Abstract
Background
Neutralizing monoclonal antibody (MAB) therapies may benefit patients with mild to moderate COVID-19 at high risk for progressing to severe COVID-19 or hospitalization. Studies documenting approaches to deliver MAB infusions and demonstrating their efficacy are lacking.
Objective
We describe our experience and the outcomes of almost 3000 patients who received MAB infusion therapy at Northwell Health, a large integrated health care system in New York.
Methods
This is a descriptive study of adult patients who received MAB therapy between November 20, 2020, to January 31, 2021, and a retrospective cohort survival analysis comparing patients who received MAB therapy prior to admission versus those who did not. A multivariable Cox model with inverse probability weighting according to the propensity score including covariates (sociodemographic, comorbidities, and presenting vital signs) was used. The primary outcome was in-hospital mortality; additional evaluations included emergency department use and hospitalization within 28 days of a positive COVID-19 test for patients who received MAB therapy.
Results
During the study period, 2818 adult patients received MAB infusion. Following therapy and within 28 days of a COVID-19 test, 123 (4.4%) patients presented to the emergency department and were released, and 145 (5.1%) patients were hospitalized. These 145 patients were compared with 200 controls who were eligible for but did not receive MAB therapy and were hospitalized. In the MAB group, 16 (11%) patients met the primary outcome of in-hospital mortality, versus 21 (10.5%) in the control group. In an unadjusted Cox model, the hazard ratio (HR) for time to in-hospital mortality for the MAB group was 1.38 (95% CI 0.696-2.719). Models adjusting for demographics (HR 1.1, 95% CI 0.53-2.23), demographics and Charlson Comorbidity Index (HR 1.22, 95% CI 0.573-2.59), and with inverse probability weighting according to propensity scores (HR 1.19, 95% CI 0.619-2.29) did not demonstrate significance. The hospitalization rate was 4.4% for patients who received MAB therapy within 0 to 4 days, 5% within 5 to 7 days, and 6.1% in ≥8 days of symptom onset (P=.15).
Conclusions
Establishing the capability to provide neutralizing MAB infusion therapy requires substantial planning and coordination. Although this therapy may be an important treatment option for early mild to moderate COVID-19 in patients who are at high risk, further investigations are needed to define the optimal timing of MAB treatment to reduce hospitalization and mortality.
Keywords: infectious disease, monoclonal antibody therapy, COVID-19, experience, therapy, drug, patient outcome, risk, efficacy, approach, treatment, pandemic, antibody, immunotherapy, immune therapy
Introduction
In November 2020, the Federal Drug Administration (FDA) issued an Emergency Use Authorization (EUA) for the neutralizing monoclonal antibody (MAB) infusions bamlanivimab and casirivimab/imdevimab for treatment of early mild to moderate SARS-CoV-2 infection in patients at high risk for progressing to severe COVID-19 or hospitalization [1]. Bamlanivimab has been found to decrease viral load at 11 days, and exploratory analysis of COVID-19–related hospitalization suggested a decrease in hospitalization rate from 6.3% to 1.6% [2]. Additional studies of bamlanivimab in combination with etesevimab also found reductions in viral load and similarly found a reduction in hospitalization, although the latter was not the primary outcome [3]. Most recently, bamlanivimab coadministered with remdesivir did not demonstrate efficacy among patients who were hospitalized with COVID-19 without end organ failure [4]. To date, published data on the effectiveness of these therapies is mixed, and the National Institutes of Health correspondingly notes that data are insufficient to recommend for or against the use of MAB therapy for ambulatory patients [5].
Given the operational complexity and uncertain clinical effectiveness of setting up a MAB infusion program, widespread use has been slow across the United States [6]. Potential barriers to implementation include staffing challenges during disease resurgence, the necessity to provide infusions in a COVID-19 contained environment, transportation of underserved and older patients to infusion centers, and the need to obtain timely referrals from providers [7]. Mobile units have shown to be successful in a small study [8], although the ability to scale this solution appears limited. The Mayo Clinic recently reported their implementation of a program across multiple facilities in different states, culminating in over 4000 doses delivered [9].
Northwell Health, a 23-hospital integrated health care system in metropolitan New York, established outpatient infusion centers based on their experience with the spring 2020 surge [10], which stretched inpatient capacity. At the peak of the early surge, Northwell had more than 3400 COVID-19 inpatients, with over 800 receiving invasive mechanical ventilation. With the goal of reducing hospitalizations, intensive care unit admissions, and deaths during the fall and winter 2020 rise in cases, Northwell rapidly scaled a MAB infusion program. We reviewed our initial experience in using MAB therapy and describe the outcomes of almost 3000 patients who received this outpatient infusion therapy, the largest cohort with outcomes published to date.
Methods
This was a retrospective study of a large integrated health care system, with 23 hospitals and over 800 ambulatory locations. Data for this study were obtained from the enterprise inpatient and outpatient electronic health record (Sunrise Clinical Manager and Touchworks, respectively; Allscripts), our health information exchange (Healthshare; Intersystems), and our locally developed population health management tool (CareTool Listapp; Northwell Health).
Monoclonal Antibody Infusion Eligibility Criteria
Eligibility to receive MAB therapy as directed by the FDA EUA is limited to patients with a positive direct viral test for SARS-CoV-2 within 10 days of symptom onset. Patients must be ≥12 years of age, weigh at least 40 kg, and be at high risk for progressing to severe COVID-19 or hospitalization. High risk is defined as having one of the following conditions: age ≥65 years, obesity (BMI≥35 kg/m2), diabetes mellitus (DM), chronic kidney disease (CKD), immunosuppressive disease, or currently receiving immunosuppressive treatment. Patients 55-64 years of age who have cardiovascular disease, hypertension, chronic obstructive pulmonary disease (COPD), or chronic respiratory disease also are eligible. Pediatric patients aged 12-17 years with one of the following conditions were also eligible: BMI≥85th percentile for age and gender, sickle cell disease, congenital or acquired heart disease, neurodevelopmental disorders, a medical-related technological dependence, asthma, reactive airway, or other chronic respiratory disease that requires daily medication for control.
Two MAB therapies were offered at Northwell, based upon availability: bamlanivimab (Eli Lilly and Company) and casirivimab/imdevimab (Regeneron Pharmaceuticals, Inc).
Monoclonal Antibody Infusion Operations
Northwell established a taskforce of clinicians paired with an operational team to develop a four-phase strategy and operational plan for MAB infusion. The initial phase established five outpatient infusion sites, all located on hospital campuses in freestanding buildings or in mobile hospital tents previously erected to accommodate the spring 2020 COVID-19 surge.
In recognition that the emergency department (ED) is often the health care access point in underserved areas, phase 2 established MAB infusions directly for treat-and-release ED patients meeting EUA criteria, who otherwise lacked resources to travel to an infusion center. Phase 3 included administration of MAB therapy to eligible inpatients who developed COVID-19 while hospitalized for another cause and were COVID-19 negative on admission (all patients were tested upon hospital admission). The final phase included MAB therapy administration to patients in skilled nursing facilities, although with the rapid vaccine deployment supporting these facilities, this phase contributed only a small group of patients.
Information technology systems were configured to support patient referral, registration, and throughput in the infusion centers. Information about MAB therapy, the EUA, and referral instructions were disseminated widely to all Northwell’s New York metropolitan area–affiliated providers. A dedicated call center and secure internal webpage were deployed to facilitate easy referral. The information collected included patient demographics and location, referring provider information, presence and details of COVID-19 symptoms and onset date, and screening of eligible comorbidities. The dedicated call center handled referrals, questions from providers and patients, and scheduling.
All patients were screened based on the EUA criteria at the time of referral. Infusion center staff training was created and deployed, including nursing competencies in biologic infusions and preparation with appropriate advanced cardiovascular life support protocols and equipment in the event of an infusion reaction. Specific patient protocols were developed to treat patient reactions to the infusion, including rapid response team evaluation and transfer to the local ED most proximate to the infusion center if necessary. To accommodate the EUA mandate for infusion within 10 days of COVID-19 symptom onset, the infusion centers were staffed 7 days a week.
Study Population
All adult patients (age ≥18 years) who received MAB therapy in an ambulatory or ED location between November 20, 2020, and January 31, 2021, were included. Pediatric patients, inpatients, and skilled nursing facility patients that received MAB therapy in this date range were excluded from the analysis. Data collected include demographics, comorbidities, symptoms and their date of onset, date of COVID-19 test, and outcomes (including ED presentation, hospital admission, and mortality).
We further identified all patients aged ≥18 years with a positive COVID-19 test between November 20, 2020, and January 31, 2021, who did not receive MAB therapy but were eligible based upon EUA criteria. We excluded patients with a COVID-19 positive test or hospitalization prior to the study period. The outpatient outcomes of these patients are described but not directly compared to the treatment group, as we did not have symptoms (presence, timing, type, or severity) for the nontreatment group.
Outcomes
We examined ED use and hospitalization within 28 days of a positive COVID-19 test for patients who received MAB therapy. A total of 9 patients were missing a COVID-19 test date; for these patients, we used the date of MAB therapy subtracted by the cohort median number of days from test to MAB therapy (4 days). The hospitalization rate by timing of MAB therapy relative to symptoms was also assessed.
For patients who were hospitalized, we performed a retrospective cohort study with a time-to-event survival analysis and a primary outcome of in-hospital mortality. The control group was selected from the population of patients who met eligibility for MAB therapy but did not receive it during the evaluation period.
Covariates
We included sociodemographic and clinical features, including patient age, sex, race or ethnicity, number of hospital visits in the prior year, comorbidities, and presenting vital signs. Race or ethnicity was categorized as non-Hispanic White, non-Hispanic Black, Hispanic, Asian, other or multiracial, and unknown or declined. The comorbidities included DM, obesity, chronic respiratory conditions, COPD, CKD, hypertension, and immuno-compromising conditions (including the use of immunosuppressive medications). Presenting vital signs for patients hospitalized include heart rate, oxyhemoglobin saturation, temperature, and systolic and diastolic blood pressure.
Statistical Analysis
We reported descriptive statistics including median and IQR for skewed continuous measures and proportions for categorical measures. We compared baseline clinical characteristics between patients who were and were not hospitalized using Fisher exact tests for categorical variables and nonparametric Kruskal-Wallis tests for continuous variables. Patients were categorized into 3 groups based on timing of MAB therapy relative to symptom onset date (0-4 days, 5-7 days, and ≥8 days) to assess the difference in hospitalization rate.
For a univariable time-to-event analysis comparing mortality risk, we used the Kaplan-Meier survival curve to estimate in-hospital mortality to 28 days. Cox proportional hazards regression models were used to estimate the association between MAB therapy and in-hospital mortality. We initially evaluated an unadjusted model; a model adjusted for age, sex, and race or ethnicity; and a model that added the Charlson Comorbidity Index (CCI) to the prior model. The primary analysis used inverse probability weighting (IPW), whereby the predicted probabilities from a propensity score model were used to calculate the stabilized IPW weight. The covariates included in the propensity model were age, sex, race or ethnicity, number of hospitalizations in prior year, and comorbidities and presenting vital signs (listed in the Covariates section).
All analyses were performed using the R programming language, version 4.0.3 (R Foundation for Statistical Computing). A P value <.05 was considered significant. The Institutional Review Board of Northwell Health approved the study protocol before the commencement of the study. Individual-level informed consent was not obtained given the retrospective nature of the analysis of a large electronic medical record.
Results
Overview
From November 20, 2020, to January 31, 2021, 2818 adult patients with symptomatic COVID-19 received MAB infusion at Northwell Health: 2745 (97%) ambulatory and 73 (3%) ED (Table 1). An additional 21 pediatric patients and 59 hospitalized patients received MAB therapy and were not included in the analysis. The median patient age was 67 (IQR 58-74) years, and 59% (1648/2818) were 65 years or older. The gender distribution was split evenly between males (n=1412, 50.1%) and females (n=1406, 49.9%). Most patients were non-Hispanic White (n=2061, 73%), 104 (3.7%) were non-Hispanic Black, and 168 (6%) were Hispanic. Hypertension was the most common comorbidity (n=1011, 36%), followed by obesity (n=401, 23%). The most common symptom was cough (n=1954, 70% of patients), followed by malaise (n=1471, 53%), fever (n=1422, 51%), and headache (n=820, 30%). Although cough as the sole documented symptom was most common, many patients had multiple presenting symptoms (Figure S1 in Multimedia Appendix 1).
Table 1.
Characteristics of 2818 patients with COVID-19 who received monoclonal antibody therapy in ambulatory or emergency department setting.
| Variables | Overall (N=2818) | No inpatient visit (n=2673) | Inpatient visit (n=145) | P value | |||||
| Age (years), median (IQR) | 67.00 (58.00-74.00) | 66.00 (58.00-74.00) | 75.00 (64.00-82.00) | <.001 | |||||
| Age categories (years), n (%) | <.001 | ||||||||
|
|
<55 | 460 (16.3) | 450 (16.8) | 10 (6.9) |
|
||||
|
|
55-64 | 710 (25.2) | 683 (25.6) | 27 (18.6) |
|
||||
|
|
65-74 | 964 (34.2) | 930 (34.8) | 34 (23.4) |
|
||||
|
|
≥75 | 684 (24.3) | 610 (22.8) | 74 (51.0) |
|
||||
| Female sex, n (%) | 1406 (49.9) | 1343 (50.2) | 63 (43.4) | .13 | |||||
| Race/ethnicity, n (%) | .39 | ||||||||
|
|
Hispanic | 168 (6.0) | 160 (6.0) | 8 (5.5) |
|
||||
|
|
Non-Hispanic Black | 104 (3.7) | 99 (3.7) | 5 (3.4) |
|
||||
|
|
Asian | 110 (3.9) | 103 (3.9) | 7 (4.8) |
|
||||
|
|
Non-Hispanic White | 2061 (73.1) | 1948 (72.9) | 113 (77.9) |
|
||||
|
|
Other/multiracial | 332 (11.8) | 323 (12.1) | 9 (6.2) |
|
||||
|
|
Unknown/declined | 43 (1.5) | 40 (1.5) | 3 (2.1) |
|
||||
| Comorbidities, n (%) | |||||||||
|
|
Obesity | 401 (23.3) | 377 (23.4) | 24 (21.4) | .71 | ||||
|
|
Diabetes mellitus | 484 (17.2) | 421 (15.8) | 63 (43.4) | <.001 | ||||
|
|
Hypertension | 1011 (35.9) | 901 (33.7) | 110 (75.9) | <.001 | ||||
|
|
Chronic kidney disease | 113 (4.0) | 85 (3.2) | 28 (19.3) | <.001 | ||||
|
|
Chronic obstructive pulmonary disease | 434 (15.4) | 394 (14.7) | 40 (27.6) | <.001 | ||||
|
|
Chronic respiratory disease | 463 (16.4) | 418 (15.6) | 45 (31.0) | <.001 | ||||
|
|
Immunosuppressed | 179 (6.4) | 161 (6.0) | 18 (12.4) | .004 | ||||
| COVID-19 symptoms, n (%) | |||||||||
|
|
Cough | 1954 (70.4) | 1847 (70.2) | 107 (74.3) | .34 | ||||
|
|
Malaise | 1471 (53.0) | 1398 (53.1) | 73 (50.7) | .63 | ||||
|
|
Fever | 1422 (51.2) | 1350 (51.3) | 72 (50.0) | .83 | ||||
|
|
Headache | 820 (29.5) | 788 (30.0) | 32 (22.2) | .06 | ||||
|
|
Sore throat | 555 (20.0) | 532 (20.2) | 23 (16.0) | .26 | ||||
|
|
Gastrointestinal | 371 (13.4) | 351 (13.3) | 20 (13.9) | .95 | ||||
|
|
Loss taste/smell | 309 (11.1) | 296 (11.3) | 13 (9.0) | .49 | ||||
|
|
Muscle pain | 256 (9.2) | 240 (9.1) | 16 (11.1) | .51 | ||||
|
|
Shortness of breath | 143 (5.2) | 131 (5.0) | 12 (8.3) | .11 | ||||
| Monoclonal antibody type, n (%) | .30 | ||||||||
|
|
Casirivimab/imdevimab | 317 (11.2) | 305 (11.4) | 12 (8.3) |
|
||||
|
|
Bamlanivimab | 2501 (88.8) | 2368 (88.6) | 133 (91.7) |
|
||||
| Monoclonal antibody timing, median (IQR) | |||||||||
|
|
Days from symptom onset to therapy | 6.00 (4.00-8.00) | 6.00 (4.00-8.00) | 6.00 (5.00-8.00) | .39 | ||||
|
|
Days from symptom onset to COVID-19 test | 2.00 (1.00-3.00) | 2.00 (1.00-3.00) | 2.00 (1.00-3.25) | .03 | ||||
| EDa and hospital use | |||||||||
|
|
ED visit within 28 days, n (%) | 123 (4.4) | 112 (4.2) | 11 (7.6) | .08 | ||||
|
|
Days from COVID-19 test to ED visit, median (IQR) | 7.00 (5.00-11.00) | 7.00 (5.00-11.00) | 6.00 (3.00-10.50) | .49 | ||||
|
|
Days from therapy to ED visit, median (IQR) | 3.00 (0.00-6.00) | 3.00 (0.00-6.00) | 2.00 (0.50-4.50) | .56 | ||||
|
|
Days from COVID-19 test to hospitalization, median (IQR) | N/Ab | N/A | 7.00 (5.00-11.00) | N/A | ||||
|
|
Days from therapy to hospitalization, median (IQR) | N/A | N/A | 3.00 (1.00-8.00) | N/A | ||||
aED: emergency department.
bN/A: not applicable.
Most patients developed symptoms prior to a COVID-19 test (median 2, IQR 1-3 days; Figure S2 in Multimedia Appendix 1). Among the patients with known symptom onset date, the median time from symptom onset to MAB therapy was 6 days (IQR 4-8; Figure S3 in Multimedia Appendix 1). MAB referral to infusion scheduling occurred in under half a day (median 0.05, IQR 0.01-0.54 days), and the MAB infusion occurred a median 1.75 (IQR 0.85-1.88) days after referral. Most patients received bamlanivimab (n=2501, 89%), with the remainder receiving casirivimab/imdevimab (n=317, 11%).
Following MAB therapy and within 28 days of a COVID-19 test, 123 (4.4%) patients presented to the ED and were released a median of 7 (IQR 5-11) days from a COVID-19 test. In a similar time frame, 145 (5.1%) patients who received MAB therapy were hospitalized a median of 7 (IQR 5-11) days after a COVID-19 test. The median time from MAB therapy to ED presentation therapy was 3 (IQR 0-6) days, and the median time from MAB therapy to hospitalization was 3 (IQR 1-8) days. A greater proportion of patients who were hospitalized following MAB therapy had comorbidities, including diabetes, hypertension, chronic kidney disease, respiratory disease, and immunosuppressive disease (see Table 1).
In the subgroup of patients where symptom onset date was known (n=2721, 96.6%), the hospitalization rate within 28 days of COVID-19 test was 4.4% (95% CI 2.9%-5.9%) for patients who received MAB therapy early (within 0-4 days of symptom onset), 5% (95% CI 3.6%-6.2%) for those within 5 to 7 days, and 6.1% (95% CI 4.6%-7.4%) for those who received it ≥8 days, although this was not statistically significant (P value for trend .15; Figure 1).
Figure 1.
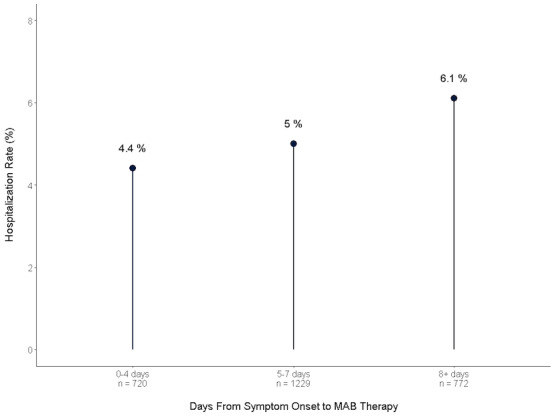
Timing of MAB therapy and hospitalization rate. MAB: monoclonal antibody.
Among 2713 COVID-19–positive patients meeting eligibility criteria based on age or comorbidities but not receiving MAB therapy, the median age was 66 (IQR 55-73) years and 55% (n=1497) were female. Non-Hispanic White patients were most common (n=1596, 59%), and there were 183 (6.7%) non-Hispanic Black and 334 (12.3%) Hispanic patients. Symptoms were not ascertained for this group, but similar to the MAB therapy group, hypertension was the most common comorbidity (n=1119, 41%). A total of 142 (5.2%) patients and 200 (7.4%) patients in this group had an ED visit and inpatient hospitalization, respectively, within 28 days of a COVID-19 test. Patients hospitalized had a higher burden of comorbid conditions (Table S1 in Multimedia Appendix 1).
Hospital Outcomes
A total of 145 MAB patients were hospitalized and were compared with 200 controls who otherwise met MAB therapy eligibility criteria and were hospitalized (Table 2). The MAB group was slightly older (median age 75, IQR 64-82 years vs median age 69, IQR 57-78 years), with a lower proportion of women (63/145, 43% vs 106/200, 53%) and a higher proportion of non-Hispanic White race (113/145, 78% vs 118/200, 59%). There was no significant difference in the presence of comorbidities between the groups.
Table 2.
Characteristics of patients who received and did not receive prehospital monoclonal antibody therapy and were hospitalized within 28 days of a COVID-19 test.
| Variables | All hospitalized patients (n=345) | Control group (n=200) | Monoclonal antibody treatment group (n=145) | P value | |
| Age (years), median (IQR) | 72.00 (61.00-80.00) | 69.00 (57.00-78.00) | 75.00 (64.00-82.00) | .001 | |
| Age categories (years), n (%) | .001 | ||||
|
|
<55 | 52 (15.1) | 42 (21.0) | 10 (6.9) |
|
|
|
55-64 | 62 (18.0) | 35 (17.5) | 27 (18.6) |
|
|
|
65-74 | 89 (25.8) | 55 (27.5) | 34 (23.4) |
|
|
|
≥75 | 142 (41.2) | 68 (34.0) | 74 (51.0) |
|
| Female sex, n (%) | 169 (49.0) | 106 (53.0) | 63 (43.4) | .10 | |
| Race/ethnicity, n (%) | .02 | ||||
|
|
Hispanic | 32 (9.3) | 24 (12.0) | 8 (5.5) |
|
|
|
Non-Hispanic Black | 25 (7.2) | 20 (10.0) | 5 (3.4) |
|
|
|
Asian | 19 (5.5) | 12 (6.0) | 7 (4.8) |
|
|
|
Non-Hispanic White | 231 (67.0) | 118 (59.0) | 113 (77.9) |
|
|
|
Other/multiracial | 29 (8.4) | 20 (10.0) | 9 (6.2) |
|
|
|
Unknown/declined | 9 (2.6) | 6 (3.0) | 3 (2.1) |
|
| Comorbidities, n (%) | |||||
|
|
Obesity | 73 (23.4) | 49 (24.5) | 24 (21.4) | .64 |
|
|
Diabetes mellitus | 149 (43.2) | 86 (43.0) | 63 (43.4) | >.99 |
|
|
Hypertension | 259 (75.1) | 149 (74.5) | 110 (75.9) | .87 |
|
|
Chronic kidney disease | 50 (14.5) | 25 (12.5) | 25 (17.2) | .28 |
|
|
Chronic obstructive pulmonary disease | 95 (27.5) | 55 (27.5) | 40 (27.6) | >.99 |
|
|
Chronic respiratory disease | 113 (32.8) | 68 (34.0) | 45 (31.0) | .64 |
|
|
Immunosuppressed | 38 (11.0) | 20 (10.0) | 18 (12.4) | .59 |
| Charlson Comorbidity Index, median (IQR) | 6.00 (4.00-8.00) | 5.00 (3.00-8.00) | 6.00 (4.00-8.00) | .22 | |
| Presentation vital signs, median (IQR) | |||||
|
|
Heart rate (beats per minute) | 89.00 (78.00-102.00) | 89.50 (77.00-103.00) | 89.00 (79.00-100.00) | .58 |
|
|
Systolic blood pressure (mmHg) | 131.00 (119.00-147.00) | 131.50 (118.75-146.25) | 130.00 (121.00-147.00) | .98 |
|
|
Diastolic blood pressure (mmHg) | 74.00 (67.00-83.00) | 74.00 (67.00-83.00) | 75.00 (66.00-82.00) | .44 |
|
|
Temperature (°C) | 37.00 (36.70-37.60) | 36.90 (36.70-37.42) | 37.10 (36.70-37.70) | .04 |
|
|
Oxygen saturation (%) | 96.00 (92.00-98.00) | 96.00 (92.00-98.00) | 96.00 (93.00-97.00) | .48 |
In the MAB group, 16 (11%) patients met the primary outcome of in-hospital mortality, versus 21 (10.5%) in the control group. Kaplan-Meier survival curve showed no difference between the two groups for event-free probability (log-rank P=.41; Figure 2). In an unadjusted Cox proportional hazards model, the hazard ratio (HR) for time to inpatient mortality for the MAB group was 1.38 (95% CI 0.696-2.719). There was no significant association between prehospitalization MAB use and the primary end point in both a model adjusted for demographics (HR 1.1, 95% CI 0.53-2.23), a model adjusted for demographics and CCI (HR 1.22, 95% CI 0.573-2.59), and a model with IPW according to the propensity score (HR 1.19, 95% CI 0.619-2.29).
Figure 2.
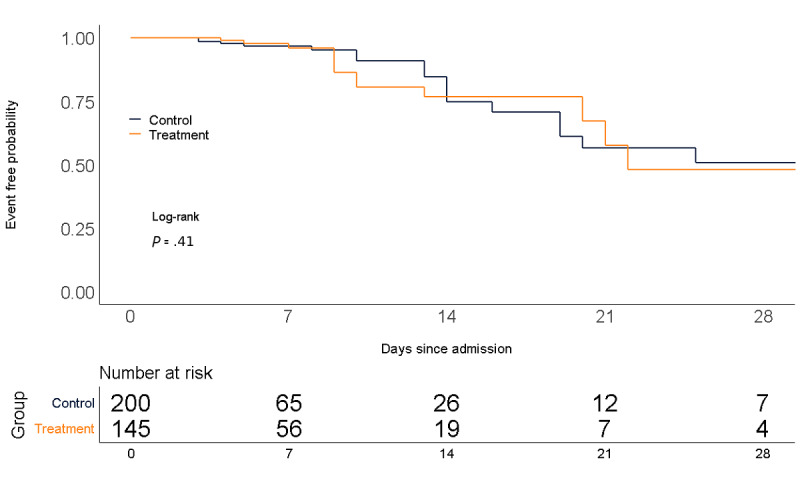
Freedom from the end point of in-hospital mortality.
Discussion
Principal Findings
Despite the issuance of an FDA EUA for two MAB therapies in late 2020 to treat mild to moderate COVID-19 in high-risk outpatients, adoption and use nationally has been slow [5]. Hesitancy may be related to questions of treatment effectiveness, logistical challenges, and staffing requirements during the pandemic [9]. In the 2.5-month period following the EUA, Northwell scaled up an ambulatory MAB infusion operation and successfully administered therapy to over 2800 eligible patients, with most patients receiving therapy within 1.8 days of referral. The operational success required close collaboration and coordination of clinical, operation, informatics, information technology, ambulatory, and population health leadership to ensure the appropriate requirements were in place.
Among the patients who received MAB therapy, a majority received bamlanivimab due to availability. A total of 145 (5.1%) patients were hospitalized within 28 days of a COVID-19 test, and 16 died (0.6% of total population and 11% of patients who were hospitalized). We did find a trend toward a lower rate of hospitalization for patients receiving therapy more proximate to symptom onset date, although this finding was not statistically significant. Inasmuch as the effect of MAB therapy is to reduce SARS-CoV-2 viral load [11], receiving these therapies earlier in the disease course should be beneficial; the low numbers of hospitalized patients in our treatment group may contribute to the lack of statistical significance. Among the 2713 patients who tested positive for COVID-19 during the same time period in our health system, and who met age or comorbidity eligibility criteria for MAB yet did not receive it, 200 (7.4%) were hospitalized within 28 days. A direct comparison to our MAB cohort, however, is not feasible given the lack of symptom data for these non-MAB patients.
Compared to a matched control group, there was no significant difference in the hospital outcome of in-hospital mortality. Although our sample size of patients who were hospitalized was small, this finding may be more related to COVID-19 disease burden; once a patient meets clinical requirements for hospitalization, prior MAB therapy likely does not alter the clinical trajectory. Indeed, randomized trials of MAB in patients who were hospitalized did not demonstrate efficacy [4].
Although the published randomized control trials to date presented promising efficacy data, the primary endpoint was focused on viral load rather than clinically meaningful outcomes such as hospitalization or death [2,3]. A case series suggesting benefit has been described but had a small sample size and lack of control [12]. We were able to describe the outcomes in 2818 patients receiving MAB therapy and further compared in-hospital mortality with an appropriately matched control group. Our study did not demonstrate effectiveness of MAB therapy on preventing in-hospital mortality, and we did not have a control group to examine the effectiveness of MAB therapy on preventing hospitalization. Nonetheless, the trend toward reduced hospitalization seen in the early treatment cohort is intriguing; timely referral and operational efficiency to administer MAB therapy early in the course of disease would benefit hospital operations by reducing the burden on capacity issues. Although we invested resources to specifically staff the MAB infusion facilities, such a derived benefit may outweigh the MAB resource use. Certainly, preventing mortality is the most critical outcome, however, a reduced burden of patients who are critically ill would allow the hospital staff to focus on non–COVID-19 patients as well. In addition, the administration of MAB therapy in the ED helped facilitate health equity, since many underserved communities, challenged by the lack of primary care and a high prevalence of comorbid conditions, were disproportionately affected by severe COVID-19. Interestingly, this phase of our MAB program did not result in ED overcrowding.
Future efforts for MAB therapy may include home infusion or mobile treatment options. Although these were considered in our original MAB strategy, staffing burden for the number of patients that could be treated was high and operational considerations such as preparation and transportation of the mixed MAB infusion were considerable. It is hoped that alternate routes (eg, intramuscular or subcutaneous) of administering MAB therapies can be developed to offset these operational and staffing challenges.
As many health systems continue to deal with COVID-19 surges, we recommend establishing a national database to analyze MAB treatment in larger cohorts. Although randomized placebo-controlled trials may not be logistically feasible, further meta-analyses of centers leveraging these therapies may be in order.
Limitations
Limitations of our study include the observational and retrospective study design. In addition, our health system is based in New York and may not be generalizable to other regions. Due to the lack of symptom documentation for our control group of patients, we were unable to assess the impact of MAB therapy on hospitalization rate. Given the small number of patients and low event rate, our analysis of inpatient mortality may be underpowered to detect a difference.
Conclusions
The EUA for the MAB infusions provides a foundation for treatment of early mild to moderate COVID-19 in patients who are at high risk. This study describes the rapid development of a MAB infusion program to provide such treatment for over 2800 patients. Establishing the capability to perform MAB infusion therapy requires close collaboration and coordination of numerous stakeholders and can support hospital operations in the setting of a pandemic surge. Further investigation is required to define the optimal timing of MAB therapy and the potential attendant reduction in hospitalization and mortality.
Abbreviations
- CCI
Charlson Comorbidity Index
- CKD
chronic kidney disease
- COPD
chronic obstructive pulmonary disease
- DM
diabetes mellitus
- ED
emergency department
- EUA
Emergency Use Authorization
- FDA
Federal Drug Administration
- HR
hazard ratio
- IPW
inverse probability weighting
- MAB
monoclonal antibody
Supplementary material.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Coronavirus (COVID-19) update: FDA authorizes monoclonal antibody for treatment of COVID-19. US Food and Drug Administration. [2021-01-21]. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-monoclonal-antibody-treatment-covid-19 .
- 2.Chen P, Nirula A, Heller B, Gottlieb RL, Boscia J, Morris J, Huhn G, Cardona J, Mocherla B, Stosor V, Shawa I, Adams AC, Van Naarden J, Custer KL, Shen L, Durante M, Oakley G, Schade AE, Sabo J, Patel DR, Klekotka P, Skovronsky DM, BLAZE-1 Investigators SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with Covid-19. N Engl J Med. 2021 Jan 21;384(3):229–237. doi: 10.1056/NEJMoa2029849. http://europepmc.org/abstract/MED/33113295 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gottlieb RL, Nirula A, Chen P, Boscia J, Heller B, Morris J, Huhn G, Cardona J, Mocherla B, Stosor V, Shawa I, Kumar P, Adams AC, Van Naarden J, Custer KL, Durante M, Oakley G, Schade AE, Holzer TR, Ebert PJ, Higgs RE, Kallewaard NL, Sabo J, Patel DR, Klekotka P, Shen L, Skovronsky DM. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA. 2021 Feb 16;325(7):632–644. doi: 10.1001/jama.2021.0202. http://europepmc.org/abstract/MED/33475701 .2775647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ACTIV-3/TICO LY-CoV555 Study Group. Lundgren JD, Grund B, Barkauskas CE, Holland TL, Gottlieb RL, Sandkovsky U, Brown SM, Knowlton KU, Self WH, Files DC, Jain MK, Benfield T, Bowdish ME, Leshnower BG, Baker JV, Jensen JU, Gardner EM, Ginde AA, Harris ES, Johansen IS, Markowitz N, Matthay MA, Østergaard L, Chang CC, Davey VJ, Goodman A, Higgs ES, Murray DD, Murray TA, Paredes R, Parmar MKB, Phillips AN, Reilly C, Sharma S, Dewar RL, Teitelbaum M, Wentworth D, Cao H, Klekotka P, Babiker AG, Gelijns AC, Kan VL, Polizzotto MN, Thompson BT, Lane HC, Neaton JD. A neutralizing monoclonal antibody for hospitalized patients with Covid-19. N Engl J Med. 2021 Mar 11;384(10):905–914. doi: 10.1056/NEJMoa2033130. http://europepmc.org/abstract/MED/33356051 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pallotta AM, Kim C, Gordon SM, Kim A. Monoclonal antibodies for treating COVID-19. Cleve Clin J Med. 2021 Feb 17;:1. doi: 10.3949/ccjm.88a.ccc074. https://www.ccjm.org/cgi/pmidlookup?view=long&pmid=33597176 .ccjm.88a.ccc074 [DOI] [PubMed] [Google Scholar]
- 6.Toy S, Walker J, Evans M. Highly touted monoclonal antibody therapies sit unused in hospitals. Wall Street Journal. [2020-12-27]. https://www.wsj.com/articles/highly-touted-monoclonal-antibody-therapies-sit-unused-in-hospitals-11609087364 .
- 7.Goldstein RH, Walensky RP. The challenges ahead with monoclonal antibodies: from authorization to access. JAMA. 2020 Dec 01;324(21):2151–2152. doi: 10.1001/jama.2020.21872.2773057 [DOI] [PubMed] [Google Scholar]
- 8.Tulledge-Scheitel S, Bell SJ, Larsen JJ, Bierle DM, Takahashi P, Moehnke DE, Destro Borgen MJ, Springer DJ, Reinschmidt KJ, Baumbach LJ, Matoush JA, Heyliger A, Hanson SN, Razonable RR, Ganesh R. A mobile unit overcomes the challenges to monoclonal antibody infusion for COVID-19 in skilled care facilities. J Am Geriatr Soc. 2021 Apr;69(4):868–873. doi: 10.1111/jgs.17090. http://europepmc.org/abstract/MED/33619724 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Razonable RR, Aloia NC, Anderson RJ, Anil G, Arndt LL, Arndt RF, Ausman SE, Bell SJ, Bierle DM, Billings ML, Bishop RK, Cramer CH, Culbertson TL, Dababneh AS, Derr AN, Epps K, Flaker SM, Ganesh R, Gilmer MA, Urena EG, Gulden CR, Haack TL, Hanson SN, Herzog JR, Heyliger A, Hokanson LD, Hopkins LH, Horecki RJ, Krishna BH, Huskins WC, Jackson TA, Johnson RR, Jorgenson B, Kudrna C, Kennedy BD, Klingsporn MK, Kottke B, Larsen JJ, Lessard SR, Lutwick LI, Malone EJ, Matoush JA, Micallef IN, Moehnke DE, Mohamed M, Ness CN, Olson SM, Orenstein R, Palraj R, Patel J, Paulson DJ, Phelan D, Peinovich MT, Ramsey WL, Rau-Kane TJ, Reid KI, Reinschmidt KJ, Seville MT, Skold EC, Smith JM, Speicher LL, Spielman LA, Springer DJ, Sweeten PW, Tempelis JM, Tulledge-Scheitel S, Vergidis P, Whipple DC, Wilker CG, Destro Borgen MJ. A framework for outpatient infusion of antispike monoclonal antibodies to high-risk patients with mild-to-moderate coronavirus disease-19: the Mayo Clinic Model. Mayo Clin Proc. 2021 May;96(5):1250–1261. doi: 10.1016/j.mayocp.2021.03.010. http://europepmc.org/abstract/MED/33958056 .S0025-6196(21)00191-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, the Northwell COVID-19 Research Consortium. Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ, Duer-Hefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020 May 26;323(20):2052–2059. doi: 10.1001/jama.2020.6775. http://europepmc.org/abstract/MED/32320003 .2765184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baum A, Ajithdoss D, Copin R, Zhou A, Lanza K, Negron N, Ni M, Wei Y, Mohammadi K, Musser B, Atwal GS, Oyejide A, Goez-Gazi Y, Dutton J, Clemmons E, Staples HM, Bartley C, Klaffke B, Alfson K, Gazi M, Gonzalez O, Dick E, Carrion R, Pessaint L, Porto M, Cook A, Brown R, Ali V, Greenhouse J, Taylor T, Andersen H, Lewis MG, Stahl N, Murphy AJ, Yancopoulos GD, Kyratsous CA. REGN-COV2 antibodies prevent and treat SARS-CoV-2 infection in rhesus macaques and hamsters. Science. 2020 Nov 27;370(6520):1110–1115. doi: 10.1126/science.abe2402. http://europepmc.org/abstract/MED/33037066 .science.abe2402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dhand A, Lobo SA, Wolfe K, Feola N, Nabors C. Bamlanivimab for treatment of COVID-19 in solid organ transplant recipients: early single-center experience. Clin Transplant. 2021 Apr;35(4):e14245. doi: 10.1111/ctr.14245. http://europepmc.org/abstract/MED/33595145 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.


