Abstract
Background: The effects of ethnic and social inequalities on patient outcomes in acute healthcare remain poorly understood.
Methods: Prospectively-defined analysis of registry data from four acute NHS hospitals in east London including all patients ≥ 18 years with a first emergency admission between 1st January 2013 and 31st December 2018. We calculated adjusted one-year mortality risk using logistic regression. Results are presented as n (%), median (IQR), and odds ratios (OR) with 95% confidence intervals.
Findings: We included 203,182 patients. 43,101 (21%) patients described themselves as Asian, 21,388 (10.5%) Black, 2,982 (1.4%) Mixed, 13,946 (6.8%) Other ethnicity, and 100,065 (49%) White. We excluded 21,700 (10.7%) patients with undisclosed ethnicity. 16,054 (7.9%) patients died within one year. Non-white patients were younger (Asian: 43 [31–62] years; Black: 48 [33–63] years; Mixed 36 [26–52] years) than White patients (55 [35–75] years), with a higher incidence of comorbid disease. In each age-group, non-white patients were more likely to be admitted to hospital. This effect was greatest in the ≥ 80 years age-group (32% non-white admitted to hospital versus 23% non-white in community population). Deprivation was associated with increased mortality in all ethnic groups (OR 1.41 [1.33–1.50]; p < 0.001). However, when adjusted for age, Asian (0.69 [0.66–0.73], p < 0.0001) and Black patients (0.79 [0.74–0.85]; p < 0.0001) experienced a lower mortality risk than White patients.
Interpretation: Ethnic and social disparities are associated with important differences in acute health outcomes. However, these differences are masked by statistical adjustment because patients from ethnic minorities present at a younger age.
Funding: None
Research in context.
Evidence before this study
Health inequalities affecting minority ethnic people in the UK have been documented across the spectrum of healthcare including access to and uptake of services, and quality and experience of care with people of Black, Asian and other minority ethnic groups reporting worse general health and experiencing higher levels of significant comorbidity compared to the White British group. The COVID-19 pandemic has highlighted inequalities which reflect those consistently demonstrated across chronic conditions such as cardiovascular disease, diabetes, stroke, and hypertension including a disproportionate burden of disease incidence and mortality reported particularly in Black and Asian groups. However, evidence characterizing ethnic disparities in acute illness is limited and studies with sufficient sample size and adjustment for confounders are lacking.
Added value of this study
We carried out a comparative analysis in a non-COVID cohort to examine if these differences in outcomes across ethnic groups extend more generally across acute healthcare settings, including comparing a range of specific indications for emergency hospital admission from four hospitals over a six-year period. We found that patients from minority ethnic groups presented acutely to hospital at a younger age with a distinct and earlier onset burden of comorbid disease which could potentially drive need to access secondary healthcare for reasons less associated with short to medium-term risk of death. Accounting for all age groups, overall survival in the year following an acute hospital admission was better for patients of Black, Asian, and Mixed ethnicity even after adjustment for socioeconomic deprivation in contrast to the higher age-adjusted mortality seen recently in minority ethnic groups in COVID-19.
Implications of all the available evidence
There is further evidence to support that ethnic and socioeconomic disparities are associated with important differences in health outcomes, including in acute illness. In particular, there are differences in healthcare use, age and comorbidity profiles across ethnic groups. However, these differences are masked by statistical adjustment because patients from ethnic minorities present at a younger age highlighting the need for further research to understand and address community level causes of health inequalities.
Alt-text: Unlabelled box
1. Introduction
Health inequalities affecting minority ethnic people in the UK are well-documented [1,2]. Inequalities occur across the spectrum of healthcare including access to and uptake of services, and quality and experience of care [3], [4], [5], [6]. People of Black, Asian and other minority ethnic groups report worse general health, and experience higher levels of significant comorbidity compared to White British groups [7]. While there have been improvements in healthcare provision and outcomes for the overall population, it remains unclear how these changes have affected minority ethnic groups. The COVID-19 pandemic has highlighted the impact of these inequalities on health outcomes [8]. Despite making up less than 14% of the UK population, Black, Asian, and minority ethnic groups accounted for 19% of deaths in hospital and 35% of critical care admissions following COVID-19 [9,10]. In east London, Black and Asian patients hospitalised due to COVID-19 are younger and more likely to die [11].
A number of explanatory factors may account for these inequalities including pre-existing health conditions, socioeconomic status, and environmental or structural determinants of health [12], [13], [14]. However, the relationship between ethnicity and health is complex as risk factors are likely to interact and are inextricably linked with wider social determinants of disease. The ethnic disparities identified during the COVID-19 pandemic reflect those consistently demonstrated across chronic conditions such as cardiovascular disease, diabetes, stroke, and hypertension prior to the pandemic [15], [16], [17]. These studies demonstrate that ethnic minorities tend to have poorer baseline health compared to majority ethnic groups and coupled with recent findings suggest that imbalances in outcomes following illness persist between ethnic groups. This highlights the fact that determinants of ethnic inequalities in general remain poorly understood. Whilst there is a body of evidence characterising ethnic disparities in chronic diseases, information focusing on acute illness is limited [18], [19], [20]. Most studies are descriptive, of small sample size and limited by inadequate risk adjustment for important risk factors such as socioeconomic status [20], [21], [22], [23].
Understanding ethnicity disparities in healthcare use in general and outcomes following a range of acute illnesses may identify population specific interventions to improve overall health status. We aimed to describe differences in demographics, comorbidity, and outcomes for patients in different ethnic groups after acute hospital admission for a range of disease indications.
2. Methods
2.1. Study cohort
All adult patients presenting with an acute illness and admitted to any of the four acute hospital within Barts Health NHS Trust (The Royal London Hospital, Whipps Cross University Hospital, St Bartholomew's Hospital, and Newham University Hospital) between 1st January 2013 and 31st December 2018 were identified, data were available for Newham University Hospital from 14th February 2016. The study was approved as anonymized analysis of routine patient data without need for consent by NHS England Health Research Authority. Data access and dataset curation was restricted to YIW and JRP during September and October 2020 for this analysis. Patients aged < 18 years, patients with undefined age in with context of trauma admissions, obstetric and antenatal admissions, planned and booked admissions were excluded. The first emergency hospital episode during the study period was identified as the index admission. Total numbers of separate hospital episodes were identified. Patients with unknown or undisclosed ethnicity were included in assessment of baseline characteristics but excluded from outcomes analysis. Clinical, demographic, and coding data were collated from the Barts Health Cerner Millennium Electronic Medical Record data warehouse and locally held ICNARC databases by members of the direct clinical care team. ICNARC data was complete up to 31st December 2017. Survival data was extracted to 18th September 2020.
2.2. Definitions of key variables
Ethnicity was defined using the NHS ethnic category codes and based on five high-level groups: White, Asian or Asian British, Black or Black British, Mixed, and Other [24]. Relative measures of socioeconomic deprivation were assessed using the English Indices of Deprivation 2020 by matching patient postcode to national index of multiple deprivation (IMD) quintiles [25]. National quintiles are presented in descriptive tables. Analyses were carried out using local quintiles within the study cohort to account for potential disproportionate grouping in national quintiles in our dataset. Baseline comorbid diseases, Charlson comorbidity index (CCI), and Hospital Frailty Risk Score (HFRS) were mapped to ICD-10 coding. Healthcare Resource Group coding was used to identify specific indications for hospital admission. Population-level distribution of age, sex, and ethnicity in the London boroughs of Tower Hamlets, Newham, and Waltham Forest were taken from the 2011 census provided by Official Labour Market Statistics [26]. Full definitions are in supplementary materials.
2.3. Outcome measures
The co-primary outcomes were survival assessed at 30-days and one-year. The secondary outcomes were admission to the intensive care unit (ICU), ICU length of stay, need for advanced organ support on ICU defined by mechanical ventilation or renal replacement therapy, hospital length of stay, and discharge destination if discharged alive from hospital.
2.4. Statistical analysis
Analyses were carried out in accordance with a pre-published statistical analysis plan [27]. We compared baseline characteristics across ethnic groups. Due to non-proportionality between ethnic groups and risk of death over-time observed in preliminary analysis, logistic regression models were used to assess survival adjusted for age and sex at 30-days and one-year in preference to Cox survival analysis. To account for non-linear effects of age, a restricted cubic spline model with five knots was used. A further multivariable model was developed to assess the effect of pre-defined risk factors: IMD quintile, smoking status, BMI ≥ 30 kg/m2, diabetes, hypertension, and chronic kidney disease (CKD). These were chosen to allow a comparative analysis [11]. Association between ethnic group and admission to ICU or requirement for advanced organ support were investigated by logistic regression. To account for potential differences in care, hospital site was included in all models as a fixed-effect variable. An unadjusted Kaplan-Meier survival plot to one-year was generated. We also investigated potential interaction between ethnicity and IMD quintile. Finally, amongst patients with an address in the London Boroughs of Tower Hamlets, Newham, and Waltham Forest (a population of around 1 million served by our hospital system), we compared distribution of admissions by age across ethnic groups with distribution of people by age across ethnic groups within these boroughs. To account for differences in age structure between ethnic groups, we calculated comparative mortality rates using age-standardised mortality rates based on the 2013 European Standard Population figures. Data are presented as mean (SD), median (IQR) or n (%). Effect measures are presented as odds ratios (OR) with 95% confidence intervals (CI). All analyses were performed using R version 4.0.2 (R Core Team 2020).
2.5. Sensitivity analyses
To assess the effect of including patients living outside the Barts Health NHS Trust catchment area, the primary survival analysis was repeated using a subset of patients residing within Tower Hamlets, Newham, and Waltham Forest only. In usual circumstances, patients tend to only attend hospitals within their catchment area measured by physical proximity, particularly in an acute emergency setting. Additional multivariable models were carried out using CCI as an aggregate measure of total comorbid disease burden and HFRS [28]. Finally, mortality rates were compared, and separate multivariable models carried out to assess survival following specific indications for hospital admission: pneumonia or lower respiratory tract infection or respiratory failure, acute myocardial infarction, stroke or transient ischaemic event, infection or sepsis, and trauma including head injury. Indications for admission were identified by tagging hospital resource group codes assigned to each admission.
2.6. Role of funding source
No funding was received for conducting this study.
3. Results
Between 2013 and 2018, 203,182 adults experienced a total of 542,848 emergency, non-obstetric, hospital admissions. Survival follow-up to 18th September 2020 was complete for the entire cohort with median follow-up period of 1344 [IQR 861–1975] days. All patients with baseline data were included (Fig. S1). Using high-level ethnic group categories, the ethnicity distribution was majority White (n = 100,065, 49.2%), followed by Asian or Asian British (n = 43,101, 21•2%), Black or Black British (n = 21,388, 10.5%), Other (n = 13,946, 6.9%), and Mixed (n = 2982, 2.5%). Around a tenth of patients were of unknown or undisclosed ethnicity (n = 21,700, 10.7%). Distributions within sub-categories are shown in Table S1. Baseline characteristics across ethnic groups are shown in Table 1. Non-white patients were significantly younger on admission with a median age of 36 [26–52] years (Mixed), 43 [31–62] years (Asian or Asian British), 43 [26–52] years (Other), and 48 [33–63] years (Black) compared to 55 [35–74] years in the White group (p < 0.001). The majority of patients were classified as being in the two most deprived socioeconomic quintiles in England: IMD1 (37.8%) and IMD2 (34.2%). Levels of deprivation were highest in the Asian and Black groups with 83.3% of Asian and 87.2% of Black patients being in IMD1 and IMD2 compared to 64.0% (White), 73.8% (Other), and 77.5% (Mixed). Considering only locally domiciled patients, socioeconomic deprivation remained higher in non-white groups: 94.2% Asian and 92.7% Black compared to 74.2% White being classed within the 40% most economically deprived patients.
Table 1.
Study population baseline characteristics stratified by ethnic group. n (%) unless otherwise stated. Total n = 203,182 unless otherwise stated. P values based on Chi-square (for categorical) or Kruskal-Wallis test (for continuous). SD: standard deviation, IQR: interquartile range, IMD: index of multiple deprivation, LRTI: lower respiratory tract infection, RF: respiratory failure, TIA: transient ischaemic attack, HTN: hypertension, CVA: cerebrovascular accident, COPD: chronic obstructive pulmonary disease, CKD: chronic kidney disease, RRT: renal replacement therapy, HIV: human immunodeficiency virus.
| All patients |
Stratified by ethnic group |
|||||||
|---|---|---|---|---|---|---|---|---|
| Asian or Asian British | Black or Black British | Mixed | Other | Unknown and undisclosed | White | p value | ||
| n | 203,182 | 43,101 | 21,388 | 2982 | 13,946 | 21,700 | 100,065 | |
| Age (years) (median (IQR)) | 50.0 (33.0, 69.0) | 43.0 (31.0, 62.0) | 48.0 (33.0, 63.0) | 36.0 (26.0, 52.0) | 43.0 (30.0, 60.0) | 47.0 (32.0, 66.0) | 55.0 (35.0, 74.0) | <0.001 |
| Male [n = 203,165] | 104,552 (51.2) | 21,087 (48.9) | 9742 (45.6) | 1310 (43.9) | 7604 (54.5) | 12,918 (59.5) | 51,891 (51.9) | <0.001 |
| National IMD quintile [n = 195,695] | <0.001 | |||||||
| 1 (most deprived) | 73,934 (37.8) | 18,735 (44.3) | 10,629 (50.6) | 1252 (43.1) | 5058 (39.2) | 7045 (35.1) | 31,215 (32.3) | |
| 2 | 66,934 (34.2) | 16,473 (38.9) | 7675 (36.6) | 1000 (34.4) | 4469 (34.6) | 6687 (33.3) | 30,630 (31.7) | |
| 3 | 25,488 (13.0) | 3806 (9.0) | 1793 (8.5) | 371 (12.8) | 1703 (13.2) | 2780 (13.9) | 15,035 (15.6) | |
| 4 | 17,001 (8.7) | 2243 (5.3) | 631 (3.0) | 185 (6.4) | 1026 (7.9) | 2040 (10.2) | 10,876 (11.3) | |
| 5 (least deprived) | 12,338 (6.3) | 1079 (2.5) | 258 (1.2) | 98 (3.4) | 661 (5.1) | 1503 (7.5) | 8739 (9.1) | |
| Number of admissions | <0.001 | |||||||
| 1 | 139,906 (68.9) | 28,127 (65.3) | 13,805 (64.5) | 2143 (71.9) | 11,029 (79.1) | 18,777 (86.5) | 66,025 (66.0) | |
| 2–4 | 50,398 (24.8) | 11,839 (27.5) | 5802 (27.1) | 689 (23.1) | 2539 (18.2) | 2700 (12.4) | 26,829 (26.8) | |
| ≥5 | 12,878 (6.3) | 3135 (7.3) | 1781 (8.3) | 150 (5.0) | 378 (2.7) | 223 (1.0) | 7211 (7.2) | |
| Disease specific admissions | <0.001 | |||||||
| Pneumonia or LRTI or RF | 4026 (2.0) | 851 (2.0) | 338 (1.6) | 36 (1.2) | 177 (1.3) | 269 (1.2) | 2355 (2.4) | |
| Acute myocardial infarction | 1913 (0.9) | 608 (1.4) | 131 (0.6) | 20 (0.7) | 104 (0.7) | 219 (1.0) | 831 (0.8) | |
| Stroke or TIA | 2422 (1.2) | 421 (1.0) | 298 (1.4) | 26 (0.9) | 249 (1.8) | 370 (1.7) | 1058 (1.1) | |
| Infection or sepsis | 9712 (4.8) | 2347 (5.4) | 999 (4.7) | 114 (3.8) | 639 (4.6) | 796 (3.7) | 4817 (4.8) | |
| Trauma | 14,514 (7.1) | 1535 (3.6) | 950 (4.4) | 180 (6.0) | 1459 (10.5) | 3170 (14.6) | 7220 (7.2) | |
| Other | 170,595 (84.0) | 37,339 (86.6) | 18,672 (87.3) | 2606 (87.3) | 11,318 (81.2) | 16,876 (77.8) | 83,784 (83.7) | |
| Comorbid disease [n = 202,852] | ||||||||
| Smoking | 30,255 (14.9) | 4957 (11.5) | 2370 (11.1) | 529 (17.8) | 1907 (13.7) | 2631 (12.2) | 17,861 (17.9) | <0.001 |
| Obesity | 6621 (3.3) | 1486 (3.5) | 892 (4.2) | 81 (2.7) | 289 (2.1) | 472 (2.2) | 3401 (3.4) | <0.001 |
| Diabetes | 33,115 (31.8) | 11,373 (26.4) | 4293 (20.1) | 364 (12.2) | 1680 (12.1) | 2679 (12.4) | 12,726 (12.7) | <0.001 |
| HTN | 64,575 (31.8) | 14,778 (34.3) | 8056 (37.7) | 619 (20.8) | 3204 (23.0) | 5421 (25.1) | 32,497 (32.5) | <0.001 |
| Ischaemic heart disease | 26,943 (13.3) | 7135 (16.6) | 1722 (8.1) | 200 (6.7) | 1108 (8.0) | 2731 (12.6) | 14,047 (14.1) | <0.001 |
| Myocardial infarction | 16,662 (8.2) | 4520 (10.5) | 961 (4.5) | 128 (4.3) | 707 (5.1) | 1759 (8.1) | 8587 (8.6) | <0.001 |
| Congestive heart failure | 16,916 (8.3) | 3332 (7.7) | 1493 (7.0) | 144 (4.8) | 698 (5.0) | 1764 (8.2) | 9485 (9.5) | <0.001 |
| Peripheral vascular disease | 8333 (4.1) | 1132 (2.6) | 802 (3.8) | 75 (2.5) | 365 (2.6) | 767 (3.5) | 5192 (5.2) | <0.001 |
| CVA or TIA | 17,718 (8.7) | 2997 (7.0) | 2024 (9.5) | 154 (5.2) | 1079 (7.8) | 1726 (8.0) | 9738 (9.7) | <0.001 |
| Dementia | 8887 (4.4) | 1056 (2.5) | 839 (3.9) | 59 (2.0) | 354 (2.5) | 650 (3.0) | 5929 (5.9) | <0.001 |
| COPD | 30,720 (15.1) | 6480 (15.1) | 2657 (12.4) | 430 (14.4) | 1345 (9.7) | 2162 (10.0) | 17,646 (17.7) | <0.001 |
| Liver disease | 9394 (4.6) | 2045 (4.8) | 1012 (4.7) | 104 (3.5) | 540 (3.9) | 711 (3.3) | 4982 (5.0) | <0.001 |
| Moderate to severe CKD | 16,065 (7.9) | 3788 (8.8) | 2285 (10.7) | 137 (4.6) | 593 (4.3) | 1237 (5.7) | 8025 (8.0) | <0.001 |
| End-stage renal disease | 584 (0.3) | 193 (0.4) | 158 (0.7) | 8 (0.3) | 26 (0.2) | 22 (0.1) | 177 (0.2) | <0.001 |
| Cancer | 7433 (3.7) | 924 (0.4) | 158 (0.7) | 8 (0.3) | 26 (0.2) | 22 (0.1) | 177 (0.2) | <0.001 |
| HIV | 796 (0.4) | 33 (0.1) | 293 (1.4) | 19 (0.6) | 54 (0.4) | 88 (0.4) | 309 (0.3) | <0.001 |
| Charlson comorbidity index | <0.001 | |||||||
| 0 | 105,213 (51.9) | 21,949 (51.0) | 10,967 (51.4) | 1842 (61.8) | 8683 (62.4) | 12,599 (58.3) | 49,173 (49.2) | |
| 1–2 | 60,566 (29.9) | 13,655 (31.7) | 6039 (28.3) | 806 (27.0) | 3572 (25.7) | 6022 (27.8) | 30,472 (30.5) | |
| 3–4 | 19,589 (9.7) | 4074 (9.5) | 2074 (9.7) | 188 (6.3) | 851 (6.1) | 1747 (8.1) | 10,655 (10.7) | |
| ≥5 | 17,484 (8.6) | 3356 (7.8) | 2270 (10.6) | 144 (4.8) | 798 (5.7) | 1258 (5.8) | 9658 (9.7) | |
| Hospital frailty Risk Score | <0.001 | |||||||
| <5 (low risk) | 148,290 (73.1) | 33,775 (78.5) | 15,975 (74.8) | 2477 (83.1) | 10,954 (78.8) | 16,451 (76.1) | 68,658 (68.7) | |
| 5–15 (intermediate risk) | 37,391 (18.4) | 6798 (15.8) | 3744 (17.5) | 397 (13.3) | 2315 (16.6) | 4156 (19.2) | 19,981 (20.0) | |
| >15 (high risk) | 17,171 (8.5) | 2461 (5.7) | 1631 (7.6) | 106 (3.6) | 635 (4.6) | 1019 (4.7) | 11,319 (11.3) | |
| ICU [n = 154,602] | ||||||||
| Admission to ICU | 7557 (4.9) | 999 (3.1) | 564 (3.6) | 76 (3.3) | 552 (5.4) | 1832 (11.4) | 3534 (4.5) | <0.001 |
| Mechanical ventilation | 3870 (47.8) | 538 (47.8) | 250 (40.7) | 32 (38.6) | 291 (50.9) | 1108 (59.3) | 1651 (43.1) | <0.001 |
| RRT | 690 (8.5) | 106 (9.4) | 65 (10.6) | 3 (3.6) | 47 (8.2) | 136 (7.3) | 333 (8.7) | 0.053 |
| Total number of organ systems | <0.001 | |||||||
| 0 | 407 (5.0) | 45 (4.0) | 26 (4.2) | 6 (7.2) | 23 (4.0) | 84 (4.5) | 223 (5.8) | |
| 1 | 2297 (28.4) | 317 (28.2) | 195 (31.7) | 26 (31.3) | 172 (30.1) | 389 (20.8) | 1198 (31.2) | |
| 2 | 2589 (32.0) | 385 (34.2) | 207 (33.7) | 27 (32.5) | 170 (29.7) | 599 (32.1) | 1201 (31.3) | |
| ≥3 | 2804 (34.6) | 378 (33.6) | 187 (30.4) | 24 (28.9) | 207 (36.2) | 796 (42.6) | 1212 (31.6) | |
| ICU length of stay | ||||||||
| (mean (SD)) | 5.33 (8.61) | 4.98 (8.58) | 4.81 (6.78) | 4.08 (4.72) | 5.42 (8.09) | 5.96 (8.14) | 5.23 (9.22) | 0.006 |
| (median (IQR)) | 3.0 (1.0, 6.0) | 3.0 (1.0, 5.0) | 3.0 (1.0, 6.0) | 2.0 (1.0, 5.0) | 3.0 (1.0, 6.0) | 3.0 (2.0, 7.0) | 3.0 (1.0, 6.0) | <0.001 |
| Died on ICU | 1274 (15.7) | 167 (14.8) | 61 (9.9) | 7 (8.4) | 89 (15.6) | 407 (21.8) | 543 (14.2) | <0.001 |
| Death | ||||||||
| Died | 27,638 (13.6) | 4170 (9.7) | 2526 (11.8) | 202 (6.8) | 1235 (8.9) | 2494 (11.5) | 17,011 (17.0) | <0.001 |
| Died within 30 days | 5913 (2.9) | 739 (1.7) | 378 (1.8) | 28 (0.9) | 355 (2.5) | 1101 (5.1) | 3312 (3.3) | <0.001 |
| Died within 1 year | 16,054 (7.9) | 2082 (4.8) | 1280 (6.0) | 103 (3.5) | 830 (6.0) | 2007 (9.2) | 9752 (9.7) | <0.001 |
| Age died (years) (median (IQR)) | 77.8 (65.8, 86.0) | 75.5 (63.5, 82.3) | 74.9 (59.3, 83.0) | 75.3 (55.9, 81.3) | 72.7 (58.5, 83.8) | 73.4 (59.6, 83.8) | 79.8 (68.6, 87.8) | <0.001 |
| Hospital length of stay | ||||||||
| (mean (SD)) | 5.88 (11.93) | 3.51 (9.57) | 4.49 (10.95) | 3.79 (11.42) | 4.76 (12.00) | 6.06 (13.60) | 5.35 (12.58) | <0.001 |
| (median (IQR)) | 1.0 (0.0, 5.0) | 1.0 (0.0, 3.0) | 1.0 (0.0, 4.0) | 1.0 (0.0, 3.0) | 1.0 (0.0, 3.0) | 2.0 (0.0, 6.0) | 2.0 (0.0, 5.0) | <0.001 |
| Discharge destination | <0.001 | |||||||
| Usual place of residence | 184,820 (93.4) | 40,610 (95.6) | 19,745 (93.7) | 2776 (94.0) | 12,619 (92.6) | 18,567 (90.1) | 90,503 (93.2) | |
| Care home or equivalent | 1188 (0.6) | 102 (0.2) | 96 (0.5) | 8 (0.3) | 57 (0.4) | 104 (0.5) | 821 (0.8) | |
| Health-related institution | 9768 (4.9) | 1403 (3.3) | 1006 (4.8) | 142 (4.8) | 786 (5.8) | 1648 (8.0) | 4783 (4.9) | |
| Hospice or equivalent | 70 (0.0) | 6 (0.0) | 11 (0.1) | 0 (0.0) | 5 (0.0) | 16 (0.1) | 32 (0.0) | |
| Temporary residence | 1764 (0.9) | 336 (0.8) | 175 (0.8) | 22 (0.7) | 136 (1.0) | 201 (1.0) | 894 (0.9) | |
| Other | 230 (0.1) | 29 (0.1) | 31 (0.1) | 5 (0.2) | 22 (0.2) | 69 (0.3) | 74 (0.1) | |
3.1. Hospital admissions by age-group
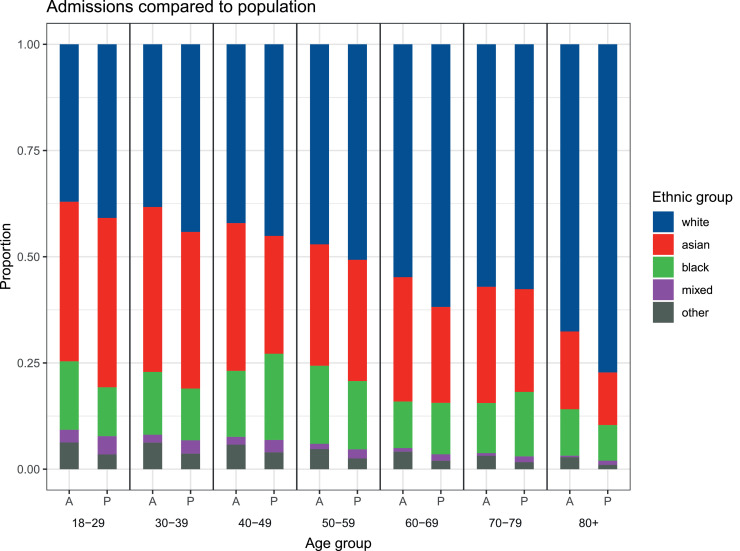
For non-white compared to White patients residing in Tower hamlets, Newham, and Waltham Forest, there was a small but consistently greater proportion of hospital admissions relative to the local population at every age group (Fig. 1). Differences were statistically significant (p < 0.001) for all age groups apart from the 70–79 years group (p = 0.14), most marked at the extreme of age with 32.4% of hospital admissions compared to 22.8% of the local population in the ≥ 80 years group.
Fig. 1.
Age at admission compared to population distribution by age and ethnic group showing proportions within each ethnic group by age group. * p < 0.001.
3.2. Burden of comorbid disease
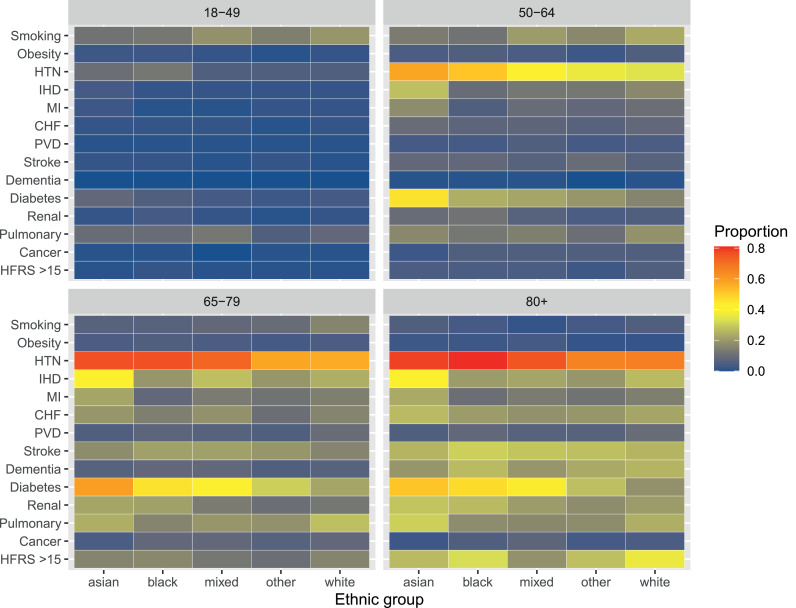
Burden of comorbid disease varied between ethnic groups in prevalence, type and age-distribution (all p values based on Chi-square test < 0.001 for listed diseases). Prevalence of diabetes (26.4% vs 12.7% White), ischaemic heart disease (16.6% vs 14.1% White), and myocardial infarction (10.5% vs 8.6% White) were highest in the Asian group; HTN (37.7% vs 32.5% White), CKD (10.7% vs 8.0% White), and HIV (1.3% vs 0.3% White) in the Black group; and congestive heart failure (9.5% vs 7.7% Asian and 7.0% Black), peripheral vascular disease (5.2% vs 2.6% Asian and 3.8% Black), and dementia (5.9% vs 2.5% Asian and 3.9% Black) in the White group. CCI was similar between ethnic groups, but White patients had higher frailty scores (> 15 group 11.3% vs 5.9% Asian and 7.6% Black). There was a higher prevalence of comorbid diseases at a younger age in non-white ethnic groups, including for diseases with higher overall prevalence in White patients such as congestive heart failure being more prevalent at younger age groups in Asian patients, and dementia in Black patients (Fig. 2).
Fig. 2.
Heat map of comorbid disease by age and ethnic group showing proportions within each ethnic group by age group. Obesity defined as BMI ≥ 30 kg/m2, HTN: hypertension, IHD: ischaemic heart disease, MI: myocardial infarction, CHF: congestive heart failure, PVD: peripheral vascular disease, HFRS: hospital frailty risk score.
3.3. Survival analyses
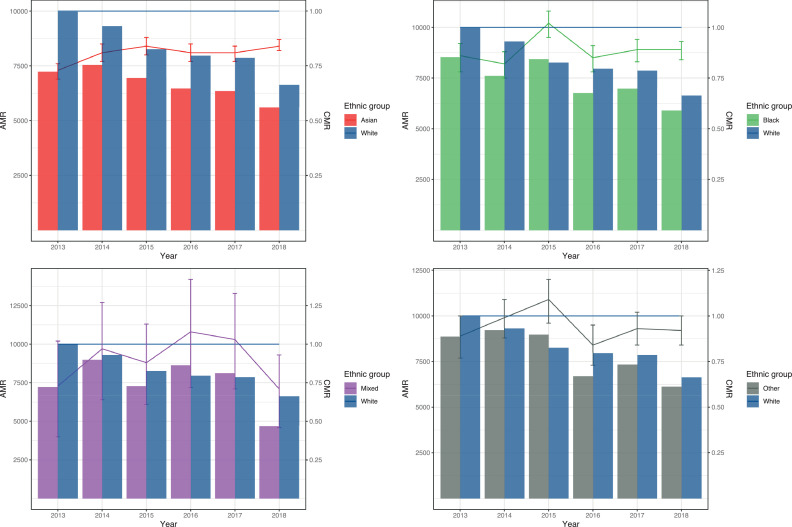
The overall survival rate following a first emergency admission for the cohort was 97.1% at 30-days and 92.1% at 1-year (Table S2 and Fig. S2). A greater proportion of total deaths occurred in the White group. However, of patients who died, non-White patients died at a younger age: median age 75.5 years (Asian), 74.9 years (Black), 75.3 years (Mixed), 72.7 (Other), 73.4 (unknown or undisclosed) compared to 79.8 years (White) (Table 1). A total of 181,467 patients were included in age and sex-adjusted survival analysis excluding patients with unknown or undisclosed ethnicity. Risk of death was significantly lower in Asian, Black, and Mixed patients compared to White both at 30-days and 1-year (Table 2). These effects persisted in multivariable analyses at both 30-days and 1-year with similar effect sizes (Table 3). Adjusted survival was highest at 30-days in the Mixed ethnic group (OR 0.60 [0.40–0.89], p = 0.01), and at 1-year in the Asian group (OR 0.69 [0.66–0.73], p < 0.0001). Accounting for differences in age structure, comparative mortality rates were lower in Asian and Black groups compared to White (Fig. 3). There was a strong association with increasing deprivation based on IMD and reduced survival. The 20% most deprived patients in the study population had an increased rate of death over 30% compared to the least deprived 20% at both 30-days and 1-year. Distribution of comorbidity differed between IMD quintiles (Fig. S3). Accounting for differences in age structure between IMD, there was a consistent effect with increased mortality with higher levels of deprivation (Fig. S4). There was no overall statistical evidence for an interaction between ethnicity and IMD on survival (p = 0.48).
Table 2.
Association of ethnic group with 30-day and 1-year survival using logistic regression modelling, age and sex corrected, hospital site included as a fixed effect. Total n = 181,467, deaths at 30-days = 4812, deaths at 1-year =14,044.
| Total |
Deaths (%) |
30-day |
1-year |
||||
|---|---|---|---|---|---|---|---|
| 30-day | 1-year | Odds ratio (95% CI) | p value | Odds ratio (95% CI) | p value | ||
| Age (69 vs 33 years) | – | – | – | 13.8 (11.65–16.34) | < 0·0001 | 16.39 (14.84–18.10) | < 0.0001 |
| Male | – | – | – | 1.19 (1.12–1.27) | < 0·0001 | 1.20 (1.16–1.25) | < 0.0001 |
| Ethnic group | |||||||
| Asian or Asian British | 43,098 | 739 (1.7) | 2082 (4.8) | 0.84 (0.77–0.91) | < 0·0001 | 0.75 (0.72–0.79) | < 0.0001 |
| Black or Black British | 21,387 | 378 (1.8) | 1279 (6.0) | 0.78 (0.70–0.87) | < 0.0001 | 0.86 (0.81–0.92) | < 0.0001 |
| Mixed | 2982 | 38 (1.3) | 103 (3.5) | 0.62 (0.42–0.91) | 0·01 | 0.75 (0.61–0.93) | 0.007 |
| Other | 13,945 | 355 (2.5) | 830 (6.0) | 1.25 (1.11–1.40) | < 0.001 | 0.95 (0.87–1.02) | 0.17 |
| White | 100,055 | 3312 (3.3) | 9750 (9.7) | Reference | – | Reference | – |
Table 3.
Multivariable analysis of 30-day and 1-year survival using logistic regression modelling, age and sex corrected, hospital site included as a fixed effect. Variables included Index of Multiple Deprivation (IMD) quintile, Body Mass Index (BMI) ≥ 30 kg/m2, diabetes, Hypertension (HTN), Chronic Kidney Disease (CKD). Total n = 175,372, deaths at 30-days =4649, deaths at 1-year =13,686.
|
Adjusted 30-day |
Adjusted 1-year |
|||
|---|---|---|---|---|
| Odds ratio (95% CI) | p value | Odds ratio (95% CI) | p value | |
| Age (69 vs 33 years) | 18.18 (15.16–21.80) | < 0·0001 | 17.73 (15.97–19.69) | < 0.0001 |
| Male | 1.19 (1.12–1.27) | < 0.0001 | 1.18 (1.13–1.22) | < 0.0001 |
| Ethnic group | ||||
| Asian or Asian British | 0.85 (0.78–0.93) | < 0.001 | 0.69 (0.66–0.73) | < 0.0001 |
| Black or Black British | 0.77 (0.69–0.86) | < 0.0001 | 0.79 (0.74–0.85) | < 0.0001 |
| Mixed | 0.60 (0.40–0.89) | 0.01 | 0.72 (0.58–0.89) | 0.002 |
| Other | 1.21 (1.08–1.37) | 0.002 | 0.95 (0.88–1.03) | 0.22 |
| White | Reference | – | Reference | – |
| IMD study quintile | ||||
| 1 (most deprived) | 1.34 (1.22–1.48) | < 0.0001 | 1.41 (1.33–1.50) | < 0.0001 |
| 2 | 1.29 (1.17–1.42) | < 0.0001 | 1.37 (1.29–1.45) | < 0.0001 |
| 3 | 1.26 (1.14–1.39) | < 0.0001 | 1.29 (1.21–1.37) | < 0.0001 |
| 4 | 1.15 (1.04–1.26) | 0.005 | 1.18 (1.11–1.25) | < 0.0001 |
| 5 (least deprived) | Reference | – | Reference | – |
| Smoking | 1.00 (0.91–1.10) | 0.94 | 1.11 (1.05–1.18) | < 0.001 |
| BMI ≥ 30 kg/m2 | 0.99 (0.83–1.17) | 0.90 | 0.95 (0.86–1.05) | 0.34 |
| Diabetes | 0.98 (0.91–1.06) | 0.64 | 1.15 (1.10–1.20) | < 0.0001 |
| HTN | 0.70 (0.66–0.75) | < 0.0001 | 0.76 (0.73–0.79) | < 0.0001 |
| CKD | 1.05 (0.96–1.14) | 0.27 | 1.47 (1.40–1.55) | < 0.0001 |
Fig. 3.
Bar charts showing the age-standardised mortality rate (AMR) per 100,000 population per year. Using the 2013 European Standard Population, axis on the left-hand side of each plot. AMR for England available for years 2013 to 2016 were 979 in 2013, 947 in 2014, 987 in 2015, 960 in 2016 per 100,000 population. Line graph showing the comparative mortality ratio (CMR) for each ethnic group compared to white, axis on the right-hand side of each plot. 95% CI shown by error bars.
3.4. Secondary outcomes
Patients with White ethnicity had longer hospital lengths of stay (mean 5.35 days (12.6) compared to 3.51 (9.6) Asian and 4.49 (11.0) Black) and were least likely to return to their usual place of residence on discharge (93.2% compared to 95.6% Asian and 93.7% Black). Rates of admission to ICU were highest in patients with Other (5.4%), unknown and undisclosed ethnicity (11.4%) (Table 1). Patients in the Asian group were least likely to be admitted to ICU compared to the White group (OR 0.70 [0.65–0.76], p = 0.0001) (Table S3). However, if admitted to ICU, Asian and Other ethnic groups were more likely to receive mechanical ventilation compared to the White group (Table S4). There were no differences between ethnic groups in use of renal replacement therapy on ICU after adjustment for comorbid diseases (Table S5). In multivariable analyses, likelihood of admission to ICU was lower with increasing levels of socioeconomic deprivation: the most deprived 20% (OR 0.79 [0.73–0.84], p < 0.0001) compared to the least deprived 20% of study population (Table S4).
3.5. Sensitivity analyses
After excluding out-of-area patients, association between reduced survival and White patients remained (Tables S6–S8). In multivariable analyses examining the influence of total comorbidity burden as assessed by CCI and frailty measured using HFRS, associations between different ethnic groups with survival were unchanged (Tables S9 and S10). Effects of ethnic group and IMD persisted with lower survival at 1 year in White and more-deprived patients across a range of specific disease presentations (Tables S11–S16). The top 10 hospital resource group codes assigned to admissions were similar across ethnic groups (Table S17).
4. Discussion
This study has examined the impact of ethnicity on acute hospital admissions within an ethnically diverse and deprived urban area. We provide some baseline, pre-pandemic data to feed into further research. The principal finding was that overall survival following an acute hospital admission was better in patients of Asian, Black or Mixed compared to White background. This finding is in contrast to the higher age-adjusted mortality seen recently in minority ethnic groups in COVID-19. However, patients from minority ethnic groups presented at a younger age and made up a greater proportion of total admissions relative to the ethnic distribution of the background population at every age group. Differences identified in comorbidity profiles between ethnic groups in this study support previously reported patterns [17,[29], [30], [31]]. Non-white patients had a distinct and earlier onset burden of comorbid disease which could potentially drive need to access secondary healthcare for reasons less associated with short to medium-term risk of death. Inclusion of IMD as a measure of socioeconomic deprivation did not alter ethnicity-survival relationships, but the greater effects of deprivation on reduced survival was consistent in adjusted analyses across acute disease presentations.
It is well known that socioeconomic deprivation has a detrimental impact on health [32]. Despite efforts from local authorities to reduce inequalities, life expectancy has declined over the last decade and time spent in poor health increased for some of the most deprived groups in the UK [33]. Overall levels of deprivation were higher in patients residing within the Barts Health catchment area, compared to the total cohort. In this subset, risks for poorer survival conferred by relative deprivation were reduced (perhaps reflecting a more homogenous level of deprivation) but risks conferred by ethnic group remained the same with White patients continuing to have the lowest survival. This suggests that patients from a highly deprived White ethnicity background could have the worst outcomes, supporting findings from linkage studies in Scotland [34,35]. Understanding the complex relationship between ethnicity and socioeconomic status remains a challenge [36]. Based on previous evidence, different socioeconomic gradients in health exist between ethnic groups resulting in different effects of risk relating to ill health [37,38]. Research in Scotland has shown that the majority white Scottish group suffered poorer health overall, and that the south Asian group had higher risk of ill health and mortality from specific diseases [16,39,40]. In England, area deprivation has been shown to have a greater and more detrimental effect on the health of white British people compared to some minority groups [37]. Assessment of socioeconomic status tend to use aggregated measures of area deprivation from multiple components of which, different aspects such as education, occupation, income will have different levels of relevance across ethnic groups [16]. Furthermore, some indicators of deprivation such as housing may not accurately capture the life circumstances of some ethnicities and reflect cultural norms rather than deprivation or health.
Disproportionate acute hospital presentation may reflect differences in access and healthcare use within the east London population. However, comparisons were made against the 2011 census and differences seen may reflect population ageing across ethnic groups. First acute hospital episodes in Asian and Black patients were less likely to require ICU admission which may reflect a lower disease severity on presentation. There may be other influences on health seeking behavior and patterns of healthcare access including cultural practices. Causal determinants of these relationships are unclear. To better understand the reasons behind this, analysis of primary care data, waiting list times for non-acute secondary services, as well as qualitative analysis of experiences and attitudes of the population are required.
This study has used a comprehensive dataset from four hospitals including a range of acute hospital presentations over a six-year period. The contribution of socioeconomic deprivation, baseline health status and comorbid disease were assessed through inclusion in multivariable models. A pre-specified statistical analysis plan was followed, and multiple sensitivity analyses were performed to test the robustness of these findings. There are however some limitations. Like many datasets, ethnic categorizations were aggregated and did not reflect the considerable heterogeneity within ethnic groups. Despite the size of the study, there was insufficient statistical power to assess a more detailed ethnicity breakdown. A large proportion of patients were classed as unknown or undisclosed ethnicity, this may be due to current categorization systems being too restrictive, inaccuracy in hospital-assigned status for patients unable to self-report, or patients identifying differently when seeking healthcare compared to in a census return. Misclassification of patients into both unknown or other ethnic groups may occur more frequently in emergency admissions and therefore lead to over-representation of these ethnic categories compared to census data. As a result, survival risks cannot be clearly interpreted in these groups due to potential allocation bias. Importantly such concerns are likely to apply to analysis of all NHS datasets that are not linked to census data. Similarly, socioeconomic deprivation has been assessed using a composite measure. Therefore, we were not able to evaluate the direct effects of variations in other social determinants of health, differences in access to appropriate healthcare, or follow-up services. In determining IMD, although there was no change in our results when using the 2020 and 2015 versions of the English Indices of Deprivation, regions may change over time and this should be considered in future studies. Specific disease presentations were identified through hospital resource group coding, which were incomplete for 17% of admission episodes limiting more detailed subgroup analyses. Reliance on clinical coding meant that assessment of important additional variables including occupation, lifestyle risk factors, variations in disease severity on admission, chronic disease management, and hospital process measures was not possible.
Ethnic and socioeconomic disparities exist in healthcare use, age and comorbidity profiles in east London. Patients from minority ethnic groups present acutely to hospital at a younger age on a background of increased comorbidity. Accounting for all age groups, overall survival in the year following an acute hospital admission was better for patients of Black, Asian, and Mixed ethnicity. Further research is necessary to understand and address community-level causes of health inequalities.
Data sharing statement
The statistical analysis plan can be accessed online. The authors will be happy to consider additional analyses of the anonymised dataset on request. The need for stringent measures to prevent re-identification of individuals within a discrete geographical location and limited time-period however preclude sharing of patient level dataset in a GDPR compliant form.
Funding
No funding was received for conducting this study.
Declaration of Competing Interest
All authors declare no other competing interests.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2021.101077.
Appendix. Supplementary materials
References
- 1.Smith G.D., Chaturvedi N., Harding S., Nazroo J., Williams R. Ethnic inequalities in health: a review of UK epidemiological evidence. Crit Public Health. 2000;10(4):375–408. [Google Scholar]
- 2.Karlsen S., Nazroo J.Y. Religious and ethnic differences in health: evidence from the health surveys for England 1999 and 2004. Ethn Health. 2010;15(6):549–568. doi: 10.1080/13557858.2010.497204. [DOI] [PubMed] [Google Scholar]
- 3.Szczepura A. Access to health care for ethnic minority populations. Postgrad Med J. 2005;81(953):141–147. doi: 10.1136/pgmj.2004.026237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nazroo J.Y., Falaschetti E., Pierce M., Primatesta P. Ethnic inequalities in access to and outcomes of healthcare: analysis of the health survey for England. J Epidemiol Community Health. 2009;63(12):1022–1027. doi: 10.1136/jech.2009.089409. [DOI] [PubMed] [Google Scholar]
- 5.Davidson E., Liu J.J., Sheikh A. The impact of ethnicity on asthma care. Prim Care Respir J. 2010;19(3):202–208. doi: 10.4104/pcrj.2010.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manuel J.I. Racial/Ethnic and gender disparities in health care use and access. Health Serv Res. 2018;53(3):1407–1429. doi: 10.1111/1475-6773.12705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evandrou M. Social inequalities in later life: the socio-economic position of older people from ethnic minority groups in Britain. Popul Trends. 2000;(101):11–18. [PubMed] [Google Scholar]
- 8.European Centre for Disease Prevention and Control Updated rapid risk assessment from ECDC on the novel coronavirus disease 2019 (COVID-19) pandemic: increased transmission in the EU/EEA and the UK. Euro Surveill. 2020;25(10) doi: 10.2807/1560-7917.ES.2020.25.10.2003121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.2020. Department of health and social care (DHSC) and the office for national statistics (ONS) 2020.https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-daily-deaths/ COVID-19 Daily Deaths. Accessed 30th December. [Google Scholar]
- 10.Intensive Care National Audit & Research Centre (ICNARC) 2020. ICNARC report on COVID-19 in critical care england, wales and northern ireland 25 september 2020.https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports/ London: Intensive Care National Audit and Research Centre. Accessed 30th December 2020. [Google Scholar]
- 11.Apea V.J., Wan Y.I., Dhairyawan R. Ethnicity and outcomes in patients hospitalised with COVID-19 infection in East London: an observational cohort study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-042140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrison E.M., Doherty A.B., Barr B. 2020. Ethnicity and outcomes from COVID-19: the ISARIC CCP-UK prospective observational cohort study of hospitalised patients. 2020. Available at SSRN: https://ssrn.com/abstract=3618215. [DOI] [Google Scholar]
- 13.Khunti K., Singh A.K., Pareek M., Hanif W. Is ethnicity linked to incidence or outcomes of covid-19? BMJ. 2020;369:m1548. doi: 10.1136/bmj.m1548. [DOI] [PubMed] [Google Scholar]
- 14.Pareek M., Bangash M.N., Pareek N. Ethnicity and COVID-19: an urgent public health research priority. Lancet. 2020;395(10234):1421–1422. doi: 10.1016/S0140-6736(20)30922-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nazroo J.Y. Bristol University Press; 2002. Patterns of and explanations for ethnic inequalities in health; pp. 87–104. Explaining ethnic differences. [Google Scholar]
- 16.Allik M., Brown D., Dundas R., Leyland A.H. Differences in ill health and in socioeconomic inequalities in health by ethnic groups: a cross-sectional study using 2011 Scottish census. Ethn Health. 2019:1–19. doi: 10.1080/13557858.2019.1643009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pham T.M., Carpenter J.R., Morris T.P., Sharma M., Petersen I. Ethnic differences in the prevalence of type 2 diabetes diagnoses in the UK: cross-sectional analysis of the health improvement network primary care database. Clin Epidemiol. 2019;11:1081–1088. doi: 10.2147/CLEP.S227621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foreman M.G., Willsie S.K., Vincent J.L. Springer-Verlag; Berlin, Germany: 2006. Healthcare disparities in critically ill patients. editorYearbook of Intensive Care and Emergency Medicine. [Google Scholar]
- 19.Foreman M.G., Willsie S.K. Health care disparities in critical illness. Clin Chest Med. 2006;27(3):473–486. doi: 10.1016/j.ccm.2006.04.007. vii. [DOI] [PubMed] [Google Scholar]
- 20.Soto G.J., Martin G.S., Gong M.N. Healthcare disparities in critical illness. Crit Care Med. 2013;41(12):2784–2793. doi: 10.1097/CCM.0b013e3182a84a43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gruer L.D., Millard A.D., Williams L.J. Differences in all-cause hospitalisation by ethnic group: a data linkage cohort study of 4.62 million people in Scotland, 2001–2013. Public Health. 2018;161:5–11. doi: 10.1016/j.puhe.2018.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bansal N., Fischbacher C.M., Bhopal R.S. Myocardial infarction incidence and survival by ethnic group: scottish health and ethnicity linkage retrospective cohort study. BMJ Open. 2013;3(9) doi: 10.1136/bmjopen-2013-003415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhopal R., Steiner M.F., Cezard G. Risk of respiratory hospitalization and death, readmission and subsequent mortality: scottish health and ethnicity linkage study. Eur J Public Health. 2015;25(5):769–774. doi: 10.1093/eurpub/ckv064. [DOI] [PubMed] [Google Scholar]
- 24.Office for National Statistics (ONS) 2008. Harmonised concepts and questions for social data courses: primary standards-ethnic group.https://www.ons.gov.uk/methodology/classificationsandstandards/measuringequality/ethnicgroupnationalidentityandreligion/ Accessed 30th December 2020. [Google Scholar]
- 25.Office for National Statistics (ONS) 2019. English indices of deprivation 2019.https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019/ Accessed 30th December 2020. [Google Scholar]
- 26.2011. Official labour market statistics. LC2101EW-ethnic group by sex by age.https://www.nomisweb.co.uk/query/construct/summary.asp?mode=construct&version=0&dataset=801 Accessed 30th December 2020. [Google Scholar]
- 27.Wan Y., Puthucheary Z., Prowle J. 2020. Comorbid disease and ethnicity in emergency hospital admissions in east London (statistical analysis plan) [DOI] [Google Scholar]
- 28.Gilbert T., Neuburger J., Kraindler J. Development and validation of a hospital frailty risk score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391(10132):1775–1782. doi: 10.1016/S0140-6736(18)30668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gasevic D., Ross E.S., Lear S.A. Ethnic differences in cardiovascular disease risk factors: a systematic review of North American evidence. Can J Cardiol. 2015;31(9):1169–1179. doi: 10.1016/j.cjca.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 30.Lee H., Shin S.H., Gu S. Racial differences in comorbidity profile among patients with chronic obstructive pulmonary disease. BMC Med. 2018;16(1):178. doi: 10.1186/s12916-018-1159-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Primatesta P., Bost L., Poulter N.R. Blood pressure levels and hypertension status among ethnic groups in England. J Hum Hypertens. 2000;14(2):143–148. doi: 10.1038/sj.jhh.1000960. [DOI] [PubMed] [Google Scholar]
- 32.Marmot M., Friel S., Bell R., Houweling T.A., Taylor S., CoSDo H. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 33.Marmot M. Health equity in England: the marmot review 10 years on. BMJ. 2020:m693. doi: 10.1136/bmj.m693. [DOI] [PubMed] [Google Scholar]
- 34.Bhopal R.S., Gruer L., Cezard G. Mortality, ethnicity, and country of birth on a national scale, 2001-2013: a retrospective cohort (scottish health and ethnicity linkage study) PLoS Med. 2018;15(3) doi: 10.1371/journal.pmed.1002515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gruer L., Cézard G., Clark E. Life expectancy of different ethnic groups using death records linked to population census data for 4.62 million people in Scotland. J Epidemiol Community Health. 2016;70(12):1251–1254. doi: 10.1136/jech-2016-207426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stronks K., Kunst A.E. The complex interrelationship between ethnic and socio-economic inequalities in health. J Public Health. 2009;31(3):324–325. doi: 10.1093/pubmed/fdp070. [DOI] [PubMed] [Google Scholar]
- 37.Bécares L., Nazroo J., Albor C., Chandola T., Stafford M. Examining the differential association between self-rated health and area deprivation among white British and ethnic minority people in England. Soc Sci Med. 2012;74(4):616–624. doi: 10.1016/j.socscimed.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 38.Fischbacher C.M., Cezard G., Bhopal R.S. Measures of socioeconomic position are not consistently associated with ethnic differences in cardiovascular disease in Scotland: methods from the scottish health and ethnicity linkage study (SHELS) Int J Epidemiol. 2014;43(1):129–139. doi: 10.1093/ije/dyt237. [DOI] [PubMed] [Google Scholar]
- 39.Bhopal R.S., Bansal N., Fischbacher C.M. Ethnic variations in the incidence and mortality of stroke in the scottish health and ethnicity linkage study of 4.65 million people. Eur J Prev Cardiol. 2012;19(6):1503–1508. doi: 10.1177/1741826711423217. [DOI] [PubMed] [Google Scholar]
- 40.Katikireddi S.V., Cezard G., Bhopal R.S. Assessment of health care, hospital admissions, and mortality by ethnicity: population-based cohort study of health-system performance in Scotland. Lancet Public Health. 2018;3(5):e226–ee36. doi: 10.1016/S2468-2667(18)30068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.