Abstract
Multiple health behaviors could have greater impact on chronic diseases than single behaviors, but correlates of behavioral clusters are relatively understudied. Using data from NIH-AARP Diet and Health Study (initiated in 1995) for 324,522 participants from the U.S. (age 50–71), we conducted exploratory factor analysis to identify clusters of adherence to eight cancer prevention behaviors. Poisson regressions examined associations between cluster scores and neighborhood socioeconomic deprivation, measured with census block group (1) poverty and (2) low education. Four clusters emerged: Movement (adequate physical activity/less TV); Abstinence (never smoked/less alcohol); Weight control (healthy body mass index/high fruits and vegetables); and Other (adequate sleep/receiving cancer screenings). Scores on all clusters were lower for participants in neighborhoods with the highest poverty (most deprived quintile versus least deprived: relative risk [RR]=0.95 (95% confidence interval[CI]=0.94–0.96) for Movement, 0.98 (95% CI=0.97–0.99) for Abstinence, 0.94 (95% CI=0.92–0.95) for Weight control, and 0.94 (95% CI=0.93–0.95) for Other; all p<.001). Scores on three clusters were lower for participants in neighborhoods with the lowest education (RR=0.88 (95% CI=0.87–0.89) for Movement, 0.89 (95% CI=0.88–0.90) for Weight control, and 0.90 (95% CI=0.89–0.91) for Other; all p<.001). Health behaviors among older adults demonstrated four clusters. Neighborhood deprivation was associated with lower scores on clusters, suggesting that interventions to reduce concentrated deprivation may be an efficient approach for improving multiple behaviors simultaneously.
Keywords: Cancer, cancer prevention, multiple health behaviors, area socioeconomic status, socioeconomic deprivation, older adults
The National Cancer Institute estimated that the 2016 cancer incidence rate was 454 per 100,000 people per year (Howlader et al., 2016) in the United States. Many of these cases will be detected in adults ages 65 years of older (Howlader et al., 2016). However, up to 50% of cancer cases could be prevented through behavior change (Song and Giovannucci, 2016), including avoiding smoking, limiting alcohol use, consuming a healthy diet, and maintaining a physically active lifestyle.
Many Americans fail to meet these guidelines and remain at excess risk of cancer (Kabat et al., 2015; Song and Giovannucci, 2016; Warren Andersen et al., 2016). Epidemiologic research has evaluated correlates of cancer prevention behaviors, finding consistent differences by factors such as race/ethnicity (Wang and Beydoun, 2007; Williams and Collins, 1995) and individual- or area-level socioeconomic status (Braveman et al., 2010; Wang and Beydoun, 2007; Williams and Collins, 1995). Less research has examined how behaviors overlap with one another, but evidence suggests that individuals who engage in one prevention behavior are more likely to engage in others (Berrigan et al., 2003; Kabat et al., 2015; Patterson et al., 1994; Pronk et al., 2004). For example, individuals who routinely consume high numbers of fruits and vegetables are more likely to be physically active and individuals who smoke are more likely to be heavy drinkers (Berrigan et al., 2003; Patterson et al., 1994). To date, most research on clusters of health behaviors have focused on individual-level correlates, with less analysis of area-level correlates.
Intervening to affect overlapping clusters of health behaviors may be more efficient than single-behavior interventions for resource allocation and impact on public health (Noar et al., 2008; Prochaska et al., 2008). A better understanding of the prevalence of these clusters as well as their individual- and area-level correlates could inform interventions aiming to change multiple health behaviors with the goal of reducing cancer risk.
In this study, we leveraged data from a cohort study including more than half a million participants, the National Institutes of Health (NIH)-AARP Diet and Health Study (Schatzkin et al., 2001) (formerly, the American Association of Retired Persons (AARP)), to understand the epidemiology of clusters of health behaviors related to cancer risk, examining intrapersonal and neighborhood correlates of these clusters. The findings from this analysis could inform future interventions aiming to improve cancer prevention behaviors among middle-aged and older adults.
Methods
Data source
The NIH-AARP Diet and Health Study is a prospective study of individuals who were members of AARP, focusing on the relationship between dietary factors and health among middle-aged and older adults (Schatzkin et al., 2001). Eligible participants were ages 50–71 years (selected to optimize analysis of cancer outcomes) and lived in selected states and metropolitan areas (California; Florida; Pennsylvania; New Jersey; North Carolina; Louisiana; Atlanta, Georgia; or Detroit, Michigan). In 1995–1996, NIH-AARP sent baseline questionnaires (primarily asking about diet and lifestyle factors related to health) to 3.5 million AARP members, and 567,169 eligible participants returned completed questionnaires (~18% response rate). In 1996–1997, NIH-AARP sent additional questionnaires focused on risk behaviors to the baseline cohort. Data collection for NIH-AARP was approved by the institutional review board of the National Cancer Institute. More details on the design and administration of NIH-AARP are available (Schatzkin et al., 2001).
Analytic Sample
The current analysis draws upon data from participants who completed both the baseline and risk factor questionnaires (n=334,921). Additional exclusion criteria included having a proxy respondent on either questionnaire (i.e., if another person filled out the questionnaire on behalf of the participant), not providing an address at baseline, and having a cancer diagnosed before completing the baseline questionnaire. Thus, the analytic sample comprised 324,522 participants.
Measures
Cancer prevention behaviors.
Behavioral variables of interest in the present study included adherence or non-adherence to several guidelines from national organizations (when available) or recent scientific research about cancer risk reduction (Song and Giovannucci, 2016). We created dichotomous indicators of whether participants had never smoked (U. S. Department of Health Human Services, 2014); had a body mass index (BMI) of <25kg/m2 at baseline (NHLBI Obesity Education Initiative, 2010); consumed ≥2 fruits and 3 vegetables per day (Department of Health and Human Services, 2015); engaged in ≥60 minutes of physical activity per week (Office of Disease Prevention and Health Promotion, 2008); consumed ≤2 servings of alcohol per day (Department of Health and Human Services, 2015); slept ≥7 hours per night (Office of Disease Prevention and Health Promotion, 2018); spent ≤2 hours per day watching television (Keadle et al., 2015; Matthews et al., 2008; Patel et al., 2010); and had received selected cancer screenings in the past 3 years (males: received screenings for colorectal and prostate cancer; females: received screenings for colorectal, breast, and ovarian cancer) (Centers for Disease Control and Prevention, 2012). Complete details about item wording are available through the NIH-AARP Diet and Health Study website (www.dietandhealth.cancer.gov). Each variable was coded such that 1 indicated that the participant engaged in the behavior and 0 indicated that the participant had not engaged in the behavior.
Socioeconomic factors.
Each participant’s residential address at baseline was linked to census block groups (99% of participants in the analytic sample were matched), which we used as a proxy for participants’ neighborhood. Using data from the 2000 U.S. Census, neighborhood socioeconomic deprivation was estimated with two measures (Krieger et al., 2002): (1) the percent of residents (all ages) in each census block group living below the federal poverty line, and (2) the percent of adults (ages 18+ years) in each census block group with less than a high school degree. Data were divided into quintiles based on the distribution of the sample, with 20% of participants in each quintile. Quintiles were scored such that the first quintile was the least socioeconomically deprived while the fifth quintile was the most deprived.
Covariates.
We controlled for individual-level sociodemographic and health information. Sociodemographic covariates were sex (male or female); age category at baseline (<65 years or 65+ years); race/ethnicity (non-Hispanic white or other, due to small sample sizes in the non-white categories (Schatzkin et al., 2001)); marital status (married/living as married or other); and educational attainment (high school degree or less, or more than high school degree). We used self-reported health status (less than very good, or excellent or very good) to summarize baseline health.
Statistical analysis
First, we conducted a descriptive analysis of participants’ health behaviors. We estimated the prevalence of engaging in each behavior and generated a phi correlation matrix of the correlations among each pair of behaviors (Stokes et al., 2012). The phi correlation coefficient summarizes correlations between dichotomous variables and theoretically ranges from −1 to +1. Then, we conducted an exploratory factor analysis to determine which behaviors clustered together. Specifically, we implemented a principal component analysis with an oblique promax rotation (Kim and Mueller, 1978) for all eight behaviors. We retained factors with eigenvalues greater than 1 (n=4) and examined which factor each of the behaviors loaded on most strongly. We created factor scores by summing (with equal weights) participants’ responses on the behaviors that loaded on each factor. We examined the associations between scores on each factor and the socioeconomic factors and covariates by conducting chi-square tests.
Next, we examined the associations between neighborhood socioeconomic deprivation and scores on the factors. Using multivariable Poisson regression to model the “count” scores on each factor, we modeled the association between participants’ poverty or education quintile and each health behavior score, adjusting for covariates. We had greater than 90% power to detect an association between neighborhood SES quintile and the dependent variables, assuming an alpha of .05 and based on the observed distribution of health behavior factors scores.
Finally, we examined the cross-level interactions between socioeconomic deprivation and covariates with health behavior scores. We repeated the Poisson regressions with multiplicative interaction terms for the product of neighborhood poverty or education quintile and each covariate. Wald chi-square tests analyzed whether each interactions term contributed significantly to the model. If so, we probed the interactions by stratifying models across levels of the covariates.
Supplementary analyses included alternate combinations of behaviors. We examined the associations between neighborhood socioeconomic deprivation and (1) an a priori factor summing participants’ scores on four behavioral recommendations from the American Cancer Society (ACS) (Kabat et al., 2015; Kushi et al., 2012) (having a healthy BMI, engaging in frequent physical activity, high fruit and vegetable consumption, and low alcohol consumption) and (2) an additive index of all eight health behaviors. In addition, we examined the associations between neighborhood poverty and education (simultaneously) with health behavior scores. All analyses were conducted using SAS version 9.3 (Cary, NC). Statistical tests used a two-sided p value of .05. The present analysis was approved by the NIH-AARP Diet and Health Study Steering Committee.
Results
Of 324,522 participants, 58.0% were male and 42.0% were female. Most participants were non-Hispanic white (92.5%) and had attained more than a high school degree (64.1%).
Engagement in prevention behaviors ranged from 35.1% (low television watching) to 88.6% (low alcohol consumption) (Table 1), and almost all behaviors were significantly correlated with each other. Only four pairs of behaviors had phi coefficients ≥0.100: never smoked with low alcohol consumption (φ=0.136); healthy BMI with high physical activity (φ=0.103); healthy BMI with low television watching (φ=0.107); and high fruit and vegetable consumption with high physical activity (φ=0.135) (all p<.001) (Table 1).
Table 1.
Prevalence of and phi correlations among health behaviors of NIH-AARP participants.
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| φ | p | φ | p | φ | p | φ | p | φ | p | φ | p | φ | p | ||
| (1) Never smoked | 36.7 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| (2) Healthy BMI | 37.0 | 0.047 | *** | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| (3) High F&V consumption | 42.3 | 0.056 | *** | 0.006 | ** | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| (4) High physical activity | 47.4 | 0.017 | *** | 0.103 | *** | 0.135 | *** | -- | -- | -- | -- | -- | -- | -- | -- |
| (5) Low alcohol consumption | 88.6 | 0.136 | *** | 0.006 | *** | 0.027 | *** | −0.011 | *** | -- | -- | -- | -- | -- | -- |
| (6) 7+ hours sleep/night | 65.3 | 0.004 | * | 0.048 | *** | 0.000 | 0.033 | *** | −0.048 | *** | -- | -- | -- | -- | |
| (7) Low TV watching | 35.1 | 0.083 | *** | 0.107 | *** | 0.048 | *** | 0.073 | *** | 0.010 | *** | 0.035 | *** | -- | -- |
| (8) All recent screenings | 65.8 | −0.002 | −0.011 | *** | 0.044 | *** | 0.066 | *** | −0.005 | ** | 0.033 | *** | 0.032 | *** | |
Note. Boldface indicates correlation magnitude greater than 0.10. BMI=body mass index; F&V=fruit and vegetable; TV=television.
p<.05;
p<.01;
p<.001.
Health behavior factor analysis
Four health behavior factors emerged. Two health behaviors loaded on the first factor, which we described as “Movement”: high physical activity (standardized factor loading=0.56) and low television watching (loading=0.52). Two behaviors loaded on the second factor, “Abstinence”: never smoked (loading=0.57) and low alcohol consumption (loading=0.70). Two behaviors loaded on the third factor, “Weight control”: healthy BMI (loading=−0.53) and high fruit and vegetable consumption (loading=0.55). Finally, two behaviors loaded on the fourth factor, “Other”: adequate sleep (loading=0.57) and received all recent cancer screenings (loading=0.60) (for all factor loadings, see Supplementary Table S1).
Overall, 19% of the sample scored the maximum (2) on Movement; 35% of the sample scored the maximum on Abstinence; 16% on Weight control; and 44% on Other (Table 2). The mean scores were 0.83 for Movement, 1.25 for Abstinence, 0.79 for Weight control, and 1.31 for Other. Health behavior scores differed across all sociodemographic variables and covariates (all p<.001). For example, 21% of participants living in the least deprived neighborhoods, as measured by poverty quintile, scored the maximum on Movement (mean score=0.89, 95% confidence interval [CI]=0.88–0.89) compared to 16% of participants in the most deprived neighborhoods (mean score=0.77, 95% CI=0.76–0.77). Individuals with higher educational attainment and in excellent or very good health had higher scores than their counterparts on all four factors. Males and individuals who were married/living as married had higher scores than their counterparts on the Movement and Other factors but lower scores on the Abstinence and Weight Control factors.
Table 2.
Prevalence of achieving each score, and mean score, on four health behavior factors, overall and by sociodemographic variables, among NIH-AARP participants.
| Factor 1: Movement | Factor 2: Abstinence | Factor 3: Weight control | Factor 4: Other | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | M | 95% CI | % | M | 95% CI | % | M | 95% CI | % | M | 95% CI | |||||||||
| 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | |||||||||
| 35 | 46 | 19 | 0.83 | (0.83–0.83) | 9 | 56 | 35 | 1.25 | (1.25–1.26) | 36 | 48 | 16 | 0.79 | (0.79–0.80) | 13 | 44 | 44 | 1.31 | (1.31–1.31) | |
| Poverty quintiles | ||||||||||||||||||||
| 1 (least deprived) | 32 | 46 | 21 | 0.89 | (0.88–0.89) | 10 | 55 | 36 | 1.26 | (1.26–1.27) | 35 | 48 | 17 | 0.82 | (0.82–0.83) | 10 | 42 | 47 | 1.37 | (1.36–1.38) |
| 2 | 33 | 46 | 20 | 0.87 | (0.86–0.87) | 10 | 56 | 35 | 1.25 | (1.25–1.26) | 35 | 48 | 17 | 0.81 | (0.81–0.82) | 11 | 43 | 46 | 1.35 | (1.34–1.35) |
| 3 | 35 | 46 | 18 | 0.83 | (0.83–0.84) | 9 | 56 | 34 | 1.25 | (1.24–1.25) | 36 | 48 | 16 | 0.80 | (0.79–0.80) | 12 | 43 | 44 | 1.32 | (1.32–1.33) |
| 4 | 37 | 46 | 17 | 0.80 | (0.80–0.81) | 9 | 57 | 34 | 1.24 | (1.24–1.25) | 37 | 48 | 15 | 0.78 | (0.78–0.79) | 13 | 44 | 42 | 1.29 | (1.28–1.29) |
| 5 (most deprived) | 39 | 45 | 16 | 0.77 | (0.76–0.77) | 9 | 57 | 34 | 1.26 | (1.25–1.26) | 39 | 47 | 14 | 0.75 | (0.75–0.76) | 16 | 46 | 38 | 1.22 | (1.22–1.23) |
| Education quintiles | ||||||||||||||||||||
| 1 (least deprived) | 28 | 47 | 25 | 0.97 | (0.97–0.98) | 10 | 53 | 36 | 1.26 | (1.25–1.26) | 32 | 48 | 20 | 0.87 | (0.87–0.88) | 9 | 40 | 51 | 1.43 | (1.42–1.43) |
| 2 | 33 | 47 | 20 | 0.87 | (0.87–0.88) | 10 | 56 | 35 | 1.25 | (1.25–1.26) | 35 | 48 | 17 | 0.82 | (0.81–0.82) | 11 | 43 | 46 | 1.36 | (1.35–1.36) |
| 3 | 36 | 46 | 17 | 0.81 | (0.80–0.82) | 9 | 57 | 34 | 1.25 | (1.24–1.25) | 37 | 48 | 15 | 0.78 | (0.78–0.79) | 13 | 44 | 44 | 1.31 | (1.30–1.31) |
| 4 | 39 | 45 | 15 | 0.76 | (0.76–0.77) | 9 | 57 | 34 | 1.25 | (1.24–1.25) | 38 | 47 | 14 | 0.76 | (0.75–0.76) | 14 | 45 | 40 | 1.26 | (1.25–1.26) |
| 5 (most deprived) | 41 | 44 | 15 | 0.73 | (0.73–0.74) | 8 | 58 | 34 | 1.26 | (1.26–1.27) | 40 | 47 | 13 | 0.73 | (0.73–0.74) | 17 | 47 | 37 | 1.20 | (1.19–1.20) |
| Sex | ||||||||||||||||||||
| Male | 33 | 47 | 20 | 0.87 | (0.87–0.88) | 13 | 59 | 28 | 1.15 | (1.14–1.15) | 39 | 47 | 14 | 0.74 | (0.74–0.75) | 10 | 42 | 48 | 1.38 | (1.37–1.38) |
| Female | 39 | 44 | 17 | 0.77 | (0.77–0.78) | 4 | 52 | 44 | 1.40 | (1.40–1.40) | 32 | 49 | 19 | 0.87 | (0.86–0.87) | 16 | 46 | 38 | 1.22 | (1.21–1.22) |
| Age group | ||||||||||||||||||||
| <65 years | 35 | 45 | 20 | 0.85 | (0.84–0.85) | 9 | 55 | 35 | 1.26 | (1.26–1.26) | 37 | 48 | 15 | 0.77 | (0.77–0.78) | 14 | 45 | 41 | 1.27 | (1.27–1.27) |
| 65+ years | 36 | 47 | 17 | 0.81 | (0.81–0.81) | 9 | 57 | 34 | 1.24 | (1.24–1.24) | 35 | 48 | 17 | 0.82 | (0.82–0.82) | 11 | 42 | 48 | 1.37 | (1.36–1.37) |
| Race/ethnicity | ||||||||||||||||||||
| Non-Hispanic white | 35 | 46 | 19 | 0.84 | (0.83–0.84) | 10 | 56 | 34 | 1.25 | (1.24–1.25) | 36 | 48 | 16 | 0.80 | (0.79–0.80) | 12 | 43 | 45 | 1.32 | (1.32–1.33) |
| Other | 39 | 46 | 15 | 0.76 | (0.75–0.77) | 6 | 54 | 40 | 1.34 | (1.33–1.35) | 38 | 48 | 14 | 0.77 | (0.76–0.78) | 19 | 50 | 31 | 1.12 | (1.11–1.13) |
| Marital status | ||||||||||||||||||||
| Married/living as married | 33 | 47 | 20 | 0.86 | (0.76–0.77) | 10 | 56 | 34 | 1.23 | (1.29–1.30) | 37 | 48 | 15 | 0.79 | (0.81–0.82) | 11 | 42 | 47 | 1.37 | (1.18–1.19) |
| Other | 40 | 44 | 16 | 0.76 | (0.86–0.87) | 7 | 56 | 37 | 1.29 | (1.23–1.24) | 35 | 48 | 17 | 0.81 | (0.78–0.79) | 17 | 47 | 36 | 1.19 | (1.36–1.37) |
| Educational attainment | ||||||||||||||||||||
| High school degree or less | 44 | 44 | 12 | 0.67 | (0.67–0.68) | 8 | 59 | 33 | 1.25 | (1.25–1.25) | 40 | 47 | 13 | 0.73 | (0.73–0.74) | 16 | 47 | 37 | 1.20 | (1.20–1.21) |
| More than high school | 31 | 47 | 22 | 0.92 | (0.91–0.92) | 10 | 55 | 35 | 1.26 | (1.25–1.26) | 35 | 48 | 17 | 0.83 | (0.82–0.83) | 11 | 42 | 47 | 1.37 | (1.37–1.37) |
| Self-reported health status | ||||||||||||||||||||
| Less than very good | 45 | 43 | 12 | 0.66 | (0.66–0.67) | 9 | 59 | 32 | 1.23 | (1.22–1.23) | 42 | 47 | 11 | 0.69 | (0.69–0.70) | 14 | 45 | 41 | 1.27 | (1.26–1.27) |
| Excellent or very good | 27 | 48 | 25 | 0.97 | (0.97–0.98) | 10 | 53 | 37 | 1.28 | (1.27–1.28) | 32 | 49 | 20 | 0.88 | (0.88–0.88) | 11 | 43 | 46 | 1.35 | (1.34–1.35) |
Note. Chi-square tests of differences in the distribution of scores for each factor across the respective characteristic were all p<.001. M=mean; CI=confidence interval.
Associations between neighborhood poverty and health behavior scores
Greater neighborhood poverty was associated with lower scores on all health behavior factors (Table 3). For example, compared to the first poverty quintile (least deprived), participants in the fifth quintile (most deprived) had a relative risk (RR) for scores on Movement of 0.95 (95% CI=0.94–0.96), on Abstinence of 0.98 (95% CI=0.97–0.99), on Weight control of 0.94 (95% CI=0.92–0.95), and on Other of 0.94 (95% CI=0.93–0.95). These associations adjusted for the covariates, all of which were also significantly associated with health behavior factors (except for age group and Abstinence).
Table 3.
Poisson regressions examining the association between neighborhood-level poverty quintile and scores on health behavior factors, controlling for individual-level demographic characteristics, among NIH-AARP participants.
| Movement | Abstinence | Weight control | Other | |||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Poverty quintiles | ||||||||
| 1 (least deprived) | (ref) | (ref) | (ref) | (ref) | ||||
| 2 | 0.99 | (0.98–1.01) | 0.99 | (0.98–1.00) | 0.99 | (0.98–1.00) | 0.99 | (0.98–1.00) |
| 3 | 0.97 | (0.96–0.99) | 0.98 | (0.97–0.99) | 0.97 | (0.96–0.98) | 0.98 | (0.97–0.99) |
| 4 | 0.96 | (0.95–0.97) | 0.98 | (0.97–0.98) | 0.96 | (0.95–0.97) | 0.97 | (0.96–0.98) |
| 5 (most deprived) | 0.95 | (0.94–0.96) | 0.98 | (0.97–0.99) | 0.94 | (0.92–0.95) | 0.94 | (0.93–0.95) |
| Individual-level characteristics | ||||||||
| Sex | ||||||||
| Male | (ref) | (ref) | (ref) | (ref) | ||||
| Female | 0.94 | (0.94–0.95) | 1.25 | (1.25–1.26) | 1.21 | (1.20–1.22) | 0.94 | (0.94–0.95) |
| Age group | ||||||||
| <65 years | (ref) | (ref) | (ref) | (ref) | ||||
| 65+ years | 0.99 | (0.98–1.00) | 1.00 | (0.99–1.01) | 1.09 | (1.08–1.10) | 1.08 | (1.08–1.09) |
| Race/ethnicity | ||||||||
| Non-Hispanic white | (ref) | (ref) | (ref) | (ref) | ||||
| Other | 0.96 | (0.94–0.97) | 1.07 | (1.05–1.08) | 0.99 | (0.97–1.01) | 0.88 | (0.87–0.89) |
| Marital status | ||||||||
| Married/living as married | (ref) | (ref) | (ref) | (ref) | ||||
| Other | 0.94 | (0.93–0.95) | 0.95 | (0.94–0.95) | 0.97 | (0.96–0.97) | 0.91 | (0.90–0.91) |
| Educational attainment | ||||||||
| High school degree or less | (ref) | (ref) | (ref) | (ref) | ||||
| More than high school | 1.28 | (1.26–1.29) | 1.03 | (1.02–1.03) | 1.12 | (1.11–1.13) | 1.12 | (1.11–1.12) |
| Self-reported health status | ||||||||
| Less than very good | (ref) | (ref) | (ref) | (ref) | ||||
| Excellent or very good | 1.41 | (1.40–1.42) | 1.04 | (1.03–1.04) | 1.25 | (1.24–1.26) | 1.04 | (1.04–1.05) |
Note. Each column represents one multivariable model. Shaded cells indicate statistically-significant interactions between the respective individual-level demographic characteristic and neighborhood-level poverty quintile in their association with the column health behavior factor. RR=relative risk; CI=confidence interval; ref=reference category.
Several cross-level interactions between neighborhood poverty and covariates were observed. For example, the negative association between poverty quintile and Abstinence was limited to the males (Figure 1A; interaction p<.001), but the negative association with Weight control was stronger for females than males (Figure 1B; interaction p<.001). In addition, the negative association between poverty quintile and Movement was limited to participants with more than a high school degree (Figure 2A; interaction p<.001).
Fig. 1.
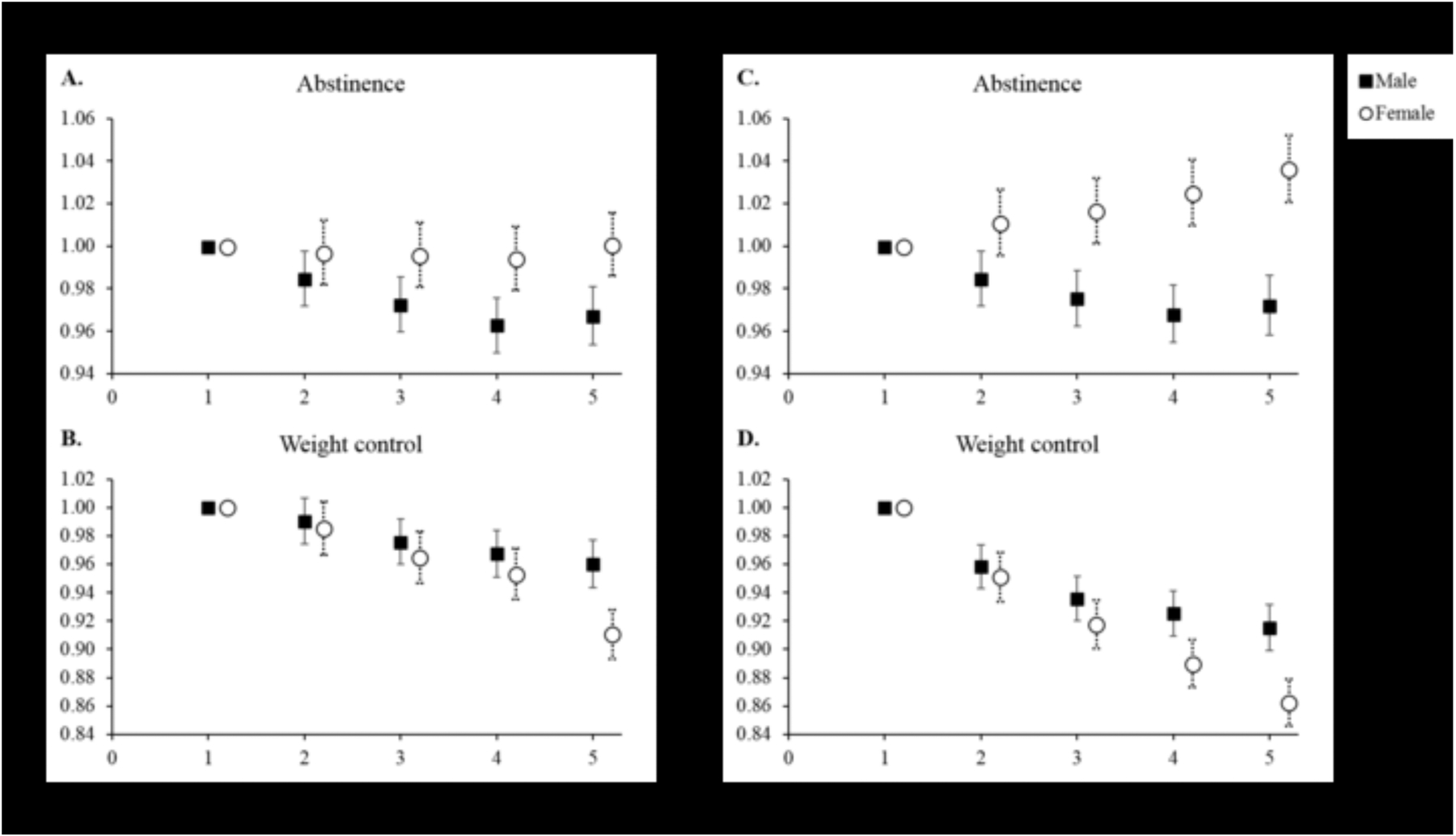
Cross-level interactions between neighborhood poverty quintiles (panels A–B) and education quintiles (C–D) with participant sex in their association with selected health behavior factors among NIH-AARP participants. Error bars are 95% confidence intervals. RR=relative risk
Figure 2.
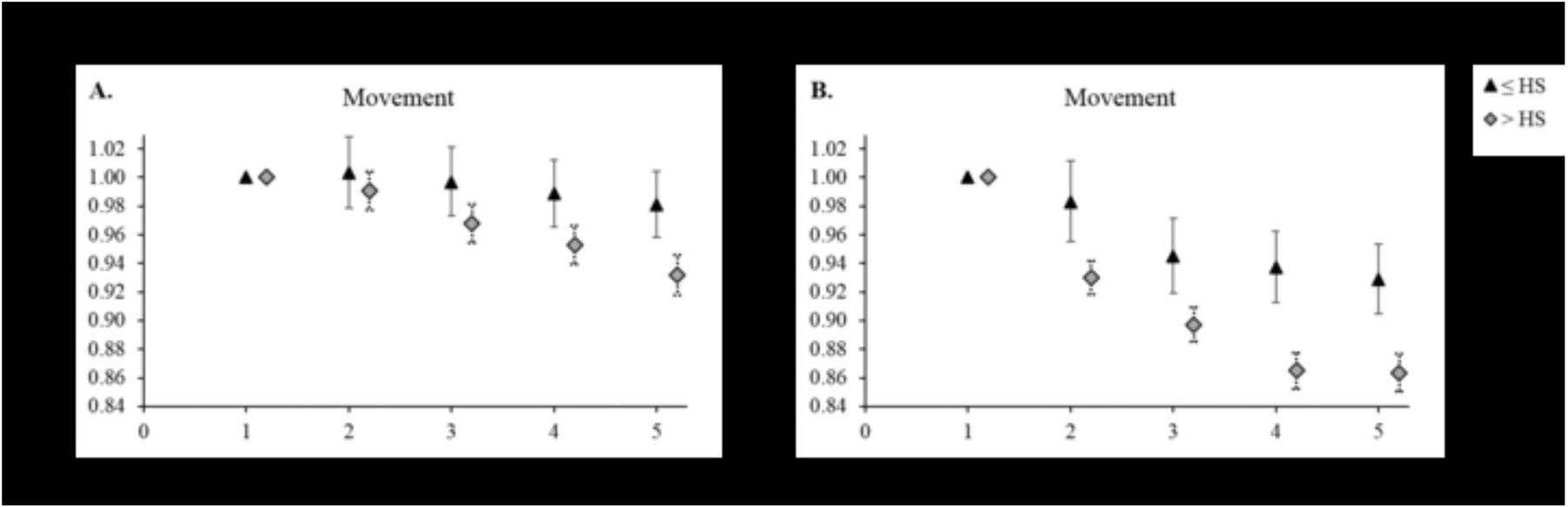
Cross-level interactions between neighborhood poverty quintiles (panel A) and education quintiles (B) with participant educational attainment in their association with selected health behavior factors among NIH-AARP participants. Error bars are 95% confidence intervals. RR=relative risk; HS=high school degree
Associations between neighborhood education and health behavior scores
Greater concentrations of residents with low education in a neighborhood were associated with lower scores on Movement, Weight control, and Other health behavior factors (Table 4). Compared to the first education quintile, participants in the fifth quintile had an RR for scores on Movement of 0.88 (95% CI=0.87–0.89), on Weight control of 0.89 (95% CI=0.88–0.90), and on Other of 0.90 (95% CI=0.89–0.91). Notably, no association was observed between neighborhood education and Abstinence. These associations adjusted for the covariates, most of which were also associated with health behavior factors.
Table 4.
Poisson regressions examining the association between neighborhood-level education quintile and scores on health behavior factors, controlling for individual-level demographic characteristics, among NIH-AARP participants.
| Movement | Abstinence | Weight control | Other | |||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Education quintiles | ||||||||
| 1 (least deprived) | (ref) | (ref) | (ref) | (ref) | ||||
| 2 | 0.94 | (0.93–0.95) | 0.99 | (0.99–1.00) | 0.96 | (0.94–0.97) | 0.97 | (0.96–0.98) |
| 3 | 0.90 | (0.89–0.91) | 0.99 | (0.98–1.00) | 0.93 | (0.92–0.94) | 0.95 | (0.94–0.95) |
| 4 | 0.88 | (0.87–0.89) | 0.99 | (0.98–1.00) | 0.91 | (0.90–0.92) | 0.92 | (0.91–0.93) |
| 5 (most deprived) | 0.88 | (0.87–0.89) | 1.00 | (0.99–1.01) | 0.89 | (0.88–0.90) | 0.90 | (0.89–0.91) |
| Individual-level characteristics | ||||||||
| Sex | ||||||||
| Male | (ref) | (ref) | (ref) | (ref) | ||||
| Female | 0.94 | (0.94–0.95) | 1.25 | (1.24–1.26) | 1.21 | (1.20–1.22) | 0.94 | (0.94–0.95) |
| Age group | ||||||||
| <65 years | (ref) | (ref) | (ref) | (ref) | ||||
| 65+ years | 0.99 | (0.98–1.00) | 1.00 | (0.99–1.01) | 1.09 | (1.08–1.10) | 1.08 | (1.08–1.09) |
| Race/ethnicity | ||||||||
| Non-Hispanic white | (ref) | (ref) | (ref) | (ref) | ||||
| Other | 0.96 | (0.95–0.98) | 1.06 | (1.05–1.08) | 0.99 | (0.98–1.01) | 0.88 | (0.87–0.89) |
| Marital status | ||||||||
| Married/living as married | (ref) | (ref) | (ref) | (ref) | ||||
| Other | 0.94 | (0.93–0.95) | 0.95 | (0.94–0.95) | 0.97 | (0.96–0.97) | 0.91 | (0.90–0.91) |
| Educational attainment | ||||||||
| High school degree or less | (ref) | (ref) | (ref) | (ref) | ||||
| More than high school | 1.25 | (1.24–1.26) | 1.03 | (1.02–1.03) | 1.10 | (1.09–1.11) | 1.10 | (1.09–1.11) |
| Self-reported health status | ||||||||
| Less than very good | (ref) | (ref) | (ref) | (ref) | ||||
| Excellent or very good | 1.40 | (1.39–1.41) | 1.04 | (1.03–1.04) | 1.24 | (1.23–1.25) | 1.04 | (1.03–1.04) |
Note. Each column represents one multivariable model. Shaded cells indicate statistically-significant interactions between the respective individual-level demographic characteristic and neighborhood-level education quintile in their association with the column health behavior factor. RR=relative risk; CI=confidence interval; ref=reference category.
Again, several cross-level interactions between neighborhood education and covariates were observed. For example, the association between education quintile and Abstinence was negative for males but positive for females (Figure 1C; interaction p<.001). The negative association between education quintile and Weight control was stronger for females than males (Figure 1D; interaction p<.001). In addition, the negative association between education quintile and Movement was stronger for participants with more than a high school degree compared to those with a high school degree or less (Figure 2B; interaction p<.001).
Supplementary analyses
The results of the revised Poisson regressions demonstrated findings consistent with the main analysis: increasing quintiles of neighborhood deprivation were associated with lower scores on the ACS behavior factor and the eight-point index (Supplementary Table S2). For example, compared to the first poverty quintile, participants in the fifth quintile had an RR of 0.98 (95% CI=0.97–0.98) for the ACS behavior factor and of 0.95 (95% CI=0.95–0.96) for the eight-point index. Compared to the first education quintile, participants in the fifth quintile had an RR of 0.95 (95% CI=0.94–0.96) for the ACS behavior factor and of 0.92 (95% CI=0.92–0.93) for the eight-point index.
When modelling the association between each health behavior score and neighborhood poverty and education quintiles simultaneously (Supplementary Table S3), the negative associations with education for Movement, Weight control, and Other were maintained after controlling for poverty (which, generally, was no longer associated with these scores). For Abstinence, the negative association with poverty maintained statistical significance, but education was not generally associated with Abstinence (in the main analysis or in this model).
Discussion
In an analysis of more than 300,000 middle-aged and older U.S. adults, eight cancer prevention behaviors clustered into four factors: adequate physical activity and low TV watching (Movement); never having smoked and low alcohol consumption (Abstinence); healthy BMI and high fruit and vegetable consumption (Weight control); and adequate sleep and receiving selected cancer screenings (Other). We found less engagement in these behavioral clusters for those living in more deprived neighborhoods compared to their counterparts in less deprived neighborhoods.
The behaviors examined in this study are associated with cancer risk (Kushi et al., 2012; Song and Giovannucci, 2016). Some of the four behavioral clusters have been examined in other studies. For example, the overlap of smoking and alcohol use (Abstinence) has been demonstrated previously (Berrigan et al., 2003; Patterson et al., 1994). These two behaviors are independently associated with about 27% (Peto et al., 1994) and 4% (Boffetta et al., 2006) of cancer deaths, respectively. Based on their overlap, interventions to simultaneously discourage smoking and to moderate alcohol use may be more efficient than programs targeting just one behavior (Prochaska et al., 2008). Given the clustering of high physical activity and low television viewing (Movement), interventions to replace television viewing with physical activity may be especially effective at improving health (although much of this work has focused on children (Jenvey, 2007)).
Engagement in the clusters of cancer prevention behaviors varied by neighborhood poverty. Scores for all four factors were lower in the more deprived census block groups (i.e., with higher levels of poverty) compared to less deprived areas, even after controlling for individual-level covariates. Previous studies have demonstrated negative associations between neighborhood poverty and health behaviors (Datta et al., 2006; Kershaw et al., 2013). The associations in the present study were relatively small (RR=0.94–0.98 across factors); however, at the population level, these associations could translate into substantial public health impact (Rose, 2001), especially given the compounding risk of engaging in multiple risk behaviors (Warren Andersen et al., 2016). Some of the associations between neighborhood poverty and health behavior scores were moderated by individual-level characteristics. For instance, the negative association between neighborhood poverty and Movement was only statistically significant among participants with higher educational achievement. The observed interaction could indicate that the association for individual-level education was more important than the association for neighborhood-level SES with healthy BMI and fruit and vegetable consumption.
In addition, health behavior scores varied by neighborhood education level, consistent with previous studies (Finch et al., 2010; Ross, 2000). Scores for three factors were lower in more deprived census block groups compared to less areas. These associations were larger than those observed for neighborhood poverty (RR=0.88–0.90 versus RR=0.94–0.98, respectively) and were maintained even after controlling for neighborhood poverty in supplementary analysis. Notably, Abstinence scores did not vary by neighborhood education level. Previous studies have demonstrated higher rates of smoking in more deprived neighborhoods (Cubbin et al., 2001; Ross, 2000), but the associations for drinking are mixed (Fone et al., 2013; Stimpson et al., 2007); it could be that the combination of these two behaviors (with potentially opposing associations with deprivation) into one factor resulted in a net null finding. In interaction analyses, the association between neighborhood education and Abstinence was positive for females but negative for males. A potential confound for this relationship is relation: Individuals with higher levels of religiosity are more likely to live in deprived neighborhoods (Hoverd et al., 2013) and more likely to abstain from substance use (Chitwood et al., 2008; Strawbridge et al., 2001). Further, this association between religiosity and abstinence tends to be stronger for women than for men (Parenteau, 2017; Strawbridge et al., 2001). Additional multilevel studies are needed to explicate the relationships among neighborhood-level SES and individual-level sex, religiosity, and substance use. However, the main effects and interactions for Abstinence with neighborhood education were slightly different from those demonstrated for neighborhood poverty (Tables 3 and 4; Figure 1A and 1C), which speaks to issues around indicators of area-level SES and what they capture (Krieger et al., 2002). That is, while there is overlap, neighborhoods classified as deprived in terms of poverty may not be the same neighborhoods that are classified as deprived in terms of education, and resources supporting Abstinence (e.g., cessation tools, lower density of tobacco and alcohol outlets) may vary across these areas (Cantrell et al., 2015; Diez Roux and Mair, 2010).
These findings may have implications for public health interventions aiming to reduce cancer risk, particularly among older adults. Increasingly, research suggests that intervening on multiple behaviors simultaneously can be more effective and efficient (Prochaska et al., 2008; Warren Andersen et al., 2016). In the present study, we observed consistently lower engagement in multiple health behaviors in more deprived neighborhoods compared to less deprived neighborhoods. Although more research is needed, it is possible that programs to improve neighborhood-level poverty and education levels (Berkman et al., 2014), or to ameliorate the deleterious effects of concentrated disadvantage on health (Finch et al., 2010; Massey, 1996), could be useful for increasing multiple cancer prevention behaviors concurrently.
In terms of study limitations, the NIH-AARP data used in the present analysis were observational and cross-sectional, limiting our ability to draw causal inferences. In addition, engagement in health behaviors was self-reported, which may be subject to social desirability bias (Johnson et al., 2005). The data were collected in the mid-1990s among primarily non-Hispanic white middle-aged and older adults, which limits the generalizability of the results to other periods or groups. The response rate could have introduced bias if people who engaged in fewer preventive behaviors were less likely to respond. Alternative methods of classifying health behaviors and creating clusters could result in different relationships with neighborhood SES; to begin to address this concern, we ran the two supplementary analyses using alternative methods, but found overall similar results to the main analysis. As with all studies, not all relevant variables were included; important variables, such as participants’ household income, were not collected (Schatzkin et al., 2001) and thus excluded from the analysis.
In terms of study strengths, we used data from a large, geographically-diverse cohort. We evaluated engagement with health behaviors documented to influence cancer (Song and Giovannucci, 2016). This research represents a synthetic analysis of multiple health behaviors, advancing the work of numerous previous studies examining one or two health behaviors in isolation. Our results were consistent across neighborhood sociodemographic variables (poverty and education) and across supplementary analyses, increasing our confidence in the validity of the observed associations.
Conclusions
Among middle-aged and older U.S. adults, we found that eight cancer prevention behaviors clustered into four behavioral factors. Scores on these factors demonstrated consistent negative associations with neighborhood deprivation measured by poverty and education. Theoretical and intervention work on multiple behavior change suggests that intervening on more than one health behavior can be efficient at improving public health (Prochaska et al., 2008; Warren Andersen et al., 2016). Future studies should seek to establish causal associations between neighborhood deprivation and health behavior clusters to support the development of multiple health behavior change interventions.
Supplementary Material
Acknowledgements
This research was supported (in part) by the Intramural Research Program of the NIH, National Cancer Institute. Cancer incidence data from the Atlanta metropolitan area were collected by the Georgia Center for Cancer Statistics, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia. Cancer incidence data from California were collected by the California Cancer Registry, California Department of Public Health’s Cancer Surveillance and Research Branch, Sacramento, California. Cancer incidence data from the Detroit metropolitan area were collected by the Michigan Cancer Surveillance Program, Community Health Administration, Lansing, Michigan. The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System (Miami, Florida) under contract with the Florida Department of Health, Tallahassee, Florida. The views expressed herein are solely those of the authors and do not necessarily reflect those of the FCDC or FDOH. Cancer incidence data from Louisiana were collected by the Louisiana Tumor Registry, Louisiana State University Health Sciences Center School of Public Health, New Orleans, Louisiana. Cancer incidence data from New Jersey were collected by the New Jersey State Cancer Registry, The Rutgers Cancer Institute of New Jersey, New Brunswick, New Jersey. Cancer incidence data from North Carolina were collected by the North Carolina Central Cancer Registry, Raleigh, North Carolina. Cancer incidence data from Pennsylvania were supplied by the Division of Health Statistics and Research, Pennsylvania Department of Health, Harrisburg, Pennsylvania. The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations or conclusions. Cancer incidence data from Arizona were collected by the Arizona Cancer Registry, Division of Public Health Services, Arizona Department of Health Services, Phoenix, Arizona. Cancer incidence data from Texas were collected by the Texas Cancer Registry, Cancer Epidemiology and Surveillance Branch, Texas Department of State Health Services, Austin, Texas. Cancer incidence data from Nevada were collected by the Nevada Central Cancer Registry, Division of Public and Behavioral Health, State of Nevada Department of Health and Human Services, Carson City, Nevada.
We are indebted to the participants in the NIH-AARP Diet and Health Study for their outstanding cooperation. We also thank Sigurd Hermansen and Kerry Grace Morrissey from Westat for study outcomes ascertainment and management and Leslie Carroll at Information Management Services for data support and analysis.
Footnotes
The authors have no conflicts of interest to report.
References
- Berkman LF, Kawachi I, Glymour MM, 2014. Social epidemiology. Oxford University Press, Oxford. [Google Scholar]
- Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB, 2003. Patterns of health behavior in U.S. adults. Preventive medicine 36:615–23. [DOI] [PubMed] [Google Scholar]
- Boffetta P, Hashibe M, La Vecchia C, Zatonski W, Rehm J, 2006. The burden of cancer attributable to alcohol drinking. international Journal of Cancer 119:884–87. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E, 2010. Socioeconomic disparities in health in the United States: what the patterns tell us. American Journal of Public Health 100:S186–S96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantrell J, Anesetti-Rothermel A, Pearson JL, Xiao H, Vallone D, Kirchner TR, 2015. The impact of the tobacco retail outlet environment on adult cessation and differences by neighborhood poverty. Addiction 110:152–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2012. Cancer screening - United States, 2010. MMWR.Morbidity and mortality weekly report 61:41–45. [PubMed] [Google Scholar]
- Chitwood DD, Weiss ML, Leukefeld CG, 2008. A systematic review of recent literature on religiosity and substance use. Journal of Drug Issues 38:653–88. [Google Scholar]
- Cubbin C, Hadden WC, Winkleby MA, 2001. Neighborhood context and cardiovascular disease risk factors: the contribution of material deprivation. Ethnicity & disease 11:687–700. [PubMed] [Google Scholar]
- Datta GD, Colditz GA, Kawachi I, Subramanian SV, Palmer JR, Rosenberg L, 2006. Individual-, neighborhood-, and state-level socioeconomic predictors of cervical carcinoma screening among U.S. black women: a multilevel analysis. Cancer 106:664–69. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services, 2015. Dietary Guidelines for Americans, 2015–2020. [Google Scholar]
- Diez Roux AV, Mair C, 2010. Neighborhoods and health. Annals of the New York Academy of Sciences 1186:125–45. [DOI] [PubMed] [Google Scholar]
- Finch BK, Phuong Do D, Heron M, Bird C, Seeman T, Lurie N, 2010. Neighborhood effects on health: Concentrated advantage and disadvantage. Health & place 16:1058–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fone DL, Farewell DM, White J, Lyons RA, Dunstan FD, 2013. Socioeconomic patterning of excess alcohol consumption and binge drinking: a cross-sectional study of multilevel associations with neighbourhood deprivation. BMJ open 3: 10.1136/bmjopen-2012-002337.Print 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoverd WJ, Bulbulia J, Sibley CG, 2013. Does poverty predict religion? Religion, Brain & Behavior 3:185–200. [Google Scholar]
- Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, Kosary CL, Yu M, Ruhl J, et al. , 2016. SEER Cancer Statistics Review, 1975–2013. [Google Scholar]
- Jenvey VB, 2007. The relationship between television viewing and obesity in young children: a review of existing explanations. Early Child Development and Care 177:809–20. [Google Scholar]
- Johnson TP, O’Rourke DP, Burris JE, Warnecke RB, 2005. An investigation of the effects of social desirability on the validity of self-reports of cancer screening behaviors. Medical care 43:565–73. [DOI] [PubMed] [Google Scholar]
- Kabat GC, Matthews CE, Kamensky V, Hollenbeck AR, Rohan TE, 2015. Adherence to cancer prevention guidelines and cancer incidence, cancer mortality, and total mortality: a prospective cohort study. The American Journal of Clinical Nutrition 101:558–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keadle SK, Moore SC, Sampson JN, Xiao Q, Albanes D, Matthews CE, 2015. Causes of Death Associated With Prolonged TV Viewing. American journal of preventive medicine 49:811–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Albrecht SS, Carnethon MR, 2013. Racial and ethnic residential segregation, the neighborhood socioeconomic environment, and obesity among Blacks and Mexican Americans. American Journal of Epidemiology 177:299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Mueller CW, 1978. Factor analysis: Statistical methods and practical issues. Sage Publications, Newbury Park, CA. [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R, 2002. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. American Journal of Epidemiology 156:471–82. [DOI] [PubMed] [Google Scholar]
- Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, Gapstur S, Patel AV, Andrews K, et al. , 2012. American Cancer Society guidelines on nutrition and physical activity for cancer prevention. CA: a cancer journal for clinicians 62:30–67. [DOI] [PubMed] [Google Scholar]
- Massey DS, 1996. The age of extremes: concentrated affluence and poverty in the twenty-first century. Demography 33:395–412; discussion 13–6. [PubMed] [Google Scholar]
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP, 2008. Amount of time spent in sedentary behaviors in the United States, 2003–2004. American journal of epidemiology 167:875–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHLBI Obesity Education Initiative, 2010. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Google Scholar. [Google Scholar]
- Noar SM, Chabot M, Zimmerman RS, 2008. Applying health behavior theory to multiple behavior change: considerations and approaches. Preventive medicine 46:275–80. [DOI] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion, 2008. Physical activity guidelines for Americans. Washington, DC: US Department of Health and Human Services. [Google Scholar]
- Office of Disease Prevention and Health Promotion, 2018. Healthy People 2020 Topics and Objectives: Sleep Health.
- Parenteau SC, 2017. Religious coping and substance use: the moderating role of sex. Journal of religion and health 56:380–87. [DOI] [PubMed] [Google Scholar]
- Patel AV, Bernstein L, Deka A, Feigelson HS, Campbell PT, Gapstur SM, Colditz GA, Thun MJ, 2010. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. American journal of epidemiology 172:419–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson RE, Haines PS, Popkin BM, 1994. Health lifestyle patterns of U.S. adults. Preventive medicine 23:453–60. [DOI] [PubMed] [Google Scholar]
- Peto R, Lopez AD, Boreham J, Thun M, Heath C, 1994. Mortality from smoking in developed countries 1950–2000. Indirect estimates from national statistics. [Google Scholar]
- Prochaska JJ, Spring B, Nigg CR, 2008. Multiple health behavior change research: an introduction and overview. Preventive medicine 46:181–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk NP, Anderson LH, Crain AL, Martinson BC, O’Connor PJ, Sherwood NE, Whitebird RR, 2004. Meeting recommendations for multiple healthy lifestyle factors. Prevalence, clustering, and predictors among adolescent, adult, and senior health plan members. American Journal of Preventive Medicine 27:25–33. [DOI] [PubMed] [Google Scholar]
- Rose G, 2001. Sick individuals and sick populations. International journal of epidemiology 30:427–32; discussion 33–4. [DOI] [PubMed] [Google Scholar]
- Ross CE, 2000. Walking, exercising, and smoking: does neighborhood matter? Social science & medicine 51:265–74. [DOI] [PubMed] [Google Scholar]
- Schatzkin A, Subar AF, Thompson FE, Harlan LC, Tangrea J, Hollenbeck AR, Hurwitz PE, Coyle L, Schussler N, et al. , 2001. Design and serendipity in establishing a large cohort with wide dietary intake distributions : the National Institutes of Health-American Association of Retired Persons Diet and Health Study. American Journal of Epidemiology 154:1119–25. [DOI] [PubMed] [Google Scholar]
- Song M, Giovannucci E, 2016. Preventable Incidence and Mortality of Carcinoma Associated With Lifestyle Factors Among White Adults in the United States. JAMA oncology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimpson JP, Ju H, Raji MA, Eschbach K, 2007. Neighborhood deprivation and health risk behaviors in NHANES III. American Journal of Health Behavior 31:215–22. [DOI] [PubMed] [Google Scholar]
- Stokes ME, Davis CS, Koch GG, 2012. Categorical data analysis using SAS, 3 ed.SAS Institute Inc, Cary, NC. [Google Scholar]
- Strawbridge WJ, Shema SJ, Cohen RD, Kaplan GA, 2001. Religious attendance increases survival by improving and maintaining good health behaviors, mental health, and social relationships. Annals of Behavioral Medicine 23:68–74. [DOI] [PubMed] [Google Scholar]
- U. S. Department of Health Human Services, 2014. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 17. [Google Scholar]
- Wang Y, Beydoun MA, 2007. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiologic reviews 29:6–28. [DOI] [PubMed] [Google Scholar]
- Warren Andersen S, Zheng W, Sonderman J, Shu XO, Matthews CE, Yu D, Steinwandel M, McLaughlin JK, Hargreaves MK, et al. , 2016. Combined Impact of Health Behaviors on Mortality in Low-Income Americans. American Journal of Preventive Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C, 1995. US socioeconomic and racial differences in health: patterns and explanations. Annual review of sociology 21:349–86. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


