Abstract
Objectives:
Anemia is a common medical problem among pregnant women that will influence pregnancy and birth outcomes. In Ethiopia, there is a paucity of evidences regarding the problem among pregnant women admitted to labor ward. Therefore, the objective of this study was to assess the magnitude and factors associated with anemia among pregnant women admitted to labor ward for deliveries at Hiwot Fana Specialized University Hospital, Eastern Ethiopia.
Methods:
A cross-sectional study was conducted among 314 pregnant women admitted to labor ward at Hiwot Fana Specialized University Hospital in June 2020. Data were collected using an interviewer administered questionnaire and were entered into EpiData and analyzed using SPSS. Descriptive statistics and multiple logistic regression analysis were done to identify predictors of anemia.
Results:
In this study, the magnitude of anemia was 37.9% (95% confidence interval: 32.4, 43.0). Short birth interval (adjusted odds ratio = 2.5; 95% confidence interval: 1.02, 6.13), history of blood loss during pregnancy (adjusted odds ratio = 4.3; 95% confidence interval: 1.86, 9.9), less consumption of citrus fruit within a week (adjusted odds ratio = 2.9; 95% confidence interval: 1.2, 6.9), and meal frequency less than three times per day during pregnancy (adjusted odds ratio = 2.2; 95% confidence interval: 1.0, 4.6) were significantly associated with anemia, respectively.
Conclusion:
This study pointed out that more than one-third of pregnant women affected by anemia. Thus, interventions that could reduce anemia, such as counseling about increasing of meal frequency during pregnancy, foods rich in iron, and prevention and management of blood loss are recommended.
Keywords: Anemia, labor ward, pregnant women, associated factors, Eastern Ethiopia
Introduction
Anemia is a common medical problem in pregnancy in which the number of red blood cells or their oxygen carrying capacity is insufficient to meet physiologic needs.1 The cutoff values for defining anemia in pregnant women differ depending on the trimesters. In general, anemia is defined as a hemoglobin concentration level < 11 g/dL, the severity of anemia in pregnancy is classified based on the hemoglobin level as mild (10–10.9 g/dL), moderate when the hemoglobin level is between 7 and 9.9 g/dL, and severe (<7 g/dL).2,3 Globally, it is estimated that around 1.62 billion people are affected with anemia and among which 41.8% are pregnant women. In Africa, the problem is a bit excess, the prevalence rate among pregnant women population is 61.3%.3,4
Globally, nearly 510,000 maternal deaths occur yearly, and out of this anemia accounts 20% of maternal death; with majority of death occurred in developing countries.5 Anemia is a serious public health concern in this region and causes severe maternal and fetal abnormality consequences, such as low birth weight, premature delivery, low APGAR (Appearance (color), Pulse/heart rate, Grimace (response to stimulation, such as suctioning the baby’s nose), Activity/ muscle tone and Respiratory) score, mental impairment, and infant mortality.6–9 The study pointed out that 12% of low birth weight, 19% of preterm births, and 18% of prenatal mortality in low- and middle-income countries attributed to maternal deaths.10
In developing countries, the cause of anemia during pregnancy is multi-factorial and includes nutritional deficiencies of iron, folate, and vitamin B12 and also parasitic diseases. The relative contribution of each of these factors to anemia during pregnancy varies greatly by geographical location, season, and dietary practice. In sub-Saharan Africa, iron and folate deficiencies are the most common causes of anemia in pregnant women.5,6
The government of Ethiopia and stakeholders has launched different interventions to decrease the burden of anemia. These include, provision of iron and iron folate supplementations and advise on nutrition as routine services during antenatal care (ANC). However, significant changes have not yet been observed and anemia during pregnancy has remained a major public health problem. Besides, though, the health sector development program (HSDP)-IV target is planned to reduce the national prevalence of anemia to 12%, anemia is a significant problem affecting 22% of pregnant women.7
In Ethiopia, the prevalence of anemia among the reproductive aged women increased from 17%8 to 24% in 5 years.9 A systematic review and meta-analysis conducted among pregnant women in Ethiopia, reported the pooled prevalence of anemia as 31.66%.10 As to the knowledge of investigators concerned, there is a shortage of documented information on the same subject matter among women attending health facilities for labor. This is an indicative of the success of intervention during pregnancy, and would be a very good input in devising an appropriate plan to prevent the problem. This study tried to assess the magnitude and factors associated with anemia among pregnant women attending labor and delivery service at Hiwot Fana Specialized University Hospitals, Eastern Ethiopia.
Methods
Study area and period
The study was conducted from June 01 to 30/2020 at Hiwot Fana Specialized University Hospital (HFSUH) situated in the Harari regional state. Hiwot Fana Specialized University Hospital is one of the referral Hospitals at Harari regional state serving surrounding population estimated to be 5,800,000 people and area of East Hararghe Zone and some part of Somali region.
Study population and design
A cross-sectional study was conducted among pregnant women admitted to labor ward service during the study period. Women who visited the hospital who completed more than 28 weeks of gestation were included. The women who came with bleeding (postpartum hemorrhage), unable to communicate, and severely ill during the data collection period were excluded.
Sample size and sampling techniques
The required sample size for this study was determined using a single population proportion, with a prevalence of 27% from the previous study,11 with 0.05 of margin of error. Thus, the final sample size for this study was 314.
The previous 1-month clients’ flow to the health facilities for delivery service was reviewed from the registration book to estimate the expected number of women who will come for the delivery in the 1-month period. Individuals were selected using a systematic random sampling technique (every Kth, i.e., 2). And the first sample was selected by a lottery.
Data collection tools and procedures
The data were collected using a modified, semi-structured, and pre-tested questionnaire translated to Afaan Oromo and Amharic versions which were adapted from various published literatures.5,12,13 The wording and sequence of questions were designed in such a way that the sequence of ideas (from general to specific, and from easy to difficult questions) was maintained. The data related to that of women are collected during the intrapartum period, while the women are in relatively stable condition. The questionnaire consists of socio-demographic, obstetrics, and medication-related factors and lifestyle of participants, which includes smoking and meal frequency.
Blood specimen collection and examination
Blood samples were taken under strict aseptic conditions by senior laboratory technologists at HFSUH. The hemoglobin estimation was done using a HemoCue® B-Hemoglobin system. Pregnant women having Hb value below 11 g/dL were classified as anemic. Study participants with Hb value between 10 and 10.9 g/dL, 7–9.9 g/dl, and <7 g/dl were considered mild, moderate, and severe anemic, respectively.14 The hemoglobin records were finally adjusted for altitude.
Stool specimen collection and examination
Stool samples were collected from each study participant using clean, labeled, wide-mouthed, and leak-proof containers. Then, stool smears were prepared using physiological saline for direct microscopic detection and identification of eggs, cysts, and trophozoite stages of intestinal helminths and protozoans.
Pregnant woman height and weight were also measured on the same day of sample collection. Every height and weight measurements were performed two times; the mean values were used for body mass index (BMI) calculation.
The women were labeled as anemic when the hemoglobin (Hb) level is less than 11 g per deciliter.15
Five data collectors; three BSc degree holder midwifery professionals and two lab technicians were involved in the data collection and the data abstraction process.
Data quality control
The questionnaire was prepared in English and was translated into Amharic and Afaan Oromo for data collection and then re-translated back to English by language experts. Two days’ training was provided to the data collectors and supervisors on the data collection tools and the data collection procedures. Then, the questionnaire was pre-tested on 5% of the sample size in another nearby hospital to ensure its validity. Data collectors were closely supervised by the supervisors and the principal investigator. Data consistency was checked through completeness of the questionnaires and double data entry was also performed.
Data processing and analysis
Data were coded, cleaned, edited, and entered into EPI data to minimize logical errors and design skipping patterns. Then, the data were exported to SPSS window for data analysis. Descriptive analysis was also done by computing proportions and summary statistics. Then, the information was presented using simple frequencies, summary measures, tables, and figures.
Bi-variate crude and adjusted analyses were done to see the association between each independent variable with outcome variables using logistic regression. The assumption of logistic regression was checked. The goodness of fit was checked by Hosmer–Lemeshow statistic and omnibus tests. All variables with p < 0.25 in the bi-variate analysis were included in the final model to control for confounders. Multi-collinearity test was carried out using standard error, and collinearity statistics (variance inflation factors > 10 and standard error > 2) was considered as suggestive of the existence of multi-collinearity. The direction and statistical association were measured by odd ratio with 95% confidence interval (CI). Adjusted odds ratio along with 95% CI was estimated to identify predictors of anemia using adjusted analysis, and p value < 0.05 were considered to declare a statistically significant.
Ethical consideration
The study was approved by the Institutional Health Research Ethics Review Committee at the College of Health and Medical Sciences, Haramaya University. An informed written voluntary signed consent was obtained from each participating mothers and heads of the hospital. Confidentiality was maintained using identification numbers instead of individual names. The risk and benefits of participating in the study were discussed. Participants were informed about the rights to terminate participating in the research at any time of the study.
Results
Socio-demographic characteristics of the study participants
Among a total of 333 pregnant women, 314 respondents enrolled in the study giving a response rate of 94.3%. The mean age of the respondent was 26 (±2.15) years. The majority (58.9%) of the respondents were from rural areas. Almost half (44.9%) of the respondent were unable to read and write, and majority (78.7%) of the respondents were Muslim by religion, and 99.7% were married. The median household income of the respondents was 3000 ETB which ranges from 200 to 20,000 ETB (Table 1).
Table 1.
Socio-economic and demographic characteristics of pregnant women admitted to the labor ward of HFSUH, 2020 (N = 314).
| Variables | Category | Frequency | (%) |
|---|---|---|---|
| Age (in years) | 18–25 | 142 | 45.2 |
| 26–35 | 158 | 50.3 | |
| ⩾36 | 14 | 4.5 | |
| Current marital status | Married | 313 | 99.7 |
| Unmarried | 1 | 0.3 | |
| Educational status | Unable to read and write | 141 | 44.9 |
| Able to read | 58 | 18.5 | |
| Primary | 48 | 15.3 | |
| Secondary | 29 | 9.2 | |
| College and above | 38 | 12.1 | |
| Religion | Orthodox | 33 | 10.5 |
| Muslim | 247 | 78.7 | |
| Protestant | 34 | 10.8 | |
| Occupation | Housewife | 245 | 78.0 |
| Government employee | 20 | 6.4 | |
| Private | 4 | 1.3 | |
| Daily laborer | 12 | 3.8 | |
| Farmer | 21 | 6.7 | |
| Merchant | 12 | 3.8 | |
| Family monthly income (ETB) | ⩽2000 | 123 | 39.1 |
| 2100–10,000 | 182 | 58.0 | |
| >10,000 | 9 | 2.9 | |
| Place of residences | Urban | 129 | 41.1 |
| Rural | 185 | 58.9 | |
| Age at first marriage (in years) | ⩽18 | 67 | 21.3 |
| 19–25 | 217 | 69.1 | |
| ⩾26 | 30 | 9.6 |
HFSUH: Hiwot Fana Specialized University Hospital.
Obstetric and medical characteristics
Among the study participants, 58.9% of them had at least one ANC visit, and half of these, 50.3%, reported for receiving iron supplementation during the current pregnancy. More than half, 69.4%, reported they had no experience of taking contraception before the current pregnancy (Table 2).
Table 2.
Obstetric and reproductive health profile of pregnant women admitted to the labor ward of HFSUH, 2020 (N = 314).
| Variable | Category | Frequency | (%) |
|---|---|---|---|
| ANC follow up | No | 129 | 41.1 |
| Yes | 185 | 58.9 | |
| Iron folic acid supplementation | No | 156 | 49.7 |
| Yes | 158 | 50.3 | |
| Parity | Primigravida | 0 | 0 |
| Multigravida | 314 | 100 | |
| Birth interval | ⩽2 year | 154 | 49 |
| >2 year | 160 | 51 | |
| Blood loss during pregnancy (APH) | No | 256 | 81.5 |
| Yes | 58 | 18.5 | |
| MUAC | <23 | 142 | 45.2 |
| ⩾23 | 172 | 54.8 | |
| BMI | Underweight | 13 | 4.1 |
| Normal | 228 | 72.6 | |
| Overweight | 73 | 23.2 | |
| Abortion | No | 229 | 72.9 |
| Yes | 85 | 27.1 | |
| Hypertension | No | 303 | 96.5 |
| Yes | 11 | 3.5 | |
| Diabetes mellitus | No | 313 | 99.7 |
| Yes | 1 | 0.3 | |
| IUFD | No | 301 | 95.9 |
| Yes | 13 | 4.1 |
HFSUH: Hiwot Fana Specialized University Hospital; ANC: antenatal care; MUAC: mid-upper arm circumference; BMI: body max index; IUFD: intrauterine fetal death.
Dietary and lifestyle characteristics
A 7-day food consumption score indicated that 24.5% of the mothers reported to consume meat, from these, six of them consumed more than three times in a week. More than 95% (300) reported to consume dark-green leafy vegetables, and of these, 223 (71.0%) ate below three times per week. Only two participants ate chicken in the past 7 days. Among all the respondents, 302 (96.2%) of them reported eating cereals in the past 7 days. A third of respondents (29.2%) chew khat in the past 3 months, and 6.7% of them reported to be infected with intestinal parasites which majority of them infected by hookworm, 17 (5.4%). Close to half (55.7%) had food 1–3 times per day. Similarly, nearly half, 55.4%, of the study participants reported taking coffee after meal. Daily consumption of tea after meals was experienced by 25.2% of the respondent (Table 3).
Table 3.
Distribution of dietary and life style–related factor among pregnant women admitted to the labor ward of HFSUH, 2020 (N = 314).
| Variable | Category | Frequency | (%) |
|---|---|---|---|
| Eating dark green in a week | 1–3 times | 223 | 71.0 |
| >3 times | 91 | 29.0 | |
| Eating cabbage in a week | 1–3 times | 167 | 53.2 |
| >3 times | 147 | 46.8 | |
| Eating liver in a week | 1–3 times | 16 | 99.7 |
| >3 times | 1 | 0.3 | |
| Eating bean in a week | 1–3 times | 202 | 68.2 |
| >3 times | 100 | 31.8 | |
| Eating citrus fruit | 1–3 times | 243 | 77.4 |
| >3 times | 71 | 22.6 | |
| Eating vegetable in a week | 1–3 times | 267 | 85 |
| >3 times | 47 | 15 | |
| Eating Cereal in a week | 1–3 times | 151 | 48. |
| >3 times | 163 | 51.9 | |
| Khat chewing | No | 220 | 70.1 |
| Yes | 94 | 29.9 | |
| Alcohol drink | No | 311 | 99 |
| Yes | 3 | 1 | |
| Frequency of meals per day | 1–3 times | 175 | 55.7 |
| >3 times | 139 | 44.3 | |
| Special drink after meals | Milk | 61 | 19.4 |
| Coffee | 174 | 55.4 | |
| Milk with tea | 79 | 25.2 | |
| Frequency of special drink after meals | 1–2 cup of coffee | 74 | 23.7 |
| >3 cup of coffee | 100 | 31.3 |
HFSUH: Hiwot Fana Specialized University Hospital.
Magnitude of anemia
In this study, the overall magnitude of anemia was 37.9 % with 95% CI: 32.4, 43.0. Of this 18.5%, 12.5%, and 6.9% had mild, moderate, and severe anemia, respectively (Figure 1).
Figure 1.
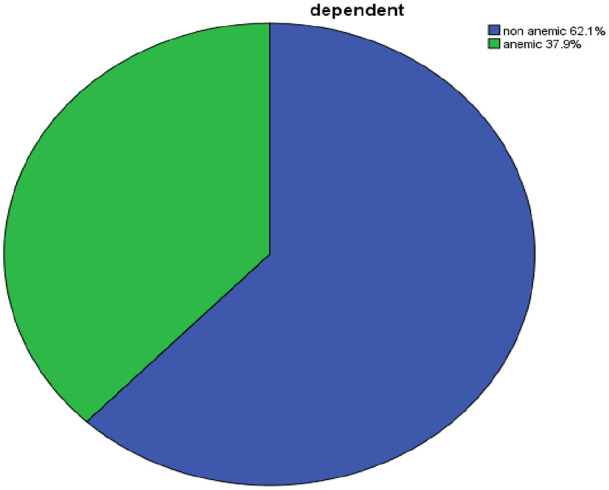
Prevalence of anemia and associated factors among pregnant women admitted to the labor ward of HFSUH, 2020, (n = 314) 4.6.
Anemia and its associated factors
In bi-variate analysis, occupation, educational status, marital status, ANC visit, birth interval, history of contraceptive use, IFA supplementation, blood loss in the current pregnancy, khat chewing, drinking alcohol, eating leafy vegetables, MUAC, hypertension, citrus fruit intake, drinking milk with tea after meals, and meal frequency per day were significantly associated with anemia among pregnant women. But, in the multivariable logistic regression, short birth interval, blood loss, citrus fruit intake, and frequency of meals were factors significantly associated with anemia.
Women whose birth intervals less than or equal to 2 years were 2.5 times more likely to be anemic than their counterparts (adjusted odds ratio (AOR) = 2.5; 95% CI: 1.02, 6.13). Pregnant women who experienced blood loss in current pregnancy were 4.3 times more likely to develop anemia than their counterparts (AOR = 4.3; 95% CI: 1.86, 9.9). Pregnant women who eat citrus fruit less than three times in a week were more likely to have anemia than those who eat more that three times in a week (AOR = 2.9; 95% CI: 1.2, 6.9). Pregnant women who had meal frequency of less than three times per day were more likely to be anemic than their counterparts (AOR: 3.9; 95% CI: 1.69, 8.97) (Table 4).
Table 4.
Factors associated with anemia among pregnant women admitted to labor wards of HFSUH, 2020 (N = 314).
| Variable | Category | Anemia |
COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Yes, n (%) | No, n (%) | ||||
| Residences | Urban | 24 (18.7) | 105 (81.3) | 1 | 1 |
| Rural | 95 (51.3) | 90 (48.7) | 4.6 (2.7, 7.8) | 1.6 (0.6, 4.6) | |
| Abortion | No | 73 (31.8) | 156 (68.2) | 1 | 1 |
| Yes | 46 (54.1) | 39 (45.9) | 2.5 (1.5, 4.1) | 0.6 (0.3, 1.3) | |
| ANC | No | 66 (51.1) | 63 (48.9) | 0.4 (0.24, 0.61) | 1.1 (0.4, 3.3) |
| Yes | 53 (28.6) | 132 (71.4) | 1 | 1 | |
| MUAC | <23 | 76 (53.5) | 66 (46.5) | 3.4 (2.1, 5.6) | 1.3 (0.9, 3.4) |
| ⩾23 | 43 (25) | 129 (75) | 1 | 1 | |
| BMI | Underweight | 5 (38.4) | 8 (61.6) | 0.6 (0.4, 1.0) | 1.5 (0.7, 6.1) |
| Normal | 94 (41.2) | 134 (58.8) | 1 | 1.6 (0.3, 8.3) | |
| Overweight | 20 (27.3) | 53 (72.7) | 1 | 1 | |
| Contraceptive | No | 89 (40.8) | 129 (59.2) | 1.72 (1.02, 2.8) | 0.6 (0.28, 1.4) |
| Yes | 30 (31.2) | 66 (68.7) | 1 | 1 | |
| Gravida | ⩽3 | 60 (30.1) | 139 (69.9) | 1.8 (1.3, 2.4) | 0.6 (0.2, 1.6) |
| 4–6 | 29 (45.3) | 35 (54.7) | 1 | 1 | |
| ⩾7 | 30 (58.8) | 21 (41.2) | 1 | 1 | |
| Blood loss during pregnancy | No | 81 (31.6) | 175 (68.4) | 1 | 1 |
| Yes | 38 (65.5) | 20 (34.5) | 4.1 (2.2, 7.4) | 4.3 (1.9, 9.9) | |
| Birth interval | ⩽2 year | 79 (51.2) | 75 (48.8) | 0.3 (0.19, 0.51) | 2.5 (1.02, 6.13) |
| >2 year | 40 (25) | 120 (75) | 1 | 1 | |
| Frequency of eating citrus fruit/week | 1–3 times | 86 (35.3) | 157 (64.7) | 0.29 (0.14, 0.59) | 2.9 (1.2, 6.9) |
| >3 times | 33 (46.4) | 38 (53.6) | 1 | 1 | |
| Meal frequency/week | 1–3 times | 91 (48) | 84 (52) | 0.23 (0.14, 0.38) | 2.2 (1.0, 4.6) |
| >3 times | 28 (20.1) | 111 (79.9) | 1 | 1 | |
HFSUH: Hiwot Fana Specialized University Hospital; COR: crude odds ratio; CI: confidence interval; AOR: adjusted odds ratio; ANC: antenatal care; MUAC: Mid-Upper Arm Circumference; BMI: body max index.
Discussion
The overall magnitude of anemia in this study was 37.9% (95% CI: 32.4, 43.0). According to the WHO classification of the public health importance,16 anemia was moderate public health problems in our study area. The magnitude of anemia in this study was in harmony with a study done in West Arsi Zone of Ethiopia (36.6%),17 India (33%),18 North west Ethiopia 30%,19 North Western Zone of Tigray, (36.1%),4 and Gamo Gofa zone of Ethiopia (32.8%).20 In contrast to this, our finding was higher compared to a study conducted in Illu aba bora (31%), Ethiopia, India (29.9%), Gonder (25%), and from finding of EDHS 2016 (24%),18,21–23 respectively. Our finding was lower than the study conducted in Eastern Ethiopia 56.8%.24 This discrepancy might be due to socio-economical, seasonal, dietary, and health-seeking behavior across the different culture.25
Pregnant women with history of blood loss during pregnancy were more likely to experience anemia than their counterparts. This was in line with the study conducted Mekele, North Ethiopia.26 This is due to the fact that having blood loss during pregnancy leads to decrement of red blood cell volume, which in turn significantly contributes to reduction of hemoglobin that plays a vital role in carrying oxygen from the lungs to the rest of the body.27
This study has shown that there was a statistically significant association between frequency of feeding more than three times a day and anemia. This finding was also documented in other studies.4,17,28 This might be due to the fact that pregnancy is a special period with increased energy and nutrient requirement that can be fulfilled by increased meal frequency. Poor dietary intake during pregnancy causes deficiency of mineral and vitamin.
Moreover, this study showed that pregnant women with short inter-pregnancy interval was another important statistically significant factor associated with anemia. This finding was consistent with a study conducted in Pakistan29 and Saudi Arabia.30 The reason behind this could be the short inter-pregnancy interval to relate with adverse pregnancy maternal outcome such as anemia. This could be explained as insufficient time for the mother to recover from the nutritional burden and stress of the previous pregnancy.31
In addition, pregnant women who had a habit of eating less citrus fruit were more likely to experience anemia than their counterparts. This was in agreement with finding from west Arsi zone.17 This is due to the fact that citrus fruit is one of the ingredients for the production of non-heme iron and is the main (90%–95%) source of dietary iron.32
Strength and limitation of the study
The strength of this study, in addition to its primary nature, is the determination of hemoglobin level and stool examination of clients in spite of recorded previous test report in the medical records of the women. This has given an opportunity to validate the result.
The limitation of this study is, it was difficult to account for other unknown factors associated with anemia like genetic disorders. Some of the study participants did not accurately recall what they ate in the past 1 week, and this has affected the results from the week of food frequency. In addition to this, it is difficult to change food into portion size. Variables such as meal frequency and life style were prone to social desirability bias.
Conclusion
The prevalence of anemia among pregnant women admitted to labor ward is high. Although, the condition appears a moderate as per WHO criteria, awareness creation on prevention, and also the use of contraceptives to widen the inter-pregnancy interval is important to further prevent pregnancy-related anemia. Health education on creating awareness on maternal nutrition based on the portion size, food type, and nutritional content of food during pregnancy should be emphasized during ANC.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211047389 for Magnitude and factors associated with anemia among pregnant women admitted to labor ward of Hiwot Fana Specialized University Hospital, Eastern Ethiopia by Serkalem Abdu, Tilahun Ali, Adera Debella, Nega Assefa and Kedir Teji Roba in SAGE Open Medicine
Acknowledgments
The authors would like to acknowledge HFSUH for making this research a success. They also appreciate the study participants for their cooperation in providing the necessary information.
Footnotes
Author contributions: S.A., T.A., A.D., N.A., and K.T.R. were involved in the conception and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising the article, agreed to submit to the current journal, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The study was approved by Institutional Health Research Ethics Review Committee at the College of Health and Medical Science, Haramaya University (Ref. No: IHRERC/113/2020).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects or their legally authorized representatives before the study.
ORCID iDs: Tilahun Ali  https://orcid.org/0000-0003-0523-8336
https://orcid.org/0000-0003-0523-8336
Nega Assefa  https://orcid.org/0000-0003-0341-2329
https://orcid.org/0000-0003-0341-2329
Supplemental material: Supplemental material for this article is available online.
References
- 1.World Health Organization. Iron deficiency anaemia: assessment, prevention and control. Geneva: World Health Organization, 2001. [Google Scholar]
- 2.Puolakka J, Janne O, Pakarinen A, et al. Serum ferritin as a measure of iron stores during and after normal pregnancy with and without iron supplements. Acta Obstet Gynecol Scand Supp 2000; 95(12): 43–51. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Worldwide prevalence of anaemia 1993-2005: WHO global database on anaemia. Geneva: World Health Organization, 2008. [Google Scholar]
- 4.Gebre A, Mulugeta A. Prevalence of anemia and associated factors among pregnant women in North Western zone of Tigray, Northern Ethiopia: a cross-sectional study. J Nutr Metab 2015; 2015: 165430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Getahun W, Belachew T, Wolide AD. Burden and associated factors of anemia among pregnant women attending antenatal care in southern Ethiopia: cross sectional study. BMC Res Notes 2017; 10(1): 276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeMaeyer E, Adiels-Tegman M. The prevalence of anaemia in the world. World Health Stat Q 1985; 38(3): 302–316. [PubMed] [Google Scholar]
- 7.Jennings J, Hirbaye M. Review of incorporation of essential nutrition actions into public health programs in Ethiopia. Washington, DC: The Food and Nutrition Technical Assistance Project (FANTA) Equinet Newsletter, 2008, pp. 1–25. [Google Scholar]
- 8.Central Statistical Agency [Ethiopia] and ICF International. Ethiopia demographic and health survey 2011. Addis Ababa, Ethiopia; Calverton, MD: Central Statistics Agency and ICF International, 2012. [Google Scholar]
- 9.Central Statistical Agency—CSA/Ethiopia I. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia: CSA and ICF, 2016. [Google Scholar]
- 10.Kassa GM, Muche AA, Berhe AK, et al. Prevalence and determinants of anemia among pregnant women in Ethiopia; a systematic review and meta-analysis. BMC Hematol 2017; 17: 17–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kefiyalew F, Zemene E, Asres Y, et al. Anemia among pregnant women in Southeast Ethiopia: prevalence, severity and associated risk factors. BMC Res Notes 2014; 7(1): 771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta A. Prevalence of maternal anemia and its impact on perinatal outcome in a rural area of Dakshina Kannada. Int J Med Sci Public Health 2017; 6(7): 1209–1213. [Google Scholar]
- 13.Getachew M, Yewhalaw D, Tafess K, et al. Anaemia and associated risk factors among pregnant women in Gilgel Gibe dam area, southwest Ethiopia. Parasit Vectors BMC Res Notes 2012; 5(1): 296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva: World Health Organization, 2011. [Google Scholar]
- 15.WHO. World health statistics 2015. Geneva: World Health Organization, 2015. [Google Scholar]
- 16.De Benoist B, Cogswell M, Egli I, et al. Worldwide prevalence of anaemia 1993-2005; WHO global database of anaemia. Geneva: World Health Organization, 2008. [Google Scholar]
- 17.Obse N, Mossie A, Gobena T. Magnitude of anemia and associated risk factors among pregnant women attending antenatal care in Shalla Woreda, West Arsi Zone, Oromia Region, Ethiopia. Ethiop J Health Sci 2013; 23(2): 165–173. [PMC free article] [PubMed] [Google Scholar]
- 18.Vindhya J, Nath A, Murthy GVS, et al. Prevalence and risk factors of anemia among pregnant women attending a public-sector hospital in Bangalore, South India. J Family Med Prim Care 2019; 8(1): 37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Derso T, Abera Z, Tariku A. Magnitude and associated factors of anemia among pregnant women in Dera District: a cross-sectional study in northwest Ethiopia. BMC Res Notes 2017; 10(1): 359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bekele A, Tilahun M, Mekuria A. Prevalence of anemia and its associated factors among pregnant women attending antenatal care in health institutions of Arba Minch Town, Gamo Gofa Zone, Ethiopia: a cross-sectional study. Anemia 2016; 2016: 1073192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kenea A, Negash E, Bacha L, et al. Magnitude of anemia and associated factors among pregnant women attending antenatal care in public hospitals of Ilu Abba Bora Zone, South West Ethiopia: a cross-sectional study. Anemia 2018; 2018: 9201383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Enawgaw B, Birhanie M, Terefe B, et al. Prevalence of anemia and iron deficiency among pregnant women attending antenatal care service at University of Gondar Hospital, Northwest Ethiopia. Clin Lab 2019; 65(4). [DOI] [PubMed] [Google Scholar]
- 23.EDHS. Ethiopian demographic and health survey 2016, 2016, https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf
- 24.Addis Alene K, Mohamed Dohe A. Prevalence of anemia and associated factors among pregnant women in an urban area of Eastern Ethiopia. Anemia 2014; 2014: 561567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu Y, Ye H, Liu J, et al. Prevalence of anemia and sociodemographic characteristics among pregnant and non-pregnant women in southwest China: a longitudinal observational study. BMC Pregnancy Childbirth 2020; 20(1): 535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ebuy Y, Alemayehu M, Mitiku M, et al. Determinants of severe anemia among laboring mothers in Mekelle city public hospitals, Tigray region, Ethiopia. PLoS ONE 2017; 12(11): e0186724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Talaulikar VS. Anemia in pregnancy. London: University College Hospital, 2014. [Google Scholar]
- 28.Jufar AH, Zewde T. Prevalence of anemia among pregnant women attending antenatal care at Tikur Anbessa Specialized Hospital, Addis Ababa Ethiopia. J Hematol Thromb Dis 2014; 2(1): 1000125. [Google Scholar]
- 29.Noor T, Maheen E, Latif F. Association of short interpregnancy interval (IPI) with maternal anemia at a tertiary care hospital. J Med Physiol Biophys 2018; 40: 36–39. [Google Scholar]
- 30.Abdelhafez AM, El-Soadaa SS. Prevalence and risk factors of anemia among a sample of pregnant females attending primary health care centers in Makkah, Saudi Arabia. Pak J Nutr 2012; 11(12): 1113. [Google Scholar]
- 31.Howard EJ, Harville E, Kissinger P, et al. The association between short interpregnancy interval and preterm birth in Louisiana: a comparison of methods. Matern Child Health J 2013; 17(5): 933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diamond-Smith NG, Gupta M, Kaur M, et al. Determinants of persistent anemia in poor, urban pregnant women of Chandigarh city, North India: a mixed method approach. Food Nutr Bull 2016; 37(2): 132–143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211047389 for Magnitude and factors associated with anemia among pregnant women admitted to labor ward of Hiwot Fana Specialized University Hospital, Eastern Ethiopia by Serkalem Abdu, Tilahun Ali, Adera Debella, Nega Assefa and Kedir Teji Roba in SAGE Open Medicine


