PURPOSE
Patients with cancer experience high rates of morbidity and unplanned health care utilization and may benefit from new models of care. We evaluated an adult oncology hospital at home program's rate of unplanned hospitalizations and health care costs and secondarily, emergency department (ED) use, length of hospital stays, and intensive care unit (ICU) admissions during the 30 days after enrollment.
METHODS
We conducted a prospective, nonrandomized, real-world cohort comparison of 367 hospitalized patients with cancer—169 patients consecutively admitted after hospital discharge to Huntsman at Home (HH), a hospital-at-home program, compared with 198 usual care patients concurrently identified at hospital discharge. All patients met clinical criteria for HH admission, but those in usual care lived outside the HH service area. Primary outcomes were the number of unplanned hospitalizations and costs during the 30 days after enrollment. Secondary outcomes included length of hospital stays, ICU admissions, and ED visits during the 30 days after enrollment.
RESULTS
Groups were comparable except that more women received HH care. In propensity-weighted analyses, the odds of unplanned hospitalizations was reduced in the HH group by 55% (odds ratio, 0.45, 95% CI, 0.29 to 0.70; P < .001) and health care costs were 47% lower (mean cost ratio, 0.53; 95% CI, 0.39 to 0.72; P < .001) over the 30-day period. Secondary outcomes also favored HH. Total hospital stay days were reduced by 1.1 days (P = .004) and ED visits were reduced by 45% (odds ratio, 0.55; 95% CI, 0.33 to 0.92; P = .022). There was no evidence of a difference in ICU admissions (P = .972).
CONCLUSION
This oncology hospital at home program shows initial promise as a model for oncology care that may lower unplanned health care utilization and health care costs.
INTRODUCTION
Cancer and its associated morbidity ranks among the top reasons for health care utilization in the United States.1,2 Although cancer treatment is largely provided in the ambulatory setting, unplanned hospitalizations and emergency department (ED) visits are common, particularly for symptoms and toxicities such as pain, dehydration, and neutropenic fever, and contribute to substantial costs.3-5 Patients residing at home between treatment and clinic visits experience these distressing symptoms, toxicities, and disease progression that affect their quality of life and result in high rates of unplanned health care utilization.6-9
CONTEXT
Key Objective
There are few models of cancer care delivery in the home, yet patients with cancer frequently experience acute episodes of illness at home related to cancer treatment or disease progression. These result in emergency department visits and unplanned hospitalizations. This evaluation examined the hospital-at-home model of acute-level care in the home for patients with cancer on subsequent 30-day health care utilization and secondarily costs.
Knowledge Generated
Health care utilization and costs were markedly decreased for those in the Huntsman at Home program in comparison with a usual care cohort who did not receive hospital-at-home services.
Relevance
A hospital-at-home model of acute care shows promise for reducing unplanned health care utilization and costs in cancer care delivery. This evaluation supports further consideration and study of this innovative model of care for oncology.
There are few models of care that address the home support needs of patients with cancer or provide alternatives to ED use and readmission for unresolved and emergent symptoms and acute toxicities. Patients with cancer may benefit from additional approaches to care in the home, especially when acute-level monitoring and services are needed to resolve symptoms and toxicities. The hospital-at-home model of care is an approach that has demonstrated efficacy in nononcology populations.10-15 There is increasing interest in evaluating this model in adult oncology patients.16
As the name suggests, hospital-at-home programs bring hospital-level care to the home. These programs have primarily focused on care for pneumonia, cellulitis, urinary tract infections, and exacerbations of chronic diseases such as chronic obstructive pulmonary disease or heart failure.10-15 It is more commonly found in single-payer health systems such as the United Kingdom, Spain, and Australia. The earliest roots for hospital at home in the United States focused on gerontology.10,11 However, these programs have not been widely integrated into US health care, primarily because reimbursement models do not adequately compensate for intensive home-based care that would otherwise require hospitalization.
Hospital at home is a promising model that could improve outcomes and add value for oncology patients.16 Such programs could keep patients at home, provide services that would otherwise require hospitalization, and better control symptom fluctuations while protecting immunosuppressed and frail patients with cancer from exposure to hospital-acquired bacterial and viral infections. Such programs also have the potential to reduce costs. Although there are limited trials and variability in models studied, hospital-at-home programs outside of oncology have demonstrated safety, reduced rates of hospitalizations and ED use, and reduced costs.14,17 The purpose of this work is to prospectively evaluate whether a novel oncology hospital at home program reduces unplanned hospitalizations and health care costs in the 30 days after enrollment. To ensure that any observed benefits in these outcomes do not contribute to increases in utilization of other health care services, we also evaluated the program's impact on ED and intensive care unit (ICU) admissions and the overall length of hospitalizations.
METHODS
We conducted, to our knowledge, the first prospective evaluation of an adult oncology hospital at home program in the United States, Huntsman at Home (HH). The design was a nonrandomized, prospective cohort comparison of patients enrolled in HH or a usual care (UC) comparison group from August 2018 through October 2019. For the binary end point, any unplanned hospitalization over the 30 days after discharge, effective sample sizes of 120 per group ensured > 80% power for odds ratios (ORs) < 0.45 for an underlying overall rate of unplanned hospitalization of approximately 30%. The Protocol (online only) was submitted to the University of Utah Institutional Review Board and deemed a quality improvement project.
Participant Selection
We prospectively enrolled consecutive patients 18 years or older with cancer who were admitted by inpatient hospitalists' referral to HH after hospitalization. To be eligible for HH program admission, patients had to reside in a 20-mile geographic service area of the Huntsman Cancer Institute (HCI), an NCI-designated comprehensive cancer center located in Salt Lake City, Utah, and along the metropolitan Wasatch Front. The comparison group was identified concurrently from patients who qualified for HH admission but were found to live outside the HH geographic service area but within the metropolitan Wasatch Front or lived within the HH service area and were offered HH admission but declined. UC patients were included if they discharged to a residence and were excluded if they were transferred to a care facility such as a rehabilitation center or skilled nursing facility.
Intervention
The HH program began service in 2018 for patients with cancer who had acute medical or postsurgical care needs at home. Patients were admitted who required continued acute-level medical care after hospitalization or who had continuing unstable symptoms related to treatment or disease progression that would otherwise require ED evaluation or further hospitalization. The acuity level and need for frequent monitoring and acute visits was judged by the referring clinicians to be beyond traditional episodic home health services. For this evaluation, referral was made by the hospitalist team during a hospitalization at the Huntsman Cancer Hospital. Common admission diagnoses were dehydration, electrolyte disorders, neutropenic fever, infection, uncontrolled pain, other symptom disorders, respiratory distress, failure to thrive, and small-bowel obstruction. Services depended upon patient condition and could include acute symptom management; clinical monitoring of cardiovascular parameters and oxygen therapy; laboratory value monitoring and replacement; medication titration; and intravenous administration of fluids, antibiotics, and other intravenous medications. Chemotherapy or other anticancer infusions were not a provided service. Visits were determined by need and typically included three nurse practitioner (NP) and five registered nurse (RN) visits during the initial week and occasionally required several RN visits per day along with daily NP visits. Because current payer reimbursement for home care services is inadequate to fully cover costs of acute-level care at home, the HCI covered unreimbursed costs so a full evaluation of the program could be conducted. Care was provided by a team of HCI-employed NPs in partnership with RNs from a not-for-profit home health agency. The HH Medical Director had both medical oncology and palliative care board certifications and provided medical oversight along with a part-time palliative care physician. HH NPs also worked directly with the patient's oncologist to coordinate care needs. Other services such as social work and physical therapy were used as needed.
Data Collection
Patients were enrolled when identified as clinically eligible during hospitalization. The 30-day observation period began at discharge. Outcome measures included cumulative unplanned hospitalizations, costs, length of hospital stays (LOS), ICU admissions, and ED visits over the 30-day period after enrollment to HH or comparison group. These data, along with patient demographics and disease characteristics, were captured in the electronic health record and extracted from the University of Utah's Electronic Data Warehouse for analysis, augmented by manual cross-validated data checks. Billed charges were converted to costs using the 2015 hospital-level cost-to-charge ratio for University of Utah Health.18 Potential unplanned health care utilization from other health care systems was not retrievable, and costs for at-home services were not accessible for UC patients and only included NP visits for HH patients.
Statistical Analysis
Patient characteristics at enrollment and health care utilization during the 30 days prior to enrollment were summarized overall and within each group as number (percent) and mean (standard deviation), respectively, for categorical and quantitative variables. These characteristics were compared between groups through chi-squared or t tests, as appropriate. Probability of enrollment in HH propensity scores was constructed using a random forest19 on the basis of patient characteristics at enrollment—age; race; sex; stage; cancer site; presence of brain, lung, or liver metastases; Charlson Comorbidity Index; census tract–level median income; number of hospitalizations; LOS; number of ED visits; and total costs during the 30 days prior to enrollment, as well as date of enrollment.
The primary comparative effectiveness of utilization outcomes during the 30 days after enrollment was based on models inversely weighted by HH versus UC propensity score, with patient-wise bootstrap standard errors.20 Inverse propensity-weighted linear and logistic generalized linear models were used, respectively, for length of stay and binary outcomes. Balance of the groups on the potential confounders included in the propensity model (listed above) was assessed after weighting via weighted chi-squared or t tests, as appropriate. Potential confounders that did not show adequate balance between groups after propensity weighting (P < .05) were included as covariates in the primary outcome comparison models.21 Costs were compared in the context of inverse propensity-weighted two-part binomial and gamma model, respectively, for nonzero costs and total costs given that costs were nonzero to accommodate the zero-inflated costs end point.22 Model fit of the gamma component of the cost model was assessed with Park's test.23 For ease of interpretation, we report the percent reduction in costs and the absolute reduction in costs for the combined two-part costs model.
RESULTS
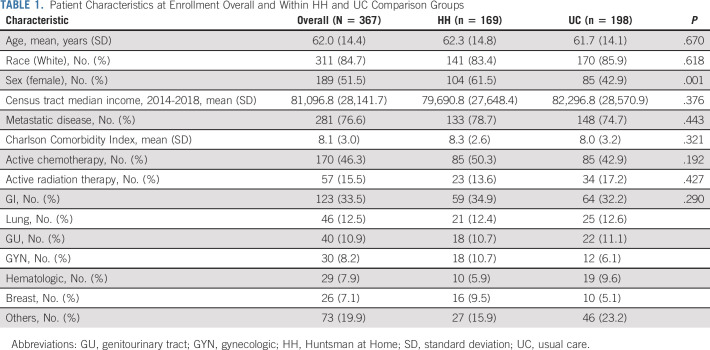
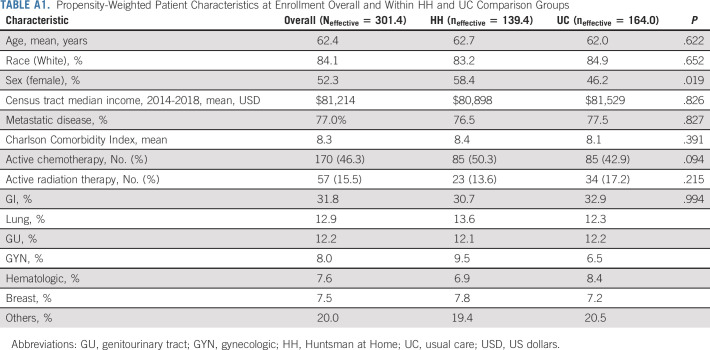
Of the 367 patients, 169 were in HH and 198 were in the UC comparison group. The average age was 62 years, 85% were White, and 77% had stage IV cancer. A variety of malignancies were represented, with the following most common malignancy types: colon, pancreas, gynecologic, prostate, and lung cancer. Seventeen patients (9%) who were offered HH admission, declined that admission. Three did not want providers visiting their homes, and 14 had a relationship with another home health agency and did not want to switch. Before propensity weighting, HH patients were more likely to be female (62% v 43%) and have a longer hospital LOS in the 30 days prior to HH admission (7.3 v 5.5 days) when compared with UC. Groups did not show evidence of differences on disease stage, number receiving active treatment, or census tract–level median income. Table 1 summarizes the patient characteristics overall and for each group, whereas Appendix Table A1 (online only) summarizes patient characteristics after propensity weighting, including effective sample sizes overall and within groups.24 After propensity weighting, sex showed some residual imbalance between the groups (weighted rate of female sex 58% in HH v 46% in UC, P = .019; Appendix Table A1) and was included as an adjustment variable in the primary end point comparison models. After propensity weighting, there were no other statistically significant differences in patient characteristics at enrollment in the prior 30 days and date of enrollment between the groups (all P > .05). Park's test did not indicate a lack of fit of the Gamma model for nonzero costs (P = .92).
TABLE 1.
Patient Characteristics at Enrollment Overall and Within HH and UC Comparison Groups
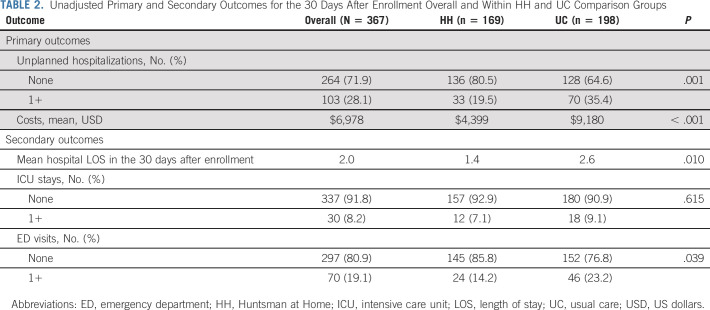
Unadjusted comparisons of the primary and secondary outcomes (Table 2) during the 30 days after admission demonstrated that HH patients had significantly fewer unplanned hospitalizations (≥ 1 hospitalization; 19.5% v 35.4%; P = .001) and mean costs ($4,399 v $9,180 US dollars [USD]; P < .001). Secondary outcomes favored HH with fewer cumulative days of hospitalization (1.4 v 2.6 days; P = .010) and fewer ED visits (≥ 1 visit; 14.2% v 23.2%; P = .039) There was no evidence of a difference in ICU admissions (≥ 1 admission; 7.1% v 9.1%; P = .615).
TABLE 2.
Unadjusted Primary and Secondary Outcomes for the 30 Days After Enrollment Overall and Within HH and UC Comparison Groups
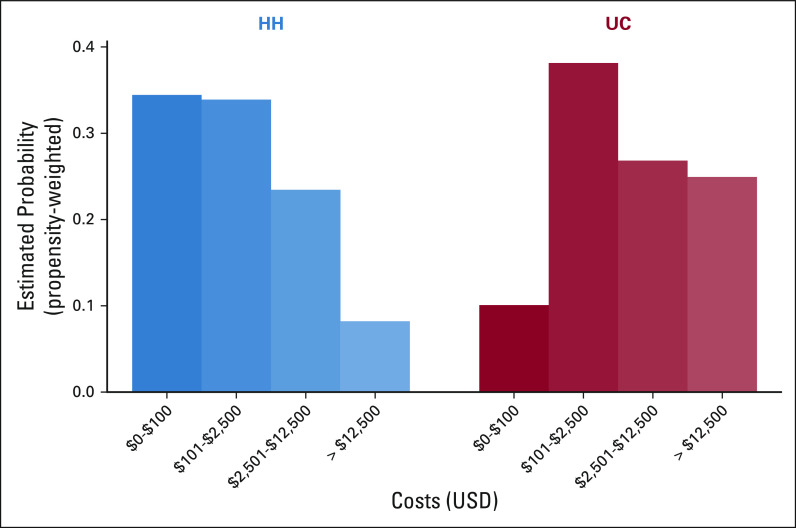
The primary and secondary outcomes analyses on the basis of propensity-weighted modeling (Table 3 and Fig 1) had similarly favorable results for HH, suggesting a 55% reduction in odds of unplanned hospitalizations (OR, 0.45; 95% CI, 0.29 to 0.70; P < .001) and a 47% reduction in costs (mean cost ratio, 0.53; 95% CI, 0.39 to 0.72; P < .001) during the first 30 days after enrollment when compared with UC. The 47% reduction in costs corresponded to an average absolute reduction in costs of $4,315 USD (95% CI, $3,580 to $6,610 USD). Notably, the primary comparisons of costs are reported in a 50% female, 50% male counter-factual population. Propensity-weighted secondary outcome comparisons suggested a 1.13-day reduction in days of hospitalization (95% CI, 0.37 to 1.89; P = .004) and a 45% reduction in odds of ED visits (OR, 0.55; 95% CI, 0.33 to 0.92; P = .022). There was no evidence of a difference in ICU admissions (P = .972).
TABLE 3.
Propensity-Weighted Comparisons of Primary and Secondary Outcomes for the 30 Days After Enrollment (HH Relative to UC)
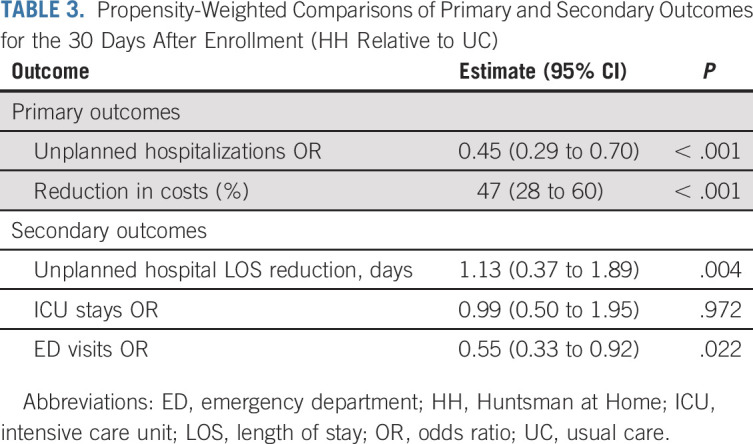
FIG 1.
Propensity-weighted estimates of the distributions of costs during the 30 days after enrollment for HH and UC. HH, Huntsman at Home; UC, usual care; USD, US dollars.
DISCUSSION
The HH intervention was associated with reductions in unplanned hospitalizations and health care costs in comparison with UC. In addition, other measures of health care utilization including shorter hospital LOS and fewer ED visits support evidence of benefit for HH. During the course of cancer treatment, many patients require acute-level care to manage disease and treatment-associated morbidity.25 These unaddressed needs may be prevented or reduced by an oncology hospital at home program that may lower the cost of care and reduce pressure on hospital bed capacity and ED use, all while minimizing exposure of high-risk patients to potential harms associated with inpatient care and ED visits.
HH patients experienced substantially fewer hospitalizations than UC (OR, 0.45) and had fewer hospital stay days (1.13 day mean reduction). Despite lower use of inpatient services, HH was also associated with reduced ED visits (OR, 0.55). The program significantly reduced pressure on bed capacity at the Huntsman Cancer Hospital and pressure on the University Hospital ED, both of which facilities regularly operate at capacity.
These findings of fewer hospitalizations and shorter hospital stays for HH patients may be underestimates of the true benefit of HH because of limitations in the nonrandomized design. Although we sought to identify a comparable comparison group and used advanced statistical approaches to account for between-group differences, some HH patients likely had higher acuity at study entry since hospitalists knew patients could be discharged and receive acute-level monitoring and services at home. In contrast, some UC patients may have had longer hospitalizations to stabilize. This difference biases results to the null for HH, suggesting there may be greater benefit in preventing readmission, which could be better addressed in a randomized trial.
Our study reinforces the results published in previous studies on hospital-at-home care for a range of health conditions other than oncology.11,12,14,15,17,26 To our knowledge, this is the first report of results for an adult oncology hospital at home program in the United States and demonstrates initial evidence of improved outcomes and benefits broadly for oncology populations. Programs that show promise to half the standard hospitalization and ED use rate offer transformative approaches to cancer care.
HH was not associated with a greater need for ICU admissions. ICU-level care is not appropriate for hospital-at-home services. This finding is reassuring as it suggests patients receiving hospital-level care at home received appropriate escalation in care when needed. Similarly, there were lower, not higher, rates of hospitalization and ED visits suggesting that HH staff did not need to escalate back to hospital or ED in comparison with standard care and HH patients received acute-level care safely at home.
The HH model involved NP and RN home visit teams backed by both oncology and palliative care physician expertise in addition to the patient's primary oncology team guidance. Other nononcology hospital at home models have used physician and RN home visit teams.15,17,26 The HH oncology model provider mix was shown to be a promising delivery model and could be considered in staffing oncology models moving forward.
Cost is an important issue for new care models. HH patients had half (53%) the costs in the 30 days after enrollment in comparison with UC. However, full HH costs were not included as only NP-billed charges were obtained and no UC home health costs. Our results are similar to or better than those reported by US nononcology hospital at home programs.15,17,26 Currently, traditional fee-for-service home health payment models do not adequately reimburse hospital-at-home services. In November 2020, because of the COVID-19 pandemic, Medicare issued a temporary Public Health Emergency Centers for Medicare & Medicaid Services waiver27 that allows hospital-level reimbursement for acute hospital-at-home care. This may provide additional experience to the current evidence that these programs result in equal or better care outcomes, improved patient satisfaction, and lower cost and may lead to sustainable payment models.10,11,14,15,17,26
On the basis of our initial evaluation, further study of oncology hospital at home programs is warranted to evaluate efficacy, full cost, and the optimal combination of services that add value in oncology care. Our evaluation focused on acute-level oncology hospital at home services after hospitalization. We have admitted patients from clinic referral but these patients were not included in this analysis. In the next year, HH will begin an expansion, accepting admissions directly from an ED visit and extending the program to three rural communities located 2 to 4 hours from HCI using a combination of telehealth, remote technologies, and on-ground care.
Our study has several limitations. Although we used a prospective design with a concurrent comparison cohort and propensity score balancing, we did not use a randomized design. Instead we used real-world evidence to broadly evaluate initial outcomes.28-30 For this nonrandomized design, the primary comparisons may be subject to some degree of unmeasured confounding, where groups differed in some unknown manner that is associated with utilization and cost outcomes. However, given the large magnitude of estimated effects, their consistency across propensity-weighted and unadjusted models, and the relatively large number of potential confounders considered, a complete removal or reversal of outcome differences resulting from unmeasured confounding is unlikely.31 Because of lack of adequate reimbursement, hospital-at-home programs are difficult to scale and evaluate, so determining an effect in real-world oncology practice rather than a highly controlled randomized design provides relevant information for payers and policy makers.32
In other limitations, our estimation of costs was based on a health system–level cost-to-charge ratio that could be imprecise. We did not capture the costs of all at-home services regardless of group or whether there was unplanned health care utilization from other health systems.
Missing data were very minimal, and manual chart review and verification were used for uncertain data elements. However, as discussed, unplanned health care utilization and costs outside of the University Health System were not captured. The evaluation is also from one oncology hospital at home program from a single cancer center. Other oncology hospital at home programs would need to be developed and operationalized to pursue multisite evaluation.
Finally, although participants represented multiple cancers and acute needs, there was limited ethnic, racial, and geographic diversity. We also did not capture the patient experience or collect patient-reported outcomes. Referral was limited to inpatient stays and did not capture the potential benefit of intake from the ED, clinics, and enrollment of patients from distant rural communities.
In conclusion, oncology hospital at home shows promise for provision of acute-level care to patients at home while simultaneously improving value and reserving inpatient beds and ED services for critically ill patients. Significant improvements in health care utilization may be achievable through oncology hospital at home programs. These benefits will only be realized if new payment models recognize the value of providing cancer care at home.
Appendix
TABLE A1.
Propensity-Weighted Patient Characteristics at Enrollment Overall and Within HH and UC Comparison Groups
Kathi Mooney
Consulting or Advisory Role: Cognitive Medical System
Patents, Royalties, Other Intellectual Property: Intellectual property disclosed to the University of Utah for the development of Symptom Care at Home, a remote symptom-monitoring platform developed through research grants funded by NCI. No royalties have been received to date.
Benjamin Haaland
Consulting or Advisory Role: Prometic Life Sciences, Value Analytics Labs, AstraZeneca, National Kidney Foundation
Travel, Accommodations, Expenses: Flatiron Health
Lorinda A. Coombs
Consulting or Advisory Role: Alexion Pharmaceuticals
Speakers' Bureau: Sanofi
Travel, Accommodations, Expenses: Alexion Pharmaceuticals
Anne C. Kirchhoff
Stock and Other Ownership Interests: Medtronic
John H. Ward
Honoraria: Myriad Genetics
Consulting or Advisory Role: Myriad Genetics
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented at the ASCO 2020 Virtual Annual Meeting, May 29-June 1, 2020.
SUPPORT
Supported by Cambia Health Foundation grant.
AUTHOR CONTRIBUTIONS
Conception and design: Kathi Mooney, Karen Titchener, Benjamin Haaland, Brock O'Neil, Richard Nelson, Jordan P. McPherson, Anna C. Beck, John H. Ward
Provision of study materials or patients: Anna C. Beck
Collection and assembly of data: Kathi Mooney, Karen Titchener, Benjamin Haaland, Lorinda A. Coombs, Brock O'Neil, Richard Nelson, Jordan P. McPherson
Data analysis and interpretation: Kathi Mooney, Benjamin Haaland, Lorinda A. Coombs, Brock O'Neil, Richard Nelson, Jordan P. McPherson, Anne C. Kirchhoff, John H. Ward
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Evaluation of Oncology Hospital at Home: Unplanned Health Care Utilization and Costs in the Huntsman at Home Real-World Trial
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Kathi Mooney
Consulting or Advisory Role: Cognitive Medical System
Patents, Royalties, Other Intellectual Property: Intellectual property disclosed to the University of Utah for the development of Symptom Care at Home, a remote symptom-monitoring platform developed through research grants funded by NCI. No royalties have been received to date.
Benjamin Haaland
Consulting or Advisory Role: Prometic Life Sciences, Value Analytics Labs, AstraZeneca, National Kidney Foundation
Travel, Accommodations, Expenses: Flatiron Health
Lorinda A. Coombs
Consulting or Advisory Role: Alexion Pharmaceuticals
Speakers' Bureau: Sanofi
Travel, Accommodations, Expenses: Alexion Pharmaceuticals
Anne C. Kirchhoff
Stock and Other Ownership Interests: Medtronic
John H. Ward
Honoraria: Myriad Genetics
Consulting or Advisory Role: Myriad Genetics
No other potential conflicts of interest were reported.
REFERENCES
- 1.Park J, Look KA: Health care expenditure burden of cancer care in the United States. Inquiry 56:46958019880696, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Narang AK, Nicholas LH: Out-of-pocket spending and financial burden among Medicare beneficiaries with cancer. JAMA Oncol 3:757-765, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siefert ML, Bonquist TM, Berry DL, et al. : Symptom-related emergency department visits and hospital admissions during ambulatory cancer treatment. J Community Support Oncol 13:188-194, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Numico G, Cristofano A, Mozzicafreddo A, et al. : Hospital admission of cancer patients: Avoidable practice or necessary care? PLoS One 10:e0120827, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Handley NR, Schuchter LM, Bekelman JE: Best practices for reducing unplanned acute care for patients with cancer. JCO Oncol Pract 14:306-313, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nipp RD, El-Jawahri A, Moran SM, et al. : The relationship between physical and psychological symptoms and health care utilization in hospitalized patients with advanced cancer. Cancer 123:4720-4727, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panattoni L, Fedorenko C, Greenwood-Hickman MA, et al. : Characterizing potentially preventable cancer- and chronic disease-related emergency department use in the year after treatment initiation: A regional study. JCO Oncol Pract 14:e176-e185, 2018 [DOI] [PubMed] [Google Scholar]
- 8.Whitney RL, Bell JF, Tancredi DJ, et al. : Hospitalization rates and predictors of rehospitalization among individuals with advanced cancer in the year after diagnosis. J Clin Oncol 35:3610-3617, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Z, Yang R, Kwak MJ, et al. : Oncologic emergencies in a cancer center emergency department and in general emergency departments countywide and nationwide. PLoS One 13:e0191658, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leff B, Burton L, Mader S, et al. : Satisfaction with hospital at home care. J Am Geriatr Soc 54:1355-1363, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Leff B, Burton L, Mader SL, et al. : Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med 143:798-808, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Montalto M: The 500-bed hospital that isn't there: The Victorian Department of Health Review of the Hospital in the Home program. Med J Aust 193:598-601, 2010 [DOI] [PubMed] [Google Scholar]
- 13.Lee GA, Titchener K: The Guy's and St Thomas's NHS Foundation Trust @home service: An overview of a new service. Lond J Prim Care (Abingdon) 9:18-22, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Federman AD, Soones T, DeCherrie LV, et al. : Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med 178:1033-1040, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levine DM, Ouchi K, Blanchfield B, et al. : Hospital-level care at home for acutely ill adults: A pilot randomized controlled trial. J Gen Intern Med 33:729-736, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Handley NR, Bekelman JE: The oncology hospital at home. J Clin Oncol 37:448-452, 2019 [DOI] [PubMed] [Google Scholar]
- 17.Levine DM, Ouchi K, Blanchfield B, et al. : Hospital-level care at home for acutely ill adults: A randomized controlled trial. Ann Intern Med 172:77-85, 2020 [DOI] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services : Hospital Cost Report Public Use File 2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Cost-Report/HospitalCostPUF [Google Scholar]
- 19.Breiman L: Random forests. Machine Learn 45:27, 2001 [Google Scholar]
- 20.Lunceford JK, Davidian M: Stratification and weighting via the propensity score in estimation of causal treatment effects: A comparative study. Stat Med 23:2937-2960, 2004 [DOI] [PubMed] [Google Scholar]
- 21.Nguyen T-L, Collins GS, Spence J, et al. : Double-adjustment in propensity score matching analysis: Choosing a threshold for considering residual imbalance. BMC Med Res Methodol 17:78, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diehr P, Yanez D, Ash A, et al. : Methods for analyzing health care utilization and costs. Annu Rev Public Health 20:125-144, 1999 [DOI] [PubMed] [Google Scholar]
- 23.Park RE: Estimation with heteroscedastic error terms. Econometrica 34:888, 1966 [Google Scholar]
- 24.Wiegand H, Kish L: Survey sampling. John Wiley & Sons, Inc., New York, London 1965, IX + 643 S., 31 Abb., 56 Tab., preis 83 s. Biometrische Zeitschrift 10:88-89, 1968 [Google Scholar]
- 25.Young A, Marshall E, Krzyzanowska M, et al. : Responding to acute care needs of patients with cancer: Recent trends across continents. Oncologist 21:301-307, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cryer L, Shannon SB, Van Amsterdam M, et al. : Costs for 'hospital at home' patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood) 31:1237-1243, 2012 [DOI] [PubMed] [Google Scholar]
- 27.Centers for Medicare & Medicaid Services : CMS announces comprehensive strategy to enhance hospital capacity amid COVID-19 surge. November 25, 2020. https://www.cms.gov/newsroom/press-releases/cms-announces-comprehensive-strategy-enhance-hospital-capacity-amid-covid-19-surge [Google Scholar]
- 28.De Lusignan S, Crawford L: Creating and using real-world evidence to answer questions about clinical effectiveness. J Innov Health Inform 22:368-373, 2015 [DOI] [PubMed] [Google Scholar]
- 29.Kamal AH, Krzyzanowska MK: Real-world approaches to quality improvement in oncology. JCO Oncol Pract 14:757-759, 2018 [DOI] [PubMed] [Google Scholar]
- 30.Sherman RE, Anderson SA, Dal Pan GJ, et al. : Real-world evidence—What is it and what can it tell us. N Engl J Med 375:2293-2297, 2016 [DOI] [PubMed] [Google Scholar]
- 31.Vanderweele TJ, Arah OA: Bias formulas for sensitivity analysis of unmeasured confounding for general outcomes, treatments, and confounders. Epidemiology 22:42-52, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garrison LP Jr, Neumann PJ, Erickson P, et al. : Using real‐world data for coverage and payment decisions: The ISPOR real‐world data task force report. Value health 10:326-335, 2007 [DOI] [PubMed] [Google Scholar]