 1.34] |
| 6.1.1 Vaccinations at up to 6 months | 5 | 1586 | Risk Ratio (IV, Random, 95% CI) | 1.14 [1.01, 1.28] |
| 6.1.2 Vaccinations at 12 months | 4 | 3832 | Risk Ratio (IV, Random, 95% CI) | 1.24 [1.02, 1.52] |
| 6.1.3 HIV medical appointment 2 days after reminder | 1 | 242 | Risk Ratio (IV, Random, 95% CI) | 1.63 [1.26, 2.11] |
| 6.2 Timeliness of vaccination | 4 | 2400 | Risk Ratio (IV, Random, 95% CI) | 1.18 [1.04, 1.34] |
| 6.3 Service utilisation – no emergency department attendance (6 months) | 1 | 129 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.03, 1.70] |
Comparison 7. Digital targeted client communication (TCC) compared to non‐digital targeted client communication (parents of children aged under five years).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Health behaviour change – oral health in children (Visible Plaque Index, [0–100%], low = good) | 1 | 143 | Mean Difference (IV, Random, 95% CI) | ‐2.10 [‐7.54, 3.34] |
| 7.2 Service utilisation – attendance for vaccinations at 14 weeks | 1 | 744 | Risk Ratio (IV, Random, 95% CI) | 1.13 [1.00, 1.28] |
Comparison 8. Digital targeted client communication (TCC) compared to digital non‐targeted client communication (parents of children aged under five years).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Service utilisation – attendance for vaccinations at 7 months | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.33, 1.20] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahlers‐Schmidt 2012.
| Study characteristics | ||
| Methods |
Aim: to evaluate feasibility, stability of mobile service, and effect size. Study design: parallel individual RCT Recruitment: parents of newborns being discharged from a local hospital who intended to seek child health care at the university resident and faculty clinic. Parents enrolled in the study by texting "TRICKs" to the research phone number. Study duration: up to 1 year Study dates: January 2011 to February 2011 |
|
| Participants |
Inclusion criteria: English‐ and Spanish‐speaking parents of newborns were eligible if they owned a mobile phone with text messaging capability. Sample size (n): 90 (intervention: 50; standard care: 40) Age (mean): intervention: 26 (SD 5) years; control: 26 (SD 6) years Sex (female): intervention: 84%; control: 83% County: USA (high‐income) Setting: local hospital, university resident and faculty clinic in a Midwestern metropolitan area |
|
| Interventions |
Intervention: reminder text messages 7 days before their child's immunisations which were due at 2, 4, and 6 months of age. Content: reminder and request to respond to query whether their child was immunised. Frequency and intensity: 7 days before immunisations at 2, 4, and 6 months, assumed to be single text messages. Control: standard care/no intervention: parents in the control arm received standard notification (an appointment card) of immunisations due only. Co‐interventions: none reported |
|
| Outcomes | 1. Attendance for vaccinations; 2. Timely attendance for vaccinations; 3. Satisfaction with the service (time point not reported) Outcome assessment time point: 2, 4, 6 months – we included the longest time point (6 months). |
|
| Funding/declarations of interest |
Funding: funded by a Wichita Center for Graduate Medical Education and Kansas Bioscience Authority Level III grant. Conflicts of interest: none |
|
| Notes | Trial ID: NCT01396902 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation scheme. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants or personnel. |
| Blinding of objective outcome assessment (detection bias) | Low risk | Vaccination results were abstracted from immunisation registry records and were considered low risk of detection bias. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐reported measures were at high risk of detection bias since the study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 participants excluded from analysis, reason provided. |
| Selective reporting (reporting bias) | Unclear risk | All relevant outcomes appear to be reported but there was no protocol or online trial registration. |
| Other bias | Unclear risk | Intervention and control arm participants differ significantly on income, with 28% (11/40) of control parents having an income level ≥ USD 25,000 annually compared with 12% (6/50) of intervention parents. |
Bangure 2015.
| Study characteristics | ||
| Methods |
Aim: to assess whether immunisation coverage among those receiving short message reminders and routine immunisation health education differ from those receiving routine immunisation health educations only. Study design: parallel individual RCT Recruitment: mother or carer soon after delivery or at third or seventh day visit after delivery Study duration: 14 weeks Study dates: 1 January 2013 to 31 August 2013 |
|
| Participants |
Inclusion criteria: mother or carer soon after delivery or at third or seventh day visit after delivery, must have mobile phone and be a resident of Kadoma City. Sample size (n): 304 (intervention: 152; control: 152) Age (median): intervention: 26 (Q1 21, Q3 30); control: 27 (Q1 23, Q3 32) Sex: not reported Country: Zimbabwe (low‐income) Setting: city clinics and general hospital |
|
| Interventions |
Intervention: 3 automatic text message reminders. First message sent 7 days before due date for immunisation, second message sent 3 days before, last message sent 1 day before immunisation appointment. Content: appointment reminder Frequency and intensity: 3 text message reminders before the 6‐, 10‐, and 14‐week appointments Control: standard care/no intervention: informed about next scheduled visit Co‐interventions: all participants received routine health education. |
|
| Outcomes | 1. Attendance for vaccinations (6, 10, 14 weeks – we included the longest time point, 14 weeks); 3. opinion of SMS; 4. Cost of SMS service Outcomes reported but not included in the review: 2. Age of child when immunised (outcome not eligible for inclusion) Outcome assessment time point: 6, 10, 14 weeks |
|
| Funding/declarations of interest |
Funding: Center for Disease Control and Prevention, Zimbabwe Conflicts of interest: none declared |
|
| Notes | Trial ID: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study participants assigned by computer‐generated random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants or personnel. |
| Blinding of objective outcome assessment (detection bias) | Unclear risk | Not reported. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐reported measures were at high risk of detection bias since the study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 0 lost. |
| Selective reporting (reporting bias) | Low risk | Only outcome reported in registration is immunisation coverage at 6, 10, and 14 weeks. |
| Other bias | Low risk | No apparent baseline differences. |
Bigna 2015.
| Study characteristics | ||
| Methods |
Aim: to determine 1. if reminders sent by text message, phone call, or concomitant text and phone calls most increase the presence at medical appointments of HIV‐infected or HIV‐exposed children, and 2. which is the most efficient related to working time and financial cost. Study design: parallel individual RCT Recruitment: adult–child (carer–patient) pairs were recruited for HIV‐infected or exposed children aged < 15 years attending HIV care. Study duration: not reported Study dates: January 2013 to May 2013 |
|
| Participants |
Inclusion criteria: people aged ≥ 18 years accompanying an HIV‐infected or HIV‐exposed child aged < 15 years for HIV care Sample size (n): 242 (text message: 60; text message + call: 61; call: 60; control: 61) Age: children: age range up to 15 years, although we could not confirm that ≥ 70% of included children were ≤ 5 years we decided to include this study since the weighted mean age of children was 2.8 years. Carers (mean): text message + call group: 36.5 (SD 12.4) years; text message group: 41.4 (SD 12.8) years; call group: 50.5 (SD 13.2) years; control group: 42.6 (SD 12.6) Sex: carers – men: text message + call group: 20%; text message group: 13%; call group: 15%; control group: 13%; children – boys: text message + call group: 52%; text message group: 47%; call group: 47%; control group: 49% Country: Cameroon (lower middle‐income) Setting: 3 hospitals serving urban (Essos), semi‐urban (Kousséri), and rural (Goulfey) settings |
|
| Interventions |
Intervention: appointment reminders via text message; voice call; or text message + voice call Content: appointment reminder Frequency and intensity: 1 call, or 1 text message then 1 call 2–3 days before appointment Control: standard care/no intervention. No reminder (usual practice), all participants attended standard HIV care appointments Co‐interventions: HIV care (to all participants) |
|
| Outcomes | 1. Attendance at HIV medical appointments; 2. Direct costs; 3. Staff working time Outcome assessment time point: 2 days |
|
| Funding/declarations of interest |
Funding: no external funding, done as part of an academic degree financed from the personal funds of the corresponding author Jean Joel R Bigna. Conflicts of interest: authors declare no competing interests |
|
| Notes | Trial ID: PACTR201304000528276 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence. Quote: "Randomisation and allocation were done centrally with WinPepi version 11.25. Eligible participants (adult–child pairs) were randomly assigned in blocks of four and allocated (1:1:1:1) sequentially in the order of receipt of a randomisation code." |
| Allocation concealment (selection bias) | Low risk | Central allocation. Quote: "Randomisation and allocation were done centrally with WinPepi version 11.25. Eligible participants (adult–child pairs) were randomly assigned in blocks of four and allocated (1:1:1:1) sequentially in the order of receipt of a randomisation code." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel were blinded. Not possible to blind participants. Quote: "The treating physician, the medical administrative assistant responsible for contacting participants in the intervention groups 2, 3, and 4 via mobile phone … were all masked to group assignments." |
| Blinding of objective outcome assessment (detection bias) | Low risk | Outcome assessors and analysts were blinded. Quote: "the nurse (outcome assessor) responsible for recording the patient's presence or absence at the appointment, and the data analysts were all masked to group assignments." |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐reported measures would have been at high risk of detection bias since the study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants, whether or not they received the intervention, were included in the ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in the protocol were fully reported. |
| Other bias | Unclear risk | Some baseline characteristics (ages of children and carers, carers' education, and time to appointment) were unevenly distributed between groups. |
Brown 2016.
| Study characteristics | ||
| Methods |
Aim: to assess the effect of reminder/recall system and primary healthcare immunisation providers' training intervention on routine immunisation. Study design: cluster RCT Recruitment: children aged 0–12 weeks at their first immunisation appointment Study duration: until child was 12 months old Study dates: August 2012 to September 2013 |
|
| Participants |
Inclusion criteria: children aged 0–12 weeks at their first immunisation visits, parents living in study communities Sample size: 595 (reminder: 153 participants, 1 cluster; usual care: 152 participants, 1 cluster; reminder + HCP training: 149 participants, 1 cluster – not eligible or included in review; HCP training: 141 participants, 1 cluster – not eligible or included in review) Age: children: 0–12 months; parents: not reported Sex (female): children: 51.4% Country: Nigeria (lower middle‐income) Setting: community/health facility |
|
| Interventions |
Intervention: mobile phone calls for the reminder/recall interventions sessions, reminder of immunisation appointment, recall for missed appointment Content: appointment reminder and recall for missed appointments Frequency and intensity: 2 telephone reminders to the contact person whose mobile phone number was provided by the mother – 2 days before and 1 day before the appointment. Control: standard care/no intervention: usual care Co‐interventions: 2‐day refresher training conducted for primary healthcare immunisation providers |
|
| Outcomes | 1. "immunization completed" = receipt of all scheduled routine childhood immunisation = 1 dose of BCG vaccine, at ≥ 4 doses of OPV, 3 doses of DPT vaccine, 3 doses of hepatitis B vaccines, and 1 dose each of measles and yellow fever vaccine by age of 12 months Outcome assessment time point: 12 months |
|
| Funding/declarations of interest |
Funding: not reported Conflicts of interest: not reported |
|
| Notes | 2 arms that included primary healthcare training were not extracted. Trial ID: not reported Cluster features: 4 local government authorities were randomised. Mean cluster size: 152.5 (for the 2 study arms included in the review). The study did not adjust for clustering effect; we used ICC 0.0487 (derived from k = 0.089 reported in Gibson 2017) to adjust for cluster effect in the analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Using ballot system, the four randomly selected LGAs [local government association] were then allocated into three intervention groups and one control group." Comment: no further details reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Selective cluster recruitment | Unclear risk | Quote: "A total of 605 eligible children aged 0–12 weeks at their first immunization visits having their parents living in the study communities were consecutively recruited into four different study groups from August to November 2012." Comment: unclear whether participants were recruited before or after clusters were randomised. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants or personnel since interventions were active and different. |
| Blinding of objective outcome assessment (detection bias) | Unclear risk | Outcome data collected using a standard instrument to extract data from comprehensive immunisation records, but unclear blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analyses were not ITT but there were few dropouts, due to either relocation or death. |
| Selective reporting (reporting bias) | Unclear risk | Reports the outcome described in methods, but no protocol or online trial record. |
| Other bias | High risk | Significant religious and social differences between clusters at baseline. |
Domek 2016.
| Study characteristics | ||
| Methods |
Aim: 1. to test the feasibility and acceptance of SMS vaccination reminders sent to parents of children presenting for their infant primary immunisation series, and 2. to evaluate the potential of a larger‐scale programme to optimise immunisation delivery in a LMIC. Study design: parallel individual RCT Recruitment: parents of infants aged 8–14 weeks recruited when presenting for the first dose of the 3‐dose infant primary immunisation series Study duration: 6 months Study dates: March 2013 to October 2013 (6 months after last enrolment April 2013) |
|
| Participants |
Inclusion criteria: parents of infants aged 8–14 weeks, presenting for the first dose of the 3‐dose infant primary immunisation series, owned a mobile phone with SMS text messaging capability, ≥ 1 parent had to be literate and able to use SMS technology. Sample size (n): 321 (intervention: 160; control: 161) Age (mean): parents: not reported; infants: intervention: 9.7 (SD 9.1) months; control: 9.4 (SD 9.0 months) Sex (male): intervention: 52.5%; control: 44.4% Country: Guatemala (lower middle‐income) Setting: community, served by 2 public health clinics in Guatemala City |
|
| Interventions |
Intervention: SMS reminders for infant immunisation Content: appointment reminders Frequency and intensity: SMS text messages at 6, 4, and 2 days before scheduled vaccination visits 2 and 3 (at 4 and 6 months of age) Control: standard care/no intervention Co‐interventions: all participants received written reminders in the child's immunisation card for the next dose of vaccines at the time of each vaccination based on the usual standard of care at both clinics. |
|
| Outcomes | 1. Attendance for vaccinations: completing all vaccinations (6 months); 2. Client satisfaction Outcomes reported but not included in review: 1. Completing any vaccination (6 months) – instead, we included completion of all vaccinations (see above); 2. Attendance for vaccinations at second (4 months) and third visit (6 months) – instead, we included completion of all vaccinations (see above); 3. Completing pentavalent (3 doses)/pneumococcal (2 doses)/poliomyelitis (3 doses)/rotavirus (2 doses) vaccination; 4. Age at visits 2 and 3 (outcome not eligible for inclusion); 5. Proportion of parents sent SMS messages (outcome not eligible for inclusion) Outcome assessment time point: 4, 6 months |
|
| Funding/declarations of interest |
Funding: Bill & Melinda Gates Foundation Grand Challenges Explorations grant and a small operational grant from the Pan American Health Organization Conflicts of interest: none declared |
|
| Notes | Trial ID: NCT01663636 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were allocated to either an intervention or usual care group using a computer‐generated randomization scheme." |
| Allocation concealment (selection bias) | Low risk | Quote: "Participants were allocated to either an intervention or usual care group … with the investigators being blind to the allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants. Personnel blind to allocation, but unclear whether this blinding was sustained. |
| Blinding of objective outcome assessment (detection bias) | Unclear risk | Not reported whether research nurses that collected data were blinded. Immunisation records were able to be confirmed only for children who returned to either of the 2 study sites. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐reported measures were at high risk of detection bias since the study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 17.4% were lost to follow‐up but analyses were ITT. |
| Selective reporting (reporting bias) | Low risk | Outcomes listed in online trial record were reported. |
| Other bias | Unclear risk | Parents in the usual care group had significantly higher income with more fathers working; otherwise, there were no significant differences between the baseline demographics of intervention and usual care children and their parents. |
Evans 2014.
| Study characteristics | ||
| Methods |
Aim: to evaluate initial outcomes of the Text4baby intervention at 4 weeks postbaseline. Study design: parallel individual RCT Recruitment: women recruited at the end of their initial ANC visit to the Madigan Obstetrics and Gynecology clinic. Study duration: 4 weeks (intervention planned to continue for whole pregnancy) Study dates: December 2011 (recruitment) to January 2013 (recruitment) |
|
| Participants |
Inclusion criteria: women military healthcare beneficiaries (both active duty and family members), aged 18–45 years, presented for ANC prior to 14 weeks' gestation, working mobile phone, speaking, and reading fluent English Sample size (n): 943 (completers (number randomised per arm not reported): intervention: 229; control: 230) Age (mean): 26.53 years Sex: 100% women Country: USA (high‐income) Setting: community (military) served by a large tertiary‐care army medical centre |
|
| Interventions |
Intervention: SMS messages Content: 135 distinct antenatal text messages aimed at promoting ways to live a satisfying lifestyle while reducing risk and promoting maternal and child health Frequency and intensity: 3 messages per week for 4 weeks in this report (intervention intended for whole pregnancy) Control: standard care/no intervention. No SMS messages Co‐interventions: not reported |
|
| Outcomes | 1. Self‐reported consumption of alcohol since becoming aware of pregnancy; 2. Smoking in last 30 days (self‐report) Outcomes reported but not included in the review: 1. Attitudes and knowledge on pregnancy risks, self‐report (outcome not eligible for inclusion) Outcome assessment time point: 4 weeks |
|
| Funding/declarations of interest |
Funding: Telemedicine and Advanced Technology Research Center (TATRC), US Army Medical and Materiel Command Conflicts of interest: none declared |
|
| Notes | Trial ID: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using an algorithm that generated a randomized list of individual assignments to treatment or control condition …" |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants. Clinicians who met with participants were blinded – the randomisation occurred outside the actual clinical visit and the trial data were not accessed by the clinicians during the study. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Subjective outcomes self‐reported by unblinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High level of attrition – 459/943 (48.7%) completed a 4‐week follow‐up survey. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported, as per methods in the protocol/early results paper. |
| Other bias | Unclear risk | Control group reported a larger, statistically significant percent smoking in the last 30 days and consuming ≥ 3 vegetables per day at baseline compared with the intervention group. |
Eze 2015.
| Study characteristics | ||
| Methods |
Aim: 1. To provide evidence validating the need for development and deployment of automated client reminder‐recall systems for the Nigerian National Routine Immunisation Program and 2. to compare its projected cost with the cost of a health personnel‐based defaulter tracking system. Study design: parallel individual RCT Recruitment: carers were selected using multistage sampling method from 8 health facilities in Egor local government area of Edo State. Study duration: each child recruited into the study at its first immunisation session (BCG) was followed up for 18 weeks while those who were recruited at their second session (DPT1) were followed up for 12 weeks to allow for 4 extra weeks after the recommended dates of receipt of DPT3. Study dates: June 2010 to June 2011 |
|
| Participants |
Inclusion criteria: bringing child for routine immunisation for the first or second schedules Sample size (n): 1001 (intervention: 500; control: 501) Age (mean): carers: 29.35 (SD 5.3) years Sex: 895 (89%) mothers, and 10 classed as 'other' but sex not stated Country: Nigeria (lower middle‐income) Setting: facilities included 1 tertiary hospital, 2 primary health centres, and 5 privately owned health facilities all of which provided routine immunisation services. |
|
| Interventions |
Intervention: reminder and recall text messages Authors also report that (quote), "All text messages were by internet‐based web‐to‐SMS (Bulk SMS) service and were tagged the name of client's health facility for easy recognition." Messages sent the day before an immunisation appointment. There were 4 immunisation time points for BCG, DPT1, DPT2, and DPT3. Content: short reminder text message, and recall messages to those who missed appointments Frequency and intensity: reminder messages sent 1 day before the appointment, the number of reminder messages received depended the time point at which the participant was recruited. Recall messages were sent to defaulters. The total number of these messages was not reported. Control: standard care/no intervention, details not reported Co‐interventions: none reported |
|
| Outcomes | 1. Timeliness of receipt of DPT3; 2. Cost and cost‐effectiveness (compared to estimated cost of home visits) Outcomes reported but not included in the review: 1. Barriers to receiving text message reminders (outcome not eligible for inclusion) Outcome assessment time point: postintervention, exact follow‐up time not reported |
|
| Funding/declarations of interest |
Funding: not reported Conflicts of interest: not reported |
|
| Notes | Trial ID: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants recruited per facility were randomized into 2 equal groups: intervention and Control groups using the RANDOM. EXE function of the Programme for Epidemiologists (PEPI) version 4.0." |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants or personnel. |
| Blinding of objective outcome assessment (detection bias) | Low risk | Quote: "Data collectors could not tell if a client was in the intervention or control group." |
| Blinding of subjective outcome assessment (detection bias) | High risk | Unblinded carers interviewed using follow‐up questionnaires. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Available‐case analysis with 9.6% (96 carers) attrition. Reasons for dropping out were provided and dropouts were balanced between groups. |
| Selective reporting (reporting bias) | Unclear risk | All expected outcomes and outcomes listed in the methods section were reported in the results, but no protocol or online trial record was identified to check against. |
| Other bias | High risk | Some participants switched groups after randomisation. Authors stated that, "Some respondents, who did not have mobile phones but were randomized into the Interventional group initially, were eventually matched for age and sex and swapped with persons who own mobile phones and were randomized into the Control group." Comment: in addition, carers provided answers to questions by recall; this could have led to recall bias in the information supplied. |
Gibson 2017.
| Study characteristics | ||
| Methods |
Aim: to assess whether SMS reminders, with or without mobile money incentives, improve the proportion of children fully immunised by their first birthday. Study design: cluster RCT Recruitment: the Health and Demographic Surveillance System village reporters identified eligible carers and their infants. Village reporters used mobile phones to send birth notification text messages. Birth notifications were relayed to field‐based community interviewers who then screened carers of newborns for eligibility into the study. Study duration: 12 months Study dates: October 2013 (start date of recruitment) to October 2014 (end date of recruitment) |
|
| Participants |
Inclusion criteria: mothers/carers of infants aged 0–34 days during the study period, current resident of 1 of the participating study villages, willing to sign informed consent for the study Sample size: 2018 (intervention: 476 participants, 38 clusters; control: 489 participants, 38 clusters)* Age: mothers aged ≤ 25 years: 52% (n = 825); aged > 25 years 48% (n = 769); infants: mean 14 (SD 8) days Sex: 100% female (mothers) Country: Kenya (lower middle‐income) Setting: community‐based (villages) |
|
| Interventions |
Intervention: SMS reminders composed of a core text and a motivational saying Frequency and intensity: 3 days and the day before scheduled immunisation visits at ages 6 weeks, 10 weeks, and 14 weeks for the 3 doses of pentavalent vaccine and age 9 months for measles vaccine Control: standard care/no intervention, did not receive SMS reminders or incentives Co‐interventions: all carers received a single text message at enrolment welcoming them to the study |
|
| Outcomes | 1. Fully immunised child by 12 months of age, defined as receiving BCG, 3 doses of OPV, 3 doses of pentavalent vaccine, and measles vaccine; 2. Timely fully immunised child defined as being fully immunised within 2 weeks of the measles EPI due date; 3. Carer's opinion on number of SMS reminders per vaccine and about the influence of SMS reminder on decision to vaccinate the child Outcomes reported but not included in the review: 1. Timely vaccinations for individual vaccines defined as receiving pentavalent 1, 2, and 3 vaccine; OPV; or measles vaccines within 2 weeks (we included overall measure instead of individual measures per vaccine); 2. Receiving all timely vaccines (children who received pentavalent 1, 2, and 3, and measles vaccines within 2 weeks of their respective EPI due date) (we included fully immunised child by measles due date instead (see above)) Outcome assessment time point: 12 months (1 time point for all outcomes) |
|
| Funding/declarations of interest |
Funding: Bill & Melinda Gates Foundation Conflicts of interest: none declared |
|
| Notes | *SMS plus incentives (KES 75 or KES 200) groups were not considered relevant for this systematic review and were not extracted. Trial ID: NCT01878435 Cluster features: 152 villages were randomised. The study adjusted outcomes for cluster effect using coefficient of variation (k) = 0.089 in the control group; k = 0.069 in the SMS only group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. Quote: "A constrained randomisation was done with GAUSS Mathematical and Statistical System by one of the study investigators, which randomly generated 1000 allocations." |
| Allocation concealment (selection bias) | Low risk | The 1000 sequences were labelled with 3‐digit numbers, 000 to 999, each 1 assigning 38 villages to each of the 4 groupings (A–D). At a public randomisation ceremony on 12 September 2013, village chiefs determined the final randomisation outcome by picking numbered balls from a cloth sack to select 1 of these 1000 sequences, then picking labelled (study group) balls to assign the interventions to the chosen allocation. |
| Selective cluster recruitment | High risk | Enrolment of participants took place after cluster allocation had been made. Quote: "Birth notifications were relayed to field‐based community interviewers who then screened caregivers of newborns for eligibility into the study." Quote: "Participants provided written informed consent and were enrolled into the study by community interviewers after villages were randomly assigned." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to nature of intervention and study design, study participants were not blinded to their study group allocation. Field staff were not informed of a village's allocation, but this could be inferred from some enrolment and follow‐up survey questions. |
| Blinding of objective outcome assessment (detection bias) | Low risk | Data cleaning was performed by a statistician blinded to the allocation. |
| Blinding of subjective outcome assessment (detection bias) | Unclear risk | Field staff were not informed of a village's allocation, but this could be inferred from some enrolment and follow‐up survey questions. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 14% in the SMS only arm and 19% in the control arm were lost to follow‐up (out‐migration and death), 4.4% in the SMS only arm and 7.4% in the control arm reported immunisation verbally (no vaccination booklet) and were excluded. Primary analyses were performed with modified ITT analyses at the participant level so that participants' outcomes were analysed regardless of the degree of exposure to study interventions. The term modified refers to the requirement of being able to determine the 12‐month immunisation outcomes. |
| Selective reporting (reporting bias) | Low risk | Table and figures reporting all outcomes stated in the paper and online trial registration (NCT0187843). |
| Other bias | Low risk | Sociodemographic characteristics of the analytic sample were similar across the 4 groups. |
Haji 2016.
| Study characteristics | ||
| Methods |
Aim: to assess the impact of SMS and sticker reminders to reduce dropout rates for routine childhood vaccinations, and determined factors associated with missed vaccination in selected districts in Kenya. Study design: cluster RCT Recruitment: children aged < 12 months who were brought to the selected vaccinating health facilities in the 3 districts for their first dose of pentavalent vaccine were recruited on a first‐come basis until the strategy‐level target sample sizes was reached. Study duration: 8 weeks Study dates: February 2014 to December 2014 (enrolment ceased October 2014) |
|
| Participants |
Inclusion criteria: children aged < 12 months attending for first dose of pentavalent vaccine Sample size: 1116 (SMS: 372 participants, 3 clusters; targeted non‐digital communication (stickers): 372 participants, 3 clusters; usual care: 372 participants, 3 clusters) Age (mean): carers: 26 (range 14–45) years Sex (male): infants = 51% Country: Kenya (lower middle‐income) Setting: community‐based, linked to 9 vaccinating health facilities in 3 districts (Machakos, Langata, and Njoro), 3 facilities in each district |
|
| Interventions |
Intervention: SMS reminders sent from an automated web‐based system in Kiswahili and English, sent 2 days before (reminding the date of next vaccine and which health facility to attend) and on the day of the scheduled vaccination for the second and third doses of pentavalent vaccine. Content: SMS reminders Frequency and intensity: 4 reminders (2 days before and on day of both second and third dose), reminders were at 10 weeks (–2 days) until 14 weeks Control: 1. standard care/no intervention. 2. targeted non‐digital communication: reminder sticker Co‐interventions: scheduled vaccination due date was indicated on the child's health booklet as per routine procedures. All groups received routine health education and advice on vaccination. |
|
| Outcomes | 1. Receipt of pentavalent vaccine (at 10 and 14 weeks of age); 2. Costs Outcomes reported but not included in the review: 1. Mean days delay in receiving vaccine doses (at 10 and 14 weeks of age) (outcome not eligible for inclusion); 2. Factors associated with missed vaccination (not included in review, results were not reported per group; 3. Did not return for vaccinations (not included in review, those receiving vaccinations were extracted) Outcome assessment time point: 10 and 14 weeks of age corresponding to the second and third doses of the pentavalent vaccine |
|
| Funding/declarations of interest |
Funding: US Center for Disease Control and Prevention Conflicts of interest: authors declared no competing interests. |
|
| Notes | Districts were selected that had > 10% dropout rate for third dose of pentavalent vaccine. Trial ID: not reported Cluster features: 9 health facilities were randomised. Mean cluster size: 124. The study did not adjust for clustering effect for any of the relevant outcomes; we used ICC 0.0487 (derived from k = 0.089 reported in Gibson 2017) to adjust for cluster effect in the analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We selected three health facilities in each district, and randomly allocated each facility …" Comment: no further details reported. |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment. |
| Selective cluster recruitment | High risk | Convenient enrolment of participants likely to have taken place after cluster allocation to intervention arms. Quote: "We selected three health facilities in each district, and randomly allocated each facility to one of the two interventions … or to serve as the control group … Participants were conveniently enrolled in the selected health facilities until the strategy‐level target sample sizes were reached." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind; participants and personnel were aware of cluster allocations for data collection purposes. |
| Blinding of objective outcome assessment (detection bias) | High risk | Personnel were aware of cluster allocations for data collection purposes. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐reported measures were at high risk of detection bias since the study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Flow of participants and clusters through the study was not clearly reported. |
| Selective reporting (reporting bias) | Low risk | Outcomes are reported exhaustively, including for acknowledged limitations. |
| Other bias | High risk | Contamination: acknowledged limitation was that (quote) "If a care giver took the child to another facility for second or third pentavalent dose, the system considered the child unvaccinated." Follow‐up phone‐calls determined that 35 infants had been taken to other centres. Baseline differences: there were no statistical differences in demographic characteristics among carers and children enrolled in each of the 3 groups. |
Hannan 2016.
| Study characteristics | ||
| Methods |
Aim: to test the effects of a NP 2‐way communication mobile phone and texting follow‐up intervention for the first 6 months postbirth in low‐income first‐time mothers and their healthy full‐term infants. Study design: parallel individual RCT Recruitment: first‐time low‐income mothers were enrolled from the Mother Baby Unit at Jackson Memorial Hospital in Miami, FL. Study duration: 6 months Study dates: not reported |
|
| Participants |
Inclusion criteria: first‐time mothers, aged 18 years, any racial/ethnic group, low‐income, understood spoken English or Spanish, access to a mobile phone, delivered a singleton healthy full‐term infant, only infants with limited access to health care were included. Sample size (n): 141 (intervention: 63; control: 66) Age (mean): mothers: 25.3 (SD 5.6) years Sex (male): infants: 55% Country: USA (high‐income) Setting: community, linked to hospital mother and baby unit |
|
| Interventions |
Intervention: 2‐way NP mobile phone intervention that included calls and SMS messages Content: calls and text messages assessing health problems or concerns regarding the infant Frequency and intensity: mobile phone contact and texting on posthospital discharge days 3, 7, 14, 21, then monthly for 6 months. Additionally, intervention group mothers were able to contact the NPs by mobile phone or texting Monday to Saturday Control: standard care/no intervention. Routine hospital discharge care Co‐interventions: if a healthcare concern was stated, the NP followed US paediatric protocols to implement care. If the mother voiced a serious infant complaint such as fever, excessive crying, vomiting, lethargy, or seizure‐like activity, the mother was instructed to contact the 911 emergency systems. Backup paediatricians were available to the NPs for consultation on infant health concerns. |
|
| Outcomes | 1. Immunisations up to date (at 2, 4, 6 months – we included data for the longest time point (6 months)); 2. Infant emergency room attendance (6 months) Outcomes reported but not included in review: 1. Infant hospitalisations (6 months) (outcome not included, for healthcare attendance we included immunisations and emergency department visits); 2. Infant urgent care seeking (6 months) (outcome not included, for healthcare attendance we included immunisations and emergency department visits); 3. Time in days to first well visit (postnatal care appointment) – outcome not eligible for inclusion; 4. Mothers' perceived stress (posthospital discharge) – outcome not eligible for inclusion; 5. Mothers' perceived social support (posthospital discharge) – outcome not eligible for inclusion; 6. Infant well visits received late (first visit, month 1, month 2, month 4, month 6) – outcome not eligible for inclusion Outcome assessment time point: specified above after each outcome |
|
| Funding/declarations of interest |
Funding: funded by MBRS Score National Institute of Health; Eunice Kennedy Shriver National Institute of Child Health & Human Development. Conflicts of interest: author(s) declared no potential conflicts of interest. |
|
| Notes | Trial ID: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "mothers were randomized to a control or intervention group using a table of random numbers." |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants, no information on blinding of study personnel. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Measures collected from mothers were at high risk of detection bias since the study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12 mothers were lost to contact postdischarge due to disconnected mobile phones. It is not reported how many from each group. |
| Selective reporting (reporting bias) | Unclear risk | All expected outcomes and all outcomes listed in the methods section were reported, but no protocol or online trial record available to check against. |
| Other bias | Unclear risk | There were no significant differences in the demographic characteristics between the groups except for the number of years in the US. |
Hofstetter 2015a.
| Study characteristics | ||
| Methods |
Aim: assessed the impact of text message reminders to parents on timely MMR vaccination. Study design: parallel individual RCT Recruitment: parents/children identified through the hospital registration system and its immunisation registry. The registration system included demographic and visit data for participants, and all vaccine doses administered to participants at the hospital and affiliated clinics through the electronic health record. Study duration: 2.5–3.5 months Study dates: June 2011 to October 2012 |
|
| Participants |
Inclusion criteria: parents were eligible for participation if their child: was age 9.5–10.5 months, had a participating clinic visit in the past 6 months, had a mobile phone number listed in the hospital registration system. Sample size (n): 2054 (SMS only: 686; scheduling + SMS: 686; usual care: 682) Age: parents' age not reported, children: 9.5–10.5 months at enrolment Sex (female): SMS only: 48.1%; scheduling + SMS: 49.4%; usual care: 49.0% Country: USA (high‐income) Setting: community, linked to 4 paediatric practices in an ambulatory care network affiliated with a large academic medical centre in New York City. |
|
| Interventions |
Intervention: reminder SMS message 2 days before scheduled appointment. Scheduled SMS messages not sent if a previously arranged appointment was detected in the system. Content: SMS message reminded parents 2 days before a scheduled 1‐year appointment, informed them that doctor would discuss needed vaccines, and asked them to remember to bring the child's vaccination card. SMS messages included the clinic contact information and mentioned the child's need for important vaccines such as measles following the first birthday. Frequency and intensity: 1 reminder SMS 2 days before child's 1‐year vaccination. Up to 3 weekly SMS after randomisation (at child age of 9.5–10.5 months) followed by 1 reminder 2 days before child's 1‐year vaccination. Control: standard care/no intervention. The usual care arm received no text message reminders. Co‐interventions: children in all arms received "usual care," which included a routine automated telephone appointment reminder provided directly from the clinic network 1 day before existing appointments. |
|
| Outcomes | 1. Child receives MMR vaccine between 361 days and 13 months of age; 2. Client satisfaction (13 months) Outcomes reported but not included in the review: 1. 1‐year preventive care visit scheduled at 11–13 months of age (outcome not eligible for inclusion); 2. 1‐year preventive care visit attended 11–13 months of age (outcome not eligible for inclusion); 3. MMR vaccination by 16 months of age (only overall proportion and P value were reported – not included in review, 13‐month time point was included) Outcome assessment time point: 13 months |
|
| Funding/declarations of interest |
Funding: supported by National Center for Immunization and Respiratory Diseases of the Centers for Disease Control and Prevention. Conflicts of interest: unclear: under 'Funding' the authors have listed personal research funding, apparently linked to a different study: quote: "Dr. Hofstetter receives research support for an investigator initiated study funded by the Pfizer Medical Education Group." |
|
| Notes | Trial ID: NCT01199666 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised (quote): "Using a random sample algorithm generator in SPSS 19.0." |
| Allocation concealment (selection bias) | Low risk | Randomisation and delivery of intervention automated and integrated within the hospital registration system and its immunisation registry. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were not aware that they were in a study. Quote: "The study was approved by the Columbia University Medical Center Institutional Review Board with a waiver of consent." Intervention delivered by an automated "text messaging platform integrated with the hospital registration system and its immunization registry." |
| Blinding of objective outcome assessment (detection bias) | Low risk | Data were retrieved electronically from hospital and registry records. Quote: "Study analysts were blinded to group assignments." |
| Blinding of subjective outcome assessment (detection bias) | Low risk | Participants and study analysts were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Medical and vaccination records available for all participants. |
| Selective reporting (reporting bias) | Unclear risk | Online trial record available, but all outcomes listed in methods were reported. |
| Other bias | Low risk | Baseline demographic characteristics were similar between arms. |
Jareethum 2008.
| Study characteristics | ||
| Methods |
Aim: to compare the satisfaction levels of ANC between healthy pregnant women who received SMS via mobile phone for antenatal support, and those who did not. Study design: parallel individual RCT Recruitment: all pregnant women who received ANC and planned to give birth at the study site. Study duration: from 28 weeks of gestation until delivery Study dates: May 2007 to October 2007 |
|
| Participants |
Inclusion criteria: aged > 18 years, no medical diseases or obstetric complications, singleton pregnancy, gestational age < 28 weeks (confirmed by ultrasound) when enrolled in the present study, owner of a mobile phone, able to receive and understand SMS messages Sample size (n): 68 (intervention: 34; standard care: 34) Age (mean): intervention: 28.72 (SD 4.9) years; standard care: 25.97 (SD 6.1) years Sex (female): 100% Country: Thailand (upper middle‐income) Setting: Siriraj Hospital, Bangkok |
|
| Interventions |
Intervention: SMS messages appropriate to the women's gestational age Content: information and warnings relating to abnormal symptoms Frequency and intensity: twice a week (Mondays and Thursdays during the daytime) Control: standard care/no intervention Co‐interventions: all participants received phone calls at 32 weeks' gestation to check both groups were still contacted by the Siriraj antenatal clinic and to confirm that participants could receive and understand SMS messages. All participants received routine antenatal and perinatal care. |
|
| Outcomes | 1. Preterm delivery; 2. Birth weight; 3. Gestational age at birth; 4. Patient satisfaction with intervention (antenatal and perinatal periods) Outcomes reported but not included in the review: 1. Self‐reported level of confidence (outcome not eligible for inclusion); 2. Anxiety (scale not verified, not eligible for inclusion); 3. Route of delivery (vaginal or Caesarean) (outcome not eligible for inclusion) Outcome assessment time point: postpartum |
|
| Funding/declarations of interest |
Funding: not reported Conflicts of interest: not reported |
|
| Notes | Trial ID: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The pregnant women who participated were randomly allocated into 2 groups using a table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No attempts to blind the participants or personnel were reported. Not possible to blind participants due to the nature of the intervention. |
| Blinding of objective outcome assessment (detection bias) | Low risk | It was not reported whether outcome assessors were blinded, but objective pregnancy outcomes (preterm delivery, birth weight, route of delivery, etc.) were collected from the obstetric records at the postpartum ward and were thus considered at low risk of bias. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Subjective outcomes (client satisfaction, confidence, anxiety) were self‐reported by unblinded participants using a questionnaire. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Available‐case analysis with low attrition (10%). 2 (6.3%) women in study group and 2 (6.9%) women in control group changed to deliver at another hospital. 2 (6.9%) women were lost during the follow‐up and 1 (3.4%) woman had her pregnancy aborted before 28 weeks of gestation. The remaining 32 women in study group and 29 in control group were included in analyses. |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the method section were reported in the results section. |
| Other bias | Low risk | No baseline differences between groups. |
Joshi 2015.
| Study characteristics | ||
| Methods |
Aim: to conduct an RCT to test and document the effectiveness of 2 mHealth interventions provided to target women. Study design: cluster RCT Recruitment: a list of all villages in Osmanabad, Solapur, and Washim districts was sent to biostatisticians to randomly select 100 villages each from Osmanabad and Solapur (being larger districts) and 50 villages from Washim district. Then 1743 pregnant women from the 250 villages were enrolled and divided into 2 groups. Study duration: 11–39 weeks of pregnancy Study dates: not reported |
|
| Participants |
Inclusion criteria: women in project area were enrolled from the third or fourth month of pregnancy. Sample size: 1743 (intervention: 1162 participants, 166 clusters; control: 581 participants, 84 clusters*) Age: not reported Sex (female): 100% Country: India (lower middle‐income) Setting: home‐based care |
|
| Interventions |
Intervention: twice‐a‐week mobile phone voice messaging service in local dialect that disseminates targeted, timely, and culturally sensitive preventive information directly to the pregnant women. Content of voice messages as well as animation films were culturally appropriate; timed and targeted as per beneficiary's gestational age; sent in a user specified language and time slot. The range of functions served by mHealth tools included: client education and counselling; diagnostic alerts; information giving; actionable tips to pregnant women for self‐care and foetal health; and encouragement to clients for behaviour change. Content: the voice messaging service was supported by short educational animation film clips displayed on mobile phones for reinforcement of preventive health information. Frequency and intensity: twice a week from 11–39 weeks of pregnancy Control: standard care/no intervention. Co‐interventions: none reported |
|
| Outcomes | 1. Proportion of pregnant women who took iron and folic acid tablets for 100 days; 2. Proportion of births attended by skilled birth assistant/skilled health personnel; 3. Client satisfaction Outcomes reported but not included in the review: 1. Knowledge gain (outcome not eligible for inclusion) Outcome assessment timepoint: not reported |
|
| Funding/declarations of interest |
Funding: Department for International Development (DFID), UK Conflicts of interest: not reported |
|
| Notes | *number of clusters in the control group was not reported but we assumed 84 since the total was 250 and there were 166 intervention clusters. Trial ID: not reported Cluster features: 250 villages were randomised. Mean cluster size: 6.97. The study did not adjust for clustering effect; we used ICC 0.041 for skilled birth attendance and ICC 0.154 for iron and folate tablet adherence (reported in Pagel 2011) to adjust for cluster effects in the analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Villages were randomly selected by a biostatistician, but it is unclear how the participants were randomised. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Selective cluster recruitment | Unclear risk | Unclear whether participants were enrolled before or after clusters had been randomised. Quote: "In the next step, 1743 pregnant women from 250 villages enrolled in RCT were divided into two groups." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐reported measures were at high risk of detection bias since the study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The flow of participants and clusters through the study was not clearly reported. |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registration was mentioned and few details were reported in the paper to determine the risk of reporting bias. |
| Other bias | Unclear risk | Very few details were mentioned to determine any other risk of bias. |
Kamau‐Mbuthia 2013.
| Study characteristics | ||
| Methods |
Aim: to investigate pathways through which mobile phone‐based support may promote exclusive breastfeeding. Study design: parallel individual RCT Recruitment: women in third trimester attending ANC Study duration: up to 3 months postpartum Study dates: not reported |
|
| Participants |
Inclusion criteria: low‐income women in the third trimester attending ANC at a large hospital Sample size (n): 505 (intervention: 153; control: 179)* Age: not reported Sex (female): 100% Country: Kenya (lower middle‐income) Setting: facility based |
|
| Interventions |
Intervention: mobile phone‐based peer support provided by trained peer leaders Content: not reported Frequency and intensity: not reported Control: standard care/no intervention. existing facility‐based standard of care Co‐interventions: not reported |
|
| Outcomes | 1. Receiving postpartum help with breastfeeding; 2. Neonatal morbidity: infant diarrhoeal disease; 3. Infant length and weight (no SD reported); 4. Mastitis: breast pain and engorgement Outcomes reported but not included in the review: 1. Any infant illness (outcome not included, for neonatal morbidity we included 'infant diarrhoeal disease' (see above)); 2. Receiving infant feeding advice from HCWs or others (outcome not included, we included 'receiving postpartum help with breastfeeding' (see above)); 3. Give medicines, vitamins, and minerals (outcome not eligible for inclusion); 5. Return to work by 3 months postpartum (results were not reported) Outcome assessment time point: 3 months postpartum (1 time point for all outcomes) |
|
| Funding/declarations of interest |
Funding: Bill & Melinda Gates Foundation through the Alive and Thrive small grants programme Conflicts of interest: not reported |
|
| Notes |
Trial ID: not reported *1 study arm (peer support group) was not eligible for inclusion in the review. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomized", no further details reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐report by mothers who were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | High risk | Not all outcomes were reported (return to work by 3 months postpartum). |
| Other bias | Unclear risk | The study was reported in 2 conference abstracts with limited information to determine any other risk of bias. |
Kassaye 2016.
| Study characteristics | ||
| Methods |
Aim: to determine the utility of text messages to improve uptake of antenatal and PMTCT service. Study design: cluster RCT Recruitment: HIV‐positive women presenting for ANC Study duration: from enrolment (< 32 weeks' gestation) to 6–8 weeks postpartum Study dates: June 2012 to June 2013 |
|
| Participants |
Inclusion criteria: HIV‐positive pregnant women, < 32 weeks' gestational age, were not currently receiving ARV therapy, were planning to remain in the area for the duration of the study period, and agreed to follow‐up of their infants until 6 weeks following delivery Sample size: 550 (intervention: 280 participants, 13 clusters; control: 270 participants, 13 clusters) Age (median): intervention: 25.5 (IQR 21–29) years; control: 25.6 (IQR 22–29) years Sex (female): 100% Country: Kenya (lower middle‐income) Setting: community, health facilities |
|
| Interventions |
Intervention: automated text messages Content: PMTCT services including appointment reminders and adherence support, motivational messages, male‐partner involvement and engagement in delivery planning and essential child health messages including warning signs and nutrition Frequency and intensity: 3–6 text messages each week (< 32 weeks' gestation to 6–8 weeks postpartum) Control: standard care/no intervention Co‐interventions: none |
|
| Outcomes | 1. ARV adherence – any maternal missed doses in the past week (6–8 weeks postpartum, we did not include earlier time points 36 weeks of gestation and at delivery); 2. Birth in health facility; 3. infant ARV treatment adherence (6 weeks postpartum); 4. infant HIV test (6 weeks postpartum); 5. infant HIV DNA PCR test positive (6 weeks postpartum); 6. number of face‐to‐face or mobile phone communications (delivery) Outcomes reported but not included in the review: 1. Mother on combination ARV therapy (time points: 34–36 weeks' gestation, 7 days, and 6–8 weeks postpartum, outcome not eligible for inclusion) Outcome assessment time point: see above |
|
| Funding/declarations of interest |
Funding: WHO through a grant to the Elizabeth Glaser Pediatric AIDS foundation and the Elizabeth Glaser Pediatric AIDS Foundation. Conflicts of interest: no competing interests to report |
|
| Notes |
Trial ID: NCT01645865 Cluster features: 26 healthcare facilities were randomised. Mean cluster size: 21.15. The study adjusted some outcomes (mother taking antenatal and postnatal ARV) for cluster effect and confounding variables (participant age, gestational age, whether the woman was newly diagnosed with HIV, and disclosure of HIV status to her partner and family). For the remaining outcomes, we used ICCs reported in Pagel 2011: ICC 0.127 (birth in health facility), ICC 0.055 (infant ARV, infant HIV test uptake, infant HIV test positive), and ICC 0.030 (communications between HCW and participant) to adjust for cluster effect in the analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All health facilities were randomly allocated to be an intervention or control site, stratified by high volume (hospitals) and medium and low volumes (health centers and dispensaries)." Comment: information on sequence generation were not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Selective cluster recruitment | Unclear risk | Unclear whether participants were enrolled before or after clusters were allocated to intervention arms. Quote: "Consecutive eligible HIV‐positive pregnant women presenting for ANC were invited to participate." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unable to blind participants. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐report by unblinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition at each stage of follow‐up, no reasons provided, dropouts not included in analysis. |
| Selective reporting (reporting bias) | Unclear risk | Trial registry includes an additional secondary outcome that was not reported in the publication – time to initiation of ARV (clinicaltrials.gov/ct2/show/NCT01645865). |
| Other bias | High risk | There were baseline differences between groups. |
Kebaya 2014.
| Study characteristics | ||
| Methods |
Aim: to compare self‐reported adherence to infant nevirapine prophylaxis and retention in care in HIV‐exposed infants randomised to 2‐weekly mobile phone call vs control (no phone calls). Study design: parallel individual RCT Recruitment: recruited from postnatal wards of 3 health facilities and randomised within 24 hours of birth Study duration: not reported Study dates: not reported |
|
| Participants |
Inclusion criteria: HIV‐positive women and their infants Sample size (n): 150 (intervention: 75; control: 75) Age: not reported Sex (female): 100% Country: Kenya (lower middle‐income) Setting: recruited from postnatal wards of 3 health facilities in Kisumu, treatment was home based. |
|
| Interventions |
Intervention: mobile phone calls Content: reminders on PMTCT messages Frequency and intensity: fortnightly Control: digital, non‐targeted communication: "standard health care messages (no calls)" Co‐interventions: infants received nevirapine prophylaxis for PMTCT |
|
| Outcomes | 1. Attendance for postpartum care appointment (10 weeks); 2. Adherence to newborn PMTCT treatment (nevirapine) (6 weeks) Outcomes reported but not included in the review: 1. Mode of infant feeding (mother report) (results were not reported); 2. Early HIV testing (results were not reported) Outcome assessment time point: 6, 10 weeks |
|
| Funding/declarations of interest |
Funding: not reported Conflicts of interest: not reported |
|
| Notes | Limited information reported in 2 abstracts, no author contact details in abstracts. Trial ID: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report states the study was randomised but no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | Details of allocation concealment not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label RCT. |
| Blinding of objective outcome assessment (detection bias) | Unclear risk | Limited information reported in 2 abstracts. |
| Blinding of subjective outcome assessment (detection bias) | Unclear risk | Limited information reported in 2 abstracts. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Limited information reported in 2 abstracts. |
| Selective reporting (reporting bias) | High risk | Limited information reported in 2 abstracts. However, safe infant feeding and HIV testing were outcome measures mentioned for which results were not reported in any of the abstracts. |
| Other bias | Unclear risk | The study was reported in 2 conference abstracts with limited information to determine any other risk of bias. |
Lund 2012.
| Study characteristics | ||
| Methods |
Aim: to examine the effect of the wired mothers' intervention on ANC, skilled delivery attendance, access to emergency obstetric care, and perinatal mortality. Study design: cluster RCT Recruitment: women who attended ANC at 1 of the 24 selected healthcare facilities were included in their first ANC visit and followed until 42 days after delivery. Study duration: until 6 weeks after delivery Study dates: March 2009 to March 2010 |
|
| Participants |
Inclusion criteria: 1. Clusters: health facilities with the highest number of ANC clients in 2008; availability of ≥ 1 midwife in the facility; mobile phone network coverage; 2. Participants: women aged 14–45 years; pregnant women attending ANC at 1 of 24 selected primary healthcare facilities Sample size: 2637 (intervention: 1351 participants, 12 clusters; control: 1286 participants, 12 clusters) Age group: < 19 years: intervention: 9%; control: 10%; 20–24 years: intervention: 25%; control: 26%; 25–29 years: intervention: 29%; control: 26%; 30–34 years: intervention: 20%; control: 22%; ≥ 35 years: intervention: 18%; control: 17% Sex (female): 100% Country: Tanzania (low‐income) Setting: primary healthcare facilities |
|
| Interventions |
Intervention: SMS + voucher. The frequency of the messages varied depending on the stage of the pregnancy. Content: simple health education and appointment reminders to encourage attendance to routine ANC, skilled delivery attendance, and postnatal care Frequency and intensity: early in the pregnancy, women received 2 messages a month, after gestational week 36, the intensity increased to 2 a week, until 6 weeks after delivery Control: standard care/no intervention. Standard antenatal, delivery, and postnatal services consisted of ≥ 4 ANC visits, skilled attendance at delivery, and a postnatal visit within the first 48 hours for deliveries taking place outside healthcare facilities. Co‐interventions: if the women could not provide a phone number, they received only the mobile phone voucher component. All enrolled women were offered the standard antenatal, delivery, and postnatal services. |
|
| Outcomes | 1. Maternal deaths; 2. Skilled attendant at birth (adjusted ORs split by rural and urban populations); 3. Neonatal death; 4. Attendance ≥ 4 ANC appointments (outcome was selected among attendance at 0 to > 5 appointments because it is the local and global WHO recommendation); 5. Antenatal antitetanus vaccinations; 6. Antenatal preventive treatment for malaria; 7. Premature deliveries; 8. Severe obstetric complications (mother); 9. Client satisfaction with intervention (only reported in intervention group) Outcomes reported but not included in the review: 1. Gestational age at last ANC visit (outcome not eligible for inclusion); 2. Antepartum referrals (outcome not eligible for inclusion); 3. Timing of the mentioned services (outcome not eligible for inclusion); 4. Caesarean section (outcome not eligible for inclusion); 5. Perinatal death (combination of neonatal death and stillbirth) (outcome not eligible for inclusion, we included neonatal deaths) Outcome assessment time point: 6 weeks after delivery (1 time point for all outcomes) |
|
| Funding/declarations of interest |
Funding: Danish International Development Cooperation Conflicts of interest: none declared |
|
| Notes |
Trial ID: NCT01821222 Cluster features: 24 primary healthcare facilities were randomised. Mean cluster size: 110. The study adjusted some outcomes (skilled attendant at birth, attendance at > 4 ANC appointments, perinatal death, antenatal antitetanus vaccinations, antenatal preventive treatment for malaria) for cluster design effect. For the remaining outcomes, we used ICCs reported in Pagel 2011: ICC 0.003 (maternal deaths, premature delivery, severe maternal complications) to adjust for cluster effect in the analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Primary healthcare facilities were assigned by simple random allocation to the mobile phone intervention. Method not described. |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation concealment reported. |
| Selective cluster recruitment | Low risk | All eligible women from the selected clusters were included. Quote: "Women who attended antenatal care at one of the 24 selected healthcare facilities were included on their first antenatal care visit and followed until 42 days after delivery. Women were eligible for study participation irrespective of their mobile phone and literacy status." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither study participants nor clinic staff blinded because of the nature of the intervention requiring overt participation. |
| Blinding of objective outcome assessment (detection bias) | Unclear risk | Antenatal, intrapartum, and neonatal outcomes measured objectively. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No clusters were lost to follow‐up and rate of participant loss to follow‐up was low: 3.0% (40/1351) participants in the intervention group and 3.7% (47/1286) in the control group were lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the online trial register were reported in 3 different publications. |
| Other bias | Low risk | No significant differences between intervention and control groups with regard to baseline characteristics. Cluster sizes were reported and some analyses were adjusted for clustering effects. |
Maslowsky 2016.
| Study characteristics | ||
| Methods |
Aim: to evaluate the effects of a mobile phone‐based intervention, providing postpartum health education and support + 30 days of telephone access to a dedicated on‐call nurse, on postnatal maternal health behaviour, and maternal and infant health. Study design: parallel individual RCT Recruitment: study enrolled consecutive inpatient mothers after delivery of their newborn at a large public hospital or a community clinic with a birthing centre Study duration: 1 call + 30‐day access to call nurse Study dates: 1 June 2012 (start of recruitment) to 31 August 2012 (end of recruitment) |
|
| Participants |
Inclusion criteria: mothers aged ≥ 15 years, spoke Spanish, newborn not admitted to neonatal intensive care unit Sample size (n): 178 (intervention: 102; control: 76) Age (mean): intervention: 27.0 (SD 5.4) years; control: 25.5 (SD 6.2) years Sex (female): 100% Country: Ecuador (upper middle‐income) Setting: community served by a large public hospital or a community clinic with a birthing centre. |
|
| Interventions |
Intervention: telephone‐based education intervention in 2 parts: 1. educational session administered by nurse via phone within 48 hours of hospital discharge; 2. Access to a nurse on‐call during the first 30 days of the newborn's life Content: initial session: advice on newborn feeding, safe sleeping, environment, health red flags, recommended appointments, and excessive crying + advice on mother recognising/preventing infection, bleeding, pain, voiding, contraception, and mood. Second part: mothers could call the nurse to ask questions regarding their own or their newborn's health and care, as needed. Frequency and intensity: 1 call and 30 days of telephone access to receive support from a nurse Control: standard care/no intervention. Brief discharge instructions delivered by a nurse at the time of hospital or clinic discharge, typically including a newborn check‐up within 1 week, a maternal follow‐up visit within 6 weeks, and initiation of a family planning regimen. If mothers required additional support during the postnatal period, they were instructed to attend a local health centre or emergency department. Co‐interventions: none |
|
| Outcomes | 1. Self‐reported breastfeeding; 2. Self‐reported use of contraception; 3. Infant attended newborn check‐up (reported by mother); 4. Self‐reported attendance for postpartum care appointment (narrative result); 5. Acute episodes of illness in infants and mothers (reported by mother); 6. Client satisfaction (only intervention group) Outcomes reported but not included in the review: 1. Infant attended 2‐month check‐up (outcome not eligible for inclusion) Outcome assessment time point: 3 months (1 time point for all outcomes) |
|
| Funding/declarations of interest |
Funding: pilot grant from the University of Michigan Center for Global Health; 2 authors' salaries supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development; 1 author supported in part by grants from the Breast Cancer Research Foundation and the National Cancer Institute. Conflicts of interest: none. |
|
| Notes | Trial ID: not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "… participants were assigned via a random number generator to either the intervention or the control group." |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants not possible, no information on blinding of personnel. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Outcomes were self‐reported by unblinded participants. No information on blinding of study personnel. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate: intervention: 27/102 (26%); control: 16/76 (21%). |
| Selective reporting (reporting bias) | Unclear risk | All outcomes in methods reported, but no protocol available. |
| Other bias | Low risk | Intervention and control groups did not significantly differ in any demographic (Table 2 in paper) or obstetric (Table 3 in paper) characteristic. |
McConnell 2016.
| Study characteristics | ||
| Methods |
Aim: to pilot a programme implemented 3 days after delivery in which a checklist was used by a CHW to assess the health of mother and newborn and targeted health education was offered. Study design: parallel individual RCT Recruitment: women attending selected health facilities were approached by a CHW for recruitment after a normal delivery just prior to their discharge home. Study duration: 1 week (at day 7 after birth) Study dates: April 2014 to October 2014 |
|
| Participants |
Inclusion criteria: women aged 18–40 years, safe normal delivery of a live infant at a Jacaranda Health facility, reside within a 20 km radius from the Jacaranda Health's hospital facility in peri‐urban Nairobi, provide 2 phone numbers Sample size (n): 104 (phone call: 41; home visit: 32; standard care: 31) Age (mean): phone call: 25.6 years; home visit: 25.9 years; standard care: 26.7 years Sex (female): 100% Country: Kenya (lower middle‐income) Setting: facility‐based, i.e. at Jacaranda Health's 10‐inpatient bed hospital in a peri‐urban setting just outside Nairobi |
|
| Interventions |
Intervention: phone/mobile call Content: CHWs call to screen for maternal and newborn danger signs, to deliver targeted postnatal health education, and to refer mothers and their newborns to facility‐based care if necessary using a checklist to guide them through the process that was available in English and Kiswahili. Frequency and intensity: once (at day 3 after delivery) Control: 1. Standard care/no intervention. Standard care from Jacaranda clinic and did not receive any additional postpartum check‐in from CHW. 2. Home visit. Same health screening and education as the intervention, but during CHW house calls Co‐interventions: none |
|
| Outcomes | 1. Exclusive breastfeeding (9 weeks postpartum, the study also reported on this outcome at 10 days postpartum, but we only included the longest follow‐up); 2. Newborn postpartum care sought (10 days postpartum); 3. Maternal postpartum care sought (10 days postpartum); 4. Newborn health problems (10 days postpartum); 5. Maternal health problems (10 days postpartum); 6. Use of family planning method (9 weeks postpartum); 7. Newborn vaccination: ≥ 1 dose of OPV and pentavalent vaccines (9 weeks postpartum) Outcomes reported but not included in review: 1. Days postpartum maternal care sought, among maternal care‐seekers, mean (no SD was reported, outcome not eligible for inclusion) (10 days postpartum); 2. Days postpartum newborn care sought, among maternal care‐seekers, mean (no SD was reported, outcome not eligible for inclusion) (10 days postpartum); 3. Postnatal knowledge (10 days postpartum, outcome not eligible for inclusion); 4. Breastfed ≥ 3 times in past 8 hours (10 days postpartum, 9 weeks postpartum) – outcome not included, we included exclusive breastfeeding (see above); 5. Combined outcome of health knowledge (10 days postdelivery, outcome not eligible for inclusion); 6. Combined outcome of health practices (10 days' and 9 weeks postdelivery, outcome not eligible for inclusion) Outcome assessment time point: 10 days and 9 weeks postpartum |
|
| Funding/declarations of interest |
Funding: Grand Challenges Canada Conflicts of interest: none declared |
|
| Notes | Trial ID: NCT02104635 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment of patient identifiers was done using a randomisation sequence generated by the principal investigators. |
| Allocation concealment (selection bias) | Unclear risk | Participants were individually randomised prior to enrolment using numeric patient identifiers assigned by Jacaranda Health. A unique identifier was given to each Jacaranda Health client seeking any service (including ANC, delivery, postnatal care, and child wellness care) during the client's first visit to Jacaranda. No further details provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to phone call, home visit, or no intervention. |
| Blinding of subjective outcome assessment (detection bias) | High risk | All outcomes collected through a survey with the mothers who were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "We test for differences in outcomes across study arms on an intention‐to‐treat basis, with the treatment arms defined as participants' randomized treatment assignment and the sample including all respondents where data is available (not just those reached by a day 3 intervention)." Many participants could not be reached for outcome surveys, 16–22% for 10‐day survey and 41–45% for 9‐week survey. |
| Selective reporting (reporting bias) | Low risk | All study outcomes were explained and reported. See also ClinicalTrials.gov Identifier: NCT02104635. |
| Other bias | Unclear risk | There were some baseline differences. Quote: "Most of the differences in characteristics across arms are small and not statistically significant, except for a somewhat lower rate of marriage in the call arm (85 % (35/41) vs. 97 % (30/31) and 97 % (30/31) in the standard of care and home visit arms, respectively) and a lower employment rate in the visit arm (41 % (11/27) vs. 66 % (21/32) to 70 % (16/23) in the other arms)." |
Moniz 2013.
| Study characteristics | ||
| Methods |
Aim: to estimate whether text messages encouraging influenza vaccination sent to an ambulatory obstetric population could improve influenza vaccination rates among women unsure about or unwilling to receive the vaccine. Study design: parallel individual RCT Recruitment: participants recruited and enrolled at routine obstetric visits to a Women's Hospital's outpatient clinic Study duration: 12 weeks Study dates: September 2010 (recruitment) to February 2012 (recruitment) |
|
| Participants |
Inclusion criteria: pregnant women, < 28 weeks' gestation, aged 14–50 years, owned a personal mobile phone with text messaging capabilities, reported not receiving that season's influenza vaccine, electronic record lacked documentation of influenza vaccine administration in that season Sample size (n): 216 (intervention SMS: 104; control SMS: 100) Age group: 13–17 years: control/general: 2 (2%), intervention/influenza: 3 (3%); 18–25 years: control/general: 67 (67%), intervention/influenza: 77 (74%); 26–49 years: control/general: 31 (31%), intervention/influenza: 24 (23%) Sex (female): 100% Country: USA (high‐income) Setting: community, served by a single women's hospital |
|
| Interventions |
Intervention: SMS messages Content: SMS messages regarding general preventive health in pregnancy plus the importance of influenza vaccination during pregnancy Frequency and intensity: 12 weekly messages Control: non‐targeted, client communication: participants received 12 weekly text messages regarding general preventive health in pregnancy. General preventive health messages received by all participants covered topics such as the importance of antenatal vitamins, nutritional foods, and seat belt use during pregnancy Co‐interventions: participants in both groups received usual ANC in the outpatient clinic, where ANC providers (nurses, midlevel HCPs, physicians) verbally recommend and offer influenza vaccination at each antenatal visit. |
|
| Outcomes | 1. Attendance for antenatal influenza vaccination; 2. Acceptability of text messaging Outcomes reported but not included in the review: 1. Self‐reported reasons for declining influenza vaccination (outcome not eligible for inclusion) Outcome assessment time point: 12 weeks |
|
| Funding/declarations of interest |
Funding: grant from the Amy Roberts Health Promotion Foundation Conflicts of interest: authors did not report any potential conflicts of interest. |
|
| Notes | Trial ID: NCT01248520 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised to the 2 study arms with equal frequency using a permuted block design with random block sizes of 2, 4, and 6. A researcher uninvolved in participant recruitment or clinical care generated the randomisation sequence. |
| Allocation concealment (selection bias) | Low risk | A researcher uninvolved in participant recruitment or clinical care generated the randomisation sequence and placed group assignments in sequentially numbered, sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Both groups received SMS messages, but only 1 group's messages contained information about influenza vaccination. Uncertain to what extent women were cognisant that the influenza vaccine content was the intervention. HCPs were blind to the groups to which participants were randomised. |
| Blinding of objective outcome assessment (detection bias) | Low risk | Vaccine receipt was verified by review of the clinic's electronic medical record, which automatically documents date of vaccination at the time of vaccine administration. Record review was conducted after exit surveys were completed by a researcher unaware of participants' randomisation allocation. |
| Blinding of subjective outcome assessment (detection bias) | Unclear risk | Unclear whether participants were blinded, thus unclear whether self‐reported measures were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete for ITT analysis, all exclusions accounted for in per‐protocol analysis. |
| Selective reporting (reporting bias) | Low risk | No reason to suspect selective reporting, online trial record was available and results for listed outcomes were reported. |
| Other bias | Low risk | No baseline differences between groups. |
Naughton 2017.
| Study characteristics | ||
| Methods |
Aim: to 1. estimate the effectiveness of pregnancy smoking cessation support delivered by SMS text message, and 2. key parameters needed to plan a definitive trial. Study design: parallel individual RCT Recruitment: research midwives identified potential participants in antenatal clinics via their clinic notes or a screening questionnaire, and interested women were provided with participant information sheets. Study duration: 12 weeks Study dates: February 2014 (start of recruitment) to September 2014 (end recruitment) |
|
| Participants |
Inclusion criteria: pregnant and < 25 weeks' gestation, smoking ≥ 5 cigarettes per day prepregnancy, smoking ≥ 1 cigarette on a typical day during pregnancy, aged ≥ 16 years, agreed to accept information to assist cessation, had own or had primary use of a mobile phone, familiar with sending and receiving text messages, able to understand written English, able to give informed consent Sample size (n): 407 (intervention: 2013; control: 204) Age (mean): intervention: 26.6 (SD 5.7) years; control: 26.4 (SD 5.7) years Sex (female): 100% Country: England (high‐income) Setting: English NHS hospital antenatal clinics |
|
| Interventions |
Intervention: SMS (MiQuit) Content: motivational messages, advice about preparing for a quit attempt, how to manage cravings and withdrawal, dealing with trigger situations, information about how smoking affects babies, and general encouragement Frequency and intensity: daily, according to a delivery schedule (0, 1, or 2 daily texts). Women were able to alter support frequency by texting the keywords MORE or LESS Control: standard care/no intervention Co‐interventions: all participants were given a standard NHS booklet on smoking cessation for mothers‐to‐be and could access smoking cessation information, advice, or support for stopping smoking offered as part of routine ANC. |
|
| Outcomes | 1. Continuous abstinence (i.e. no more than 5 cigarettes in total) between 4 weeks postrandomisation until late pregnancy (approximately 36 weeks' gestation) (both self‐report and objectively verified, we only included the objectively verified measure); 2. Client acceptability (SMS quite or extremely useful, SMS quite or extremely annoying); 3. Economic analysis: total per participant cost (of intervention); 4. Economic analysis: incremental cost per additional quitter Outcomes reported but not included in the review: 1. 7‐day point abstinence at 4 weeks postrandomisation and 36 weeks' gestation (both self‐report and objectively verified) – we excluded these measures and included the long‐term continuous abstinence outcome instead (see above); 2. Use of smoking cessation support during the trial period (outcome not eligible for inclusion); 3. Number of quit smoking attempts between baseline and late pregnancy (we excluded this smoking cessation outcome and included the long‐term continuous abstinence outcome instead (see above)) Outcome assessment time point: assessed at approximately 36 weeks' gestation unless otherwise stated above. |
|
| Funding/declarations of interest |
Funding: National Institute for Health Research (NIHR) under the Programme Grants for Applied Research programme; the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, and the Department of Health, under the auspices of the UK Clinical Research Collaboration. Conflicts of interest: on 2 occasions since 2008, TC paid to attend and present at symposia arranged by Pierre Fabre Laboratories (PFL); PFL is a manufacturer of nicotine replacement therapy. All other authors had no competing interests. |
|
| Notes | Trial ID: NCT02043509 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised individually to usual care or the MiQuit intervention in a 1:1 ratio using the Nottingham Clinical Trials Unit web‐based system. |
| Allocation concealment (selection bias) | Unclear risk | Randomisation used a computer‐generated pseudo‐random code with random permuted blocks of randomly varying size, and stratification was by study site and gestation (< 16 vs ≥ 16 weeks). Following randomisation, unblinded trial team members sent arm‐specific information packs to participants, which included the usual care booklet. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants. |
| Blinding of objective outcome assessment (detection bias) | Low risk | Trial staff involved in follow‐up remained unaware of participants' treatments until questions on the intervention were asked at the end of the study, after smoking outcome data had been collected. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Subjective outcomes self‐reported by unblinded participants. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ITT analysis used. Participants lost to follow‐up or with missing outcome data (around 30–40% depending on outcome and time point) were assumed to be smoking. Quote: "At 4 weeks, 295 (72%) participants provided smoking outcome data (68% MiQuit, 77% usual care). Further attrition in late pregnancy was fairly minimal, with 261 (64%) participants providing these outcome data (64% MiQuit, 65% usual care). Two hundred and thirty (57%) provided smoking outcome data at both time‐points (55% MiQuit, 58% usual care) and 254 (62%) gave data used for smoking outcome 1 on abstinence between 4 weeks and late pregnancy (61% MiQuit, 64% usual care)." |
| Selective reporting (reporting bias) | Low risk | No evidence that outcomes were selectively reported. |
| Other bias | Unclear risk | Quote: "Participants' characteristics were similar in both groups, apart from that women randomized into the usual care group were more likely to reside in the most deprived (e.g. lower income) areas and have a non‐smoking partner." Comment: for the main smoking cessation outcome. Quote: "We obtained validation samples for 37 of 64 (58%) of participants who reported abstinence at 36 weeks gestation (56% MiQuit, 61% usual care); with two (3.1%) and 15 (23%) participants providing only CO [carbon monoxide] or cotinine readings, respectively." |
Niederhauser 2015.
| Study characteristics | ||
| Methods |
Aim: to examine the effect text messages immunisation reminders have on immunisation rates in the first 7 months of life. Study design: parallel individual RCT Recruitment: enrolment at health facilities Study duration: 5 months Study dates: not reported |
|
| Participants |
Inclusion criteria: parent of a child aged 1–28 days, able to speak and read English, having a mobile telephone with text message capabilities, willingness to participate in study for 6 months Sample size (n): 57 (intervention: 30; control: 27) Age (mean): intervention: 31.5 (SD 6.9) years; control: 30.7 (SD 5.7) years Sex: 98% females (mothers). Just 1 father was included in the study. Country: USA (high‐income) Setting: 4 health facilities: 1 large federally qualified health centre, 1 women/infants and children clinic, 1 private paediatric clinic, and the Honolulu Baby Expo, Hawaii |
|
| Interventions |
Intervention: SMS Content: child immunisation reminders Frequency and intensity: 4 and 2 weeks prior to the due date for the infant's 2, 4, and 6‐month vaccinations. From 2 to 7 months of age, i.e. 5 months' duration Control: digital, non‐targeted communication. Messages were age‐appropriate and based on well‐baby information found in Bright Futures in addition to their routine reminders that they received from their HCPs. Co‐interventions: 10% of the parents were randomly selected to receive phone calls verifying the receiving of the messages. |
|
| Outcomes | 1. Immunisation compliance with 5 vaccines (DTaP; hepatitis B; haemophilus influenzae type B; pneumococcal conjugate vaccine; and polio) at 7 months of age Outcomes reported but not included in the review: 1. Barriers to immunisation Survey (SHOTS survey), total score and subscales (outcome not eligible for inclusion) Outcome assessment time point: 2 months and 7 days, 2 months and 14 days, 4 months and 7 days, 4 months and 14 days, 6 months and 7 days, 6 months and 14 days, and 7 months of age – we reported on the longest (7 months) time point only. |
|
| Funding/declarations of interest |
Funding: not reported Conflicts of interest: none declared |
|
| Notes | Trial ID: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | After obtaining a written consent and contact information, using a random number table, parents were assigned to the intervention (30) or control group (27). |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not reported. |
| Blinding of objective outcome assessment (detection bias) | Unclear risk | Not reported. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐reported measures were at high risk of detection bias since the study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The loss to follow‐up of 39% of the intervention group compared to a loss of 10% of the control group, only per‐protocol analysis was done. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes described in the Measures section were included in the Results section, but no protocol or online trial record was available. |
| Other bias | Unclear risk | In comparing the 2 groups, the only difference in the 2 groups that nearly reached significance (P = 0.07), was a higher percentage of intervention (58%) than control (30%) were not married. |
Odeny 2014.
| Study characteristics | ||
| Methods |
Aim: evaluated effect of an interactive, individually tailored, 2‐way text messaging system informed by behavioural theory on maternal postpartum clinic attendance and infant HIV testing within 8 weeks after birth. Study design: parallel individual RCT Recruitment: not reported Study duration: from pregnancy to 6 weeks after delivery Study dates: April 2012 to March 2013 |
|
| Participants |
Inclusion criteria: aged ≥ 18 years, between 28 weeks' gestation and delivery, enrolled in PMTCT, planning to remain in study area, access to a mobile phone, and reported ability to read or had someone who read SMS on their behalf. Women who shared phones were eligible only if they had disclosed their HIV status to the person with whom the phone was shared. Sample size (n): 388 (intervention: 195; standard care: 193) Age (n): 18–24 years: intervention: 60 (30.8%); control: 65 (33.7%); 25–34 years: intervention: 111 (56.9%); control: 111 (57.5%); ≥ 35 years: intervention: 24 (12.3%); control: 17 (8.8%) Sex (female): 100% Country: Kenya (lower middle‐income) Setting: ANC or HIV clinics at 5 health facilities, including a mix of rural and urban settings |
|
| Interventions |
Intervention: text messages Content: educational or motivational messages tailored to gestation week or newborn age Frequency and intensity: 14 messages. Up to 8 were sent during pregnancy (weeks 28, 30, 32, 34, 36, 38, 39, and 40). Additional messages were sent weekly for the first 6 weeks after delivery. Control: standard care/no intervention Co‐interventions: participants in both arms were allowed to call or send SMS to the study nurse at any time. Baseline treatments (n): on ART for own health: 101 (51.8%); 102 (52.8%); received ZDV prophylaxis: 85 (43.6%); 81 (42.0%); received ZDV + 3TC + nevirapine (delivery pack): 60 (30.8%); 53 (27.5%); received ZDV + 3TC (postdelivery pack): 60 (30.8%); 51 (26.4%); nevirapine prophylaxis for baby issued: 139 (71.3%); 133 (68.9%) |
|
| Outcomes | 1. Infant HIV testing; 2. Infant positive virological HIV test results; 3. Maternal postnatal appointment attendance within 8 weeks; 4. Neonatal death/stillbirth Outcome assessment time point: 8 weeks postpartum |
|
| Funding/declarations of interest |
Funding: the National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Eye Institute, National Heart, Blood, and Lung Institute, National Institute of Dental and Craniofacial Research, National Institute On Drug Abuse, National Institute of Mental Health, National Institute of Allergy and Infectious Diseases, and National Institutes of Health Office of Women's Health and Research through the Fogarty International Clinical Research Scholars and Fellows Program at Vanderbilt University and the American Relief and Recovery Act. TAO was a Fogarty International Clinical Research Fellow. CSC was supported by a Research Scientist Development Award from the National Institute of Mental Health, KY was supported by the University of Washington Center for AIDS Research (CFAR), an NIH funded programme. Conflicts of interest: financial competing interests include but are not limited to paid employment or consultancy: CRC served as a paid consultant for CerMed Inc. to help them develop a barrier contraceptive/HIV prevention device. This consultancy ended in 2012. Research grants (from any source, restricted or unrestricted): CRC has active grants from the US NIH, CDC, and Bill & Melinda Gates Foundation. RSM has active grants from the US NIH and Hologic/Gen‐Probe. Travel grants and honoraria for speaking or participation at meetings: CRC received a travel grant to consult with Gynuity on a study they conducted to investigate infections following medical abortion in the United States. Nonfinancial (professional): acting as an expert witness – CRC has served as an expert witness on a case in New York City involving a malpractice suit of a woman who died after delivery due to infectious complications. Membership in a government or other advisory board: CRC was a non‐paid consultant on a WHO panel to assess the risk of hormonal contraception and HIV acquisition in women. RSM has received a donation of study product for treatment of vaginal infections from Embil Pharmaceutical Company. |
|
| Notes | Trial ID: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation scheme with variable block sizes. Investigators and study staff were unaware of block numbers, sizes, or sequences. |
| Allocation concealment (selection bias) | Low risk | Intervention groups assigned using sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Labelled as unblinded. |
| Blinding of objective outcome assessment (detection bias) | Low risk | Women's return visits and infant HIV testing data extracted from clinic records. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analyses were ITT. There were few withdrawals or losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes reported, but no protocol or online trial register to check against. |
| Other bias | Low risk | Maternal characteristics balanced between study arms at baseline. |
Omole 2018.
| Study characteristics | ||
| Methods |
Aim: to determine the impact of pregnancy information and appointment reminder SMSs on maternal health behaviour. Study design: cluster RCT Recruitment: public launch of the project to sensitise health workers and select stakeholders followed by recruitment of random selection of pregnant women in their first trimester who were attending antenatal clinics in selected health facilities in the Ife‐Ijesa zone. Study duration: participants followed up to delivery and completion of immunisation for their children Study dates: December 2013 (start of enrolment) to December 2014 (end of enrolment) |
|
| Participants |
Inclusion criteria: pregnant women residing in Ife‐Ijesa zone, owner of a mobile phone, able to read and write in English or Yoruba (local dialect) language Sample size: 508 (targeted SMS: 260 participants, 2 clusters; non‐targeted SMS: 248 participants, 2 clusters) Age group: 15–24 years: 27.8%; 25–34 years: 59.3%; > 35 years: 13% Sex (female): 100% Country: Nigeria (lower middle‐income) Setting: public health facilities in Ife‐Ijesa area, Osun State, south‐west Nigeria. These are secondary health facilities with the highest number of ANC attendees and delivery within the zone. |
|
| Interventions |
Intervention: pregnancy information and appointment reminder text messages Content: messages for the intervention group included pregnancy‐related information such as birth preparedness, complication readiness, and reminders of antenatal visits. Study participants in the intervention group also had the opportunity of sending text messages to the project team to seek for health information. Frequency and intensity: once a week Control: digital, non‐targeted communication. General health tips, which excluded pregnancy‐related health information and clinic schedule reminders Co‐interventions: none |
|
| Outcomes | 1. Place of birth (health facility); 2. Opinion of respondents about SMS intervention (only intervention group) Outcome assessment time point: at delivery (place of birth) or 6 weeks postpartum (self‐reported questionnaire) |
|
| Funding/declarations of interest |
Funding: The Madiro Fund: Gillian and Adrian Schauer Foundation, Montreal, Canada. Conflicts of interest: none declared |
|
| Notes |
Trial ID: not reported Cluster features: 4 government health facilities were randomised. Mean cluster size: 127. Study did not adjust for clustering effect for the relevant outcome; we used ICC 0.127 (reported in Pagel 2011) to adjust for cluster effect in the analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random sequence generation not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not mentioned/reported. |
| Selective cluster recruitment | High risk | Participants were enrolled after clusters had been allocated to intervention arms. Quote: "This phase started with the public launch of the project to sensitize health workers and select stakeholders. This was followed by recruitment of participants." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants. |
| Blinding of objective outcome assessment (detection bias) | Unclear risk | Blinding of objective outcome assessment not mentioned/reported. |
| Blinding of subjective outcome assessment (detection bias) | Unclear risk | Blinding of subjective outcome assessment not mentioned/reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Table 4 shows primary outcome with high attrition. |
| Selective reporting (reporting bias) | High risk | Primary outcome of study was complete ANC defined as "attendance of at least 4 antenatal clinic visits and delivery in a health facility." The authors only reported on the proportions of delivery in a health facility for a subgroup of pregnant women. |
| Other bias | Unclear risk | Groups differed significantly in their occupational distribution, occupational category of spouses, proportion that had delivered in a health facility in their previous pregnancy, and in reasons for the choice of place of delivery. |
Sharma 2011.
| Study characteristics | ||
| Methods |
Aim: to evaluate the effect of providing oral health education by 2 different modes (text messages and pamphlets), on the knowledge, attitude, and practices of mothers of preschool children and plaque scores of their children. Study design: parallel individual RCT Recruitment: not reported Study duration: 4 weeks Study dates: not reported |
|
| Participants |
Inclusion criteria: mothers proficient in English, owners of a personal mobile phone, familiar with text messaging Sample size: 150 children enrolled, 143 completed study (SMS: 71; control: 72 at completion, numbers per group at enrolment not reported) Age (mean): mothers: not reported; children: text messages: 3.6 (SD 0.5) years; pamphlet: 3.3. (SD 0.5) years Sex: mothers: not reported; children: 83 boys/60 girls (among those who completed the study) Country: India (lower middle‐income) Setting: not reported |
|
| Interventions |
Intervention: SMS Content: messages covered topics that would help the mothers to maintain an optimum oral health for their children and themselves Frequency and intensity: total of 21 messages, either in the form of text messages or pamphlets, were sent in 7 days (3 messages per day). Messages repeated every week for 4 weeks Control: non‐digital, targeted communication. Pamphlets sent daily to the mothers through the children; 3 messages printed on the pamphlet and attached to the daily work diary of each child belonging to the pamphlet group Co‐interventions: not reported |
|
| Outcomes | 1. Visible Plaque Index in children Outcomes reported but not included in the review: 1. Knowledge, attitude, and practices of the mothers (outcome not eligible for inclusion) Outcome assessment time point: 4 weeks (1 time point for all outcomes) |
|
| Funding/declarations of interest |
Funding: not reported Conflicts of interest: not reported |
|
| Notes | Trial ID: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly allocated to the text message group or the pamphlets group. Method of generating sequence not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported/mentioned. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Given nature of intervention, participants could not be blinded. The examiner and statistician who analysed data were blinded. |
| Blinding of objective outcome assessment (detection bias) | Low risk | Examiner and statistician who analysed the data were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 143/150 preschool children and their mothers completed the study. It was not reported which groups the dropouts belonged to. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes described in the Measures section were included in the Results section, but no protocol or online trial record was available. |
| Other bias | Low risk | No apparent baseline differences between groups. |
Stockwell 2015.
| Study characteristics | ||
| Methods |
Aim: to compare the effectiveness of text message vaccine reminders with and without vaccine education vs written reminder‐only on receipt of second dose of influenza vaccine in young, low‐income children. Study design: parallel individual RCT Recruitment: study sites were part of an ambulatory‐care network staffed by 1 centrally administered paediatric group practice, all eligible children seen when research assistants were on‐site were approached. Study duration: 42 days Study dates: August 2012 to March 2013 |
|
| Participants |
Inclusion criteria: parenting adult of child age 6 months to 8 years, child received care at study site (visit in last 12 months), child received 1 dose influenza vaccine and was in need of a second dose in same season season*, parent had mobile phone with text message capability, parent spoke English or Spanish and could read text messages Sample size (n): 660 (conventional SMS: 225; educational SMS: 216; usual care: 219) Age: parents: not reported; children: age group: < 5 years: 83% (550/660); 5–8 years: 17% (110/660) Sex (female): children: 49.5% Country: USA (high‐income) Setting: 3 community‐based paediatric clinics affiliated with New York‐Presbyterian Hospital/Columbia University Medical Center in Northern Manhattan in New York City |
|
| Interventions |
Intervention: 1. SMS vaccine reminders only; 2. SMS vaccine reminders and educational messages Content: SMS reminders contained the date after which the next dose was due and clinic‐specific walk‐in hours. Those in the educational text message arm additionally received educational information that included that the child was not protected until he or she received the second dose, that reaching full protection could take 2 weeks after second dose administration, and that doctors recommended a second dose. In addition, in 1 interactive message, parents could select to receive more information via text message. Messages were sent in English or Spanish based on the participant's request at enrolment. Frequency and intensity: 5 messages – 3 dates before dose was due (day 7, day 21, and day 25 after first influenza vaccine dose), on the day it was due (day 28), and 2 weeks after it was due (day 42) Control: standard care/no intervention. Parents of children randomly assigned to receive usual care did not receive any further intervention beyond the written reminder. Co‐interventions: all families received a written reminder with the date the next influenza vaccine dose was due (routine practice) |
|
| Outcomes | 1. Attendance for second vaccination before end of influenza season; 2. Receipt of a second influenza vaccine dose by 42 days postvaccination (i.e. on time); 3. Client satisfaction Outcome assessment time point: see above |
|
| Funding/declarations of interest |
Funding: institutional career development grant funded by the National Institutes of Health. Conflicts of interest: Dr Hofstetter received support from the Pfizer Medical Education Group for a different investigator‐initiated study; Dr Stockwell is a co‐investigator but received no financial support; Dr Hofstetter also received support through the Investigator‐Initiate. |
|
| Notes |
Trial ID: NCT01662583 *Children in need of a second dose were those who had not received 2 doses of vaccine since July 2010 (the first season the 2009 H1N1‐strain was included in the seasonal vaccine) or those who had not received 2 previous seasonal influenza vaccinations + ≥ 1 × 2009 H1N1‐containing vaccination, either as a seasonal or monovalent pandemic vaccine. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on sequence generation. Quote: "Subjects were randomly assigned centrally with a 1:1:1 allocation at an individual level by using a permuted block design with a block size of 9, stratified by age and clinic site." |
| Allocation concealment (selection bias) | Low risk | Central allocation. Quote: "Subjects were randomly assigned centrally with a 1:1:1 allocation at an individual level by using a permuted block design with a block size of 9, stratified by age and clinic site." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not reported/mentioned. However, due to the nature of the intervention participants (at least) could not be blinded to the intervention. |
| Blinding of objective outcome assessment (detection bias) | Low risk | Vaccination status retrieved from medical records and study analyst was blinded to individual group assignment. |
| Blinding of subjective outcome assessment (detection bias) | High risk | Self‐reported measures were at high risk of detection bias since study was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analyses were ITT, there was only 2 exclusions after randomisation but this was before the launching of the interventions. |
| Selective reporting (reporting bias) | Low risk | All outcomes listed in the online trial record (NCT01662583) were reported. |
| Other bias | Low risk | No significant baseline differences. |
Yudin 2017.
| Study characteristics | ||
| Methods |
Aim: to evaluate if text message reminders increase the likelihood of receiving the influenza vaccine among pregnant women. Study design: parallel individual RCT Recruitment: women were approached in the waiting room by research personnel who were not part of the clinical care team and were asked if they were interested in enrolling in a study investigating the use of text messages in pregnancy. Women were told the messages would be about health‐related behaviour in pregnancy, but no mention was made of influenza or vaccination at the time of recruitment. Study duration: 4 weeks Study dates: November 2014 (start recruitment) to March 2014 (end recruitment) |
|
| Participants |
Inclusion criteria: pregnant woman, aged ≥ 18 years, working mobile phone with ability to receive text messages, ability to speak or understand English Sample size (n): 317 (SMS: 153; standard care: 164) Age (mean): intervention: 32.2 (SD 4.5) years; control: 32.4 (SD 4.9) years Sex (female): 100% Country: Canada (high‐income) Setting: hospital‐based antenatal clinic at St Michael's Hospital, which is a women's health ambulatory care clinic in downtown Toronto |
|
| Interventions |
Intervention: SMS Content: SMS messages reinforcing that the influenza vaccine is recommended for all pregnant women and safe during pregnancy and breastfeeding Frequency and intensity: weekly (2 SMS/week) Control: standard care/no intervention. All women attending the clinic were given a pamphlet containing information about the risks of influenza during pregnancy, the importance of the vaccine for pregnant women, and the fact that the vaccine is safe in pregnancy and breastfeeding. Co‐interventions: all women received usual ANC, including the verbal recommendation for influenza vaccination. |
|
| Outcomes | 1. Attendance for influenza vaccination; 2. Satisfaction with receiving SMS and opinion on timing and number of SMS received Outcomes reported but not included in the review: Outcome assessment time point: 6 weeks postpartum (1 time point for all outcomes) |
|
| Funding/declarations of interest |
Funding: St Michael's Hospital Innovation Fund Grant Conflicts of interest: not reported |
|
| Notes | Trial ID: NCT02428738 (registered as a case control study) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator. |
| Allocation concealment (selection bias) | Low risk | Group allocation was assigned using sequentially numbered, sealed, opaque envelopes which were opened at the time of randomisation by study staff. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Women were told the messages would be about health‐related behaviour in pregnancy, but no mention was made of influenza or vaccination at the time of recruitment. Medical and nursing staff caring for the women were blinded to study group allocation and were not involved in any aspects of the study. |
| Blinding of subjective outcome assessment (detection bias) | Low risk | Self‐reported subjective outcomes among participants who were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The final analysis was based on the actual treatment received and included 281/317 randomised participants. All analyses using ITT groupings were repeated and there were no changes in results when compared to the analyses based on treatment received (data available upon request). |
| Selective reporting (reporting bias) | Low risk | Outcomes listed in the online trial registration were reported. |
| Other bias | Unclear risk | No significant baseline differences. |
3TC: lamivudine; ANC: antenatal care; ART: antiretroviral therapy; ARV: antiretroviral; BCG: Bacillus Calmette‐Guérin; CHW: community health worker; DPT: diphtheria, pertussis (whooping cough), and tetanus; DTaP: diphtheria, tetanus, and whooping cough (pertussis); EPI: Expanded Programme on Immunisations; HCP: healthcare provider; HCW: healthcare worker; ICC: intracluster correlation coefficient; IQR: interquartile range; ITT: intention to treat; KES: Kenyan shilling; LMIC: low‐ to middle‐income country; n: number of participants; NHS: National Health Service; NP: nurse practitioner; OPV: oral polio vaccine; OR: odds ratio; PCR: polymerase chain reaction; PMTCT: prevention of mother‐to‐child transmission; RCT: randomised controlled trial; SD: standard deviation; SMS: short message service; WHO: World Health Organization; ZDV: zidovudine.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Atukunda 2017 | Irrelevant intervention – including digital tracking component. |
| Bracken 2014 | Irrelevant intervention – not exclusively using mobile device. |
| Broberg 2013 | Irrelevant intervention – not exclusively using mobile device. |
| Carlsen 2013 | Irrelevant intervention – not exclusively using mobile device. |
| Collier 2005 | Irrelevant intervention – not exclusively using mobile device. |
| Gallegos 2014 | Irrelevant study design – not randomised controlled trial. |
| Haberer 2016 | Irrelevant intervention – including digital tracking component. |
| Hashemian 2015 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Herring 2016 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Hofstetter 2015b | Irrelevant population – parents of children older than 5 years. |
| Irons 2015 | Irrelevant study design – not randomised controlled trial. |
| Jimenez 2017 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Kofinas 2014 | Irrelevant intervention – not targeted client communication. |
| Lau 2013 | Irrelevant study design – not randomised controlled trial. |
| Lau 2014 | Irrelevant study design – not randomised controlled trial. |
| Lewis 2012 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Maduka 2013 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Mauriello 2016 | Irrelevant intervention – not exclusively using mobile device. |
| Milani 2015 | Irrelevant intervention – not exclusively using mobile device. |
| Moore 2013 | Irrelevant intervention – including digital tracking component. |
| Moore 2015 | Irrelevant intervention – including digital tracking component. |
| Murthy 2019 | Quasi‐randomised study. |
| Mwapasa 2017 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Oakley‐Girvan 2016 | Irrelevant study design – not randomised controlled trial. |
| Patel 2014 | Irrelevant intervention – not exclusively using mobile device. |
| Peitzmeier 2016 | Irrelevant intervention – not exclusively using mobile device. |
| Pollak 2014 | Irrelevant intervention – including digital tracking component. |
| Prieto 2016 | Irrelevant study design – not randomised controlled trial. |
| Pérez‐Ferre 2010 | Irrelevant intervention – including digital tracking component. |
| Rampersaud 2016 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Rand 2015 | Irrelevant population – parents of adolescents receiving vaccination reminders. |
| Rand 2017 | Irrelevant population – parents of adolescents receiving vaccination reminders. |
| Reeder 2014 | Irrelevant intervention – not exclusively using mobile device. |
| Reid 2014 | Irrelevant study design – not randomised controlled trial. |
| Richman 2016 | Irrelevant intervention – not exclusively using mobile device. |
| Robbins 2013 | Irrelevant intervention – not exclusively using mobile device. |
| Sridhar 2013 | Irrelevant intervention – not exclusively using mobile device. |
| Sridhar 2014 | Irrelevant intervention – not targeted communication. |
| Stern 2013 | Irrelevant intervention – not exclusively using mobile device. |
| Stockwell 2012 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Szilagyi 2013 | Irrelevant intervention – not exclusively using mobile device. |
| Takeuchi 2016 | Irrelevant intervention – targeted communication used in conjunction with other interventions. |
| Tarrant 2014 | Irrelevant intervention – not exclusively using mobile device. |
| Trent 2013 | Irrelevant study design – not randomised controlled trial. |
| Trent 2015 | Irrelevant study design – not randomised controlled trial. |
| Van Ryswyk 2015 | Irrelevant comparison group – control group also received targeted communication. |
| Wright 2012 | Irrelevant intervention – not exclusively using mobile device. |
| Young 2013 | Irrelevant intervention – not targeted communication. |
| Young 2014 | Irrelevant intervention – not targeted communication. |
Characteristics of studies awaiting classification [ordered by study ID]
Abroms 2017a.
| Methods | Aim: to test whether an interactive and intensive text messaging programme, Quit4baby, can promote smoking cessation for pregnant women already enrolled in a health text messaging programme, Text4baby. Study design: randomised controlled trial Study dates: July 2015 to February 2016 |
| Participants | 497 pregnant smokers recruited among 'Text4baby' subscribers in the USA (except CA, OK, OH, and LA) |
| Interventions | TCC: Quit4baby text messages + Text4baby text messages Control: Text4baby text messages |
| Outcomes | Smoking cessation outcomes |
| Notes | Trial ID: NCT02412865 |
Abroms 2017b.
| Methods | Aim: to test the acceptability and feasibility of SmokefreeMOM, a national smoking cessation text‐messaging programme for pregnant smokers. Study design: randomised controlled trial Study dates: September 2014 to May 2016 (recruitment) |
| Participants | 99 pregnant smokers recruited from obstetrics‐gynaecology clinics in Washington DC, USA. |
| Interventions | TCC: SmokefreeMOM text messaging programme Control: mailed self‐help materials on quitting smoking while pregnant + 1 text message referring to telephone quit line |
| Outcomes | 1. Programme acceptability and feasibility; 2. Use of treatments and resources for quitting at 1 month; 3. Smoking‐related outcomes |
| Notes | Trial ID: NCT02412956 |
Altazan 2019.
| Methods | Aim: to assess the effect of a behavioural intervention targeting excess gestational weight gain. Study design: randomised controlled trial. Study dates: February 2013 to October 2015 |
| Participants | 54 pregnant women who were overweight or obese recruited through advertisements and targeted emails and referrals from local obstetricians in Baton Rouge, LA, USA. |
| Interventions | TCC 1: SmartMoms through mobile application TCC 2: SmartMoms in person Control: usual care |
| Outcomes | 1. Weight; 2. Mood; 3. Quality of life |
| Notes | Trial ID: NCT01610752 |
Bangal 2018.
| Methods | Aim: to assess the influence of mobile communication between health facility and pregnant women on utilisation and outcome of maternal health services. Study design: randomised controlled trial Study dates: not reported |
| Participants | 400 pregnant women in India (region not reported) |
| Interventions | TCC: mobile phone calls as reminders about next visit and SMS on maternal health Control: usual care |
| Outcomes | 1. Antenatal care visits; 2. Institutional deliveries, 3. Perinatal mortality; 4. Complications during pregnancy; 5. Postnatal follow‐up |
| Notes | Trial ID: not reported |
Domek 2019.
| Methods | Randomised controlled trial |
| Participants | Carers of children aged 6 weeks to 6 months who received first dose of primary vaccination series |
| Interventions | TCC: SMS message reminders 1 week before scheduled vaccination Control: usual care |
| Outcomes | 1. Completion of vaccine primary series; 2. Factors associated with immunisation delays; 3. Acceptability of SMS vaccine reminders; 4. Timeliness of immunisation |
| Notes | Trial ID: NCT02567006 |
Forinash 2018.
| Methods | Aim: to evaluate the impact of text messaging on smoking cessation rates among pregnant women. Study design: randomised controlled trial Study dates: May 2014 to January 2016 |
| Participants | 49 pregnant women in the preparation stage of quitting smoking recruited from a maternal foetal care centre in Saint Louis, USA |
| Interventions | TCC: text messaging Control: usual care |
| Outcomes | 1. Self‐reported cessation rates at 1 month, as verified by exhaled carbon monoxide levels |
| Notes | Trial ID: NCT03024606 |
Gibson 2019.
| Methods | Aim: to determine if text message reminders, with or without mobile phone‐based incentives, can improve measles immunisation coverage and timeliness in rural western Kenya. Study design: randomised controlled trial Study dates: enrolment to March 2017 |
| Participants | 537 carers of infants aged 6–8 months in Siaya County, Kenya |
| Interventions | TCC 1: SMS reminders for measles vaccine TCC 2: SMS reminders plus a KES 150 incentive Control: usual care |
| Outcomes | 1. Measles vaccination coverage; 2. Time to measles vaccination |
| Notes | Trial ID: NCT02904642 |
Harari 2018.
| Methods | Aim: to test the acceptability and feasibility of the Lactation Advice thru Texting Can Help intervention. Study design: randomised controlled trial Study dates: not reported |
| Participants | 58 pregnant women that intended to breastfeed recruited from 2 women, infants, and children breastfeeding peer counselling programmes in CT, USA |
| Interventions | TCC: peer counselling support with texting (breastfeeding education and support from peer counsellors) Control: peer counselling support without texting |
| Outcomes | 1. Breastfeeding status; 2. Early postpartum contact; 3. Feasibility and acceptability |
| Notes | Trial ID: NCT02214849 |
Harrington 2019.
| Methods | Aim: to assess the effect of 2‐way SMS with a nurse on postpartum contraceptive use among individual women and couples. Study design: randomised controlled trial Study dates: July 2016 to September 2017 |
| Participants | 260 pregnant women (with the option to include male partners) recruited from 2 public hospitals in western Kenya |
| Interventions | TCC: automated family planning‐focused SMS messages Control: usual care |
| Outcomes | Contraceptive use |
| Notes | Trial ID: NCT02781714 |
Hmone 2017.
| Methods | Aim: to implement a breastfeeding promotion intervention using mobile phone text messages in Yangon, Myanmar, and evaluate its impact on breastfeeding practices. Study design: randomised controlled trial Study dates: January to March 2015 (recruitment) |
| Participants | 358 pregnant women of 28–34 weeks' gestation recruited from the Central Women's Hospital in Yangon, Myanmar |
| Interventions | TCC: breastfeeding promotional SMS messages 3 times a week Control: maternal and child healthcare messages (excluding breastfeeding‐related messages) once a week |
| Outcomes | 1. Breastfeeding outcomes; 2. Other infant feeding practices; 3. Client satisfaction |
| Notes | Trial ID: ACTRN12615000063516 |
Jasemzadeh 2018.
| Methods | Aim: to investigate the impact of extended parallel process model (EPPM)‐based SMS on protective behaviours of pregnant women in reducing diseases caused by air pollution. Study design: randomised controlled trial Study dates: May 2015 to March 2016 |
| Participants | 130 pregnant women in Ahvaz, Iran |
| Interventions | TCC: SMS intervention Control: usual care |
| Outcomes | 1. Perceived severity or air pollution; 2. Response efficacy; 3. Self‐efficacy; 4. Protective behaviours against air pollution |
| Notes | Trial ID: IRCT2016102810804N8 |
Oliveira‐Ciabati 2017.
| Methods | Aim: to determine whether PRENACEL (a bi‐directional, mobile‐phone based, SMS) increases the coverage of recommended antenatal care practices. Study design: cluster‐randomised controlled trial Study dates: April to June 2015 |
| Participants | 1210 pregnant women invited through leaflets and posters in Brazil |
| Interventions | TCC: text messages with health education and health promotion content related to pregnancy and childbirth Control: usual care |
| Outcomes | Antenatal care outcomes |
| Notes | Trial ID: RBR‐54zf73 |
Ortiz 2018.
| Methods | Aim: to explore the safety and feasibility of using text messages in Colombia as an alternative to in‐person follow‐up after medication abortion for women with no clinical indication for an in‐person visit. Study design: randomised controlled trial Study dates: 2014 |
| Participants | Women after medication abortion recruited from a medical health centre in Bogota, Colombia (number of participants not reported in this conference abstract) |
| Interventions | TCC: SMS over 14 days containing clinical information and supportive messaging Control: usual care |
| Outcomes | 1. Abortion complications; 2. Client satisfaction |
| Notes | Trial ID: not reported |
Palacios 2018.
| Methods | Aim: to test the effects of weekly SMS for improving infant feeding practices and infant weight. Study design: randomised controlled trial Study dates: not reported |
| Participants | 202 carers of healthy term infants aged 0–2 months participating in the women, infants and children programme in Puerto Rico and Hawaii, USA |
| Interventions | TCC: text messages on breastfeeding, preventing overfeeding, delaying introduction of solid foods, and delaying and reducing baby juice consumption Control: text messages related to general infant's health issues related to sleeping, bathing, teething, travelling in a car, medications, handling baby, smoking, information related to immunisation, and care of common illnesses |
| Outcomes | 1. Infant feeding practices; 2. Infant weight status |
| Notes | Trial ID: NCT02903186 |
Patel 2018.
| Methods | Aim: to assess effectiveness of mobile phones for personalised lactation consultation to improve breastfeeding practices. Study design: cluster‐randomised controlled trial Study dates: August 2010 to June 2012 |
| Participants | 1036 pregnant women residing in urban slums recruited from 4 urban, public, maternity hospitals in Nagpur, India |
| Interventions | TCC: weekly mobile phone counselling and daily text messages Control: usual care |
| Outcomes | 1. Breastfeeding outcomes; 2. Other infant feeding practices; 3. Client satisfaction; 4. Cost effectiveness |
| Notes | Trial ID: CTRI/2011/06/001822 |
Seth 2018.
| Methods | Aim: to evaluate the role of compliance‐linked incentives vs mobile phone messaging to improve childhood immunisations. Study design: randomised controlled trial Study dates: July 2016 to July 2017 |
| Participants | 608 carers of children aged ≤ 24 months and pregnant women from a rural community in Mewat region, Haryana state, India |
| Interventions | TCC: automated text and voice reminders TCC 2: automated text and voice reminders + incentives (mobile‐phone minutes) Control: usual care |
| Outcomes | 1. Immunisation coverage; 2. Timeliness of immunisations |
| Notes | Trial ID: NCT03180138 |
Shinde 2018.
| Methods | Aim: to evaluate the effectiveness of the vaccine reminder system among nursing mothers. Study design: randomised controlled trial Study dates: December 2016 and March 2017 (recruitment) |
| Participants | 125 nursing mothers of newborn babies aged 0–3 weeks recruited from maternity wards of a tertiary care teaching hospital in South Canara district, Karnataka state, India |
| Interventions | TCC: SMS vaccination reminders Control: usual care |
| Outcomes | 1. Vaccination coverage; 2. Client satisfaction |
| Notes | Trial ID: not reported |
Shorey 2017.
| Methods | Aim: to examine the effectiveness of Home‐but not Alone, a postnatal psychoeducational programme delivered via a mobile‐health application for parents during the early postpartum period to improve parenting outcomes. Study design: randomised controlled trial Study dates: December 2015 to May 2016 |
| Participants | 250 parents recruited from a local tertiary hospital in Singapore |
| Interventions | TCC: mobile‐health application Control: usual care |
| Outcomes | 1. Parental self‐efficacy, 2. Social support; 3. Postnatal depression; 4. Parenting satisfaction |
| Notes | Trial ID: ISRCTN99092313 |
Unger 2018.
| Methods | Aim: to assess the effect of SMS communication on facility delivery, exclusive breastfeeding, and contraceptive use. Study design: randomised controlled trial Study dates: August 2013 to April 2014 (recruitment) |
| Participants | 300 pregnant women attending antenatal care recruited from a public sector maternal child health clinic in Nairobi, Kenya |
| Interventions | TCC 1: 1‐way SMS TCC 2: 2‐way SMS Control: usual care |
| Outcomes | 1. Facility delivery; 2. Exclusive breastfeeding; 3. Contraceptive use |
| Notes | Trial ID: NCT01894126 |
Wang 2018.
| Methods | Aim: to evaluate the effectiveness of daily text messages as a means to improve carers' adherence to infant micronutrient powder in rural Shaanxi Province of China. Study design: cluster‐randomised controlled trial Study dates: April to July 2013 |
| Participants | 638 carers of infants aged 6–11 months in randomly selected villages in rural Shaanxi Province, China |
| Interventions | TCC: daily text messages + free micronutrient powder packets Control: usual care + free micronutrient powder packets |
| Outcomes | 1. Adherence to infant micronutrient powder |
| Notes | Trial ID: ISRCTN44149146 |
Xie 2018.
| Methods | Aim: to evaluate the potential benefits of implementing the World Health Organization maternal education programme using text messaging in a remote area in China. Study design: cluster‐randomised controlled trial Study dates: October 2011 to August 2012 (recruitment) |
| Participants | 13,937 pregnant women aged 16–45 years who were registered by local Maternal Child Health unit during the study period in Hunan, China |
| Interventions | TCC: mobile phone text messages containing maternal and newborn healthcare education Control: usual care |
| Outcomes | Neonatal and maternal mortality and morbidity |
| Notes | Trial ID: NCT01775150 |
SMS: short message service; TCC: targeted client communication.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12618000636257.
| Study name | Investigating the impact of short automated text message reminder system in improving influenza vaccine uptake in children with chronic lung conditions: a randomised controlled trial. |
| Methods | Randomised controlled trial |
| Participants | Parents of children aged 6 months to 18 years with chronic lung diseases attending the Sydney Children's Hospital, Australia |
| Interventions | TCC: SMS text reminder + education flyer Control: usual care |
| Outcomes | 1. Vaccination coverage; 2. Parental attitudes towards vaccination; 3. Client satisfaction |
| Starting date | April 2018 |
| Contact information | Dr Nusrat Homaira; n.homaira@unsw.edu.au |
| Notes | Trial ID: ACTNR12618000636257 |
Adam 2019.
| Study name | The Philani MOVIE study: a cluster‐randomised controlled trial of a mobile video entertainment‐education intervention to promote exclusive breastfeeding in South Africa. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Pregnant women within the under‐resourced settlements of the Western Cape Province in South Africa |
| Interventions | TCC: 13 short (2–5 minutes), educational videos shared via smartphones Control: usual care |
| Outcomes | 1. Exclusive breastfeeding (1 and 5 months); 2. Other breastfeeding and infant feeding outcomes |
| Starting date | November 2018 |
| Contact information | Maya Adam; madam@stanford.edu and Charles Prober; cprober@stanford.edu |
| Notes | Trial ID: NCT03688217 |
CTRI/2018/04/013510.
| Study name | Effectiveness of mHealth for improving fetal outcome: a community based intervention trial. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Pregnant women gestation > 16 weeks in urban slums of Jaipur, India |
| Interventions | TCC: daily audio calls via interactive voice response system Control: usual care |
| Outcomes | 1. Birth weight; 2. Post‐term/preterm; 3. Healthcare service utilisation |
| Starting date | February 2016 |
| Contact information | Manisha Malik (drmanishamalik@gmail.com); Vaseem Naheed Baig (drvaseemnaheed@yahoo.com) |
| Notes | Trial ID: CTRI/2018/04/013510 |
Cyan 2016.
| Study name | Affordable technology for saving maternal and infant lives |
| Methods | Cluster‐randomised controlled trial |
| Participants | Pregnant women enrolled during the first trimester of pregnancy in villages in Pakistan |
| Interventions | Trial has 5 arms to test the effectiveness of higher vs lower frequency of messages, messages timed with progression of pregnancy and messages linked with small financial incentives. A concurrent intervention provides health literacy support to LHWs. |
| Outcomes | 1. Adoption of intrapartum care; 2. Health literacy scores; 3. Health outcomes of mother and infant |
| Starting date | Not reported |
| Contact information | R Cyan, Georgia State University, Atlanta |
| Notes | Trial ID: not reported |
Gelano 2018.
| Study name | Effect of mobile‐health on maternal health care service utilization in Eastern Ethiopia: study protocol for a randomised controlled trial. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Pregnant women in Haramaya and Kombolcha districts, Oromia Regional State, Eastern Ethiopia |
| Interventions | TCC: voice messages Control: usual care |
| Outcomes | 1. Antenatal care visits; 2. Institutional delivery; 3. Postnatal care visits; 4. Pregnancy outcomes |
| Starting date | Not reported |
| Contact information | Tilayie Feto, gelanotilaye@gmail.com |
| Notes | Trial ID: PACTR201704002216259 |
Gul 2019.
| Study name | An mHealth trial to promote the use of postpartum contraception (PPFP). |
| Methods | Randomised controlled trial |
| Participants | Married, pregnant women with gestational age up to 20 weeks |
| Interventions | TCC 1: text and voice messages regarding antenatal and postnatal care and family planning services TCC 2: interactive phone calls regarding antenatal and postnatal care and family planning services Control: usual care |
| Outcomes | 1. Postpartum contraceptive uptake; 2. Skilled birth; 3. Immunisation; 4. Intention to adopt modern contraception |
| Starting date | September 2018 |
| Contact information | Ishaque Sheikh (ishaque.sheikh@mariestopes.org.pk); Junaid‐ur‐Rehman Siddiqui (junaidrehman1994@hotmail.com) |
| Notes | Trial ID: NCT03612518 |
IRCT20180520039728N1.
| Study name | Effectiveness of the distance education program on the mothers' empowerment in breast‐feeding. |
| Methods | Randomised controlled trial |
| Participants | 72 pregnant women referred to midwifery clinics of educational hospitals affiliated to Babol University of Medical Sciences, Iran |
| Interventions | TCC: text messages Control: standard care |
| Outcomes | 1. Mothers' breastfeeding empowerment; 2. Exclusive breastfeeding |
| Starting date | June 2018 |
| Contact information | Fatemeh Bakouei, f.bakouei@mubabol.ac.ir |
| Notes | Trial ID: IRCT20180520039728N1 |
ISRCTN13224744.
| Study name | The effectiveness of theory based intervention using social media to reduce urinary incontinence among postpartum women in Hebron city hospitals. |
| Methods | Randomised controlled trial |
| Participants | Women with urinary incontinence after child delivery in Hebron City, Palestinian Territory |
| Interventions | TCC: WhatsApp messages Control: usual care |
| Outcomes | 1. Severity of urinary incontinence; 2. Level of practice of pelvic floor muscle exercise |
| Starting date | August 2018 |
| Contact information | zinat.mesk@gmail.com |
| Notes | Trial ID: ISRCTN13224744 |
ISRCTN15017499.
| Study name | A trial exploring the feasibility of using telephone support (SMS and call) as a means of supporting young mothers (12–19 years) in Western Kenya soon after giving birth. |
| Methods | Randomised controlled trial |
| Participants | New mothers aged 12–19 and qualified midwives at the study hospitals in western Kenya |
| Interventions | TCC: weekly text messages and telephone calls every 3 weeks for 10 weeks in total Control: usual care |
| Outcomes | 1. Feasibility and acceptability of the intervention; 2. Quality of data available; 3. Maternal social support; 4. Maternal self‐esteem; 5. Mother–infant bonding; 6. Postnatal depression |
| Starting date | September 2015 |
| Contact information | Mr Elijah Kirop (elroprotich@gmail.com) |
| Notes | Trial ID: ISRCTN15017499 |
Kazi 2019.
| Study name | Mobile phone SMS messages and automated calls in improving vaccine coverage among children in Pakistan. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Carers of children aged < 14 days |
| Interventions | TCC 1: 1‐way SMS messages related to routine immunisation TCC 2: 2‐way SMS messages related to routine immunisation with the option to reply and receive more information through text messages TCC 3: 1‐way automated calls related to routine immunisation TCC 4: 2‐way automated calls related to routine immunisation with the option to reply and receive more information through phone call Control: usual care |
| Outcomes | 1. Number of children who got vaccinated for routine immunisation scheduled at 6, 10, and 14 weeks of life; 2. Mean improvement in on‐time vaccination for routine immunisation scheduled at 6, 10 and 14 weeks of life |
| Starting date | January 2018 |
| Contact information | Abdul M Kazi (momin.kazi@aku.edu) |
| Notes | Trial ID: NCT03341195 |
Lefevre 2019.
| Study name | Impact evaluation of maternal health information messaging in India. |
| Methods | Randomised controlled trial |
| Participants | Women 5–7 months pregnant |
| Interventions | TCC: mobile phone health information messages Control: usual care |
| Outcomes | 1. Exclusive breastfeeding; 2. Immediate breastfeeding |
| Starting date | July 2018 |
| Contact information | Amnesty LeFevre (aelefevre@gmail.com); Aarushi Bhatnagar (aarushi.bhatnagar@btspmle.com) |
| Notes | Trial ID: NCT03576157 |
Maycock 2015.
| Study name | Parent Infant Feeding Initiative (PIFI) |
| Methods | Randomised controlled trial |
| Participants | Mothers and their male partners attending antenatal classes at selected public and private hospitals with maternity departments in Perth, Western Australia |
| Interventions | Fathers will be randomly allocated to either the usual care control group, 1 of 2 medium intensity (MI1 and MI2) interventions, or a high intensity (HI) intervention. MI1 will include a specialised antenatal breastfeeding education session for fathers with supporting print materials. MI2 will involve the delivery of an antenatal and postnatal social support intervention delivered via a smartphone application and HI will include both the specialised antenatal class and the social support intervention. |
| Outcomes | 1. Duration of any and exclusive breastfeeding; 2. Age of introduction of formula and complementary foods; 3. Infant feeding attitudes of both partners |
| Starting date | August 2015 |
| Contact information | Jane A Scott (jane.scott@curtin.edu.au) |
| Notes | Trial ID: ACTRN12614000605695 |
NCT02371213.
| Study name | Social networking on mobile phone to improve maternal and neonatal outcomes (HISONET). |
| Methods | Randomised controlled trial |
| Participants | Thai women who attend antenatal care clinic and have intention to deliver at the study hospital. |
| Interventions | TCC: audio‐video media via social networking on mobile phone to antenatal women from the first antenatal care visit 4 times every month and 4 times biweekly + usual antenatal care group‐health education Control: usual care |
| Outcomes | 1. Rates of premature birth; 2. Rate of respiratory distress syndrome; 3. Rate of stillbirth; 4. Rate of perinatal mortality |
| Starting date | April 2015 |
| Contact information | Krissada Tomyabatra, Nopparatrajathanee Hospital |
| Notes | Trial ID: NCT02371213 |
NCT03023033.
| Study name | Supporting attendance for facility delivery and infant health (SAFI). |
| Methods | Randomised controlled trial |
| Participants | HIV positive and HIV negative pregnant women in Tanzania |
| Interventions | TCC 1: SMS health promotion and reminder messages TCC 2: SMS health promotion and reminder messages + payment scaled to reflect typical transport costs to facility Control: usual care |
| Outcomes | 1. Attendance for early infant diagnosis of HIV; 2. Early identification of HIV exposed infants at reproductive and child health clinic; 3. Antenatal care visits; 4. Facility delivery; 5. Postnatal care visits; 6. Nevirapine at delivery |
| Starting date | October 2014 |
| Contact information | Godfrey Woelk, Elizabeth Glaser Pediatric AIDS Foundation |
| Notes | Trial ID: NCT03023033 |
NCT03135288.
| Study name | Cell‐phone assisted postpartum counseling on the use of long‐acting reversible contraceptives. |
| Methods | Randomised controlled trial |
| Participants | Women that gave birth at > 28 weeks' gestation and desire birth spacing for > 1 year |
| Interventions | TCC: mobile phone assistance regarding postpartum family planning, including reminders and 2 follow‐up phone calls Control: usual care |
| Outcomes | Initiation of long acting reversible contraception method |
| Starting date | July 2017 |
| Contact information | Dr Ahmed Mohamed Abbas, Assiut University, Egypt |
| Notes | Trial ID: NCT03135288 |
NCT03332108.
| Study name | Novel approach to improving lactation support with mobile health technology. |
| Methods | Randomised controlled trial |
| Participants | Women having given birth with the intention to breastfeed |
| Interventions | TCC: EpxBreastfeeding, a phone, and text message‐based system that query patients via their personal phones and subsequently collect response data, allowing clinically relevant responses to trigger alerts to designated healthcare providers + baby book survey Control: baby book survey |
| Outcomes | 1. Exclusive breastfeeding duration; 2. Time to transition feeding status; 3. Time to reported problems with: latching, concern regarding deficiency in milk production, concern for inadequate child's weight gain; 4. Time from event to provider intervention; 5. Time to nursing status change; 6. Engagement; 7. Patient satisfaction with provider, service, and survey; 8. Breastfeeding status at 6 weeks postpartum and at 3 months postpartum; 9. Proportion of mothers exclusively breastfeeding at 6 months postpartum |
| Starting date | September 2017 |
| Contact information | Camaryn Chrisman Robbins, Washington University School of Medicine, Saint Louis, MO, USA |
| Notes | Trial ID: NCT03332108 |
NCT03355989.
| Study name | Evaluation of conditional cash transfers (CCTs) for immunization. |
| Methods | Randomised controlled trial |
| Participants | Carers of children aged 0–23 months visiting the Expanded Programme on Immunization Center for vaccination, residing within Korangi Town in Karachi, Pakistan |
| Interventions | TCC: SMS reminder Control: usual care Study includes 10 more study arms of SMS reminders with various combinations of different incentives and lotteries. |
| Outcomes | 1. Proportion of fully immunised children aged 2 years; 2. Penta3, Polio3, PCV3, or Measles1 coverage at 12–23 months; 3. Penta3, Polio3, PCV3, or Measles1 coverage at 12 months; 4. Proportion of fully immunised children at 12 months; 5. Proportion timely receipt of vaccine doses; 6. Immunisation system utilisation (dropout rate) |
| Starting date | November 2017 |
| Contact information | Aamir Khan and Subhash Chandir, Interactive Research and Development |
| Notes | Trial ID: NCT03355989 |
NCT03379467.
| Study name | Use of SMS and interactive reminders to improve timely immunisation coverage. |
| Methods | Randomised controlled trial |
| Participants | Carers of children presenting for pentavalent 1 vaccine residing in Korangi Town in Karachi, Pakistan |
| Interventions | TCC 1: SMS reminder TCC 2: interactive SMS reminder Control: usual care |
| Outcomes | 1. Measles; 2. Completion |
| Starting date | May 2011 |
| Contact information | Subhash Chandir, Interactive Research and Development |
| Notes | Trial ID: NCT03379467 |
NCT03399058.
| Study name | Innovative nutrition and mHealth Evidence Building Project. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Carers of underweight (weight for age z‐score < –1) children aged 6–23 months in Cambodia |
| Interventions | TCC 1: messages on child‐feeding practices TCC 2: messages on child‐feeding practices with follow‐up phone calls Control: usual care Co‐intervention: all participants receive the basic health and nutrition service package in Cambodia called 5+5+5 |
| Outcomes | 1. Change in prevalence of underweight children over time; 2. Change in mean of weight (grams) over time; 3. Change in percentage of carers correctly answering questions on child feeding, hygiene, health‐seeking, and caring practices over time; 4. Change in percentage of carers who have adopted proper child feeding, hygiene, health‐seeking, and caring practices; 5. Change in percentage of carers self‐reporting confidence in ability to adopt proper child feeding, hygiene, health‐seeking, and caring practices over time; 6. Percentage of siblings of enrolled children in each group with a weight for height z‐score < –2 |
| Starting date | November 2017 |
| Contact information | Oy Sreymom (sreymomoy@gmail.com); Chhea Chhorvann (cchhorvann@niph.org.kh) |
| Notes | Trial ID: NCT03399058 |
NCT03402646.
| Study name | Mobile phone reminders (and photovoice) for routine immunisation in Nigeria – the MOPING study. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Carers of healthy infants aged 0–12 months |
| Interventions | TCC: automated SMS and phone call reminders for routine immunisation Other: photovoice: participants will be shown photographs of debilitating consequences of non‐immunisation, which will form the basis of group discussions, knowledge sharing and consensus‐building sessions Control: usual care |
| Outcomes | 1. Immunisation coverage; 2. Timeliness of receipt of scheduled immunisation; 3. Incidence of any childhood vaccine‐preventable disease |
| Starting date | May 2018 |
| Contact information | Surajudeen A Abdulrahman (abdulsuraj@gmail.com) |
| Notes | Trial ID: NCT03402646 |
NCT03516682.
| Study name | Reducing delay in vaccination of children: logistic barriers (REDIVAC‐LB). |
| Methods | Randomised controlled trial |
| Participants | Parents of children aged < 11 months with missing recommended vaccinations currently enrolled at Kaiser Permanente Colorado |
| Interventions | TCC: automated vaccination reminders (text, phone, email, or a combination) Control: usual care |
| Outcomes | 1. Vaccines received; 2. Vaccine dose |
| Starting date | June 2018 |
| Contact information | Jason Glanz, Kaiser Permanente, Denver, CO |
| Notes | Trial ID: NCT03516682 |
NCT03705455.
| Study name | Immunization schedule alert platform: determining ISAP SMS efficacy in improving childhood immunization timeliness and completeness in Nigeria. |
| Methods | Randomised controlled trial |
| Participants | Carer with child due for birth dose vaccination or at 6 weeks |
| Interventions | TCC: text messages that provides immunisation schedule and vaccine availability at the nearest immunisation clinic Control: usual care |
| Outcomes | 1. Proportion of timely and complete vaccine uptake |
| Starting date | November 2018 |
| Contact information | Emmanuel Ihedioha (emmanuel.ihedioha@lifespanhcr.com) |
| Notes | Trial ID: NCT03705455 |
NCT03797950.
| Study name | Mobile nudges to increase early vaccination coverage in rural areas: a pilot investigation in Ghana's northern region. |
| Methods | Randomised controlled trial |
| Participants | Women who have given birth to a live‐born, surviving infant in the last 2 weeks |
| Interventions | TCC: voice reminder Other: cash incentive Control: usual care |
| Outcomes | 1. Full on time early vaccination coverage (OPV0 and BCG); 2. On time BCG coverage; 3. On time OPV coverage; 4. Birth documentation and reporting coverage |
| Starting date | November 2018 |
| Contact information | Guenther Fink (guenther.fink@swisstph.ch); Gillian Levine (gillian.levine@swisstph.ch) |
| Notes | Trial ID: NCT03797950 |
NCT03890978.
| Study name | Improving exclusive breastfeeding via mobile phone text messages: a randomized controlled trial in southern Jordan. |
| Methods | Randomised controlled trial |
| Participants | Women who had an uncomplicated singleton pregnancy and express interest in breastfeeding |
| Interventions | TCC: promotional exclusive breastfeeding text messages will be sent to women via mobile phone Non‐TCC: child healthcare‐related text messages (except breastfeeding messages) will be sent to women via mobile phone |
| Outcomes | 1. Rate of exclusive breastfeeding; 2. Median duration of exclusive breastfeeding; 3. Rates of early initiation of breastfeeding |
| Starting date | January 2018 |
| Contact information | Reham M Khresheh, Mutah University, Jordan |
| Notes | Trial ID: NCT03890978 |
Odeny 2018.
| Study name | Maximizing adherence and retention for women living with HIV and their infants in Kenya (MOTIVATE! study). |
| Methods | 2 × 2 factorial cluster‐randomised controlled trial |
| Participants | HIV‐infected pregnant women and their HIV‐exposed infants attending antenatal care clinic at 1 of the study sites in Migori, Kisumu, and Homa Bay, Kenya |
| Interventions | TCC: mobile phone text messaging intervention TCC 2: mobile phone text messaging intervention + community mentor mother home visits TCC 3: community mentor mother home visits Control: usual care |
| Outcomes | 1. Self‐reported adherence on antiretroviral therapy; 2. Retention in care; 3. Maternal CD4 count change; 4. Uptake of intervention services; 5. Mother‐to‐child‐transmission; 6. Male partner involvement |
| Starting date | May 2014 |
| Contact information | Thomas A Odeny (taodeny@gmail.com) |
| Notes | Trial ID: NCT02491177 |
PACTR201703002093382.
| Study name | Effect of enhanced reminders on postnatal clinic attendance in Addis Ababa: a cluster randomized control trial. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Women who gave birth during the study period in public health centres in Ibadan, Ethiopia |
| Interventions | TCC: SMS or voice call appointment reminders Control: usual care |
| Outcomes | 1. Number of postnatal visits; 2. Acceptability |
| Starting date | June 2017 |
| Contact information | Abraham Sahilemichael Kebede (abrishya@yahoo.com) |
| Notes | Trial ID: PACTR201703002093382 |
PACTR201711002737120.
| Study name | Zinc adherence: a follow‐up study of under‐fives with acute watery diarrhoea using mobile phones: a randomised controlled trial. |
| Methods | Randomised controlled trial |
| Participants | Parents of children aged < 5 years with acute watery diarrhoea recruited from a health centre in Dar es Salaam, Tanzania |
| Interventions | TCC: voice calls and text messages Control: usual care |
| Outcomes | 1. 10‐day adherence to zinc sulphate prescribed; 2. Clinic attendance for follow‐up visit; 3. Acceptability of mHealth; 4. Dependability of mHealth |
| Starting date | December 2016 |
| Contact information | Fatimah Zahra Karim (fzahrakarim@gmail.com) |
| Notes | Trial ID: PACTR201711002737120 |
PACTR201801002231314.
| Study name | Utilization of short message service to enhance uptake of focused ante‐natal care among women in Tharaka Nithi County, Kenya. |
| Methods | Randomised controlled trial |
| Participants | Pregnant women attending rural health centres in Kenya |
| Interventions | TCC: SMS reminder to attend antenatal clinic Non‐digital TCC: date reminder in a book to attend antenatal clinic |
| Outcomes | 1. Enhance uptake of focused antenatal care; 2. Skilled birth attendance at birth; 3. Postnatal care at 2 weeks |
| Starting date | January 2016 |
| Contact information | Eliphas Gitonga (gitonga.eliphas@ku.ac.ke) |
| Notes | Trial ID; PACTR201801002231314 |
PACTR201806003369302.
| Study name | Efficacy of text messages, voice calls and community visits on developmental milestones of children from teenage pregnancies: a randomized intervention trial. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Teenage mother, aged < 20 years with a child aged < 3 months |
| Interventions | TCC 1: 1 voice call weekly, 3 text messages every week TCC 2: 3 messages every week TCC 3: messages to participants' phones, 1 voice call every week and visits by a community health volunteer every month Control: usual care |
| Outcomes | 1. Head circumference as a marker for overall brain development (6 and 12 months); 2. Diarrhoea incidence, wasting, stunting, motor and language milestones (6 and 12 months) |
| Starting date | April 2019 |
| Contact information | Valerian Mwenda (valmwenda@gmail.com) |
| Notes | Trial ID: PACTR201806003369302 |
Rossing 2016.
| Study name | mHealth to improve measles immunization in Guinea‐Bissau. |
| Methods | Randomised controlled trial |
| Participants | Mothers of children receiving measles vaccination in the Republic of Guinea‐Bissau |
| Interventions | TCC 1: scheduled SMS reminder of the measles vaccination TCC 2: scheduled SMS reminder + voice call reminder of the measles vaccination Control: usual care |
| Outcomes | 1. Measles vaccination coverage and timeliness when children reach 12 months of age; 2. Mean number of health centre visits (with intention to obtain the measles vaccination) required before successful administration |
| Starting date | March 2016 |
| Contact information | Emil Rossing (emro@ssi.dk) |
| Notes | NCT02662595 |
Salam 2018.
| Study name | Saving lives with better gestational age estimation: improving the accuracy of recall and reporting of the date of last menstrual period (LMP) in Rural Bangladesh. |
| Methods | Cluster‐randomised controlled trial |
| Participants | 3360 adolescent girls and recently married women with no or a single child selected from the Demographic surveillance system database in Mirzapur subdistrict of Tangail district, Bangladesh |
| Interventions | TCC 1: counselling and a mobile phone‐based SMS alert system TCC 2: counselling and smart‐phone application TCC 3: counselling and a paper‐based calendar Control: usual care |
| Outcomes | Accuracy and certainty of last menstrual period – recall dates |
| Starting date | January 2017 |
| Contact information | Shumona Sharmin Salam (shumona@icddrb.org) |
| Notes | Trial ID: NCT02944747 |
Tobe 2018.
| Study name | Mobile‐health tool to improve maternal and neonatal health care in Bangladesh. |
| Methods | Cluster‐randomised controlled trial |
| Participants | Pregnant women in Lohagora of Narail District and Dhamrai of Dhaka District, Bangladesh |
| Interventions | TCC: mobile short messaging and audio system Control: usual care |
| Outcomes | 1. Neonatal mortality; 2. Maternal mortality; 3. Stillbirth; 4. Miscarriage; 5. Preterm birth; 6. Low birth weight; 7. Maternal morbidities; 8. Frequency of antenatal care visits; 9. Accessibility to skilled birth attendants for delivery; 10. Referral for identified complications; 11. Utilisation of postpartum care; 12. Status of initiating breastfeeding |
| Starting date | February 2017 |
| Contact information | Ruoyan Gai Tobe (gai‐r@ncchd.go.jp); Syed Emdadul Haque (emdad91@gmail.com) |
| Notes | Trial ID: UMIN000025628 |
BCG: Bacillus Calmette‐Guérin; OPV: oral polio vaccine; SMS: short message service; TCC: targeted client communication.
Differences between protocol and review
In the protocol, we specified that the 'Summary of findings' tables for pregnant and postpartum populations would include the following outcomes: maternal morbidity and mortality combined; neonatal morbidity and mortality combined; initiation of breastfeeding; attendance for antenatal care; birth in a health facility; and unintended consequences (Palmer 2018a). In conducting the review, we decided to include any measure of breastfeeding, instead of only including initiation of breastfeeding, and any measure of access to intrapartum care, thereby including births in a health facility and births occurring with a skilled attendant present.
We had planned that when a study reported the same outcome measure for multiple time points of follow‐up, we would extract data from all time points. However, in the review, we extracted data for the outcome at the longest follow‐up point.
For the purpose of pooling data, we planned to categorise lengths of follow‐up as follows: short‐term follow‐up: three months or less; moderate‐term follow‐up: three to 12 months; long‐term follow‐up: greater than 12 months. However, given the limited number of studies with the same aim, comparison, and outcome measure that could we pooled, we decided to pool across different lengths of follow‐up.
We planned to carry out the following subgroup analyses for the objective outcomes of health status: income region (by World Bank income group) (World Bank 2017); and delivery mechanisms (i.e. mobile phone messaging only, mobile applications only, combined mobile phone messaging and applications, combined application, and other). However, there were an insufficient number of studies reporting the same objective health status outcomes to conduct these subgroup analyses.
We planned to carry out the following sensitivity analyses: only including studies with low risk of bias on the sequence generation, allocation concealment, and incomplete outcome data domains; and only including studies with objectively measured outcomes. However, there were insufficient studies to conduct the second specified sensitivity analyses.
As part of the risk of bias assessments of included studies, we also reported an assessment of 'Other bias'. Under this domain, we considered other potential sources of bias such as the presence of baseline imbalances related to the outcome under study, and evidence of contamination.
In the protocol, we stated we would not pool studies with substantial heterogeneity in meta‐analyses. However, some of the pooled analyses do exhibit substantial statistical heterogeneity. We intended to explore possible reasons for variability by conducting our prespecified subgroup analysis; however, there was an insufficient number of studies in the pooled analyses to conduct meaningful subgroup analyses. Where we noted other potential explanations for high heterogeneity (e.g. differing baseline level of risk), and there were a sufficient number of studies, subgroup analyses were conducted to examine these.
Contributions of authors
Conceiving the protocol: CG, TT, SL, GM.
Designing the protocol: CG, TT, SL, GM, MP, CF, NH.
Designing search strategies: JE, CF, MP.
Writing the protocol: MP, CF, TT.
Providing general advice on the protocol: CG, SL, GV, NH, NM, HB, MF.
Securing funding for the protocol and review: GM, TT, SL, CG, CF.
Data collection for the review: NH, GV, NM, HB, MP.
Data management for the review: NH, GV, NM, HB, MP.
Analysis of data: NH, GV, NM, HB, MP.
Interpretation of data: MP, CF, GC, TT SL.
Writing the review: MP, CF, CG.
Providing general advice on the review: CG, SL, GV, NH, NM, HB, MF.
Sources of support
Internal sources
No sources of support supplied
External sources
-
World Health Organization, Switzerland
This work, including the open access publication costs, was funded by the UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a co‐sponsored program executed by the World Health Organization (WHO).
Declarations of interest
MP: was contracted by the World Health Organization (WHO) to produce this review.
NH: is employed by Cochrane Response, an evidence services unit operated by Cochrane. The WHO contacted Cochrane Response to produce this review.
HB: is employed by Cochrane Response, an evidence services unit operated by Cochrane. The WHO contacted Cochrane Response to produce this review.
GV: is employed by Cochrane Response, an evidence services unit operated by Cochrane. The WHO contacted Cochrane Response to produce this review.
NM: previously worked for Enhanced Reviews Ltd, a company that conducts systematic reviews mostly for the public sector. NM is employed by Cochrane Response, an evidence services unit operated by Cochrane. The WHO contacted Cochrane Response to produce this review.
TT: none known.
GM: owns stock in Apple Computer.
CG: none known.
SL: is the Joint Co‐ordinating Editor for the Cochrane Effective Practice and Organisation of Care Review Group.
MF: none known.
CF: was contracted by the WHO to produce this review.
New
References
References to studies included in this review
Ahlers‐Schmidt 2012 {published data only}
- Ahlers-Schmidt CR, Chesser AK, Nguyen T, Brannon J, Hart TA, Williams KS, et al. Feasibility of a randomized controlled trial to evaluate Text Reminders for Immunization Compliance in Kids (TRICKs). Vaccine 2012;30(36):5305-9. [DOI] [PubMed] [Google Scholar]
Bangure 2015 {published data only}
- Bangure D, Chirundu D, Gombe N, Marufu T, Mandozana G, Tshimanga M, et al. Effectiveness of short message services reminder on childhood immunization programme in Kadoma, Zimbabwe – a randomized controlled trial, 2013. BMC Public Health 2015;15:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bigna 2015 {published data only}
- Bigna JJ, Noubiap JJ, Kouanfack C, Plottel CS, Koulla-Shiro S. Effect of mobile phone reminders on follow-up medical care of children exposed to or infected with HIV in Cameroon (MORE CARE): a multicentre, single-blind, factorial, randomised controlled trial. Lancet Infectious Diseases 2014;14(7):600-8. [DOI] [PubMed] [Google Scholar]
- Bigna JJ, Noubiap JJ, Plottel CS, Kouanfack C, Koulla-Shiro S. Barriers to the implementation of mobile phone reminders in pediatric HIV care: a pre-trial analysis of the Cameroonian MORE CARE study. BMC Health Services Research 2014;14:523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigna JJ, Noubiap JJ, Plottel CS, Kouanfack C, Koulla-Shiro S. Factors associated with non-adherence to scheduled medical follow-up appointments among Cameroonian children requiring HIV care: a case-control analysis of the usual-care group in the MORE CARE trial. Infectious Diseases of Poverty 2014;3(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Bigna JJ. Automated text message reminders to promote good health. Lancet Infectious Diseases 2015;15(1):19-20. [DOI] [PubMed] [Google Scholar]
- Mbuagbaw L. Mobile phone reminders for paediatric HIV follow-up care. Lancet Infectious Diseases 2014;14(7):540-1. [DOI] [PubMed] [Google Scholar]
Brown 2016 {published data only}
- Brown VB, Oluwatosin OA, Akinyemi JO, Adeyemo AA. Effects of community health nurse-led intervention on childhood routine immunization completion in primary health care centers in Ibadan, Nigeria. Journal of Community Health 2016;41(2):265-73. [DOI] [PubMed] [Google Scholar]
Domek 2016 {published data only}
- Domek GJ, Contreras-Roldan IL, O'Leary ST, Bull S, Furniss A, Kempe A, et al. SMS text message reminders to improve infant vaccination coverage in Guatemala: a pilot randomized controlled trial. Vaccine 2016;34(21):2437-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Evans 2014 {published data only}
- Evans WD, Wallace B, Szekely D, Nielsen P, Murray E, Abroms L, et al. Initial outcomes from a 4-week follow-up study of the text4baby program in the military women's population: randomized controlled trial. Journal of Medical Internet Research 2014;16(5):e131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eze 2015 {published data only}
- Eze GU, Adeleye OO. Enhancing routine immunization performance using innovative technology in an urban area of Nigeria. West African Journal of Medicine 2015;34(1):3-10. [PubMed] [Google Scholar]
Gibson 2017 {published data only}
- Gibson DG, Ochieng B, Kagucia EW, Were J, Hayford K, Moulton LH, et al. Mobile phone-delivered reminders and incentives to improve childhood immunisation coverage and timeliness in Kenya (M-SIMU): a cluster randomised controlled trial. Lancet Global Health 2017;5(4):e428-e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haji 2016 {published data only}
- Haji A, Lowther S, Ngan'ga Z, Gura Z, Tabu C, Sandhu H, et al. Reducing routine vaccination dropout rates: evaluating two interventions in three Kenyan districts, 2014. BMC Public Health 2016;16:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hannan 2016 {published data only}
- Hannan J, Brooten D, Page T, Galindo A, Torres M. Low-income first-time mothers: effects of APN follow-up using mobile technology on maternal and infant outcomes. Global Pediatric Health 2016;3:2333794X16660234. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hofstetter 2015a {published data only}
- Hofstetter AM, DuRivage N, Vargas CY, Camargo S, Vawdrey DK, Fisher A, et al. Text message reminders for timely routine MMR vaccination: a randomized controlled trial. Vaccine 2015;33(43):5741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jareethum 2008 {published data only}
- Jareethum R, Titapant V, Chantra T, Sommai V, Chuenwattana P, Jirawan C. Satisfaction of healthy pregnant women receiving short message service via mobile phone for prenatal support: a randomized controlled trial. Journal of the Medical Association of Thailand 2008;91(4):458-63. [PubMed] [Google Scholar]
Joshi 2015 {published data only}
- Joshi S, Patil N, Hegde A. Impact of mHealth initiative on utilization of antenatal care services in rural Maharashtra, India. Indian Journal of Maternal and Child Health 2015;17(2):1-7. [Google Scholar]
Kamau‐Mbuthia 2013 {published data only}
- *.Kamau-Mbuthia E, Mbugua S, Webb G, Kalungu S, Sarange C, Lou W, et al. Cell phone based peer counseling to support exclusive breastfeeding is associated with more frequent help and decreased breastfeeding problems. Annals of Nutrition & Metabolism 2013;63:196-7. [Google Scholar]
- Webb G, Kamau-Mbuthia E, Mbugua S, Kalungu S, Sarange C, Lou W, et al. Infant medication, illness and growth in a randomized controlled trial of exclusive breastfeeding support in Kenya. Annals of Nutrition & Metabolism 2013;63:752. [Google Scholar]
Kassaye 2016 {published data only}
- Kassaye SG, Ong'ech J, Sirengo M, Kose J, Matu L, McOdida P, et al. Cluster-randomized controlled study of SMS text messages for prevention of mother-to-child transmission of HIV in rural Kenya. AIDS Research & Treatment 2016;2016:1289328. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kebaya 2014 {published data only}
- *.Kebaya L, Nduati R, Wamalwa D, Kariuki N, Bashir A. Efficacy of mobile phone use on adherence to nevirapine prophylaxis and retention in care among the HIV-exposed infants in PMTCT: a randomised controlled trial. Archives of Disease in Childhood 2014;99:A329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kebaya LM, Wamalwa D, Kariuki N, Admani B, Nduati RW. Efficacy of mobile phone use on adherence to nevirapine prophylaxis and retention in care among HIV-exposed infants. Topics in Antiviral Medicine 2015;23:407. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lund 2012 {published data only}
- *.Lund S, Hemed M, Nielsen BB, Said A, Said K, Makungu MH, et al. Mobile phones as a health communication tool to improve skilled attendance at delivery in Zanzibar: a cluster-randomised controlled trial. BJOG 2012;119(10):1256-64. [DOI] [PubMed] [Google Scholar]
- Lund S, Nielsen BB, Hemed M, Boas IM, Said A, Said K, et al. Mobile phones improve antenatal care attendance in Zanzibar: a cluster randomized controlled trial. BMC Pregnancy & Childbirth 2014;14:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund S, Nielsen BB, Hemed M, Said A, Said K, Makungu MH, et al. Mobile phones as a health communication tool to improve maternal and perinatal health in Zanzibar: a cluster randomised controlled trial. Tropical Medicine & International Health 2013;18:22. [DOI] [PubMed] [Google Scholar]
- Lund S, Rasch V, Hemed M, Boas IM, Said A, Said K, et al. Mobile phone intervention reduces perinatal mortality in Zanzibar: secondary outcomes of a cluster randomized controlled trial. JMIR mHealth and uHealth 2014;2(1):e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maslowsky 2016 {published data only}
- Maslowsky J, Frost S, Hendrick CE, Trujillo Cruz FO, Merajver SD. Effects of postpartum mobile phone-based education on maternal and infant health in Ecuador. International Journal of Gynaecology & Obstetrics 2016;134(1):93-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
McConnell 2016 {published data only}
- McConnell M, Ettenger A, Rothschild CW, Muigai F, Cohen J. Can a community health worker administered postnatal checklist increase health-seeking behaviors and knowledge?: evidence from a randomized trial with a private maternity facility in Kiambu County, Kenya. BMC Pregnancy Childbirth 2016;16(1):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moniz 2013 {published data only}
- Moniz MH, Hasley S, Meyn LA, Beigi RH. Improving influenza vaccination rates in pregnancy through text messaging: a randomized controlled trial. Obstetrics & Gynecology 2013;121(4):734-40. [DOI] [PubMed] [Google Scholar]
Naughton 2017 {published data only}
- Cooper S, Foster K, Naughton F, Leonardi-Bee J, Sutton S, Ussher M, et al. Pilot study to evaluate a tailored text message intervention for pregnant smokers (MiQuit): study protocol for a randomised controlled trial. Trials 2015;16:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Naughton F, Cooper S, Foster K, Emery J, Leonardi-Bee J, Sutton S, et al. Large multi-centre pilot randomized controlled trial testing a low-cost, tailored, self-help smoking cessation text message intervention for pregnant smokers (MiQuit). Addiction 2017;112(7):1238-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niederhauser 2015 {published data only}
- Niederhauser V, Johnson M, Tavakoli AS. Vaccines4Kids: assessing the impact of text message reminders on immunization rates in infants. Vaccine 2015;33(26):2984-9. [DOI] [PubMed] [Google Scholar]
Odeny 2014 {published data only}
- Odeny TA, Bukusi EA, Cohen CR, Yuhas K, Camlin CS, McClelland RS. Texting improves testing: a randomized trial of two-way SMS to increase postpartum prevention of mother-to-child transmission retention and infant HIV testing. AIDS 2014;28(15):2307-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Omole 2018 {published data only}
- Omole O, Ijadunola MY, Olotu E, Omotoso O, Bello B, Awoniran O, et al. The effect of mobile phone short message service on maternal health in south-west Nigeria. International Journal of Health Planning and Management 2018;33(1):155-70. [DOI] [PubMed] [Google Scholar]
Sharma 2011 {published data only}
- Sharma R, Hebbal M, Ankola AV, Murugabupathy V. Mobile-phone text messaging (SMS) for providing oral health education to mothers of preschool children in Belgaum City. Journal of Telemedicine & Telecare 2011;17(8):432-6. [DOI] [PubMed] [Google Scholar]
Stockwell 2015 {published data only}
- Stockwell MS, Hofstetter AM, DuRivage N, Barrett A, Fernandez N, Vargas CY, et al. Text message reminders for second dose of influenza vaccine: a randomized controlled trial. Pediatrics 2015;135(1):e83-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yudin 2017 {published data only}
- Yudin MH, Mistry N, De Souza LR, Besel K, Patel V, Blanco Mejia S, et al. Text messages for influenza vaccination among pregnant women: a randomized controlled trial. Vaccine 2017;35(5):842-8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Atukunda 2017 {published data only}
- Atukunda EC, Musiimenta A, Musinguzi N, Wyatt MA, Ashaba J, Ware NC, et al. Understanding patterns of social support and their relationship to an ART adherence intervention among adults in rural Southwestern Uganda. AIDS and Behavior 2017;21(2):428-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bracken 2014 {published data only}
- Bracken H, Lohr PA, Taylor J, Morroni C, Winikoff B. RU OK? The acceptability and feasibility of remote technologies for follow-up after early medical abortion. Contraception 2014;90(1):29-35. [DOI] [PubMed] [Google Scholar]
Broberg 2013 {published data only}
- Broberg G, Jonasson JM, Ellis J, Gyrd-Hansen D, Anjemark B, Glantz A, et al. Increasing participation in cervical cancer screening: telephone contact with long-term non-attendees in Sweden. Results from RACOMIP, a randomized controlled trial. International Journal of Cancer 2013;133(1):164-71. [DOI] [PubMed] [Google Scholar]
Carlsen 2013 {published data only}
- Carlsen EM, Kyhnaeb A, Renault KM, Cortes D, Michaelsen KF, Pryds O. Telephone-based support prolongs breastfeeding duration in obese women: a randomized trial. American Journal of Clinical Nutrition 2013;98(5):1226-32. [DOI] [PubMed] [Google Scholar]
Collier 2005 {published data only}
- Collier AC, Ribaudo H, Mukherjee AL, Feinberg J, Fischl MA, Chesney M, et al. A randomized study of serial telephone call support to increase adherence and thereby improve virologic outcome in persons initiating antiretroviral therapy. Journal of Infectious Diseases 2005;192(8):1398-406. [DOI] [PubMed] [Google Scholar]
Gallegos 2014 {published data only}
- Gallegos D, Russell-Bennett R, Previte J, Parkinson J. Can a text message a week improve breastfeeding? BMC Pregnancy and Childbirth 2014;14(1):374. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haberer 2016 {published data only}
- Haberer JE, Musiimenta A, Atukunda EC, Musinguzi N, Wyatt MA, Ware NC, et al. Short message service (SMS) reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS 2016;30(8):1295-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hashemian 2015 {published data only}
- Hashemian TS, Kritz-Silverstein D, Baker R. Text2floss: the feasibility and acceptability of a text messaging intervention to improve oral health behavior and knowledge. Journal of Public Health Dentistry 2015;75(1):34-41. [DOI] [PubMed] [Google Scholar]
Herring 2016 {published data only}
- Herring SJ, Cruice JF, Bennett GG, Rose MZ, Davey A, Foster GD. Preventing excessive gestational weight gain among African American women: a randomized clinical trial. Obesity 2016;24(1):30-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hofstetter 2015b {published data only}
- Hofstetter AM, Vargas CY, Camargo S, Holleran S, Vawdrey DK, Kharbanda EO, et al. Impacting delayed pediatric influenza vaccination: a randomized controlled trial of text message reminders. American Journal of Preventive Medicine 2015;48(4):392-401. [DOI] [PubMed] [Google Scholar]
Irons 2015 {published data only}
- Irons M, Tomaszewski K, Buchanan CR, Trent M. Understanding adolescent nonresponsiveness to text messages: lessons from the Depotext trial. Journal of Urban Health 2015;92(3):502-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jimenez 2017 {published data only}
- Jimenez ME, DuRivage NE, Bezpalko O, Suh A, Wade R, Blum NJ, et al. A pilot randomized trial of a video patient decision aid to facilitate early intervention referrals from primary care. Clinical Pediatrics 2017;56(3):268-77. [DOI] [PubMed] [Google Scholar]
Kofinas 2014 {published data only}
- Kofinas JD, Varrey A, Sapra KJ, Kanj RV, Chervenak FA, Asfaw T. Adjunctive social media for more effective contraceptive counseling: a randomized controlled trial. Obstetrics & Gynecology 2014;123(4):763-70. [DOI] [PubMed] [Google Scholar]
Lau 2013 {published data only}
- Lau JT, Tsui HY, Lau MM. A pilot clustered randomized control trial evaluating the efficacy of a network-based HIV peer-education intervention targeting men who have sex with men in Hong Kong, China. AIDS Care 2013;25(7):812-9. [DOI] [PubMed] [Google Scholar]
Lau 2014 {published data only}
- Lau YK, Cassidy T, Hacking D, Brittain K, Haricharan HJ, Heap M. Antenatal health promotion via short message service at a midwife obstetrics unit in South Africa: a mixed methods study. BMC Pregnancy and Childbirth 2014;14(1):284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewis 2012 {published data only}
- Lewis BA, Gjerdingen DK, Avery MD, Guo H, Sirard JR, Bonikowske AR, et al. Examination of a telephone-based exercise intervention for the prevention of postpartum depression: design, methodology, and baseline data from the healthy mom study. Contemporary Clinical Trials 2012;33(6):1150-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maduka 2013 {published data only}
- Maduka O, Tobin-West CI. Adherence counseling and reminder text messages improve uptake of antiretroviral therapy in a tertiary hospital in Nigeria. Nigerian Journal of Clinical Practice 2013;16(3):302-8. [DOI] [PubMed] [Google Scholar]
Mauriello 2016 {published data only}
- Mauriello LM, Van Marter DF, Umanzor CD, Castle PH, Aguiar EL. Using mHealth to deliver behavior change interventions within prenatal care at community health centers. American Journal of Health Promotion 2016;30(7):554-62. [DOI] [PubMed] [Google Scholar]
Milani 2015 {published data only}
- Milani HS, Azargashb E, Beyraghi N, Defaie S, Asbaghi T. Effect of telephone-based support on postpartum depression: a randomized controlled trial. International Journal of Fertility & Sterility 2015;9(2):247-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 2013 {published data only}
- Moore DJ, Montoya JL, Blackstone K, Rooney A, Gouaux B, Georges S, et al. Preliminary evidence for feasibility, use, and acceptability of individualized texting for adherence building for antiretroviral adherence and substance use assessment among HIV-infected methamphetamine users. AIDS Research and Treatment 2013;2013:585143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 2015 {published data only}
- Moore DJ, Poquette A, Casaletto KB, Gouaux B, Montoya JL, Posada C, et al. Individualized texting for adherence building (iTAB): improving antiretroviral dose timing among HIV-infected persons with co-occurring bipolar disorder. AIDS and Behavior 2015;19(3):459-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murthy 2019 {published data only}
- Murthy N, Chandrasekharan S, Prakash MP, Kaonga NN, Peter J, Ganju A, et al. The impact of an mHealth voice message service (mMitra) on infant care knowledge, and practices among low-income women in India: findings from a pseudo-randomized controlled trial. Maternal Child Health Journal 2019;23(12):1658-69. [DOI] [PMC free article] [PubMed]
Mwapasa 2017 {published data only}
- Mwapasa V, Joseph J, Tchereni T, Jousset A, Gunda A. Impact of mother–infant pair clinics and short-text messaging service (SMS) reminders on retention of HIV-infected women and HIV-exposed infants in eMTCT care in Malawi: a cluster randomized trial. Journal of Acquired Immune Deficiency Syndromes 2017;75:S123-31. [DOI] [PubMed] [Google Scholar]
Oakley‐Girvan 2016 {published data only}
- Oakley-Girvan I, Londono C, Canchola A, Watkins Davis S. Text messaging may improve abnormal mammogram follow-up in Latinas. Oncology Nursing Forum 2016;43(1):36-43. [DOI] [PubMed] [Google Scholar]
Patel 2014 {published data only}
- Patel A, Stern L, Unger Z, Debevec E, Roston A, Hanover R, et al. Staying on track: a cluster randomized controlled trial of automated reminders aimed at increasing human papillomavirus vaccine completion. Vaccine 2014;32(21):2428-33. [DOI] [PubMed] [Google Scholar]
Peitzmeier 2016 {published data only}
- Peitzmeier SM, Khullar K, Potter J. Effectiveness of four outreach modalities to patients overdue for cervical cancer screening in the primary care setting: a randomized trial. Cancer Causes & Control 2016;27(9):1081-91. [DOI] [PubMed] [Google Scholar]
Pérez‐Ferre 2010 {published data only}
- Pérez-Ferre N, Galindo M, Fernández MD, Velasco V, Runkle I, la Cruz MJ, et al. The outcomes of gestational diabetes mellitus after a telecare approach are not inferior to traditional outpatient clinic visits. International Journal of Endocrinology 2010;2010:386941. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pollak 2014 {published data only}
- Pollak KI, Alexander SC, Bennett G, Lyna P, Coffman CJ, Bilheimer A, et al. Weight-related SMS texts promoting appropriate pregnancy weight gain: a pilot study. Patient Education and Counseling 2014;97(2):256-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prieto 2016 {published data only}
- Prieto JT, Zuleta C, Rodríguez JT. Modeling and testing maternal and newborn care mHealth interventions: a pilot impact evaluation and follow-up qualitative study in Guatemala. Journal of the American Medical Informatics Association 2016;24(2):352-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rampersaud 2016 {published data only}
- Rampersaud GC, Sokolow A, Gruspe A, Colee JC, Kauwell GP. Folate/folic acid knowledge, intake, and self-efficacy of college-aged women: impact of text messaging and availability of a folic acid-containing supplement. Journal of American College Health 2016;64(6):460-8. [DOI] [PubMed] [Google Scholar]
Rand 2015 {published data only}
- Rand CM, Brill H, Albertin C, Humiston SG, Schaffer S, Shone LP, et al. Effectiveness of centralized text message reminders on human papillomavirus immunization coverage for publicly insured adolescents. Journal of Adolescent Health 2015;56(5):S17-20. [DOI] [PubMed] [Google Scholar]
Rand 2017 {published data only}
- Rand CM, Vincelli P, Goldstein NP, Blumkin A, Szilagyi PG. Effects of phone and text message reminders on completion of the human papillomavirus vaccine series. Journal of Adolescent Health 2017;60(1):113-9. [DOI] [PubMed] [Google Scholar]
Reeder 2014 {published data only}
- Reeder JA, Joyce T, Sibley K, Arnold D, Altindag O. Telephone peer counseling of breastfeeding among WIC participants: a randomized controlled trial. Pediatrics 2014;134(3):e700. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reid 2014 {published data only}
- Reid MJ, Dhar SI, Cary M, Liang P, Thompson J, Gabaitiri L, et al. Opinions and attitudes of participants in a randomized controlled trial examining the efficacy of SMS reminders to enhance antiretroviral adherence: a cross-sectional survey. Journal of Acquired Immune Deficiency Syndromes 2014;65(2):e86-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Richman 2016 {published data only}
- Richman AR, Maddy L, Torres E, Goldberg EJ. A randomized intervention study to evaluate whether electronic messaging can increase human papillomavirus vaccine completion and knowledge among college students. Journal of American College Health 2016;64(4):269-78. [DOI] [PubMed] [Google Scholar]
Robbins 2013 {published data only}
- Robbins GK, Testa MA, Su M, Safren SA, Morse G, Lammert S, et al. Site nurse-initiated adherence and symptom support telephone calls for HIV-positive individuals starting antiretroviral therapy, ACTG 5031: substudy of ACTG 384. HIV Clinical Trials 2013;14(5):235-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sridhar 2013 {published data only}
- Sridhar A, Chen A, Glik D. Plan a birth control: randomized controlled trial of a mobile health application. Contraception 2013;88(3):463. [Google Scholar]
Sridhar 2014 {published data only}
- Sridhar A, Chen AY. Mobile health application for long-acting reversible contraceptive information: a secondary analysis. Obstetrics & Gynecology 2014;123:111S. [Google Scholar]
Stern 2013 {published data only}
- Stern L, Unger Z, Debevec E, Ginde S, Morfesis J, Patel A. Staying on track: a cluster randomized controlled trial of automated reminders for HPV vaccine series completion. Contraception 2013;88(3):438-9. [DOI] [PubMed] [Google Scholar]
Stockwell 2012 {published data only}
- Stockwell MS, Kharbanda EO, Martinez RA, Vargas CY, Vawdrey DK, Camargo S. Effect of a text messaging intervention on influenza vaccination in an urban, low-income pediatric and adolescent population: a randomized controlled trial. Journal of the American Medical Association 2012;307(16):1702-8. [DOI] [PubMed] [Google Scholar]
Szilagyi 2013 {published data only}
- Szilagyi PG, Albertin C, Humiston SG, Rand CM, Schaffer S, Brill H, et al. A randomized trial of the effect of centralized reminder/recall on immunizations and preventive care visits for adolescents. Academic Pediatrics 2013;13(3):204-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Takeuchi 2016 {published data only}
- Takeuchi S, Horiuchi S. Randomised controlled trial using smartphone website vs leaflet to support antenatal perineal massage practice for pregnant women. Women and Birth 2016;29(5):430-5. [DOI] [PubMed] [Google Scholar]
Tarrant 2014 {published data only}
- Tarrant AM, Fong DY, Heys M, Lee IL, Sham A, Hui Choi WH. Professional breastfeeding support to increase the exclusivity and duration of breastfeeding: a randomised controlled trial. Hong Kong Medical Journal 2014;20:34. [PubMed] [Google Scholar]
Trent 2013 {published data only}
- Trent M, Tomaszewski K. Family planning appointment attendance among urban youth: results from the Depotext trial. Journal of Adolescent Health 2013;52(2):S88. [Google Scholar]
Trent 2015 {published data only}
- Trent M, Thompson C, Tomaszewski K. Text messaging support for urban adolescents and young adults using injectable contraception: outcomes of the DepoText pilot trial. Journal of Adolescent Health 2015;57(1):100-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Ryswyk 2015 {published data only}
- Van Ryswyk EM, Middleton PF, Hague WM, Crowther CA. Postpartum SMS reminders to women who have experienced gestational diabetes to test for type 2 diabetes: the DIAMIND randomized trial. Diabetic Medicine 2015;32(10):1368-76. [DOI] [PubMed] [Google Scholar]
Wright 2012 {published data only}
- Wright A, Poon EG, Wald J, Feblowitz J, Pang JE, Schnipper JL, et al. Randomized controlled trial of health maintenance reminders provided directly to patients through an electronic PHR. Journal of General Internal Medicine 2012;27(1):85-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2013 {published data only}
- Young SD, Cumberland WG, Lee SJ, Jaganath D, Szekeres G, Coates T. Social networking technologies as an emerging tool for HIV prevention: a cluster randomized trial. Annals of Internal Medicine 2013;159(5):318-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2014 {published data only}
- Young SD, Holloway I, Jaganath D, Rice E, Westmoreland D, Coates T. Project HOPE: online social network changes in an HIV prevention randomized controlled trial for African American and Latino men who have sex with men. American Journal of Public Health 2014;104(9):1707-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Abroms 2017a {published data only}
- Abroms LC, Johnson PR, Leavitt LE, Cleary SD, Bushar J, Brandon TH, et al. A randomized trial of text messaging for smoking cessation in pregnant women. American Journal of Preventive Medicine 2017;53(6):781-90. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Abroms 2017b {published data only}
- Abroms LC, Chiang S, Macherelli L, Leavitt L, Montgomery M. Assessing the National Cancer Institute's smokefreeMOM text-messaging program for pregnant smokers: pilot randomized trial. Journal of Medical Internet Research 2017;19(10):e333. [DOI] [PMC free article] [PubMed] [Google Scholar]
Altazan 2019 {published data only}
- Altazan AD, Redman LM, Burton JH, Beyl RA, Cain LE, Sutton EF, et al. Mood and quality of life changes in pregnancy and postpartum and the effect of a behavioral intervention targeting excess gestational weight gain in women with overweight and obesity: a parallel-arm randomized controlled pilot trial. BMC Pregnancy and Childbirth 2019;19(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bangal 2018 {published data only}
- Bangal V, Somasundaram KV, Thitame S. Influence of mobile communication on utilization and outcome of maternal health services in rural area. Indian Journal of Public Health Research & Development 2018;9(5):504-8. [Google Scholar]
Domek 2019 {published data only}
- Domek GJ, Contreras-Roldan IL, Bull S, O'Leary ST, Bolaños Ventura GA, Bronsert M, et al. Text message reminders to improve infant immunization in Guatemala: a randomized clinical trial. Vaccine 2019;37(42):6192-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Forinash 2018 {published data only}
- Forinash AB, Yancey A, Chamness D, Koerner J, Inteso C, Miller C, et al. Smoking cessation following text message intervention in pregnant women. Annals of Pharmacotherapy 2018;52(11):1109-16. [DOI] [PubMed] [Google Scholar]
Gibson 2019 {published data only}
- Gibson DG, Kagucia EW, Were J, Obor D, Hayford K, Ochieng B. Text message reminders and unconditional monetary incentives to improve measles vaccination in western Kenya: study protocol for the mobile and scalable innovations for measles immunization randomized controlled trial. JMIR Research Protocols 2019;8(7):e13221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harari 2018 {published data only}
- *.Harari N, Rosenthal MS, Bozzi V, Goeschel L, Jayewickreme T, Onyebeke C, et al. Feasibility and acceptability of a text message intervention used as an adjunct tool by WIC breastfeeding peer counsellors: the LATCH pilot. Maternal & Child Nutrition 2018;14(1):e12488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Brockman JL, Harari N, Segura-Pérez S, Goeschel L, Bozzi V, Pérez-Escamilla R. Impact of the lactation advice through texting can help (LATCH) trial on time to first contact and exclusive breastfeeding among WIC participants. Journal of Nutrition Education and Behavior 2018;50(1):33-42. [DOI] [PubMed] [Google Scholar]
- Martinez-Brockman JL, Harari N, Segura-Perez S, Goeschel L, Perez-Escamilla R. Impact of the lactation advice through texting can help (LATCH) randomized controlled trial. FASEB Journal 2017;31(Suppl):457.7. [Google Scholar]
Harrington 2019 {published data only}
- *.Harrington EK, Drake AL, Matemo D, Ronen K, Osoti AO, John-Stewart G, et al. An mhealth SMS intervention on postpartum contraceptive use among women and couples in Kenya: a randomized controlled trial. American Journal of Public Health 2019;109(6):934-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington EK. Evaluation of an mHealth SMS Dialogue Strategy to Meet Women's and Couples' Postpartum Contraceptive Needs in Kenya (Mobile WACh XY): a Randomized Controlled Trial [Masters' thesis]. Vol. 10688609. Washington (DC): University of Washington, 2017. [Google Scholar]
Hmone 2017 {published data only}
- *.Hmone MP, Li M, Agho K, Dibley M. Impact of SMS text messages to improve exclusive breastfeeding and reduce other adverse infant feeding practices in Yangon, Myanmar: a randomized controlled trial. Annals of Nutrition and Metabolism 2017;71:610-11. [Google Scholar]
- Hmone MP, Li M, Agho K, Dibley MJ. Impact of SMS text messages to improve exclusive breastfeeding: a randomized controlled trial in Myanmar. FASEB Journal 2017;31(1):313.3.
- Hmone MP, Li M, Alam A, Dibley MJ. Mobile phone short messages to improve exclusive breastfeeding and reduce adverse infant feeding practices: protocol for a randomized controlled trial in Yangon, Myanmar. JMIR Research Protocols 2017;6(6):e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jasemzadeh 2018 {published data only}IRCT2016102810804N8
- Jasemzadeh M, Khafaie MA, Jaafarzadeh N, Araban M. Effectiveness of a theory-based mobile phone text message intervention for improving protective behaviors of pregnant women against air pollution: a randomized controlled trial. Environmental Science and Pollution Research 2018;25(7):6648-55. [DOI] [PubMed] [Google Scholar]
Oliveira‐Ciabati 2017 {published data only}
- Oliveira-Ciabati L, Vieira CS, Franzon AC, Alves D, Zaratini FS, Braga GC, et al. PRENACEL– a mHealth messaging system to complement antenatal care: a cluster randomized trial. Reproductive Health 2017;14(1):146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ortiz 2018 {published data only}
- Ortiz J. Post-abortion follow-up through SMS: texting alternatives to unnecessary follow-up visits. International Journal of Gynaecology and Obstetrics 2018;143(Suppl 3):54.
Palacios 2018 {published data only}
- Banna J, Campos M, Gibby C, Graulau RE, Melendez M, Reyes A, et al. Multi-site trial using short mobile messages (SMS) to improve infant weight in low-income minorities: development, implementation, lessons learned and future applications. Contemporary Clinical Trials 2017;62:56-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palacios C, Campos M, Gibby C, Banna J. Multi-site trial using short mobile messages (SMS) to improve infant feeding practices among participants in the WIC program. FASEB Journal 2017;31(Suppl):959.8-959.8.
- *.Palacios C, Campos M, Gibby C, Meléndez M, Lee JE, Banna J. Effect of a multi-site trial using short message service (SMS) on infant feeding practices and weight gain in low-income minorities. Journal of the American College of Nutrition 2018;37(7):605-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2018 {published data only}
- Patel A, Kuhite P, Puranik A, Khan SS, Borkar J, Dhande L. Effectiveness of weekly cell phone counselling calls and daily text messages to improve breastfeeding indicators. BMC Pediatrics 2018;18(1):337. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seth 2018 {published data only}
- Seth R, Akinboyo I, Chhabra A, Qaiyum Y, Shet A, Gupte N, et al. Mobile phone incentives for childhood immunizations in rural India. Pediatrics 2018;141(4):e20173455. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shinde 2018 {published data only}
- Shinde K, Rani U, Kumar PN. Assessing the effectiveness of immunization reminder system among nursing mothers of South India. Research Journal of Pharmacy and Technology 2018;11(5):1761-7. [Google Scholar]
Shorey 2017 {published data only}ISRCTN99092313
- *.Shorey S, Lau Y, Dennis CL, Chan YS, Tam WW, Chan YH. A randomized-controlled trial to examine the effectiveness of the 'Home-but not Alone' mobile-health application educational programme on parental outcomes. Journal of Advanced Nursing 2017;73(9):2103-17. [DOI] [PubMed] [Google Scholar]
- Shorey S, Ng YP, Danbjorg DB, Dennis CL, Morelius E. Effectiveness of the 'Home-but not Alone' mobile health application educational programme on parental outcomes: a randomized controlled trial, study protocol. Journal of Advanced Nursing 2017;73:253-64. [DOI] [PubMed] [Google Scholar]
Unger 2018 {published data only}
- Unger JA, Ronen K, Perrier T, DeRenzi B, Slyker J, Drake AL, et al. Short message service communication improves exclusive breastfeeding and early postpartum contraception in a low- to middle-income country setting: a randomised trial. BJOG 2018;125(12):1620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2018 {published data only}ISRCTN44149146
- Wang X, Luo R, Liu C, Zhang L, Yue A, Medina A, et al. Using daily text messages to improve adherence to infant micronutrient powder (MNP) packets in rural western China: a cluster-randomized controlled trial. PloS One 2018;13(1):e0191549. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xie 2018 {published data only}
- Xie RH, Tan H, Taljaard M, Liao Y, Krewski D, Du Q, et al. The impact of a maternal education program through text messaging in rural China: cluster randomized controlled trial. JMIR mHealth and uHealth 2018;6(12):e11213. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12618000636257 {published data only}
- ACTRN12618000636257. Investigating the impact of short automated text message reminder system in improving influenza vaccine uptake in children with chronic lung conditions: a randomised controlled trial. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=374892 (first received 12 April 2018).
Adam 2019 {published data only}
- Adam M, Tomlinson M, Le Roux I, LeFevre AE, McMahon SA, Johnston J, et al. The Philani MOVIE study: a cluster-randomized controlled trial of a mobile video entertainment-education intervention to promote exclusive breastfeeding in South Africa. BMC Health Services Research 2019;19:211. [DOI] [PMC free article] [PubMed]
CTRI/2018/04/013510 {published data only}
- CTRI/2018/04/013510. Effectiveness of mHealth for improving fetal outcome: a community based intervention trial. ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=20357 (first received 27 April 2018).
Cyan 2016 {published data only}
- Cyan R, Hussain H, Shehki I, Ishaq Z, Khan T, Rothenberg R. Affordable technology for saving maternal and infant lives: moving on with solutions. Annals of Global Health 2016;82:382.
Gelano 2018 {published data only}
- Gelano TF, Assefa N, Bacha YD, Mahamed AA, Roba KT, Hambisa MT. Effect of mobile-health on maternal health care service utilization in Eastern Ethiopia: study protocol for a randomized controlled trial. Trials 2018;19(1):102. [DOI] [PMC free article] [PubMed]
Gul 2019 {published data only}
- Gul X, Hameed W, Hussain S, Sheikh I, Siddiqui JU. A study protocol for an mhealth, multi-centre randomized control trial to promote use of postpartum contraception amongst rural women in Punjab, Pakistan. BMC Pregnancy Childbirth 2019;19(1):283. [DOI] [PMC free article] [PubMed] [Google Scholar]
IRCT20180520039728N1 {published data only}IRCT20180520039728N1
- IRCT20180520039728N1. Effectiveness of the distance education program on the mothers' empowerment in breast-feeding. en.irct.ir/trial/31317 (first received 3 July 2018).
ISRCTN13224744 {published data only}ISRCTN13224744
- ISRCTN13224744. The effectiveness of theory based intervention using social media to reduce urinary incontinence among postpartum women in Hebron city hospitals. isrctn.com/ISRCTN13224744 (first received 26 July 2018).
ISRCTN15017499 {published data only}ISRCTN15017499
- ISRCTN15017499. A trial exploring the feasibility of using telephone support (SMS and call) as a means of supporting young mothers (12–19 years) in Western Kenya soon after giving birth. isrctn.com/ISRCTN15017499 (first received 21 June 2017).
Kazi 2019 {published data only}
- Kazi AM, Ahsan N, Khan A, Jamal S, Kalimuddin H, Ghulamhussain N, et al. Personalized text messages and automated calls for improving vaccine coverage among children in Pakistan: protocol for a community-based cluster randomized clinical trial. JMIR Research Protocols 2019;8(5):e12851. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefevre 2019 {published data only}
- Lefevre A, Agarwal S, Chamberlain S, Scott K, Godfrey A, Chandra R, et al. Are stage-based health information messages effective and good value for money in improving maternal newborn and child health outcomes in India? Protocol for an individually randomized controlled trial. Trials 2019;20(1):272. [DOI] [PMC free article] [PubMed]
Maycock 2015 {published data only}
- Maycock BR, Scott JA, Hauck YL, Burns SK, Robinson S, Giglia R, et al. A study to prolong breastfeeding duration: design and rationale of the Parent Infant Feeding Initiative (PIFI) randomised controlled trial. BMC Pregnancy and Childbirth 2015;15(1):159. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02371213 {published data only}
- NCT02371213. Social networking on mobile phone to improve maternal and neonatal outcomes (HISONET). clinicaltrials.gov/show/NCT02371213 (first received 25 February 2015).
NCT03023033 {published data only}
- NCT03023033. Supporting attendance for facility delivery and infant health (SAFI). clinicaltrials.gov/show/NCT03023033 (first received 18 January 2017).
NCT03135288 {published data only}
- NCT03135288. Cell-phone assisted postpartum counseling on the use of long-acting reversible contraceptives. clinicaltrials.gov/ct2/show/NCT03135288 (first received 1 May 2017).
NCT03332108 {published data only}
- NCT03332108. Novel approach to improving lactation support using mobile health technology. clinicaltrials.gov/ct2/show/NCT03332108 (first received 6 November 2017).
NCT03355989 {published data only}
- NCT03355989. Evaluation of conditional cash transfers (CCTs) for immunization. clinicaltrials.gov/ct2/show/NCT03355989 (first received 29 November 2017).
NCT03379467 {published data only}
- NCT03379467. Use of SMS and interactive reminders to improve timely immunization coverage: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT03379467 (first received 20 November 2017).
NCT03399058 {published data only}
- NCT03399058. Innovative nutrition and mhealth evidence building project. clinicaltrials.gov/ct2/show/NCT03399058 (first received 16 January 2018).
NCT03402646 {published data only}
- NCT03402646. Mobile phone reminders (and photovoice) for routine immunization in Nigeria – the MOPING study. clinicaltrials.gov/ct2/show/NCT03402646 (first received 18 January 2018).
NCT03516682 {published data only}
- NCT03516682. The REDIVAC study-reducing delay in vaccination of children study. clinicaltrials.gov/ct2/show/NCT03516682 (first received 4 May 2018).
NCT03705455 {published data only}
- NCT03705455. Immunization schedule alert platform: determining ISAP SMS efficacy in improving childhood immunization timeliness and completeness in Nigeria. clinicaltrials.gov/ct2/show/NCT03705455 (first received 15 October 2018).
NCT03797950 {published data only}
- NCT03797950. Mobile nudges to increase early vaccination coverage in rural areas: a pilot Investigation in Ghana's northern region. clinicaltrials.gov/ct2/show/NCT03797950 (first received 9 January 2019).
NCT03890978 {published data only}
- NCT03890978. Improving exclusive breastfeeding via mobile phone text messages: a randomized controlled trial in southern Jordan. clinicaltrials.gov/ct2/show/NCT03890978 (first received 26 March 2019).
Odeny 2018 {published data only}
- Odeny TA, Onono M, Owuor K, Helova A, Wanga I, Bukusi EA, et al. Maximizing adherence and retention for women living with HIV and their infants in Kenya (MOTIVATE! study): study protocol for a randomized controlled trial. Trials 2018;19(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
PACTR201703002093382 {published data only}
- PACTR201703002093382. Effect of enhanced reminders on postnatal clinic attendance in Addis Ababa: a cluster randomized control trial. pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=2093 (first received 11 March 2017).
PACTR201711002737120 {published data only}
- PACTR201711002737120. Zinc adherence: a follow-up study of under-fives with acute watery diarrhoea using mobile phones: a randomised controlled trial. pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=2737 (first received 31 October 2017).
PACTR201801002231314 {published data only}
- PACTR201801002231314. Utilization of short message service to enhance uptake of focused ante-natal care among women in Tharaka Nithi County, Kenya. pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=2231 (first received 23 April 2017).
PACTR201806003369302 {published data only}
- PACTR201806003369302. Efficacy of text messages, voice calls and community visits on developmental milestones of children from teenage pregnancies: a randomized intervention trial. pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=3369 (first received 4 May 2018).
Rossing 2016 {published data only}
- Rossing E, Ravn H, Batista CS, Rodrigues A. MHealth to improve measles immunization in Guinea-Bissau: study protocol for a randomized controlled trial. JMIR Research Protocols 2016;5(3):e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Salam 2018 {published data only}
- Salam SS, Ali NB, Rahman AE, Tahsina T, Islam MI, Iqbal A, et al. Study protocol of a 4-parallel arm, superiority, community based cluster randomized controlled trial comparing paper and e-platform based interventions to improve accuracy of recall of last menstrual period (LMP) dates in rural Bangladesh. BMC Public Health 2018;18(1):1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tobe 2018 {published data only}
- Tobe RG, Haque SE, Ikegami K, Mori R. Mobile-health tool to improve maternal and neonatal health care in Bangladesh: a cluster randomized controlled trial. BMC Pregnancy and Childbirth 2018;18(1):102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Agarwal 2016
- Agarwal S, LeFevre AE, Lee J, L'Engle K, Mehl G, Sinha C, et al. Guidelines for reporting of health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist. BMJ 2016;352:i1174. [DOI: ] [DOI] [PubMed] [Google Scholar]
Agarwal 2018
- Agarwal S, Vasudevan L, Tamrat T, Glenton C, Lewin S, Bergman H, et al. Digital tracking, provider decision support systems, and targeted client communication via mobile devices to improve primary health care. Cochrane Database of Systematic Reviews 2018, Issue 1. Art. No: CD012925. [DOI: 10.1002/14651858.CD012925] [DOI] [Google Scholar]
Alkema 2016
- Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016;387(10017):462-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Amankwaa 2018
- Amankwaa I, Boateng D, Quansah DY, Akuoko CP, Evans C. Effectiveness of short message services and voice call interventions for antiretroviral therapy adherence and other outcomes: a systematic review and meta-analysis. PloS One 2018;13(9):e0204091. [DOI: 10.1371/journal.pone.0204091] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ames 2019
- Ames HM, Glenton C, Lewin S, Tamrat T, Akama E, Leon N. Clients’ perceptions and experiences of targeted digital communication accessible via mobile devices for reproductive, maternal, newborn, child, and adolescent health: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2019, Issue 10. Art. No: CD013447. [DOI: 10.1002/14651858.CD013447] [DOI] [PMC free article] [PubMed] [Google Scholar]
Black 2016
- Black RE, Levin C, Walker N, Chou D, Liu L, Temmerman M, et al. Reproductive, maternal, newborn, and child health: key messages from Disease Control Priorities 3rd Edition. Lancet 2016;388(10061):2811-24. [DOI] [PubMed] [Google Scholar]
Chamberlain 2017
- Chamberlain C, O'Mara-Eves A, Porter J, Coleman T, Perlen SM, Thomas J, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No: CD001055. [DOI: 10.1002/14651858.CD001055.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
de Jongh 2012
- Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database of Systematic Reviews 2012, Issue 12. Art. No: CD007459. [DOI: 10.1002/14651858.CD007459.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Every Women Every Child 2015
- Every Woman Every Child. The global strategy for women's and children's and adolescents' health (2016-2030): survive, thrive, transform. www.who.int/life-course/partners/global-strategy/globalstrategyreport2016-2030-lowres.pdf (accessed prior to 3 May 2020).
Free 2011
- Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet 2011;378(9785):49-55. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Free 2013a
- Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Medicine 2013;10(1):e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
Free 2013b
- Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Medicine 2013;10(1):e1001363. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gonçalves‐Bradley 2018
- Gonçalves-Bradley DC, Buckley BS, Fønhus MS, Glenton C, Henschke N, Lewin S, et al. Mobile-based technologies to support client to healthcare provider communication and management of care. Cochrane Database of Systematic Reviews 2018, Issue 1. Art. No: CD012928. [DOI: 10.1002/14651858.CD012928] [DOI] [PMC free article] [PubMed] [Google Scholar]
Griffiths 2018
- Griffiths SE, Parsons J, Naughton F, Fulton EA, Tombor I, Brown KE. Are digital interventions for smoking cessation in pregnancy effective? A systematic review and meta-analysis. Health Psychology Review 2018;12(4):333-56. [DOI: ] [DOI] [PubMed] [Google Scholar]
Guerriero 2013
- Guerriero C, Cairns J, Roberts I, Rodgers A, Whittaker R, Free C. The cost-effectiveness of smoking cessation support delivered by mobile phone text messaging: Txt2stop. European Journal of Health Economics 2013;14(5):789-97. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gurol‐Urganci 2013
- Gurol-Urganci I, Jongh T, Vodopivec-Jamsek V, Atun R, Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database of Systematic Reviews 2013, Issue 12. Art. No: CD007458. [DOI: 10.1002/14651858.CD007458.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawkins 2008
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Education Research 2008;23(3):454-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hay 2016
- Hay SI, Abajobit AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2016;390:1260-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hoffmann 2014
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI: ] [DOI] [PubMed] [Google Scholar]
Horvath 2012
- Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database of Systematic Reviews 2012, Issue 3. Art. No: CD009756. [DOI: 10.1002/14651858.CD009756] [DOI] [PMC free article] [PubMed] [Google Scholar]
ICT 2016
- ICT. Key ICT indicators for developed and developing countries and the world. idp.nz/Global-Rankings/ITU-Key-ICT-Indicators/6mef-ytg6 (accessed 1 December 2016).
Kaufman 2017
- Kaufman J, Ames H, Bosch-Capblanch X, Cartier Y, Cliff J, Glenton C, et al. The comprehensive 'Communicate to Vaccinate' taxonomy of communication interventions for childhood vaccination in routine and campaign contexts. BMC Public Health 2017;17(1):423. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaufman 2018
- Kaufman J, Ryan R, Walsh L, Horey D, Leask J, Robinson P, et al. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database of Systematic Reviews 2018, Issue 5. Art. No: CD010038. [DOI: 10.1002/14651858.CD010038.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2016
- Lee SH, Nurmatov UB, Nwaru BI, Mukherjee M, Grant L, Pagliari C. Effectiveness of mHealth interventions for maternal, newborn and child health in low- and middle-income countries: systematic review and meta-analysis. Journal of Global Health 2016;6(1):010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lorencatto 2012
- Lorencatto F, West R, Michie S. Specifying evidence-based behavior change techniques to aid smoking cessation in pregnancy. Nicotine and Tobacco Research 2012;14(9):1019-26. [DOI: ] [DOI] [PubMed] [Google Scholar]
McFadden 2017
- McFadden A, Gavine A, Renfrew MJ, Wade A, Buchanan P, Taylor JL, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No: CD001141. [DOI: 10.1002/14651858.CD001141.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Naghavi 2017
- Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1151-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pagel 2011
- Pagel C, Prost A, Lewycka S, Das S, Colbourn T, Mahapatra R, et al. Intracluster correlation coefficients and coefficients of variation for perinatal outcomes from five cluster-randomised controlled trials in low and middle-income countries: results and methodological implications. Trials 2011;12(1):151. [DOI: 10.1186/1745-6215-12-151] [DOI] [PMC free article] [PubMed] [Google Scholar]
Palmer 2018b
- Palmer M, Sutherland J, Barnard S, Wynne A, Rezel E, Doel A, et al. The effectiveness of smoking cessation, physical activity/diet and alcohol reduction interventions delivered by mobile phones for the prevention of non-communicable diseases: a systematic review of randomised controlled trials. PloS One 2018;13(1):e0189801. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Palmer in preparation
- Palmer MJ, Henschke N, Villanueva G, Maayan N, Bergman H, Glenton C, et al. Targeted client communication via mobile devices for improving reproductive and sexual health. Cochrane Database of Systematic Reviews In preparation. [DOI] [PMC free article] [PubMed]
PMNCH 2011
- The Partnership for Maternal, Newborn and Child Health. A global review of the key interventions related to reproductive, maternal, newborn and child health (RMNCH). Geneva: PMNCH 2011.
Quintana 2018
- Quintana Y, Martorell EA, Fahy D, Safran C. A systematic review on promoting adherence to antiretroviral therapy in HIV-infected patients using mobile phone technology. Applied Clinical Informatics 2018;9(2):450-66. [DOI: 10.1055/s-0038-1660516] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ryan 2013
- Ryan R, Hill S, Prictor M, McKenzie J, Cochrane Consumers and Communication Group. Study quality guide, May 2013. cccrg.cochrane.org/authorresources (accessed 8 January 2018).
Ryan 2016
- Ryan R, Horey D, Oliver S, McKenzie J, Prictor M, Santesso N, et al. Cochrane Consumers and Communication Group standard protocol text and additional guidance for review authors. CCCG cccrg.cochrane.org/author-resources (accessed October 2017).
Say 2014
- Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health 2014;2(6):e323-33. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JP, Green S, editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Shah 2019
- Shah R, Watson J, Free C. A systematic review and meta-analysis in the effectiveness of mobile phone interventions used to improve adherence to antiretroviral therapy in HIV infection. BMC Public Health 2019;19(1):915. [DOI: 10.1186/s12889-019-6899-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2014
- Singh N. Community-based and innovative technological approaches to improve child nutrition in India [PhD thesis]. London: LSHTM University of London, 2014. [Google Scholar]
Smith 2015
- Smith C, Ngo TD, Gold J, Edwards P, Vannak U, Sokhey L, et al. Effect of a mobile phone-based intervention on post-abortion contraception: a randomized controlled trial in Cambodia. Bulletin of the World Health Organization 2015;93(12):842-50a. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stade 2009
- Stade BC, Bailey C, Dzendoletas D, Sgro M, Dowswell T, Bennett D. Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD004228. [DOI: 10.1002/14651858.CD004228.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
UN 2015
- United Nations. Transforming our world: the 2030 agenda for sustainable development. Geneva: United Nations (A/RES/70/1) 2015.
Vodopivec‐Jamsek 2012
- Vodopivec-Jamsek V, Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews 2012, Issue 12. Art. No: CD007457. [DOI: 10.1002/14651858.CD007457.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Whittaker 2016
- Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database of Systematic Reviews 2016, Issue 4. Art. No: CD006611. [DOI: 10.1002/14651858.CD006611.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2010
- World Health Organization. Packages of interventions for family planning, safe abortion care, maternal, newborn and child health. apps.who.int/iris/handle/10665/70428 (accessed prior to 3 May 2020).
WHO 2013
- World Health Organization, London School of Hygiene and Tropical Medicine, South Africa Medical Research Council. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. apps.who.int/iris/handle/10665/85239 (accessed prior to 3 May 2020).
WHO 2017
- World Health Organization, United Nations Children's Fund. Reaching the every newborn national 2020 milestones: country progress, plans and moving forward. apps.who.int/iris/handle/10665/255719 (accessed prior to 3 May 2020).
WHO 2018
- World Health Organization. Classification of digital health interventions v1.0A shared language to describe the uses of digital technology for health. apps.who.int/iris/handle/10665/260480 (accessed prior to 3 May 2020).
WHO 2019
- World Health Organization. WHO guideline: recommendations on digital interventions for health system strengthening. apps.who.int/iris/handle/10665/311980 (accessed prior to 3 May 2020). [PubMed]
WHO/ITU 2015
- World Health Organization and International Telecommunication Union. A handbook on how to implement mTobaccoCessation. apps.who.int/iris/handle/10665/251719 (accessed prior to 3 May 2020).
World Bank 2017
- World Bank. World Development Indicators 2017. IGO.openknowledge.worldbank.org/handle/10986/26447 (accessed 30 July 2017).
References to other published versions of this review
Palmer 2018a
- Palmer MJ, Free C, Tamrat T, Henschke N, Glenton C, Lewin L, Fønhus M, Mehl G, Villanueva G, Maayan N, Bergman H. Targeted client communication via mobile devices for maternal, neonatal, and child health: systematic review protocol. CRD42018087234. PROSPERO 2018. [DOI] [PMC free article] [PubMed]


