Supplemental Digital Content is available in the text.
Keywords: social mixing, contact patterns, physical distancing, SARS-CoV-2 transmission, COVID-19 pandemic
Background:
Physical distancing measures aim to reduce person-to-person contact, a key driver of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission. In response to unprecedented restrictions on human contact during the coronavirus disease 2019 (COVID-19) pandemic, studies measured social contact patterns under the implementation of physical distancing measures. This rapid review synthesizes empirical data on the changing social contact patterns during the COVID-19 pandemic.
Method:
We conducted a systematic review using PubMed, Medline, Embase, and Google Scholar following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. We descriptively compared the distribution of contacts observed during the pandemic to pre-COVID data across countries to explore changes in contact patterns during physical distancing measures.
Results:
We identified 12 studies reporting social contact patterns during the COVID-19 pandemic. Eight studies were conducted in European countries and eleven collected data during the initial mitigation period in the spring of 2020 marked by government-declared lockdowns. Some studies collected additional data after relaxation of initial mitigation. Most study settings reported a mean of between 2 and 5 contacts per person per day, a substantial reduction compared to pre-COVID rates, which ranged from 7 to 26 contacts per day. This reduction was pronounced for contacts outside of the home. Consequently, levels of assortative mixing by age substantially declined. After relaxation of initial mitigation, mean contact rates increased but did not return to pre-COVID levels. Increases in contacts post-relaxation were driven by working-age adults.
Conclusion:
Information on changes in contact patterns during physical distancing measures can guide more realistic representations of contact patterns in mathematical models for SARS-CoV-2 transmission.
Close, person-to-person interactions drive how respiratory infections, such as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), spread through populations. Physical distancing measures aim to mitigate the spread of respiratory infections by reducing the quantity and intensity of person-to-person contacts. In response to the first waves of coronavirus disease 2019 (COVID-19) in the spring and summer of 2020, countries around the world announced government-mandated lockdowns and implemented drastic physical distancing measures such as city-wide stay-at-home orders and curfews, school closures, cancellation of large gatherings, and suspension of operations for nonessential businesses to curb transmission of SARS-CoV-2. These strategies were generally associated with reductions in COVID-19 cases,1,2 yet the impact varied widely across countries and age groups.
In response to these unprecedented restrictions on human contact and movement, a number of studies measured social contact patterns under physical distancing measures. These studies recorded the number of contacts made by participants over a 24-hour period, attributes of each contact (location, proximity, and duration), and demographic characteristics of contacts (gender and age). This information describes the topography of contact patterns by age, location, and other characteristics important for understanding how physical distancing measures may result in changes in transmission patterns over time.
Social contact studies conducted prior to the pandemic provide an important reference for contact patterns before physical distancing measures. Pre-pandemic estimates include both empirically collected data such as the POLYMOD3 study conducted in 2008 and simulated data.4,5 Age, gender, household size, and day of the week are determinants of contact rate.3,6,7 Contact patterns are consistently assortative by age, meaning that individuals contact other individuals of the same age group at a higher frequency than those in other age groups. Contact location further dictates age-specific mixing patterns. Mixing of children at school tends to be highly assortative while mixing at workplaces for adults is less assortative. At the population level, demographic characteristics, family structure, and culture-specific practices4,5 further influence contact structure. In European countries, contact among the elderly is assortative.3 In contrast, in Zimbabwe7 and Kenya,8 elderly individuals more proportionally contact individuals of different ages due to a younger population age distribution and the practice of residing in extended families. Heterogeneity in contact patterns can result in differential impact of physical distancing measures on transmission.
Data on social contact patterns, and their changes in response to physical distancing measures, form a critical input for mathematical models of infectious diseases, such as SARS-CoV-2. Mathematical models are widely used to understand infection dynamics, forecast outbreak trajectories, and evaluate the impact of control measures such as stay-at-home orders and school closures on disease transmission.9–12 Variation in age-specific and location-specific contact patterns underpin transmission dynamics, determining the size and timing of an epidemic peak,13 population groups most susceptible to early infection, and how infection propagates through social networks.14 For example, models for seasonal influenza show that outbreaks are driven by intense contact at school between school-aged children followed by secondary transmission to household members.15,16 The influence of contact patterns (between and within age groups and at specific locations) on transmission highlights the value of incorporating age-specific, location-stratified contact rates to more realistically simulate the spread of infection.17–20 Understanding to what extent contact patterns are generalizable, or more context-specific, across countries can aid modelers in parameterizing transmission models that aim to answer critical questions about the control and prevention of SARS-CoV-2.
This rapid review aims to synthesize information on the changing social contact patterns during the COVID-19 pandemic. We describe the distribution of contact rates observed during the period of initial mitigation in the spring of 2020 when the most stringent interventions were in place and during periods of relaxation compared to pre-COVID contact rates. We use the time periods of government-declared lockdowns and the Oxford Stringency Index (OSI)21 to broadly categorize data collection periods. We further explore changes stratified by age group, contact location, gender, and household size, and compare reductions in contacts across age-specific contact matrices. Last, we describe how studies used changes in contact patterns to estimate the impact of physical distancing measures on SARS-CoV-2 transmission.
METHODS
We developed our protocol and reported our findings according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.22
Eligibility
We considered for review all published articles on face-to-face social contact patterns collected from surveys conducted between the beginning of physical distancing measures to contain the COVID-19 pandemic (15 January 2020) and time of last search (15 February 2021). The inclusion criteria were adapted from a previously published systematic review on social contact patterns conducted in 2017.6 According to the following criteria, we selected the studies that (1) primarily focused on face-to-face contacts of humans, implying the physical presence of at least two persons during contact; (2) collected information through an online survey, by phone, or face-to-face interview with a participant; (3) quantified contact patterns during implementation of physical distancing measures by government (federal or state) to control the COVID-19 pandemic; (4) included a comparison with contact patterns prior to the COVID-19 pandemic (either based on participant recall or data available through another comparable study); and (5) considered as target the general population rather than a specific population group such as households with children, office workers, or hospital staff. We excluded studies that (1) primarily focused on human–animal or animal–animal contacts or contacts exclusively relevant for sexually transmitted, food-borne, vector-borne, or water-borne diseases; (2) were not conducted during the COVID-19 pandemic period; (3) included contact without physical presence, such as through phone or social media, without the ability to distinguish from in-person contacts; and (4) did not collect empirical data but rather used mobility data or pre-COVID data as proxies.
Search Strategy
Literature searches were conducted in PubMed, Medline, Embase, and Google Scholar and included pre-print articles in MedRxiv and bioRxiv from 15 January 2020 to 15 February 2021. We considered search terms used in a previously published systematic review on social contact patterns6 and made adjustments to include articles that collected data during the COVID-19 pandemic (eAppendix 1; http://links.lww.com/EDE/B848).
Selection Process
We screened articles first by reviewing title and abstract and then, if determined to fit inclusion and exclusion criteria, reviewing the full-article text. We used a data extraction sheet to record key information. Two independent reviewers familiar with social contact studies performed full-text review and data extraction with a third reviewer arbitrating on discrepancies.
Data Management and Extraction
We used Zotero (V 5.0) and Covidence Systematic Review Software by Veritas Health Innovation to manage references and articles. We conducted title and abstract screening within Covidence. We downloaded articles selected for full-text review and imported them into Zotero. For our data synthesis of contact patterns, we collated data from supplementary materials; http://links.lww.com/EDE/B848 and public repositories such as publicly-available social contact datasets hosted on the Zenodo platform.23–29
Data Synthesis/Analysis
Physical distancing measures varied by location. To provide context for contact data, we used government (national and provincial/state) declaration of lockdowns (SI.6) and the OSI21 for each country to broadly categorize data collection periods into the following (1) initial mitigation period characterized by national and/or regional declaration of lockdown and the most stringent OSI measures; (2) 1-month after relaxation of initial mitigation, defined as one month after the beginning of relaxation of any physical distancing measures, and (3) 2 or more months after relaxation. The OSI is a composite index of nine mitigation interventions weighted on strictness and has been used to compare the impact of mitigation policies across countries.30,31 The nine interventions included in the OSI are stay-at-home orders, closure of schools, workplaces and public transport, restrictions on gatherings, cancellation of public events movement restrictions, and international travel controls.
For our data synthesis, we compared the mean contact rates per person under different periods of physical distancing measures during COVID-19 with pre-COVID contacts for each country or region. Data were either extracted from studies or GitHub repositories, requested from authors, or calculated via the RShiny application SOCRATES24 (http://www.socialcontactdata.org/socrates/) (eTable 1; http://links.lww.com/EDE/B848). SOCRATES enables users to access empirical social contact data collected pre-pandemic stratified by country, age groups, and contact location, weighted to survey sampling weights. Since a few studies covered the same countries, multiple results for the same country were possible. We summarized the mean daily contact rate per person pre-COVID and during COVID stratified by age group, gender or sex, household size, and contact location. Categorizations for age group and contact location varied between studies. For age group, we used the smallest age group categorization reported and ensured the same age group categories were used both pre-COVID and during COVID. For location, we used categories of home, school, work, and others, where others include public transport, someone else’s home, and other general community locations such as grocery stores, bars, restaurants, parks, healthcare facilities, or church.
Changes in Age Mixing
To calculate changes in age-specific contacts, we compared age-specific contact matrices before and during initial mitigation (details on data sources in eTable 2; http://links.lww.com/EDE/B848). Age-specific contact matrices summarize the mean daily contact rates made by a participant from age group i with a contact from age group j. We estimate the absolute change in age-specific contacts with Eq 1. We further explored changes in age-specific and location stratified matrices (Methods in eAppendix 2; http://links.lww.com/EDE/B848).
Ethics
An Institutional Review Board (IRB) review was not required since we used data from previously published studies that was publicly available and not identifiable.
RESULTS
Summary of Articles Included
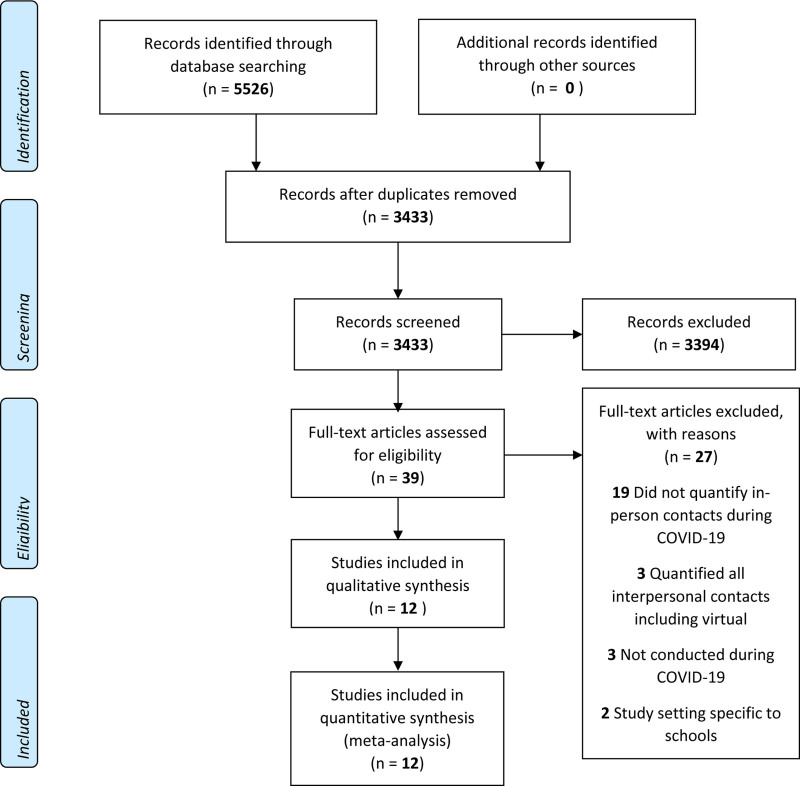
A total of 5,527 unique records were identified from our search strategy. During title and abstract screening, articles from other areas of research during the COVID-19 pandemic (e.g., economic impact, psychological impact, and socio-behavioral impact) or modeling studies that solely used contact data as model inputs but did not collect empirical data were excluded. After title and abstract screening, we reviewed the full text of 39 studies of which we selected 12 for inclusion in our review (Figure 1 and Table). We excluded articles during full-text review if they did not quantify contacts during COVID-19 (n = 19), included virtual contacts (n = 3), did not collect data during COVID-19 (n = 3), or were specific to school settings (n = 2) (details in eTable 3; http://links.lww.com/EDE/B848). All studies except one32 were based on surveys conducted in single countries. The majority (8/12) of studies were based in high-income countries: European countries (n = 6), the United States (n = 1) or both (n = 1). Eight studies surveyed participants with the intention of describing contact patterns representative of an entire country32–39 and four studies aimed to describe subnational areas such as cities (Shanghai and Wuhan in one study, Shenzhen and Changsha in a second),40,41 an informal settlement in Nairobi, Kenya42 and a district in KwaZulu-Natal, South Africa.43 Six studies included adults aged 18 years and above only,32,34–36,38,42 four studies included participants of all ages,33,39–41 and two studies included teenagers and above.37,43
FIGURE 1.
PRISMA flow diagram for article search, title and abstract screening and full-text review. PRISMA indicates Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
TABLE.
Description of Studies Included in the Systematic Review
| Reference | Article | Authors | Country | Study Subjects | Sample Sizea | Study Design | Collection Mode | Time Periodb |
|---|---|---|---|---|---|---|---|---|
| 32 | The differential impact of physical distancing strategies on social contacts relevant for the spread of COVID-1932 | Del Fava et al | Belgium, France Germany, Italy Netherlands Spain, UK, US | Adults | 53,708 | Repeated cross-sectional | Online | 13 March to 13 April 2020 |
| 33 | The impact of physical distancing measures against COVID-19 transmission on contacts and mixing patterns in the Netherlands: repeated cross-sectional surveys33 | Backer et al | Netherlands | All age | 2,830 | One-time cross-sectional | Online | March to April 2020 |
| 34 | CoMix: comparing mixing patterns in the Belgian population during and after lockdown34 | Coletti et al | Belgium | Adults | 1,542 | Longitudinal | Online | 24 April to 30 July 2020 |
| 35 | Quantifying interpersonal contact in the US during the spread of COVID-19: first results from the Berkeley Interpersonal Contact Study35 | Feehan et al | US | Adults | 1,425 | Repeated cross-sectional | Online | 22 March to 21 September 2020 |
| 36 | Quantifying the impact of physical distance measures on transmission of COVID-19 in the UK36 | Jarvis et al | UK | Adults | 1,356 | One-time cross-sectionalc | Online | 24 March to 27 March 2020 |
| 37 | Evolving social contact patterns during the COVID-19 crisis in Luxembourg37 | Latsuzbaia et al | Luxembourg | Age 13+ | 5,664 | Repeated cross-sectional | Online | 2 April to 25 June 2020 |
| 38 | Lockdown impact on age-specific contact patterns and behaviors in France38 | Bosetti et al | France | Adults | 42,036 | One-time cross-sectional | Online | 10 April to 28 April 2020 |
| 39 | Modelling the SARS-CoV-2 first epidemic wave in Greece: social contact patterns for impact assessment and an exit strategy from physical distancing measures39 | Sypsa et al | Greece | All ages | 602 | One-time cross-sectional | Phone | 31 March to April 2020 |
| 40 | Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China40 | Zhang et al | China | All ages | 1,193 | One-time cross-sectional | Phone | 1 February to 10 February 2020 |
| 41 | The impact of relaxing interventions on human contact patterns and SARS-CoV-2 transmission in China41 | Zhang et al | China | All ages | 9,205 | One-time cross-sectional | Phone | 1 March to March or 7 May to 15 May 2020 |
| 42 | The impact of COVID-19 control measures on social contacts and transmission in Kenyan informal settlements42 | Quaife et al | Kenya | Adults | 213 | One-time cross-sectional | Phone | May 2020 |
| 43 | Impact of social distancing regulations and epidemic risk perception on social contact and SARS-CoV-2 transmission potential in rural South Africa43 | McCreesh et al | South Africa | Age 15+ | 216 | Repeated cross-sectional | Phone | 3 June to 17 August 2020 |
aFor studies that collected data over multiple waves, sample size refers to participants from the first wave of data collection during lockdown.
bTime period described here refers to the entire data collection period presented in each study even if we do not present data for all waves of data collection.
cThe UK CoMix study continues to collect data on contact patterns in the UK. For this review, we include data from the published manuscript that presents data on only the first wave.
COVID-19 indicates coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
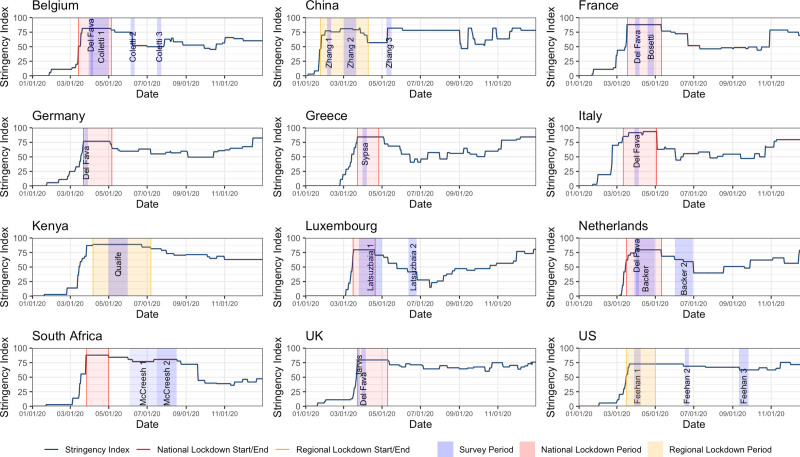
Eleven32–42 studies collected data during the initial mitigation period between February and May 2020 with the most stringent physical distancing measures (Figure 2) with seven32–34,36–39 collecting data during nationally declared lockdown and four35,40–42 during regional lockdown. Five33–35,37,41 studies also collected additional data when interventions were relaxed (April and May for China and between May and September for other settings) and one43 study collected data exclusively during the period of relaxation.43 Policies in place during data collection period were similar but varied (eTable 4; http://links.lww.com/EDE/B848 and eFigure 7; http://links.lww.com/EDE/B848) as did the epidemic situation (eFigure 1; http://links.lww.com/EDE/B848). The majority of studies were one-time cross-sectional surveys,33,36,38–42 one was longitudinal (a cohort of participants repeatedly responded to surveys over time),34 and four were repeated cross-sectional surveys (surveys were repeated over time with different participants).32,35,37,43 The majority (7/12) used online surveys to recruit participants and collect contact data, while the remaining studies were conducted using phone-based surveys. Sample sizes ranged from 200 for the study conducted in Nairobi, Kenya42 to approximately 54,000 for one study conducted across several countries.32 The exact definitions of contacts varied but most studies described a contact as either physical (defined as skin-to-skin touching) or conversational (defined as being within 2 meters or arms-length with another person for an exchange of two or more words) (eTable 5; http://links.lww.com/EDE/B848).3
FIGURE 2.
Timing of contact surveys for each country with the Oxford Stringency Index (OSI) for stringency of physical distancing measures, time period of government-mandated lockdowns for context. Contact data collected during either government-mandated lockdowns or during the most stringent OSI in the spring of 2020 were classified as contacts during initial mitigation measures and data collected after the initial mitigation measures were classified as post-relaxation.
Overall Mean Contacts During Initial Mitigation
During the initial mitigation period between February and May 2020, the mean contact rates reported by participants was two to five per day for most (16/18) study settings (eTable 6; http://links.lww.com/EDE/B848), equivalent to a 65%–87% reduction in mean contact rate compared to pre-COVID contact rates of seven to 26 per person per day. The reduction in contact rates corresponded with a shift in the distribution of contacts, with fewer participants reporting extremely high numbers of contacts during initial mitigation. One study conducted in informal settlements in Nairobi, Kenya, found a high mean of 18 contacts per person per day, though the authors estimate that this still represented a reduction relative to the pre-COVID period.
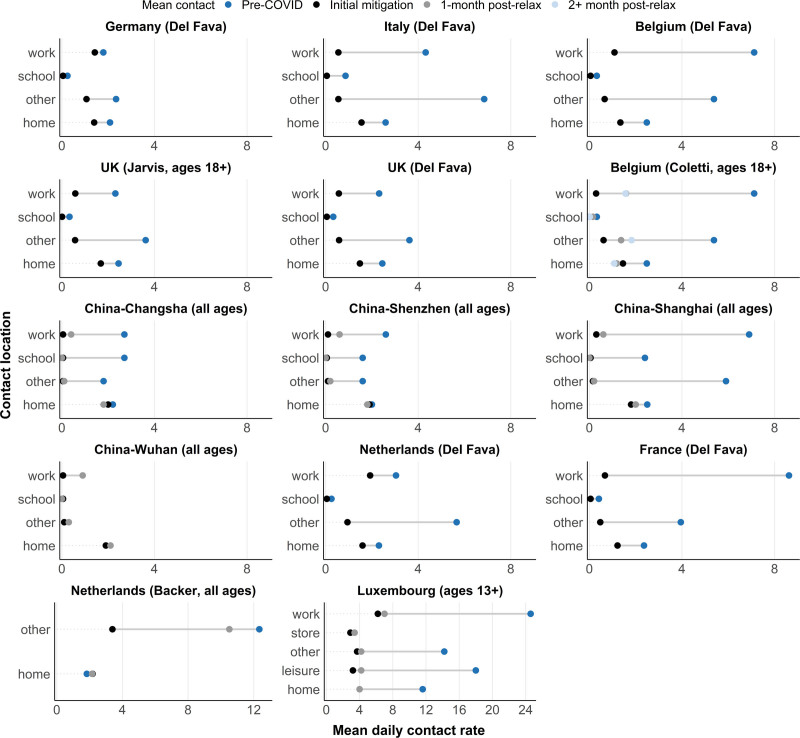
Marked Reductions in Contacts Outside of Home During Initial Mitigation
We compared changes in the mean contact rates by contact location (Figure 3 and eFigure 2; http://links.lww.com/EDE/B848). All study settings showed marked reductions in contacts at work and in the general community (e.g., public transport, restaurants and bars, and other places of leisure). Percent reductions in work contacts varied: cities in China observed a 100% reduction, while Italy, UK, Belgium, Luxembourg, and France observed a 75%–90% reduction. Germany and the Netherlands observed the lowest reductions, at 24% and 27%, respectively. Studies that included children in their sample33,40,41 showed the complete elimination (100% reduction) of contacts at school, corresponding with school closures. Similar patterns were observed among people aged 18 years or older in settings with university closures.32 Italy and China observed a nearly complete elimination (100% reduction) in contacts in the general community, while all other study settings reported a 50%–80% reduction. Some settings showed a marginal reduction in contacts at home (Luxembourg, UK, Germany, Italy, Belgium, and France), whereas other study settings showed no reduction (China and the Netherlands).
FIGURE 3.
Changes in contact rates pre-COVID (dark blue), during initial mitigation measures in spring 2020 (black), 1-month post first relaxation of mitigation measures (gray) and 2+ months post first relaxation (light blue). stratified by contact location. Estimates during COVID-19 were extracted from studies, estimates pre-COVID were either extracted from studies or from SOCRATES.24 No pre-COVID data stratified by contact location was available for Wuhan. X-axis limits for Netherlands (Backer) and Luxembourg were increased to capture larger pre-COVID contact rates. COVID-19 indicates coronavirus disease 2019.
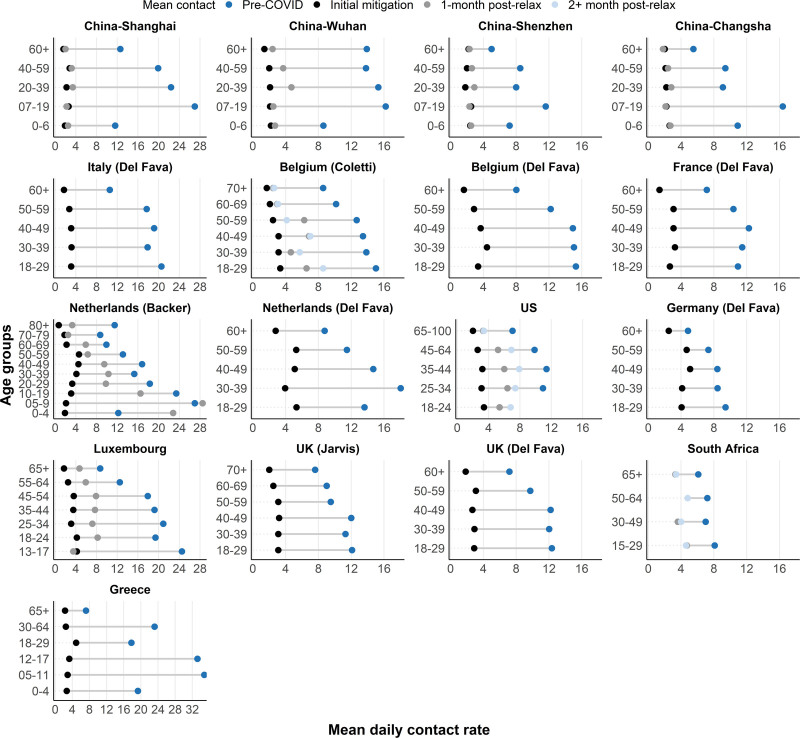
Reductions in Contacts During Initial Mitigation Driven by Reductions in Contact Between Individuals of the Same Age
During the initial mitigation, mean contact rates were similar across age groups, erasing pronounced variations in mean contacts by age group observed pre-COVID. For example, working-age adults had substantially higher contacts compared to the elderly pre-COVID. During initial mitigation, the mean contact rates between these two age groups became more comparable (Figure 4 and eFigure 3; http://links.lww.com/EDE/B848). There were noticeable reductions in assortative contacts by age for nine of ten study settings with available data (the Netherlands, Belgium, UK, US, France, and four cities in China) (eFigure 4; http://links.lww.com/EDE/B848). Due to variations in contact patterns by study setting pre-COVID, the magnitude of change varied by study. In studies that included children (the Netherlands and China), school-aged children displayed an even more pronounced reduction in age-assortative contacts, presumably due to school closures. We found pronounced reductions in assortative mixing in the general community and school (eFigure 5; http://links.lww.com/EDE/B848).3,44 We also observed smaller, but noticeable, reductions in contact at home, where reductions were more similar across contacts between age groups.
FIGURE 4.
Changes in contact rates pre-COVID (dark blue), during initial mitigation measures in spring 2020 (black), 1-month post first relaxation of mitigation measures (gray) and 2+ months post first relaxation (light blue), stratified by age group. Estimates during COVID-19 were extracted from studies, estimates pre-COVID were either extracted from studies or from SOCRATES.24 No initial mitigation data was available for South Africa. X-axis limits for Shanghai, Italy, Netherlands (Backer), Luxembourg and Greece were increased to capture larger pre-COVID contact rates. COVID-19 indicates coronavirus disease 2019.
Changes in Contact After Relaxation of Initial Mitigation Driven by Working-age Adults
Beginning in May 2020, most countries represented in this review began gradually relaxing physical distancing measures, lifting stay-at-home orders, and opening workplaces45 (eFigure 7; http://links.lww.com/EDE/B848). In the eight study settings that measured contacts within 1 month of the beginning of relaxation, mean contact rates varied between 2 and 9 per person per day, higher than mean contact rates during initial mitigation but fewer than pre-COVID levels. In seven of the eight studies, working-age adults experienced larger increases in contact rates compared to older adults and children. Notably, older adults at the highest risk for severe outcomes from SARS-CoV-2 infection46 had few increases in contact rates post-relaxation. Across all studies that measured contacts after the easing of physical distancing measures, mean contact rates had not returned to pre-COVID levels.
Other Observations in Changes in Contact Patterns
We find almost no differences in changes in contact by gender, although a few studies (France,38 Kenya,42 and Greece39) noted slightly higher contacts among men at the workplace during initial mitigation32,38 (eTable 7; http://links.lww.com/EDE/B848). Furthermore, some studies reported differential changes in contact by occupation and income level of participants. In China, employed individuals were more likely to have higher contact rates and in the Netherlands and Kenya working individuals with a lower income were more likely to have lower reductions in contact.33,40,42
Estimating Impact of Contact Changes on SARS-CoV-2 Transmission
Studies estimated the impact of physical distancing measures on transmission by calculating the change in the net reproduction number, Rt, from changes in the age-specific contact matrices. Rt is the average number of secondary infections generated by an infected individual at time t accounting for behavioral responses to the epidemic in a population that is either partially or fully susceptible. This was done by assuming that Rt under physical distancing measures is proportional to the ratio of the dominant eigenvalues of the age-specific contact matrices before and during initial mitigation.34,36 Seven studies reported comparable calculations of which 13 of 14 study settings estimated that mitigation-driven age-specific contact patterns reduced Rt between 62%–83%32–34,36,39,42 (eTable 8; http://links.lww.com/EDE/B848). In all study settings except for Germany,32 this amount of reduction was enough to bring the median estimate of Rt to below 1, suggesting a slowing of transmission under initial mitigation contact patterns. In general, larger proportional reductions in mean contact rates corresponded with larger proportional reductions in Rt. Several studies estimated Rt during the post-relaxation period. The median estimates for Rt increased to above 1 in the USA,35 Belgium,34 and in online reports from the UK47 but remained below 1 in China.40,41
DISCUSSION
Our review synthesized data on social contact patterns under physical distancing measures implemented to mitigate the spread of COVID-19. Despite marked variation in pre-pandemic contact patterns across a diverse range of countries, we found universal reductions in contact sufficient to bring R0 below one during the most stringent period of measures between February and May 2020. We report several other unifying trends in age-specific contact rates, including that reductions primarily occurred between individuals of the same age, children’s contacts were reduced dramatically, and that the elderly displayed the lowest absolute contact rates while distancing interventions were in place. Contacts increased following relaxation of initial mitigation measures but did not return to pre-COVID levels. Increases in contacts after relaxation were primarily observed among working-age adults, with the oldest age groups experiencing few increases in contact rates.
Our study compiled data from countries with similar, although not identical, physical distancing measures in place. In all countries, physical distancing measures included school closures, resulting in complete elimination of school-based contacts. All countries mandated some form of workplace closures that either targeted specific sectors (Germany) or targeted all but essential workplaces (all other countries and some regions in the USA) (eFigure 7; http://links.lww.com/EDE/B848). Countries with less stringent workplace closure interventions in place (Germany and the Netherlands) observed lower percentage reduction in workplace contacts during the initial mitigation period. The stringency of stay-at-home orders varied between and within countries. Parts of Italy and China implemented the most stringent orders and prohibited individuals from leaving the house except with permission for work, health, or extenuating reasons.48 These measures corresponded with a near 100% reduction in contacts in the general community. All other study settings allowed exceptions for exercise and essential trips which may have resulted in variations in percent reduction of contacts in the general community. Post-relaxation, variation in the extent of relaxation may have contributed to further variation in contact rates and patterns across countries. Our observation that increases in contact rates post-relaxation were driven by working-age adults is consistent with the concomitant opening of workplaces and a rebound in mobility within this age group previously reported from cell phone data.49 This observation supports the notion that contacts at work and in the community by the working population played a key role in driving and sustaining SARS-CoV-2 transmission in the summer of 2020.49,50
We note several limitations in our review. First, the time period of data collection for pre-COVID data varied. Some were based on the POLYMOD study conducted in 2008,3 while others44,51,52 were conducted more recently and likely more comparable to contact patterns immediately before mitigation measures. A few studies asked participants to recall contacts before COVID-19, potentially producing recall error where participants’ current lifestyle under mitigation influenced their recall. Second, populations sampled for surveys conducted pre-COVID and during COVID-19 may have differed. For example, the POLYMOD study recruited participants through random digit dialing or face-to-face interviews whereas studies conducted during COVID-19 primarily recruited through Facebook advertisements or commercial polling companies. Third, policies and adherence to physical distancing measures differed between and within countries. We provide context for the data collection periods with the OSI indices and the epidemic curves for each country. Fourth, most studies used comparable definitions of contact that included both physical (skin-to-skin) contact and conversational contact, contact definitions were not identical. Small inconsistencies in contact definition may reduce comparability of results across different studies. Finally, there is a lack of data and published studies on the evolution of contact patterns over time during post-relaxation, especially in low-income countries. Contact surveys can be integrated into ongoing population-level health surveys measuring behavior changes during the COVID-19 pandemic,53–57such as adherence to physical distancing and mask-wearing, to fill this literature gap.
In conclusion, we reviewed the literature for contact studies conducted during the COVID-19 pandemic among the general population. We further synthesized data on magnitude and percent reduction in contacts stratified by location and age group across diverse study time periods. We observed substantial reductions in contact rates across all study settings during the initial mitigation period followed by increases in contact rates after relaxation of measures that are driven by working-age adults. This information can be used to guide mathematical models seeking to represent contact patterns relevant during COVID-related physical distancing measures.
Supplementary Material
Footnotes
Supported by CDC U01 CK000572-01-02 and NIH/NICHD R01 HD097175.
Data availability: Code and data are available at https://github.com/lopmanlab/review_socialcontact_covid19.
The authors report no conflicts of interest.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com).
REFERENCES
- 1.Liu Y. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Medicine. 2021;19:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brauner JM, Mindermann S, Sharma M, et al. Inferring the effectiveness of government interventions against COVID-19. Science. 2020;371:eabd9338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mossong J, Hens N, Jit M, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5:e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prem K, Cook AR, Jit M. Projecting social contact matrices in 152 countries using contact surveys and demographic data. PLoS Comput Biol. 2017;13:e1005697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mistry D, Litvinova M, Pastore Y Piontti A, et al. Inferring high-resolution human mixing patterns for disease modeling. Nat Commun. 2021;12:323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoang T, Coletti P, Melegaro A, et al. A systematic review of social contact surveys to inform transmission models of close-contact infections. Epidemiology. 2019;30:723–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melegaro A, Del Fava E, Poletti P, et al. Social contact structures and time use patterns in the Manicaland Province of Zimbabwe. PLoS One. 2017;12:e0170459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kiti MC, Kinyanjui TM, Koech DC, Munywoki PK, Medley GF, Nokes DJ. Quantifying age-related rates of social contact using diaries in a rural coastal population of Kenya. PLoS One. 2014;9:e104786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ambikapathy B, Krishnamurthy K. Mathematical modelling to assess the impact of lockdown on COVID-19 transmission in india: model development and validation. JMIR Public Health Surveill. 2020;6:e19368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kucharski AJ, Klepac P, Conlan AJK, et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis. 2020;20:1151–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziauddeen H, Subramaniam N, Gurdasani D. Modelling the impact of lockdown easing measures on cumulative COVID-19 cases and deaths in England. medRxiv. Published online June 23, 2020. doi: 10.1101/2020.06.21.20136853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peak CM, Childs LM, Grad YH, Buckee CO. Comparing nonpharmaceutical interventions for containing emerging epidemics. Proc Natl Acad Sci USA. 2017;114:4023–4028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edmunds WJ, Kafatos G, Wallinga J, Mossong JR. Mixing patterns and the spread of close-contact infectious diseases. Emerg Themes Epidemiol. 2006;3:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aleta A, de Arruda GF, Moreno Y. Data-driven contact structures: from homogeneous mixing to multilayer networks. PLoS Comput Biol. 2020;16:e1008035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kucharski AJ, Kwok KO, Wei VW, et al. The contribution of social behaviour to the transmission of influenza A in a human population. PLoS Pathog. 2014;10:e1004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamigaki T, Mimura S, Takahashi Y, Oshitani H. Analysis of influenza transmission in the households of primary and junior high school students during the 2012-13 influenza season in Odate, Japan. BMC Infect Dis. 2015;15:282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kyrychko YN, Blyuss KB, Brovchenko I. Mathematical modelling of the dynamics and containment of COVID-19 in Ukraine. Sci Rep. 2020;10:19662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kimathi M, Mwalili S, Ojiambo V, Gathungu DK. Age-structured model for COVID-19: effectiveness of social distancing and contact reduction in Kenya. Infect Dis Model. 2021;6:15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marziano V, Guzzetta G, Rondinone BM, et al. Retrospective analysis of the Italian exit strategy from COVID-19 lockdown. Proc Natl Acad Sci U S A. 2021;118:e2019617118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Domenico L, Pullano G, Sabbatini CE, Boëlle PY, Colizza V. Impact of lockdown on COVID-19 epidemic in Île-de-France and possible exit strategies. BMC Med. 2020;18:240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hale T, Webster S, Petherick A, Phillips T, Kira B. Oxford COVID-19 government response tracker, 2020. Blavatnik School of Government. Data Use Policy: Creative Commons Attribution CC BY Standard. [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Med. 2009;6:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mossong J, Hens N, Jit M, et al. POLYMOD social contact data (Version 2.0) [Dataset]. Published online 2020. 10.5281/zenodo.3874557. Accessed 11 December 2020. [DOI]
- 24.Willem L, Van Hoang T, Funk S, Coletti P, Beutels P, Hens N. SOCRATES: an online tool leveraging a social contact data sharing initiative to assess mitigation strategies for COVID-19. BMC Res Notes. 2020;13:293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Béraud G, Kazmercziak S, Beutels P, et al. Social Contact Data for France (Version 2) [Dataset]. Published online June 9, 2020. 10.5281/zenodo.3886590. Accessed 11 December 2020. [DOI]
- 26.Coletti P, Wambua J, Gimma A, et al. CoMix Social Contact Data (Belgium, Version 2) [Dataset]. Published online September 17, 2020. 10.5281/zenodo.4147585. Accessed 11 December 2020. [DOI]
- 27.Willem L, Van Kerkhove K, Chao DL, Hens N, Beutels P. Social Contact Data for Belgium (2010-2011) (Version 1.2) [Dataset]. Published online December 2, 2020. 10.5281/zenodo.4302055. Accessed 11 December 2020. [DOI]
- 28.Zhang J, Litvinova M, Liang Y, et al. Social Contact Data Before and During COVID-19 in China (Version 1.0) [Dataset]. Published online October 12, 2020. 10.5281/zenodo.4081140. Accessed 11 December 2020. [DOI]
- 29.Zhang J, Klepac P, Read J, et al. Social Contact Data for China Mainland (Verion 6) [Dataset]. Published online June 5, 2020. 10.5281/zenodo.3878754. Accessed 11 December 2020. [DOI]
- 30.Fuller JA, Hakim A, Victory KR, et al. ; CDC COVID-19 Response Team. Mitigation policies and COVID-19-associated mortality – 37 European Countries, January 23-June 30, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhu D, Mishra SR, Han X, Santo K. Social distancing in Latin America during the COVID-19 pandemic: an analysis using the Stringency Index and Google Community Mobility Reports. J Travel Med. 2020;27:taaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Del Fava E, Cimentada J, Perrotta D, et al. The differential impact of physical distancing strategies on social contacts relevant for the spread of COVID-19. medRxiv. Published online: May 15, 2020. doi: 10.1101/2020.05.15.20102657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Backer J, Mollema L, Klinkenberg D, et al. Impact of physical distancing measures against COVID-19 on contacts and mixing patterns: repeated cross-sectional surveys, the Netherlands, 2016–17, April 2020 and June 2020. Eurosurveillance. 2021;26. doi:10.2807/1560-7917.ES.2021.26.8.2000994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coletti P, Wambua J, Gimma A, et al. CoMix: comparing mixing patterns in the Belgian population during and after lockdown. Sci Rep. 2020;10:21885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feehan DM, Mahmud A. Quantifying interpersonal contact in the United States during the spread of COVID-19: first results from the Berkeley Interpersonal Contact Study. Nat Commun. 2021;12:8.33397891 [Google Scholar]
- 36.Jarvis CI, Van Zandvoort K, Gimma A, et al. ; CMMID COVID-19 working group. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020;18:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Latsuzbaia A, Herold M, Bertemes JP, Mossong J. Evolving social contact patterns during the COVID-19 crisis in Luxembourg. PLoS One. 2020;15:e0237128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bosetti P, Huynh B-T, Abdou AY, et al. Lockdown impact on age-specific contact patterns and behaviours in France. Medrxiv Published online October 11, 2020. doi: 10.1101/2020.10.07.20205104 [Google Scholar]
- 39.Sypsa V, Roussos S, Paraskevis D, Lytras T, Tsiodras S, Hatzakis A. Effects of social distancing measures during the first epidemic wave of severe acute respiratory syndrome infection, Greece. Emerg Infect Dis. 2021;27:452–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang J, Litvinova M, Liang Y, et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368:1481–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang J, Litvinova M, Liang Y, et al. The impact of relaxing interventions on human contact patterns and SARS-CoV-2 transmission in China. Sci Adv. 2021;7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quaife M, van Zandvoort K, Gimma A, et al.; CMMID COVID-19 Working Group. The impact of COVID-19 control measures on social contacts and transmission in Kenyan informal settlements. BMC Med. 2020;18:316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCreesh N, Dlamini V, Edwards A, et al. Impact of social distancing regulations and epidemic risk perception on social contact and SARS-CoV-2 transmission potential in Rural South Africa: analysis of repeated cross-sectional surveys. medRxiv. Published online December 3, 2020. doi: 10.1101/2020.12.01.20241877 [Google Scholar]
- 44.Zhang J, Klepac P, Read JM, et al. Patterns of human social contact and contact with animals in Shanghai, China. Sci Rep. 2019;9:15141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.ACAPS. COVID-19 Government Measures Dataset. Published March 18, 2020. Available at: https://www.acaps.org/covid-19-government-measures-dataset. Accessed 28 January 2021.
- 46.Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20:669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.CMMID Repository. CoMix Study – Social Contact Survey in the UK. Available at: https://cmmid.github.io/topics/covid19/comix-reports.html. Accessed March 7, 2021.
- 48.The New York Times. Italy Announces Restrictions Over Entire Country in Attempt to Halt Coronavirus. Available at: https://www.nytimes.com/2020/03/09/world/europe/italy-lockdown-coronavirus.html. Accessed March 3, 2021.
- 49.Monod M, Blenkinsop A, Xi X, et al. Age groups that sustain resurging COVID-19 epidemics in the United States. Science. 2021;371:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harris JE. Data from the COVID-19 epidemic in Florida suggest that younger cohorts have been transmitting their infections to less socially mobile older adults. Rev Econ Household. 2020;18:1019–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Béraud G, Kazmercziak S, Beutels P, et al. The French connection: the first large population-based contact survey in France relevant for the spread of infectious diseases. PLoS ONE. 2015;10:e0133203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Willem L, Van Kerckhove K, Chao DL, Hens N, Beutels P. A nice day for an infection? Weather conditions and social contact patterns relevant to influenza transmission. PLoS One. 2012;7:e48695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Szwarcwald CL, Souza Júnior PRB, Malta DC, et al. Adherence to physical contact restriction measures and the spread of COVID-19 in Brazil. Epidemiol Serv Saude. 2020;29:e2020432. [DOI] [PubMed] [Google Scholar]
- 54.Oliver N, Barber X, Roomp K, Roomp K. Assessing the Impact of the COVID-19 Pandemic in Spain: large-scale, online, self-reported population survey. J Med Internet Res. 2020;22:e21319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Quandt SA, LaMonto NJ, Mora DC, Talton JW, Laurienti PJ, Arcury TA. COVID-19 Pandemic among Latinx farmworker and nonfarmworker families in North Carolina: knowledge, risk perceptions, and preventive behaviors. Int J Environ Res Public Health. 2020;17:E5786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Arpino B, Pasqualini M, Bordone V. Physically distant but socially close? changes in intergenerational non-physical contacts during the COVID-19 pandemic among older people in France, Italy and Spain. SocArXiv; Published online October 9, 2020. doi: 10.31235/osf.io/7qf5w [DOI] [PMC free article] [PubMed]
- 57.Radon K, Saathoff E, Pritsch M, et al. Protocol of a population-based prospective COVID-19 cohort study Munich, Germany (KoCo19). BMC Public Health. 2020;20:1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.