Abstract
Exposure to metalworking fluid has been shown to cause health problems among workers. The aim of this study was to compare health outcomes and levels of exposure among workers exposed to metalworking fluid before and after the implementation of preventive measures. The frequencies of self-reported symptoms, as well as the concentrations of measured substances were lower after the implementation of preventive measures. Logistic regression showed statistically significant differences in the report of irritations, a stuffy or runny nose, eye irritation, a hoarse or dry throat, and a cough with odds ratios of 0.31 (95% confidence interval [CI] 0.21 to 0.47), 0.12 (95% CI 0.05 to 0.29), 0.13 (95% CI 0.06 to 0.28), and 0.24 (95% CI 0.12 to 0.46), respectively. This confirms the efficiency of the performed intervention and highlights the importance of eliminating the recirculation of contaminated air.
Keywords: airway symptoms, intervention study, metalworking fluid, occupational exposure, preventive measures
Metalworking fluid (MWF) is a solution commonly used in the metalworking industry. During metal processing, the fluid serves the purpose of cooling and lubricating the metal, as well as removing machine-generated metal chips. Furthermore, MWFs contain substances with the ability to prevent corrosion and other additives such as surfactants and biocides. There are different types of MWFs, which are divided into four major classes: straight (made up mostly of mineral or vegetable oils), soluble (with a high oil content emulsified in water), semisynthetic (with a lower oil content emulsified in water), and synthetic (containing detergent-like components and no oil).1
MWFs are often kept in central tanks and they are pumped from these between the machine and the tank in a closed recirculating system. When the machine is used, the MWF is applied by either a high-pressure beam, a fine beam, or by spraying the workpiece. During this process, aerosols of different sizes are generated, depending on the velocity of the machine, the composition of the MWF, and the pressure of the applied beam.2 A higher machine velocity generates greater emissions compared with a lower velocity and the amount of aerosol generated increases with the rotational speed of the machine.3
The presence of airway symptoms among those exposed to MWF has been analyzed in several studies. Eisen et al4 reported an increased risk of developing occupational asthma when exposed to MWF, especially synthetic fluids. In a Swedish study carried out at five different companies, the results showed a statistically significant association between wheezing and exposure to synthetic MWF. Similar outcomes were concluded in a Finnish study.5,6 Furthermore, coughing has been linked to exposure to MWF.7 There is also an association between nasal irritation and exposure to MWF and, in addition to airway symptoms, MWFs have been shown to cause occupational dermatoses.8–11
The composition of the MWF may change during the time of usage and microbial contamination and growth have been described, which can lead to the accumulation of allergens and toxins in the MWF.12,13 Traditionally, oil mist or airborne particles from the MWF have been measured to quantify the exposure to it in the workplace. However, several studies have shown that other irritants (eg, volatile organic compounds [VOC], formaldehyde, and ethanolamines) can be emitted into the air from the MWF.2,14–16 The Swedish Occupational Exposure Limit for MWF is 0.2 mg/m3.
A large metalworking factory in Sweden, with a history of skin problems among the workers exposed to MWF, decided to introduce oil mist separators into the machinery and switch metalworking fluid from mineral emulsion to semi-synthetic emulsion to improve air quality. Following the changes, the metalworking factory experienced an outbreak of airway symptoms among personnel working in the large processing hall were MWF was used. As a consequence, preventive actions were implemented to reduce the airway symptoms among personnel. In brief, the preventive actions included improvements of the general ventilation, no recirculation of air, increased influx of fresh air as well as introduction of door blocking to prevent personnel from entering the machines to soon and training on how to handle MWFs. The potential long-term effects of these preventive actions have not been evaluated.
The purpose of this study was to compare exposure and health outcomes before and after the implementation of preventive actions to reduce the exposure of metal workers to MWF at a large metalworking factory in Sweden.
METHOD
Study Design and Subjects
This intervention study was performed at a metalworking factory in Sweden where workers were exposed to MWF. The collection of data were conducted through measurements of exposure and questionnaires in 2006 and 2016. The company was selected due to an outbreak of airway symptoms reported by personnel following the introduction of oil mist separators in the machinery to improve air quality and switching the type of metalworking fluid from a mineral emulsion to a semi-synthetic emulsion. The reported symptoms ranged from irritated, stuffy and running nose, hoarse and dry throat, caught and also eye irritation, and some cases of adult asthma.
The air from the oil mist separators was let out into the factory and the regular ventilation system was assessed as insufficient to meet the factory's level of production. Smoke tests showed that air in the factory ceiling was transported over long distances from areas with a high machine density and polluted air was carried to other areas in the factory. Furthermore, a simulation showed that air exchange only occurred 2 m above ground level. Together, this led to the conclusion that the factory experienced problems regarding the recirculation of air. Prior to the changes described above, only a small number of workers reported health symptoms and these were mainly skin problems. The increase in airway symptoms reported by personnel not only occurred among those directly exposed to MWF (defined as those operating machines that used MWF) but also among workers who were indirectly exposed (defined as not operating machines that used MWF). Together, the directly and indirectly exposed workers constitute the study population of MWF-exposed workers defined as working in a processing hall were MWF was used.
In 2006, a standardized questionnaire (MM 040 NA) concerning the work environment, the indoor climate, and the health status of personnel (see Supplement 1) was sent out to all 460 workers.17 Exposure measurements were performed at the same time. The factory then implemented preventive measures to tackle exposure to MWF. Several preventive measures were introduced as advised by an occupational hygienist. A follow-up questionnaire was repeated in 2016 (446 workers) along with additional environmental exposure measurements.
Exposure Measurements
Stationary measurements of oil mist, dust, MWF, formaldehyde, ethanolamine, and volatile organic compounds (VOC), as well as personal measurements of formaldehyde were performed during two measuring campaigns with a 10-year interval. Both measuring campaigns were conducted over 2 days.
The first campaign has been described previously.11 In summary, morpholine and monoethanolamine were collected using acid-treated silica tubes and acid-treated glass fiber filters, which were analyzed by liquid chromatography with a mass selective detector. Dust and oil mist were collected on glass fiber filters, coupled and determined gravimetrically. Endotoxin was collected using polycarbonate filters and measured with a limulus amebocyte lysate test. Formaldehyde was sampled with UMEx 100 passive samplers and analyzed with liquid chromatography.
In the second campaign, personal measurements of formaldehyde were performed using Supelco DSD-DNPH passive sampling devices (Sigma-Aldrich, St. Louis, MO) during full working shifts (8 hours) and stationary sampling of aldehydes was performed using Waters Sep-Pak DNPH-Silica cartridges (Walters Corporation, Milford, MA) coupled to an AirCheck 2000 pump (SKC, Dorset, UK) with a flow rate of 2 L/min for 6 hours. Both the formaldehyde and aldehydes were analyzed using a high-performance liquid chromatography system (HPLC, G1311A, Agilent Technologies, Santa Clara, CA) coupled to an ultraviolet detector (G1315B, Agilent Technologies, Santa Clara, CA).
Volatile organic compounds (VOC) were collected using Tenax TA thermal desorption tubes (Markes International, Llantrisant, UK) coupled to an SKC PocketPump (SKC, Dorset, UK) with a flow rate of 0.2 L/min for 20 minutes. The VOC samples were then analyzed using automated thermal desorption (ATD, Thermal Desorber TD-100, Markes International, Llantrisant, UK) coupled with a gas chromatograph (GC, 7890B, Agilent Technologies, Santa Clara, CA) connected to a mass spectrometer (MS, 5977A, Agilent Technologies, Santa Clara, CA).
Ethanolamines were collected on acid-treated Whatman GF/B glass microfiber filters with a diameter of 25 mm (Cytiva, Malborough, MA) coupled to an AirCheck 2000 pump (SKC, Dorset, UK) with a flow rate of 2 L/min for 6 hours before they were analyzed using a UHPLC Accela 1250 with an Accela Autosampler and a TSQ Quantum Access MAX Triple Quadrupole Mass Spectrometer with a HESI-II detector (Thermo Fisher Scientific, Waltham, MA).
Oil mist and dust were collected on 25 mm Teflon filters (Pall Industries, New York, NY). The filters where then left for conditioning in a climate-controlled weighing room (20 ± 1 °C and RH% 40 ± 2%) for 48 hours before the collected mass was determined gravimetrically using a Mettler Toledo MX5 (Colombus, OH).
Preventive Measures
All preventive measures were proposed by an occupational hygienist and implemented between 2007 and 2012. These included improving the general ventilation by modernizing ventilation units with new control equipment, installing four large exhaust air fans in the factory ceiling and new process ventilation to all larger capsulated machines. All ventilated air was taken out of the factory and, to save energy, the recirculation of air was stopped. Air exhaust from oil mist separators was taken to the outside environment instead of back into the factory. Also, the influx of fresh air into the workplace was increased and the distribution of fresh air in the workplace was optimized to ensure air exchange at ground level. Furthermore, larger machines were provided with machine door blocking along with forced ventilation to prevent personnel from entering the machine before the MWF had been ventilated. Also, training on managing MWFs was implemented and is now given to all workers operating machines using MWFs.
Statistical Analysis
Demographic characteristics are presented descriptively with answering frequency. Exposure levels are also presented descriptively as mean values with minimum and maximum values. Answers from the questionnaire was classified as (1) “yes, often” and (0) “yes, sometimes” and “no”. Answers from the questionnaire regarding the indoor climate were presented as a rose diagram with a non-exposed reference group consisting of school and office personnel. Self-reported health data were analyzed using multiple logistic regression adjusted for the years worked at the current workplace as continuous variables and sex. Differences in groups regarding health outcomes are presented as odds ratios (OR) with a 95% confidence interval (CI). The statistical analysis was performed using IBM SPSS 25. A P-value of ≤0.05 was considered statistically significant.
Ethics
This project obtained ethical approval by the ethical board in Linköping, reference number M39–09. The collected data were anonymized.
RESULTS
Questionnaire
In 2006, the questionnaire was handed out to all factory workers, a total of 460 workers. This resulted in 351 answers and an answering frequency of 76%. Of these 351 answers, only workers who worked in production areas where MWF were used were included in the subsequent analysis (267 workers). In 2016, the questionnaire was handed out to a total of 446 workers. This resulted in 408 answers and an answer frequency of 91%. As in previous analysis, only workers in production areas where MWF were used were included (377 workers). The demographic characteristics of the study populations are presented in Table 1. There was limited internal dropout.
TABLE 1.
Demographic Characteristics of the Study Population in 2006 and 2016
| Demographics | 2006 (n = 267) | 2016 (n = 377) |
| Gender, n (%) | ||
| Male | 252 (94.7) | 360 (96.8) |
| Female | 14 (5.3) | 12 (3.2) |
| Age at survey, n (%) | ||
| ≤29 | 27 (10.2) | 63 (17.1) |
| 30–39 | 84 (31.6) | 54 (14.7) |
| 40–49 | 64 (24.1) | 132 (35.9) |
| 50–59 | 69 (25.9) | 85 (23.1) |
| ≥60 | 22 (8.3) | 34 (9.2) |
| Years at current workplace, n (%) | ||
| <1 | 16 (6.2) | 18 (4.9) |
| 1–5 | 93 (35.9) | 128 (35.0) |
| 6–10 | 83 (32.0) | 89 (24.3) |
| 11–15 | 17 (6.6) | 45 (12.3) |
| 16–20 | 20 (7.7) | 44 (12.0) |
| ≥21 | 30 (11.6) | 42 (11.5) |
| Smoker, n (%) | ||
| Yes | 39 (15.2) | 50 (13.8) |
| No | 217 (84.8) | 313 (86.2) |
Not all respondents answered all questions. n, number of individuals.
The two groups were similar in sex distribution with a high proportion of men in both 2006 and 2016. There was a difference in age distribution, with more workers aged 30 to 39 in 2006 and more workers aged 40 to 49 in 2016. The percentage of workers who smoked was similar in the two groups. The mean number of years at the current workplace was 8.9 and 10.3 in 2006 and 2016, respectively.
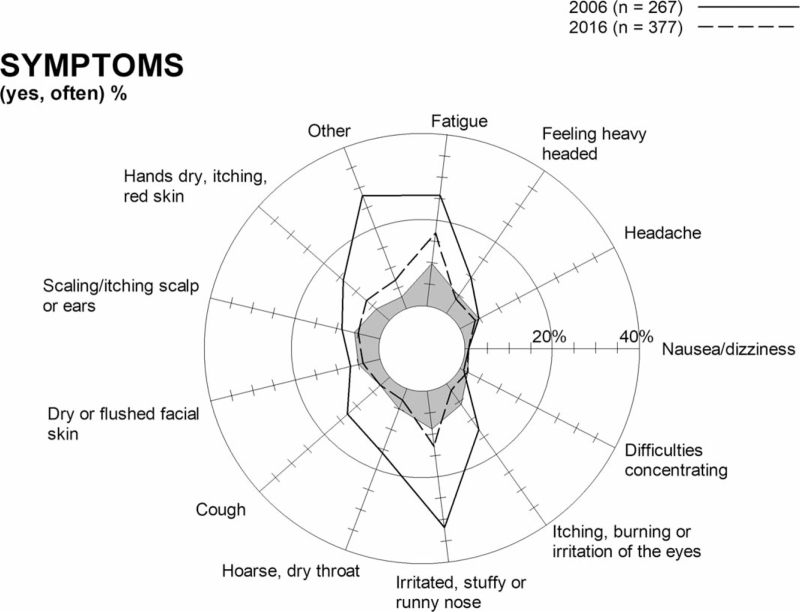
In 2006, the most frequent self-reported problems were airway symptoms, including an irritated, stuffy or runny nose, eye irritations, a hoarse or dry throat, and cough. Furthermore, problems regarding fatigue and dry, red, or itchy hands were also commonly reported. Table 2 shows that the frequency of self-reported symptoms in categories mentioned above were lower in 2016 compared with 2006. Logistic regression showed statistically significant differences in the reporting of an irritated, stuffy or runny nose, eye irritation, hoarse or dry throat, and cough with ORs of 0.31 (95% CI 0.21 to 0.47), 0.12 (95% CI 0.05 to 0.29), 0.13 (95% CI 0.06 to 0.28), and 0.24 (95% CI 0.12 to 0.46) respectively. Nausea or dizziness were reported by 1.1% of the workers in 2016 compared with 0.8% in 2006 with an OR of 1.43 (95% CI 0.26 to 7.86). However, the difference was not statistically significant. The frequency of reports regarding concentration difficulties was also higher in 2016, with an OR of 5.72 (95% CI 0.71 to 46.03). The difference was not statistically significant. Figure 1 illustrates the differences in the reporting of health symptoms in 2006 and 2016, including a reference group consisting of office and school personnel.
TABLE 2.
Health Outcomes and Symptoms Reported by Workers Exposed to Metalworking Fluids (MWFs) Before and After Reconstructions at the Workplace
| Simple Logistic Regression | Multiple Logistic Regressiona | |||||||||
| Health Problems | Year | Yes, Often (%) | B | Sig. | OR | 95% CI | B | Sig. | OR | 95% CI |
| Fatigue | 2006 | 66 (25.7) | 1 | |||||||
| 2016 | 63 (17.4) | –0.50 | 0.012∗ | 0.61 | 0.41–0.90 | –0.50 | 0.013∗ | 0.60 | 0.41–0.90 | |
| Heavy-headed feeling | 2006 | 26 (10.2) | 1 | |||||||
| 2016 | 16 (4.4) | –0.90 | 0.006∗ | 0.41 | 0.21–0.77 | –0.95 | 0.005∗ | 0.39 | 0.20–0.75 | |
| Headache | 2006 | 12 (4.7) | 1 | |||||||
| 2016 | 13 (3.6) | –0.28 | 0.499 | 0.76 | 0.34–1.69 | –0.31 | 0.447 | 0.73 | 0.33–1.64 | |
| Nausea or dizziness | 2006 | 2 (0.8) | 1 | |||||||
| 2016 | 4 (1.1) | 0.36 | 0.681 | 1.43 | 0.26–7.86 | 0.32 | 0.716 | 1.37 | 0.25–7.60 | |
| Difficulty concentrating | 2006 | 1 (0.4) | 1 | |||||||
| 2016 | 8 (2.2) | 1.74 | 0.101 | 5.72 | 0.71–46.03 | 1.75 | 0.101 | 5.73 | 0.71–46.19 | |
| Itching, burning or irritation of the eye | 2006 | 32 (12.5) | 1 | |||||||
| 2016 | 6 (1.7) | –2.12 | <0.001∗ | 0.12 | 0.05–0.29 | –2.14 | <0.001∗ | 0.12 | 0.05–0.29 | |
| Irritated, stuffy or runny nose | 2006 | 81 (31.5) | 1 | |||||||
| 2016 | 45 (12.5) | –1.17 | <0.001∗ | 0.31 | 0.21–0.47 | –1.15 | <0.001∗ | 0.32 | 0.21–0.48 | |
| Hoarse, dry throat | 2006 | 41 (16.1) | 1 | |||||||
| 2016 | 9 (2.5) | –2.01 | <0.001∗ | 0.13 | 0.06–0.28 | –2.01 | <0.001∗ | 0.13 | 0.06–0.28 | |
| Cough | 2006 | 33 (12.9) | 1 | |||||||
| 2016 | 12 (3.4) | –1.45 | <0.001∗ | 0.24 | 0.12–0.46 | –1.54 | <0.001∗ | 0.21 | 0.11–0.43 | |
| Dry or flushed facial skin | 2006 | 17 (6.6) | 1 | |||||||
| 2016 | 14 (3.9) | –0.55 | 0.138 | 0.58 | 0.28–1.19 | –0.61 | 0.109 | 0.54 | 0.26–1-15 | |
| Scaling or itching scalp | 2006 | 23 (8.9) | 1 | |||||||
| 2016 | 17 (4.7) | –0.68 | 0.041∗ | 0.51 | 0.27–0.97 | –0.73 | 0.033∗ | 0.48 | 0.25–0.94 | |
| Dry hands, itching or red skin | 2006 | 35 (13.6) | 1 | |||||||
| 2016 | 24 (6.7) | –0.79 | 0.005∗ | 0.45 | 0.26–0.78 | –0.76 | 0.007∗ | 0.47 | 0.27–0.82 | |
OR, odds ratio; CI, confidence interval.
Adjusted for number of years at the current workplace and gender.
Statistically significant.
FIGURE 1.
Frequencies of self-reported symptoms among workers exposed to metalworking fluid in 2006 (267 individuals) and 2016 (377 individuals) and a non-exposed reference group, consisting of office and school personnel represented by the grey area in the figure (4780 individuals).
When adjusted for years at the current workplace and sex, the results still showed a statistically significant difference in self-reported airway symptoms, as well as symptoms relating to fatigue and dry, itching or red skin of the hands.
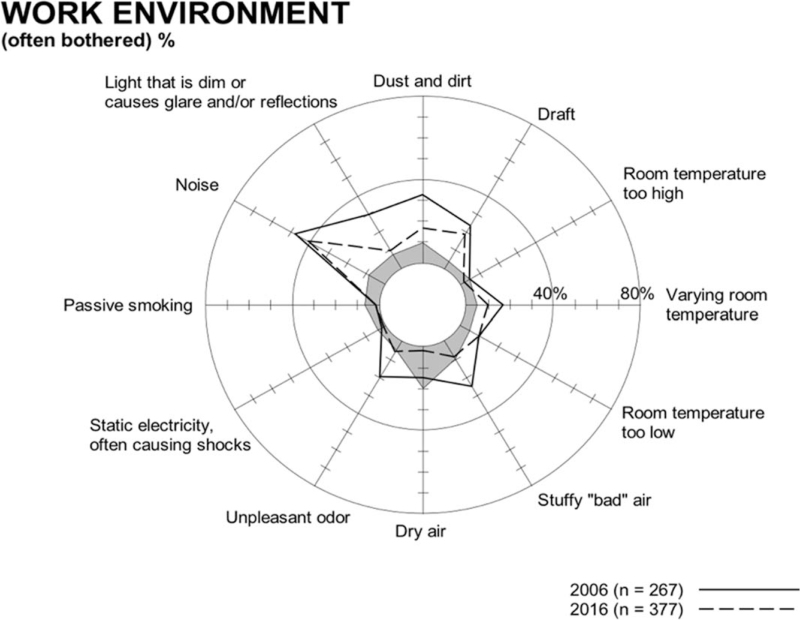
Figure 2 shows the frequency of reported complaints regarding the work environment among workers exposed to MWF. In 2006, the frequency of complaints regarding an unpleasant odor, dry air, stuffy or “bad” air, and dust and dirt were 20.3%, 14.9%, 25.3%, and 32.6%, respectively. In 2016, the report of these work environment factors was lower, with frequencies of 5.6%, 2.4%, 8.9%, and 17.2%, respectively.
FIGURE 2.
Frequencies of complaints regarding the work environment reported by workers exposed to metalworking fluid in 2006 (267 individuals), 2016 (377 individuals), and a non-exposed reference group consisting of office and school personnel represented by the grey area in the figure (4780 individuals).
Levels of Airborne Irritants
In 2016, lower levels of all measured substances generated by the MWF were found compared with 2006 (Table 3). In 2016, the levels of dust, oil mist, stationary formaldehyde, and formaldehyde carried by personnel were below the limit of detection (LOD) for analytic methods. The stationary measurement of VOC showed a total level of 140 μg/m3. No measurement of the levels of VOC was performed in 2006. The workers were not using respiratory protective equipment.
TABLE 3.
Average Indoor Concentrations (mg/m3) of Substances Generated by Metalworking Fluids (MWFs) Before and After Reconstructions at the Workplace
| 2006 | 2016 | |||
| Substance | N | Concentration, Mean (Min–Max) | n | Concentration, Max |
| Dust | 3 | 0.46 (0.14–0.94) | 4 | <0.20a |
| Oil mist | 4 | 0.46 (0.20–1.20) | 4 | <0.20a |
| Formaldehyde, stationary | 18 | 0.04 (0.02–0.08) | 5 | <0.01a |
| Formaldehyde, personnel | 4 | 0.1 (0.02–0.31) | 9 | <0.01a |
| Monoethanolamine | 4 | 0.05 (0.005–0.16) | 1 | 0.04b |
n, number of exposure measurements.
Only max values due to levels being below the limit of detection by analytical methods.
Only one value due to only one exposure measurement.
DISCUSSION
Exposure to MWF is a known contributor to negative health effects among personnel in the industry and preventive measures constitutes an efficient strategy to increase productivity and sustain or improve worker health. This intervention study demonstrates that the implemented preventive actions, such as modernizing ventilation and training of personnel in handling MWF, had a statistically significant effect on the frequency of health symptoms among workers exposed to MWF, as well as a lowering effect on the levels of substances generated by the MWF.
Prior to the performed intervention, the factory had problems with air being recirculated from the machine outlets to the indoor environment. The cutting machinery was equipped with oil mist separators to improve air quality. Since these types of separators only remove oil mist mechanically, they do not prevent gases or aerosols generated from the water-based MWF from spreading into the work environment. It is likely that this recirculation of air worsened the indoor working climate, resulting in the increase of reported airway symptoms among all workers in the processing hall.
The preventive measures in this study can be compared with the United States National Institute for Occupational Safety and Health (NIOSH) Hierarchy of Control, which is a control system to minimize exposure to occupational hazards. There are five steps ranging from the most effective measures to the least effective.18 By focusing on the ventilation of the factory and removing as much emissions from MWF as possible, the efforts can be equated with the third step, which is engineering controls, that is, isolating personnel from the hazard. As mentioned, the preventive measures taken in this study focused on factory ventilation mainly to correct the issues regarding the recirculation of air. This is in agreement with a study reviewing published outbreaks and clinical cases of hypersensitivity pneumonitis among workers exposed to MWF.19 The studies conclude that the extensive use of biocides and machine enclosures with delayed door opening are often insufficient to prevent exposure and that disease prevention should focus on the removing the recirculation of air. With the exception of ventilation, additional preventive measures were taken at the studied workplace. That included training in the management of MWF, which is equal to the fourth step (administrative controls), and delayed machine door opening, which is equal to the third step (engineering controls) in the NIOSH Hierarchy of Controls. In 2016, when the air from the oil mist separators along with the general ventilation was taken to the outside environment, our results show that the levels of measured substances decreased as shown in Table 3. Formaldehyde derives from the biocide in the MWF and was used as an indicator for the spread of MWF in the factory. In 2006, the mean levels of stationery and formaldehyde carried by personnel were 0.04 and 0.1 mg/m3, respectively. Although these levels were below the Swedish OEL of 0.37 mg/m3, they must be interpreted as if there was a spread of MWF in the factory. In 2016, the levels of formaldehyde were below the LOD for the analytical method, which demonstrates that the preventive actions were successful in reducing the spread of MWF. The measured stationery levels and levels of formaldehyde carried by personnel did not differ in 2016, which is likely to depend on the low exposure and the fact that the workers spend most of their work shift in the vicinity of the CNC-machines.
Prior to the intervention, in 2006, a large proportion of workers reported airway symptoms as shown in Table 1. Beside airway symptoms, skin problems were also common. In 2016, after the implementation of preventive measures, our results showed a statistically significant decrease in the report of both symptom categories, implying that the lower exposure levels had a clear effect on the workers’ health. Earlier studies have shown that symptoms among workers may be prevalent even at values below the exposure limits. Oudyk et al20 reported respiratory symptoms for operators exposed to MWF aerosols in the range of 0.25 to 0.84 mg/m3 and a large Finnish study suggested that exposure to aerosol concentrations above 0.17 mg/m3 was related to both upper and lower respiratory symptoms.6 A Swedish study performed in several machine shops showed that even though the mean exposure is low, specific tasks may result in high peak concentrations and, thereby, might play an important role in the development of airway symptoms.21 These findings are in line with the results in this study, with exposure levels below the OEL in both 2006 and 2016, which means that there is no distinct limit of MWF exposure where health problems could be avoided. To date, no single factor has been identified as the causative agent of the health problems associated with exposure to MWFs, but some argue that microbial contamination is important in the development of respiratory disease.22,23 With the above in mind, the current study shows that by keeping the MWF exposure to a minimum, health problems among workers could clearly decrease.
Although health symptoms among the personnel exposed to MWF has decreased, Table 2 shows that some workers still experience health problems after the performed intervention. When these frequencies are compared with those of a reference group consisting of personnel in an office and school environment (Fig. 1), the results show only a small difference, indicating that the factory work environment has clearly improved. However, in order to assure and maintain the health and well-being of the metal industry workers, it is important to keep monitoring exposure levels in the working environment and provide health monitoring for the personnel on a regular basis.
This study has some limitations. The symptoms reported from the workers at the metalworking factory have not been confirmed by medical examination by a physician. The answers in the questionnaire are thus the subjective experience of each worker's health. There is no follow up of workers who quit or changed workplace during the 10-year period in which this study was performed. Although the mean number of years at the current workplace among workers in 2016 was 10.3 years in this study, a healthy worker effect cannot be ruled out. Lastly, the regression models have not been adjusted for smoking, but the percentage of smokers seems to be stable during the study period (15.2% to 13.8%).
CONCLUSION
Prior to the performed intervention, each cutting machine was equipped with oil mist separators but there was no separation of aerosol or gas and the air was recirculated into the work environment. In 2016, all ventilation, including local exhaust from the cutting machines, was taken to the outside environment and the recirculation of air no longer occurred. The study demonstrated lower levels of MWF-derived substances in the work environment and a statistically significant decrease in self-reported health problems among MWF-exposed workers in 2016 compared with 2006. This confirms the efficiency of the performed intervention and highlights the importance of eliminating the recirculation of contaminated air. Future research should study the different components of MWF and aim to specify their role in disease pathology.
Supplementary Material
Footnotes
Clinical significance: This paper shows how preventive measures, that reduce the air concentrations of contaminants derived from the metal working fluids in the work environment, gives a significant decrease in self-reported health problems among exposed workers. This highlights the importance of eliminating the recirculation of contaminated air and reducing the workers exposure to air contaminants from metal working fluids.
Funding: This study was funded by the Research Council of South East Sweden (FORSS- 37321).
Declaration of interest: The authors declare that they have no conflict of interest, whether commercial or non-commercial. E.N. and H.J. work in companies that uses metalworking fluids in their production, but do not produce or sell metalworking fluids.
P.G. (the manuscript's guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported.
The Corresponding Author has the right to on behalf of all authors and does grant on behalf of all authors.
The study was approved by the ethical board in Linköping, reference number M39-09.
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (www.joem.org).
REFERENCES
- 1.Brinksmeier E, Meyer D, Huesmann-Cordes AG, Herrmann C. Metalworking fluids—mechanisms and performance. CIRP Annals 2015; 64:605–628. [Google Scholar]
- 2.Park D, Stewart PA, Coble JB. Determinants of exposure to metalworking fluid aerosols: a literature review and analysis of reported measurements. Ann Occup Hyg 2009; 53:271–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thornburg J, Leith D. Size distribution of mist generated during metal machining. Appl Occup Environ Hyg 2000; 15:618–628. [DOI] [PubMed] [Google Scholar]
- 4.Eisen EA, Holcroft CA, Greaves IA, Wegman DH, Woskie SR, Monson RR. A strategy to reduce healthy worker effect in a cross-sectional study of asthma and metalworking fluids. Am J Ind Med 1997; 31:671–677. [DOI] [PubMed] [Google Scholar]
- 5.Lillienberg L, Andersson EM, Jarvholm B, Toren K. Respiratory symptoms and exposure-response relations in workers exposed to metalworking fluid aerosols. Ann Occup Hyg 2010; 54:403–411. [DOI] [PubMed] [Google Scholar]
- 6.Jaakkola MS, Suuronen K, Luukkonen R, et al. Respiratory symptoms and conditions related to occupational exposures in machine shops. Scand J Work Environ Health 2009; 35:64–73. [DOI] [PubMed] [Google Scholar]
- 7.Massin N, Bohadana AB, Wild P, Goutet P, Kirstetter H, Toamain JP. Airway responsiveness, respiratory symptoms, and exposures to soluble oil mist in mechanical workers. Occup Environ Med 1996; 53:748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meza F, Chen L, Hudson N. Investigation of respiratory and dermal symptoms associated with metal working fluids at an aircraft engine manufacturing facility. Am J Ind Med 2013; 56:1394–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hannu T, Suuronen K, Aalto-Korte K, et al. Occupational respiratory and skin diseases among Finnish machinists: findings of a large clinical study. Int Arch Occup Environ Health 2013; 86:189–197. [DOI] [PubMed] [Google Scholar]
- 10.Nett RJ, Stanton M, Grimes GR. Occupational respiratory and skin diseases among workers exposed to metalworking fluids. Curr Opin Allergy Clin Immunol 2021; 21:121–127. [DOI] [PubMed] [Google Scholar]
- 11.Fornander L, Graff P, Wahlen K, et al. Airway symptoms and biological markers in nasal lavage fluid in subjects exposed to metalworking fluids. PLoS One 2013; 8:e83089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marchand G, Lavoie J, Racine L, et al. Evaluation of bacterial contamination and control methods in soluble metalworking fluids. J Occup Environ Hyg 2010; 7:358–366. [DOI] [PubMed] [Google Scholar]
- 13.Dilger S, Fluri A, Sonntag HG. Bacterial contamination of preserved and non-preserved metal working fluids. Int J Hyg Environ Health 2005; 208:467–476. [DOI] [PubMed] [Google Scholar]
- 14.Graff P, Elmsjo L, Bjorkander J, Flodin U. Occupational rhinitis caused by tolyltriazole in metalworking fluids. Scand J Work Environ Health 2008; 34:403–404. [DOI] [PubMed] [Google Scholar]
- 15.Suuronen K, Henriks-Eckerman ML, Riala R, Tuomi T. Respiratory exposure to components of water-miscible metalworking fluids. Ann Occup Hyg 2008; 52:607–614. [DOI] [PubMed] [Google Scholar]
- 16.Chen MR, Tsai PJ, Chang CC, Shih TS, Lee WJ, Liao PC. Particle size distributions of oil mists in workplace atmospheres and their exposure concentrations to workers in a fastener manufacturing industry. J Hazard Mater 2007; 146:393–398. [DOI] [PubMed] [Google Scholar]
- 17.Reijula K, Sundman-Digert C. Assessment of indoor air problems at work with a questionnaire. Occup Environ Med 2004; 61:33–38. [PMC free article] [PubMed] [Google Scholar]
- 18.IOSH. The State of the National Initiative on Prevention Through Design. Cincinnati, OH, U.S.: Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH); 2013. [Google Scholar]
- 19.Burge PS. Hypersensitivity pneumonitis due to metalworking fluid aerosols. Curr Allergy Asthma Rep 2016; 16:59. [DOI] [PubMed] [Google Scholar]
- 20.Oudyk J, Haines AT, D’Arcy J. Investigating respiratory responses to metalworking fluid exposure. Appl Occup Environ Hyg 2003; 18:939–946. [DOI] [PubMed] [Google Scholar]
- 21.Lillienberg L, Burdorf A, Mathiasson L, Thorneby L. Exposure to metalworking fluid aerosols and determinants of exposure. Ann Occup Hyg 2008; 52:597–605. [DOI] [PubMed] [Google Scholar]
- 22.Barber CM, Burton CM, Robinson E, Crook B, Evans G, Fishwick D. Hypersensitivity pneumonitis due to metalworking fluid exposures. Chest 2013; 143:1189. [DOI] [PubMed] [Google Scholar]
- 23.Tillie-Leblond I, Grenouillet F, Reboux G, et al. Hypersensitivity pneumonitis and metalworking fluids contaminated by mycobacteria. Eur Respir J 2011; 37:640–647. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.