Abstract
Pregnancy identifies women who may be at a greater risk of cardiovascular disease (CVD), based on the development of adverse pregnancy outcomes (APOs), and may identify women who may benefit from atherosclerotic CVD (ASCVD) risk reduction efforts. APOs are common and although they are separate diagnoses, all these disorders seem to share an underlying pathogenesis. What is not clear is whether the APO itself initiates a pathway that results in CVD or whether the APO uncovers a woman’s predisposition to CVD. Regardless, APOs have immediate risks to maternal and foetal health, in addition to longer-term CVD consequences. CVD risk assessment and stratification in women remains complex and, historically, has underestimated risk, especially in young women. Further research is needed into the role of ASCVD risk assessment and the effect of aggressive ASCVD risk modification on CVD outcomes in women with a history of APOs.
Keywords: Hypertensive disorders of pregnancy, pre-eclampsia, preterm delivery, cardiovascular disease, cardiovascular risk
In women, cardiovascular disease (CVD) is the leading cause of death and, despite great strides in reducing mortality from CVD, the number of women dying because of CVD has increased recently.[1] The increase in mortality has been attributed, in part, to the risk of death in younger women with CVD due to a lack of recognition and undertreatment of young women with CVD.[2] CVD is also the leading cause of maternal mortality, accounting for one in three maternal deaths.[3] The peripartum and postpartum risk of CVD mortality is only one part of the risk to a young woman’s health. Pregnancy also identifies women who may be at a greater risk of CVD, based on the development of adverse pregnancy outcomes (APOs), and, in essence, may identify women who could benefit from atherosclerotic CVD (ASCVD) risk reduction efforts. As such, APOs are considered as risk enhancers of ASCVD by the 2018 American College of Cardiology (ACC)/American Heart Association (AHA) guideline on the management of blood cholesterol and the 2019 ACC/AHA guideline on the primary prevention of CVD.[4,5] Identifying women with such risk enhancers and addressing ASCVD risk has been identified as an important component of care in the ‘fouth trimester’, which should involve comprehensive care and risk assessment within the 12-week postpartum period.[6]
The risk of APOs is not rare, with approximately 30% of women experiencing an APO. This includes gestational hypertension (3–14% of births), pre-eclampsia (2–5% of births), gestational diabetes (5%), preterm delivery (6–12%) and the delivery of a small-for-gestational-age (SGA) infant (prevalence varies by country; Table 1).[7] APOs occur more frequently in black and Asian women, who often present with more severe clinical presentations and have poorer outcomes.[8–10] There are numerous observational studies showing a strong association between these APOs and CVD, including premature CVD.[7,11–15] Identifying women with a history of APOs provides a unique opportunity to identify women at risk for CVD and initiate early primary prevention efforts in a higher-risk group before the onset of adverse cardiovascular events. The American College of Obstetrics and Gynecology and the AHA have proposed a new paradigm for postpartum care to identify women at risk for future CVD, aptly named the ‘fourth trimester’.[6,16] The purpose of this paper is to discuss the effects of pregnancy and APOs on the risk of CVD.
Table 1: Definitions of Adverse Pregnancy Outcomes.
| Adverse Pregnancy Outcome | Definition |
|---|---|
| Gestational diabetes | Any degree of glucose intolerance with its onset or first recognition during pregnancy |
| Gestational hypertension | New hypertension that develops after week 20 of pregnancy without proteinuria |
| Pre-eclampsia | New hypertension that develops after week 20 of pregnancy, with proteinuria or evidence of end-organ dysfunction |
| Preterm delivery | Delivery before 37 weeks gestational age (regardless of cause) |
| Small-for-gestational age | Birthweight in the 10th percentile or less for gestational age |
Pregnancy as a Stress Test
Pregnancy is a physiological stress test to the heart. During pregnancy, there is an increase in circulating blood volume. This occurs in the setting of a reduction in systemic vascular resistance, lower blood pressure and increased cardiac output, which is essential for the optimal growth of the developing foetus.[17] These adaptive changes are designed to provide adequate uteroplacental circulation, given the increased metabolic demands during the gravid state. Insufficient haemodynamic changes can result in significant maternal and fetal morbidity and mortality. In addition, even after these acute issues resolve, some studies have shown an association between APOs and hypertension, left ventricular changes, vascular dysfunction, chronic kidney disease and CVD after the reproductive years.[12,18–23]
Adverse Pregnancy Outcomes and Associated Adverse Cardiovascular Outcomes
Gestational hypertension and pre-eclampsia have been associated with a 2- to 4-fold increased risk of CHD, heart failure and stroke, with recurrent pre-eclampsia having the highest risk.[24–26] Although the relative risk is highest within the first year postpartum, the risks persist decades after the pregnancy, when the absolute risks are greater than those immediately postpartum.[25,26] Hypertensive disorders of pregnancy (HDP) are associated with accelerated cardiovascular aging, with a greater prevalence of subclinical atherosclerosis and arterial stiffness index among women aged >40 years.[26,27] In addition, HDP have been associated with aortic stenosis and mitral regurgitation, as demonstrated by the UK Biobank cohort, showing that the CVD risk goes beyond the impact of just the development of chronic hypertension.[26]
Women who had gestational diabetes have up to seven- and twofold increased risks of developing type 2 diabetes and major cardiovascular events (independent of type 2 diabetes), respectively, than those without gestational diabetes.[28,29] Studies have shown a 16–29% cumulative incidence of diabetes after 10–20 years of follow-up in women with gestational diabetes.[30,31] Preterm delivery has been associated with a 1.4- to 2-fold risk of CVD, CHD and stroke.[12,32] The highest risks occurred when the deliveries occurred before 32 weeks gestation or in medically indicated preterm deliveries.[12]
A recent study showed that at 5 years postpartum, the incidence of MI increased more rapidly in preterm than term deliveries, whereas for ischaemic stroke this occurred after 10 years.[33] A recent meta-analysis did not pool studies on women with delivery of a SGA infant due to variations in the definition of SGA between the studies.[34] However, the authors of that analysis noted a consistent trend of increased CVD risk in these women across all 10 studies included, with an effect estimate ranging between 1.09 and 3.50 and a follow-up period of up to 21 years.[34]
Mechanisms Driving the Association Between Adverse Pregnancy Outcomes and Cardiovascular Disease
APOs are common and, although they are separate diagnoses, all these disorders seem to share an underlying pathogenesis, including placental ischaemia, maternal inflammation and vascular dysfunction.[35–39] What is not clear is whether the APO itself initiates a pathway that results in CVD or whether the APO uncovers a woman’s predisposition to CVD (Figure 1). Regardless, APOs have immediate risks to maternal and fetal health, in addition to longer-term CVD consequences.[7,12,40,41] As such, the occurrence of APOs provides an insight into a woman’s future cardiovascular health.
Figure 1: Impact of Adverse Pregnancy Outcomes on the Cardiovascular System.
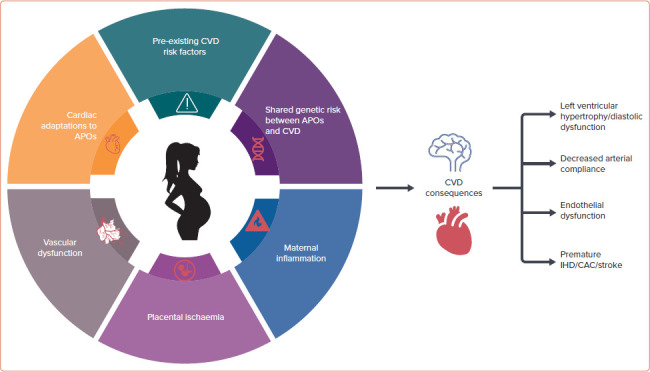
APOs = adverse pregnancy outcomes; CAC = coronary artery calcium; CVD = cardiovascular disease; IHD = ischaemic heart disease.
Systemic Endothelial/Microvascular Dysfunction
APOs appear to share similar metabolic and/or vascular abnormalities, which are reflected within the placenta. In a pregnancy without any APOs, the maternal spiral arteries widen after a trophoblast invasion, resulting in low-resistance blood flow in the uteroplacental unit.[37] In contrast, in a pregnancy affected by pre-eclampsia, the trophoblast invasion is shallow, with inadequate spiral artery remodelling that results in poor perfusion of the placenta, placental ischaemia and oxidative stress. There is also evidence of inflammatory markers within the maternal blood in those with APOs, which are not seen in those with an uncomplicated pregnancy.[37,42–44] Theoretically, the inflammatory state and the anti-angiogenic state could be the shared mechanisms by which APOs increase underlying CVD risk.[45] Placental lesions have also been associated with cardiovascular risk factors.[46–48] Increased soluble fms-like tyrosine kinase-1 has been associated with atherosclerosis.[49]
Furthermore, women exposed to pre-eclampsia may also have arterial stiffness or endothelial damage, which, in turn, are related to their increased long-term CVD risk.[50,51] Women with spontaneous preterm delivery have been observed to have a proinflammatory phenotype, with higher C-reactive protein levels during pregnancy.[52,53] It may be that the inflammatory processes associated with preterm delivery increase the risk of endothelial dysfunction and subclinical vascular disease, and consequently increase CVD risk in the future.[52,54]
In addition, because placental dysfunction may be due to vascular and endothelial cell dysfunction, women who have subclinical CVD phenotypes may not be able to mount an appropriate haemodynamic response in pregnancy. For example, placental growth factor, a hormone that promotes angiogenesis, is significantly reduced in pregnancies with pre-eclampsia, with or without SGA infants.[55,56] The shared placental and maternal vascular characteristics in those with APOs support an overlapping pathophysiology for future CVD, regardless of how different the APOs appear in their presentation.
Cardiac and Coronary Changes
Structural changes in the myocardium can occur in women with APOs. In pre-eclampsia specifically, afterload-dependent cardiac remodelling can be seen that is similar to the remodelling of the myocardium seen in hypertension. Specifically, an increase in left ventricular wall thickness, particularly concentric left ventricular hypertrophy, has been seen even in those with mild gestational hypertension.[57,58] Diastolic dysfunction and impaired left ventricular relaxation have been documented in patients with pre-eclampsia.[58] Left atrial remodelling may also develop, most noted in preterm pre-eclampsia.[59] These changes can also persist many years after the incident pregnancy.[22,23]
Furthermore, women with previous pre-eclampsia had higher carotid intima–media thickness, lower coronary flow reserve and higher high-sensitivity C-reactive protein values than those without pre-eclampsia.[60] In addition, both pre-eclampsia and high parity number have been linked with accelerated atherosclerosis.[27,61] Women with previous preterm births also have higher atherogenic lipids and carotid arterial wall thickening in the decade after delivery than women who had term births.[62] For women with ischaemia without obstructive coronary artery disease, a history of APO is associated with lower coronary flow reserve suggestive of coronary microvascular dysfunction.[63]
Role of Cardiovascular Disease Risk Factors
APOs and CVD share ASCVD risk factors, and women with APOs have been shown to have a higher CVD risk factor burden, with a greater prevalence of hypertension, hyperlipidaemia, diabetes, kidney disease, obesity and tobacco use, in addition to a greater risk of developing these risk factors several years after the pregnancy.[7,64–66] Except for tobacco use, which is inversely associated with pre-eclampsia, the other biochemical risk factors have been shown to persist in women years after HDP.[67] Therefore, pre-eclampsia and gestational hypertension may be independent risk factors for future CVD because the post-pregnancy body may not fully recover from the damage to the vascular, endothelial and metabolic systems during pregnancy. With further insults to the body over time, the damage sustained during pregnancy may manifest in later life as cardiovascular events.[68] Women with pre-existing cardiovascular risk factors, such as an adverse lipid profile and glucose status, are also at increased risk of preterm delivery.[69] Similarly, delivery of SGA infants is linked to the development of maternal hyperlipidaemia, hypertension and increased calculated 10-year CVD risk prior to the onset of CVD.[70,71] Nonetheless, the excess risk based on risk factors does not fully account for the amount of CVD seen women with APOs.[72] Therefore, other mechanisms are likely to be involved in the association between APOs and CVD.
Other Mechanisms
Families of women with an APO also have increased risks of APOs and CVD, suggesting that underlying genetic factors may also contribute to the association.[73,74] Women at risk of APOs and CVD may also have genetic mutations that are involved in the disease process. For example, there are maternal sequence variants associated with both pre-eclampsia and hypertension.[75] Similarly, genetic predisposition to hypertension has been associated with HDP.[76] Furthermore, an association was found between single nucleotide polymorphism variations in genes for cholesterol metabolism and preterm delivery.[77]
Conversely, multifactorial mechanisms may explain the association of APO with CVD, and socioeconomic factors have also been considered. For example, CVD and high parity number are both more frequently observed in low socioeconomic classes.[78] High parity number is also associated with a small increased future paternal CVD risk.[79–81] Because the observed associations in both mothers and fathers attenuated following adjustment for lifestyle factors, there may be residual confounding by socioeconomic class and/or lifestyle.[80]
Evolving Role of Adverse Pregnancy Outcomes in the Prediction of Cardiovascular Disease Risk
CVD risk assessment and stratification in women remain complex and, historically, have underestimated risk, especially in young women.[82] Not only do traditional CVD risk factors such as hypertension, hyperlipidaemia and tobacco use, among others, need to be considered, but additional sex-specific factors, such as APOs, should also be included. However, existing risk stratification schemes, such as the ASCVD Pooled Cohort Equations model, do not include pregnancy or other gynaecological history.[82] Whether routine incorporation of pregnancy complications improves the ability to risk stratify women for CVD is unknown and has more recently been investigated. The HUNT study by Markovitz et al. assessed the long-term risk of CVD, including MI, CHD and stroke, in women without prior CVD history in approximately 18,000 subjects with a prevalence of APOs of 39%.[11] In that study, of all APOs, only pre-eclampsia was associated with increased CVD risk. The inclusion of pregnancy complications only led to the reclassification of 0.4% of women without events into lower-risk categories and 2% of women with events were correctly reclassified into higher-risk categories.[11] A similar study by Timpka et al. assessed HDP and low birth weight in subjects aged ≥50 years and found that the inclusion of these APOs did not significantly improve CVD risk prediction.[83] In the US, Stuart et al. studied the role of HDP and parity in a cohort of women aged ≥40 years without CVD risk factors or history of CVD.[24] HDP and parity were added to the ASCVD Pooled Cohort Equations model, and these variables were associated with elevated ASCVD risk independent of established CVD risk factors; however, the risk reclassification across risk groups or age stratification did not change: 0.6% of previously low-risk women who developed CVD were reclassified into a higher-risk group, but 8.3% of women previously classified as being of intermediate risk were incorrectly reclassified as low risk.[24] Dam et al. compared CVD risk prediction in women with and without a history of HDP among the Framingham Risk Score, the Pooled Cohort Equations model and the Systematic Coronary Risk Evaluation (SCORE) model, and similarly found that none of the models was more predictive in women with than without a history of HDP.[84] Although these studies do not demonstrate improved discrimination of risk with the inclusion of APOs, this may be explained by underlying embedded association of APO risk with traditional CVD risk factors such as hypertension and diabetes.
APOs serve as a ‘window’ into future CVD risk, either through development of traditional CVD risk factors and/or an independent association with underlying vascular dysfunction. As such, it is important to screen for APOs as risk markers to guide potential risk mitigation strategies. In 2018, the ACC/AHA cholesterol guidelines for the first time acknowledged APOs as CVD ‘risk enhancers’ for consideration of statin use in women with borderline to intermediate risk, as calculated by the Pooled Cohort Equation.[4] The inclusion of APOs among other risk enhancers allows clinicians to personalise decision making regarding statin therapy beyond just generalised risk assessment. The ACC/AHA cholesterol guidelines also recommend the consideration of coronary artery calcium (CAC) assessment to help further guide decisions regarding statin therapy.[4] The use of CAC to guide prevention therapies, such as statins, is particularly intriguing in women with a history of APOs.
Several studies have noted an association between coronary CT angiography (CTA)/calcium scoring in young women and a history of APOs (Figure 2). Benschop et al. found that, compared with women without a history of pre-eclampsia, pre-eclampsia is independently associated with CAC even when accounting for traditional CVD risk factors.[85] Another study assessed a broader set of APOs in Black women, including preterm delivery, pre-eclampsia and gestational diabetes, against matched controls without APOs with regard to coronary CTA findings.[86] In that study, any APO was associated with higher rates of atherosclerotic coronary disease, defined as ≥20% luminal narrowing disease and obstructive ≥50% luminal narrowing disease. That study was particular important because research in this area in Black women, who have high rates of pregnancy complications, is lacking. Whether coronary CTA should play a more routine role in assessing CVD risk in women with APOs is unknown and an area in need of further study.
Figure 2: Incorporation of Adverse Pregnancy Outcomes into the Atherosclerotic Cardiovascular Disease Risk Assessment of Women.
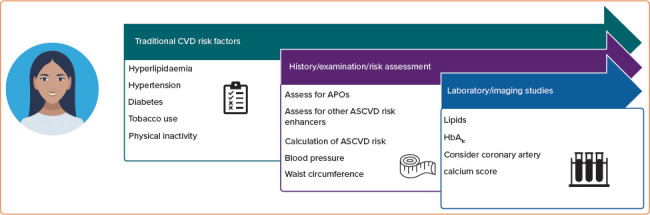
The incorporation of APOs involves traditional ASCVD risk factors, other risk enhancers, blood pressure and waist circumference on examination, as well as the assessment of lipids, HbA1c and consideration of coronary CT angiography. APOs = adverse pregnancy outcomes; ASCVD = atherosclerotic cardiovascular disease.
Conclusion
Associations of APOs with future CVD have been reported in the literature. However, the underlying causal mechanisms remain unknown. It is important to raise awareness of the importance of these associations and the current recommendations among healthcare professionals, as well as among the women themselves. Further research is needed to elucidate the pathophysiology behind these associations. This, in turn, will inform future research in the role of ASCVD risk assessment and the effect of aggressive ASCVD risk modification on CVD outcomes in women with a history of APOs.
References
- 1.Virani SS, Alonso A, Aparicio HJ et al. Heart disease and stroke statistics – 2021 update: a report from the American Heart Association. Circulation. 2021;143:e254–743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 2.Khan SU, Yedlapati SH, Lone AN et al. A comparative analysis of premature heart disease- and cancer-related mortality in women in the USA, 1999–2018. Eur Heart J Qual Care Clin Outcomes. 2021;qcaa099 doi: 10.1093/ehjqcco/qcaa099. [DOI] [PubMed] [Google Scholar]
- 3.Petersen EE, Davis NL, Goodman D et al. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;68:423–9. doi: 10.15585/mmwr.mm6818e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grundy SM, Stone NJ, Bailey AL et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–143. doi: 10.1161/CIR.0000000000000699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnett DK, Blumenthal RS, Albert MA et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e563–95. doi: 10.1161/CIR.0000000000000725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stuebe AM, Auguste TC, Gulati M. Optimizing postpartum care. ACOG Committee Opinion No. 736. American College of Obstetricians and Gynecologists. ACOG Presidential Task Force. Obstet Gynecol. 2018;131:e140–50. doi: 10.1097/AOG.0000000000002633. [DOI] [PubMed] [Google Scholar]
- 7.Wu P, Mamas MA, Gulati M. Pregnancy as a predictor of maternal cardiovascular disease: the era of CardioObstetrics. J Womens Health (Larchmt) 2019;28:1037–50. doi: 10.1089/jwh.2018.7480. [DOI] [PubMed] [Google Scholar]
- 8.Grobman WA, Parker CB, Willinger M et al. Racial disparities in adverse pregnancy outcomes and psychosocial stress. Obstet Gynecol. 2018;131:328–35. doi: 10.1097/AOG.0000000000002441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khalil A, Rezende J, Akolekar R et al. Maternal racial origin and adverse pregnancy outcome: a cohort study. Ultrasound Obstet Gynecol. 2013;41:278–85. doi: 10.1002/uog.12313. [DOI] [PubMed] [Google Scholar]
- 10.Zeng N, Erwin E, Wen W et al. Comparison of adverse perinatal outcomes between Asians and Caucasians: a population-based retrospective cohort study in Ontario. BMC Pregnancy Childbirth. 2021;21:9. doi: 10.1186/s12884-020-03467-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Markovitz AR, Stuart JJ, Horn J et al. Does pregnancy complication history improve cardiovascular disease risk prediction? Findings from the HUNT study in Norway. Eur Heart J. 2019;40:1113–20. doi: 10.1093/eurheartj/ehy863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu P, Gulati M, Kwok CS et al. Preterm delivery and future risk of maternal cardiovascular disease: a systematic review and meta-analysis. J Am Heart Assoc. 2018;7:e007809. doi: 10.1161/JAHA.117.007809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu P, Chew-Graham CA, Maas AH et al. Temporal changes in hypertensive disorders of pregnancy and impact on cardiovascular and obstetric outcomes. Am J Cardiol. 2020;125:1508–16. doi: 10.1016/j.amjcard.2020.02.029. [DOI] [PubMed] [Google Scholar]
- 14.Oliver-Williams CT, Heydon EE, Smith GC, Wood AM. Miscarriage and future maternal cardiovascular disease: a systematic review and meta-analysis. Heart. 2013;99:1636–44. doi: 10.1136/heartjnl-2012-303237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hooijschuur MC, Ghossein-Doha C, Al-Nasiry S, Spaanderman ME. Maternal metabolic syndrome, preeclampsia, and small for gestational age infancy. Am J Obstet Gynecol. 2015;213:370–e1–7. doi: 10.1016/j.ajog.2015.05.045. [DOI] [PubMed] [Google Scholar]
- 16.Brown HL, Warner JJ, Gianos E et al. Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a Presidential Advisory from the American Heart Association and the American College of Obstetricians and Gynecologists. Circulation. 2018;137:e843–52. doi: 10.1161/CIR.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 17.Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014;130:1003–8. doi: 10.1161/CIRCULATIONAHA.114.009029. [DOI] [PubMed] [Google Scholar]
- 18.Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974. doi: 10.1136/bmj.39335.385301.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grand’Maison S, Pilote L, Okano M et al. Markers of vascular dysfunction after hypertensive disorders of pregnancy: a systematic review and meta-analysis. Hypertension. 2016;68:1447–58. doi: 10.1161/HYPERTENSIONAHA.116.07907. [DOI] [PubMed] [Google Scholar]
- 20.Barrett PM, McCarthy FP, Kublickiene K et al. Adverse pregnancy outcomes and long-term maternal kidney disease: a systematic review and meta-analysis. JAMA Netw Open. 2020;3:e1920–964. doi: 10.1001/jamanetworkopen.2019.20964. [DOI] [PubMed] [Google Scholar]
- 21.Covella B, Vinturache AE, Cabiddu G et al. A systematic review and meta-analysis indicates long-term risk of chronic and end-stage kidney disease after preeclampsia. Kidney Int. 2019;96:711–27. doi: 10.1016/j.kint.2019.03.033. [DOI] [PubMed] [Google Scholar]
- 22.Scantlebury DC, Kane GC, Wiste HJ et al. Left ventricular hypertrophy after hypertensive pregnancy disorders. Heart. 2015;101:1584–90. doi: 10.1136/heartjnl-2015-308098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melchiorre K, Sutherland GR, Liberati M, Thilaganathan B. Preeclampsia is associated with persistent postpartum cardiovascular impairment. Hypertension. 2011;58:709–15. doi: 10.1161/HYPERTENSIONAHA.111.176537. [DOI] [PubMed] [Google Scholar]
- 24.Stuart JJ, Tanz LJ, Cook NR et al. Hypertensive disorders of pregnancy and 10-year cardiovascular risk prediction. J Am Coll Cardiol. 2018;72:1252–63. doi: 10.1016/j.jacc.2018.05.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu P, Haththotuwa R, Kwok CS et al. Preeclampsia and future cardiovascular health. Circ Cardiovasc Qual Outcomes. 2017;10:e003497. doi: 10.1161/CIRCOUTCOMES.116.003497. [DOI] [PubMed] [Google Scholar]
- 26.Honigberg MC, Zekavat SM, Aragam K et al. Long-term cardiovascular risk in women with hypertension during pregnancy. J Am Coll Cardiol. 2019;74:2743–54. doi: 10.1016/j.jacc.2019.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zoet GA, Benschop L, Boersma E et al. Prevalence of subclinical coronary artery disease assessed by coronary computed tomography angiography in 45- to 55-year-old women with a history of preeclampsia. Circulation. 2018;137:877–9. doi: 10.1161/CIRCULATIONAHA.117.032695. [DOI] [PubMed] [Google Scholar]
- 28.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373:1773–9. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 29.Kramer CK, Campbell S, Retnakaran R. Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Diabetologia. 2019;62:905–14. doi: 10.1007/s00125-019-4840-2. [DOI] [PubMed] [Google Scholar]
- 30.Li Z, Cheng Y, Wang D et al. Incidence rate of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review and meta-analysis of 170,139 women. J Diabetes Res. 2020;2020:3076463. doi: 10.1155/2020/3076463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vounzoulaki E, Khunti K, Abner SC et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361. doi: 10.1136/bmj.m1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heida KY, Velthuis BK, Oudijk MA et al. Cardiovascular disease risk in women with a history of spontaneous preterm delivery: a systematic review and meta-analysis. Eur J Prev Cardiol. 2016;23:253–63. doi: 10.1177/2047487314566758. [DOI] [PubMed] [Google Scholar]
- 33.Auger N, Potter BJ, He S et al. Maternal cardiovascular disease 3 decades after preterm birth: longitudinal cohort study of pregnancy vascular disorders. Hypertension. 2020;75:788–95. doi: 10.1161/HYPERTENSIONAHA.119.14221. [DOI] [PubMed] [Google Scholar]
- 34.Grandi SM, Filion KB, Yoon S et al. Cardiovascular disease-related morbidity and mortality in women with a history of pregnancy complications. Circulation. 2019;139:1069–79. doi: 10.1161/CIRCULATIONAHA.118.036748. [DOI] [PubMed] [Google Scholar]
- 35.Andraweera PH, Dekker GA, Roberts CT. The vascular endothelial growth factor family in adverse pregnancy outcomes. Hum Reprod Update. 2012;18:436–57. doi: 10.1093/humupd/dms011. [DOI] [PubMed] [Google Scholar]
- 36.Ilekis JV, Tsilou E, Fisher S et al. Placental origins of adverse pregnancy outcomes: potential molecular targets: an executive workshop summary of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Am J Obstet Gynecol. 2016;215((Suppl)):S1–46. doi: 10.1016/j.ajog.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roberts JM, Hubel CA. The two stage model of preeclampsia: variations on the theme. Placenta. 2009;30((Suppl A)):S32–7. doi: 10.1016/j.placenta.2008.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen LW, Aubert AM, Shivappa N et al. Associations of maternal dietary inflammatory potential and quality with offspring birth outcomes: an individual participant data pooled analysis of 7 European cohorts in the ALPHABET consortium. PLoS Med. 2021;18:e1003491. doi: 10.1371/journal.pmed.1003491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peters SA, Woodward M. Women’s reproductive factors and incident cardiovascular disease in the UK Biobank. Heart. 2018;104:1069–75. doi: 10.1136/heartjnl-2017-312289. [DOI] [PubMed] [Google Scholar]
- 41.Goueslard K, Cottenet J, Mariet AS et al. Early cardiovascular events in women with a history of gestational diabetes mellitus. Cardiovasc Diabetol. 2016;15:15. doi: 10.1186/s12933-016-0338-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shibata E, Rajakumar A, Powers RW et al. Soluble fms-like tyrosine kinase 1 is increased in preeclampsia but not in normotensive pregnancies with small-for-gestational-age neonates: relationship to circulating placental growth factor. J Clin Endocrinol Metab. 2005;90:4895–03. doi: 10.1210/jc.2004-1955. [DOI] [PubMed] [Google Scholar]
- 43.Sultana Z, Maiti K, Aitken J et al. Oxidative stress, placental ageing-related pathologies and adverse pregnancy outcomes. Am J Reprod Immunol. 2017;77:e12653. doi: 10.1111/aji.12653. [DOI] [PubMed] [Google Scholar]
- 44.Thornburg KL, O’Tierney PF, Louey S. Review: the placenta is a programming agent for cardiovascular disease. Placenta. 2010;31((Suppl)):S54–9. doi: 10.1016/j.placenta.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Scantlebury DC, Hayes SN. How does preeclampsia predispose to future cardiovascular disease? Curr Hypertens Rep. 2014;16:472. doi: 10.1007/s11906-014-0472-6. [DOI] [PubMed] [Google Scholar]
- 46.Catov J, Muldoon M, Reis S et al. Preterm birth with placental evidence of malperfusion is associated with cardiovascular risk factors after pregnancy: a prospective cohort study. BJOG. 2018;125:1009–17. doi: 10.1111/1471-0528.15040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gao Q, Tang J, Li N et al. New conception for the development of hypertension in preeclampsia. Oncotarget. 2016;7:78387–95. doi: 10.18632/oncotarget.13410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gilbert JS, Nijland MJ, Knoblich P. Placental ischemia and cardiovascular dysfunction in preeclampsia and beyond: making the connections. Expert Rev Cardiovasc Ther. 2008;6:1367–77. doi: 10.1586/14779072.6.10.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shin S, Lee SH, Park S et al. Soluble fms-like tyrosine kinase-1 and the progression of carotid intima–media thickness – 24-month follow-up study. Circ J. 2010;74:2211–15. doi: 10.1253/circj.CJ-10-0432. [DOI] [PubMed] [Google Scholar]
- 50.Hausvater A, Giannone T, Sandoval Y-HG et al. The association between preeclampsia and arterial stiffness. J Hypertens. 2012;30:17–33. doi: 10.1097/HJH.0b013e32834e4b0f. [DOI] [PubMed] [Google Scholar]
- 51.Rangaswami J, Naranjo M, McCullough PA. Preeclampsia as a form of type 5 cardiorenal syndrome: an underrecognized entity in women’s cardiovascular health. Cardiorenal Med. 2018;8:160–72. doi: 10.1159/000487646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pitiphat W, Gillman MW, Joshipura KJ et al. Plasma C-reactive protein in early pregnancy and preterm delivery. Am J Epidemiol. 2005;162:1108–13. doi: 10.1093/aje/kwi323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moghaddam Banaem L, Mohamadi B, Asghari Jaafarabadi M, Aliyan Moghadam N. Maternal serum C-reactive protein in early pregnancy and occurrence of preterm premature rupture of membranes and preterm birth. J Obstet Gynaecol Res. 2012;38:780–6. doi: 10.1111/j.1447-07562011.01804.x. [DOI] [PubMed] [Google Scholar]
- 54.Blake GJ, Ridker PM. Novel clinical markers of vascular wall inflammation. Circ Res. 2001;89:763–71. doi: 10.1161/hh2101.099270. [DOI] [PubMed] [Google Scholar]
- 55.Smith GC, Crossley JA, Aitken DA et al. Circulating angiogenic factors in early pregnancy and the risk of preeclampsia, intrauterine growth restriction, spontaneous preterm birth, and stillbirth. Obstet Gynecol. 2007;109:1316–24. doi: 10.1097/01.AOG.0000265804.09161.0d. [DOI] [PubMed] [Google Scholar]
- 56.Luttun A, Tjwa M, Moons L et al. Revascularization of ischemic tissues by PlGF treatment, and inhibition of tumor angiogenesis, arthritis and atherosclerosis by anti-Flt1. Nat Med. 2002;8:831–40. doi: 10.1038/nm731. [DOI] [PubMed] [Google Scholar]
- 57.Novelli GP, Valensise H, Vasapollo B et al. Left ventricular concentric geometry as a risk factor in gestational hypertension. Hypertension. 2003;41:469–75. doi: 10.1161/01.HYP.0000058001.67791.0A. [DOI] [PubMed] [Google Scholar]
- 58.Melchiorre K, Sutherland G, Sharma R et al. Mid-gestational maternal cardiovascular profile in preterm and term pre-eclampsia: a prospective study. BJOG. 2013;120:496–504. doi: 10.1111/1471-0528.12068. [DOI] [PubMed] [Google Scholar]
- 59.Ingec M, Yilmaz M, Gundogdu F. Left atrial mechanical functions in pre-eclampsia. J Obstet Gynaecol Res. 2005;31:535–9. doi: 10.1111/j.1447-07562005.00332.x. [DOI] [PubMed] [Google Scholar]
- 60.Ciftci FC, Caliskan M, Ciftci O et al. Impaired coronary microvascular function and increased intima-media thickness in preeclampsia. J Am Soc Hypertens. 2014;8:820–6. doi: 10.1016/j.jash.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 61.Skilton MR, Sérusclat A, Begg LM et al. Parity and carotid atherosclerosis in men and women: insights into the roles of childbearing and child-rearing. Stroke. 2009;40:1152–7. doi: 10.1161/STROKEAHA.108.535807. [DOI] [PubMed] [Google Scholar]
- 62.Catov JM, Dodge R, Barinas-Mitchell E et al. Prior preterm birth and maternal subclinical cardiovascular disease 4 to 12 years after pregnancy. J Womens Health (Larchmt) 2013;22:835–43. doi: 10.1089/jwh.2013.4248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Park K, Ouesada O, Galen Cook-Wiens M, Wei J. Adverse pregnancy outcomes are associated with reduced coronary flow reserve in women with signs and symptoms of ischemia without obstructive coronary artery disease: a report from the Women’s Ischemia Syndrome Evaluation – Coronary Vascular Dysfunction Study. J Womens Health (Larchmt) 2020;29:487–92. doi: 10.1089/jwh.2019.7925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Thilaganathan B, Kalafat E. Cardiovascular system in preeclampsia and beyond. Hypertension. 2019;73:522–31. doi: 10.1161/HYPERTENSIONAHA.118.11191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kalafat E, Sukur YE, Abdi A et al. Metformin for prevention of hypertensive disorders of pregnancy in women with gestational diabetes or obesity: systematic review and meta-analysis of randomized trials. Ultrasound Obstet Gynecol. 2018;52:706–14. doi: 10.1002/uog.19084. [DOI] [PubMed] [Google Scholar]
- 66.Giannakou K, Evangelou E, Papatheodorou SI. Genetic and non-genetic risk factors for pre-eclampsia: umbrella review of systematic reviews and meta-analyses of observational studies. Ultrasound Obstet Gynecol. 2018;51:720–30. doi: 10.1002/uog.18959. [DOI] [PubMed] [Google Scholar]
- 67.Hermes W, Ket JCF, van Pampus MG et al. Biochemical cardiovascular risk factors after hypertensive pregnancy disorders: a systematic review and meta-analysis. Obstet Gynecol Surv. 2012;67:792–808. doi: 10.1097/OGX.0b013e31827682fc. [DOI] [PubMed] [Google Scholar]
- 68.Ahmed R, Dunford J, Mehran R et al. Pre-eclampsia and future cardiovascular risk among women: a review. J Am Coll Cardiol. 2014;63:1815–22. doi: 10.1016/j.jacc.2014.02.529. [DOI] [PubMed] [Google Scholar]
- 69.Magnussen EB, Vatten LJ, Myklestad K et al. Cardiovascular risk factors prior to conception and the length of pregnancy: population-based cohort study. Am J Obstet Gynecol. 2011;204:526–e1–8. doi: 10.1016/j.ajog.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 70.Kanagalingam MG, Nelson SM, Freeman DJ et al. Vascular dysfunction and alteration of novel and classic cardiovascular risk factors in mothers of growth restricted offspring. Atherosclerosis. 2009;205:244–50. doi: 10.1016/j.atherosclerosis.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 71.Fraser A, Nelson SM, Macdonald-Wallis C et al. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon Longitudinal Study of Parents and Children. Circulation. 2012;125:1367–80. doi: 10.1161/CIRCULATIONAHA.111.044784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tanz LJ, Stuart JJ, Williams PL et al. Preterm delivery and maternal cardiovascular disease in young and middle-aged adult women. Circulation. 2017;135:578–89. doi: 10.1161/CIRCULATIONAHA.116.025954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mahendru AA, Everett TR, McEniery CM et al. Cardiovascular function in women with recurrent miscarriage, pre-eclampsia and/or intrauterine growth restriction. J Matern Fetal Neonatal Med. 2013;26:351–6. doi: 10.3109/14767058.2012.733774. [DOI] [PubMed] [Google Scholar]
- 74.Smith G, Wood A, Pell J, Hattie J. Recurrent miscarriage is associated with a family history of ischaemic heart disease: a retrospective cohort study. BJOG. 2011;118:557–63. doi: 10.1111/j.1471-0528.2010.02890.x. [DOI] [PubMed] [Google Scholar]
- 75.Steinthorsdottir V, McGinnis R, Williams NO et al. Genetic predisposition to hypertension is associated with preeclampsia in European and Central Asian women. Nat Commun. 2020;11:5976. doi: 10.1038/s41467-020-19733-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Honigberg MC, Chaffin M, Aragam K et al. Genetic variation in cardiometabolic traits and medication targets and the risk of hypertensive disorders of pregnancy. Circulation. 2020;142:711–13. doi: 10.1161/CIRCULATIONAHA.120.047936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Steffen KM, Cooper ME, Shi M et al. Maternal and fetal variation in genes of cholesterol metabolism is associated with preterm delivery. J Perinatol. 2007;27:672–80. doi: 10.1038/sj.jp.7211806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dior UP, Hochner H, Friedlander Y et al. Association between number of children and mortality of mothers: results of a 37-year follow-up study. Ann Epidemiol. 2013;23:13–8. doi: 10.1016/j.annepidem.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ness RB, Cobb J, Harris T, D’Agostino RB. Does number of children increase the rate of coronary heart disease in men? Epidemiology. 1995;6:442–5. doi: 10.1097/00001648-199507000-00023. [DOI] [PubMed] [Google Scholar]
- 80.Lawlor DA, Emberson JR, Ebrahim S et al. Is the association between parity and coronary heart disease due to biological effects of pregnancy or adverse lifestyle risk factors associated with child-rearing? Findings from the British Women’s Heart and Health Study and the British Regional Heart Study. Circulation. 2003;107:1260–4. doi: 10.1161/01.CIR.0000053441.43495.1A. [DOI] [PubMed] [Google Scholar]
- 81.Dekker JM, Schouten EG. Number of pregnancies and risk of cardiovascular disease. N Engl J Med. 1993;329:1893–4. doi: 10.1056/NEJM199312163292515. [DOI] [PubMed] [Google Scholar]
- 82.Goff DC Jr, Lloyd-Jones DM, Bennett G et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–59. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Timpka S, Fraser A, Schyman T et al. The value of pregnancy complication history for 10-year cardiovascular disease risk prediction in middle-aged women. Eur J Epidemiol. 2018;33:1003–10. doi: 10.1007/s10654-018-0429-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dam V, Onland-Moret NC, Verschuren WMM et al. Cardiovascular risk model performance in women with and without hypertensive disorders of pregnancy. Heart. 2019;105:330–6. doi: 10.1136/heartjnl-2018-313439. [DOI] [PubMed] [Google Scholar]
- 85.Benschop L, Brouwers L, Zoet GA et al. Early onset of coronary artery calcification in women with previous preeclampsia. Circ Cardiovasc Imaging. 2020;13:e010340. doi: 10.1161/CIRCIMAGING.119.010340. [DOI] [PubMed] [Google Scholar]
- 86.Wichmann JL, Takx RAP, Nunez JH et al. Relationship between pregnancy complications and subsequent coronary artery disease assessed by coronary computed tomographic angiography in black women. Circ Cardiovasc Imaging. 2019;12:e008754. doi: 10.1161/CIRCIMAGING.118.008754. [DOI] [PubMed] [Google Scholar]


