Abstract
Background:
Alcohol cessation improves mortality in alcohol-associated liver disease (ALD), but access to treatment is limited. To address this gap, implementation and early feasibility and outcomes of a multidisciplinary ALD clinic are described.
Methods:
The clinic comprised a hepatologist, psychiatrist, psychologist, nurse, and social worker. Patients included those with alcohol-associated cirrhosis or acute alcoholic hepatitis who were not in the transplant evaluation process, who had less than 6 months’ sobriety and willingness to engage in alcohol use treatment. Psychosocial metrics in addition to routine hepatic function labs were collected. Treatment plans were tailored based on patient preferences and needs after multidisciplinary discussion.
Results:
89 patients were referred from both inpatient and outpatient settings, with 51 seen during the initial year. 38 remained active in clinic (4 died, 6 discharged, 3 moved to transplant clinic). 55% were women, 88% were white, 61% had private insurance. 49% had alcoholic hepatitis. 71% were decompensated. 80% had severe alcohol use disorder (AUD) and 84% had at least 1 comorbid psychiatric or substance use disorder. 63% chose one-on-one AUD treatment, 57% were prescribed relapse prevention medications. Mean MELD-Na score improved from baseline of 14 (SD 6.6) to 11.3 at 6 months (p=0.01). Hospital utilization significantly declined when comparing 6 months before to 6 months after initial visit (emergency department visits: 0.51 to 0.20 per person-month; inpatient admission: 0.34 to 0.14 per person-month; (β= −0.89, 95% CI −1.18 to −0.60).
Conclusions:
A multidisciplinary ALD clinic showed feasibility and encouraging early outcomes. Further research should explore ways to expand this model and increase clinic capacity.
Keywords: alcoholic cirrhosis, psychiatry, addiction, alcohol use disorder, quality
1. Introduction1
The prevalence of alcohol-associated liver disease (ALD) has markedly increased throughout the United States (US) as well as globally in the last decade. While rates of ALD remain highest among older men, recent increases are most pronounced among women and young people, with mortality from ALD rising most rapidly in those ages 25–34 (Mellinger et al., 2018, Mellinger, 2019, Tapper and Parikh, 2018). The ALD epidemic is driven by an increase in alcohol use disorder (AUD) globally and in the US, particularly among young people ages 18–29, and more so in women than in men (Grant et al., 2017).
Treatment of ALD patients is complex, involving medical management of liver disease and other comorbidities and of underlying psychological problems and addiction. In addition to counseling, alcohol relapse prevention medications are effective for alcohol cessation, but ALD patients infrequently receive such medications (Mellinger et al., 2019). Hepatology society guidelines recommend referral to AUD treatment for all advanced ALD patients, but access remains low (Mellinger et al., 2019, Crabb et al., 2020). To bridge these gaps in care, quality metrics for ALD include routine screening for alcohol use and referral to AUD treatment (Kanwal et al., 2019). Integrated medical-psychiatric care is recommended by the AASLD as a primary means of effective ALD management and is crucial for advanced ALD patients, who may focus solely on their liver disease, not recognizing the importance of mental health care as well (Crabb et al., 2020).
A multidisciplinary ALD clinic links hepatology care with easier access to necessary mental health and addiction care (Winder et al., 2019). However, very few centers delivering hepatology care provide such integrated care outside of transplant programs due to resource constraints, lack of dedicated staff with appropriate expertise, and insurance restrictions, as well as other barriers. In July 2018, the multidisciplinary Michigan Alcohol Improvement Network (MAIN) ALD clinic was established with the goal of increasing access to AUD treatment for patients with advanced ALD. Herein, the implementation, feasibility, and early outcomes of this clinic are described.
2. Methods
2.1. Clinic Structure
The inception and operation of the ALD clinic has been described in detail elsewhere (Winder et al., 2019). The clinic is composed of a hepatologist [JLM], psychologist [ACF], psychiatrist [GSW], nurse [AJ], social worker [KK] who share common goals and visions for AUD and ALD treatment, which are essential for successful relationship building in multidisciplinary collaboration. The clinic operates one half-day 2–3 times per month, and is located in the Transplant Clinic utilizing its space as well as staff for clinic operations.
2.2. Referral process and patient population
Currently, the clinic accepts internal referrals only. Referred patients must satisfy 3 requirements: 1) clinical or biopsy-proven alcohol-associated cirrhosis or acute alcoholic hepatitis, 2) active drinking of any amount within the last 6 months, and 3) willingness to speak with mental health clinicians. Patients are not required to commit to any length of AUD treatment nor are they required to be abstinent. Inclusion criteria are limited to those with more advanced ALD to focus on those most in need of hepatology care and potential transplantation. Patients with comorbid liver disease are eligible for referral and are treated according to standard-of-care. Patients who, at the time of referral, have an open evaluation in the liver transplant clinic, are listed for transplant, or who had received a liver transplant in the past are excluded because these patients already have access to mental health care via the transplant program. The referral process is detailed in Supplemental Figure 1. Patients who lack insurance coverage for clinic AUD treatment providers are scheduled to be seen in the general hepatology clinic. Patients are discharged from clinic any time after their first visit if they no longer want AUD treatment, are physically or verbally abusive to clinic staff, or begin evaluation for liver transplantation.
2.3. Clinic operations
During each half-day clinic, 2–3 new patients are evaluated by hepatology, psychiatry, and either psychology or social work. To maximize utility of clinic services, social work calls each patient ahead of the clinic appointment to encourage attendance. At the initial visit, each new patient receives a printed instructional booklet authored specifically for this clinic containing information about liver health, alcohol education and treatment, behavioral coping strategies, diet and nutrition, and medication management. Each patient undergoes a thorough review of social, past medical, psychiatric, and substance use histories, physical and mental status examinations, and laboratory tests. Psychometric instruments, detailed below, are used to gauge baseline symptoms of mood, anxiety, sleep, alcohol and drug use.
Treatment planning is personalized as efforts are made throughout each evaluation not only to assess patient readiness and AUD treatment preferences but also to actively engage patients toward making changes. All clinic staff, including nursing, have been trained in motivational interviewing (Miller and Rollnick, 2013). The team meets at the end of each clinic session to review the patients seen that day. Treatment plans include combinations of hepatology care with assorted options of psychotherapy and psychopharmacology within the clinic and in the patient’s community. Clinic providers often refer to higher tiers of AUD care (intensive outpatient programs, residential rehabilitation) when needed and in accordance with patients’ insurance coverage. Clinic providers also use telemedicine visits, where available and reimbursable by insurance, to reach patients with limited access to clinic care or local AUD/mental health care.
In addition to meetings on patient care at the end of each clinic session, the clinic team regularly meets (1–2 times monthly) to review patient census and, using interval patient data, to strategize on next steps for each patient. These meetings provide opportunities for cross-training on each provider’s unique knowledge bases and skill sets, implementing quality improvements, exchanging research ideas, and collaborating on publications and grant proposals. The clinic is designed to collect data for use in joint clinical, educational, and research missions.
2.4. Data Collection and Outcome Definitions
All patients undergo routine lab testing at the first visit. Additional tests are performed as deemed medically necessary. Labs are repeated every 3–6 months and more often if clinically indicated. Model for End-Stage Liver Disease –Sodium (MELD Sodium) scores are calculated for each patient. All patients undergo screening for alcohol and drug use with urine ethyl glucuronide, drug screens, and cotinine, and serum phosphatidylethanol at baseline and at each subsequent return visit, with interval testing as clinically necessary.
Diagnosis of psychiatric and substance use disorders are made by psychiatry, psychology and social work (GSW, ACF, KK) based on established psychiatric criteria (American Psychiatric Association. and American Psychiatric Association. DSM-5 Task Force., 2013). History of prior and current AUD treatment is determined based on review of clinic notes and patient interview. Abstinence is defined as the lack of any alcohol consumption and is determined by patient interview at the time of clinic visits or phone follow-ups, negative results of alcohol biomarker tests and review of medical records. A positive alcohol biomarker in the absence of any known false-positive exposure is counted as a break in abstinence with re-start of abstinence time at that point. Structured psychometrics (see Table 1) (Spitzer et al., 1999, Spitzer et al., 2006, Bohn et al., 1995, Skinner, 1982, Bastien et al., 2001) are used at initial evaluation and subsequent return visits and are interpreted according to each instrument’s validated cutoffs to inform care decisions.
Table 1.
Demographics of MAIN clinic patients at time of initial evaluation. Results expressed as N(%) or mean (standard deviation)
| Total N=51 | Women N=28 (55%) | Men N=23 (45%) | P value | |
|---|---|---|---|---|
|
| ||||
| Age, years | 47 (11.2) | 46 (12.3) | 48 (9.8) | 0.48 |
|
| ||||
| Ethnicity | ||||
| -Non-Hispanic | 49 (96%) | 28 (100%) | 21 (91%) | 0.28 |
| -Hispanic | 1 (2%) | 0 | 1 (4%) | |
| -Declined | 1 (2%) | 0 | 1 (4%) | |
|
| ||||
| Race | ||||
| -White | 45 (88%) | 27 (96%) | 18 (78%) | 0.06 |
| -Black | 3 (6%) | 0 | 3 (13%) | |
| -Asian | 1 (2%) | 1 (4%) | 0 | |
| -Declined | 2 (4%) | 0 | 2 (9%) | |
|
| ||||
| Marital Status | ||||
| -Single | 20 (39%) | 10 (36%) | 10 (43.5%) | 0.85 |
| -Married | 24 (47%) | 14 (50%) | 10 (43.5%) | |
| -Divorced | 7 (14%) | 4 (14%) | 3 (13) | |
| -Widowed | 0 | 0 | 0 | |
|
| ||||
| Have children | ||||
| -Yes | 16 (32%) | 9 (32%) | 7 (30%) | 0.99 |
| -No | 20 (39%) | 11 (39%) | 9 (39%) | |
| -Declined | 15 (29%) | 8 (29%) | 7 (30%) | |
|
| ||||
| Insurance | ||||
| -Medicare | 6 (12%) | 2 (7%) | 4 (17%) | 0.41 |
| -Medicaid | 13 (25%) | 7 (25%) | 6 (26%) | |
| -Private | 31 (61%) | 19 (68%) | 12 (52%) | |
| -None | 1 (2%) | 0 | 1 (4%) | |
|
| ||||
| Alcohol-associated cirrhosis | 26 (51%) | 13 (46%) | 13 (56%) | 0.47 |
|
| ||||
| Alcoholic hepatitis | 25 (49%) | 15 (54%) | 10 (44%) | 0.47 |
|
| ||||
| Ascites | 34 (67%) | 20 (71%) | 14 (67%) | 0.43 |
|
| ||||
| Variceal bleed | 10 (20%) | 6 (21%) | 4 (17%) | 0.72 |
|
| ||||
| Hepatic encephalopathy | 25 (49%) | 11 (39%) | 14 (61%) | 0.12 |
|
| ||||
| Decompensated | 36 (71%) | 20 (71%) | 16 (70%) | 0.89 |
|
| ||||
| BMI (kg/m2) | 26 (4.9) | 25.6 (5.2) | 27.2 (4.6) | 0.25 |
|
| ||||
| AST (U/L) | 96 (73) | 98 (67) | 92 (81) | 0.78 |
|
| ||||
| ALT (U/L) | 60 (43) | 51 (25) | 69 (57) | 0.17 |
|
| ||||
| Alkaline Phosphatase (U/L) | 168 (81) | 168 (78) | 169 (86) | 0.97 |
|
| ||||
|
| ||||
| Total bilirubin (mg/dL) | 3.9 (4.7) | 3.7 (5.1) | 4.1 (4.3) | 0.74 |
|
| ||||
| Albumin (g/dL) | 3.7 (0.7) | 3.8 (0.7) | 3.7 (0.7) | 0.53 |
|
| ||||
| Sodium (mmol/L) | 137 (4.1) | 137 (3.2) | 137 (5.1) | 0.77 |
|
| ||||
| Creatinine (mg/dL) | 0.81 (0.18) | 0.80 (0.21) | 0.82 (0.14) | 0.72 |
|
| ||||
| Platelets (1000/uL) | 167 (80) | 177 (81) | 155 (78) | 0.32 |
|
| ||||
| INR | 1.3 (0.26) | 1.3 (0.25) | 1.3 (0.27) | 0.50 |
|
| ||||
| MELD-Na | 14.1 (6.6) | 13.1 (6.2) | 15.3 (7.0) | 0.27 |
|
| ||||
| Psychiatric Diagnoses | ||||
|
| ||||
| Anxiety | 37 (73%) | 23 (82%) | 14 (61%) | 0.09 |
|
| ||||
| Depression | 17 (33%) | 9 (32%) | 8 (35%) | 0.84 |
|
| ||||
| Bipolar | 1 (2%) | 0 | 1 (4%) | 0.26 |
|
| ||||
| Trauma | 14 (27%) | 9 (32%) | 5 (22%) | 0.41 |
|
| ||||
| Other* | 12 (23%) | 8 (29%) | 4 (17%) | 0.35 |
|
| ||||
| None | 8 (16%) | 4(14%) | 4 (17%) | 0.76 |
|
| ||||
| DAST@ | 1.34 (2.27) | 1.15 (2.03) | 1.54 (2.57) | 0.66 |
|
| ||||
| ISI@ | 11.2 (8.3) | 13.1 (8.2) | 9.6 (6.9) | 0.22 |
|
| ||||
| Substance Use Diagnoses | ||||
|
| ||||
| AUD | ||||
| -moderate | 10 (20%) | 6 (21%) | 4 (17%) | 0.72 |
| -severe | 41 (80%) | 22 (79%) | 19 (83%) | |
|
| ||||
| Tobacco | 26 (51%) | 14 (50%) | 12 (52%) | 0.88 |
|
| ||||
| Marijuana | 33 (65%) | 17 (61%) | 16 (70%) | 0.51 |
|
| ||||
| Opioids | 9 (18%) | 4 (14%) | 5 (22%) | 0.49 |
|
| ||||
| Cocaine | 12 (23%) | 9 (32%) | 3 (13%) | 0.11 |
|
| ||||
| Other@ | 7 (14%) | 4 (14%) | 3 (13%) | 0.89 |
|
| ||||
| None | 8 (16%) | 5 (18%) | 3 (13%) | 0.64 |
Trauma defined as psychological trauma resulting from a distressing event. “Other” includes personality disorders and eating disorders.
Number of psychometrics completed: PHQ9: n=32, GAD7: n=31, AUDIT: n=28, ISI: n=30
A clinic visit is defined as a day a patient came to at least one appointment with a clinic provider. On many clinic visits, patients will see more than one provider. Clinic treatment engagement is reported as the median and mean number of ALD clinic visits completed. Due to differential follow-up times, emergency department and inpatient utilization are reported as visits per person-month in the 6 months before and after initial evaluation. Medical records were reviewed for the period 6 months prior to and up to 6 months following initial clinic evaluation. Michigan Medicine utilizes the EPIC electronic health record. All available outside records accessible through EPIC Care Everywhere and Great Lakes Health Consortium (which connects electronic health records in over 117 health systems in the state of Michigan) were also searched. ER visits and hospital admissions at outside facilities were queried at each clinic visit and recorded in clinic notes. Completed clinic visits, no-shows, and cancellations were determined based on query of these electronic health records.
2.5. Patient Feedback Surveys
Structured qualitative surveys of all patients seen at least once in the ALD clinic were conducted by phone after their initial visit by a member of the clinic team (JB) to gain patient perspective on the clinic structure, personnel, flow, and effectiveness. See Supplemental Information for structured survey questions and summary of patient responses. Surveys were completely de-identified to preserve patient confidentiality. Responses were transcribed at time of interview.
2.6. Statistical Analysis
Descriptive statistics were calculated for all variables, using Chi-squared and t-tests as appropriate for categorical or continuous variable comparisons. Pre- and post-clinic admission variables to inpatient or emergency departments were calculated using rate per patient-month of follow-up. All patients, regardless of length of follow-up before and after initial visit, were included. Logistic regression for categorical or dichotomous variables and Poisson regression for count variables was used in regressions, as appropriate. Generalized estimating equations using mixed-effects Poisson regression to account for variable follow-up timeframes was additionally used to analyze unadjusted pre- and post-clinic visit hospital and ED utilization data. In all cases, except admissions, only cases with complete data for the given time point were analyzed. A statistical significance level of α = 0.05 was used. Data was analyzed using STATA-MP version 13 (StataCorp, College Station TX).
3. Results
Referral process:
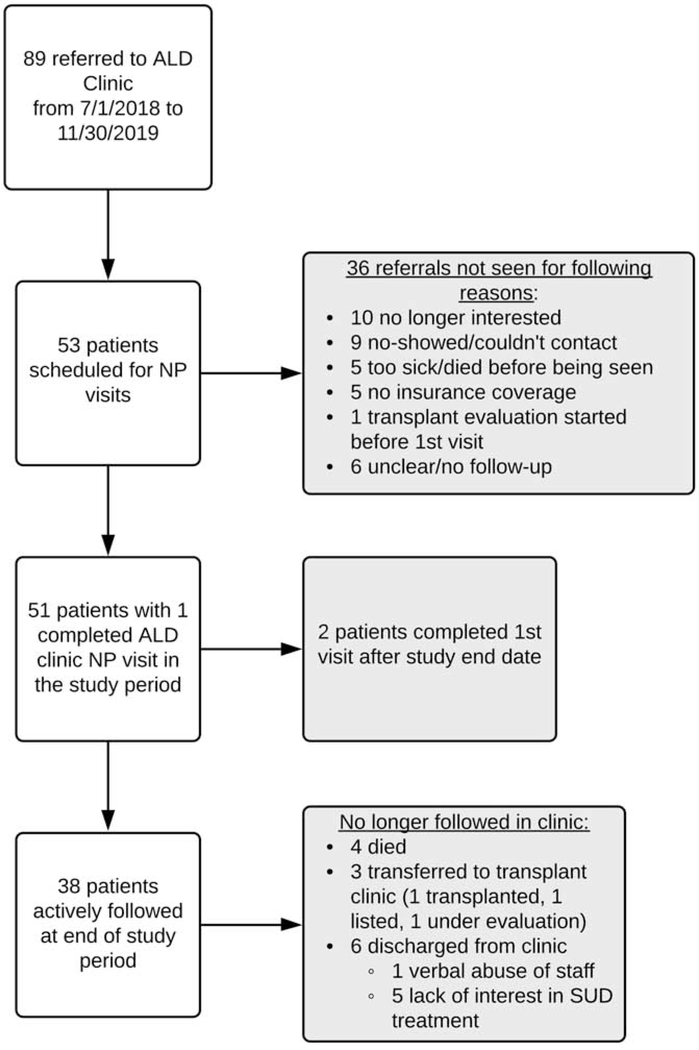
89 referrals from both inpatient and outpatient settings within the healthcare system were received over the study timeframe from July 1, 2018 through November 30, 2019 (see Figure 1). The most common reason for lack of referral completion was a ‘lack of interest’ in clinic attendance (ten patients) (see Figure 1 for further reasons for lack of referral). Nine patients no-showed or cancelled and did not reschedule, while five patients died before they could be seen in clinic. Only five patients could not be seen due to lack of insurance coverage. Of the thirty-six patients who did not attend their scheduled visit, the average age was 49 years (range 28–71), eleven (30%) were women, eighteen (50%) has decompensated cirrhosis, sixteen (42%) alcoholic hepatitis and two did not have advanced ALD (incorrect referrals). Among these thirty-six patients, eleven (30%) died within one year after their referral and ten of these eleven died within 6 months of referral. All patients referred were already connected to medical care. Hepatologists referred the largest proportion of patients, (n=61; 69%) followed by primary care (n=12), hospitalists (n=9), and other (cardiology n=1; rheumatology n=2; gastroenterology n=4).
Fig. 1.
Population and referral process.
3.1. Population Characteristics
Characteristics of the fifty-one patients who completed a new patient visit during the study timeframe are included in Table 1. Slightly more than half (n=29; 55%) were women, average age was 47 years, 88% were Caucasian, and 47% were married. Approximately half (n=26; 51%) had alcohol-associated cirrhosis alone and the remaining half (n=25; 49%; 10 men and 15 women) had alcoholic hepatitis; of the latter, twenty patients also had clear evidence of alcohol-associated cirrhosis. Fourteen had a comorbid liver disease in addition to ALD (1 hepatitis B, 4 hepatitis C, 10 non-alcoholic steatohepatitis, 1 primary biliary cholangitis). Most, (n=36; 71%) had hepatic decompensation. The mean MELD-Na score was 14.0 (SD=6.5), with no difference between men and women (15.4 vs 13.1, p=0.27). Comorbid psychiatric and/or substance use disorders were present in 84% of patients; 73% had an anxiety disorder and 33% had depression. More women than men had an anxiety disorder, though the difference was not significant (p=0.09). As expected, the majority of patients (80%) had severe AUD.
3.2. Outcomes
3.2.1. Alcohol Use Treatment and Sobriety
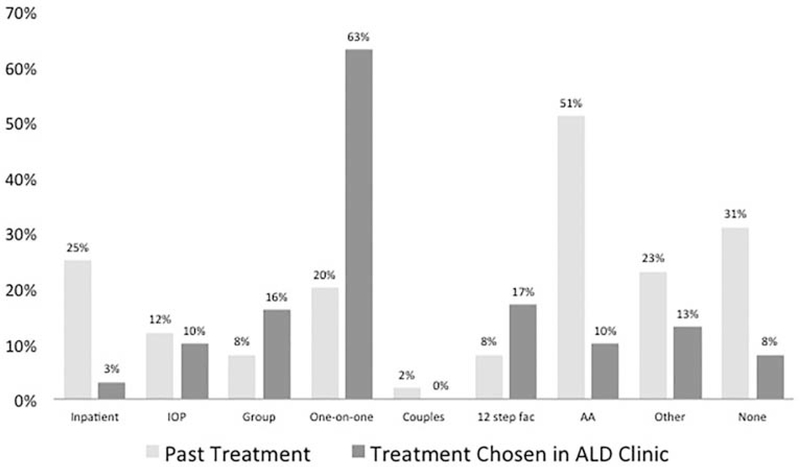
Thirty-five patients (68%) had a prior history of AUD treatment (see Figure 2). No difference between men and women in receipt or type of AUD treatment in the past was seen, except for more frequent use of intensive outpatient therapy by men (n=5; 22%) relative to women (n=1; 4%; p=0.04].
Fig. 2.
Treatment modalities used before initial evaluation in clinic compared with treatments chosen at initial evaluation in ALD clinic. IOP: intensive outpatient program; 12 step fac: 12 step facilitation; AA: Alcoholics Anonymous
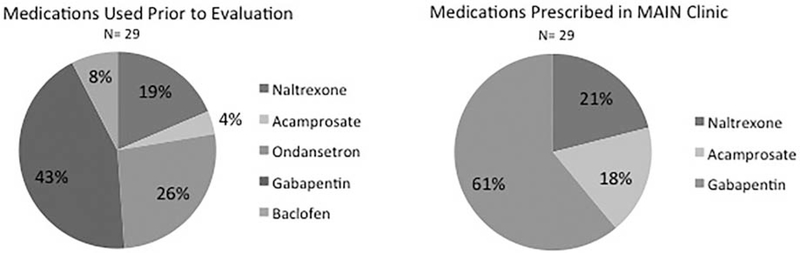
After their initial clinic visit, patient preference for one-on-one therapy increased compared to pre-clinic treatment utilization (20% prior versus 63% after), while there was a decline in those who chose Alcoholics Anonymous compared to those who reported having used this modality prior to the clinic visit (51% to 10%; see Figure 2). Twenty-nine patients (57%; n=19 women, n=10 men; p =0.08) had a relapse prevention medication prescribed at some point prior to their initial evaluation with fourteen patients on relapse prevention medications at the time of their initial visit (see Figure 3). Twenty-nine patients were prescribed alcohol relapse medications after the initial visit (see Figure 3). Of these twenty-nine patients, eighteen were prescribed gabapentin followed by six prescribed naltrexone and five prescribed acamprosate.
Fig. 3.
Relapse prevention medications prescribed before and after initial evaluation in clinic
At initial evaluation, mean abstinence time was 58 days (SD=65) and median was 48 days (range, 0–334; n=57 women, n=59 men; p=0.89), with twenty-two (43%) patients having less than 30 days of abstinence. Thirty-six patients had abstinence data at 3 months and twenty-eight had data at 6 months. Factors associated with less than 30-day abstinence at evaluation were alcohol-associated cirrhosis without alcoholic hepatitis (p=0.03) and a lack of decompensating symptoms (p=0.03). Being married was the only factor associated with higher likelihood of alcohol abstinence at 3 months (p=0.03) while patients with depression (p=0.04) and relapse prevention medications (p<0.001) were associated with lower likelihood of abstinence. There were no factors associated with abstinence at 6 months, though decompensation’s association with a greater likelihood of 6-month abstinence approached significance (p=0.05).
Thirty patients had follow-up labs at 3 months and twenty-five patients had full labs at 6 months. MELD scores were available at 3 months for twenty-five patients and at 6 months for twenty-one patients. There were statistically significant decreases for mean ALT at 3 months (72 vs 49, p=0.02) and 6 months (58 vs 42, p=0.04), alkaline phosphatase at 3 months (181 vs 151, p=0.02), total bilirubin at 6 months (3.8 vs 2.1, p=0.02), and MELD at 6 months (14.1 vs 11.8, p=0.03). All other comparisons were non-significant.
3.2.2. Survival and Retention in Clinic
Thirty-eight (75%) (15 men and 23 women) remained actively followed in the clinic. Four patients (2 men and 2 women) died. Two died within 3 months and two others more than 6 months after initial visit (n=3 from cirrhosis complications and n=1 from unknown cause). Six were discharged, one for being verbally abusive to staff and five for lack of desire to engage in any AUD treatment. Three patients were transferred to the liver transplant clinic and were no longer actively followed in the MAIN clinic.
3.2.3. Utilization outcomes
The mean number of visits completed was 4.4 (SD=5.7) and median was 3 (range 1–29) over the study timeframe. Higher numbers of visits in some patients were due to more frequent (weekly or biweekly) therapy visits with psychology or psychiatry providers. Women tended to complete more visits than men, though this was not significant (women: 5.5, SD=7.0; men: 3.0, SD=3.4; p=0.11). There was a mean of 0.84 no-shows (SD=1.47) and 2.14 cancellations (SD=2.02) per person over the study period. There was a lower likelihood of abstinence among those with more no-shows or cancellations at 3 months (OR=0.74) and at 6 months (OR=0.69) (p=0.04 for both).
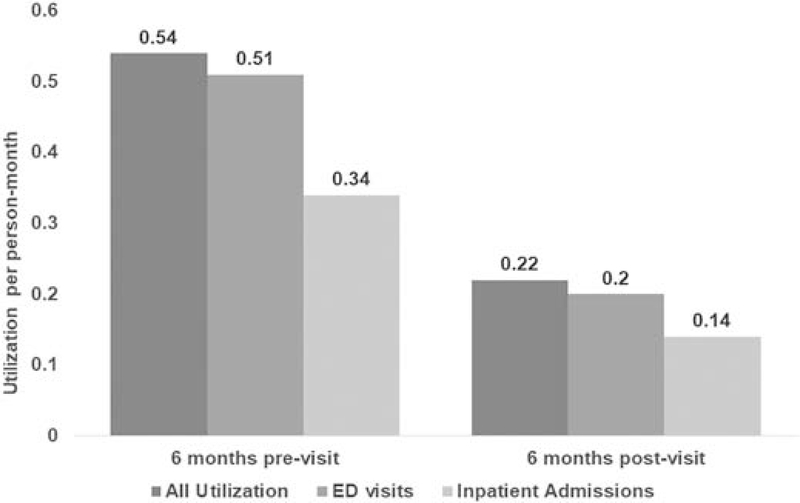
Inpatient admissions and ED utilization substantially decreased in the 6-month period after the initial visit, compared to the 6 months prior (see Figure 4). The median number of hospital admissions decreased from 0.34 to 0.14 per person-month and the median number of ED visits from 0.51 to 0.20 per person-month. On mixed-effects, unadjusted regression accounting for differences in pre- and post-visit follow-up time, there was a significant decrease in admissions at 6 months following the initial clinic visit (β=−0.89, 95% CI −1.18 to −0.60). There was no significant association between the number of completed clinic visits and the number of post-clinic visit inpatient admissions or ED visits within 6 months.
Fig. 4.
Rates of hospital admissions and ER utilization per person-month follow-up.
4. Discussion
In this report of the successful implementation of a multidisciplinary ALD clinic, clinic development and implementation was feasible with encouraging early outcomes, particularly ED and inpatient utilization, which decreased by over 50% during the 6-month period following the initial visit.
The experience described here and in an earlier report (Winder et al., 2019) provides a blueprint for how to implement a multidisciplinary clinic in a real-world setting. Building and implementing the clinic involved a multi-year process of relationship-building, beginning with clinic providers and building outward to encompass each respective department. Ensuring that academic departments and clinical units were supportive was a major factor in the initial success of the clinic. Responsiveness to patient feedback was also critical and clinic providers made changes to clinic structure based on this feedback, including implementing a pre-clinic call by a social worker (KK) to clarify the purpose and nature of the visit and attempt to alleviate any barriers to patients coming to their first appointment. Iterative feedback and process evaluation cycles, occurring during biweekly clinic operations meetings, were critical to maintaining an effective multidisciplinary ALD clinic.
Most patients had a comorbid psychiatric and substance use illness, in addition to an alcohol use disorder. Multiple, often complex, psychiatric illness combined with advanced liver disease highlights the need for a multidisciplinary approach. Quality care for ALD includes referral to mental health providers for AUD treatment (Kanwal et al., 2019) but this rarely happens (Mellinger et al., 2019). Integration of mental health care with hepatology care has been reported before but often in the context of a clinical trial less reflective of the “real-world” (Khan et al., 2016). Integrating clinical care is widely practiced in other specialties, as well as in liver transplant, and has been shown to produce lower rates of emergency and inpatient admissions, a finding consistent with our results (Wakeman et al., 2019).
The clinic was able to see 4% of all patients with advanced ALD in our health system during study timeframe, despite operating only one half-day every other week, and 7% were referred. For several reasons, some patients did not attend the scheduled visits. Early results showed that patients who remained connected to the clinic had longer duration of abstinence, and demonstrated small but significant associations between abstinence and fewer no-shows or cancellations. However, the effect of the clinic was not solely related to receipt of hepatology care or medical care as over two-thirds of patients were referred from other hepatologists and primary care providers.
Clinic providers used a broad range of AUD treatment modalities, including one-on-one treatment (which was the most popular amongst patients), group therapy referrals, and, for those requiring a higher level of care, intensive outpatient programs and residential rehabilitation referrals and connections. Relapse prevention medications were used in roughly half of patients both before and after the clinic visit, a larger percentage than reported in prior literature (Mellinger et al., 2019). The integrated nature of the clinic allows for carefully selection and dosing of medications for AUD and other underlying psychiatric conditions, and to close monitoring for side effects.
Inpatient and ED utilization markedly decreased, similar to studies of integrated mental health and primary care clinics (Wakeman et al., 2019). This decrease cannot be attributed to the effect of initiating medical care, as 83% of our referrals came from intramural hepatology or primary care. Reasons for the decrease are not completely clear given the retrospective nature and small sample size, but could be related to the effect of mental health and substance use care and treatment provided by a multidisciplinary team. A larger prospective study designed to assess the causative influence of our multidisciplinary clinic structure would be necessary to fully determine any causal effect of the clinic structure on outcomes. As previously reported, the one-year cost for clinic implementation was $78,300 (Winder et al., 2019). In other studies, the average cost per hospital stay for a patient with advanced ALD ranges from $9887 to $27,7292. As a result, cost savings from reduced inpatient utilization may be realized by implementing an ALD clinic in health systems accountable for population-level care, but more data from larger prospective studies are needed to fully support this conclusion.
Data was limited by the retrospective nature and small sample size, and lack of a control group for comparison. Thus, outcomes should be interpreted with caution. The analysis could not account for potential confounders including, but not limited to, patient self-selection bias. As has been reported in other clinical trials with advanced ALD patients, follow-up is challenging in this population (Comerford et al., 2017), with similar loss to follow-up at 3 and 6 months, limiting ability to provide reliable estimates of all clinic effects. Increased clinic capacity for more frequent appointments will help accelerate establishment of rapport and treatment alliances and allow providers to capitalize on increases in patient motivation, which can wane over time. Implementing an inpatient alcohol consultation service with rapid engagement, referral, and follow-up in a bridge clinic may be another way of leveraging high motivation levels during inpatient stays to increase uptake and retention in AUD treatment. Increasing the number of clinic days, by adopting teleconsultation for providers outside the hospital system, or by utilizing a group visit model, are currently being explored.
In conclusion, the implementation of a multidisciplinary ALD clinic is feasible and produced promising early outcomes. Integrating care for advanced ALD patients must become more widespread as ALD rates rise across the United States. Additional research into alternative implementation structures, wider application of telehealth, and broader application of this model in diverse practice settings is needed to determine the optimal means of durable integrated care for ALD patients.
Supplementary Material
Highlights.
Alcohol-related liver disease has become a public health emergency, particularly affecting young people and women.
Integrated, multidisciplinary management of alcohol-related liver disease is recommended.
Integrated care with hepatology, psychiatry, psychology, and social work is feasible and acceptable to patients and produced encouraging early outcomes.
Acknowledgments
Financial Support:
Dr. Mellinger and Dr. Fernandez are supported by NIAAA K23 career development awards.
Footnotes
The authors have no relevant conflict of interest to report.
ALD: alcohol-associated liver disease; AP: alkaline phosphatase; ALT: alanine aminotransferase; AST: aspartate aminotransferase; AUD: alcohol use disorder; INR: International Normalized Ratio; MAIN: Michigan Alcohol Improvement Network; MELD: Model for End-stage Liver Disease
2016 cost data taken from hcupnet.ahrq.gov. Accessed March 3, 2020.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5, Arlington, VA, American Psychiatric Association. [Google Scholar]
- Bastien CH, Vallieres A & Morin CM (2001). Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med, 2, 297–307. [DOI] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF & Kranzler HR (1995). The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol, 56, 423–32. [DOI] [PubMed] [Google Scholar]
- Comerford M, Lourens S, Liangpunsakul S, Chalansani NP, Sanyal AJ, Shah VH, Kamath PS, Puri P, Katz BP, Radaeva S & Crabb DW (2017). Challenges in Patient Enrollment and Retention in Clinical Studies for Alcoholic Hepatitis: Experience of the TREAT Consortium. Alcohol Clin Exp Res, 41, 2000–2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crabb DW, Im GY, Szabo G, Mellinger JL & Lucey MR (2020). Diagnosis and Treatment of Alcohol-Associated Liver Diseases: Practice Guidance from the American Association for the Study of Liver Diseases. Hepatology, 71, 306–333. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, Jung J, Zhang H, Fan A & Hasin DS (2017). Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry, 74, 911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanwal F, Tapper EB, Ho C, Asrani SK, Ovchinsky N, Poterucha J, Flores A, Ankoma-Sey V, Luxon B & Volk M (2019). Development of Quality Measures in Cirrhosis by the Practice Metrics Committee of the American Association for the Study of Liver Diseases. Hepatology, 69, 1787–1797. [DOI] [PubMed] [Google Scholar]
- Khan A, Tansel A, White DL, Kayani WT, Bano S, Lindsay J, El-Serag HB & Kanwak F (2016). Efficacy of Psychosocial Interventions in Inducing and Maintaining Alcohol Abstinence in Patients With Chronic Liver Disease: A Systematic Review. Clin Gastroenterol Hepatol, 14, 191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellinger JL (2019). Epidemiology of Alcohol Use and Alcoholic Liver Disease. Clin Liver Dis (Hoboken), 13, 136–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellinger JL, Fernandez A, Shedden K, Winder GS, Fontana RJ, Volk ML, Blow FC & Lok ASF (2019). Gender Disparities in Alcohol Use Disorder Treatment Among Privately Insured Patients with Alcohol-Associated Cirrhosis. Alcohol Clin Exp Res, 43, 334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellinger JL, Shedden K, Winder GS, Tapper E, Adams M, Fontana RJ, Volk ML, Blow FC & Lok ASF (2018). The high burden of alcoholic cirrhosis in privately insured persons in the United States. Hepatology, 68, 872–882. [DOI] [PubMed] [Google Scholar]
- Miller WR & Rollnick S (2013). Motivational interviewing : helping people change, New York, NY, Guilford Press. [Google Scholar]
- Skinner HA (1982). The drug abuse screening test. Addict Behav, 7, 363–71. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K & Williams JB (1999). Validation and utility of a self-report version of PRIMEMD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA, 282, 1737–44. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB & Lower B (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med, 166, 1092–7. [DOI] [PubMed] [Google Scholar]
- Tapper EB & Parikh ND (2018). Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ, 362, k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE, Rigotti NA, Chang Y, Herman GE, Erwin A, Regan S & Metlay JP (2019). Effect of Integrating Substance Use Disorder Treatment into Primary Care on Inpatient and Emergency Department Utilization. J Gen Intern Med, 34, 871–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winder GS, Fernandez AC, Klevering K & Mellinger JL (2019). Confronting the Crisis of Comorbid Alcohol Use Disorder and Alcohol-associated Liver Disease With a Novel Multidisciplinary Clinic. Psychosomatics. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.