Abstract
Approximately one-half of patients undergoing diagnostic coronary angiography for angina have no significant coronary atherosclerotic stenosis. This clinical condition has recently been described as ischaemia with non-obstructive coronary arteries (INOCA). Coronary functional abnormalities are central to the pathogenesis of INOCA, including epicardial coronary spasm and coronary microvascular dysfunction composed of a variable combination of increased vasoconstrictive reactivity and/or reduced vasodilator function. During the last decade – in INOCA patients in particular – evidence for the prognostic impact of coronary functional abnormalities has accumulated and various non-invasive and invasive diagnostic techniques have enabled the evaluation of coronary vasomotor function in a comprehensive manner. In this review, the authors briefly summarise the recent advances in the understanding of pathophysiology and diagnosis of epicardial coronary artery spasm and coronary microvascular dysfunction.
Keywords: Epicardial coronary spasm, coronary microvascular dysfunction, coronary vasoreactivity testing, coronary flow reserve, biomarker, Rho-kinase
Ischaemic heart disease (IHD) is primarily caused by various combinations of three mechanisms – epicardial organic coronary stenosis attributable to atherosclerosis, epicardial coronary artery spasm and coronary microvascular dysfunction (CMD).[1–3] The representative clinical manifestations of these three mechanisms are effort angina, vasospastic angina (VSA) and microvascular angina (MVA), respectively. To date, much attention has been paid to the first mechanism, epicardial organic coronary stenosis, leading to the successful developments of percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG). However, approximately 40% of patients with obstructive coronary artery disease (CAD) still suffer from persistent/recurrent angina even after complete revascularisation with PCI and/or CABG.[4] In fact, numerous patients with symptoms and evidence of myocardial ischaemia have no significant epicardial organic coronary stenosis (>50%).
Epicardial spasm and CMD, which represent typical manifestations of coronary functional abnormalities, account for the condition recently termed as ischaemia with non-obstructive coronary arteries (INOCA).[5] Importantly, the prevalence of INOCA has rapidly increased, reported as reaching approximately 70% in women and 50% in men undergoing coronary angiography.[6] Furthermore, to the surprise of the cardiology community, the ISCHEMIA trial convincingly demonstrated that a revascularisation strategy with PCI or CABG has no significant prognostic benefit in patients with stable CAD and proven moderate to severe myocardial ischaemia.[7] These lines of evidence indicate the importance of coronary functional abnormalities in the pathogenesis and prognosis of chronic coronary syndrome, which has been described in the excellent European Association of Percutaneous Cardiovascular Interventions expert consensus document.[8]
Although aetiologies of impaired coronary vasomotion appear to be complex and heterogeneous, they always encompass vasodilator and vasoconstrictive properties in various combinations, where endothelial dysfunction and hypercontraction of vascular smooth muscle cells (VSMC) are substantially involved.[3,9,10] Various non-invasive and invasive techniques have been developed to evaluate coronary vasomotion during the last decade.[11,12] The aim of this review is to briefly summarise the current knowledge on the pathophysiology and diagnosis of coronary functional abnormalities.
Pathophysiology of Coronary Functional Abnormalities
Endothelial Dysfunction
Endothelial dysfunction has been shown to be a key mediator in the pathogenesis of coronary functional abnormalities.[3,13,14] The endothelium plays pivotal roles in modulating the tone of underlying VSMC by synthesising and releasing endothelium-derived relaxing factors (EDRFs), including vasodilator prostaglandins, nitric oxide (NO), and endothelium-dependent hyperpolarisation (EDH) factors, as well as endothelium-derived contracting factors (Figure 1).[15–17] Endothelial dysfunction is characterised by reduced production and/or action of EDRFs, serving as the hallmark of atherosclerotic cardiovascular diseases as well as one of the major pathogenetic mechanisms of CMD. It is important to note that these EDRFs regulate vascular tone in a distinct vessel size-dependent manner (Figure 1).
Figure 1: Vessel-size-dependent Contribution of Endothelium-derived Relaxing Factors and Rho-kinase-mediated Vascular Smooth Muscle Hypercontraction.
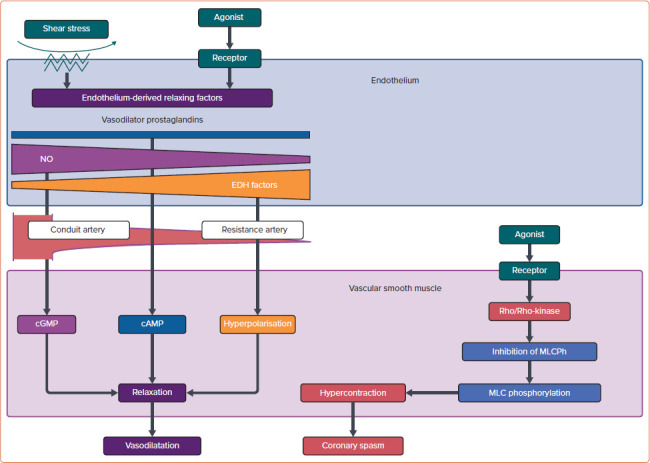
Endothelium-derived NO mainly causes vasodilation of large conduit vessels (e.g. epicardial coronary arteries), while EDH factors including H2O2 predominantly dilate resistance arteries (e.g. coronary microvessels). Rho-kinase plays a central role in the molecular mechanism of vascular smooth muscle hypercontraction caused by enhanced MLC phosphorylation through MLCPh inhibition. cAMP = cyclic adenosine monophosphate; cGMP = cyclic guanosine monophosphate; EDH = endothelium-dependent hyperpolarisation; NO = nitric oxide; MLC = myosin light chain; MLCPh = myosin light chain phosphatase.
Endothelium-derived NO mainly mediates vasodilatation of relatively large, conduit vessels (e.g. epicardial coronary arteries), while EDH factors-mediated responses are the predominant mechanisms of endothelium-dependent vasodilatation of resistance arteries (e.g. coronary microvessels).[16,17] Experimental studies have demonstrated that inhibition of endothelial NO production can aggravate myocardial hypoperfusion distal to an epicardial organic stenosis and that reduced NO bioavailability results in attenuation of endothelium-dependent vasodilatation.[16] On the other hand, endothelium-derived H2O2, which exerts various cardioprotective effects, such as metabolic coronary dilatation, coronary autoregulation, and myocardial protection against reperfusion injury, is a major EDH factor in various vascular beds including human coronary arteries.[3,17–19] Thus, it is conceivable that impaired H2O2/EDH factor-mediated vasodilatation is involved in the pathogenesis of CMD.[1,17] Indeed, our recent study revealed that both NO- and EDH-derived vasodilatations are prominently impaired in patients with MVA.[14]
Rho-kinase as a Key Molecule of Coronary Artery Spasm
Coronary artery spasm causes a primary reduction in coronary blood flow (CBF), resulting in the abrupt development of myocardial ischaemia. It can develop in both epicardial coronary arteries and coronary microvessels. Since coronary spasm can be induced by a variety of stimuli with different mechanisms of action (even in the same patient), it is not caused by abnormalities of specific agonist–receptor interaction but an enhanced reactivity (hyperreactivity) of the vessel to a generalised stimulus.[20] Reduced availability of endogenous vasodilator substances and VSMC hypersensitivity may contribute to vascular hyperreactivity leading to the onset of coronary spasm, whereas the role of endothelial dysfunction may be minimal.[3] Evidence for the primary role of VSMC hypercontraction but not endothelial dysfunction in the pathogenesis of coronary artery spasm is summarised in Table 1.[3]
Table 1: Primary Role of Vascular Smooth Muscle Hypercontraction in the Pathogenesis of Coronary Artery Spasm.
| Coronary Artery Spasm (VSMC Hypercontraction) | Endothelial Dysfunction |
|---|---|
| Local | Systemic |
| Evidence of coronary VSMC hypercontraction | Preserved endothelium-dependent response to BK and SP Failure of EPA with improved endothelial function to suppress coronary spasm |
| Racial difference | No racial difference |
| Marked diurnal change | Less diurnal change |
| Fluctuation and spontaneous remission | No fluctuation and spontaneous remission |
| Acute effects of vasodilators | No acute effects of vasodilators |
BK = bradykinin; EPA = eicosapentaenoic acid; SP = substance P; VSMC = vascular smooth muscle cells. Source: Shimokawa et al. 2014.[3] Reproduced with permission from Oxford University Press.
Accumulated evidence proves that a major mechanism of VSMC hypersensitivity is caused by enhanced Rho-kinase activity, an enzyme that controls contraction and relaxation of VSMC independently of intracellular Ca2+ concentration (Figure 1).[21] Activated Rho-kinase enhances myosin light chain phosphorylation through inhibition of the myosin-binding subunit of myosin phosphatase, leading to VSMC hypercontraction. Importantly, the Rho-kinase inhibitor fasudil has been shown to prevent acetylcholine (ACh)-induced coronary artery spasm in patients with VSA, confirming that Rho/Rho-kinase pathway plays a central role in the pathophysiology of coronary spasm.[22] It is known that various inflammatory stimuli, including angiotensin II and interleukin-1β, upregulate the expression and activity of Rho-kinase in VSMCs.[3] Intriguingly, oestrogen has an inhibitory effect on inflammation-induced Rho-kinase up-regulation, which may partly account for the increased incidence of atherosclerotic and vasospastic disorders in postmenopausal women.[5,23]
Diagnosis of Coronary Functional Abnormalities
Clinical Importance of the Evaluation of Epicardial Coronary Vasoreactivity
Coronary artery spasm plays an important role in the pathogenesis of a wide variety of IHD, including VSA, variant angina, acute MI, sudden cardiac death and intractable angina after successful coronary stent implantation.[24–26] In particular, VSA is the centre of entity among disorders that represent hyperreactivity of epicardial coronary arteries to vasoconstrictor stimuli. Thus, it is important to make a correct diagnosis of VSA and evaluate epicardial coronary vasoreactivity.
Clinical Definition and Diagnostic Criteria of Vasospastic Angina
Definite VSA is diagnosed when ischaemic ECG changes – defined as a transient ST-segment elevation or depression of >0.1 mV, or new appearance of negative U waves in at least two contiguous leads – are documented during spontaneous angina attack.[27] In cases without such diagnostic ECG ischaemic changes, definite VSA is angiographically diagnosed when transient, total, or subtotal (>90% stenosis) of a coronary artery accompanied by angina pain and ischaemic ECG changes during spasm provocation testing with ACh, ergonovine, or hyperventilation.[27] The position paper from the Coronary Artery Vasomotion Disorders International Study group also refers to typical symptoms for VSA as follows: subjective symptoms often appear at rest, especially between night and early morning; exercise tolerance is markedly reduced in the morning; hyperventilation relates to the symptoms; and calcium-channel blockers (CCBs) are effective to suppress the symptoms.[28]
Clinical Significance of Pharmacological Spasm Provocation Testing
Intracoronary pharmacological spasm provocation testing is highly recommended for patients with suspected coronary artery spasm.[27,28] In particular, high diagnostic accuracy of ACh testing for coronary spasm (90% sensitivity, 99% specificity) is universally recognised.[29] Thus, invasive ACh provocation testing remains the gold standard of diagnostic approach of coronary spasm at present, although non-invasive spasm provocation testing including transthoracic echocardiography with IV ergonovine has also been proposed.[30] Recent studies from Europe also revealed that pharmacological spasm provocation testing with ACh is safe and that coronary spasm plays a key role in development of a broad range of IHD in white patients as it does in Asian patients.[31,32] Importantly, Japanese and German patients with VSA have similar results of ACh provocation testing in terms of distribution of spasm type and frequency of multivessel spasm.[33] Moreover, risk stratification for VSA patients can be done using the findings of ACh testing. Indeed, studies have demonstrated that a mixture of focal and diffuse spasm provoked in multivessel coronary arteries strongly correlated with the occurrence of adverse events during the follow-up period, while coronary spasm induced at the site of significant organic stenosis was also associated with poor prognosis of VSA patients.[34,35]
The Japanese Coronary Spasm Association (JCSA) risk score could provide comprehensive risk assessment and prognostic stratification for VSA patients, which consists of seven variables, including history of out-of-hospital cardiac arrest (OHCA; 4 points), smoking, rest angina alone, organic coronary stenosis, multivessel spasm during spasm provocation testing (2 points each), ST-segment elevation during angina and β-blocker use (1 point each; Table 2).[36] Among those seven variables, organic coronary stenosis and multivessel spasm could be identified by angiography and pharmacological spasm provocation testing.
Table 2: The Japanese Coronary Spasm Association Risk Score.
| Predictive Factor | Score |
|---|---|
| History of out-of-hospital cardiac arrest | 4 |
| Smoking | 2 |
| Angina at rest alone | 2 |
| Significant organic stenosis | 2 |
| Multivessel spasm | 2 |
| ST-segment elevation | 1 |
| β-blocker use | 1 |
| Possible range | 0–14 |
Developed by Takagi et al. 2013.[36]
Diagnostic Approaches to Sudden Cardiac Death Related to Coronary Spasm
Syncope, which is caused by ventricular tachyarrhythmias or bradycardia due to transient conduction disturbances, is an important manifestation of VSA. It is commonly preceded by anginal pain, although not in all cases. In a subgroup of survivors with OHCA, coronary spasm and silent myocardial ischaemia were identified as a likely cause of their fatal arrhythmias.[37] Since VSA patients who survived OHCA are a particularly high-risk population, even in the current era with established effective therapies such as long-acting CCBs, implantation of an ICD with optimal medications may be appropriate for them.[38,39] We have previously reported that the dual induction tests for coronary artery spasm and lethal ventricular arrhythmias could stratify high-risk OHCA patients and evaluate the necessity of ICD by underlying mechanisms involved.[40] Among OHCA survivors without structural heart disease, provokable coronary spasm and ventricular arrhythmias were common and could also be seen in Brugada syndrome.[40] Thus, patients with coronary spasm alone but not Brugada syndrome who are treated with CCBs could be regarded as a low-risk group, indicating that ICD may not be essential for them.
Diagnostic Imaging for Coronary Spasm
Cardiovascular imaging could provide additional information at cellular and molecular levels in patients with VSA. An intravascular imaging study showed that atherosclerotic changes are more common in the segment of focal spasm site as compared with diffuse spasm.[41] In particular, optical coherence tomography (OCT), which is a high-resolution imaging modality, is capable of visualising not only morphological features of coronary vascular wall but also adventitial vasa vasorum formation at the spasm site.[42,43] Chronic inflammatory changes in the coronary adventitia play important roles in the pathogenesis of coronary spasm through Rho-kinase activation and resultant VSMC hypercontraction.[44] Indeed, OCT-delineated adventitial vasa vasorum formation was significantly enhanced at the spastic segments of VSA patients compared with those of control subjects.[43,45] Coronary perivascular adipose tissue volume measured by CT coronary angiography is also increased at the spastic segment of VSA patients.[46] Intriguingly, coronary perivascular adipose tissue inflammatory changes evaluated by [18]F-fluorodeoxyglucose PET imaging were more extensive at the spastic coronary segments of VSA patients as compared with control subjects, and the inflammatory changes were significantly suppressed after medical treatment with CCBs.[46] These imaging approaches may serve as a promising avenue for elucidation of the pathogenesis of coronary spasm in patients with VSA.
Advances in Diagnostic Approaches to Coronary Microvascular Dysfunction
CMD has emerged as a third potential mechanism of myocardial ischaemia in addition to atherosclerotic stenosis and spasm of epicardial coronary arteries.[2,3] Since the presence of CMD appears to be associated with increased risk of cardiovascular events, it is important to make a correct diagnosis of CMD based on objective and functional assessments of coronary microcirculation.[47] From a pathophysiological point of view, CMD represents the impairment in inherent regulatory mechanisms of coronary microvasculature for myocardial blood flow to adapt to changes in myocardial oxygen demand.[48] More specifically, CMD is originated by a variable combination of impaired vasodilatation and increased vasoconstriction of coronary microvessels.[48] However, in contrast with epicardial coronary arteries, coronary microvessels cannot be directly visualised in vivo with coronary angiography or intracoronary imaging devices. Thus, in the clinical setting, microvascular function must be assessed indirectly, generally through measurements of coronary blood flow regulated mainly by coronary arteriolar tone, or detection of propensity to coronary vasoconstriction.
Clinical Characteristics of Microvascular Angina Due to Coronary Microvascular Dysfunction
Patients with MVA due to CMD often have chest pain that can persist even after cessation of the activity. They have no rapid or sufficient symptom relief in response to sublingual nitroglycerin, which selectively dilates larger arteries but not arterioles or microvessels.[49] Based on these clinical features of MVA, the Coronary Vasomotor Disorders International Study group has proposed diagnostic criteria for MVA (Table 3).[50] Angina occurs in approximately 30–70% of patients with CMD, whereas other cardiac manifestations of CMD include exertional dyspnoea and possibly heart failure.[51–53] CMD may represent an ischaemic equivalent caused by left ventricle (LV) diastolic dysfunction with an excessive rise in end-diastolic pressure leading to cardiopulmonary congestion. Indeed, coexistence of CMD and LV diastolic dysfunction is associated with a remarkably increased risk of heart failure with preserved ejection fraction (HFpEF) hospitalisation.[53] Particularly in patients with hypertension and preserved systolic function, CMD as well as subclinical myocardial mechanical dysfunction predicted HF hospitalisation independently of LV remodelling severity.[54]
Table 3: Clinical Criteria for Suspecting Microvascular Angina.
| 1. Symptoms of myocardial ischaemia a. Effort and/or rest angina b. Angina equivalents (e.g. shortness of breath) |
| 2. Absence of obstructive CAD (<50% diameter reduction or FFR >0.80) by a. Coronary CTA b. Invasive coronary angiography |
| 3. Objective evidence of myocardial ischaemia a. Ischaemic ECG changes during an episode of chest pain b. Stress-induced chest pain and /or ischaemic ECG changes in the presence or absence of transient/reversible abnormal myocardial perfusion and/or wall motion abnormality |
| 4. Evidence of impaired coronary microvascular function a. Impaired coronary flow reserve (cut-off values depending on methodology use between ≤2.0 and ≤2.5) b. Coronary microvascular spasm, defined as reproduction of symptoms, ischaemic ECG shifts but no epicardial spasm during acetylcholine testing c. Abnormal coronary microvascular resistance indices (e.g. IMR >25) d. Coronary slow flow phenomenon, defined as TIMI frame count >25 |
Definite MVA is only diagnosed if all four criteria are present. Suspected MVA is diagnosed if symptoms of ischaemia are present with non-obstructive CAD but only objective evidence of myocardial ischaemia, or evidence of impaired coronary microvascular function alone. CAD = coronary artery disease; CTA = computed tomographic angiography; FFR = fractional flow reserve; IMR = index of microcirculatory resistance; TIMI = thrombolysis in myocardial infarction. Source: Ong et al. 2018.[50] Used with permission from Elsevier.
Assessment for Vasodilator Function of Coronary Microvessels
Coronary microvascular vasodilator function is usually assessed by measurement of coronary microvascular response to vasodilator stimuli. In many cases, the vasodilator capacity is often evaluated by coronary flow reserve (CFR) calculated as the ratio of CBF during maximal vasodilatation over basal CBF.[11,12] CFR reflects an integrated measurement of flow throughout both large epicardial artery and coronary microvessels. Thus, without obstructive stenosis of epicardial coronary arteries, reduced CFR indicates the entity of CMD.[11,12] Depending on the methodology, CFR cut-off values between ≤2.0 and ≤2.5 are indicative for impaired coronary microvascular function.[55]
The most widely used agent to assess coronary microvascular dilator function is adenosine. Adenosine is intravenously administered at 140 μg/kg/min, as this dose has been found to achieve maximal coronary microvascular dilatation.[56] Adenosine has possible adverse effects, including bradycardia due to atrioventricular or sino-atrial node blockade and bronchoconstriction, both of which are mediated by purinergic A1 receptors. However, a relevant advantage of adenosine is its very short half-life (10 seconds) that enables rapid regression of side-effects and repetition of the test during the same session, if necessary.[56] ACh is also used as a coronary microvascular vasodilator.[52] However, ACh is not an ideal substance to assess endothelium-dependent vasodilator function, since it also acts directly on VSMCs, leading to vasoconstriction (Table 1).[3]
There is a range of non-invasive approaches for evaluation of coronary vasodilator responses, but all of them have several limitations.[11] Transthoracic Doppler echocardiography (TTDE) enables us to measure coronary blood flow velocity of the distal left anterior descending artery as a surrogate for CBF with advantages of low cost and high feasibility. A reduced coronary blood flow velocity reserve index obtained by TTDE helps to identify patients with CMD and enables the risk stratification for them.[57] On the other hand, considerable intra- and inter-observer variabilities (~10%) need to be taken into account when examining serial recordings obtained for assessing the effects of therapy.[58]
PET is a well-validated technique that can provide non-invasive, accurate, and reproducible quantification of myocardial blood flow and CFR in humans, and thus has been used for the assessment of coronary vasomotor function.[48] PET also has the advantage of assessing all three coronary distributions, allowing a more accurate assessment of microvascular dysfunction, where CMD has been shown to have a heterogenous distribution over the three coronary arteries.[48] Recent PET studies demonstrated that coronary vasodilator dysfunction, as defined by reduced CFR, is highly prevalent among patients with CAD, increases the severity of inducible myocardial ischaemia and subclinical myocardial injury, and identifies patients at high risk for future cardiac events.[59,60]
Cardiac magnetic resonance (CMR) has also been used to quantify myocardial perfusion following the injection of a gadolinium-based contrast agent. Advantages of CMR include high spatial resolution that allows transmural characterisation of myocardial blood flow, the lack of ionising radiation, and the ability to perform a comprehensive assessment of cardiovascular structure and function. In particular, CMR-derived myocardial perfusion reserve index (MPRI) is a robust semi-quantitative imaging surrogate that reflects vasodilator capacity of coronary microvessels.[61] Recent studies demonstrated that a MPRI threshold of ≤1.84 has a diagnostic predictive value for CMD and that of ≤1.47 is associated with the occurrence of major adverse cardiac events.[62,63]
Coronary angiography combined with complementary catheter-based devices is a useful approach to examine coronary vasodilator capacity of patients with CMD.[11,12] It often involves an interventional procedure where a guidewire-based assessment of CBF is performed at rest and at hyperaemia induced by pharmacological agents (e.g. adenosine).[32,52,64] Although the procedure is invasive by nature and can be time-consuming, it has been shown to be safe and effective when performed by experienced interventional operators as discussed in detail later.[65]
Objective Documentation of Coronary Microvascular Spasm
In a sizable number of patients with angina, pressure-rate product (an index of myocardial oxygen demand) is usually comparable between at rest and at onset of attack, indicating that the decrease in CBF rather than increased myocardial oxygen consumption is a likely explanation for myocardial ischaemia.[48] Primary reduction in CBF caused by coronary spasm at not only epicardial conduit arteries but also myocardial microvasculature could be attributable to angina at rest.[66] Since a visualisation of coronary microvascular spasm (MVS) is still difficult due to the limited spatial resolution of existing intracoronary imaging devices, the development of MVS is generally identified by the reproduction of chest discomfort suggestive of angina with ischaemic ECG changes, in the absence of ≥90% epicardial stenosis during intracoronary ACh administration (Table 3).[50]
Almost a quarter of a century has passed since Mohri et al. originally described the incidence of MVS in a subset of patients with rest angina and normal epicardial coronary arteries.[67] Indeed, it has been recently reported that the vast majority (97%) of INOCA patients with coronary functional abnormalities have epicardial or microvascular vasospasm in approximately equal proportions.[68] Furthermore, in INOCA patients, MVS is sometimes provoked at lower doses of intracoronary ACh, followed by diffuse epicardial spasm at higher doses, indicating that a common mechanism is involved in both epicardial and microvascular spasms such as Rho-kinase activation.[69]
Meanwhile, for corroborating the entity of MVS, monitoring of myocardial lactate production throughout ACh provocation testing as an objective marker of myocardial ischaemia is recommended.[27] Negative myocardial lactate extraction ratio, which is calculated as the ratio of the coronary arterial–venous difference in lactate concentration to the arterial concentration, is considered to be highly sensitive for myocardial ischaemia.[69] Inevitably, MVS is defined as having a negative myocardial lactate extraction ratio despite the absence of angiographically demonstrable epicardial spasm throughout ACh provocation testing or prior to the occurrence of epicardial coronary spasm following intracoronary injection of ACh.[67,69]
Comprehensive Evaluation of Coronary Functional Abnormalities by Interventional Procedures
Recently, the combined invasive assessment of coronary vasoconstrictor and vasodilator abnormalities has been titled as an interventional diagnostic procedure (IDP), which typically consist of vasoreactivity testing with ACh and measurement of CFR and IMR with adenosine (Figure 2).[12,70] Although there has been a critical missing link between IDP for assessment of coronary vasomotor function and health outcomes of INOCA patients, this gap has recently been addressed in the CorMicA randomised controlled trial.[32,71] In this landmark study, Ford et al. demonstrated that an IDP linked to the stratified medication could ameliorate health status of patients with INOCA and that better quality of life was maintained among patients undergoing an IDP over 1 year.[71] The IDP also allows us to acknowledge that several vascular dysfunction mechanisms may co-exist and overlap in a patient with INOCA.[64,72] Furthermore, clarifying INOCA endotypes enable us to predict the clinical course of INOCA patients. The entity of impaired coronary microvascular dilator function predicts adverse cardiovascular outcomes, including death and non-fatal MI, in female INOCA patients, whereas enhanced epicardial coronary vasoconstrictive reactivity was related to angina hospitalisation.[47] Additionally, in INOCA patients, coexistence of epicardial coronary spasm and increased microvascular resistance was associated with worse prognosis, for which Rho-kinase activation appears to be involved.[64]
Figure 2: Protocol for the Invasive Diagnostic Procedure.
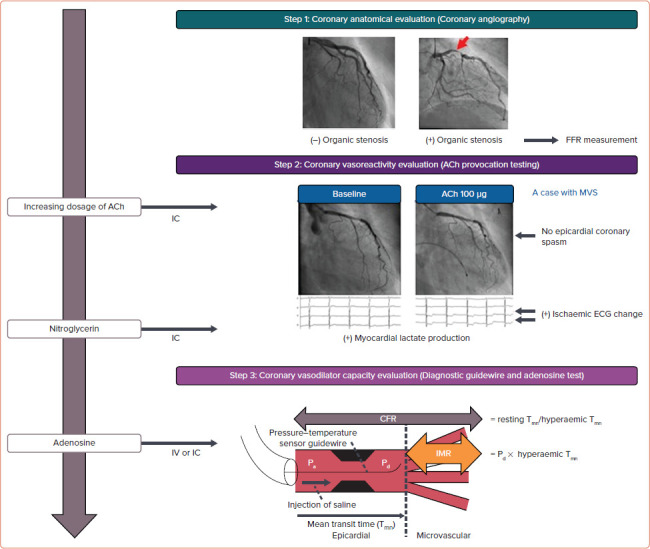
The first step is the identification of coronary organic stenosis by diagnostic coronary angiography. In patients with significant organic coronary stenosis (>50% luminal narrowing), measurement of FFR should be considered. The second step is ACh provocation testing for coronary spasm. Additional evaluation for myocardial lactate production is useful to confirm the emergence of MVS without or prior to the development of epicardial coronary spasm. A case diagnosed with MVS is demonstrated. The third step is to perform wire-based assessment of CFR and IMR for evaluation of vasodilator microvascular capacity in response to adenosine. ACh = acetylcholine; CFR = coronary flow reserve; FFR = fractional flow reserve; IC = intracoronary; IMR = index of microcirculatory resistance; MVS = microvascular spasm; Pa = mean proximal coronary pressure; Pd = mean distal coronary pressure; Tmn = mean transit time.
Taken together, comprehensive assessment of coronary functional abnormalities with the IDP could be useful to develop a strategic and distinct outlook for managements of INOCA patients. This is the reason why the IDP is highly recommended for patients with chest pain and no obstructive CAD in the recent consensus documents on INOCA by the European Society of Cardiology.[8] Meanwhile, CMD diagnosed based on the results of IDP may be associated with the presence of virtual histology intravascular-ultrasound-derived thin-cap fibroatheroma.[73] Also, in our recent work, the prognostic links between coronary morphologies evaluated by optical coherence tomography and coronary vasomotor were noted in INOCA patients.[74] These findings indicate that a combination of intracoronary imaging device-derived morphometric assessment and coronary functional assessment with IDP could greatly improve the prognostic prediction of INOCA patients.
Biomarkers of Coronary Functional Abnormalities
We have previously demonstrated that Rho-kinase activity in circulating neutrophils is a useful surrogate biomarker for coronary spasm, not only for the diagnosis of the disorder but also for the assessment of disease activity and efficacy of medical treatment.[75] Furthermore, there is a circadian variation of Rho-kinase activity in circulating neutrophils with a peak noted in the early morning, associated with alterations in coronary basal tone and vasomotor reactivity.[76]
A previous experimental study showed that sustained elevation of serum cortisol level sensitises coronary VSMC to serotonin to cause coronary vasoconstrictive responses in pigs in vivo, suggesting the cross-link between stress and coronary artery spasm.[77] In fact, Rho-kinase activity in circulating neutrophils in VSA patients was temporarily enhanced immediately after the Great East Japan Earthquake associated with disaster-related mental stress.[78] Finally, Rho-kinase activity in circulating leucocytes is also useful for prognostic stratification of VSA patients.[79] The combination of the JCSA risk score and Rho-kinase activity substantially improved risk stratification of VSA patients as compared with either alone.[79] Taking these issues into consideration, Rho-kinase activity in circulating leucocytes appears to be a useful biomarker for coronary spasm with a broad versatility, comparing favourably with B-type natriuretic peptide in patients with heart failure and high-sensitivity cardiac troponin T or I in those with acute coronary syndrome.
Although the importance of CMD has been emerging, reliable biomarkers for CMD remain to be developed. Low-grade inflammation attracts much attention in the pathogenesis of CMD, since elevated C-reactive protein levels correlated with reduced CFR in patients with cardiac syndrome X, which is indicative of CMD.[80] A recent study also demonstrated that cardiovascular protein biomarkers of inflammatory status and coagulation changes are associated with endothelium-independent CMD in female INOCA patients.[81] Although several clinical studies previously addressed the relationship between systemic serotonin concentrations and coronary vasomotor abnormalities, we have recently demonstrated that plasma concentration of serotonin was significantly higher in patients with microvascular spasm as compared with controls.[82] Importantly, in patients with INOCA, there was a positive correlation between plasma serotonin concentration and baseline thrombolysis in myocardial infarction frame count, a marker of coronary vascular resistance.[11,82] These findings suggest that plasma concentration of serotonin may be a novel biomarker to predict latent microvascular spasm and enable us to dissect it from epicardial coronary artery spasm.
Conclusion
In summary, it is important to evaluate coronary vasomotor function comprehensively and diagnose coronary functional abnormalities including VSA and CMD precisely, particularly in INOCA patients. Further studies are needed to better understand the pathophysiology of coronary vasomotor dysfunction and to develop new effective therapeutic strategies for patients with coronary functional abnormalities.
References
- 1.Shimokawa H. (ed). Coronary vasomotion abnormalities. Singapore: Springer, 2021
- 2.Knuuti J, Wijns W, Saraste A et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–77. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 3.Shimokawa H. 2014 Williams Harvey Lecture: importance of coronary vasomotion abnormalities-from bench to bedside. Eur Heart J. 2014;35:3180–93. doi: 10.1093/eurheartj/ehu427. [DOI] [PubMed] [Google Scholar]
- 4.Crea F, Bairey Merz CN, Beltrame JF et al. Mechanisms and diagnostic evaluation of persistent or recurrent angina following percutaneous coronary revascularization. Eur Heart J. 2019;40:2455–62. doi: 10.1093/eurheartj/ehy857. [DOI] [PubMed] [Google Scholar]
- 5.Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and No Obstructive Coronary Artery Disease (INOCA): Developing evidence-based therapies and research agenda for the next decade. Circulation. 2017;135:1075–92. doi: 10.1161/CIRCULATIONAHA.116.024534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jespersen L, Hvelplund A, Abildstrom SZ et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33:734–44. doi: 10.1093/eurheartj/ehr331. [DOI] [PubMed] [Google Scholar]
- 7.Maron DJ, Hochman JS, Reynolds HR et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382:1395–407. doi: 10.1056/NEJMoa1915922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kunadian V, Chieffo A, Camici PG et al. An EAPCI expert consensus document on ischaemia with non-obstructive coronary arteries in collaboration with European Society of Cardiology Working Group on coronary pathophysiology & microcirculation endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41:3504–20. doi: 10.1093/eurheartj/ehaa503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Padro T, Manfrini O, Bugiardini R et al. ESC Working Group on Coronary Pathophysiology and Microcirculation position paper on ‘coronary microvascular dysfunction in cardiovascular disease’. Cardiovasc Res. 2020;116:741–55. doi: 10.1093/cvr/cvaa003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sechtem U, Brown D, Godo S et al. Coronary microvascular dysfunction in stable ischaemic heart disease (non-obstructive coronary artery disease and obstructive coronary artery disease). Cardiovasc Res. 2020;116:771–86. doi: 10.1093/cvr/cvaa005. [DOI] [PubMed] [Google Scholar]
- 11.Ong P, Safdar B, Seitz A et al. Diagnosis of coronary microvascular dysfunction in the clinic. Cardiovasc Res. 2020;116:841–55. doi: 10.1093/cvr/cvz339. [DOI] [PubMed] [Google Scholar]
- 12.Ford TJ, Ong P, Sechtem U et al. Assessment of vascular dysfunction in patients without obstructive coronary artery disease: why, how, and when. JACC Cardiovasc Interv. 2020;13:1847–64. doi: 10.1016/j.jcin.2020.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ford TJ, Rocchiccioli P, Good R et al. Systemic microvascular dysfunction in microvascular and vasospastic angina. Eur Heart J. 2018;39:4086–97. doi: 10.1093/eurheartj/ehy529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohura-Kajitani S, Shiroto T, Godo S et al. Marked impairment of endothelium-dependent digital vasodilatations in patients with microvascular angina: evidence for systemic small artery disease. Arterioscler Thromb Vasc Biol. 2020;40:1400–12. doi: 10.1161/ATVBAHA.119.313704. [DOI] [PubMed] [Google Scholar]
- 15.Gutterman DD, Chabowski DS, Kadlec AO et al. The human microcirculation: regulation of flow and beyond. Circ Res. 2016;118:157–72. doi: 10.1161/CIRCRESAHA.115.305364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vanhoutte PM, Shimokawa H, Feletou M, Tang EH. Endothelial dysfunction and vascular disease – a 30th anniversary update. Acta Physiol (Oxf) 2017;219:22–96. doi: 10.1111/apha.12646. [DOI] [PubMed] [Google Scholar]
- 17.Godo S, Suda A, Takahashi J et al. Coronary microvascular dysfunction. Arterioscler Thromb Vasc Biol. 2021;41:1625–37. doi: 10.1161/ATVBAHA.121.316025. [DOI] [PubMed] [Google Scholar]
- 18.Matoba T, Shimokawa H, Nakashima M et al. Hydrogen peroxide is an endothelium-derived hyperpolarizing factor in mice. J Clin Invest. 2000;106:1521–30. doi: 10.1172/JCI10506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shimokawa H, Matoba T. Hydrogen peroxide as an endothelium-derived hyperpolarizing factor. Pharmacol Res. 2004;49:543–9. doi: 10.1016/j.phrs.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 20.Kaski JC, Maseri A, Vejar M et al. Spontaneous coronary artery spasm in variant angina is caused by a local hyperreactivity to a generalized constrictor stimulus. J Am Coll Cardiol. 1989;14:1456–63. doi: 10.1016/0735-1097(89)90382-3. [DOI] [PubMed] [Google Scholar]
- 21.Shimokawa H, Sunamura S, Satoh K. RhoA/Rho-kinase in the cardiovascular system. Circ Res. 2016;118:352–66. doi: 10.1161/CIRCRESAHA.115.306532. [DOI] [PubMed] [Google Scholar]
- 22.Masumoto A, Mohri M, Shimokawa H et al. Suppression of coronary artery spasm by the Rho-kinase inhibitor fasudil in patients with vasospastic angina. Circulation. 2002;105:1545–7. doi: 10.1161/hc1002.105938. [DOI] [PubMed] [Google Scholar]
- 23.Hiroki J, Shimokawa H, Mukai Y et al. Divergent effects of estrogen and nicotine on Rho-kinase expression in human coronary vascular smooth muscle cells. Biochem Biophys Res Commun. 2005;326:154–9. doi: 10.1016/j.bbrc.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Montone RA, Niccoli G, Fracassi F et al. Patients with acute myocardial infarction and non-obstructive coronary arteries: safety and prognostic relevance of invasive coronary provocative tests. Eur Heart J. 2018;39:91–8. doi: 10.1093/eurheartj/ehx667. [DOI] [PubMed] [Google Scholar]
- 25.Ahn JM, Lee KH, Yoo SY et al. Prognosis of variant angina manifesting as aborted sudden cardiac death. J Am Coll Cardiol. 2016;68:137–45. doi: 10.1016/j.jacc.2016.04.050. [DOI] [PubMed] [Google Scholar]
- 26.Ong P, Athanasiadis A, Perne A et al. Coronary vasomotor abnormalities in patients with stable angina after successful stent implantation but without in-stent restenosis. Clin Res Cardiol. 2014;103:11–9. doi: 10.1007/s00392-013-0615-9. [DOI] [PubMed] [Google Scholar]
- 27.JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (Coronary Spastic Angina) (JCS 2013). Circ J. 2014;78:2779–801. doi: 10.1253/circj.cj-66-0098. [DOI] [PubMed] [Google Scholar]
- 28.Beltrame JF, Crea F, Kaski JC et al. International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 2017;38:2565–8. doi: 10.1093/eurheartj/ehv351. [DOI] [PubMed] [Google Scholar]
- 29.Okumura K, Yasue H, Matsuyama K et al. Sensitivity and specificity of intracoronary injection of acetylcholine for the induction of coronary artery spasm. J Am Coll Cardiol. 1988;12:883–8. doi: 10.1016/0735-1097(88)90449-4. [DOI] [PubMed] [Google Scholar]
- 30.Om SY, Yoo SY, Cho GY et al. Diagnostic and prognostic value of ergonovine echocardiography for noninvasive diagnosis of coronary vasospasm. JACC Cardiovasc Imaging. 2020;13:1875–87. doi: 10.1016/j.jcmg.2020.03.008. [DOI] [PubMed] [Google Scholar]
- 31.Seitz A, Gardezy J, Pirozzolo G et al. Long-term follow-up in patients with stable angina and unobstructed coronary arteries undergoing intracoronary acetylcholine testing. JACC Cardiovasc Interv. 2020;13:1865–76. doi: 10.1016/j.jcin.2020.05.009. [DOI] [PubMed] [Google Scholar]
- 32.Ford TJ, Stanley B, Good R et al. Stratified medical therapy using invasive coronary function testing in angina: the CorMicA Trial. J Am Coll Cardiol. 2018;72:2841–55. doi: 10.1016/j.jacc.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 33.Suda A, Seitz A, Odaka Y et al. Assessment of coronary vasomotor responses to acetylcholine in German and Japanese patients with epicardial coronary spasm-more similarities than differences? Heart Vessels. 2021;36:337–44. doi: 10.1007/s00380-020-01707-9. [DOI] [PubMed] [Google Scholar]
- 34.Takagi Y, Yasuda S, Takahashi J et al. Clinical implications of provocation tests for coronary artery spasm: safety, arrhythmic complications, and prognostic impact: multicentre registry study of the Japanese Coronary Spasm Association. Eur Heart J. 2013;34:258–67. doi: 10.1093/eurheartj/ehs199. [DOI] [PubMed] [Google Scholar]
- 35.Ishii M, Kaikita K, Sato K et al. Acetylcholine-provoked coronary spasm at site of significant organic stenosis predicts poor prognosis in patients with coronary vasospastic angina. J Am Coll Cardiol. 2015;66:1105–15. doi: 10.1016/j.jacc.2015.06.1324. [DOI] [PubMed] [Google Scholar]
- 36.Takagi Y, Takahashi J, Yasuda S et al. Prognostic stratification of patients with vasospastic angina: a comprehensive clinical risk score developed by the Japanese Coronary Spasm Association. J Am Coll Cardiol. 2013;62:1144–53. doi: 10.1016/j.jacc.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 37.Myerburg RJ, Kessler KM, Mallon SM et al. Life-threatening ventricular arrhythmias in patients with silent myocardial ischemia due to coronary-artery spasm. N Engl J Med. 1992;326:1451–5. doi: 10.1056/NEJM199205283262202. [DOI] [PubMed] [Google Scholar]
- 38.Takagi Y, Yasuda S, Tsunoda R et al. Clinical characteristics and long-term prognosis of vasospastic angina patients who survived out-of-hospital cardiac arrest: multicenter registry study of the Japanese Coronary Spasm Association. Circ Arrhythm Electrophysiol. 2011;4:295–302. doi: 10.1161/CIRCEP.110.959809. [DOI] [PubMed] [Google Scholar]
- 39.Matsue Y, Suzuki M, Nishizaki M et al. Clinical implications of an implantable cardioverter-defibrillator in patients with vasospastic angina and lethal ventricular arrhythmia. J Am Coll Cardiol. 2012;60:908–13. doi: 10.1016/j.jacc.2012.03.070. [DOI] [PubMed] [Google Scholar]
- 40.Komatsu M, Takahashi J, Fukuda K et al. Usefulness of testing for coronary artery spasm and programmed ventricular stimulation in survivors of out-of-hospital cardiac arrest. Circ Arrhythm Electrophysiol. 2016;9 doi: 10.1161/CIRCEP.115.003798. [DOI] [PubMed] [Google Scholar]
- 41.Kitano D, Takayama T, Sudo M et al. Angioscopic differences of coronary intima between diffuse and focal coronary vasospasm: Comparison of optical coherence tomography findings. J Cardiol. 2018;72:200–7. doi: 10.1016/j.jjcc.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 42.Tanaka A, Taruya A, Shibata K et al. Coronary artery lumen complexity as a new marker for refractory symptoms in patients with vasospastic angina. Sci Rep. 2021;11:13. doi: 10.1038/s41598-020-79669-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nishimiya K, Matsumoto Y, Uzuka H et al. Focal vasa vasorum formation in patients with focal coronary vasospasm – an optical frequency domain imaging study. Circ J. 2016;80:2252–4. doi: 10.1253/circj.CJ-16-0580. [DOI] [PubMed] [Google Scholar]
- 44.Kandabashi T, Shimokawa H, Miyata K et al. Inhibition of myosin phosphatase by upregulated Rho-kinase plays a key role for coronary artery spasm in a porcine model with interleukin-1beta. Circulation. 2000;101:1319–23. doi: 10.1161/01.cir.101.11.1319. [DOI] [PubMed] [Google Scholar]
- 45.Nishimiya K, Matsumoto Y, Takahashi J et al. Enhanced adventitial vasa vasorum formation in patients with vasospastic angina: assessment with OFDI. J Am Coll Cardiol. 2016;67:598–600. doi: 10.1016/j.jacc.2015.11.031. [DOI] [PubMed] [Google Scholar]
- 46.Ohyama K, Matsumoto Y, Takanami K et al. Coronary adventitial and perivascular adipose tissue inflammation in patients with vasospastic angina. J Am Coll Cardiol. 2018;71:414–25. doi: 10.1016/j.jacc.2017.11.046. [DOI] [PubMed] [Google Scholar]
- 47.AlBadri A, Bairey Merz CN, Johnson BD et al. Impact of abnormal coronary reactivity on long-term clinical outcomes in women. J Am Coll Cardiol. 2019;73:684–93. doi: 10.1016/j.jacc.2018.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Camici PG, d’Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. 2015;12:48–62. doi: 10.1038/nrcardio.2014.160. [DOI] [PubMed] [Google Scholar]
- 49.Kanatsuka H, Eastham CL, Marcus ML, Lamping KG. Effects of nitroglycerin on the coronary microcirculation in normal and ischemic myocardium. J Cardiovasc Pharmacol. 1992;19:755–63. [PubMed] [Google Scholar]
- 50.Ong P, Camici PG, Beltrame JF et al. International standardization of diagnostic criteria for microvascular angina. Int J Cardiol. 2018;250:16–20. doi: 10.1016/j.ijcard.2017.08.068. [DOI] [PubMed] [Google Scholar]
- 51.Shimokawa H, Suda A, Takahashi J Clinical characteristics and prognosis of patients with microvascular angina: an international and prospective cohort study by the Coronary Vasomotor Disorders International Study (COVADIS) Group. Eur Heart J. 2021. [DOI] [PMC free article] [PubMed]
- 52.Sara JD, Widmer RJ, Matsuzawa Y et al. Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. JACC Cardiovasc Interv. 2015;8:1445–53. doi: 10.1016/j.jcin.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 53.Taqueti VR, Solomon SD, Shah AM et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J. 2018;39:840–9. doi: 10.1093/eurheartj/ehx721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhou W, Brown JM, Bajaj NS et al. Hypertensive coronary microvascular dysfunction: a subclinical marker of end organ damage and heart failure. Eur Heart J. 2020;41:2366–75. doi: 10.1093/eurheartj/ehaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Löffler AI, Bourque JM. Coronary microvascular dysfunction, microvascular angina, and management. Curr Cardiol Rep. 2016;18:1. doi: 10.1007/s11886-015-0682-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Layland J, Carrick D, Lee M et al. Adenosine: physiology, pharmacology, and clinical applications. JACC Cardiovasc Interv. 2014;7:581–91. doi: 10.1016/j.jcin.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 57.Gan LM, Svedlund S, Wittfeldt A et al. Incremental value of transthoracic Doppler echocardiography-Assessed coronary flow reserve in patients with suspected myocardial ischemia undergoing myocardial perfusion scintigraphy. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.116.004875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rigo F, Richieri M, Pasanisi E et al. Usefulness of coronary flow reserve over regional wall motion when added to dual-imaging dipyridamole echocardiography. Am J Cardiol. 2003;91:269–73. doi: 10.1016/s0002-9149(02)03153-3. [DOI] [PubMed] [Google Scholar]
- 59.Taqueti VR, Everett BM, Murthy VL et al. Interaction of impaired coronary flow reserve and cardiomyocyte injury on adverse cardiovascular outcomes in patients without overt coronary artery disease. Circulation. 2015;131:528–35. doi: 10.1161/CIRCULATIONAHA.114.009716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gupta A, Taqueti VR, van de Hoef TP et al. Integrated noninvasive physiological assessment of coronary circulatory function and impact on cardiovascular mortality in patients with stable coronary artery disease. Circulation. 2017;136:2325–36. doi: 10.1161/CIRCULATIONAHA.117.029992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wöhrle J, Nusser T, Merkle N et al. Myocardial perfusion reserve in cardiovascular magnetic resonance: correlation to coronary microvascular dysfunction. J Cardiovasc Magn Reson. 2006;8:781–7. doi: 10.1080/10976640600737649. [DOI] [PubMed] [Google Scholar]
- 62.Thomson LE, Wei J, Agarwal M et al. Cardiac magnetic resonance myocardial perfusion reserve index is reduced in women with coronary microvascular dysfunction. A National Heart, Lung, and Blood Institute-sponsored study from the Women’s Ischemia Syndrome Evaluation. Circ Cardiovasc Imaging. 2015;8 doi: 10.1161/CIRCIMAGING.114.002481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou W, Lee JCY, Leung ST et al. Long-term prognosis of patients with coronary microvascular disease using stress perfusion cardiac magnetic resonance. JACC Cardiovasc Imaging. 2021;14:602–11. doi: 10.1016/j.jcmg.2020.09.034. [DOI] [PubMed] [Google Scholar]
- 64.Suda A, Takahashi J, Hao K et al. Coronary functional abnormalities in patients with angina and nonobstructive coronary artery disease. J Am Coll Cardiol. 2019;74:2350–60. doi: 10.1016/j.jacc.2019.08.1056. [DOI] [PubMed] [Google Scholar]
- 65.Wei J, Mehta PK, Johnson BD et al. Safety of coronary reactivity testing in women with no obstructive coronary artery disease: results from the NHLBI-sponsored WISE (Women’s Ischemia Syndrome Evaluation) study. JACC Cardiovasc Interv. 2012;5:646–53. doi: 10.1016/j.jcin.2012.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pereyra VM, Seitz A, Hubert A et al. Coronary microvascular spasm as the underlying cause of the angiographic slow flow phenomenon. JACC Case Rep. 2020;2:35–39. doi: 10.1016/j.jaccas.2019.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mohri M, Koyanagi M, Egashira K et al. Angina pectoris caused by coronary microvascular spasm. Lancet. 1998;351:1165–9. doi: 10.1016/S0140-6736(97)07329-7. [DOI] [PubMed] [Google Scholar]
- 68.Konst RE, Damman P, Pellegrini D et al. Vasomotor dysfunction in patients with angina and nonobstructive coronary artery disease is dominated by vasospasm. Int J Cardiol. 2021;333:14–20. doi: 10.1016/j.ijcard.2021.02.079. [DOI] [PubMed] [Google Scholar]
- 69.Sun H, Mohri M, Shimokawa H et al. Coronary microvascular spasm causes myocardial ischemia in patients with vasospastic angina. J Am Coll Cardiol. 2002;39:847–51. doi: 10.1016/s0735-1097(02)01690-x. [DOI] [PubMed] [Google Scholar]
- 70.Ford TJ, Berry C. How to diagnose and manage angina without obstructive coronary artery disease: Lessons from the British Heart Foundation CorMicA Trial. Interv Cardiol. 2019;14:76–82. doi: 10.15420/icr.2019.04.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ford TJ, Stanley B, Sidik N et al. 1-year outcomes of angina management guided by invasive coronary function testing (CorMicA). JACC Cardiovasc Interv. 2020;13:33–45. doi: 10.1016/j.jcin.2019.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ford TJ, Yii E, Sidik N et al. Ischemia and no obstructive coronary artery disease: Prevalence and correlates of coronary vasomotion disorders. Circ Cardiovasc Interv. 2019;12:e008126. doi: 10.1161/CIRCINTERVENTIONS.119.008126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Godo S, Corban MT, Toya T et al. Association of coronary microvascular endothelial dysfunction with vulnerable plaque characteristics in early coronary atherosclerosis. EuroIntervention. 2020;16:387–94. doi: 10.4244/EIJ-D-19-00265. [DOI] [PubMed] [Google Scholar]
- 74.Nishimiya K, Suda A, Fukui K et al. Prognostic links between OCT-delineated coronary morphologies and coronary functional abnormalities in patients with INOCA. JACC Cardiovasc Interv. 2021;14:606–18. doi: 10.1016/j.jcin.2020.12.025. [DOI] [PubMed] [Google Scholar]
- 75.Kikuchi Y, Yasuda S, Aizawa K et al. Enhanced Rho-kinase activity in circulating neutrophils of patients with vasospastic angina: a possible biomarker for diagnosis and disease activity assessment. J Am Coll Cardiol. 2011;58:1231–7. doi: 10.1016/j.jacc.2011.05.046. [DOI] [PubMed] [Google Scholar]
- 76.Nihei T, Takahashi J, Tsuburaya R et al. Circadian variation of Rho-kinase activity in circulating leukocytes of patients with vasospastic angina. Circ J. 2014;78:1183–90. doi: 10.1253/circj.cj-13-1458. [DOI] [PubMed] [Google Scholar]
- 77.Hizume T, Morikawa K, Takaki A et al. Sustained elevation of serum cortisol level causes sensitization of coronary vasoconstricting responses in pigs in vivo: a possible link between stress and coronary vasospasm. Circ Res. 2006;99:767–75. doi: 10.1161/01.RES.0000244093.69985.2f. [DOI] [PubMed] [Google Scholar]
- 78.Nihei T, Takahashi J, Kikuchi Y et al. Enhanced Rho-kinase activity in patients with vasospastic angina after the Great East Japan Earthquake. Circ J. 2012;76:2892–4. doi: 10.1253/circj.cj-12-1238. [DOI] [PubMed] [Google Scholar]
- 79.Nihei T, Takahashi J, Hao K et al. Prognostic impacts of Rho-kinase activity in circulating leucocytes in patients with vasospastic angina. Eur Heart J. 2018;39:952–9. doi: 10.1093/eurheartj/ehx657. [DOI] [PubMed] [Google Scholar]
- 80.Recio-Mayoral A, Rimoldi OE, Camici PG, Kaski JC. Inflammation and microvascular dysfunction in cardiac syndrome X patients without conventional risk factors for coronary artery disease. JACC Cardiovasc Imaging. 2013;6:660–7. doi: 10.1016/j.jcmg.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 81.Schroder J, Zethner-Moller R, Bove KB et al. Protein biomarkers and coronary microvascular dilatation assessed by rubidium-82 PET in women with angina pectoris and no obstructive coronary artery disease. Atherosclerosis. 2018;275:319–27. doi: 10.1016/j.atherosclerosis.2018.06.864. [DOI] [PubMed] [Google Scholar]
- 82.Odaka Y, Takahashi J, Tsuburaya R et al. Plasma concentration of serotonin is a novel biomarker for coronary microvascular dysfunction in patients with suspected angina and unobstructive coronary arteries. Eur Heart J. 2017;38:489–96. doi: 10.1093/eurheartj/ehw448. [DOI] [PubMed] [Google Scholar]


