Abstract
Complete blood cell count-derived parameters such as neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and lymphocyte-to-monocyte ratio (LMR) have recently shown to be highly sensitive biomarkers. Their usefulness has been proven as prognostic factors in several cancers, in the stratification of mortality in major cardiac events, as predictors and markers of infectious or inflammatory pathologies, and in many other conditions. Surprisingly, the study of these biomarkers in neurological diseases is somewhat limited. This paper aims to take stock of the data present in the literature regarding the complete blood cell count-derived ratios in this group of pathologies and to formulate a hypothesis, based on the most recent data concerning innate and acquired immunity, on which diseases of the nervous system could benefit in diagnostic and prognostic terms from the in-depth study of these new biomarkers.
Keywords: Blood cell count-derived ratios, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, neurology, psychiatrics
Introduction
Recently, complete blood cell count (CBC)-derived parameters such as neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and monocyte-to-lymphocyte ratio (LMR) have been extensively studied and proven to be highly sensitive biomarkers of disease.
Neutrophil-to-lymphocyte ratio, PLR, and LMR are not only inflammatory indices, but their trend reveals alterations in the immunological balance due to various pathologies, such as neoplastic or cardiovascular ones. For example, a neutrophilic response in cancer is associated with a poor prognosis. Indeed, it can inhibit the immune system by suppressing the cytotoxic activity of T cells, and likewise, the polarization status of monocytes/macrophage cells derived from blood regulates the response to tumors in all areas of the organism. In turn, platelets can participate in the inflammatory reaction by releasing growth factors or increasing angiogenesis.
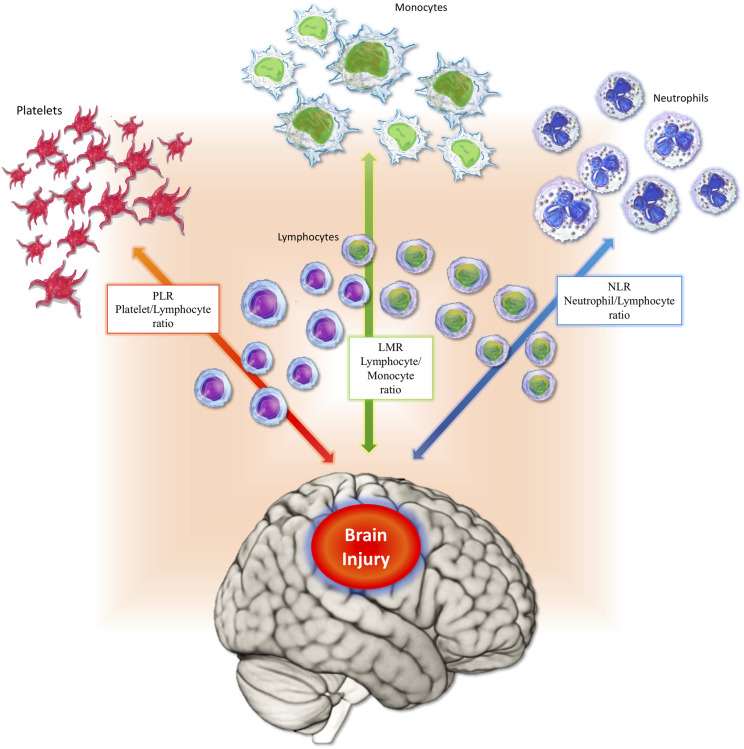
In almost all neurological diseases, an imbalance between innate immunity cells (such as neutrophils or macrophages) and acquired immunity cells (such as B and T lymphocytes) can be identified and also linked to the altered permeability of the blood–brain barrier.1 Furthermore, in recent years, NLR, LMR, and PLR indices in neurological diseases have begun to be studied (Figure 1).
Figure 1.
Complete blood cell count-derived parameters, including neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and lymphocyte-to-monocyte ratio (LMR), have recently been applied to neurological diseases as sensitive biomarkers for early diagnosis and accurate prognosis. Among diseases in this field, cerebrovascular diseases and primary and secondary brain tumors are the conditions in which these parameters have been studied better, showing good effectiveness as predictive and prognostic biomarkers. However, they have been found useful in multiple sclerosis, Alzheimer’s disease, and bipolar disorders, thus having great potential in other neurological diseases. Future applications may include neurodegenerative and neuropsychiatric diseases in which neuroinflammation has recently emerged as a key pathogenetic mechanism.
This paper aims to take stock of the study of these indices in neurological diseases and highlights the rationale for possible practical use, even in diseases in which they have not yet been studied.
Methods
Pertinent studies published were selected employing a MEDLINE search, accessed via PubMed database scanning. Search keys gave the following results: “neutrophil-to-lymphocyte ratio and neurology,” 117 outputs; “platelet-to-lymphocyte ratio and neurology,” 28 outputs; and “lymphocyte-to-monocyte ratio and neurology,” 15 outputs.
Given the short format of the paper, we made a close selection of the most representative studies. The articles we decided to cite in this paper were chosen based on their overall significance, referring to two main criteria: (i) we took into account the most recent studies in the considered topic, namely, for the ability to better represent state of the art on this focus; (ii) we considered the value of topics covered, in terms of relevance and scopes.
Results
The main results we could summarize from the literature review are that, currently, evaluating the blood cell count-derived indices (NLR, LMR, and PLR) finds its most significant application in cerebrovascular diseases and primary and secondary brain tumors. However, they have great potential also in other neurological diseases, and future applications may include neurodegenerative and neuropsychiatric diseases in which neuroinflammation is present.2
Discussion
The hematological indices studied have only recently been correlated with neurological pathologies. The first studies on NLR and LMR date back to 2013 and those on PLR date back to 2016. Interestingly, these studies focused mainly on cerebrovascular diseases. The outcome of patients with acute ischemic stroke can be related to such inflammatory indexes.3 The authors showed that high levels of NLR on hospital admission were associated with poor outcomes within 90 days, in a robust analysis, corrected for confounder variables.3 Post-thrombolysis early neurological outcomes have also been recently studied.4 The patients with early neurological deterioration (END) have higher levels of NLR, PLR, and lower levels of LMR than patients in the early neurological improvement (ENI) group.4
Another group of studies devoted to these hematological indices focused on primary and secondary brain tumors. The NLR may be a useful prognostic biomarker in brain tumors such as gliomas, meningiomas, or medulloblastomas and metastases from non-small cell lung cancer. In melanoma patients with brain metastases, higher NLR and PLR and lower LMR were associated with reduced overall survival.5
Interestingly, a significantly higher PLR and a lower LMR were found in patients with brain metastasis than in patients with glioblastoma. Both PLR and LMR had good diagnostic accuracy in differentiating glioblastoma from brain metastasis, but LMR showed the highest diagnostic accuracy. On the contrary, NLR showed low diagnostic accuracy.6
The hematological indices have also been evaluated in multiple sclerosis (MS).7 The NLR was found to be higher in MS and optic neuritis patients compared to healthy controls. The NLR may be a new supplemental marker of disease activity in relapsing–remitting MS patients, revealing an association between a high NLR value and MS occurrence.7
Inflammatory hypotheses have been suggested to explain the etiopathogenesis of several neurodegenerative and neuropsychiatric illnesses.2 Therefore, hematological indices have excellent potential in this field, but surprisingly, studies on this topic are very limited. The NLR may help identify patients with cognitive impairment from Alzheimer’s disease.8 In bipolar disorder, the NLR, PLR, and LMR were significantly higher in (hypo)manic than depressed individuals.9
The main reason why these hematological parameters are not yet widely used in diagnostics is that they are influenced by ongoing therapies and intercurrent diseases.10 Studies on this topic have only begun in recent years, but, likely, the use of parameters such as NLR, LMR, and PLR will soon become systematic in all neurological diseases.
This could have a substantial impact on diseases such as dementia and psychiatric disorders, where pathogenetic aspects of the neuroinflammatory type have emerged more recently.
Furthermore, over the last few years, new indices, including the platelet-to-neutrophil ratio (PNR) and the eosinophil-to-neutrophil ratio (ENR) and the eosinophil-to-monocyte ratio (EMR), which take into account the eosinophils, a type of immune cell involved in the acute inflammatory response, were found to have considerable effectiveness in cerebrovascular disease prognostic prediction. Future research will explore whether and how these new indices should be used to express their potential as reliable markers to guide diagnostic and therapeutic strategies in neurodegenerative diseases.
Conclusion
Complete blood cell count-derived parameters, including neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and lymphocyte-to-monocyte ratio (LMR), reveal alterations in the immunological balance and have been found helpful markers for prognostic evaluation of several diseases, such as neoplasms and cardiovascular ones. Encouraging applications of these parameters are cerebrovascular diseases and primary and secondary brain tumors, for which they displayed good effectiveness as a predictive outcome measure and prognostic biomarkers. Moreover, several lines of evidence suggest that they are useful in multiple sclerosis, Alzheimer’s disease, and bipolar disorders. These findings suggest that they have great potential in other neurological diseases. Future promising applications may include neurodegenerative and neuropsychiatric diseases in which neuroinflammation has recently been identified as a fundamental pathogenetic mechanism.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Fabiana Novellino https://orcid.org/0000-0002-5898-938X
Jose LM Madrigal https://orcid.org/0000-0002-1409-9561
References
- 1.Presta I, Vismara M, Novellino F, et al. (2018) Innate immunity cells and the neurovascular unit. International Journal of Molecular Sciences 19(12): 3856. DOI: 10.3390/ijms19123856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Novellino F, Saccà V, Donato A, et al. (2020) Innate immunity: a common denominator between neurodegenerative and neuropsychiatric diseases. International Journal of Molecular Sciences 21(3): 1115. DOI: 10.3390/ijms21031115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu Y, Huang K, Ji Z, et al. (2020) High neutrophil-to-lymphocyte ratio is associated with poor clinical outcome in patients with critically ill stroke. Minerva Anestesiologica 86(9): 939–947. DOI: 10.23736/S0375-9393.20.14310-4 [DOI] [PubMed] [Google Scholar]
- 4.Gong P, Liu Y, Gong Y, et al. (2021) The association of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio with post-thrombolysis early neurological outcomes in patients with acute ischemic stroke. Journal of Neuroinflammation 18(1): 51. DOI: 10.1186/s12974-021-02090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneider M, Schäfer N, Bode C, et al. (2021) Prognostic value of preoperative inflammatory markers in melanoma patients with brain metastases. J ournal of Clinical Medicine 10(4): 634. DOI: 10.3390/jcm10040634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baran O, Kemerdere R, Korkmaz TS, et al. (2019) Can preoperative neutrophil to lymphocyte, lymphocyte to monocyte, or platelet to lymphocyte ratios differentiate glioblastoma from brain metastasis?. Medicine 98(50): e18306. DOI: 10.1097/MD.0000000000018306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Amico E, Zanghì A, Romano A, et al. (2019) The neutrophil-to-lymphocyte ratio is related to disease activity in relapsing remitting multiple sclerosis. Cells 8(10): 1114. DOI: 10.3390/cells8101114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dong X, Nao J, Shi J, et al. (2019) Predictive value of routine peripheral blood biomarkers in alzheimer’s disease. Frontiers in Aging Neuroscience 11: 332. DOI: 10.3389/fnagi.2019.00332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fusar-Poli L, Natale A, Amerio A, et al. (2021) Neutrophil-to-lymphocyte, platelet-to-lymphocyte and monocyte-to-lymphocyte ratio in bipolar disorder. Brain Sciences 11(1): 58. DOI: 10.3390/brainsci11010058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bedel C, Korkut M, Armağan HH. (2021) NLR, d-NLR and PLR can be affected by many factors. International Immunopharmacology 90: 107154. DOI: 10.1016/j.intimp.2020.107154 [DOI] [PMC free article] [PubMed] [Google Scholar]