Abstract
Objective:
The Patient Driven Payment Model (PDPM), a new reimbursement policy for Skilled Nursing Facilities (SNFs), was implemented in October 2019. PDPM disincentivizes provision of intensive physical and occupational therapy, however, there is concern that declines in therapy staffing may negatively impact patient outcomes. This study aimed to characterize the SNF industry response to PDPM in terms of therapy staffing.
Design:
Segmented regression interrupted time series.
Setting and Participants:
15,432 SNFs in the United States.
Methods:
Using SNF Payroll Based Journal data from January 1, 2019, through March 31, 2020, we calculated national weekly averages of therapy staffing minutes per patient-day for all therapy staff and for subgroups of physical and occupational therapists, therapy assistants, contract staff, and in-house employees. We used interrupted time series regression to estimate immediate and gradual effects of PDPM implementation.
Results:
Total therapy staffing minutes per patient-day declined by 5.5% in the week immediately following PDPM implementation (P < .001), and the trend experienced an additional decline of 0.2% per week for the first 6 months after PDPM compared with the negative pre-PDPM baseline trend (P < .001), for a 14.7% total decline by the end of March 2020. Physical and occupational therapy disciplines experienced similar immediate and gradual declines in staffing. Assistant and contract staffing reductions were larger than for therapist and in-house employees, respectively. All subgroups except for assistants and contract staff experienced significantly steeper declines in staffing trends compared with pre-PDPM trends.
Conclusions and Implications:
SNFs appeared to have responded to PDPM with both immediate and gradual reductions in therapy staffing, with an average decline of 80 therapy staffing minutes over the average patient stay. Assistant and contract staff experienced the largest immediate declines. Therapy staffing and quality outcomes require ongoing monitoring to ensure staffing reductions do not have negative implications for patients.
Keywords: Skilled nursing facilities, physical therapy, occupational therapy, therapy assistants, workforce, health policy
In October 2019, the Centers for Medicare & Medicaid Services (CMS) instituted a new reimbursement system for skilled nursing facilities (SNFs), replacing a system that had linked daily payments to the volume of rehabilitation services for almost 2 decades.1 Owing to concerns about overprovision of therapy,2 the new payment system, the Patient Driven Payment Model (PDPM), decouples payments from the amount of physical therapy (PT) and occupational therapy (OT), instead basing therapy reimbursement rates on patient clinical characteristics.1
The SNF industry has previously been responsive to CMS payment policy change. Historically, changing reimbursement incentives brought about reductions in therapy provision, reductions in nurse staffing, and changes in how SNFs employed in-house vs contracted therapy staff.3–6 The SNF industry is also dominated by for-profit providers, who have been more likely to reduce therapy provision after prior payment policy changes and to employ higher proportions of lower-paid OT and PT assistants compared to therapists.3,4,7,8 There is also evidence of declines in quality outcomes after previous SNF payment policy changes.5,9 Reductions in therapy staffing and therapy provision under PDPM could have further negative implications for patient outcomes, as higher therapy staffing and more intensive therapy in SNFs are generally beneficial to patients.10–13
Patient-level data on therapy provision will not be available until Fall 2021, 2 years after PDPM implementation.14 This study aims to characterize the SNF industry response in the first 6 months after PDPM implementation by capitalizing on available facility-level data to detect changes in national therapy staffing patterns. We examined patterns in overall therapy staffing and performed subgroup analyses to determine whether changes in staffing differentially affect occupational and physical therapy disciplines, therapists vs therapy assistants, or contractors vs in-house employees.
Methods
Data Sources and Sample
We used Payroll-Based Journal (PBJ) data from January 1, 2019, through March 31, 2020, to measure staffing changes in the first 6 months after PDPM and avoid significant confounding because of the COVID-19 pandemic.15 PBJ files are publicly available and include daily facility-level data on patient census and paid staffing minutes for therapy staff. The PBJ differentiates between therapists vs assistants, and contract vs in-house employees. All Medicare-certified SNFs in the United States except for swing beds are required to submit data to PBJ, which is maintained and audited for accuracy by CMS.15 The PBJ serves as an accurate source of SNF staffing data, as paid staffing hours are easily auditable.16 Data were used from all SNFs reporting PBJ data during the study period.
Variables
We calculated facility-level averages of therapy staffing minutes per patient-day for physical therapists (PTs), occupational therapists (OTs), physical therapist assistants (PTAs), occupational therapy assistants (OTAs), and all therapy staff who were in-house vs contract staff. We then created national weekly averages of staffing minutes per patient-day across all SNFs from January 1, 2019 through March 31, 2020, for a total of 65 weeks in the study period, for the following dependent variables: (1) total staffing: total therapy staffing minutes per patient-day, which includes PTs, OTs, PTAs, and OTAs; (2) PT staffing: physical therapy staffing minutes per patient-day, which includes PTs and PTAs; (3) OT staffing: occupational therapy staffing minutes per patient-day, which includes OTs and OTAs; (4) therapist staffing: therapist staffing minutes per patient-day, which includes PTs and OTs; (5) assistant staffing: assistant staffing minutes per patient-day, which includes PTAs and OTAs; (6) contractor staffing: contract therapy minutes per patient-day, which includes all contract PTs, OTs, PTAs, and OTAs; and (7) in-house staffing: in-house employee therapy minutes per patient-day, which includes in-house PTs, OTs, PTAs, and OTAs.
Analysis
We calculated descriptive statistics for baseline averages of all staffing variables before PDPM implementation (January through September 2019). Then we plotted weekly staffing variables over time to check for linear pre-PDPM trends and detect any seasonality. Our plots demonstrated declines in therapist staffing in weeks containing major national holidays (Thanksgiving, Christmas, New Year’s Day, Memorial Day, and Labor Day). As holidays were not evenly distributed between pre- and post-PDPM time periods, an indicator for holidays was added to our models to adjust for this calendar effect.
We then used segmented regression interrupted time series analysis to determine the effect of PDPM on SNF therapy staffing. Interrupted time series is a strong quasi-experimental design that uses linear regression to establish a baseline trend prior to policy implementation, and then compares the trend after policy implementation to a counterfactual, which is the hypothetical scenario that would have occurred if the policy had not interrupted the continuation of the baseline trend.17 Using interrupted time series, we estimated immediate and gradual effects of PDPM on our staffing variables while accounting for the pre-PDPM trends in each variable by using regression models like the example below:
Models included a continuous variable for overall time in weeks, an indicator for PDPM that reflected whether the observation was pre- or post-PDPM implementation on October 1, 2019, a continuous variable for time in weeks after implementation, and an indicator for major holidays.18 Yt is the average number of therapy staffing minutes per patient per day in week t. The coefficient β2 is the change in level of the variable of interest in the week after PDPM implementation, which can be interpreted as the immediate policy effect.19,20 The coefficient β3 reflects the additional change in weekly trend after PDPM compared to the baseline trend, which can be interpreted as the gradual policy effect.19,20 The error term et represents variability not explained by the model. We plotted model residuals against time to detect autocorrelation and performed the Durbin-Watson test if residual plots indicated potential autocorrelation.21,22 When the Durbin-Watson statistic was not close to 2.0, the Prais-Winsten method was used to adjust for serious autocorrelation.17,19,22
Analyses were conducted using statistical software (RStudio, version 1.2.5019; R Foundation for Statistical Computing, Vienna Austria). This study does not involve human subjects research and is not subject to the University of Washington Institutional Review Board as all data are publicly available and deidentified.
Results
Data were included from 15,432 SNFs that reported data in the PBJ during the entire study period. Serious autocorrelation was detected only for assistant and contractor models, and these models were adjusted. Average baseline therapy staffing minutes per patient-day from January through September 2019, immediate PDPM effect, and gradual PDPM effect for all staffing variables are shown in Table 1.
Table 1.
National Average Therapy Staffing Minutes per Patient-day in Skilled Nursing Facilities (n=15,432) Between January 2019 and March 2020
| January-September 2019 Average | Immediate PDPM Effect: Level Change (95% CI)* | Gradual PDPM Effect: Weekly Change Compared to Baseline Trend (95% CI)* | |
|---|---|---|---|
| Total staffing | 21.7 | −1.2† (−1.7, −0.7) | −0.05† (−0.08, −0.03) |
| PT staffing | 11.5 | −0.6† (−0.8, −0.3) | −0.03† (−0.04, −0.01) |
| OT staffing | 10.2 | −0.6† (−0.8, −0.4) | −0.03† (−0.04, −0.01) |
| Therapist staffing | 9.7 | −0.3‡ (−0.5, −0.1) | −0.04† (−0.05, −0.03) |
| Assistant staffing | 11.9 | −0.9† (−1.2, −0.6) | −0.02 (−0.03, 0.0) |
| Contractor staffing | 13.1 | −1.1† (−1.4, −0.8) | −0.004 (−0.02, 0.02) |
| In-house staffing | 8.6 | −0.1 (−0.3, 0.1) | −0.05† (−0.06, −0.04) |
PDPM, patient driven payment model; CI, confidence interval.
Staffing variables: total staffing, total therapy staffing minutes per patient-day; PT staffing, physical therapy staffing minutes per patient-day; OT staffing, occupational therapy staffing minutes per patient-day; therapist staffing, therapist staffing minutes per patient-day; assistant staffing, assistant staffing minutes per patient-day; contractor staffing, contract therapy minutes per patient-day; in-house staffing, in-house employee therapy minutes per patient-day.
Estimate from level change regression interrupted time series models adjusted for calendar effects of major holidays. Models for assistant and contractor staffing are also adjusted for autocorrelation. Immediate PDPM effect is the change in level of the variable of interest comparing the week before and after PDPM implementation which occurred on October 1, 2019. Gradual PDPM effect is the additional change in the trend in the variable of interest per week after PDPM compared to the baseline trend.
P < .001.
P < .05.
Figure 1 shows weekly total staffing throughout the 65-week study period, with regression lines for the pre- and post-PDPM trends, unadjusted for holidays for ease of interpretation. For adjusted results, the immediate change in national average total staffing after PDPM implementation was −1.2 therapy staffing minutes per patient-day, which equates to a statistically significant 5.5% reduction (P < .001). There was a decline in total staffing in the baseline period, which accelerated downward after PDPM implementation. Compared with the trend prior to PDPM, total staffing declined by an additional 0.05 minutes, or 0.2%, per week after PDPM (P < .001). Immediate and gradual declines totaled 3.2 therapy staffing minutes per patient-day, or a 14.7% reduction by the end of the study period.
Fig. 1.
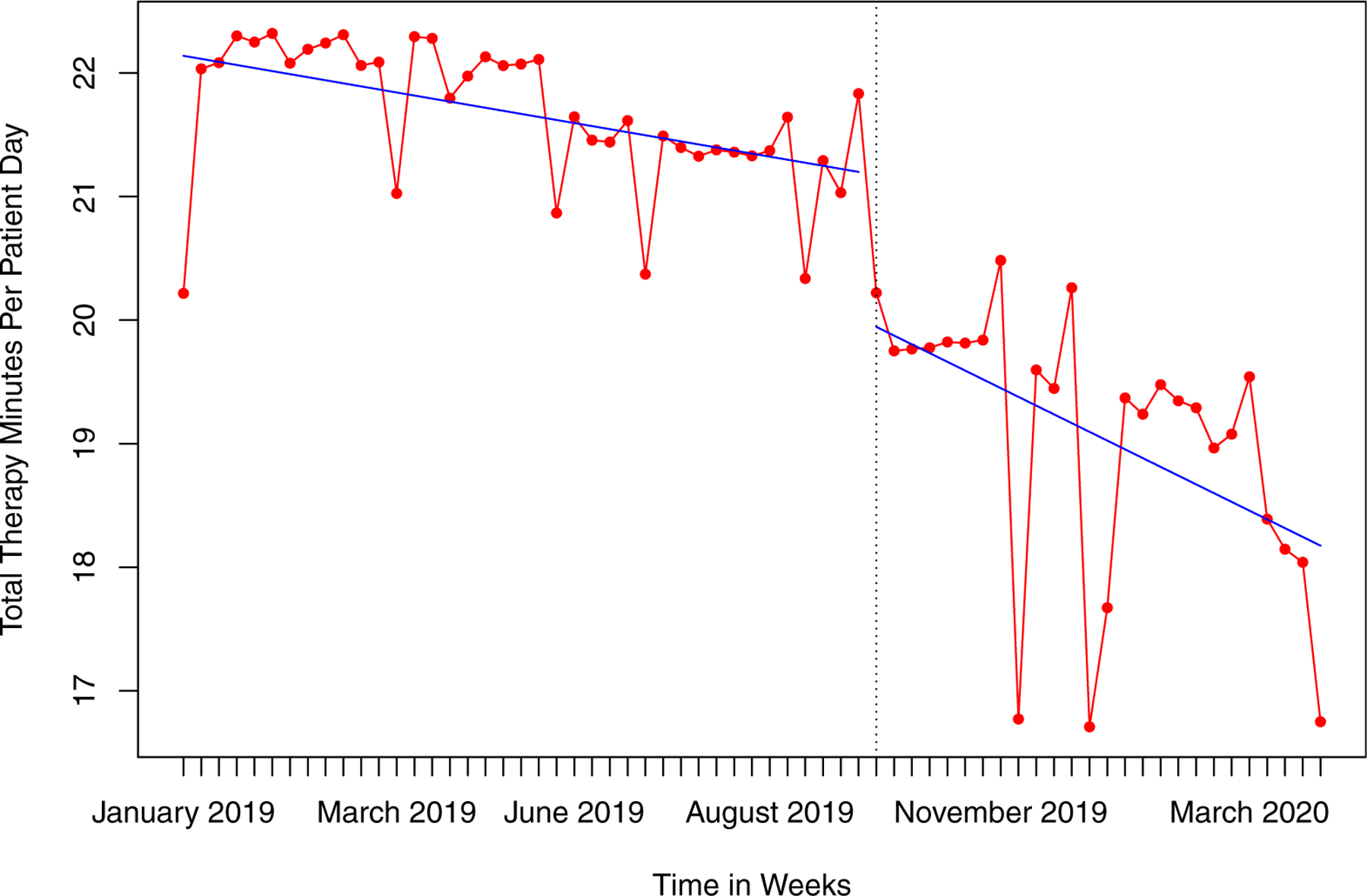
National weekly averages of total therapy minutes per patient-day in skilled nursing facilities between January 1, 2019, and March 31, 2020, with regression lines (blue) demonstrating staffing trends before and after the implementation of the Patient Driven Payment Model (PDPM). Regression lines are unadjusted for calendar effects of major holidays for ease of interpretation.
Most subgroup analyses also demonstrated a statistically significant immediate decline in the level of therapy staffing minutes after PDPM implementation, except for in-house staff (Figure 2). When adjusting for calendar effects and any autocorrelation, immediate declines in staffing minutes per patient-day ranged from 0.3 to 1.1 minutes. These declines corresponded to an immediate 5.1% decline compared to baseline for PT staffing (P < .001), a 5.2% decline for OT staffing (P < .001), a 3.1% decline for therapist staffing (P = .013), and a 7.6% decline for assistant staffing (P < .001). The largest change was for contractor staffing, which declined by 8.4% (P < .001). In contrast, the immediate change in in-house staffing after PDPM was not significant at α = 0.05. Compared with trends before PDPM implementation, all staffing variables except for assistant and contractor staffing demonstrated significantly steeper declines in the trend in staffing over time after PDPM.
Fig. 2.
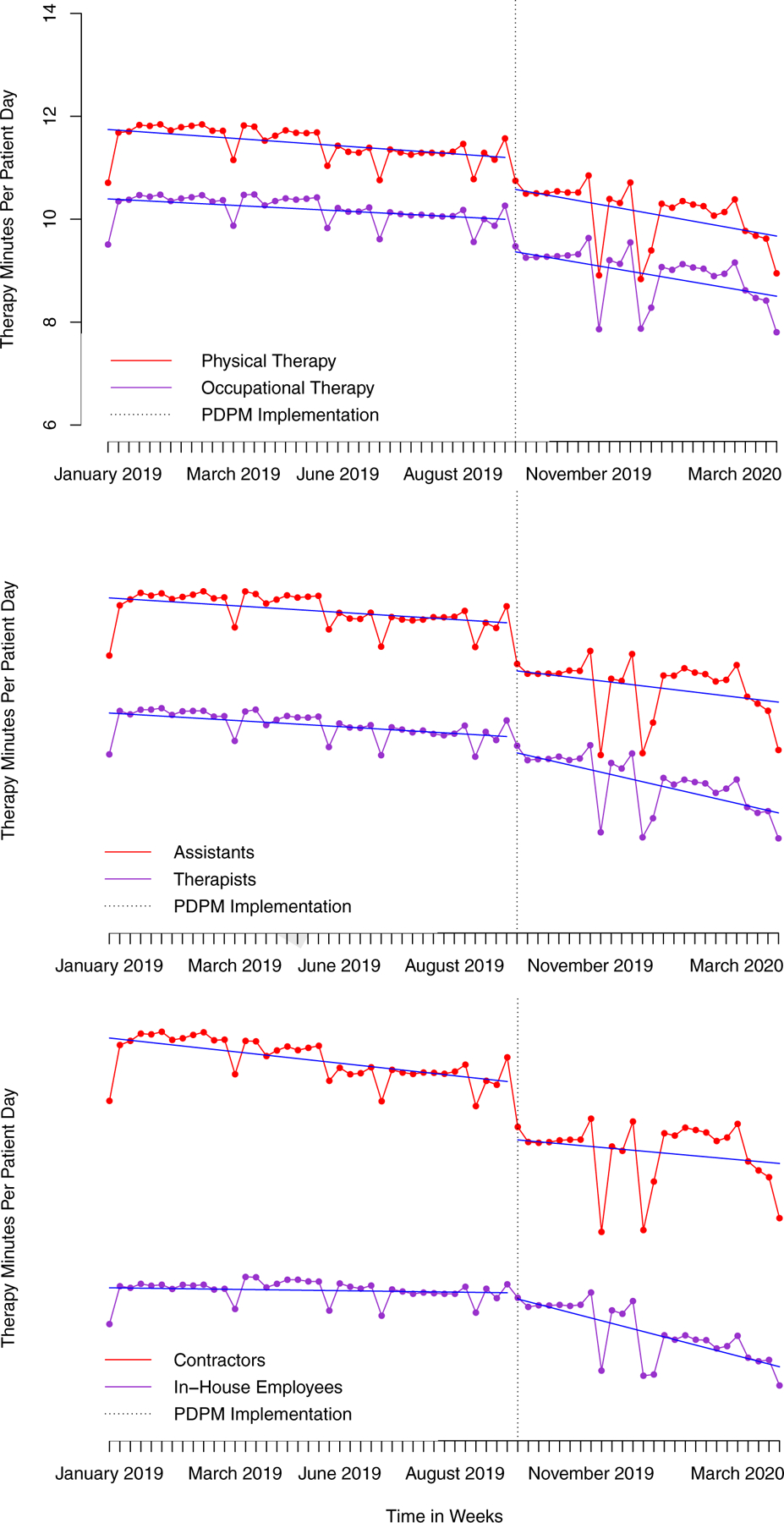
National weekly averages of subgroup analyses of therapy minutes per patient-day in skilled nursing facilities between January 1, 2019, and March 31, 2020, with regression lines (blue) demonstrating staffing trends before and after the implementation of the Patient Driven Payment Model (PDPM). Regression lines are unadjusted for ease of interpretation.
Discussion
This study focused on early national changes in therapy staffing in SNFs before and after PDPM implementation. There was a slight negative trend in staffing prior to PDPM implementation, which may be related to some SNFs reacting to CMS finalizing the PDPM model 1 year prior to policy implementation.1,23 Our analysis demonstrated that, when accounting for baseline negative trends, there was an immediate 5.5% decline in national total therapy staffing in SNFs after PDPM implementation. For an average SNF stay, which is 25 days, this equates to an immediate decline of about 30 minutes of therapy staffing per patient stay, or the duration of 1 typical therapy treatment session.7 There was also an additional decline in therapy staffing trend over time for the first 6 months after PDPM implementation beyond what would have been expected if pre-PDPM trends continued. The immediate and gradual effects of PDPM together equate to a total decline of 80 therapy staffing minutes per average patient stay in the first 6 months after PDPM implementation. This analysis supports media and stakeholder reports24,25 that PDPM had an effect on therapy staffing as well as recent work by McGarry et al26 that showed declines in staffing in the first quarter after PDPM implementation.
Subgroup analyses demonstrated that PT and OT disciplines experienced almost identical PDPM effects, which is unsurprising given the design of the PDPM model, which uses identical patient characteristics to determine payment to SNFs for both PT and OT services.23 Additionally, there were minimal financial incentives for SNFs to reduce staffing of one discipline more than another as national salaries in SNFs are similar across disciplines.27 When comparing therapists of both disciplines to assistants, assistants experienced a larger immediate decline in staffing while therapist staffing minutes declined more steeply over time. The larger immediate decline in assistant staffing may be related to the higher volume of minutes provided by assistants at baseline. SNFs also may have chosen to avoid reducing therapist staffing compared with assistants initially, as therapists must be retained to perform admission and discharge assessments and supervise assistants, who perform only treatments.28
The largest immediate decline in staffing minutes was for contractor staff. However, contractor staffing did not experience further declines in staffing trends over time. Larger immediate drops in contractor staffing may be related to higher costs of employing contractors, and is consistent with previous research demonstrating changes in contractor therapy staffing after previous payment policy reform as well as evidence that SNFs employing exclusively contractor staff are responsive to financial incentives.6,29 The reverse was true for in-house therapy staffing, which did not decline immediately after PDPM but saw the steepest negative change in trend over time.
Limitations
These results are not generalizable to swing bed providers who do not report staffing data to PBJ. Because national data were used, we could not compare trends with a control group. However, limiting the study period to prior to March 2020 reduces the confounding impact of the COVID-19 pandemic and increases confidence that national declines in staffing are attributable to PDPM. Future research must attempt to integrate the dual impacts of payment policy change and the COVID-19 pandemic on service provision and patient outcomes in SNFs. Additionally, therapy staffing minutes cannot directly predict minutes of patient-level therapy provision. Some SNFs may have also increased efficiencies to provide similar levels of therapy as they decreased staffing30; thus, patient-level data must be used when they become available to examine shifts in minutes of therapy provided and patient outcomes associated with PDPM.
Conclusions and Implications
This analysis demonstrated both immediate and gradual declines in national therapy staffing in SNFs in the first 6 months after implementation of new reimbursement policy that disincentivized intensive therapy provision. Although PT and OT disciplines were similarly impacted, therapy assistants and contract staff experienced larger immediate declines than therapists and in-house employees, respectively. Therapy staffing declines occurred despite early reports that per diem reimbursement rates increased in SNFs under PDPM.31,32 Additionally, there is evidence that higher-intensity therapy in SNFs is linked with better quality outcomes for patients.10 Thus, this work highlights the importance of ongoing monitoring and further research to determine whether PDPM was successful in reducing excessive rehabilitation and controlling costs while maintaining patient outcomes.1
Acknowledgments
This publication was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $601,188 with zero percentage financed with nongovernmental sources. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the US Government. For more information, please visit HRSA.gov. https://www.hrsa.gov/grants/manage/acknowledge-hrsa-funding.
This research was supported by the National Institute on Aging of the National Institutes of Health under award number R01AG065371. This content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institute on Aging.
Footnotes
The authors declare no conflicts of interest.
References
- 1.US Department of Health and Human Services. Medicare Program: Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities (SNF) Final Rule for FY 2019, Vol 83. Washington, DC: US Department of Health and Human Services; 2018. [Google Scholar]
- 2.Office of the Inspector General. The Medicare payment system for skilled nursing facilities needs to be reevaluated. Available at: https://www.oig.hhs.gov/oei/reports/oei-02-13-00610.pdf%5Cnhttps://oig.hhs.gov/oei/reports/oei-02-13-00610.pdf.AccessedMarch 14, 2019. Published2015.
- 3.Murray PK, Love TE, Dawson NV, et al. Rehabilitation services after the implementation of the nursing home prospective payment system: Differences related to patient and nursing home characteristics. Med Care 2005;43: 1109–1115. [DOI] [PubMed] [Google Scholar]
- 4.White C Rehabilitation therapy in skilled nursing facilities: Effects of Medicare’s new prospective payment system. Health Aff 2003;22:214–223. [DOI] [PubMed] [Google Scholar]
- 5.Konetzka RT, Yi D, Norton EC, Kilpatrick KE. Effects of Medicare payment changes on nursing home staffing and deficiencies. Health Serv Res 2004;39: 463–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zinn JS, Mor V, Intrator O, et al. The impact of the prospective payment system for skilled nursing facilities on therapy service provision: A transaction cost approach. Health Serv Res 2003;36:1467–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Medicare Payment Policy Commission (MedPAC). Skilled nursing facility services. Report to the Congress: Medicare Payment Policy. Available at: http://www.medpac.gov/-documents-/reports#.AccessedMarch 30, 2020. Published2020.
- 8.Livingstone I, Hefele J, Leland N. Characteristics of nursing home providers with distinct patterns of physical and occupational therapy staffing. J Appl Gerontol 2021;40:443–451. [DOI] [PubMed] [Google Scholar]
- 9.Wodchis WP, Fries BE, Hirth RA. The effect of Medicare’s prospective payment system on discharge outcomes of skilled nursing facility residents. Inquiry 2004;41:418–434. [DOI] [PubMed] [Google Scholar]
- 10.Prusynski RA, Gustavson AM, Shrivastav SR, Mroz TM. Rehabilitation intensity and patient outcomes in skilled nursing facilities in the United States: A systematic review. Phys Ther 2021;101:pzaa230. [DOI] [PubMed] [Google Scholar]
- 11.Jette DU, Warren RL, Wirtalla C. The relation between therapy intensity and outcomes of rehabilitation in skilled nursing facilities. Arch Phys Med Rehabil 2005;86:373–379. [DOI] [PubMed] [Google Scholar]
- 12.O’Brien SR, Zhang N. Association between therapy intensity and discharge outcomes in aged Medicare skilled nursing facilities admissions. Arch Phys Med Rehabil 2018;99:107–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Livingstone I, Hefele J, Nadash P, et al. The relationship between quality of care, physical therapy, and occupational therapy staffing levels in nursing homes in 4 years’ follow-up. J Am Med Dir Assoc 2019;20:462–469. [DOI] [PubMed] [Google Scholar]
- 14.Research Data Assistance Center. Long Term Care Minimum Data Set (MDS). Available at: https://www.resdac.org/cms-data/files/mds-3.0.AccessedOctober 1, 2021.
- 15.Centers for Medicare & Medicaid Services (CMS). Electronic Staffing Data Submission Payroll-Based Journal: Long-Term Care Facility Policy Manual. Washington, DC: US Department of Health and Human Services; 2018. [Google Scholar]
- 16.Geng F, Stevenson DG, Grabowski DC. Daily nursing home staffing levels highly variable, often below CMS expectations. Health Aff 2019;38:1095–1100. [DOI] [PubMed] [Google Scholar]
- 17.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int J Epidemiol 2017;46: 348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kontopantelis E, Doran T, Springate DA, et al. Regression based quasi-experimental approach when randomisation is not an option: Interrupted time series analysis. BMJ 2015;350:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lagarde M How to do (or not to do) … Assessing the impact of a policy change with routine longitudinal data. Health Policy Plan 2012;27:76–83. [DOI] [PubMed] [Google Scholar]
- 20.Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr 2013;13:S38–S44. [DOI] [PubMed] [Google Scholar]
- 21.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299–309. [DOI] [PubMed] [Google Scholar]
- 22.Durbin J, Watson G. Testing for serial correlation in least squares regression. Biometrika 1950;37:409–428. [PubMed] [Google Scholar]
- 23.Acumen LLC. Skilled Nursing Facilities Patient-Driven Payment Model: Technical Report. Burlingame, CA: Acumen, LLC; 2018. [Google Scholar]
- 24.Span P A change in Medicare has therapists alarmed. New York Times. November11, 2019. Available at: https://www.nytimes.com/2019/11/29/health/new-old-age-medicare-physical-therapy.html?searchResultPosition=1. [Google Scholar]
- 25.American Physical Therapy Association. APTA postacute care survey report executive summary. Available at: https://www.apta.org/your-practice/payment/medicare-payment/coding-billing/skilled-nursing-facilities/patient-driven-payment-model/postacute-care-survey-summary.AccessedSeptember 7, 2020. Published2020.
- 26.Mcgarry BBE, White EM, Resnik LJ, et al. Medicare’s new patient driven payment model resulted in reductions in therapy staffing in skilled nursing facilities. Health Aff 2021;40:392–399. [DOI] [PubMed] [Google Scholar]
- 27.US Department of Labor Bureau of Labor Statistics. Occupational employment statistics: Entries for physical therapists, occupational therapists, physical therapist assistants, occupational therapy assistants. Available at: https://www.bls.gov/oes/home.htm.AccessedJanuary 6, 2020. Published2019.
- 28.Centers for Medicare & Medicaid Services (CMS). CMS Manual System: Pub 100–02 Medicare Benefit Policy: Therapy Personnel Qualifications and Policies Effective January1, 2008. Washington, DC: US Department of Health and Human Services; 2008. [Google Scholar]
- 29.Prusynski RA, Frogner BK, Dahal A, et al. Skilled nursing facility characteristics associated with financially motivated therapy and relation to quality. J Am Med Dir Assoc 2020;21:1944–1950.e3. [DOI] [PubMed] [Google Scholar]
- 30.Gustavson AM, Forster JE, LeDoux CV, Stevens-Lapsley JE. Multiparticipant rehabilitation in skilled nursing facilities: An observational comparison study. J Am Med Dir Assoc 2020;21:1920–1925. [DOI] [PubMed] [Google Scholar]
- 31.Medicare Payment Advisory Commission (MedPAC). Report to the Congress: Medicare Payment Policy. Vol March.Washington, DC: MedPAC; 2021. [Google Scholar]
- 32.Zimmet Healthcare Services Group. PDPM Reimbursement Analysis, November Claims: Projected v. Realized Performance in the Context of Healthcare Reform Morganville, NJ: Zimmet Healthcare Services Group; 2020. [Google Scholar]


