For doing laparoscopic lower abdominal surgery, the Trendelenburg position of patient is required for adequate surgical exposure. In the Trendelenburg position, the patient's feet are kept 15 to 30 degrees higher than the patient's head.[1] Many surgeons do the surgery with Trendelenburg position of 30 to 45 degrees, particularly during laparoscopic and robotic surgery. The benefit of the Trendelenburg position is that the abdominal viscera move upwards, which improves visibility and surgical access to the abdominal and pelvic organs.
However, this position has its own limitations, as it increases intracranial tension (ICT), intraocular pressure (IOP) and postoperative vision loss.[2] Ischemic optic neuropathy is the most common cause of postoperative vision loss.[2] Periorbital swelling and venous congestion resulting from the Trendelenburg position can lead to a compartment syndrome in the orbital space that compromises blood flow to the eye, retina, and optic nerve.[3] The optic nerve sheath diameter is a simple, safe, non-invasive, reliable monitoring of intracranial pressure.[4]
Here we describe a case of elective laparoscopic vesicovaginal fistula repair, which was carried out under general anaesthesia. A 37-year-old female ASA grade I weighing 60 kg investigation CBC, kidney function test, liver function test, ECG and CXR were within normal limits. Written and informed consent was taken. In the operating room standard American society of Anesthesiologists monitor were applied. Patient was induced with Fentanyl (2 μg/kg), Propofol (2 mg/kg), Vecuronium (6 mg) and intubation was done with size 7.5 standard endotracheal tube, under direct laryngoscopy. Anaesthesia was maintained with 50% O2, 50% Air and Isoflurane. Increase in Heart rate and MAP >20% of baseline values, then it will be treated with incremental dose of Fentanyl 1 mcg/kg and Vecuronium 1 mg. Patient was initially given lithotomy position and after creation of carboperitonium, the Trendelenburg position was given slowly.
Furthermore, head tilt about 45° intra-abdominal pressure was maintained at 14 mm of Hg. The ETco2 was maintained 33-34 mmHg. Blood pressure was 130/90, heart rate was 80 beats/min. Dexamethasone (8 mg) intravenous was given for postoperative nausea vomiting associated with laparoscopic surgeries. The surgery was lasted for about 4 hrs. Total 2500 ml crystalloid was given. Estimated blood loss was 200 ml.
After completion of surgery and on return of spontaneous respiratory effort, the patient was reversed with Inj. Neostigmine (3 mg) and Inj. Glycopyrrolate (0.6 mg), but the patient was not taking adequate tidal volume, also there was no response, while oral/tracheal suctioning. Her pupils were examined, which were fully dilated and fixed. Also, her heart rate was dropped to 60-61 bpm Blood pressure was 120/80. Raised ICP was suspected 1 gm 20% mannitol was given. Ultrasonography was done to asses optic nerve sheath diameter, which was 0.71 cm Figure 1. After mannitol administration pupils size reduced than previous (still dilated) but were no reacting to light. further 1 gm of mannitol was given. After 20-30 minutes, the patient was started taking adequate tidal volume, regular respiratory rate of around 16-18/min, also started following commands, patient was extubated and urgently Non-Contrast CT brain was done and was normal.
Figure 1.
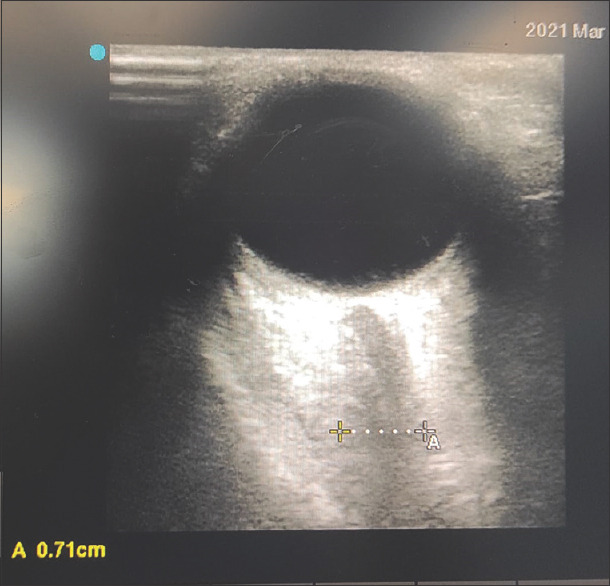
Ultrasonography of Optic nerve sheath diameter
The patient was then kept in HDU for monitoring with head up position of about 30-degree, normal saline (80 ml/hr) maintenance fluid was given. Next day, her pupil size returned to normal size and the post-operative blood investigations CBC, urea, creatinine, serum electrolytes were within the normal limit.
There are several causes of raised intraocular and intracranial pressure during laparoscopic lower abdominal surgery, which commonly includes; pneumoperitoneum, positive pressure ventilation, hypercarbia and the Trendelenburg position. The differential diagnosis of fixed dilated pupil in our case includes, residual effect of paralysis and sedation, raised intraocular and intracranial pressure which might be due to cerebrovascular accident (CVA) or due to more steeper Trendelenburg position during surgery. The raised intracranial pressure was due to the cause of fixed dilated pupil as optic nerve sheath diameter in each eye is >5 mm, indicating ICP >20 mm. We ruled out CVA as a cause of fixed dilated pupil because of its reversible nature and quickly respond with osmotic diuresis (mannitol) in our case. So, in our case, fixed dilated pupil is due to prolonged surgery (>2 hours) in stepper Trendelenburg position.
Van Wicklin[5] in a systematic review found dramatic and significant decrease in IOP that occurs before arousal from anaesthesia. They also support the implementation of periodic intraoperative position change or rest period as a mechanism to help to reduce IOP. Several studies found that induction and maintenance of anaesthesia with intravenous agents (Propofol, Dexmedetomidine) was the most effective option for mitigating the increase in IOP in adult patients undergoing surgery in the Trendelenburg position.
We advocate preoperative ocular examination and regular monitoring of optic nerve sheath diameter as a representative of raised ICT and IOP during intraoperative period to ensure early awareness of surgical team, implement early interventions to reduce ICT and IOP as needed, and thus reduces intraoperative ocular complications and postoperative vision loss. Intraoperative interventions reduce IOP, which includes, reduced the degree of the Trendelenburg position, implementing a modified Trendelenburg position, providing periodic position changes or rest periods and administering specific medications or anaesthesia technique.[2]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.MacDonald JJ, Washington SJ. Positioning the surgical patient. Anaesth Intensive Care Med. 2012;13:528–32. [Google Scholar]
- 2.Kan KM, Brown SE, Gainsburg DM. Ocular complications in robotic-assisted prostatectomy: A review of pathophysiology and prevention. Minerva Anestesiol. 2015;81:557–66. [PubMed] [Google Scholar]
- 3.Molloy BL. Implications for postoperative visual loss: Steep trendelenburg position and effects on intraocular pressure. AANA J. 2011;79:115–21. [PubMed] [Google Scholar]
- 4.Bhatia SS, Kumar BA, Itee C. Noninvasive intracranial pressure monitoring via optic nerve sheath diameter for robotic surgery in steep trendelenburg position. Saudi J Anaesth. 2015;9:239–46. doi: 10.4103/1658-354X.154693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Wicklin SA. Systematic review and meta-analysis of trendelenburg position on intraocular pressure in adults undergoing surgery. Ann Laparosc Endosc Surg. 2019;4:88–8. doi: 10.14444/7029. [DOI] [PMC free article] [PubMed] [Google Scholar]


