Abstract
Background
Medical dissolution of struvite uroliths in dogs is commonly recommended, but data on success rates and complications are limited.
Objectives
To evaluate the efficacy of medical dissolution for suspected struvite cystoliths in dogs.
Animals
Fifty client‐owned dogs fed a therapeutic dissolution diet, with or without administration of antimicrobials, for treatment of suspected struvite cystoliths.
Methods
Single institution, retrospective case series. Medical records were reviewed for dogs with at least 1 follow‐up visit. Dissolution success, complications, and possible predictors of success were evaluated.
Results
Full dissolution of cystoliths was achieved in 58% (29/50) of dogs within a median of 35 days (range, 13‐167). Of 21 dogs without success, 7 each had partial dissolution, no dissolution, or undetermined outcome. Uroliths containing >10% nonstruvite mineral were common in the nonsuccess group (11/16 analyzed). Maximum urolith diameter, number of uroliths, and baseline urine pH did not differ significantly between dogs with and without success. Dissolution was more likely in dogs receiving antimicrobial therapy (OR = 16.3, 95% confidence interval 1.9‐787.4, P = .002). Adverse events occurred in 9 dogs (18%); urethral obstructions were the most common, but 3 of 4 dogs with this complication were obstructed on presentation, before trial initiation.
Conclusions and Clinical Importance
Results support a medical dissolution trial for dogs with suspected struvite cystoliths. If no reduction in urolith size or number occurs by 1 month, a nonstruvite composition is likely, and alternative interventions should be considered. Dogs presenting with urethral obstructions should not be considered candidates for medical dissolution.
Keywords: canine, magnesium ammonium phosphate, stones, urinary tract infection
Abbreviations
- CI
confidence interval
- IQR
interquartile range
- MUC
Minnesota Urolith Center
- OR
odds ratio
- USG
urine specific gravity
- UTI
urinary tract infection
1. INTRODUCTION
Struvite uroliths, otherwise known as magnesium ammonium phosphate, comprise 36% to 43% of urolith submissions from dogs.1, 2, 3 The current recommended therapy for struvite urolithiasis, with few exceptions, is medical dissolution.4 Traditionally, this consists of an appropriate dissolution diet and antimicrobial therapy, administered for 2 to 4 weeks after radiographic resolution of uroliths.5, 6 Goals of therapy include resolution of urinary tract infection (UTI), achieving a urine pH of <6.5, and a urine specific gravity (USG) <1.015 to 1.02.5, 6 Despite the consensus that dissolution is effective and should be the treatment of choice, the Minnesota Urolith Center (MUC) received greater than 40 000 struvite uroliths from dogs for analysis from 2009 to 2010.2 This suggests a disconnect between the current recommendation for medical dissolution and what occurs in clinical practice. A barrier to acceptance of medical dissolution for struvite uroliths in dogs might be the paucity of data on safety and efficacy of treatment. Studies are limited to 6 to 11 dogs.5, 7, 8, 9 Potential concerns regarding medical dissolution are persistent clinical signs during therapy, failure of dissolution, and risk of pancreatitis or urethral obstruction.5, 7, 9
The objective of this study was to retrospectively evaluate the efficacy of medical dissolution of suspected struvite cystoliths using a therapeutic urinary diet, with or without antimicrobial therapy. We hypothesized that suspected struvite cystoliths would show evidence of partial dissolution by 4 weeks and full dissolution within 2 to 4 months in most dogs, and that the most common cause of dissolution failure would be nonstruvite urolith composition. A secondary objective was to further evaluate the risk for complications, such as persistent signs of lower urinary tract disease, pancreatitis, or urethral obstruction. Additional aims of this study were to determine if antimicrobial therapy (presence and duration), maximum stone diameter, number of stones, urine pH, or most likely urolith composition (based on results from the MUC CALCulator application) differed between dogs with and without successful dissolution.
2. MATERIALS AND METHODS
2.1. Case selection criteria
Electronic medical records from the University of Minnesota Veterinary Medical Center between the years of 2007 and 2019 were searched to identify dogs prescribed a canned therapeutic urinary diet formulated for the dissolution of struvite uroliths (Prescription Diet s/d Canine Urinary Care, Hill's Pet Nutrition, Inc, Topeka, Kansas). Inclusion criteria were: (a) cystoliths on either radiographic or ultrasonographic imaging, (b) documentation in the medical record of clinical suspicion for a struvite composition, (c) consumption of the therapeutic urinary diet, and (d) a minimum of 1 follow‐up visit after initiation of the therapeutic urinary diet.
2.2. Data collection
Signalment was recorded for each dog and inputted into the MUC CALCulator application. This outputs the distribution of urolith types that the MUC obtains from dogs that match the inputted signalment. The most common urolith composition and its proportion of total submissions were recorded for each dog's signalment.
The start date of therapeutic urinary diet therapy was established as baseline. The date for each follow‐up visit was recorded as days relative to the baseline. Historical data was extracted from the medical records for these visits and included clinical signs and duration, abdominal imaging results, the presence and duration of antimicrobial therapy, and diet. The size of cystolith at the time of detection was determined by either the longest approximate diameter (in mm) of the largest cystolith on lateral radiograph or the largest diameter reported by the radiologist based on abdominal ultrasound. If this information was not included in the radiologist's report, 1 of the authors (O.A.M.) obtained the measurement directly from the stored images. Similarly, the number of uroliths was extracted from the radiologist's report, or, if not described, obtained from stored images. Because of difficulties counting clusters of very small uroliths or many overlaying uroliths, only those ≥1 mm were counted, and counts were categorized on an ordinal scale: none, 1 to 3, 4 to 6, and >6. Follow‐up imaging results were reviewed, and the time from baseline to first noted decrease in urolith burden (reduction in urolith diameter, number, or both) was calculated in days. Body weight was also recorded from each visit and, when available, results of urinalysis, urine culture and sensitivity testing, and urolith analysis were recorded. Urolith analysis was categorized as either ≥90% struvite or >10% of nonstruvite mineral. Urine pH and USG were extracted from urinalysis results at baseline (pretreatment) and last available measurement while being fed the therapeutic urinary diet (treatment). Urinary tract infections were categorized as “confirmed” if there was bacterial growth on urine culture or “suspected” if there was bacteriuria, pyuria (White blood cells >5/hpf), or both on urinalysis but no culture available.
If the therapeutic diet was discontinued for any reason other than successful urolith dissolution, this was recorded. The reason for discontinuation was categorized as nonstruvite composition or development of potential complications associated with the dissolution trial, such as urethral obstruction, persistent signs of lower urinary tract disease, pancreatitis, or signs of gastrointestinal disease (vomiting, diarrhea, or inappetence), owner noncompliance, or failure of the dog to readily consume the diet.
2.3. Statistical analysis
Data distribution for continuous variables was assessed for normality with Q‐Q plots and the Shapiro‐Wilk test. Data with normal distributions are summarized as mean ± SD. Data that did not follow a normal distribution are summarized as median (range, interquartile range [IQR]). The primary study outcome was urolith dissolution. Outcomes were categorized into success (full dissolution of uroliths) or nonsuccess, which included partial dissolution (reduction in urolith diameter, number, or both), failure (no reduction in urolith burden on the final imaging study after a minimum of 4 weeks of therapy), or undetermined (no repeat abdominal imaging or lack of reduction in urolith diameter after fewer than 4 weeks of therapy). The proportion of all study dogs with success was calculated along with the 95% confidence interval (CI) based on the binomial distribution. A Fisher's exact test was used to compare success rates between dogs with and without struvite as the most likely composition based on the MUC CALCulator results, between male and female dogs, and between dogs that were or were not receiving antimicrobial therapy. A Fisher's exact test was also used to compare the proportions of analyzed uroliths composed of struvite between success and nonsuccess groups. A Wilcoxon rank sum test were performed to compare the MUC CALCulator results, maximum urolith diameter, number of uroliths, duration of antimicrobial therapy, urine pH (at baseline or during treatment), and USG (during treatment) between dogs with and without success. A paired t test was performed to test if urine pH and USG differed at baseline compared with during treatment. Statistical analyses were performed using R software for statistical computing (R, version 3.6.2., www.r-project.org). P values <.05 were considered significant.
3. RESULTS
3.1. Dog sample
Fifty‐two records were evaluated, of which 50 dogs were included in the study. Two cases were excluded because of no available follow‐up after the initial visit and initiation of therapy. Of the 50 dogs, 36 (72%) were spayed females, 11 (22%) were castrated males, and 3 (2%) were intact males. Mean age was 5.9 years (±3.2 years). Median weight was 9.2 kg (range, 2.4‐61.6 kg; IQR 6.4‐16.4 kg). The most common breeds were the Bichon Frise (6), Shih Tzu (5), Pug (4), and Miniature Schnauzer (4); there were 26 other breeds with n ≤ 2.
3.2. Urolith characteristics
Uroliths were identified by abdominal radiography in 41 dogs and ultrasonography in 9 dogs. The median diameter of the largest urolith was 6 mm (range, 0.5‐41 mm; IQR 3‐13 mm). For 6 dogs, all uroliths were <1 mm. Of 44 dogs with uroliths ≥1 mm, 19 had 1 to 2, 5 had 3 to 4, and 20 had >6. The MUC CALCulator showed that the signalment for 37/50 dogs (74%) matched struvite uroliths as the most common composition; the median proportion of uroliths composed of struvite for the signalments was 0.67 (range, 0.01‐0.89; IQR 0.32‐0.8). Of those dogs where struvite was not the top composition for the signalment, calcium oxalate was the most common for 12/50 (24%) and cystine was the most common for 1/50 (2%).
3.3. Urine diagnostics
Forty‐six of the 50 dogs (92%) had a urinalysis and 38/50 (76%) had a urine culture performed at baseline, before starting the therapeutic urinary diet; only 1 dog had neither urinalysis nor urine culture results available. The median baseline urine pH was 7.5 (range, 6‐8.5; IQR 7‐8). The median baseline USG was 1.035 (range, 1.01‐1.048; IQR 1.023‐1.039). In total, 27/49 dogs (55%) had UTIs confirmed by urine culture (23) or suspected based on urinalysis results (4). Eighteen of 50 dogs (36%) were receiving antimicrobials at the time of or less than 2 weeks before presentation, prescribed by the referring veterinarian. Of those 18 with prior antimicrobial therapy, 7 (39%) had confirmed (3) or suspected (4) UTIs at the baseline visit.
Of the dogs with confirmed UTIs, 20/23 (87%) urine cultures grew common urease‐producing bacteria, Staphylococcus spp. (19) and Proteus spp. (1). The 3 other positive cultures grew Escherichia coli (1), Enterococcus spp. (1), and a gram‐positive bacilli that was not speciated (1).
3.4. Antimicrobial therapy
Forty‐one of 50 dogs (82%) received antimicrobials during the dissolution trial, which included amoxicillin clavulanic acid (27; Clavamox, Zoetis, Inc, Kalamazoo, Michigan), amoxicillin (6), enrofloxacin (5; Baytril, Bayer, Shawnee Mission, Kansas), ciprofloxacin (1), cefpodoxime (1; Simplicef, Zoetis, Inc, Kalamazoo, Michigan), and trimethoprim sulfa (1). Three dogs initially receiving amoxicillin clavulanic acid and 1 dog receiving amoxicillin were later switched to a fluoroquinolone based on results of urine culture and susceptibility testing. Median duration of antimicrobial therapy was 30 days (range, 5‐272 days; IQR 14‐37 days).
3.5. Outcomes
A summary of outcomes is presented in Table 1.
TABLE 1.
Cystolith dissolution outcome of 50 dogs fed a therapeutic urinary diet with or without antimicrobial therapy
| Outcome | Proportion with outcome (#/total dogs) | Proportion female (#/total dogs) | Proportion with struvite urolith compositiona (#/total analyzed) |
|---|---|---|---|
| Success (full dissolution) | 0.58 (29/50) | 0.79 (23/29) | 1 (7/7) |
| Nonsuccess | |||
| Partial dissolution | 0.14 (7/50) | 0.71 (5/7) | 0.33 (1/3) |
| Failure | 0.14 (7/50) | 0.57 (4/7) | 0 (0/6) |
| Undetermined | 0.14 (7/50) | 0.57 (4/7) | 0.57 (4/7) |
| Total nonsuccess | 0.42 (21/50) | 0.62 (13/21) | 0.31 (5/16) |
Defined as ≥90% struvite mineral composition.
3.5.1. Full dissolution
Full dissolution of uroliths was achieved in 29/50 (58%) of dogs, with a 95% CI for the success rate in the true sample of 43% to 72%. The median time to first documented decrease in stone burden was 29 days (range, 10‐75 days; IQR 20‐40 days). The median time to full dissolution was 35 days (range, 13‐167 days; IQR 26‐69 days). The distribution of dissolution status relative to the timing of follow‐up imaging studies is shown in Figure 1.
FIGURE 1.
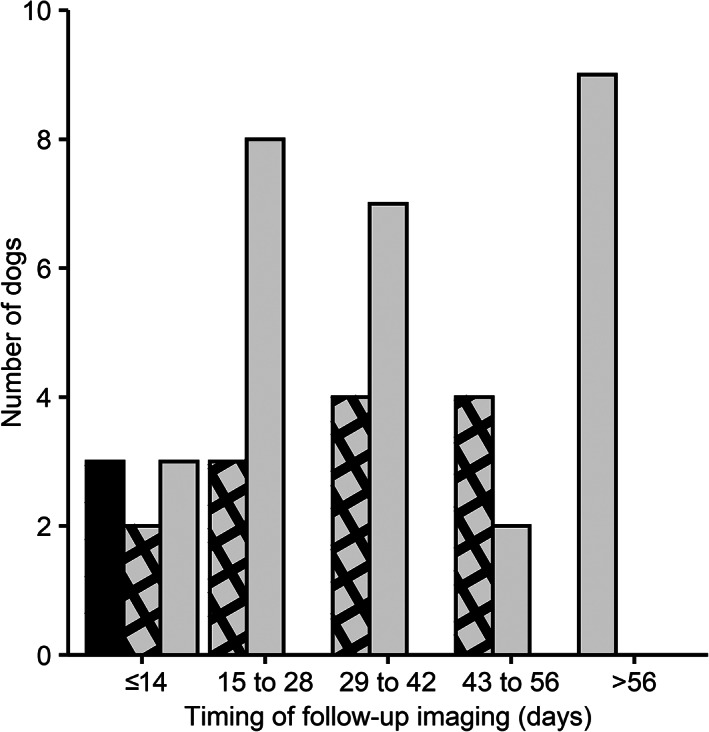
Distribution of dissolution outcome (none, partial, or full) relative to timing of 46 follow‐up imaging studies for 29 dogs that ultimately achieved full dissolution for suspected struvite cystoliths. No dissolution is indicated by the black bar, partial dissolution by the gray crosshatched bars, and full dissolution by the gray bars
Twenty‐eight of 29 dogs (97%) with dissolution of stones received antimicrobial therapy (Figure 2). Ten had the antimicrobial therapy continued for a median of 6 days (range, 2‐107; IQR 3‐10) beyond documentation of full dissolution with an overall duration of 51 days (range, 30‐187; IQR 37‐102). The other 18 dogs had antimicrobials discontinued a median of 11 days (range, 1‐137; IQR 6‐23) before documentation of full dissolution with medical imaging with an overall duration of 30 days (range, 5‐56; IQR 16‐38). Medical imaging was performed between the date of antimicrobial discontinuation and final dissolution for 3 dogs. These dogs received antimicrobials for 10 to 35 days, and cystoliths were still visible (partial dissolution apparent) on imaging at day 40 to 48. Urine culture results at the partial dissolution time point showed no microbial growth for 2 dogs. The third (which had received antimicrobials for 35 days) had bacterial growth on urine cultured 13 days after the antimicrobials were discontinued (day 48), despite no growth at an earlier visit (2 days postantimicrobial discontinuation; day 37). This was the only dog documented to have documented UTI recurrence during the dissolution trial.
FIGURE 2.
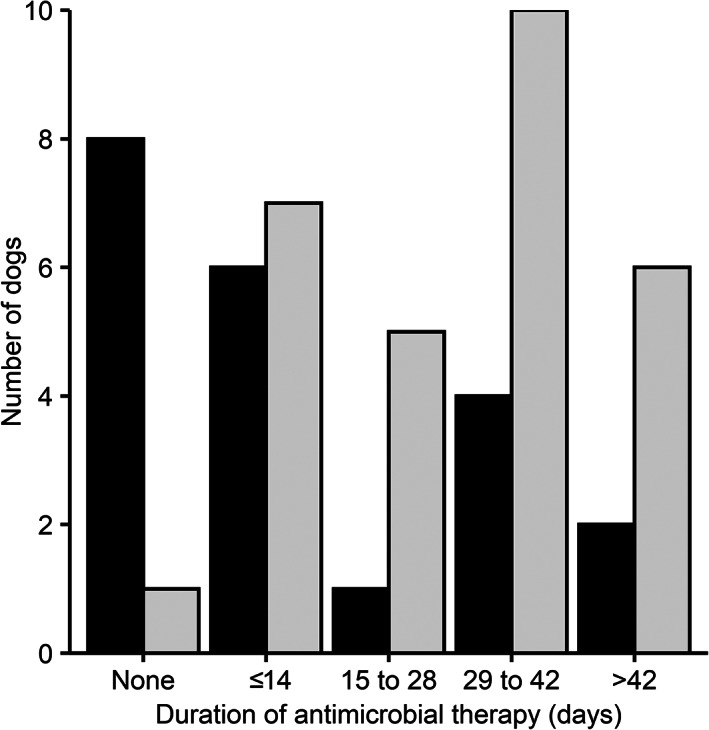
Distribution of duration of antimicrobial therapy for dogs that did or did not achieve successful dissolution of suspected struvite cystoliths. No dissolution is indicated by the black bars, and successful dissolution is indicated by the gray bars
One dog had successful dissolution without antimicrobial therapy. The dog had no current or reported past UTI or history of antimicrobial therapy within the past year. No bacteriuria or pyuria was present on urinalysis, but a urine culture was not performed.
Of the 29 dogs with full dissolution success, 7 dogs were noted to pass cystoliths during dissolution. Analysis of these stones showed 100% (7/7) with compositions of ≥90% struvite (Table 1). Four of the stones contained ≤10% of a nonstruvite mineral, including calcium phosphate (2) and urate (2).
3.5.2. Partial dissolution
Partial dissolution was achieved in 7/50 (14%) of dogs. The median time to first documented decrease in stone burden for dogs with partial dissolution was 34 days (range, 6‐49 days). Five of 7 dogs with partial dissolution received antimicrobial therapy for a median duration of 35 days (range, 14‐272). Three dogs with partial dissolution were lost to follow‐up of 27 to 73 days after the first recheck, including 1 that had a confirmed struvite composition based on analysis of small cystoliths obtained via urinary catheterization. Another case developed a urethral obstruction, lithotripsy was pursued, and urolith analysis revealed >10% nonstruvite mineral (mixed composition of struvite/calcium carbonate/urate). One case failed to demonstrate progressive dissolution, voiding urohydropropulsion was performed, and urolith analysis revealed a calcium oxalate composition. For 1 case, the therapeutic urinary diet was discontinued because of development of pancreatitis. The final case with partial dissolution was humanely euthanized for reasons unrelated to uroliths.
3.5.3. Failure (no dissolution)
Seven of 50 dogs (14%) failed to achieve any urolith dissolution. The final abdominal radiographs documenting no reduction in urolith burden were performed at a median of 44 days (range, 32‐145; IQR = 37‐47). Two of the 7 dogs received antimicrobial therapy for durations of 30 and 31 days. Uroliths were removed by lithotripsy or cystotomy and analyzed in 6/7 cases with failure, all of which were found to have uroliths with >10% of nonstruvite mineral; compositions included calcium oxalate (3), calcium oxalate/calcium phosphate (1), urate (1), and urate/struvite (1). Uroliths were not analyzed from the final dog, and the records stated owner noncompliance in exclusively feeding the therapeutic urinary diet.
3.5.4. Undetermined
Outcomes were undetermined in 7/50 (14%) of dogs. Six of 7 received antimicrobial therapy for a duration of 11 days (range, 6‐57). The therapeutic urinary diet was discontinued before initial recheck because of urethral obstruction (2), vomiting and inappetence (2), persistent stranguria, pollakiuria, and hematuria (1), unknown reason approximately 14 days after dissolution therapy initiation (1), and lack of dissolution by day 13 (1). A cystotomy was performed in 6/7 cases. Urolith analysis revealed >10% of nonstruvite mineral in 2 cases (struvite/calcium phosphate [1] and urate/xanthine [1]), and ≥90% struvite composition in 4 dogs (struvite/calcium carbonate [1], struvite/calcium phosphate carbonate [1], and struvite [2]). The seventh case presented with urethral obstruction, and analysis of the urolith showed a nonstruvite mineral (cystine) composition.
3.5.5. Adverse events
Overall, 9/50 (18%) of dogs experienced adverse events during the dissolution trial, including urethral obstruction (4), pancreatitis (2), vomiting and inappetence of undetermined etiology (2), and persistent stranguria, pollakiuria, and hematuria (1). Three of the 4 dogs that developed urethral obstructions had obstructions diagnosed at the baseline visit that were relieved with retrograde urohydropropulsion before starting the dissolution trial. Three of the dogs with urethral obstructions were male, and 1 was female.
3.6. Comparison of dogs with and without success
The maximum urolith diameter was similar between dogs with success (median of 6 mm; range, 0.5‐41 mm; IQR 2.9‐12.5) and those that did not achieve full dissolution (median of 7 mm; range, 0.5‐22 mm; IQR 3‐13 mm; Figure 3A, P = .78). The distribution of number of uroliths ≥1 mm was also similar between dogs with or without success (Figure 4, P = .67). Dogs with MUC CALCulator results showing struvite as most common composition for their signalment had a greater success rate (25/37 [68%]; OR 4.5, 95% CI 1.01‐24.5, P = .03) than those with other compositions as the top match (4/13 [31%]). However, there was a great overlap in the MUC CALCulator results for dogs with and without success (Figure 3B, P = .19). Success occurred in 6/14 (42%) male and 23/36 (64%) female dogs (OR = 2.3, 95% CI = 0.6‐10.1, P = .21). Of dogs with uroliths analyzed, those that achieved successful dissolution were more likely to have a struvite composition than the nonsuccess group (Table 1, OR = Infinity, P = .005).
FIGURE 3.
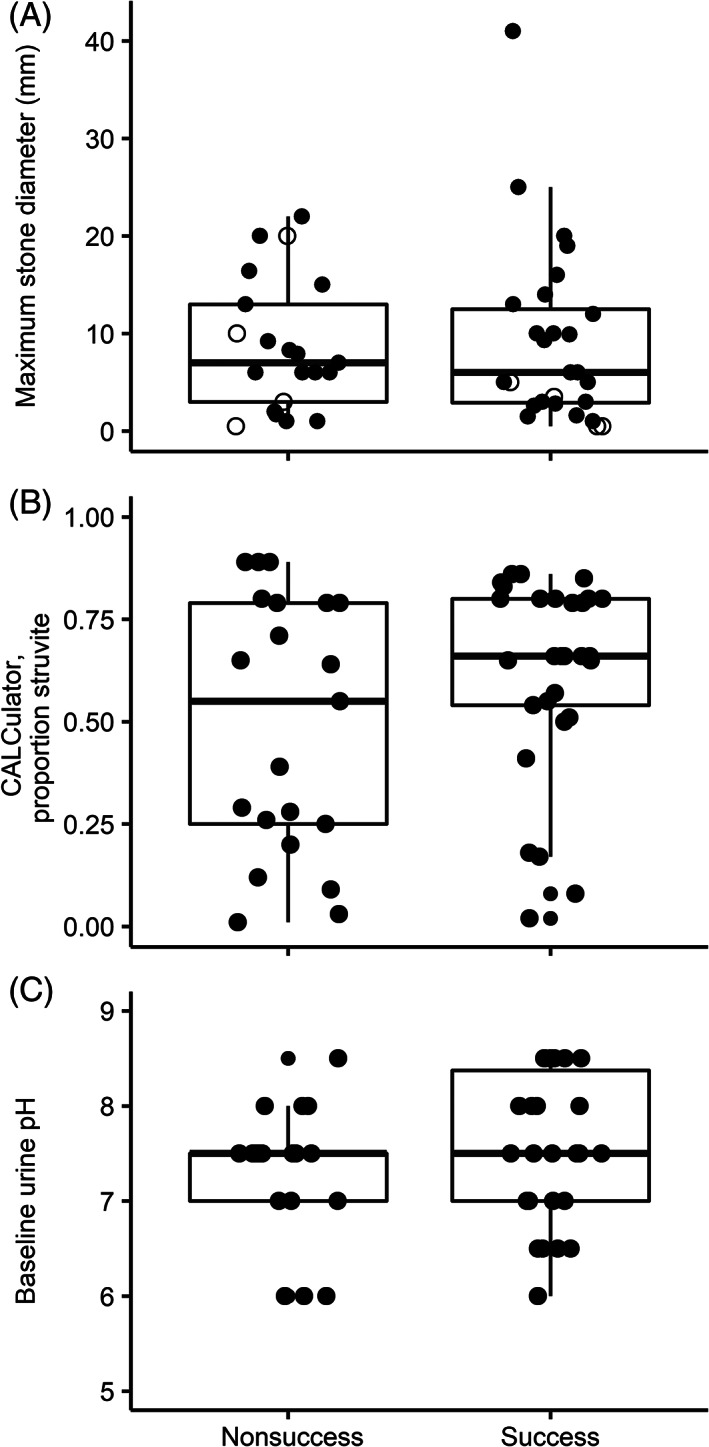
Box and whisker plots of A, maximum stone diameter, B, Minnesota Urolith Center CALCulator data for the proportion of uroliths composed of struvite submitted from dogs that match the dog signalment, and C, baseline urine pH in dogs that had successful dissolution of suspected struvite cystoliths compared to nonsuccessful dissolution (partial dissolution, failure, or undetermined outcome). The dots represent values for each individual dog; in panel A, the closed dots represent measurements obtained through radiography and open dots are those obtained through ultrasonography. The boxes represent the 25th and 75th percentiles and whiskers represent 1.5 times the interquartile range. The success and nonsuccess groups did not differ significantly for these 3 comparisons (P = .6, .19, and .32, respectively)
FIGURE 4.
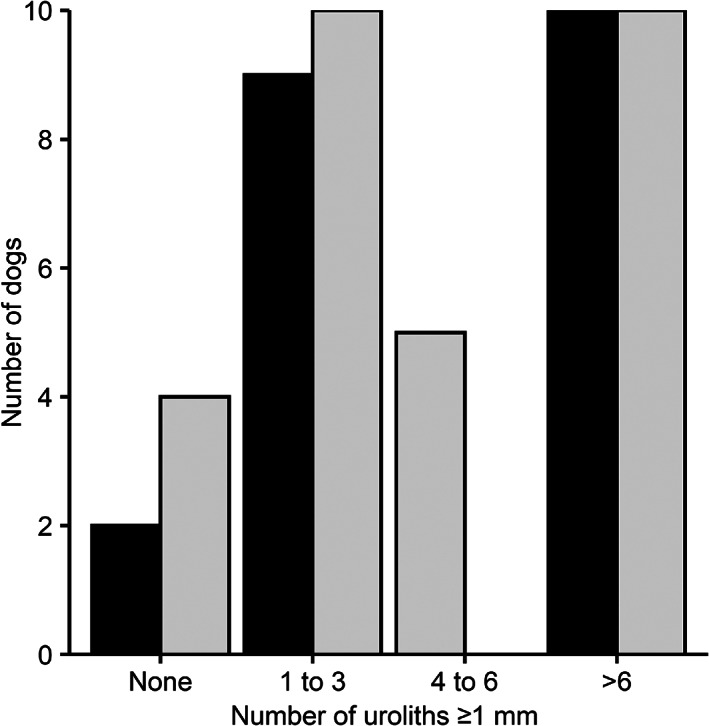
Distribution of number of uroliths ≥1 mm in dogs with and without successful dissolution of suspected struvite cystoliths. The success and nonsuccess groups did not differ significantly (P = .67)
The baseline urine pH was not significantly different between dogs with and without successful dissolution (Figure 3C, P = .32). Urinalyses during treatment were available for 13 dogs with success and 8 dogs without. Both urine pH and USG decreased during the dissolution trial (P = .007 and <.001, respectively; Figure 5). The median treatment urine pH was 6.5 (range, 5‐8.5; IQR 6‐7). The median treatment USG was 1.015 (range, 1.003‐1.035; IQR 1.01‐1.021). Neither urine pH nor USG during treatment differed significantly between dogs with and without successful dissolution (Figure 5, P = .97 and .91, respectively).
FIGURE 5.
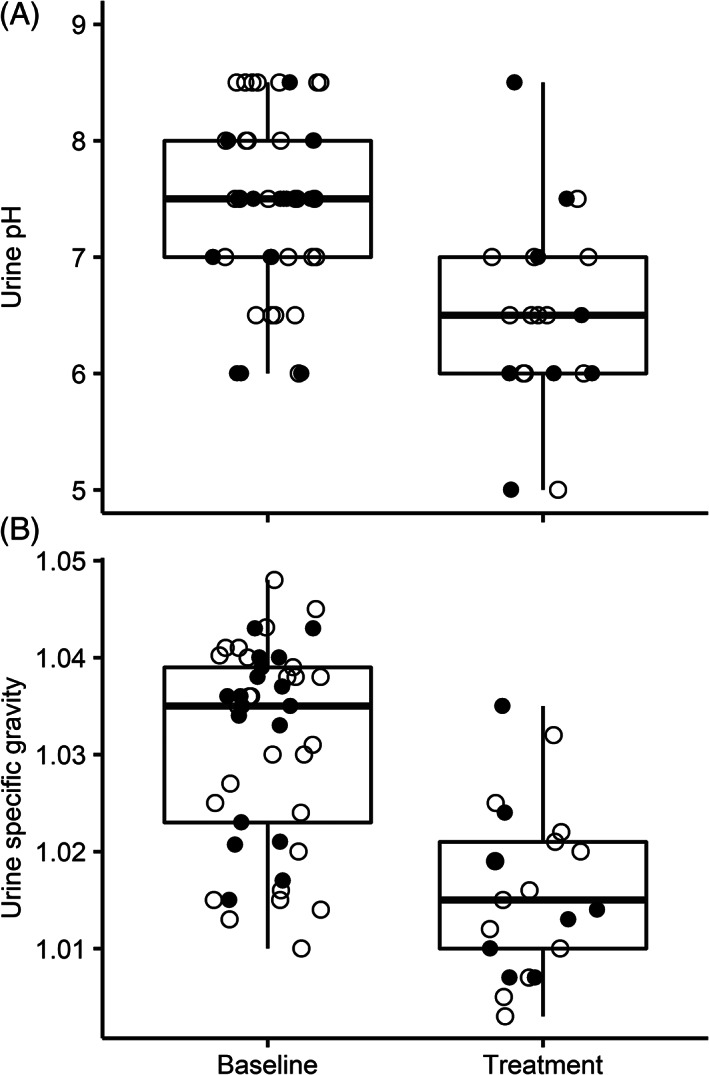
Box and whisker plots of A, urine pH and B, urine specific gravity at baseline and last follow‐up in dogs undergoing a medical dissolution trial (treatment) for suspected struvite cystoliths. The dots represent values for each individual dog that did (open dots) or did not (closed dots) achieve successful full dissolution of cystoliths. The boxes represent the 25th and 75th percentiles and whiskers represent 1.5 times the interquartile range. Both urine pH (P = .007) and urine specific gravity (P < .001) decreased with treatment
Dogs that received antimicrobial therapy, in addition to the therapeutic urinary diet, were more likely to achieve success (28/41, 68%; OR 16.3, 95% CI 1.9‐787.4, P = .002) than those that did not (1/9, 11%). The median duration of antimicrobial therapy was 30 days (range, 5‐186; IQR 16‐38) for dogs that did and 16 days (range, 6‐272; IQR 14‐35) for dogs that did not achieve success (P = .39). The distribution of antimicrobial therapy duration is presented in Figure 2.
4. DISCUSSION
Dissolution of cystoliths using a therapeutic dissolution diet, often combined with antimicrobial therapy, was successful in the majority of dogs (58%) in our retrospective study. Of the dogs with only partial dissolution, dissolution failure, or undetermined outcome, most (69%) of those with urolith analysis available had >10% nonstruvite mineral compositions. The most common complication during dissolution trials was urethral obstruction, which primarily occurred in dogs with a urethral obstruction on initial presentation and retrograde urohydropulsion before starting the dissolution trial. Other complications were uncommon and included pancreatitis, vomiting and inappetence of undetermined etiology, and persistent signs of lower urinary disease.
Effectiveness of therapeutic urinary diets for struvite urolith dissolution in dogs ranges from 50% to 100% in study reports.5, 7, 9 This likely reflects differences in the study sample of dogs undergoing the dissolution trial. In this retrospective study, we included all dogs that were prescribed a therapeutic urinary diet for suspected struvite cystoliths, whether or not they had confirmation of a urease‐producing UTI. However, results were similar to a prospective clinical trial on dissolution of naturally‐occurring uroliths in dogs with confirmed urease‐producing bacterial UTI using a dry therapeutic urinary diet and antimicrobials.9 In the prospective clinical trial, uroliths fully dissolved in 5/10 dogs within a median of 31 days.9 For comparison, uroliths completely dissolved in 29/50 dogs (58%) in the present study within a median of 35 days. In both the present study and prospective clinical trial, most cases that failed to achieve dissolution had mixed or compound uroliths with >10% of a nonstruvite component such as calcium or urate.9 Results of these studies support discontinuation of the dissolution trial if urolith burden is not reduced within 1 to 2 months, because of the likelihood of a nonstruvite composition. Prolongation of the trial might result in unnecessary antimicrobial and dietary therapy. For example, in the present study, 1 dog received both antimicrobials and the therapeutic diet for 272 days with no reduction in stone burden before ultimately undergoing a cystotomy and finding uroliths composed of calcium oxalate.
One aim of this study was to identify differences between dogs with and without success that might serve as predictors to select dogs most likely to benefit from a dissolution trial, including likelihood of struvite (based on signalment), maximum urolith diameter, urolith number, and urine pH. Dogs with struvite as the most likely composition, as determined using the MUC CALCulator, had a greater proportion with success than those where other compositions were more likely. However, the likelihood of struvite varied greatly in dogs with and without success, with substantial overlap between groups. There were dogs in the success group with a struvite likelihood less than 25% and some in the nonsuccess groups with struvite likelihoods greater than 75%. This demonstrates that even if struvite uroliths are not the most probable based on signalment, there is still a chance for dissolution. Clinician suspicion for a struvite composition likely influenced these results, as dogs with a low likelihood of struvite based on MUC CALCulator results might have had other clinical data to support a struvite composition and justify the dissolution trial. For example, the success group included a 7 year old male neutered Bichon Frise with only a 2% probability of struvite based on the MUC CALCulator results but a documented Staphylococcus UTI, alkaline urine pH, and cystoliths reported by the radiologist to have “low mineral opacity.”
Neither maximum urolith size nor number was associated with success. Most uroliths in the study sample were <2 cm in diameter. The largest urolith was 4.1 cm and was successfully dissolved. In contrast, the previous clinical trial reported failure of dissolution in 2 dogs with struvite uroliths >3 cm.9 Because of the small number of dogs with uroliths >3 cm in both studies, we cannot conclude whether or not dissolution success is impacted at this end of the size range.
Urine pH at baseline did not differ between dogs with and without success. The rationale for this comparison was that dogs with struvite uroliths are more likely to have alkaline urine than those with other stone compositions, and urine pH might predict which uroliths can be dissolved. However, some dogs were already receiving antimicrobials at the time the dissolution trial was initiated, and the urine pH might not have reflected the environment when the urolith first formed. Furthermore, dogs with calcium oxalate uroliths often have neutral or alkaline urine,10 and it is therefore not possible to rule out nonstruvite compositions based on pH.
Urine pH was not associated with outcome, although it did decrease significantly when dogs were fed the therapeutic diet similar to other studies.9, 11 The USG decreased with treatment. The therapeutic urinary diet in this study was a canned diet and is supplemented with sodium in order to further increase water consumption.5 In addition, the low dietary protein content promotes polyuria, secondary to decreased renal medullary urea concentration.5 While dilute urine should theoretically increase dissolution, the prospective trial on a dry therapeutic urinary diet achieved a similar success rate to the present study, despite an increase in USG in dogs with full dissolution.9
We additionally tested the association between antimicrobial therapy during the trial and outcome. A greater success rate was found in dogs that received antimicrobials during the dissolution trial. However, we cannot conclude that the lack of antimicrobial therapy was the cause of failure for any dog because urolith compositions for most dogs with partial or no dissolution contained nonstruvite components that are not amenable to dissolution. The association between antimicrobial therapy and outcome might be because of the fact that dogs without evidence of a UTI are both less likely to be prescribed antimicrobials and less likely to have uroliths composed of struvite. Of note, 1 successful dissolution occurred without antimicrobial therapy during the dissolution trial; the dog did not have evidence of a UTI at the start of the dissolution trial.
The optimal duration of antimicrobial therapy during a dissolution trial for suspected struvite cystoliths is not well established. Standard recommendations are to continue antimicrobial therapy until or beyond the time of radiographic dissolution,3, 5 but this has recently been questioned with shorter courses proposed.12 In the present study, nearly two thirds of the dogs with successful dissolution had antimicrobial therapy discontinued before documentation of full dissolution on medical imaging, with a median antimicrobial duration of 4 weeks. In most cases, a follow‐up visit did not occur between the time when the antimicrobial therapy was discontinued and the medical imaging that confirmed full dissolution. In those dogs, it was not possible to determine whether or not cystoliths had already dissolved by the time of antimicrobial discontinuation. However, there were 3 dogs in the success group with confirmed cystolith persistence at or after antimicrobial discontinuation. One of these dogs had UTI recurrence 2 weeks after antimicrobial discontinuation and was therefore restarted on therapy until full dissolution occurred. We are unable to draw conclusions from the dogs in this study sample as to whether antimicrobial discontinuation before full cystolith dissolution significantly affects the risk for UTI recurrence, likelihood of dissolution, or speed of dissolution. Furthermore, the interpretation of success with relatively short (≤14 days) courses of antimicrobial therapy is complicated by individual histories. For example, the dog in the success group with the shortest antimicrobial duration (5 days) was a male Pug with numerous small (<0.5 mm) cystoliths, a negative urine culture at the baseline visit, and no history of a prior UTI or antimicrobial therapy. Sterile struvite urethral plugs and cystoliths have been previously reported in Pugs,13 and antimicrobial therapy is not expected to influence dissolution success for this condition.
A limitation of the study is that it only included cases that received a therapeutic urinary diet and does not inform dissolution success rates with antimicrobials alone. The study results did find that dogs with confirmed or suspected UTIs despite current or recent antimicrobial therapy. This supports the need to perform a urine culture in dogs with suspected struvite uroliths, even if there is recent history of antimicrobial therapy. As expected, most UTIs in the present study were caused by Staphylococcus spp. However, 2 dogs had UTIs with bacteria that do not typically produce urease, Enterococcus spp. and E. coli. The dog with Enterococcus spp. was found to have calcium oxalate uroliths, but the dog with an E. coli UTI had confirmed struvite uroliths. Though uncommon, there are reports of uropathogenic E. coli with urease gene expression.14
We documented adverse events that might be attributed to the dissolution trial and found that urethral obstruction was the most common, occurring in 4/50 dogs. All but 1 dog with this complication presented with a urethral obstruction, before the dissolution trial was initiated. Current consensus on urolith management states that urethral obstruction should preclude clinicians from recommending medical dissolution.4 The findings of this study confirm that dogs with a urethral obstruction are not ideal candidates for a dissolution trial, even if the uroliths are first urohydropropulsed back into the bladder. For dogs without a history of a urethral obstruction, risk of this complication during the dissolution trial is low.
Other complications reported during the trial were pancreatitis or vomiting and inappetence of undetermined etiology. Per the manufacturer, 1 of the contraindications of the therapeutic diet in this study is that it should not be fed to dogs with a history of pancreatitis, or risk factors for pancreatitis, such as breed predispositions.15 We did not evaluate medical records to determine if dogs that developed pancreatitis, vomiting, or inappetence during the trial had a history of pancreatitis. Of the 4 dogs who experienced these complications, only 1 dog was a breed explicitly listed by the manufacturer as predisposed to pancreatitis. Since this study only evaluated a single diet, we cannot determine if the frequency of gastrointestinal complications is different for other therapeutic urinary diets.
Because of the retrospective study design, standardized criteria were not used to select dogs for medical dissolution therapy. This might have resulted in inclusion of dogs with a low likelihood of struvite cystoliths, such as those without a urease‐producing UTI, and thus decreased the success rate. Alternatively, there might have been a stronger clinical suspicion for struvite composition in the study dogs relative to those undergoing dissolution trials in general. The study was restricted to a diet that is exclusively recommended for struvite dissolution and is not formulated for long‐term maintenance. In contrast, other therapeutic urinary diets are recommended for multiple urolith types and are maintenance diets. Thus, diet selection might reflect degree of suspicion for a struvite composition.
Follow‐up to determine all case outcomes and reasons for decisions (such as discontinuation of the dissolution trial) was incomplete. Dogs with partial dissolution or undetermined outcomes were treated as nonsuccesses, along with the confirmed failures, to avoid bias. However, this approach likely underestimates the success rate. Time to first noted decrease in stone burden and to full dissolution reported in this study were based on when the dog presented for reevaluation, which was highly variable, and might overestimate true dissolution times. Diagnostic imaging modality also varied among dogs. While most dogs were imaged with radiography, a subset were imaged with ultrasonography. Ultrasonographic images overestimate cystolith size, and this might have introduced minor inaccuracies in urolith measurements.16 Treatment regimens were also not standardized, as they were selected by the clinician managing the case at the time. An advantage of our study approach is that it reflects expected success rates in clinical practice, though the study was conducted at an academic referral hospital which might differ in the dog sample and treatment protocols compared to general practice hospitals.
Although this retrospective study assessed multiple predictors of success for medical dissolution of struvite cystoliths, most were not informative, and other methods to improve the accuracy of prediction are needed. Recheck abdominal radiographs should be performed approximately 1 month after diet therapy is initiated to assess efficacy. If no dissolution is noted, a nonstruvite composition is likely. Serious adverse events are uncommon during medical dissolution, with the exception that dogs presenting with urethral obstruction often reobstruct. Thus, medical dissolution trials are not recommended for dogs with urethral obstructions.
CONFLICT OF INTEREST DECLARATION
Jody Lulich and Eva Furrow are members of the Minnesota Urolith Center which is supported in part by an educational gift from Hill's Pet Nutrition. No other authors have a conflict of interest.
OFF‐LABEL ANTIMICROBIAL DECLARATION
Ciprofloxacin and trimethoprim sulfa are not labeled for use in dogs. Some dogs received antimicrobial therapy for a duration longer than the product label recommends.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC) OR OTHER APPROVAL DECLARATION
Authors declare no IACUC or other approval was needed.
HUMAN ETHICS APPROVAL DECLARATION
Authors declare human ethics approval was not needed for this study.
ACKNOWLEDGMENT
Partial funding for Eva Furrow provided by a National Institutes of Health ORIP K01 Mentored Research Scientist Development Award (K01‐OD019912).
Wingert AM, Murray OA, Lulich JP, Hoelmer AM, Merkel LK, Furrow E. Efficacy of medical dissolution for suspected struvite cystoliths in dogs. J Vet Intern Med. 2021;35(5):2287‐2295. doi: 10.1111/jvim.16252
Funding information National Institutes of Health, Grant/Award Number: K01‐OD019912
REFERENCES
- 1.Low WW, Uhl JM, Kass PH, et al. Evaluation of trends in urolith composition and characteristics of dogs with urolithiasis: 25,499 cases (1985‐2006). J Am Vet Med Assoc. 2010;236:193‐200. [DOI] [PubMed] [Google Scholar]
- 2.Lulich JP, Osborne CA, Albasan H, Koehler LA, Ulrich LM, Lekcharoensuk C. Recent shifts in the global proportions of canine uroliths. Vet Rec. 2013;172:363. [DOI] [PubMed] [Google Scholar]
- 3.Houston DM, Weese HE, Vanstone NP, Moore AE, Weese JS. Analysis of canine urolith submissions to the Canadian Veterinary Urolith Centre, 1998‐2014. Can Vet J. 2017;58:45‐50. [PMC free article] [PubMed] [Google Scholar]
- 4.Lulich JP, Berent AC, Adams LG, Westropp JL, Bartges JW, Osborne CA. ACVIM small animal consensus recommendations on the treatment and prevention of uroliths in dogs and cats. J Vet Intern Med. 2016;30:1564‐1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osborne CA, Lulich JP, Polzin DJ, et al. Medical dissolution and prevention of canine struvite urolithiasis. Twenty years of experience. Vet Clin North Am Small Anim Pract. 1999;29:73‐111. [DOI] [PubMed] [Google Scholar]
- 6.Lulich JP, Osborne CA. Lower urinary tract urolithiasis in dogs. In: Ettinger SJ, Feldman EC, Cote E, eds. Textbook of Veterinary Internal Medicine. 8th ed.St. Louis, MO; Elsevier, Inc; 2017:1996‐2004. [Google Scholar]
- 7.Abdullahi SU, Osborne CA, Leininger JR, Fletcher TF, Griffith DP. Evaluation of a calculolytic diet in female dogs with induced struvite urolithiasis. Am J Vet Res. 1984;45:1508‐1519. [PubMed] [Google Scholar]
- 8.Rinkardt NE, Houston DM. Dissolution of infection‐induced struvite bladder stones by using a noncalculolytic diet and antibiotic therapy. Can Vet J. 2004;45:838‐840. [PMC free article] [PubMed] [Google Scholar]
- 9.Dear JD, Larsen JA, Bannasch M, et al. Evaluation of a dry therapeutic urinary diet and concurrent administration of antimicrobials for struvite cystolith dissolution in dogs. BMC Vet Res. 2019;15:273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kennedy SM, Lulich JP, Ritt MG, Furrow E. Comparison of body condition score and urinalysis variables between dogs with and without calcium oxalate uroliths. J Am Vet Med Assoc. 2016;249:1274‐1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calabrò S, Tudisco R, Bianchi S, Grossi M, de Bonis A, Isabella Cutrignelli M. Management of struvite uroliths in dogs. Br J Nutr. 2011;106:S191‐S193. [DOI] [PubMed] [Google Scholar]
- 12.Weese JS, Blondeau J, Boothe D, et al. International Society for Companion Animal Infectious Diseases (ISCAID) guidelines for the diagnosis and management of bacterial urinary tract infections in dogs and cats. Vet J. 2019;247:8‐25. [DOI] [PubMed] [Google Scholar]
- 13.Stiller AT, Lulich JP, Furrow E. Ureteral plugs in dogs. J Vet Intern Med. 2014;28:324‐330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collins CM, Falkow S. Genetic analysis of Escherichia coli urease genes: evidence for two distinct loci. J Bacteriol. 1990;172:7138‐7144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prescription Diet s/d Canine Hill's Key to Clinical Nutrition; 2020. https://www.hillsvet.ca/en-ca/practice-management/hills-key-to-clinical-nutrition. Accessed February 17, 2020.
- 16.Byl KM, Kruger JM, Kinns J, Nelson NC, Hauptman JG, Johnson CA. In vitro comparison of plain radiography, double‐contrast cystography, ultrasonography, and computed tomography for estimation of cystolith size. Am J Vet Res. 2010;71:374‐380. [DOI] [PubMed] [Google Scholar]


