Abstract
Background
Proximal humeral fractures (PHFs) account for 4–5% of all fractures in the elderly. There is still a controversy among the treatments in the displaced PHFs. Our aim was to explore the clinical outcome of PHFs with the treatment of MultiLoc nail or Philos plate in the elderly patients.
Methods
A total of 82 sustained elderly patients with PHFs were finally recruited between Dec 2016 and Dec 2017. 34 patients were treated with MultiLoc nail and 48 patients were treated with Philos plate. The demographics, fracture types, blood loss, operation time, union time, postoperative complications, visual analog scores (VASs), Constant scores, American Shoulder and Elbow Scores (ASESs), and neck-shaft-angle (NSA) between the two groups were compared.
Results
No differences were observed in the demographics, fracture types, VAS, Constant scores, and ASES scores between the two groups at final follow-up. Compared with the plate group, the blood loss, operation time, and union time were significantly lower in the nail group (all P < .05). The rate of general complications was 54.17% in the plate group, which was higher than that in the nail group (26.47%, P = .01). Three patients experienced reoperation in the plate group (3/48; 6.25%), but none in the nail group. Although there were no significant differences in intraoperative NSA between the two groups, the NSA at final follow-up in the nail group was much higher than the plate group (137.55 ± 5.53°vs 134.47 ± 5.92°, P = .02).
Conclusions
Multiloc intramedullary nail showed the similar effectiveness of final VAS, final Constant scores, and ASES scores in PHFs treatment with Philos plate. However, MultiLoc nail is superior to Philos plate in blood loss, operation time, complications, reoperation rate, and the change of NSA.
Keywords: proximal humerus, fracture, intramedullary nail, locking plate
Introduction
Proximal humeral fractures (PHFs) account for 4-5% of all fractures in the elderly.1 With the elderly osteoporotic population continuing rising in this aging society, the megatrend of PHFs incidence remains increasing in the recent years.2-4 Non-operative treatments might be beneficial to undisplaced or minimally displaced PHFs, showing good clinical outcomes.5 However, there is still a controversy among the treatments between nonoperation and operation in the displaced PHFs. Surgical patients showed not only a trend of better social participation, but higher re-intervention rates.6,7 Surgical techniques include intramedullary nails, plates, intramedullary cage, hemiarthroplasty, and reverse total shoulder arthroplasty.8
Locking plate and intramedullary nail are the most commonly used implants in the operation of PHFs and locking plate osteosynthesis is considered as the gold standard treatment.9 Whereas, placement of locking plate requires dissection of the extensive soft tissues, which might disrupt the blood supply to fracture and cause necrosis.10 In addition, the position of plate depends on the fracture and the local anatomy would have effects on the peri-implant strain and the calcar screw construct in proximal or distal position respectively.11 However, percutaneous proximal humeral plate fixation could put the axillary nerve at the risk of injury.12 Locking antegrade intramedullary nail can preserve the periosteal blood supply and retain surrounding soft tissue attachments.13 Biomechanical studies have showed that the locking nail implant provided a more significantly stiffer construct than the locking plate.14,15 Although some previous studies compared the first and second generations of intramedullary nails with locking plates, it is still controversial on whether implant osteosynthesis is superior to another in the clinical outcomes and complications.16-18
With the deepening of PHFs’ understanding, the third generation straight intramedullary nails have avoided the defects of the first or second generation of intramedullary nails. The straight intramedullary MultiLoc® nail (Depuy Synthes, Oberdorf, Switzerland) is the representative of the third generation of intramedullary nails. Though previous studies have reported the clinical outcomes of Multiloc nail vs Philos plate, influences on fracture healing and complications by comorbidities (such as hypertension, diabetes, frozen shoulder, subacromial impingement syndrome, and so on) have been neglected. The purpose of this study is to compare clinical outcomes between MultiLoc nail and Philos® plate (Depuy plate Synthes, Oberdorf, Switzerland) on relatively homogenous PHFs patients. We also believe that our use of MultiLoc may provide better outcomes in PHFs patients. Our hypothesis is outcomes with using the MultiLoc nail will be superior to the Philos plate.
Patients and Methods
Patients
A total of 82 sustained patients who met the following criteria were finally recruited from the initial 232 patients with PHFs admitted in our department for surgery between Jan 2016 and Dec 2017. 34 patients were treated with the MultiLoc nail and the remaining of 48 patients were treated with the Philos plate. The inclusion criteria were as follows: (1) Unilateral displaced OTA11A-2.1 to 11-C/Neer 2-, 3-, 4-part of PHFs without fractures in the ipsilateral limb; (2) Low-energy injury caused by falls; (3) Age ≥55 years old with normal shoulder range of motion before injury; (4) Physiologically active patients; and (5) Patients treated with plates or nails. The exclusion criteria were as follows: (1) Head-splitting fractures; (2) Open fractures or pathological fractures; (3) Fractures and dislocation of shoulder; (4) Fractures accompanied by neurovascular injury; (5) A history of chronic shoulder pain or shoulder surgery; (6) A history of fracture union and chronic infection at other sites; (7) Comorbidities of hypertension and diabetes controlling poorly or comorbidities requiring hormone therapy; (8) Valgus fractures; and (9) Mental illness. This retrospective study was approved by the ethics committee of our institution. Informed consents were obtained from the patients or their relatives.
Routinely, radiographs of standardized anteroposterior, scapular lateral, and axillary view were used to evaluate the fracture type according to the Neer/OTA classification and more information of fractures was obtained from 3D computer tomography (3D-CT) reconstructions preoperatively.
Surgical Techniques
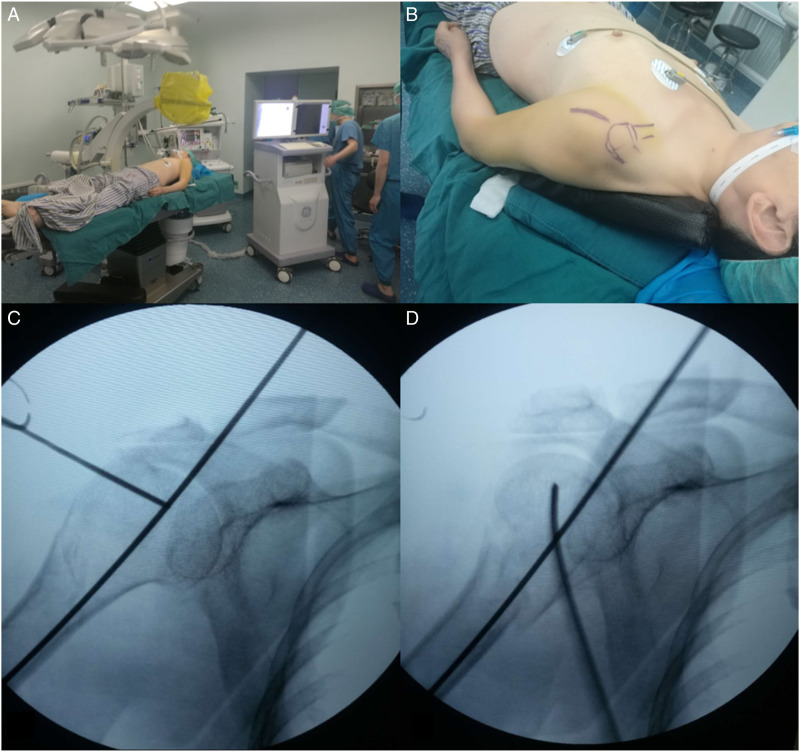
Under the general or brachial plexus anesthesia, the patients were placed in a supine position on the radiolucent operating table with a soft pad under the shoulder so that the shoulder joint could be extended backward by 30° (Figure 1). The C-arm was placed on the opposite side of the injured shoulder in horizontal plane and the humeral head was examined in an anteroposterior view (Figure 1).
Figure 1.
A and B shows the patient in a supine position with the injured arm backward 30°and C-arm on the opposite side. C and D shows the fracture was examined in an anteroposterior and lateral view under fluoroscopy.
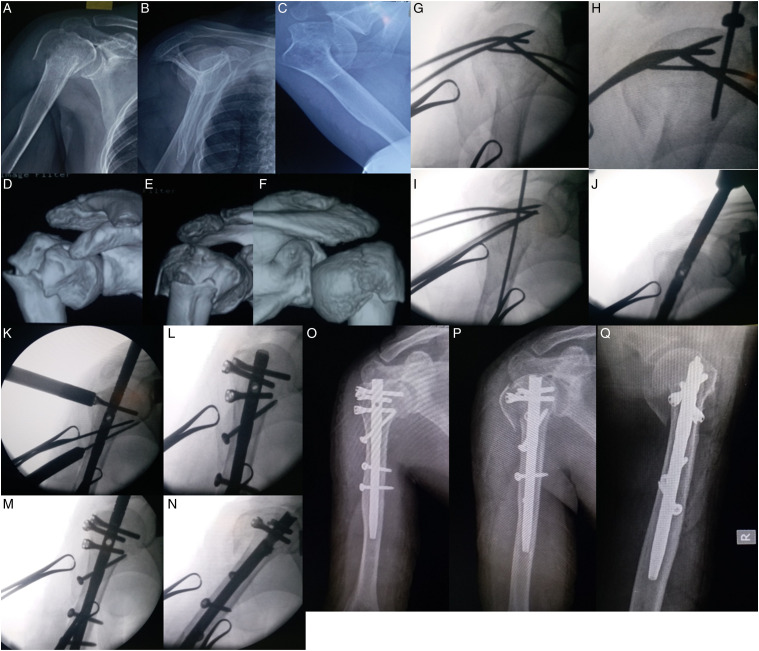
For patients in the nail group, the deltoid-splitting approach was utilized. A 4 cm incision was made at the anterior edge of the acromion directed toward the distal and lateral part. After revealing of the deltoid muscle, the anterior and middle bundles were split bluntly along the fibers direction to expose the subacromial bursa and fracture site. As for the 3- and/or 4-part fractures, the footprints of supraspinatus, infraspinatus, and subscapularis tendons were passed through by non-absorbable suture (Ethibond®, MB66) to allow for retracting and manipulating the greater and lesser tuberosities to the humeral head for reduction, then 2.0 or 2.5 mm K-wires were used to anchor the tuberosities to humeral head as an “en-block” temporarily. The wires were used as “joy-sticks” to manipulate the head in a neutral and external rotation position according the glenoid (without adduction and abduction) to determine reduction quality. If the reduction was acceptable, the guide rod was inserted into the entry point at the apex of the head which was confirmed under fluoroscopy in the anteroposterior and lateral view by rotating the K-wires internally, and then the rod was driven into the medullary cavity. At the bottom of rod, a 2 cm longitudinal incision was made in the direction of supraspinatus fibers to expose the humeral head. The medullary cavity was opened with a hollow drill. When the MultiLoc nail was inserted into the head and advanced across the fracture distally with twisting motion under fluoroscopy, the alignment of the head and shaft would be reduced automatically, and the distal humerus was slightly rotated to decrease the fracture line gap. The endpoint of nail was 3-4 mm below the cartilage level according to the ascending screw position device. Three proximal screws, two distal screws and an ascending calcar screw were inserted, and the screw fixation is applied when there was unstable fracture and poor bone quality. The sutures passing through the tendon footprint were attached to the proximal screws tightly. After the endcap was placed, the rotator cuff was repaired with non-absorbable suture. The incision was closed. Figure 2 shows the surgical process.
Figure 2.
A–G shows the plain and 3D-CT reconstruction views of a 64 years old woman with 3-part fracture. G–N shows the fracture reduction with “joy-stick” techniques, identification of entry point, and the insertion of nail. O–Q shows the intraoperative film.
For patients in the plate group, a classical deltopectoral approach was used. After the PHFs were exposed, non-absorbable sutures (Ethibond, MB66) were placed in the supraspinatus, infraspinatus, and subscapularis tendons to allow for traction. The humeral head was reduced to the shaft with K-wire or elevator and fixed temporally with K-wire, and the reduction quality of the medial portion of the calcar and neck-shaft-angle were confirmed under fluoroscopy. The greater and/or lesser tuberosities were pulled for reduction, which could be neglected in the 2 pars fractures. The plate was placed on 5–8 mm distally to the upper end of the greater tuberosity at least and 2–4 mm laterally to the bicipital groove, then at least 5 locking screws were inserted proximally and 2 screws distally. The sutures threaded through the holes in the plate and were knotted to increase the stability further.
Rehabilitation
The duration of immobilization with a sling was 6 weeks. Passive movement of shoulder started on the second day postoperatively. The shoulder was performed passive movements which included of forward flexion, backward extension, adduction, and abduction, but the latter two movements were not in the plate group. These movements were instructed by a physical therapist. Active movements started at the 7th week postoperatively.
Data Collection
The general data included age, gender, and type of fractures. Outcomes were measured by range of motion, American Shoulder and Elbow Surgeon scores (ASESs), Constant-Murley scores, and visual analog scores (VASs) at 6th month, 12th month, and the last follow-up. Radiographs were used to evaluate the process of union, neck-shaft-angle (NSA), and complications.
Statistical Analysis
Data analysis was performed with the statistical package SPSS 17.0 (SPSS Inc, Chicago, IL). Continuous variables were presented as mean ± standard deviation. Chi-square test or Fisher exact test was used to analyze categorical variables. Student t test was used to analyze continuous variables. Statistical difference is set as P value <.05.
Results
The duration of follow-up averaged 15.6 month (range 12–24 month). The baseline information was showed in Table 1. The general complications were 9 (26.47%) and 26 (54.17%) in the nail and plate group, respectively (P = .01, Table 2). The average surgical duration was less in the nail group than the plate group (87.31 ± 23.32 mins vs 101.52 ± 24.62 mins, P = .01). The volumes of blood loss were 189.34 ± 62.03 mL in the nail group, which was lower than that in the plate group (222.87 ± 76.42 mL, P = .03). Compared with the plate group, the duration of bone union was also significantly shorter in the nail group (11.64 ± 1.81 weeks vs 12.53 ± 1.75 weeks, P = .03). The differences in VASs, ASESs, and Constant scores at final follow-up were not observed between the two groups. There was no difference in NSA intraoperatively but NAS at final follow-up was higher in the nail group (137.55 ± 5.53°vs. 134.47 ± 5.92°, P = .02). Detailed data were showed in Table 2. Figure 3 shows shoulder function of a patient and the plain film at 1 year follow-up.
Table 1.
The baseline information in the two groups.
| Nail group (n = 34) | Plate group (n = 48) | P Value | |
|---|---|---|---|
| Age (years) | 67.2 ± 6.31 | 66.3 ± 7.05 | .56 |
| Male (%) | 11 (32.35) | 17 (35.42) | .81 |
| Injured left side (%) | 13 (38.24) | 15 (31.25) | .50 |
| Fracture types (%) | — | — | .97 |
| II | 19 (55.88) | 28 (58.33) | — |
| III | 10 (29.41) | 13 (27.09) | — |
| IV | 5 (14.71) | 7 (14.58) | — |
| Incision problem (%) | 2 (5.88) | 6 (12.50) | .46 |
| Shoulder pain (%) | 7 (20.59) | 16 (33.33) | .23 |
Table 2.
Clinical and radiological outcomes in the two groups.
| Nail group (n = 34) | Plate group (n = 48) | P Value | |
|---|---|---|---|
| General complications (%) | 9 (26.47) | 26 (54.17) | .01 |
| Final VAS | .38 ± .55 (0 − 2) | .52 ± .51 (0 − 1) | .26 |
| Surgical duration (mins) | 87.31 ± 23.32 (60 − 150) | 101.52 ± 24.62 (60 − 150) | .01 |
| Volumes of blood loss (mL) | 189.34 ± 62.03 (100 − 300) | 222.87 ± 76.42 (100 − 400) | .03 |
| Intraoperative NSA (°) | 139.42 ± 5.52 (125 − 155) | 138.08 ± 5.54 (125 − 150) | .26 |
| Final NSA (°) | 137.55 ± 5.53 (120 − 150) | 134.47 ± 5.92 (110 − 150) | .02 |
| Union time (weeks) | 11.64 ± 1.81 (8 − 15) | 12.53 ± 1.75 (8 − 15) | .03 |
| Final constant scores | 81.92 ± 9.68 (40−91) | 78.69 ± 8.09 (49 − 92) | .10 |
| Final ASES scores | 85.38 ± 9.17 (45 − 96) | 82.83 ± 7.14 (60 − 95) | .17 |
ASES, American Shoulder and Elbow Score; NSA, Neck-shaft-angle; VAS, Visual analog score.
Figure 3.
The excellent functional results of shoulder of the aboved patient and the plain film at 1 year.
Two plates (2/48, 4.17%) were removed due to screw cut out of articular surface, but articular surface intrusion was not found in the nail group. One patient with humeral head necrosis (1/48, 2.08%) was found in the plate group. Moreover, neurovascular injury, nonunion, and fracture displacement were not found in the two groups.
Discussion
Patients with displaced PHFs can be treated with surgical management, though no clear evidence shows 1 treatment is superior to others. Brouwe et al7 reported similar results after operative or non-operative treatment in patients (≥65 years) with the displaced 3- or 4-part humeral fractures and a better trend toward social participation in operative patients in a 10-year retrospective study. However, it was recommended to treat physiologically older or inactive PHFs patients (excluding dislocations) non-operatively and treat physiologically younger or active patients with surgery.19
In this study, the patients who required high shoulder function were selected. The strict inclusion and exclusion criteria minimized the impact of other factors on patients’ surgical outcomes, which were stated rarely in previous studies.20,21 Operative effects were susceptible to the comorbidities such as severe hypertension or diabetes, and these comorbidities might cause microvascular lesion and influence fracture union. All fractures were caused by low-energy falls, and thus the soft tissue damage was minimized. The diameter of intramedullary cavity might be narrower than that of nails in patients aged <55 years, which created some difficulty of nail insertion, and violent insertion could increase the risk of soft tissue damage. Our criteria guaranteed the homogeneity of patients as much as possible, reducing the impacts of other factors on the outcomes in the patients with PHFs.
During the surgery, the traditional beach chair position could be replaced by the supine position. It was possible to achieve the fluoroscopy of proximal humerus with C-arm placed on the opposite side before draping by the rotating the humerus, which facilitated the operation of the surgeon and reduced the chance of contamination due to moving the C-arm. Differing from the fracture reduction which used K-wires to maintain by other studies,9,22,23 the fracture reduction was unnecessary before the nail insertion in our experience because the fracture would be reduced automatically and correctly in the 2-part fracture type if the entry point was precise. When the greater and/or lesser tuberosities were reduced and maintained to the humeral head, the 3- and 4-part fracture type would change into the 2-part fracture type.
Although no secondary displacement was found in the two groups at final follow-up, the NSA in the plate group decreased more than the nail group, which reflected the biomechanical advantages of nails. Zhao et al compared the effects of Philos plate alone and Philos combined with fibular allograft in the treatment of PHFs, and the latter was superior to the former in supporting humeral head and maintaining the reduction.24 Several studies have shown similar clinical outcomes between the plate and nail on treating PHFs.9,16,17,21 However, intramedullary nails have overwhelming biomechanical advantages over plates due to the central fixation and short lever of the nail. Clavert et al tested angle-stable plate and nail in 4-part fracture, and the nail demonstrated higher values than locking plate in both stiffness and loading to failure without increasing neurological risks.25 Fuchtmeier et al reported that the intramedullary load carriers were biomechanically superior when compared to the plating systems in the 2-part fracture. Similarly, the straight design of MultiLoc nail has biomechanical advantages over curved nail.15 Gunther et al analyzed the quantitative CT of straight and bent nail bearing regions of cadaveric proximal humerus, a rapid decrease of bone density in cranio-caudal direction but more bone stock surrounding the straight nail region were observed, so they recommended the nail should be anchored in the subcortical area as close as possible.26 The subcortical area also named as the fifth anchoring point, which should be planed precisely before operation.27
Our study showed no differences between the two groups in VASs, Constant scores, and ASESs scores at final follow-up. Similarly, a prospective randomized controlled trial also showed there were no significant differences of Constant scores and VASs between these two groups at final follow-up.28 Ge et al reported the Constant scores, ASESs, and VASs were 82.03, 81.53, and .83 for the nail group, and 82.23, 80.06, and .81 for the plate group at 24 months, which were similar with ours.29 Our Constant score was higher and the VAS was lower than those reported in Gracitelli’s study9 and Boudard et al’s study.17 It may be due to the different implants. And our rehabilitation plan was also earlier. Prolonged immobilization postoperatively was not conducive to rehabilitation. Passive and active activities could relieve swelling and soft tissue adhesion, then shoulder function recovery would be promoted. Our study showed comparable intraoperative NSA, but much higher loss of NSA in the Plate Group. On the contrary, Rotman et al30 reported severe loss of NSA in patients treated with MultiLoc, and no ascending calcar screw was seen in their pictures to support the medial column and increase the axial stability which was indispensable in fracture reconstruction and avoiding secondary displacement.31-33 Biomechanical evaluation showed that two screws and a calcar screw were superior in most aspects to increase the stability.33
Our findings also demonstrated that the surgery time, blood loss, postoperative complications, and union time were less in the nail group than in the plate group. A meta-analysis which involved 2699 patients in thirty-eight retrospective studies demonstrated the intramedullary nails in the treatment of PHFs were superior to locking plates in terms of intraoperative blood loss, operative time, postoperative complications, and fracture healing time. Intramedullary nail is a minimally invasive surgery with small incision and intermuscular approach without extensive soft tissues being stripped.34 The malalignment of head and shaft should reduce automatically, while the nail passed through the fracture line. The most time-consuming procedures were reduction of the greater and lesser tuberosities for the 3- and 4-part fracture and confirmation the entry point.
MultiLoc is the 3rd intramedullary nail for PHFs. The clinical and radiological outcomes were satisfactory in our study. The 1st generation nails could not provide rotational control and adequate fixation of displaced fragments, which would lead to malunion or nonunion.35 The 2nd generation nails was inadequate security of the proximal interlocking screws, which was unable to fix constructs with stable angle, and the screws were engaged only in the cancellous bone, so fixation lost and screw backout were common.35 The entry point of the 2nd generation nail located at articular surface, which was medially to the greater tuberosity, nearly the supraspinatus tendon insertion, between the greater tubercle and humeral head fragment, and insertion of the nail may push the fracture fragments apart into the 3-part fracture.36 Nolan et al concluded that the 2nd generation nails showed high percentage of unsatisfactory results, violating the rotator cuff and being unable to resist the deforming forces that could lead to loss of fixation and varus collapse.18 The entry point of MultiLoc nail is more medial than that of the 2nd nail. With more bone stock surrounding the nail and the fifth anchor point to enhance the stability,26 it can prevent the violation of critical hypovascular zone simultaneously.37 The screw-in-screw configuration contributed to prevent varus collapse and it provided better stability and the additional calcar screw, a positive effect when regarding to the failure load reached.33,38 Due to the application of screw-in-screw and calcar screw, the mean decrease of NSA was 1.9° in our nail group, which was less than Nolan et al18 with Polaris nail (8°) and Rotman et al30 with MultiLoc nail (16.5°).
Limitations
There are several limitations in our study. First, this is a retrospective study in the single center. Second, statistical analysis could not be performed between the different fracture types due to the relatively small sample size, especially for the 4-part fractures. Lastly, the effect of osteoporosis on treatment outcomes has not been investigated between the two groups, which might affect the change of NSA and contribute to loosening of implants.
Conclusion
Changes in patient position and C-arm placement can simplify the surgical procedure. MultiLoc nail is superior to Philos plate in blood loss, operation time, complications, union time, and the change of final NSA.
Acknowledgments
The authors thank radiologist Lin Guo and Yi Cao for their imaging measurements of this study.
Author’s Note: Guoyun Bu and Weitang Sun contributed equally to this work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: We got approval from the Ethics Committee of Tianjin Hospital, and acquired the consent of reviewing the medical records of the patients.
Informed Consent: We got consent for publication from patients and hospital.
Data Availability: All data generated or analyzed during this study are included in this enclosed article. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
ORCID iD
Wanfu Wei https://orcid.org/0000-0002-4321-803X
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691-697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.McLean AS, Price N, Graves S, Hatton A, Taylor FJ. Nationwide trends in management of proximal humeral fractures: an analysis of 77,966 cases from 2008 to 2017. J Shoulder Elbow Surg. 2019;28(11):2072-2078. doi: 10.1016/j.jse.2019.03.034. [DOI] [PubMed] [Google Scholar]
- 3.Klug A, Gramlich Y, Wincheringer D, Schmidt-Horlohé K, Hoffmann R. Trends in surgical management of proximal humeral fractures in adults: a nationwide study of records in Germany from 2007 to 2016. Arch Orthop Trauma Surg. 2019;139(12):1713-1721. doi: 10.1007/s00402-019-03252-1. [DOI] [PubMed] [Google Scholar]
- 4.Launonen AP, Lepola V, Saranko A, Flinkkilä T, Laitinen M, Mattila VM. Epidemiology of proximal humerus fractures. Archives of osteoporosis. 2015;10:209. doi: 10.1007/s11657-015-0209-4. [DOI] [PubMed] [Google Scholar]
- 5.Hatzidakis AM, Shevlin MJ, Fenton DL, Curran-Everett D, Nowinski RJ, Fehringer EV. Angular-stable locked intramedullary nailing of two-part surgical neck fractures of the proximal part of the humerus. J Bone Joint Surg. 2011;93(23):2172-2179. doi: 10.2106/jbjs.J.00754. [DOI] [PubMed] [Google Scholar]
- 6.Jordan RW, Modi CS. A review of management options for proximal humeral fractures. Open Orthop J. 2014;8:148-156. doi: 10.2174/1874325001408010148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brouwer ME, Reininga IHF, El Moumni M, Wendt KW. Outcomes of operative and nonoperative treatment of 3- and 4-part proximal humeral fractures in elderly: a 10-year retrospective cohort study. Eur J Trauma Emerg Surg. 2019;45(1):131-138. doi: 10.1007/s00068-017-0890-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hudgens JL, Jang J, Aziz K, Best MJ, Srikumaran U. Three- and 4-part proximal humeral fracture fixation with an intramedullary cage: 1-year clinical and radiographic outcomes. J Should Slbow Surg. 2019;28(6s):S131-s137. doi: 10.1016/j.jse.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 9.Gracitelli MEC, Malavolta EA, Assunção JH, et al. Locking intramedullary nails compared with locking plates for two- and three-part proximal humeral surgical neck fractures: a randomized controlled trial. J Shoulder Elbow Surg. 2016;25(5):695-703. doi: 10.1016/j.jse.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Lambert SM. Ischaemia healing and outcomes in proximal humeral fractures. EFORT Open Rev. 2018;3(5):304-315. doi: 10.1302/2058-5241.3.180005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fletcher JWA, Windolf M, Richards RG, Gueorguiev B, Buschbaum J, Varga P. Importance of locking plate positioning in proximal humeral fractures as predicted by computer simulations. J Orthop Res. 2019;37(4):957-964. doi: 10.1002/jor.24235. [DOI] [PubMed] [Google Scholar]
- 12.Dang KH, Ornell SS, Reyes G, Hussey M, Dutta AK. A new risk to the axillary nerve during percutaneous proximal humeral plate fixation using the synthes PHILOS aiming system. J Shoulder Elbow Surg. 2019;28(9):1795-1800. doi: 10.1016/j.jse.2019.01.019. [DOI] [PubMed] [Google Scholar]
- 13.Laux CJ, Grubhofer F, Werner CMZ, Simmen H-P, Osterhoff G. Current concepts in locking plate fixation of proximal humerus fractures. J Orthop Surg Res. 2017;12(1):137. doi: 10.1186/s13018-017-0639-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kitson J, Booth G, Day R. A biomechanical comparison of locking plate and locking nail implants used for fractures of the proximal humerus. J Shoulder Elbow Surg. 2007;16(3):362-366. doi: 10.1016/j.jse.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 15.Füchtmeier B, May R, Hente R, et al. Proximal humerus fractures: a comparative biomechanical analysis of intra and extramedullary implants. Arch Orthop Trauma Surg. 2007;127(6):441-447. doi: 10.1007/s00402-007-0319-6. [DOI] [PubMed] [Google Scholar]
- 16.Li M, Wang Y, Zhang Y, Yang M, Zhang P, Jiang B. Intramedullary nail versus locking plate for treatment of proximal humeral fractures: a meta-analysis based on 1384 individuals. J Int Med Res. 2018;46(11):4363-4376. doi: 10.1177/0300060518781666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boudard G, Pomares G, Milin L, et al. Locking plate fixation versus antegrade nailing of 3- and 4-part proximal humerus fractures in patients without osteoporosis. comparative retrospective study of 63 cases. J Orthop Traumatol: Surgery & Research. 2014;100(8):917-924. doi: 10.1016/j.otsr.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 18.Nolan BM, Kippe MA, Wiater JM, Nowinski GP. Surgical treatment of displaced proximal humerus fractures with a short intramedullary nail. J Shoulder Elbow Surg. 2011;20(8):1241-1247. doi: 10.1016/j.jse.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Jawa A, Burnikel D. Treatment of Proximal Humeral Fractures: A Critical Analysis Review. JBJS Rev 2016;4(1):e2. doi: 10.2106/jbjs.Rvw.O.00003. [DOI] [PubMed] [Google Scholar]
- 20.Konrad G, Audigé L, Lambert S, Hertel R, Südkamp NP. Similar outcomes for nail versus plate fixation of three-part proximal humeral fractures. Clin Orthop Relat Res. 2012;470(2):602-609. doi: 10.1007/s11999-011-2056-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blum J, Hansen M, Müller M, et al. Proximal humeral fractures and intramedullary nailing: experience with a new nail system. Eur J Trauma Emerg Surg. 2009;35(5):489-498. doi: 10.1007/s00068-009-8091-7. [DOI] [PubMed] [Google Scholar]
- 22.Lopiz Y, Garcia-Coiradas J, Garcia-Fernandez C, Marco F. Proximal humerus nailing: a randomized clinical trial between curvilinear and straight nails. J Shoulder Elbow Surg. 2014;23(3):369-376. doi: 10.1016/j.jse.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 23.Hessmann MH, Nijs S, Mittlmeier T, et al. Internal fixation of fractures of the proximal humerus with the multiLoc nail. Operat Orthop Traumatol. 2012;24(4-5):418-431. doi: 10.1007/s00064-011-0085-z. [DOI] [PubMed] [Google Scholar]
- 24.Zhao L, Qi YM, Yang L, et al. Comparison of the effects of proximal humeral internal locking system (PHILOS) alone and PHILOS combined with fibular allograft in the treatment of teer three‐ or four‐part proximal humerus fractures in the elderly. Orthop Surg. 2019;11(6):1003-1012. doi: 10.1111/os.12564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clavert P, Hatzidakis A, Boileau P. Anatomical and biomechanical evaluation of an intramedullary nail for fractures of proximal humerus fractures based on tuberosity fixation. Clin BioMech. 2016;32:108-112. doi: 10.1016/j.clinbiomech.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Günther C, Müller P, Mutschler W, Sprecher C, Milz S, Braunstein V. Straight proximal humeral nails are surrounded by more bone stock in comparison to bent nails in an experimental cadaveric study. Patient Saf Surg. 2014;8:18. doi: 10.1186/1754-9493-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Euler SA, Hengg C, Kolp D, Wambacher M, Kralinger F. Lack of fifth anchoring point and violation of the insertion of the rotator cuff during antegrade humeral nailing. Bone Joint J. 2014;96-b(2):249-253. doi: 10.1302/0301-620x.96b2.31293. [DOI] [PubMed] [Google Scholar]
- 28.Plath JE, Kerschbaum C, Seebauer T, et al. Locking nail versus locking plate for proximal humeral fracture fixation in an elderly population: a prospective randomised controlled trial. BMC Muscoskel Disord. 2019;20(1):20. doi: 10.1186/s12891-019-2399-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ge W, Sun Q, Li G, Lu G, Cai M, Li S. Efficacy comparison of intramedullary nails, locking plates and conservative treatment for displaced proximal humeral fractures in the elderly. Clin Interv Aging. 2017;12:2047-2054. doi: 10.2147/cia.S144084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rotman D, Efrima B, Yoselevski N, et al. Early displacement of two part proximal humerus fractures treated with intramedullary proximal humeral nail. J Orthop. 2020;19:59-62. doi: 10.1016/j.jor.2019.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehta S, Chin M, Sanville J, Namdari S, Hast MW. Calcar screw position in proximal humerus fracture fixation: don’t miss high! Injury. 2018;49(3):624-629. doi: 10.1016/j.injury.2018.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oppebøen S, Wikerøy AKB, Fuglesang HFS, Dolatowski FC, Randsborg P-H. Calcar screws and adequate reduction reduced the risk of fixation failure in proximal humeral fractures treated with a locking plate: 190 patients followed for a mean of 3 years. J Orthop Ourgery Res. 2018;13(1):197. doi: 10.1186/s13018-018-0906-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rothstock S, Plecko M, Kloub M, Schiuma D, Windolf M, Gueorguiev B. Biomechanical evaluation of two intramedullary nailing techniques with different locking options in a three-part fracture proximal humerus model. Clin BioMech. 2012;27(7):686-691. doi: 10.1016/j.clinbiomech.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 34.Shi X, Liu H, Xing R, et al. Effect of intramedullary nail and locking plate in the treatment of proximal humerus fracture: an update systematic review and meta-analysis. J Orthop Surg Res. 2019;14(1):285. doi: 10.1186/s13018-019-1345-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dilisio MF, Nowinski RJ, Hatzidakis AM, Fehringer EV. Intramedullary nailing of the proximal humerus: evolution, technique, and results. J Shoulder Elbow Surg. 2016;25(5):e130-e138. doi: 10.1016/j.jse.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 36.Fazal M, Baloch I, Ashwood N. Polarus nail fixation for proximal humeral fractures. J Orthop Surg. 2014;22(2):195-198. doi: 10.1177/230949901402200216. [DOI] [PubMed] [Google Scholar]
- 37.Brooks C, Revell W, Heatley F. A quantitative histological study of the vascularity of the rotator cuff tendon. J Bone Jt Surg Br Vol. 1992;74-B(1):151-153. doi: 10.1302/0301-620x.74b1.1732247. [DOI] [PubMed] [Google Scholar]
- 38.Wanzl M, Foehr P, Schreiber U, Burgkart RH, Lenich A. Biomechanical testing to evaluate the cut-through resistance of intramedullary nails for the proximal humerus. Injury. 2016;47(Suppl 7):S20-S24. doi: 10.1016/s0020-1383(16)30849-x. [DOI] [PubMed] [Google Scholar]