Abstract
Using a multi-institutional EMR registry we extracted housing status and evaluated the presence of several important comorbidities in order to describe the demographics and comorbidity burden of persons experiencing homelessness in northeast Ohio and compare this to non-homeless individuals of varying socioeconomic position. Of 1,974,766 patients in the EMR registry, we identified 15,920 (0.8%) as homeless, 351,279 (17.8%) as non-homeless and in the top quintile of area deprivation index (ADI), and 1,607,567 (81.4%) as non-homeless and in the lower four quintiles of area deprivation. The comorbidity burden was highest in the homeless population with depression (48.1%), anxiety (45.8%), hypertension (44.2%), cardiovascular disease (18.4%), and hepatitis (18.1%) among the most prevalent conditions. We conclude that it is possible to identify homeless individuals and document their comorbidity burden using a multi-institutional EMR registry, in order to guide future interventions to address the health of the homeless at the health-system and community level.
Introduction
In recent years there has been growing recognition of the need for healthcare and healthcare systems to better understand and measure social and economic factors in an effort to adapt practices and care for patients.1,2 These factors, commonly described as social determinants of health, refer to aspects of the environments “in which people are born, live, learn, work, play, worship, and age” and have been linked to a number of health outcomes.3–6 These factors, and their upstream causes, may account for more of the variation in health and health outcomes than traditionally-examined aspects of the healthcare system.7–10 Housing is among the most fundamental social determinants of health, and persons who are homelessness are among the most socially and medically vulnerable populations.
Homelessness is a complex problem that is estimated to affect more than 550,000 Americans on any given night in the United States, including an estimated 23,000 persons experiencing homelessness in Cuyahoga County, Ohio in 2018.11–14 Homelessness and health influence one another through multiple, reinforcing mechanisms. For example, poor health can lead to employment problems which, in turn, affect one’s ability to afford safe and reliable housing. Conversely, stress and the experience of homelessness may introduce or exacerbate health issues such as infectious disease, high blood pressure, diabetes, and asthma.15–19 Many authors have documented the extent to which mental health issues arise with homelessness, including incident and more severe episodes of alcoholism, anxiety and depression and other psychiatric conditions.20 Less is known, however, about the extent to which this comorbidity burden can be captured using electronic health records as well as how this burden compares to groups of varying socioeconomic status and deprivation.
Multiple definitions of homelessness exist and the identification of persons experiencing homelessness presents an operationally challenging task within healthcare systems.14,21 This difficulty may partially explain why healthcare systems have had varied, and mostly limited, success in identifying and optimizing care for homeless individuals. We used a regional EMR registry to identify a population of persons experiencing homelessness who received care from either of two large health systems in Northeast Ohio – the Cleveland Clinic Health System and the MetroHealth System, the main campuses of which are located in Cuyahoga County. We then characterized the demographics and the burden of chronic disease in this population and compared it to the general population stratified by neighborhood socioeconomic deprivation. Socioeconomic deprivation refers to the “relative disadvantage an individual or social group experiences in terms of access and control over economic, material, or social resources and opportunities”.22 The goal of this comparison was to examine how the disease burden among homeless persons differs from both the non-homeless population, and the population of those who are not homeless but reside in areas of socioeconomic deprivation and thus might share similar degrees of material, economic, and other resource deprivation. Specifically, we compared the population of homeless individuals to those living in neighborhoods within the top quintile of socioeconomic deprivation (i.e., the highest level of deprivation) and then to all others.
Methods
Data Source
This study was approved by the Cleveland Clinic and MetroHealth Institutional Review Boards. The NEOCARE Learning Health Registry is an electronic medical record (EMR)-based database of patients who had at least 2 outpatient visits to either MetroHealth System or Cleveland Clinic Health System between 1999 and 2017 and were over 18 years old. Unique persons in the NEOCARE registry are de-duplicated across health systems. These health systems represent two of the three major health care systems in Northeast Ohio and, together, their patient populations capture 70% of Northeast Ohio residents. Further, the MetroHealth System serves as Cuyahoga County’s primary safety-net hospital, providing care for those who are uninsured, receiving Medicaid assistance, or otherwise vulnerable.
Patients in the NEOCARE registry are broadly demographically representative across all levels of neighborhood socioeconomic status, when compared to data from the American Community Survey, with only slight differences observed in the oldest population (those over age 80) (Table 1). The registry contains recorded clinical information such as diagnoses, procedures, residential location history, laboratory results, and medications.
Table 1.
Comparison of the NEOCARE cohort to US Census Neighborhood Population Estimates by Age and Neighborhood Socioeconomic Status
| Block Group ADI Quintile |
Age Category | ||||
|---|---|---|---|---|---|
| 18–34 | 35–49 | 50–64 | 65–79 | 80+ | |
| 1 | 5.6 : 5.2 | 6.0 : 6.3 | 7.2 : 7.7 | 4.6 : 4.1 | 3.6 : 1.9 |
|
| |||||
| 2 | 5.0 : 6.8 | 5.2 : 5.6 | 5.3 : 6.4 | 3.6 : 3.5 | 3.0 : 1.7 |
|
| |||||
| 3 | 4.9 : 6.6 | 5.1 : 5.6 | 5.2 : 5.8 | 2.9 : 2.8 | 2.6 : 1.4 |
|
| |||||
| 4 | 4.3 : 5.2 | 4.1 : 3.9 | 4.4 : 4.4 | 2.4 : 2.1 | 1.6 : 0.9 |
|
| |||||
| 5 | 3.7 : 4.2 | 3.2 : 2.7 | 3.6 : 3.2 | 1.8 : 1.5 | 1.1 : 0.6 |
Demographic comparison of the NEOCARE cohort to the American Community Survey (ACS) estimates. In each column, this table presents the percent of patients in the NEOCARE registry followed by the percent of patients estimated by ACS which fall into specific age and Census block group area deprivation index (ADI) quintiles. This table was created using the 2017 ACS 5-year estimates and only patients in the registry from 2013 to 2017 in order to ensure proper overlap with ACS. This table demonstrates that, other than the oldest old (80+), the demographics of the registry are congruent with the demographics of Northeast Ohio.
Exposure
We identified persons ever experiencing homelessness using the address recorded at any visit to a Cleveland Clinic or MetroHealth facility. Individuals with no address ever listed (n = 562,626), with addresses outside of Ohio or whose census tract contained zero households (n = 481,039) were excluded. We identified addresses that contained the term “homeless” or common misspellings (e.g., homesless, hiomeless, homless, homelss, etc.). Next, we matched addresses to a known list of homeless shelters in the Cleveland region either by identifying the shelter name (e.g. ‘Salvation Army’, ‘Shelter’, etc.) or by matching the address with a list of known shelter addresses provided by the CWRU Center on Urban Poverty and Community Development which was obtained directly from their historical roster of regional homeless service agencies. Finally, we manually reviewed commonly occurring addresses to establish if they represented the location of current or former homeless shelters not captured in the preceding steps. Individuals who had no documented history of homelessness were divided into those living in areas in the top quintile of neighborhood socioeconomic deprivation and all others, as described below.
Outcomes
We first describe the demographics of the population including patient age as listed at the first recorded homeless encounter or at the first encounter for the never homeless population, and further describe the burden of conditions present. Specific conditions include the 31 Elixhauser comorbidities23 plus cardiovascular disease, tuberculosis, hepatitis, kidney disease, hypotension, anxiety, dissociative and somatoform disorders, and other neoplasms. Diagnoses were identified from all available information in the medical record including the problem list, history, and inpatient or outpatient encounter diagnoses using Clinical Classification Software (CCS) codes, ICD-9-CM and ICD-10-CM codes. Further, we used a count of the total number of unique conditions as a measure of multimorbidity.
Statistical Methods
We calculated summary counts, percentages, means, and medians to describe the demographics (age, sex, race, ethnicity) and number of comorbidities of the groups. To operationalize neighborhood socioeconomic deprivation, we used a modified version of the Area Deprivation Index (ADI).24,25 The ADI is an index which describes an area’s socioeconomic disadvantage, with higher values representing more disadvantage.25 We used the R sociome package24 to calculate the ADI for all census tracts in Ohio using factor weights based on the Ohio population. Thus, our locally weighted ADI reflects the population of Ohio rather than that of the entire US. Data to calculate the ADI were derived from the 2010 census and the 2010–2015 five-year American Community Survey. Other work using ADI values from our region found that the ADI was stable over time and reported a 2009 to 2017 temporal association of 0.94.26 We used the ADI to establish two comparison populations: those who were never homeless and lived in areas in the top quintile of ADI (also termed the high area deprivation population), and those who were never homeless and lived in areas in all other quintiles of the ADI (the reference population). In line with recent efforts to reduce the emphasis on p-values as a measure of significance and recognizing that our large sample size would have made these p-values uniformly small and not meaningful, we have chosen not to report statistical significance and instead focus on the observable and meaningful differences.27–29 We do, however, report 95% confidence intervals for the comorbidity prevalence estimates. We used SAS for Windows version 9.4 (SAS, Cary, NC) and R version 3.6.030 for all analyses and visualization, with the ‘prop.test’ function being used to compute the 95% confidence intervals.
Results
Among 1,974,766 patients in the NEOCARE registry, we identified 0.8% (n=15,920) who were ever homeless. Among those who were never homeless, 17.8% (n=351,279) lived in areas in the top quintile of area deprivation (the high area deprivation population), and 81.4% (n=1,607,567) lived in all other quintiles of area deprivation (the reference population). Demographics of the three groups are shown in Table 1. Most of the homeless population were male (66.0%) whereas in both the high area deprivation and the reference populations the majority were female (Table 1). Most (55.6%) of the homeless were African American, compared to 49.6% of the high ADI population and 7.8% in the reference group. The median age was 41.1 years old for the homeless population, 36.9 for the high area deprivation and 44.1 for the reference population.
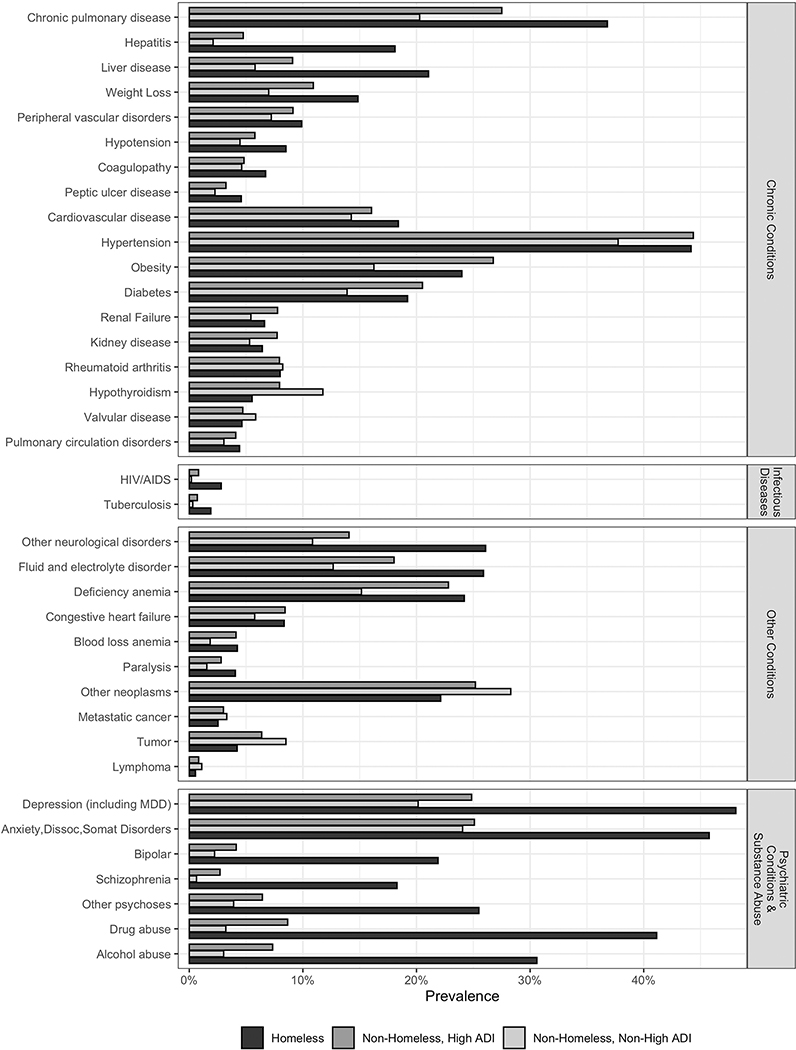
The pattern of individual comorbid conditions across the 3 populations is shown in Table 3 and Figure 1. Among the homeless population, mental health diseases and substance use disorders were common and more prevalent compared to the high ADI or reference groups. Similarly, liver disease and hepatitis were more common among the homeless population compared to the other two groups. Chronic conditions, such as diabetes, hypertension and pulmonary disease were more similar between the three groups, reinforced by the overlapping confidence intervals between the homeless and high area deprivation groups in: hypertension, congestive heart failure, valvular disease, pulmonary circulation disorders, and blood loss anemia, and overlap between all three groups for rheumatoid arthritis/collagen vascular diseases. Meanwhile, hypothyroidism, solid tumors and other neoplasms were more common among the reference population compared to the homeless or high ADI groups (Table 2 and Figure 1). The homeless population had a median of 4 chronic conditions compared to 2 in the high area deprivation and 2 in the reference population.
Table 3.
Prevalence of conditions of interest, with 95% confidence intervals, based on the Elixhauser Comorbidities, of the homeless, non-homeless with high area deprivation, and non-homeless with non-high area deprivation. High area deprivation is defined as the top quintile of the Area Deprivation Index (ADI). Comorbidities are listed in order of prevalence in people experiencing homelessness.
| Condition % (95% CI) |
Homeless n = 15,920 |
High Area Deprivation n = 351,279 |
Non-Homeless + Non-High Area Deprivation n = 1,607,567 |
|---|---|---|---|
| Depression (including MDD)* | 48.1 (47.3, 48.9) | 24.9 (24.7, 25.0) | 20.1 (20.1, 20.2) |
| Anxiety, dissociative and somatoform disorders* | 45.8 (45.0, 46.5) | 25.1 (25.0, 25.2) | 24.1 (24.0, 24.1) |
| Hypertension | 44.2 (43.4, 44.9) | 44.4 (44.2, 44.5) | 37.7 (37.7, 37.8) |
| Drug abuse | 41.1 (40.4, 41.9) | 8.7 (8.6, 8.8) | 3.2 (3.2, 3.2) |
| Pulmonary disease (chronic) | 36.8 (36.1, 37.6) | 27.5 (27.4, 27.7) | 20.3 (20.2, 20.3) |
| Alcohol abuse | 30.6 (29.9, 31.3) | 7.3 (7.3, 7.4) | 3.0 (3.0, 3.1) |
| Other neurological disorders | 26.1 (25.4, 26.8) | 14.1 (13.9, 14.2) | 10.9 (10.8, 10.9) |
| Fluid and electrolyte disorders | 25.9 (25.2, 26.6) | 18.0 (17.9, 18.2) | 12.7 (12.6, 12.7) |
| Other psychoses* | 25.5 (24.8, 26.2) | 6.4 (6.4, 6.5) | 3.9 (3.9, 3.9) |
| Deficiency anemias | 24.2 (23.5, 24.9) | 22.8 (22.7, 23.0) | 15.2 (15.1, 15.2) |
| Obesity | 24.0 (23.3, 24.7) | 26.8 (26.6, 26.9) | 16.3 (16.2, 16.3) |
| Other neoplasms* | 22.1 (21.5, 22.8) | 25.2 (25.0, 25.3) | 28.3 (28.2, 28.4) |
| Bipolar disorders* | 21.9 (21.3, 22.5) | 4.1 (4.1, 4.2) | 2.2 (2.2, 2.3) |
| Liver disease | 21.1 (20.4, 21.7) | 9.1 (9.0, 9.2) | 5.8 (5.8, 5.8) |
| Diabetes | 19.2 (18.6, 19.8) | 20.5 (20.4, 20.7) | 13.9 (13.8, 13.9) |
| CVD* | 18.4 (17.8, 19.0) | 16.0 (15.9, 16.2) | 14.3 (14.2, 14.3) |
| Schizophrenic disorders* | 18.3 (17.7, 18.9) | 2.7 (2.7, 2.8) | 0.6 (0.6, 0.7) |
| Hepatitis* | 18.1 (17.5, 18.7) | 4.8 (4.7, 4.8) | 2.1 (2.1, 2.1) |
| Weight loss | 14.8 (14.3, 15.4) | 10.9 (10.8, 11.0) | 7.0 (7.0, 7.0) |
| Peripheral vascular disorders | 9.9 (9.4, 10.4) | 9.1 (9.0, 9.2) | 7.2 (7.2, 7.3) |
| Hypotension* | 8.5 (8.1, 9.0) | 5.8 (5.7, 5.9) | 4.5 (4.4, 4.5) |
| Congestive heart failure | 8.4 (7.9, 8.8) | 8.4 (8.3, 8.5) | 5.8 (5.7, 5.8) |
| Rheumatoid arthritis/collagen vascular diseases | 8.0 (7.6, 8.4) | 7.9 (7.9, 8.0) | 8.2 (8.2, 8.3) |
| Coagulopathy | 6.7 (6.3, 7.1) | 4.8 (4.8, 4.9) | 4.6 (4.6, 4.6) |
| Renal failure | 6.6 (6.3, 7.0) | 7.8 (7.7, 7.9) | 5.4 (5.4, 5.5) |
| Kidney disease* | 6.4 (6.1, 6.8) | 7.7 (7.6, 7.8) | 5.3 (5.3, 5.3) |
| Hypothyroidism | 5.5 (5.2, 5.9) | 7.9 (7.9, 8.0) | 11.8 (11.7, 11.8) |
| Valvular disease | 4.6 (4.3, 5.0) | 4.7 (4.6, 4.8) | 5.8 (5.8, 5.9) |
| Peptic ulcer disease excluding bleeding | 4.6 (4.3, 4.9) | 3.2 (3.2, 3.3) | 2.3 (2.2, 2.3) |
| Pulmonary circulation disorders | 4.4 (4.1, 4.8) | 4.1 (4.0, 4.2) | 3.0 (3.0, 3.1) |
| Blood loss anemia | 4.2 (3.9, 4.6) | 4.1 (4.1, 4.2) | 1.8 (1.8, 1.9) |
| Solid tumor without metastasis | 4.2 (3.9, 4.5) | 6.4 (6.3, 6.5) | 8.5 (8.5, 8.6) |
| Paralysis | 4.1 (3.8, 4.4) | 2.8 (2.8, 2.9) | 1.5 (1.5, 1.6) |
| HIV/AIDS | 2.8 (2.6, 3.1) | 0.8 (0.8, 0.8) | 0.2 (0.2, 0.2) |
| Metastatic cancer | 2.5 (2.3, 2.8) | 3.0 (3.0, 3.1) | 3.3 (3.3, 3.3) |
| Tuberculosis* | 1.9 (1.7, 2.1) | 0.7 (0.7, 0.7) | 0.3 (0.3, 0.3) |
| Lymphoma | 0.5 (0.4, 0.7) | 0.8 (0.8, 0.9) | 1.1 (1.1, 1.1) |
CVD = Cardiovascular disease; HIV/AIDS = Human immunodeficiency virus/Acquired immunodeficiency syndrome
Not an Elixhauser comorbidity and thus individuals may be counted in multiple comorbidity categories.
Figure 1. Comorbidity prevalence by housing status.
High area deprivation is defined as the top quintile of the Area Deprivation Index (ADI). The conditions are grouped by broad disease category. MDD = Major Depressive Disorder; Anxiety,Dissoc,Somat Disorders = Anxiety, Dissociative, and Somatoform Disorders; HIV/AIDS = Human immunodeficiency virus/Acquired immunodeficiency syndrome
Table 2.
Demographic summary of the homeless, non-homeless with high area deprivation, and non-homeless with non-high area deprivation. High area deprivation is defined as the top quintile of the Area Deprivation Index (ADI).
| Demographic Summary % |
Homeless n = 15,920 |
Non-Homeless + High Area Deprivation n = 351,279 |
Non-Homeless + Non-High Area Deprivation n = 1,607,567 |
|---|---|---|---|
| Sex | |||
| - Female | 34.0 | 58.7 | 56.5 |
| - Male | 66.0 | 41.3 | 43.5 |
| Race | |||
| - White | 38.0 | 38.4 | 85.3 |
| - Black / African American | 55.6 | 49.6 | 7.8 |
| - Other/Declined/Unavailable/NA | 6.4 | 12.0 | 6.9 |
| Ethnicity | |||
| - Not Hispanic or Latino | 84.2 | 77.2 | 86.4 |
| - Hispanic or Latino | 5.0 | 9.7 | 1.6 |
| - NA | 10.8 | 13.1 | 11.9 |
| Age, years (%) | |||
| - 18 – 24 | 14.2 | 27.6 | 18.1 |
| - 25 – 34 | 20.5 | 18.9 | 16.1 |
| - 35 – 44 | 25.7 | 18.2 | 17.4 |
| - 45 – 54 | 25.9 | 15.1 | 18.3 |
| - 55–64 | 11.1 | 10.2 | 14.5 |
| - 65+ | 2.6 | 10.0 | 15.7 |
| - Mean (±SD) | 40.7 (± 13.1) | 39.3 (± 17.6) | 44.8 (± 18.3) |
| - Median (IQR) | 41.1 (30.6 – 50.2) | 36.9 (23.7 – 51.4) | 44.1 (29.4 – 58.2) |
| Number of Conditions (Elixhauser only) | |||
| - Mean (±SD) | 4.8 (± 3.6) | 3.3 (± 3.3) | 2.6 (± 2.8) |
| - Median (IQR) | 4 (2 – 7) | 2 (1 – 5) | 2 (0 – 4) |
NA = Not available
Discussion
Previous literature has documented the complex relationship between homelessness and health; a number of these studies have relied on electronic medical records (EMR) and other large healthcare databases in an effort to identify the ever homeless population for research to evaluate their health outcomes.15–20,31 These studies have utilized Medicaid enrollees, health exchanges, homeless program health information systems, and state-wide hospital discharge databases, but there remains substantial variation in the definition of homelessness.15,16,32–37 Our paper demonstrates the utility of a multi-institutional electronic medical record (EMR) registry to examine the health status and demographics of the ever homeless population.
The demographic results of this study are fairly consistent with other estimates of the homeless population, with some dissimilarities likely due to population differences.11 Of note, we observed differences in the racial composition of the groups, with 55.6% of the homeless population reporting Black/African-American which was similar to the 49.6% of the high area deprivation, however both of these are substantially higher than the 7.8% in the reference group. These results reflect both a highly racially segregated region as well as a high burden of homelessness among African Americans. When compared to a point-in-time count in 2018, our population has a higher proportion of Black/African-American (55.6% vs. 44.9%).38 The region in which this study was conducted is, historically, an area of extensive redlining – the systematic practice of rejecting mortgage applications for predominately Black neighborhoods – and other lending practices which have created stark, persistent, and enduring inequities in housing, homeownership, and the accumulation of wealth over time.39 Indeed, evidence suggests that, even today, lending practices differ between neighborhoods with majority Black residents as compared to those with majority White residents.40
Studying the pattern of morbidity among the homeless population is valuable to local and national public health and policymaking leaders who need to identify areas for intervention and modifiable risk factors to reduce the disease burden and increase the well-being of this population. Overall, the disease burden among the ever homeless was substantially greater than those who were never homeless. This disease burden is reflected in the higher prevalence of multimorbidity (measured through the median and mean total number of conditions) in the homeless and high area deprivation groups compared to the reference group of never homeless and non-high area deprivation. Notably, mental health conditions were common, with nearly half of the homeless experiencing depression, and/or anxiety disorders. Further, drug and alcohol abuse were much more common in the homeless population (41.1% and 30.6% respectively). This pattern of disease prevalence across the 3 populations was also seen for chronic pulmonary disease (36.8% in the homeless; 27.5% in the high area deprivation; 20.3% in the reference). Many of the conditions identified to be disproportionately prevalent in the homeless population are amenable to clinical intervention, and improved management of these conditions would likely return considerable value to the health care system.41–43
Some conditions, including hypertension, did not follow the generally observed pattern of higher prevalence among the ever homeless. Instead, the prevalence of hypertension in the three groups was relatively similar. While unadjusted for age, sex or racial differences, this result suggests that hypertension may be related to a milieu of individual and structural level systems as opposed to housing alone.44 It seems likely that the array of disease-promoting factors contributing to both risk for homelessness and area deprivation are similar. Above all, the similarity of some conditions across the entire population suggests that there is considerable nuance and complexity in the relationship between housing and health.
While some conditions such as hypertension and diabetes have been previously identified as having a high prevalence among the homeless, the prevalence we report is higher than found in previously published data. Some of this is likely due to data-source differences, but we believe that our approach using data from the electronic health record is reliable.45,46
This study has several limitations. First, we included a specific subsample of individuals ever experiencing homelessness, namely those also seen in a healthcare setting for two outpatient visits at some point during the 20-year period. Although their identification as homeless was not tied to these specific outpatient visits, our results may not be generalizable to homeless populations selected in other ways, including those who never engaged with the healthcare system on an outpatient basis (thus not included in the registry) or are never included in the EHR. By virtue of having at least 2 outpatient visits, this homeless population may be more connected to resources in ways that have implications for health and disease burden. Further, it is possible that our approach using keywords and addresses may have missed individuals experiencing acute homelessness, especially those who never reported to the health care system that they were homeless. The exclusion criteria used to construct our registry discarded individuals who lacked a census tract attached to their medical record – a limitation that should be systematically explored to better understand underlying individual- and system-level reasons and any bias it may introduce. Similarly, the assignment of area deprivation scores using the ADI may be limited in that, although designed to be relatively permanent across time, some census tract boundaries change over time as do the relevance of certain measures that comprise the ADI.26,47 As we assigned ADI based on the most recently available address, we were unable to assess how any changes in area deprivation may have contributed to misclassification between top quintile and all others. However, as currently modeled, ADI estimates for Ohio within the current study’s time frame exhibit nearly complete overlap.26 Finally, other programs such as Housing First in Permanent Supportive Housing48 could include homeless or housing insecure individuals that we did not identify as such since their primary address would have been an apartment or home.
Our study was cross sectional and we are unable to assign causal direction to the associations we observed. For example, a lower prevalence of metastatic disease may reflect a true prevalence or an increased mortality in this population. As such, our results should be considered as hypothesis generating and need to be confirmed in other studies and regions. Lastly, the rates of medical conditions reported in our manuscript are not adjusted for covariates; differences in personal characteristics of homeless persons could potentially explain some of the observed differences in disease rates. We established the prevalence estimates using all available data irrespective of timing of documented homelessness. Both of these points provide opportunities for future research to better assess the role of homelessness on health both through adjusting for, as well as incorporating, temporality. Additionally, future work should also examine utilization and other health care outcomes for these populations. Despite these limitations, our study provides a novel methodological approach utilizing electronic medical records to evaluate the health status of a regional homeless population.
Presently, there are broad efforts to incorporate collection of social determinants of health (SDOH) data into routine clinical encounters, making this data more available in the electronic medical record (EMR).49–52 In addition to describing the comorbidity burden, our study also highlights that while identifying homeless or housing-insecure individuals via the address recorded is feasible, it is not necessarily a sustainable practice. For more rapid and real-time research and intervention based on these factors it is likely inefficient to rely on fragments contained in address fields, when it is possible to record this data more efficiently. A greater emphasis on structured and standardized fields – as well as buy-in from providers on regularly using these fields – would be critical to assess the health needs of homeless and housing-insecure individuals. This would permit more rapid data querying and referral to social services. In addition to a specific field to document homelessness, the growing focus on ICD-10-CM diagnosis codes for health-related social needs provides another opportunity to collect this type of information in a structured way.53–56 However, in the interim our approach fills critical gaps in the literature and provides a strong foundation for focusing intervention efforts. Additional work to combine EMR data with Homeless Management Information System data will be necessary to confirm and extend our findings.
Acknowledgements
Research reported in this publication was supported by The National Institute on Aging of the National Institutes of Health under award number R01AG055480. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- EMR
Electronic Medical Record
- ADI
Area Deprivation Index
References
- 1.Schroeder SA. Shattuck Lecture. We can do better--improving the health of the American people. N Engl J Med. 2007;357(12):1221–1228. [DOI] [PubMed] [Google Scholar]
- 2.Dalton JE, Perzynski AT, Zidar DA, et al. Accuracy of Cardiovascular Risk Prediction Varies by Neighborhood Socioeconomic Position: A Retrospective Cohort Study. Ann Intern Med. 2017;167(7):456–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE. Independent effects of socioeconomic and psychological social determinants of health on self-care and outcomes in Type 2 diabetes. Gen Hosp Psychiatry. 2014;36(6):662–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Office of Disease Prevention and Health Promotion. Social Determinants of Health. Department of Health and Human Services. Healthy People 2030 Web site. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Published 2021. Accessed 26 July, 2021. [Google Scholar]
- 5.Artiga S, Hinton E. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. Washington, DC: Henry J Kaiser Family Foundation;2018. [Google Scholar]
- 6.Marmot M Social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. [DOI] [PubMed] [Google Scholar]
- 7.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129Suppl 2:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207–2212. [PubMed] [Google Scholar]
- 9.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398. [DOI] [PubMed] [Google Scholar]
- 10.Penman-Aguilar A, Talih M, Huang D, Moonesinghe R, Bouye K, Beckles G. Measurement of Health Disparities, Health Inequities, and Social Determinants of Health to Support the Advancement of Health Equity. J Public Health Manag Pract. 2016;22Suppl 1:S33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Housing and Urban Development. The 2018 Annual Homeless Assessment Report (AHAR) To Congress. United States Department of Housing and Urban Development;2018. [Google Scholar]
- 12.National Alliance to End Homelessness. State of Homelessness. https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness-report/. Published 2018.Accessed 2 February 2019, 2018.
- 13.Northeast Ohio Coalition for the Homeless. Just the Facts: Poverty and Homlessness in Our Community. https://www.neoch.org/poverty-stats-2017/. Published 2017. Accessed.
- 14.Henry M, Mahathey A, Morrill T, Robinson A, Shivji A, Watt A. The 2018 Annual Homeless Assessment Report (AHAR) to Congress. Washington, DC: United States Department of Housing and Urban Development;2018. [Google Scholar]
- 15.Bharel M, Lin WC, Zhang J, O’Connell E, Taube R, Clark RE. Health care utilization patterns of homeless individuals in Boston: preparing for Medicaid expansion under the Affordable Care Act. Am J Public Health. 2013;103Suppl 2:S311–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cushman M, Cantrell RA, McClure LA, et al. Estimated 10-year stroke risk by region and race in the United States: geographic and racial differences in stroke risk. Ann Neurol. 2008;64(5):507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris M, Gadermann A, Norena M, et al. Residential moves and its association with substance use, healthcare needs, and acute care use among homeless and vulnerably housed persons in Canada. Int J Public Health. 2019;64(3):399–409. [DOI] [PubMed] [Google Scholar]
- 18.Lam CN, Arora S, Menchine M. Increased 30-Day Emergency Department Revisits Among Homeless Patients with Mental Health Conditions. West J Emerg Med. 2016;17(5):607–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mackelprang JL, Qiu Q, Rivara FP. Predictors of Emergency Department Visits and Inpatient Admissions Among Homeless and Unstably Housed Adolescents and Young Adults. Med Care. 2015;53(12):1010–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Health Care for the Homeless Council. Homelessness and Health: What’s the Connection. https://nhchc.org/wp-content/uploads/2019/08/homelessness-and-health.pdf. Published 2019. Accessed 21 September, 2021.
- 21.youth.gov. Runaway and Homeless Youth: Federal Definitions. https://youth.gov/youth-topics/runaway-and-homeless-youth/federal-definitions. Published 2018. Accessed 21 September, 2021.
- 22.Lamnisos D, Lambrianidou G, Middleton N. Small-area socioeconomic deprivation indices in Cyprus: development and association with premature mortality. BMC Public Health. 2019;19(1):627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elixhauser A, Steiner C, Harris DR, Coffey RN. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 24.Krieger N sociome: Operationalizing Social Determinants of Health Data for Researchers. https://cran.r-project.org/web/packages/sociome/index.html. Published 2019. Accessed.
- 25.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93(7):1137–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adie Y, Kats DJ, Tlimat A, et al. Neighborhood Disadvantage and Lung Cancer Incidence in Ever-Smokers at a Safety Net Health-Care System: A Retrospective Study. Chest. 2020;157(4):1021–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenland S, Senn SJ, Rothman KJ, et al. Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Eur J Epidemiol. 2016;31(4):337–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kennedy-Shaffer L Before p < 0.05 to Beyond p < 0.05: Using History to Contextualize p-Values and Significance Testing. Am Stat. 2019;73(Suppl 1):82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McShane BB, Gal D, Gelman A, Robert C, Tackett JL. Abandon Statistical Significance. American Statistician. 2019;73(sup1):235–245. [Google Scholar]
- 30.R: A language and environment for statistical computing [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2019. [Google Scholar]
- 31.National Law Center on Homelessness & Poverty. Homelessness in America: Overview of Data and Causes. 2015. [Google Scholar]
- 32.Baggett TP, Liauw SS, Hwang SW. Cardiovascular Disease and Homelessness. J Am Coll Cardiol. 2018;71(22):2585–2597. [DOI] [PubMed] [Google Scholar]
- 33.Bejan CA, Angiolillo J, Conway D, et al. Mining 100 million notes to find homelessness and adverse childhood experiences: 2 case studies of rare and severe social determinants of health in electronic health records. J Am Med Inform Assoc. 2018;25(1):61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cavacuiti C, Svoboda T. The use of electronic medical records for homeless outreach. J Health Care Poor Underserved. 2008;19(4):1270–1281. [DOI] [PubMed] [Google Scholar]
- 35.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338(24):1734–1740. [DOI] [PubMed] [Google Scholar]
- 36.Vickery KD, Shippee ND, Bodurtha P, et al. Identifying Homeless Medicaid Enrollees Using Enrollment Addresses. Health Serv Res. 2018;53(3):1992–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zech J, Husk G, Moore T, Kuperman GJ, Shapiro JS. Identifying homelessness using health information exchange data. J Am Med Inform Assoc. 2015;22(3):682–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.United States Department of Housing and Urban Development. 2018 Continuum of Care Homeless Assistance Programs Homeless Populations and Subpopulations. 2018. [Google Scholar]
- 39.Gross TA ‘Forgotten History’ Of How The U.S. Government Segregated America. National Public Radio; 2017. [Google Scholar]
- 40.Lepley M, Mangiarelli L. Cuyahoga County Mortgage Lending Patterns. Cleveland, Ohio: Fair Housing Center for Rights & Research;2018. [Google Scholar]
- 41.O’Toole TP, Buckel L, Bourgault C, et al. Applying the chronic care model to homeless veterans: effect of a population approach to primary care on utilization and clinical outcomes. Am J Public Health. 2010;100(12):2493–2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Desilva MB, Manworren J, Targonski P. Impact of a housing first program on health utilization outcomes among chronically homeless persons. J Prim Care Community Health. 2011;2(1):16–20. [DOI] [PubMed] [Google Scholar]
- 43.O’Toole TP, Johnson EE, Borgia ML, Rose J. Tailoring Outreach Efforts to Increase Primary Care Use Among Homeless Veterans: Results of a Randomized Controlled Trial. J Gen Intern Med. 2015;30(7):886–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lackland DT. Racial differences in hypertension: implications for high blood pressure management. Am J Med Sci. 2014;348(2):135–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Institute of Medicine. Homelessness, Health, and Human Needs. Washington, DC: The National Academies Press; 1988. [PubMed] [Google Scholar]
- 46.Bernstein RS, Meurer LN, Plumb EJ, Jackson JL. Diabetes and hypertension prevalence in homeless adults in the United States: a systematic review and meta-analysis. Am J Public Health. 2015;105(2):e46–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Berg KA, Dalton JE, Gunzler DD, et al. The ADI-3: a revised neighborhood risk index of the social determinants of health over time and place. Health Services and Outcomes Research Methodology. 2021. [Google Scholar]
- 48.Department of Housing and Urban Development. Housing FIrst in Permanent Supportive Housing. Washington, DC: 2014. [Google Scholar]
- 49.King TE, Wheeler MB. Medical Management of Vulnerable and Underserved Patients: Principles, Practice, and Populations, Second Edition. 2nd ed. New York, NY: McGraw-Hill; 2016. [Google Scholar]
- 50.Gottlieb L, Manchanda R, Sandel M. Practical Strategies in Addressing Social Determinants of Health in Clinical Settings. In: King TE, Wheeler MB, eds. Medical Management of Vulnerable and Underserved Patients: Principles, Practice, and Populations, 2e.New York, NY: McGraw-Hill Education; 2016. [Google Scholar]
- 51.Lagasse J Social determinants of health data can be difficult to collect and share, but it’s imperative to success. Healthcare Finance. https://www.healthcarefinancenews.com/news/social-determinants-health-data-can-be-difficult-collect-and-share-its-imperative-success. Published 2019.Accessed 14 October, 2019.
- 52.Leon-Chisen N ICD-10-CM Coding for Social Determinants of Health. American Hospital Association; April2018. [Google Scholar]
- 53.Gottlieb L, Tobey R, Cantor J, Hessler D, Adler NE. Integrating Social And Medical Data To Improve Population Health: Opportunities And Barriers. Health Aff (Millwood). 2016;35(11):2116–2123. [DOI] [PubMed] [Google Scholar]
- 54.Orlowski JM. Comments on Proposal to Expand ICD-10-CM Codes for Social Determinants of Health. In. Washington, DC: Association of American Medical Colleges; 2019. [Google Scholar]
- 55.Reidhead M, Moyer L, Gerimann A. Z Codes for Social Determinants of Health: Which hospitals are most likely to use them and for which patients? : Missouri Hospital Association;2020. [Google Scholar]
- 56.Weeks WB, Cao SY, Lester CM, Weinstein JN, Morden NE. Use of Z-Codes to Record Social Determinants of Health Among Fee-for-service Medicare Beneficiaries in 2017. J Gen Intern Med. 2020;35(3):952–955. [DOI] [PMC free article] [PubMed] [Google Scholar]