Abstract
Introduction
Hot flushes/flashes (HFs) or other vasomotor symptoms affect between 45 and 97% of women during menopause. Hormone replacement therapy (HRT) is effective at alleviating menopausal symptoms, but some women cannot or prefer not to take HRT. Since current non-hormonal options have suboptimal efficacy/tolerability, there is a pressing need for an effective, well-tolerated alternative. The neurokinin 3 receptor (NK3R) has recently been implicated in the generation of menopausal HFs and represents a novel therapeutic target to ameliorate HF symptoms. This review aims to assess if NK3R antagonists (NK3Ras) are more effective than Serotonin Norepinephrine Reuptake Inhibitors (SNRIs)—currently a common choice for non-hormonal treatment of menopausal HFs.
Methods
Studies were identified after systematically searching Ovid MEDLINE and EMBASE databases based on PRISMA guidelines. Trial quality and bias were assessed. Key efficacy outcomes (HF frequency, HF severity and number of night-time awakenings/night-sweats) and selected safety outcomes were extracted and analysed.
Results
Seven SNRI and four NK3Ra placebo-controlled randomised trials (plus four follow-up reports) were included in this review. NK3Ra administration resulted in a larger reduction from baseline in HF frequency, HF severity and night-sweats compared to SNRIs. Five of seven SNRI trials showed a reduction in HF frequency that was statistically significant (by 48–67% from baseline at weeks 8 or 12) whereas all NK3Ra trials showed a statistically significant reduction in HF frequency (by 62–93% from baseline at weeks 2, 4 or 12). While SNRI trials reported poor tolerability, particularly nausea, NK3Ra trials reported good tolerability overall, although two trials reported elevation in transaminases.
Conclusion
NK3Ras trials show encouraging efficacy and tolerability/safety. Completion of phase 3 NK3Ra trials are required to confirm efficacy and uphold safety/tolerability data but phase 2 results suggest that NK3Ras are more effective than SNRIs for non-hormonal treatment of menopausal HFs.
Keywords: Menopause, Vasomotor symptoms, Hot flushes/flashes, Neurokinin 3 receptor antagonist, Fezolinetant, Elinzanetant (NT-814), MLE4901, Serotonin Norepinephrine Reuptake Inhibitor, Venlafaxine, Desvenlafaxine
Key Summary Points
| Between 45 and 97% of menopausal women suffer vasomotor symptoms (hot flushes/flashes and night-sweats) which can significantly impact their quality of life and 10–20% find them almost intolerable. |
| Conventional treatment is hormone replacement therapy (HRT) but some women cannot or prefer not to take HRT. However, current non-hormonal options have suboptimal efficacy and tolerability. |
| Neurokinin B, predominantly acting via the neurokinin 3 receptor (NK3R), has been implicated in the generation of menopausal hot flushes/flashes. |
| We undertook a systematic qualitative review to compare outcomes of placebo-controlled randomised clinical trials using neurokinin 3 receptor antagonists (NK3Ras) with those using Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) for the non-hormonal treatment of menopausal hot flushes/flashes. |
| NK3Ra trials reported numerically superior efficacy and better safety/tolerability compared with SNRIs trials. Provided that phase 3 NK3Ra trials are supportive, NK3Ras appear a promising therapy for this challenging area. |
Introduction
Hot flushes/flashes (HFs), defined as transient sensations of heat, flushing, sweating and chills, affect between 45 and 97% of women during menopause and can significantly degrade their quality of life [1]. HFs often lead to sleep disturbances for a prolonged period, with recurrent episodes occurring over a median duration of 7.4 years [2]. Between 10 and 20% of women find HFs almost intolerable [3]. While the full pathophysiological mechanism of HFs remains elusive, oestrogen deficiency appears to play a causative role. Hormone replacement therapy (HRT) remains the most commonly prescribed treatment to alleviate menopausal symptoms provided there are no contraindications (Table 1) [4]. However, the use of HRT has decreased after reports of increased risk of cardiovascular (CV) disease, breast cancer, stroke and pulmonary embolism [5]. While subsequent data suggest that the benefits of HRT typically outweigh the risks for women without contraindications, many now seek non-hormonal alternatives.
Table 1.
Typical contraindications for hormone replacement therapy [4]
| Contraindications for hormone replacement therapy |
|---|
| Current, past, or suspected breast cancer |
| Known or suspected oestrogen-dependent cancer |
| Undiagnosed vaginal bleeding |
| Untreated endometrial hyperplasia |
| Previous idiopathic or current venous thromboembolism (deep vein thrombosis or pulmonary embolism), unless the woman is already on anticoagulant treatment |
| Active or recent arterial thromboembolic disease (for example, angina or myocardial infarction) |
| Active liver disease with abnormal liver function tests |
| Pregnancy |
| Thrombophilic disorder |
Current non-hormonal treatment options include Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) or Selective Serotonin Reuptake Inhibitors (SSRIs), clonidine, gabapentin and pregabalin. Of these, SNRIs/SSRIs are probably the most commonly recommended [6], with data for venlafaxine considered the most convincing [7]. Nevertheless, none of the current non-hormonal drugs have optimal efficacy and use in clinical practice may be limited by side effects or by interactions with other medications (for example, paroxetine or other CYP2D6 inhibitors should not be co-prescribed with tamoxifen [7] which is clinically relevant considering that a key indication for a non-hormonal treatment is prior breast cancer). Therefore, there remains a pressing need for an effective and well-tolerated non-hormonal alternative.
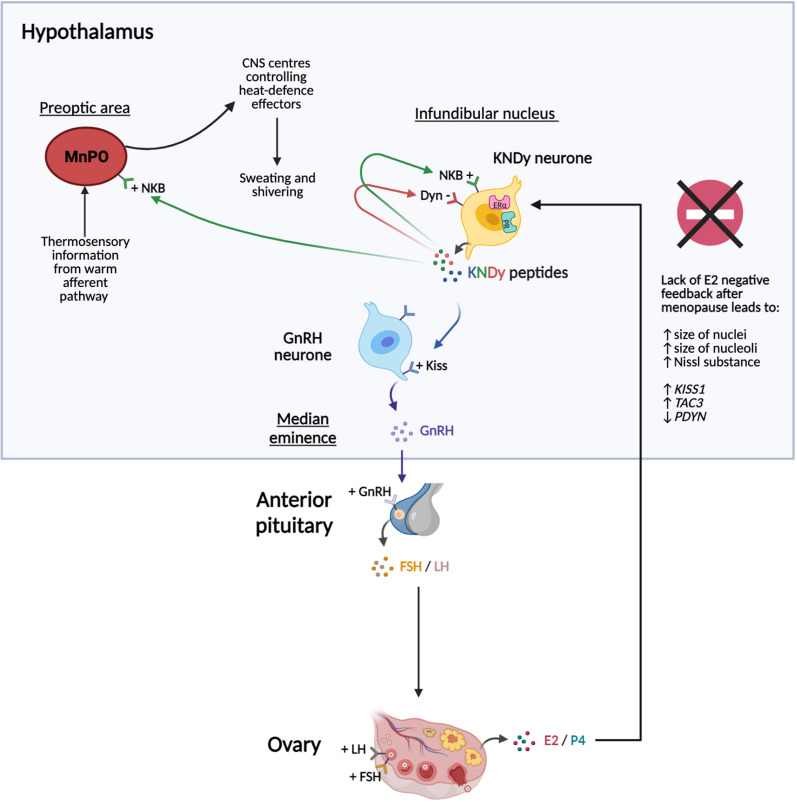
The hypothalamic neuropeptide kisspeptin (Kiss; encoded by the KISS1 gene) is required for human fertility being a potent stimulator of the hypothalamic–pituitary–gonadal axis (Fig. 1) [8]. In primates, a population of Kiss neurones located in the hypothalamic infundibular nucleus co-express the neuropeptides, neurokinin B (NKB) and dynorphin (Dyn), and are thus termed kisspeptin–neurokinin B–dynorphin (KNDy) neurones [9]. NKB [encoded by the tachykinin 3 (TAC3) gene] and Dyn [encoded by the prodynorphin (PDYN) gene] regulate pulsatile Kiss secretion from KNDy neurones by acting auto-synaptically via neurokinin 3 receptors (NK3R) and Dyn (kappa opioid) receptors to stimulate and inhibit the release of Kiss, respectively [10]. KNDy neurones project to the hypothalamic thermoregulatory centre in mammals (the median preoptic area and adjacent median preoptic nucleus) [11]. Gonadal feedback is transmitted by oestrogen receptor alpha (ERα) and progesterone receptors (PR) expressed on Kiss neurons. KNDy neurones are normally stimulated by NK3R activation and inhibited by oestrogen. However, during menopause declining oestrogen levels leads to NKB hypersecretion, and overstimulation of KNDy neurons in particular. This elicits increased activity in the thermoregulatory centre, which shifts the thermoneutral zone increasing sensitivity to external cues and triggering more frequent heat dissipation responses such as HFs [12].
Fig. 1.
Relationship between KNDy neurons, GnRH neurons, and the heat-defence pathway. KNDy neurones in the infundibular nucleus secrete the neuropeptides Kiss (encoded by the KISS1 gene), NKB (encoded by the TAC3 gene) and Dyn (encoded by the PDYN gene). NKB and Dyn act autosynaptically, stimulating and inhibiting further Kiss release, respectively. Kiss acts on GnRH neurones. GnRH stimulates LH and FSH release from the anterior pituitary which stimulates ovarian sex steroid production. During menopause, lack of oestradiol (E2) negative feedback results in increased expression of KISS1 and TAC3 mRNA but decreased expression of PDYN mRNA. Consequently, KNDy neurones become hypertrophied, as seen by increased size of nuclei/nucleoli and increased Nissl substance. KNDy neurones project to the hypothalamic thermoregulatory centre (the median POA and adjacent MnPO). During menopause, the increase in NKB signalling and overstimulation of KNDy neurons increases activity in the thermoregulatory centre which then becomes hypersensitive to external cues from peripheral sensors, leading to activation of heat dissipation effectors. KNDy kisspeptin–neurokinin B–dynorphin, Kiss kisspeptin, NKB neurokinin B, Dyn dynorphin, GnRH gonadotropin-releasing hormone, LH luteinizing hormone, FSH follicle-stimulating hormone, POA pre-optic area, MnPO median preoptic nucleus, E2 oestradiol, ERα oestrogen receptor alpha, PR progesterone receptor, KISS1 kisspeptin gene, TAC3 tachykinin 3 gene, PDYN prodynorphin gene. The figure was created with BioRender.com
Blockade of NKB signalling with the use of an NK3R antagonist (NK3Ra) is proposed to normalise KNDy neurone activity and thus may help alleviate HFs in menopausal women. This review aimed to (1) evaluate randomised controlled trials (RCTs) reporting the efficacy and tolerability of NK3Ras for the treatment of menopausal HFs and (2) to put these findings in clinical context by qualitative comparison with outcome data from RCTs using the SNRI venlafaxine (or the succinate salt of its active metabolite, desvenlafaxine) to treat menopausal HFs.
Methods
To put the clinical outcomes of the NK3Ra studies into context, a clinically relevant alternative non-hormonal therapy was required for comparison. While arguments could be made for selecting any one of the SNRIs/SSRIs, clonidine, gabapentin or pregabalin, multiple guidelines and reviews suggest that SSRIs/SNRIs are the most commonly recommended [6], with trial evidence strongest for venlafaxine/desvenlafaxine, paroxetine and citalopram/escitalopram [13]. Of these, venlafaxine (or its active metabolite desvenlafaxine) was selected for 3 reasons: modest current use was confirmed after consultation with each of 4 UK regional menopause clinics (London, Edinburgh, Cardiff and Belfast), a College report considered the most convincing SSRI/SNRI efficacy data were for venlafaxine [7], and, since venlafaxine does not interact with tamoxifen, it is the preferred treatment for breast cancer survivors taking tamoxifen [14], a key indication for a non-hormonal menopause treatment. In contrast, the SSRI paroxetine is a potent CYP2D6 inhibitor and is contra-indicated with tamoxifen. The SSRI fluoxetine and SNRI duloxetine are also CYP2D6 inhibitors (albeit more moderate).
A systematic search of the published literature up to 17/2/2021 was undertaken on Ovid MEDLINE and EMBASE, based on PRISMA guidelines [15] and using the following key words: “venlafaxine”, “desvenlafaxine”, “hot flushes”, “hot flashes”, “vasomotor symptoms”, “VMS”, “menopause”, “neurokinin B”, “dynorphin”, “kisspeptin”, “kappa”, “neurokinin 1”, “neurokinin 3”, “neurokinin B”. Further studies were identified by cross-referencing references from the qualifying studies. Duplicates were removed and studies were screened using inclusion/exclusion criteria.
Inclusion criteria were: studies of perimenopausal, menopausal and postmenopausal women (natural or surgically induced only), having HFs, receiving NK3Ra or venlafaxine/desvenlafaxine treatment, comparison with a placebo arm, frequency and severity of HFs reported, primary research design and in English language.
Exclusion criteria were: pre-menopausal women, chemically or medically induced menopause, not having HFs, not receiving treatment with NK3Ra or venlafaxine/desvenlafaxine, or receiving treatment for HFs in addition to NK3Ra or venlafaxine/desvenlafaxine. Qualifying studies were required to meet all inclusion criteria and studies discarded if they met any one of the exclusion criteria.
Only women with natural or surgically-induced menopause were included to ensure a definitive and irreversible diagnosis. Women with medically-induced menopause (such as chemotherapy or use of GnRH analogues) were excluded, as their ovarian function may have had the potential to recover (and reverse menopause). Men were excluded due to the different physiology involved in the development of HFs.
Women concurrently receiving any other medications to relieve HFs other than the study drugs were excluded so that the measured effect could be attributed solely to the drugs under investigation.
A large placebo effect is well described in HF treatment trials [16], thus only studies comparing the active drug versus placebo were selected so that the drug’s effect could be evaluated in context.
Once qualifying studies were identified, study quality was assessed using Critical Appraisal Skills Programme (CASP) methodology [17]. The CASP method evaluated four main components (study design, methodology, reporting of results and clinical implications), with each component addressed by either 2 or 3 questions. The Cochrane Collaboration’s tool [18] was used to assess for risk of bias in each study, comprising 7 questions defined by the Cochrane handbook to evaluate selection (randomisation or allocation concealment), reporting, performance, detection, attrition and other bias. One author (S.J.M.) undertook the primary detailed evaluation of quality and bias for each study. Equivocal findings were discussed with a second author (J.A.T.) to reach consensus.
To enable comparison of SNRI and NK3Ra outcomes, while studies may include different outcome measures [19], each qualifying study was assessed for the specific key efficacy outcomes of HF frequency, HF severity and, if stated, night-time awakenings due to HFs, plus safety/tolerability outcomes including common adverse events (AEs), serious adverse events (SAE) and discontinuation due to AEs. Since SNRI studies were phase 3 whereas NK3Ra trials were phase 2, a systematic qualitative review rather than a meta-analysis was considered the most appropriate.
This paper is based on previously published data and does not involve any new studies with human or animal subjects performed by any of the authors.
Results
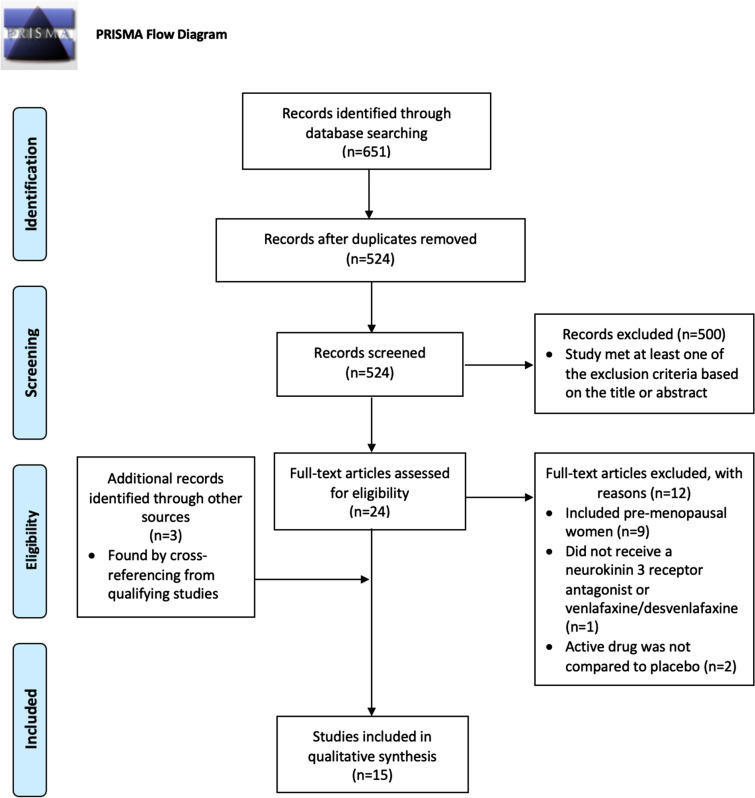
Figure 2 illustrates the PRISMA flow diagram summarising the search process. The initial search yielded 651 records. After 127 duplicates were removed, 524 studies were screened for inclusion (based on the inclusion/exclusion criteria). A total of 500 studies were excluded based on the title or abstract. The remaining 24 studies required assessment of the full text, and a further three studies were found by cross-referencing references from these studies. This resulted in 15 qualifying studies for qualitative synthesis (seven SNRI trials plus two follow-up papers [20–28] and four NK3Ra trials plus two follow-up papers [29–34]).
Fig. 2.
PRISMA flow diagram summarising the search strategy used to identify qualifying studies [15]
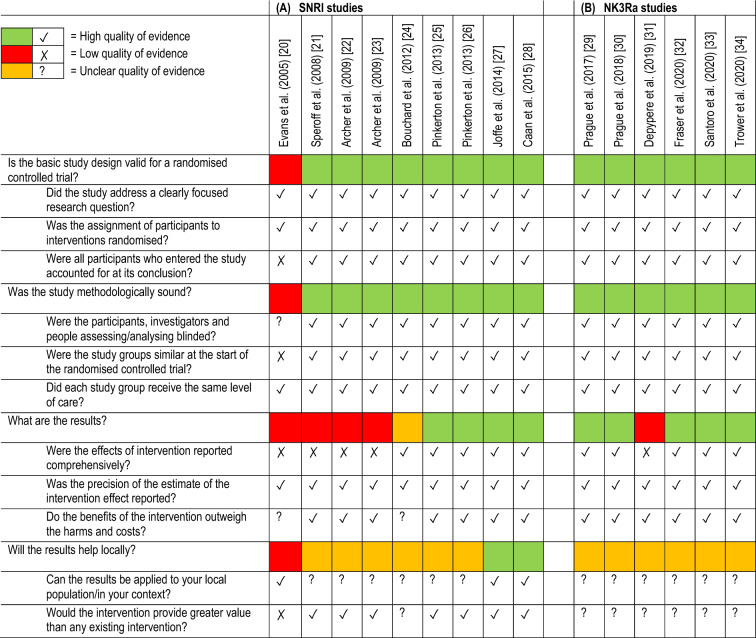
Table 2 summarises the CASP quality assessment for each study. For illustrative purposes, when assessing the four components, if all answers were ‘Yes’, the score was designated as ‘high’ quality of evidence (green). If one or more answers was ‘No’, the score was assigned as ‘low’ quality of evidence (red). If one or more answers was ‘cannot tell’ (but none was ‘no’) the score was assigned as ‘unclear’ quality of evidence (orange). The full quality analysis for each study is available upon request. Overall, the studies were mostly of high quality.
Table 2.
Quality of evidence summary for (A) SNRI and (B) NK3Ra studies, assessed using Critical Appraisal Skills Programme checklists [17]
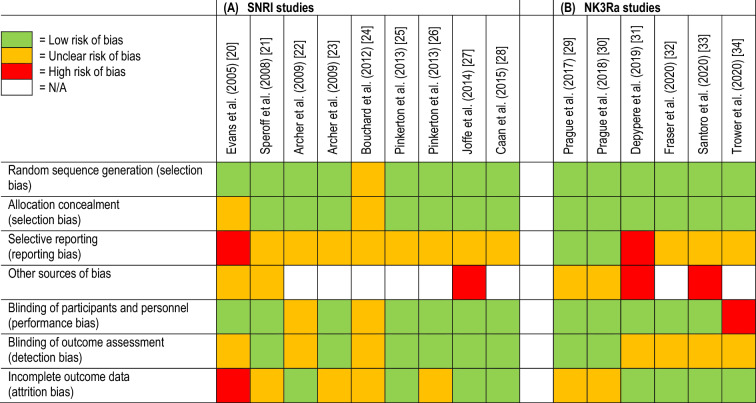
Table 3 summarises the Cochrane Collaboration’s tool bias assessment for each study. For illustrative purposes, a low risk of bias subtype was shown as green, a high risk as red and an unclear risk as orange. The full quality analysis for each study is available upon request. Overall, the studies were mostly of low bias.
Table 3.
Risk of bias summary for the (A) SNRI and (B) NK3Ra studies, assessed using the Cochrane Collaboration’s tool [18]
Table 4 summarises the study design, efficacy and tolerability/safety outcomes for SNRI trials. Overall, the SNRI trials showed modest HF reduction. There was a statistically significant reduction in HF frequency versus placebo in five of seven trials [21–23, 25, 27] (48–67% reduction from baseline at week 8 or 12 in the setting of a 25–51% placebo response) and a statistically significant reduction in HF severity versus placebo in five of seven trials [21–23, 25, 27] for at least one dose and one time point (24–31% reduction from baseline at week 12 in the setting of a 12–18% placebo response where percentage data were reported). Night-time awakenings due to HFs showed a statistically significant reduction in the three trials [21–23] that measured this outcome (53–77% reduction from baseline at week 12 in the setting of 44–63% placebo response). However, HF frequency and HF severity did not show a statistically significant reduction versus placebo in two SNRI trials [20, 24]. SNRI-treated subjects experienced more AEs (in all trials) and discontinuations due to AEs (in all but one trial [22]) versus placebo. Common AEs included nausea, dry mouth, insomnia, dizziness and constipation (with nausea being reported to be the most debilitating).
Table 4.
Serotonin-norepinephrine reuptake inhibitor (SNRI) study results
| Clinical trial | Trial design and key participant BL data | Key outcomes | Results (p values vs. placebo) |
|---|---|---|---|
|
1 Evans et al Obstetrics and Gynecology (2005) [20] |
12-week RCT: 1 US centre Mean age = 52.15 years 80 randomised (1:1) to venlafaxine XR (37.5 mg/day for 1 week, titrated to 75 mg/day for 11 weeks) vs. placebo |
1°: # of mild, mod, severe, and very severe HFs/day Avg. HF severity 2°: Important AEs/SAEs Discontinuation due to AEs |
1°: absolute or %↓ data not reported No sig. ↓ in HF # vs. placebo (p = 0.2) No sig. ↓ in mean HF severity (p value not given) 2°: AEs: ↑ in dry mouth (81% vs. 44%), ↑ in sleeplessness (88% vs. 47%) and ↓ appetite (81% vs. 53%) vs. placebo ↑ withdrawals [11 vs. 8 (p = ns)] due to difficulty sleeping, ↓ libido, nausea or anxiety |
|
2 Speroff et al Obstetrics and Gynecology (2008) [21] |
1° efficacy evaluations completed at 4 and 12 weeks Safety and tolerability data collected for 52 weeks 52 week DBRCT; dose-ranging trial: 37 US centres Mean age = 53 years (37–78) Mean BMI = 26.96 kg/m2 707 randomised (2:2:2:2:1) to desvenlafaxine 50, 100, 150, or 200 mg/day vs. placebo for 52 weeks 620 included in mITT analysis |
1°: ∆ from BL in avg. daily # of mod/severe HFs at week 4 and 12 ∆ from BL in avg. daily HF severity score at week 4 and 12 2°: ∆ from BL in daily # of night-time awakenings due to HFs at week 4 and 12 Important AEs/SAEs Discontinuation due to AEs |
1°: ↓ from BL in avg. daily # of mod/severe HFs vs. placebo (No ↓ with 50 mg or 200 mg) 100 mg ↓ at week 4 (− 6.62 vs. − 5.22; p = 0.013) and week 12 [− 7.23 (64%↓) vs. − 5.50 (51%↓); p = 0.005] 150 mg ↓ at week 12 [− 6.94 (60%↓) vs. − 5.50 (51%↓); p = 0.020], but not at week 4 ↓ from BL in avg. daily HF severity scores vs. placebo (No ↓ with 50 mg or 150 mg) 100 mg ↓ at week 12 [− 0.80 (31%↓) vs. − 0.47 (18%↓); p = 0.002], but not at week 4 200 mg ↓ at week 12 [− 0.74 (27%↓) vs. − 0.47 (18%↓); p = 0.013], but not at week 4 2°: ↓ daily # of night-time awakenings vs. placebo at week 12 (week 4 not reported) (No ↓ with 50 mg) 100 mg, 150 mg and 200 mg ↓ at week 12 [− 2.77/night (76.9%↓), p = 0.013; − 2.69/night (69%↓), p = 0.034 and − 2.68/night (70.5%↓), p = 0.043, respectively vs. − 2.21/night (63.1%↓)] AEs vs. placebo 150 mg and 200 mg ↑ AEs during week 1 only (both p < 0.05), most commonly, nausea, dry mouth, insomnia (No ↑ with 50 mg and 100 mg) 3 SAEs possibly Tx-related: 2 increased LFTs, 1 cholecystitis ↑ hypertension (5.9% overall vs. 1.3% placebo; p = ns). 5 vs. 0 CV events at 1 year (p = ns) ↑ discontinuations due to AEs 150 and 200 mg during week 1 only (both p < 0.001). (No ↑ with 50 mg and 100 mg) |
|
3 Archer et al American Journal of Obstetrics and Gynecology (2009) [22] |
12 week DBRCT: 34 US centres Mean age = 53.36 years (29–71) Mean BMI = 27.86 kg/m2 (17.2–40.1) 458 randomised to desvenlafaxine 100 mg/day or 150 mg/day vs. placebo for 12 weeks [50 mg/day for 3 days, titrated to 100 mg/day on day 4 (titrated to 150 mg/day on day 8 for 150 mg/day group)] 2 week dose-tapering 436 included in mITT analysis |
1°: ∆ from BL in avg. daily # mod/severe HFs at weeks 4 and 12 ∆ from BL in avg. daily HF severity score at weeks 4 and 12 2°: ∆ from BL in # of night-time awakenings at weeks 4 and 12 Important AEs/SAEs Discontinuation due to AEs |
1°: ↓ daily # of HF from BL vs. placebo with 100 mg and 150 mg at week 4 (both p ≤ 0.012, no % given) and week 12 (65.4%↓, p = 0.005; and 66.6%↓, p = 0.012, respectively vs. 50.8%↓) ↓ daily HF severity score from BL vs. placebo with 100 mg and 150 mg at week 12 [− 0.65 (27%↓); and − 0.66 (27.5%↓), respectively vs. − 0.33 (13.75%↓); both p < 0.001], and at all other time points 2°: ↓ daily # of night-time awakenings from BL vs. placebo with 100 mg and 150 mg at week 4 (− 1.8 and − 1.6, respectively vs. − 1.2) and week 12 [− 2.0 (60.6%↓) and − 1.8 (58.1%↓), respectively vs. − 1.4 (43.8%↓)]; all p ≤ 0.048 ↑ AEs during week 1 only vs. placebo (84.1% vs. 69.5%; p = 0.002), most commonly nausea (25.2%), dry mouth, insomnia, constipation, asthenia 2 SAEs possibly Tx-related: hypertension (1 subject with 150 mg ↑ SBP by 4.52 mmHg at week 12 (p = 0.002), bronchospasm (1 subject but on placebo) Discontinuation due to AEs: no diff. [but numerically ↑ in 150 mg group (p = ns)] |
|
4 Archer et al American Journal of Obstetrics and Gynecology (2009) [23] |
26 week DBRCT: 32 US centres Mean age = 53.7 years Mean BMI = 27.1 kg/m2 (15.9–40.4) 567 randomised to desvenlafaxine 100 mg/day or 150 mg/day vs. placebo for 26 weeks 484 included in mITT analysis |
1°: ∆ from BL in avg. daily # of mod/severe HFs at weeks 4 and 12 ∆ from BL in avg. daily HF severity at weeks 4 and 12 2°: ∆ from BL in # of night-time awakenings due to HFs Important AEs/SAEs Discontinuation due to AEs |
1°: ↓ daily # of HFs from BL vs. placebo at week 4 and 12 (week 12: 100 mg 60%↓, p = 0.002; 150 mg 66.6%↓, p < 0.001, vs. 47%↓) 150 mg maintained ↓ at week 26 (69%↓ vs. 51%↓, p = 0.001), whereas 100 mg did not (61%↓, p = 0.061) but study not powered for efficacy > 12 weeks ↓ daily HF severity from BL vs. placebo at week 4 and 12 (week 12: 100 mg 24%↓, p = 0.002; 150 mg 29%↓, p < 0.001 vs. 13%↓). 150 mg maintained ↓ at week 26 (p = 0.008, no % given) 2°: ↓ daily # of night-time awakenings from BL vs. placebo at week 4 (actual ↓ not given) and week 12 [100 mg − 2.0 (52.6%↓); 150 mg − 2.4 (68.6%↓) vs. − 1.6 (47.1%↓)]; all p ≤ 0.026 ↑ AEs during week 1 only vs. placebo (p < 0.05), most commonly nausea (44.6%), dizziness, insomnia, dry mouth, constipation ↑ SAE possibly Tx-related: hypertension (100 mg) ↑ discontinuations due to AEs during week 1 only vs. placebo (16.1% vs. 0.6%; p < 0.001) |
|
5 Bouchard et al Climacteric (2012) [24] |
12-week DBRCT: 35 European centres, 2 centres in South Africa, 1 centre in Mexico Mean age = 53.6 years (40–66 years) Mean BMI = 26 kg/m2 (16–34) ≥ 485 randomised (1:1:1) to desvenlafaxine 100 mg/day, tibolone 2.5 mg/day, vs. placebo for 12 weeks 451 included in mITT analysis |
1°: ∆ from BL in avg. daily # of mod/severe HFs at weeks 4 and 12 ∆ from BL in avg. daily HF severity at weeks 4 and 12 2°: Important AEs/SAEs Discontinuation due to AEs |
1°: No ↓ in daily # of HFs from BL vs. placebo at week 4 (− 4.63 vs. − 4.38, p = 0.558) and week 12 (− 5.78 (57.7%↓) vs. –5.82 (57.5%↓), p = 0.921] No ↓ in daily HF severity from BL vs. placebo at week 4 (− 0.37 vs. − 0.31, p = 0.352) and week 12 [− 0.61 (26.8%↓) vs. − 0.61 (26.5%↓), p = 0.943] 2°: ↑ AEs with desvenlafaxine vs. tibolone and placebo (73.4% vs. 64.5% and 55.9%, respectively), most commonly nausea (31%), dizziness and constipation ↑ bleeding with tibolone vs. desvenlafaxine and placebo [23% vs. 12% (p = 0.024) and 9% (p = 0.001), respectively] ↑ discontinuations due to AEs during week 1 only vs. placebo (p < 0.001). Most commonly nausea (8.9%) and headache (3.8%) |
|
6a Pinkerton et al Menopause (2013) [25] |
52-week DBRCT: 122 US and Canadian centres Mean age = 54 years (45–71) Mean BMI = 26.45 kg/m2 (16.9–35.3) 396 randomised (1:1) to desvenlafaxine 100 mg/day vs. placebo for 52 weeks (50 mg/day for 1 week, titrated to 100 mg/day for 51 weeks) 2 week dose-tapering 365 included in mITT analysis Pinkerton et al. (2013) [25] reports 12-week data from an efficacy substudy (part of a larger n = 2186 safety study) |
1°: ∆ from BL in avg. daily # of mod and severe HFs at weeks 4 and 12 ∆ from BL in avg. daily HF severity scores at weeks 4 and 12 2°: Important AEs/SAEs Discontinuation due to AEs |
1°: ↓ daily # of HFs vs. placebo at week 4 [− 6.5 HFs (55%↓) vs. − 3.6 (31%↓); p < 0.001] and week 12 [− 7.3 HFs (62%↓) vs. − 4.5 (38%↓); p < 0.001] ↓ daily HF severity score vs. placebo at week 4 [− 0.47 (20%↓) vs. − 0.19 (8%↓); p < 0.001] and week 12 [− 0.59 (25%↓) vs. − 0.28 (12%↓); p < 0.001] 2°: ↑ AEs vs. placebo during week 1 only (p < 0.001), mostly nausea, dry mouth, constipation (but no diff. in BP) 2 SAEs: 1 squamous cell carcinoma, 1 multi-event SAE (altered mental status with slurred speech, uncontrolled hypertension, resolved hypokalemia, polypharmacy) ↑ discontinuations due to AEs vs. placebo (10.0% vs. 3.7%; p = 0.016); rates similar after week 1 |
|
6b Pinkerton et al. Menopause (2013) [26] |
Pinkerton et al. (2013) [26] reports 52-week data from the same efficacy substudy population See above |
1°: ∆ from BL in avg. daily # of HFs at weeks 12, 26, 52 ∆ from BL in avg. daily HF severity scores at weeks 12, 26, 52 2°: Important AEs/SAEs Discontinuation due to AEs |
1°: ↓ in daily # of HFs at 12 weeks [− 7.5 HFs (64%↓) vs. –5.0 (43%↓); p < 0.001], 26 weeks [− 8.6 HFs (74%↓) vs. − 6.3 (54%↓); p < 0.001 and 52 weeks [− 7.7 HFs (66%↓) vs. − 4.8 (41%↓); p < 0.001] ↓ in daily HF severity score at 12 weeks [− 0.63 (27%↓) vs. − 0.3 (13%↓); p < 0.001], 26 weeks [− 0.85 (36%↓) vs. − 0.53 (22%↓); p = 0.001] and 52 weeks [− 0.75 (32%↓) vs. − 0.44 (19%↓); p = 0.003] 2°: includes efficacy substudy (n = 365) and larger safety population (n = 2186) ↑ AEs vs. placebo (84% vs. 79%; p = 0.006), most commonly nausea (21%), headache, dry mouth and insomnia. Rates of new-onset AEs were similar by week 3 SAEs: No excess CV ischaemic events vs. placebo over 52 weeks ↑ discontinuations due to AEs vs. placebo (18.3% vs. 9.7%; p < 0.001); rates highest during week 1 |
|
7a Joffe et al JAMA Internal Medicine (2014) [27] |
DBRCT: 3 US centres Mean age = 54.6 years Mean BMI = 28.3 kg/m2 339 randomised (2:2:3) to venlafaxine XR 75 mg/day (37.5 mg/day titrated to 75 mg/day over 1 week), oral 17-beta-oestradiol (ET) 0.5 mg/day or placebo for 8 weeks Venlafaxine followed by 2-week dose-tapering 330 included in mITT analysis |
1°: Mean daily # of HFs at weeks 4 and week 8 2°: HF severity at week 8 Important AEs/SAEs Discontinuation due to AEs |
1°: ↓ # of HFs from BL vs. placebo at week 4 (48%↓ vs. 25%↓; p = 0.005) and week 8 (48%↓ vs. 29%; p = 0.005) 2°: baseline or %↓ data not reported ↓ HF severity vs. placebo at week 8 (mean diff. vs. placebo: − 0.2, p = 0.02) ↑ AEs vs. ET and placebo (69% vs. 56% and 62%, respectively; p = ns), most commonly fatigue 12 developed SBP > 165 mmHg or DBP > 95 mmHg (10.4% venlafaxine, 2.1% ET, 0 placebo), but all had BL SBP or DBP > study population mean. Vaginal bleeding 8.2% ET, 0% venlafaxine, and 1.6% placebo ↑ discontinuations due to AEs vs. placebo (5 venlafaxine, 4 ET, 2 placebo; p = ns) |
|
7b Cann et al Menopause (2015) [28] |
Cann et al. [28] reports questionnaire endpoints from Joffe et al. [27] |
MENQoL total and domain scores Measure of pain (PEG), depression (PHQ-9) and anxiety (GAD-7) Perceived stress (PSS) |
↓ (improved) mean total MENQoL score from BL vs. placebo at week 4 and week 8 (week 8: − 0.9 vs. − 0.7, p = 0.042) Only sig. diff. vs. placebo in psychosocial domain (week 8: − 1.5 vs. − 1.3, p = 0.008) No improvements vs. placebo with respect to changes in pain (PEG), depressive symptoms (PHQ-9) or anxiety (GAD-7) at weeks 4 and 8 ↓ (improved) perceived stress vs. placebo at week 4 and week 8 (week 8: − 3.4 vs. − 2.0, p = 0.02) |
DBRCT double-blind, randomised, placebo-controlled trial, XR extended release, mod moderate, # number, HFs hot flushes/flashes, VMS vasomotor symptoms, ≥ greater than or equal to, ≤ less than or equal to, > greater than, < less than, mg/d milligrams/day, (m)ITT (modified) intention-to-treat, BL baseline, 1° primary, 2° secondary, avg. average, ∆ change, sig. significant, ns not significant, ↑ increase, ↓ reduced, diff. difference, Tx treatment, (S)AEs (serious) adverse events, (S) or (D) BP (systolic) or (diastolic) blood pressure, LFTs liver function tests, ALT alanine aminotransferase, AST aspartate aminotransferase, NASH non-alcoholic steatohepatitis, ULN upper limit of normal, MENQoL Menopause-Specific Quality of Life questionnaire, HFRDIS Hot Flash-Related Daily Interference Scale, PEG The Pain Enjoyment of Life and General Activity scale, PHQ-9 9-item Patient Health Questionnaire, GAD-7 7-item Generalized Anxiety Disorder questionnaire, PSS Perceived stress scale
Table 5 summarises the study design efficacy and tolerability/safety outcomes for NK3Ra trials.
Table 5.
Neurokinin 3 receptor antagonists (NK3Ra) study results
| Clinical trial | Trial design and key participant BL data | Key outcomes | Results (p-values vs. placebo) |
|---|---|---|---|
|
1a. Prague et al The Lancet (2017) [29] |
DBRCT; Cross-over trial: 1 UK centre Mean age = 55 years (49–62) Mean BMI = 25.85 kg/m2 38 randomised to 4 weeks MLE4901 (40 mg BID) and 4 weeks placebo (BID) in random order separated by a 2-week washout period 37 included in ITT analysis |
1°: # of weekly HFs during week 2°: HF severity, bother and interference scores at week 4 Important AEs/SAEs Discontinuations |
1°: ↓ in weekly # of HFs from BL vs. placebo [ITT adjusted means: 19.35 (73%↓) vs. 49.01 (28%↓], respectively; p < 0.001] 2°: ↓ HF severity score from BL vs. placebo [3.27 (44%↓) vs. 5.70 (5%↓), p < 0.0001], ↓ bother score (2.92 vs. 5.56, p < 0.0001), and ↓ interference score (7.94 vs. 26.48, p < 0.0001) 3 developed a transaminase rise (ALT 4.5–5.9 × upper limit of normal) but normal bilirubin, occurring 28 days after starting, which normalised within 90 days Discontinuations (24%) higher than expected (mostly not MLE4901-related) |
|
1b Prague et al Menopause (2018) [30] |
Prague et al. [30] reports a post hoc time course analysis of Prague et al. [29] to define therapeutic profile of MLE4901 by comparing the mean daily total of HFs at day 3, and mean weekly total after weeks 1, 2, 3, and 4 of both Tx periods, and also compared with week 2 of the BL period Post hoc analysis of questionnaire data (minimum n = 33, maximum n = 35) |
# of HFs HF severity, bother and interference Impact on sleep via: # of night-time HFs Individual MENQoL items Individual HFRDIS items |
↓ # of HFs from BL vs. placebo by day 3 (72%↓ vs. 21%↓; p < 0.0001), maintained through to week 4 HF severity, bother & interference continued to improve vs. placebo. At day 3: ↓ HF severity from BL by 38% (vs. 7%↓; p < 0.0001), which ↓ to − 44% by week 4 (vs. 5%↓) ↓ HF bother from BL by 39% (vs. 5%↓; p < 0.0001), which ↓ to − 50% by week 4 ↓ HF interference from BL by 61% (vs. 24%↓; p = 0.0006), which ↓ to − 70% by week 4 Impact of sleep: ↓ night-time HFs from BL vs. placebo at week 4 (78%↓ vs. 22%↓; p < 0.0001). Improvements rapid, significant by day 3 vs. placebo (p < 0.0001) Improved MENQoL psychosocial and physical domains at week 4. Authors suggested due to improved sleep since ‘difficulty sleeping’, ‘lethargy’ and ‘tiredness’ improved at week 4 (p < 0.0001, p = 0.00128, and p = 0.0002, respectively), and ‘lethargy’ and ‘tiredness’ improved by day 3 (p = 0.0474 and p = 0.0132, respectively), whereas ‘muscle ache’ and ‘physical strength’ did not improve Improved ‘sleep’ and ‘concentration’, significant by day 3 vs. placebo (sleep: p = 0.001; concentration: p = 0.0075) (HFRDIS) |
|
2 Depypere et al Journal of Clinical Endocrinology and Metabolism (2019) [31] |
DBRCT: 8 Belgian centres Mean age = 53.5 years (44–64) Mean BMI = 25.8 kg/m2 87 randomised (1:1) to fezolinetant 90 mg BID or placebo for 12 weeks 87 included in mITT analysis (inferred from Fig. 2A but this is unclear) |
1°: ∆ from BL in mean daily total VMS score (composite of # and severity) at week 12 2°: Important AEs/SAEs Discontinuation due to AEs |
1°: ↓ mean daily total VMS score from BL vs. placebo at week 4, 8 and 12 [week 12: 2.7 (91%↓) vs. 14.4 (44%↓); all comparisons p < 0.001] 2°: ↑ AEs considered Tx-related vs. placebo (30.2% vs. 25%), most commonly GI disorders (23% vs. 9%) ↑ discontinuations due to AEs (2 (4.7%) vs. 0) |
|
3a Fraser et al VESTA Menopause (2020) [32] |
DBRCT; Dose-ranging: 51 US centres Mean age = 54.6 years (41–65) Mean BMI = 28.4 kg/m2 356 randomised (1:1) to fezolinetant BID 15, 30, 60, or 90 mg, or fezolinetant QD 30, 60, or 120 mg or placebo for 12 weeks 349 included in mITT analysis |
1°: Mean ∆ in # of mod/severe HFs from BL at weeks 4 and 12 Mean ∆ in mod/severe HF severity from BL at weeks 4 and 12 2°: Important AEs/SAEs Discontinuation due to AEs |
1°: All doses ↓ # of mod/severe HFs from BL vs. placebo at week 4 (ranging 62–81%↓ vs. 39%) and week 12 (ranging 74–87%↓ vs. 55%); all p ≤ 0.024 All doses ↓ mod/severe HF severity from BL vs. placebo at week 4 (ranging 29–54%↓ vs. 12%↓; all p ≤ 0.0322) and 60 mg BID, 90 mg BID, and 60 mg QD at week 12 ranging (52–53%↓ vs. 32%↓; all p ≤ 0.016) 2°: AEs similar across Tx groups, with no indication of a dose effect. Most commonly nausea, diarrhoea, fatigue 2 severe (but not serious) AEs considered Tx-related (both 60 mg QD): 1 cholelithiasis, 1 drug-induced liver injury (ALT [14.1xULN] and AST [9.5xULN] in a woman with obesity and NASH) 9 had ALT or AST > 3xULN, and 3 (60 mg BID, 90 mg BID, and 60 mg QD) had ALT or AST > 8xULN. None had total bilirubin > 2xULN ∴no cases met criteria for Hy’s law. ALT/AST levels rapidly returned to BL values after discontinuation/trended toward normalization while on drug Discontinuations due to AEs vs. placebo: Numerical ↑ |
|
3b Santoro et al VESTA Menopause (2020) [33] |
Santoro et al. [33] reports results of 2° endpoints from VESTA [32] | % achieving 50%, 70% and 90% ↓ from BL in # of mod/severe HFs |
Responder analyses ↑ ≥ 50% responder rate (all doses p < 0.05). All doses numerical ↑ in 70% and 90% responder rates (with magnitude and sig varying by dose and responder rate) Shorter time to 50% ↓ in HFs vs. placebo (2.2–8.4 days vs. 15.1 days; no p-value given) |
|
4 Trower et al RELENT-1 Menopause (2020) [34] |
DBRCT; multiple-ascending-dose study: 3 US centres Mean age = 55 years Mean BMI = 28.18 kg/m2 76 randomised (3:1) to NT-814 vs. placebo within each of 4 sequential dose cohorts; 50, 100, 150, and 300 mg/day for 2 weeks 76 included in mITT analysis |
Pre-specified exploratory efficacy endpoints: ∆ from BL in daily # of mod/severe HFs at week 2 ∆ from BL in avg. daily HF severity at week 2 ∆ from BL in daily #. of waking due to night sweats Important AEs/SAEs Discontinuation due to AEs |
50 mg and 100 mg no significant ↓ in HF endpoints. (With 50 mg vs. placebo, mean HF frequency actually higher (p = 0.048) although median HF frequency no difference) ↓ # of mod/severe HFs from BL vs. placebo [150 mg 84%↓ (p < 0.001), 300 mg 66%↓ (p = 0.022) vs. 37%↓] Doses ≥ 150 mg improved symptoms early (within week 1 of Tx) ↓HF severity vs. placebo with 150 mg [41%↓ vs. 13%↓ (p < 0.001)]; 300 mg no sig. difference ↓waking due to night sweats vs. placebo [150 mg 81%↓ (p < 0.001), 300 mg 63%↓ (p = 0.031) vs. 32%↓)]. AEs similar with placebo, 50 mg, 100 mg and 150 mg groups (slightly higher in 300 mg group) Most common: mild somnolence and headache No discontinuation due to AEs |
DBRCT double-blind, randomised, placebo-controlled trial, XR extended release, mod moderate, # number, HFs hot flushes/flashes, VMS vasomotor symptoms, ≥ greater than or equal to, ≤ less than or equal to, > greater than, < less than, mg/d milligrams/day, (m)ITT (modified) intention-to-treat, BL baseline, 1° primary, 2° secondary, avg. average, ∆ change, sig. significant, ns not significant, ↑ increase, ↓ reduced, diff. difference, Tx treatment, (S)AEs (serious) adverse events, (S) or (D) BP (systolic) or (diastolic) blood pressure, LFTs liver function tests, ALT alanine aminotransferase, AST aspartate aminotransferase, NASH non-alcoholic steatohepatitis, ULN upper limit of normal, MENQoL Menopause-Specific Quality of Life questionnaire, HFRDIS Hot Flash-Related Daily Interference Scale, PEG The Pain Enjoyment of Life and General Activity scale, PHQ-9 9-item Patient Health Questionnaire, GAD-7 7-item Generalized Anxiety Disorder questionnaire, PSS Perceived stress scale
Overall, in comparison to SNRI trials, the NK3Ra trials reported a larger reduction versus baseline in HF outcomes. NK3Ras led to a statistically significant reduction in HF frequency versus placebo at all time points, across all four trials, apart from the two lowest doses in the dose-ranging study by Trower et al. [34] (62–93% reduction from baseline at weeks 2, 4 or 12 in the setting of a 28–55% placebo response). HF severity also showed a reduction versus placebo in all trials (41–94% reduction from baseline measured at weeks 2, 4 or 12 in the setting of a 5–46% placebo response), although not all doses reached significance at all time points in the two dose-ranging trials [32, 34]. The number of night-time HFs/frequency of waking due to night-sweats showed a statistically significantly reduction versus placebo in the two trials [30, 34] that measured this outcome (63–81% reduction from baseline at weeks 2 and 4 in the setting of a 22–32% placebo response).
Discussion
In this qualitative analysis, NK3Ras reported larger reductions from baseline compared to SNRIs in terms of HF frequency, HF severity and night-sweats. All four NK3Ra trials reported statistically significant reductions in HF frequency by 62–93% from baseline at weeks 2, 4 or 12 (in the setting of a 28–55% placebo response), whereas only five of seven SNRI trials reported reduced HF frequency by 48–67% from baseline at weeks 8 or 12 (in the setting of a 25–51% placebo response) and two of seven trials reported no significant reduction. NK3Ra trials reported generally good tolerability (although transaminases elevation was noted in two trials) whereas SNRI trials reported less favourable tolerability, with nausea being common.
Trial Strengths and Weaknesses
While both the SNRI and NKR3a trials had many strengths, potential limitations were observed regarding generalisability and trial design which are important to note in order to place overall results in context and to consider when evaluating differences between treatment groups.
Age
HF symptoms are typically most severe around the final menstrual period. While mean age in the SNRI (53–55 years) and NK3Ra (54–55 years) trials was similar, the range was much greater in the SNRI trials (29–78 years vs. 41–65 years). This is relevant since it is unknown if treatment is equally effective in all menopause phases.
Ethnicity
Studies have shown ethnicity to affect HF prevalence with the highest frequency in Turkish women (97%) and the lowest in South American (47%) and Asian (45%) women [1]. Most SNRI trials predominately (~ 75–80%) recruited Caucasian women from North American centres which is a limitation since HF frequency can vary by population, often less in Asians, but greater in African-Americans [35]. NK3Ra trial participants were mainly Caucasian with few Asians, although an ongoing trial with fezolinetant is recruiting Asian women (NCT04234204) and a trial is planned in Chinese women (NCT04793204).
Menopause Definition
It is preferable to exclude perimenopausal women since symptoms might improve secondary to fluctuating hormone levels but be mistakenly attributed to the study drug. The FDA [36] advise using the following menopause definition: 12 months spontaneous amenorrhea, or 6 months amenorrhea plus FSH > 40mIU/ml, or 6 weeks post-surgical menopause. Two SNRI trials did not appear to fulfil the FDA definition and thus could have included perimenopausal women [20, 24]. All NK3Ra trials fulfilled the FDA definition, apart from Depypere et al. [31] who allowed amenorrhea ≥ 3 months if FSH > 40 IU/L and oestradiol < 0.21 nmol/L (which usually indicates premature ovarian insufficiency but oestrogen levels can vary in early stages).
HF Frequency and Severity
The FDA [36] advise enrolling subjects with ≥ 7 moderate-severe HFs/day (or ≥ 50/week). All trials fulfilled this except 2 SNRI trials [20, 27] which only required ≥ 14 HFs/week and not all were moderate or severe. Joffe et al. [27] reasoned that by not requiring ≥ 7 HFs/day (which only occurs in 7–9%), they enrolled a more generalisable population, many of whom do seek HF treatment. However, mild HFs may be less challenging to relieve and thus Joffe’s efficacy data could be potentially exaggerated.
HF Stability
A stable HF pattern is needed to minimise the risk of a spontaneous HF reduction being attributed to a study drug. Most trials required a consistent minimum or < 50% change in pattern over 1–2 baseline weeks. However, two SNRI trials [20, 21] failed to assess baseline stability and hence their results are potentially unreliable. One SNRI trial [23] and one NK3Ra trial [32] required ≥ 50 HFs over any 7 consecutive days during the 35-day screening period, yet separately used the week prior to randomisation as the baseline comparator, potentially underestimating baseline HF comparisons.
Baseline Characteristics
Treatment and control groups were generally well balanced. However, Evans et al. [20] reported higher alcohol consumption (a potential HF trigger) in their SNRI group but addressed this using sensitivity analysis. Among NK3Ra trials, Trower et al. [34] reported that the NT-814 50 mg group had a higher baseline HF frequency, severity and night-time awakenings which likely accounts for the unexpected observation of 50 mg showing less reduction in HFs compared to placebo.
Comorbidity
All trials recruited ‘healthy’ women. While safety data for the use of SNRIs in complex patients has been collected elsewhere, it will be important to establish efficacy and safety of NK3Ras in complex patients during phase 3 or post-market registry settings.
Washout of Prior HF Treatment
To avoid potential confounding effects, the FDA [36] advises different HRT washout periods depending on administration route. However, a washout was not specified in one SNRI trial [20], and too short a washout was used for one SNRI [27] and one NK3Ra trial [31], thus a spill-over effect may have occurred.
Placebo Control
The inclusion of a placebo arm comparator was validated after a marked reduction in HF frequency was noted after placebo administration in trials [SNRI range (across all 7 trials) 25–58%; NKR3a range 28–55%]. One method to attenuate a large placebo response may be to specify increased HF bother or a similar lifestyle measure as an inclusion criterion. Pinkerton et al. [25], for example, which had the lowest placebo response at week 12, required a score of ≥ 12 on the Greene Climacteric Scale (a standard questionnaire assessing physical and psychological menopausal symptoms) at study entry.
Power and Sample Size
All SNRI trials undertook a power calculation, except Evans et al. [20] which may have been underpowered as the reduction in HF frequency of 1.4/day was not statistically significant (p = 0.06), despite a statistically significant reduction in patient-perceived severity score. Initial NK3Ra trials lacked prior efficacy data to estimate treatment effect but instead used power calculations based on the ability to detect a treatment effect double the anticipated ~ 25% placebo effect [29] or based on previous HF diary trials [31]. Fraser et al. [32] powered based on prior NK3Ra efficacy [31], but, due to drop-out, failed to achieve the planned 40 subjects in 7/8 groups which may have affected 12-week HF severity evaluation (in which only 3 groups showed a significant reduction). Trower et al. [34] based sample size on a previous pilot study suggesting 8 subjects per group was adequate, but since the 150 mg group achieved all primary endpoints, the failure of 300 mg to show a statistically significant reduction in HF severity at week 12 may have been due to being underpowered.
HF Recording
All but three trials used retrospective paper diaries to assess HF frequency and severity. However, errors in compliance are major sources of bias and backfilling is common [37]. Prospective time-stamped electronic diaries may give superior timeliness and completion versus paper diaries [37] and were used in three trials [29, 31, 32]. Encouraging respondents to report HFs as they occur (as in one NK3Ra trial [29]), rather than at the end of the day/the following morning, also reduces recall bias.
Estimating Night Sweats
Use of the ‘number of night-time awakenings’ in SNRI [21–23] and NK3Ra trials [34] is problematic. Night-sweats may not produce full awakenings and may be under-reported. Disparity between subjective and objective reporting widens at night [38]. Thus, questionnaires such as MENQoL, which evaluate sleep quality [28, 30, 31, 33] may be useful since improved scores in ‘concentration’, ‘difficulty sleeping’, ‘tiredness’ and ‘lethargy’ correlate with HF therapeutic benefit and may more accurately reflect the impact on participants’ lives.
Discontinuation
If patient drop-out is high, statistical power may be lost. With SNRI trials, early discontinuation due to AEs, often due to nausea, was common (5–29%), especially during week 1. When treating depression, SNRIs are usually titrated over 1–2 months to reduce AEs [39]. It is surprising that only four of seven SNRI trials [20, 22, 25, 27] used titration and, even in those trials that did, the titration was very rapid (over 1 week) [22, 27]. In NK3Ra trials, early discontinuation due to AEs was uncommon (5–7%). Since HFs can continue for 12 years [4], longer trials with SNRIs and NK3Ras are warranted to evaluate long-term efficacy and tolerability/safety.
SNRI Tolerability and Safety
Most SNRI trials were short (≤ 12 weeks), apart from two trials which extended to 26 and 52 weeks, albeit with high dropout rates [23, 26]. Higher-dose SNRIs have been associated with treatment-emergent hypertension (likely due to increased potentiation of noradrenergic neurotransmission). A significant or numerical increase in blood pressure was reported in three SNRI trials [21, 22, 27], although none was powered to evaluate this endpoint (Table 4). A 1-year CV safety study among 2118 subjects with HFs [40] and pooled data from > 6000 subjects receiving desvenlafaxine for various indications [21] did not report a significant excess of CV events but 1 year may be too short; the Framingham Heart Study showed an association between ~ 10 mmHg increase in blood pressure and increased CV events took 4–6 years to emerge [41].
NK3Ra Tolerability and Safety
Since only short-duration phase 2 data have been published, it was not possible to fully evaluate NK3Ra tolerability and safety. In two trials, participants taking NK3Ras reported a higher frequency of minor GI disorders [31, 32], which could be related to NK3R expression in the GI tract [42]. However, the AE incidence did not appear dose-dependent. Somnolence was also more common (69% vs. 17%) with the highest (300 mg) dose of NT-814 [34] likely due to its additional NK1Ra action [43]. Interestingly, this could be an advantage for women with sleep disturbance. Asymptomatic rises in transaminases > 3 times the upper limit of normal were reported with MLE4901 [29] and fezolinetant [32] but bilirubin did not rise > 2 times upper limit of normal. Liver function tests (LFTs) returned to normal after drug discontinuation. However, further safety analyses are required.
Potential Study Bias
Overall risk of bias was low (Table 3). Selection bias was minimised by randomised study designs. Unreported data leading to potential reporting bias was noted, including pre-specified data on quality of life [21–23, 33], 50% HF responder rates [21] and apparent differences in gastrointestinal AE frequency in abstract versus table [31]. Potential conflicts of interest were considered under reporting bias but most trials declared conflicts and often had industry co-authors, which is common for these types of studies. All trials were double-blind (except one [20] using matched placebo) which should have reduced performance bias and detection bias, although this is difficult to fully exclude. One SNRI trial included an HRT arm [24] in which subjects experienced significant bleeding compared with the desvenlafaxine or placebo groups which likely unblinded treatment allocation. High drop rates of > 20% occurred in several trials [20, 21, 23, 24, 26, 29] leading to potential attrition bias [44], although this risk was reduced by appropriate use of intention-to-treat (ITT) or modified ITT rather than per-protocol analysis for primary outcomes.
Potential Additional Benefits of NK3Ra
Onset of Therapeutic Effect
Prague et al. [30] reported symptom improvement after ~ 48 h with NK3Ras, with maximum effect by day 3. Thus, NK3Ras would be expected to give earlier symptom relief versus SNRIs, especially given the slow dose titration recommended for SNRIs.
Sleep Quality/Concentration
Improved sleep ± concentration was noted in three NK3Ra trials [30, 31, 34]. This is likely attributed to multiple factors including reduced sleep disruption from HFs, and the attenuation of NK3R actions in melanin-concentrating hormone neurons (involved in the sleep–wake cycle) and in the prefrontal cortex, an important area for concentration [45], whereas the additional NK1Ra action of NT-814 may attenuate substance P-induced arousal and facilitate sleep [43]. In contrast, SNRIs are non-sedating [46], hence a reduction in night-time awakening with SNRIs is likely due to HF reduction and anxiolysis.
Mood
SNRIs improve depressed mood (another common menopausal symptom). Although it is unclear if NK3Ras directly affect mood, the NK1Ra action of NT-814 may be of benefit [47]. In addition to pharmacotherapy, it may also be worth considering cognitive behavioural therapy (CBT) if mood is a particularly limiting symptom, as the positive effects of CBT appear to be sustained over time [48].
CV Safety
After menopause, CV risk increases. In contrast to SNRIs which may be associated with hypertension leading to increased CV risk (discussed above), NK3Ras in rats reversed spontaneous hypertension and lowered heart rate [49] via reducing midbrain dopaminergic signalling in the ventral tegmental area that highly expresses NK3Rs [50]. Vasopressin neurones also express NK3Rs [51], and NKB activity is potentiated by thromboxane A2 [52] which might also represent useful therapeutic targets for NK3Ras.
Limitations of This Analysis
Conclusions of our qualitative analysis are limited by published data for NK3Ra being only phase 2 trials. Longer duration phase 3 trials are ongoing, and findings will provide further insights into efficacy and safety outcomes [53]. Availability of phase 3 NK3Ra data would also facilitate meta-analysis, enabling determination of a weighted pooled estimate for HF reduction in NK3Ra versus SNRI trials, although the ideal trial to compare NK3Ras versus SNRIs for reduction of menopausal HFs would be a large phase 3 head-to-head trial.
Conclusions
Menopausal HFs can significantly impact a woman’s quality of life, but some women cannot or do not wish to take HRT to alleviate their symptoms. Current non-hormonal options are suboptimal due to variable efficacy and low tolerability. The recent discovery that NKB-NK3R signalling is implicated in the generation of menopausal HFs has led to recent clinical trials using NK3Ras. Qualitative analysis of these trials indicates that NK3Ras lead to greater reductions in mean HF frequency, HF severity and night-sweats with good short-term tolerability compared to SNRIs. Efficacy and safety data (including careful evaluation of LFTs) from phase 3 trials are awaited with interest.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
Both authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Both authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SJM. The first draft of the manuscript was written by SJM. Both authors read and approved the final manuscript.
Disclosures
Sara J Menown and Javier A Tello have no conflicts to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Contributor Information
Sara J. Menown, Email: sjmenown@gmail.com
Javier A. Tello, Email: jt65@st-andrews.ac.uk
References
- 1.Makara-Studzińśka MT, Kryś-Noszczyk KM, Jakiel G. Epidemiology of the symptoms of menopause—an intercontinental review. Menopause Rev/Przegląd Menopauzalny. 2014;13(3):203–211. doi: 10.5114/pm.2014.43827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avis NE, Crawford SL, Greendale G, Bromberger JT, Everson-Rose SA, Gold EB, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015;175(4):531–539. doi: 10.1001/jamainternmed.2014.8063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stearns V, Ullmer L, López JF, Smith Y, Isaacs C, Hayes D. Hot flushes. Lancet. 2002;360(9348):1851–1861. doi: 10.1016/S0140-6736(02)11774-0. [DOI] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence (NICE). Menopause: diagnosis and management [NG23] [Internet]. 2015. https://www.nice.org.uk/guidance/ng23. Accessed 11 Aug 2021.
- 5.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA. 2002;288(3):321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 6.Stuenkel CA, Davis SR, Gompel A, Lumsden MA, Murad MH, Pinkerton JV, et al. Treatment of symptoms of the menopause: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(11):3975–4011. doi: 10.1210/jc.2015-2236. [DOI] [PubMed] [Google Scholar]
- 7.Royal College of Obstetricians and Gynaecologists. Alternatives to HRT for the Management of Symptoms of the Menopause [Scientific Impact Paper No. 6] [Internet]. 2010. https://www.rcog.org.uk/globalassets/documents/guidelines/scientific-impact-papers/sip_6.pdf. Accessed 18 Feb 2021.
- 8.Topaloglu AK, Tello JA, Kotan LD, Ozbek MN, Yilmaz MB, Erdogan S, et al. Inactivating KISS1 mutation and hypogonadotropic hypogonadism. N Engl J Med. 2012;366(7):629–635. doi: 10.1056/NEJMoa1111184. [DOI] [PubMed] [Google Scholar]
- 9.Moore AM, Coolen LM, Porter DT, Goodman RL, Lehman MN. KNDy cells revisited. Endocrinology. 2018;159(9):3219–3234. doi: 10.1210/en.2018-00389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skorupskaite K, George JT, Anderson RA. The kisspeptin-GnRH pathway in human reproductive health and disease. Hum Reprod Update. 2014;20(4):485–500. doi: 10.1093/humupd/dmu009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krajewski SJ, Burke MC, Anderson MJ, McMullen NT, Rance NE. Forebrain projections of arcuate neurokinin B neurons demonstrated by anterograde tract-tracing and monosodium glutamate lesions in the rat. Neuroscience. 2010;166(2):680–697. doi: 10.1016/j.neuroscience.2009.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rance NE, Dacks PA, Mittelman-Smith MA, Romanovsky AA, Krajewski-Hall SJ. Modulation of body temperature and LH secretion by hypothalamic KNDy (kisspeptin, neurokinin B and dynorphin) neurons: a novel hypothesis on the mechanism of hot flushes. Front Neuroendocrinol. 2013;34(3):211–227. doi: 10.1016/j.yfrne.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baber RJ, Panay N, Fenton A. 2016 IMS recommendations on women's midlife health and menopause hormone therapy. Climacteric. 2016;19(2):109–150. doi: 10.3109/13697137.2015.1129166. [DOI] [PubMed] [Google Scholar]
- 14.Woyka J. Consensus statement for non-hormonal based treatments for menopausal symptoms. Post Reprod Health. 2020;26(3):137–141. doi: 10.1177/2053369120930508. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freeman EW, Ensrud KE, Larson JC, Guthrie KA, Carpenter JS, Joffe H, et al. Placebo improvement in pharmacologic treatment of menopausal hot flashes: time course, duration, and predictors. Psychosom Med. 2015;77(2):167–175. doi: 10.1097/PSY.0000000000000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Critical Appraisal Skills Programme. CASP Randomised Controlled Trials Checklist [Internet]. 2019. https://casp-uk.net/casp-tools-checklists/. Accessed 11 Aug 2021.
- 18.Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Churchill R, Chandler J, Cumpston MS (editors), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017) [Internet]. 2017. https://training.cochrane.org/handbook. Accessed 11 Aug 2021.
- 19.Lensen S, Archer D, Bell RJ, Carpenter JS, Christmas M, Davis SR, et al. A core outcome set for vasomotor symptoms associated with menopause: the COMMA (Core Outcomes in Menopause) global initiative. Menopause. 2021 doi: 10.1097/GME.0000000000001787. [DOI] [PubMed] [Google Scholar]
- 20.Evans ML, Pritts E, Vittinghoff E, McClish K, Morgan KS, Jaffe RB. Management of postmenopausal hot flushes with venlafaxine hydrochloride: a randomized, controlled trial. Obstet Gynecol. 2005;105(1):161–166. doi: 10.1097/01.AOG.0000147840.06947.46. [DOI] [PubMed] [Google Scholar]
- 21.Speroff L, Gass M, Constantine G, Olivier S. Efficacy and tolerability of desvenlafaxine succinate treatment for menopausal vasomotor symptoms: a randomized controlled trial. Obstet Gynecol. 2008;111(1):77–87. doi: 10.1097/01.AOG.0000297371.89129.b3. [DOI] [PubMed] [Google Scholar]
- 22.Archer DF, Seidman L, Constantine GD, Pickar JH, Olivier S. A double-blind, randomly assigned, placebo-controlled study of desvenlafaxine efficacy and safety for the treatment of vasomotor symptoms associated with menopause. Am J Obstetr Gynecol. 2009;200(2):172.e1–.e10. doi: 10.1016/j.ajog.2008.09.877. [DOI] [PubMed] [Google Scholar]
- 23.Archer DF, Dupont CM, Constantine GD, Pickar JH, Olivier S. Desvenlafaxine for the treatment of vasomotor symptoms associated with menopause: a double-blind, randomized, placebo-controlled trial of efficacy and safety. Am J Obstetr Gynecol. 2009;200(3):238.e1–.e10. doi: 10.1016/j.ajog.2008.10.057. [DOI] [PubMed] [Google Scholar]
- 24.Bouchard P, Panay N, De Villiers TJ, Vincendon P, Bao W, Cheng RJ, et al. Randomized placebo- and active-controlled study of desvenlafaxine for menopausal vasomotor symptoms. Climacteric. 2012;15(1):12–20. doi: 10.3109/13697137.2011.586445. [DOI] [PubMed] [Google Scholar]
- 25.Pinkerton JV, Constantine G, Hwang E, Cheng RFJ. Desvenlafaxine compared with placebo for treatment of menopausal vasomotor symptoms: A 12-week, multicenter, parallel-group, randomized, double-blind, placebo-controlled efficacy trial. Menopause. 2013;20(1):28–37. doi: 10.1097/gme.0b013e31826421a8. [DOI] [PubMed] [Google Scholar]
- 26.Pinkerton JV, Archer DF, Guico-Pabia CJ, Hwang E, Cheng RFJ. Maintenance of the efficacy of desvenlafaxine in menopausal vasomotor symptoms: A 1-year randomized controlled trial. Menopause. 2013;20(1):38–46. doi: 10.1097/gme.0b013e318274699f. [DOI] [PubMed] [Google Scholar]
- 27.Joffe H, Guthrie KA, LaCroix AZ, Reed SD, Ensrud KE, Manson JE, et al. Low-dose estradiol and the serotonin-norepinephrine reuptake inhibitor venlafaxine for vasomotor symptoms: a randomized clinical trial. JAMA Intern Med. 2014;174(7):1058–1066. doi: 10.1001/jamainternmed.2014.1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Caan B, Lacroix AZ, Joffe H, Guthrie KA, Larson JC, Carpenter JS, et al. Effects of estrogen and venlafaxine on menopause-related quality of life in healthy postmenopausal women with hot flashes: a placebo-controlled randomized trial. Menopause. 2015;22(6):607–615. doi: 10.1097/GME.0000000000000364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prague JK, Roberts RE, Comninos AN, Clarke S, Jayasena CN, Nash Z, et al. Neurokinin 3 receptor antagonism as a novel treatment for menopausal hot flushes: a phase 2, randomised, double-blind, placebo-controlled trial. The Lancet. 2017;389(10081):1809–1820. doi: 10.1016/S0140-6736(17)30823-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prague JK, Roberts RE, Comninos AN, Clarke S, Jayasena CN, Mohideen P, et al. Neurokinin 3 receptor antagonism rapidly improves vasomotor symptoms with sustained duration of action. Menopause (N Y, NY) 2018;25(8):862–869. doi: 10.1097/GME.0000000000001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Depypere H, Timmerman D, Donders G, Sieprath P, Ramael S, Combalbert J, et al. Treatment of menopausal vasomotor symptoms with fezolinetant, a neurokinin 3 receptor antagonist: a phase 2a trial. J Clin Endocrinol Metab. 2019;104(12):5893–5905. doi: 10.1210/jc.2019-00677. [DOI] [PubMed] [Google Scholar]
- 32.Fraser GL, Lederman S, Waldbaum A, Kroll R, Santoro N, Lee M, et al. A phase 2b, randomized, placebo-controlled, double-blind, dose-ranging study of the neurokinin 3 receptor antagonist fezolinetant for vasomotor symptoms associated with menopause. Menopause (N Y, NY) 2020;27(4):382–392. doi: 10.1097/GME.0000000000001510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Santoro N, Waldbaum A, Lederman S, Kroll R, Fraser GL, Lademacher C, et al. Effect of the neurokinin 3 receptor antagonist fezolinetant on patient-reported outcomes in postmenopausal women with vasomotor symptoms: results of a randomized, placebo-controlled, double-blind, dose-ranging study (VESTA) Menopause (N Y, NY) 2020;27(12):1350–1356. doi: 10.1097/GME.0000000000001621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trower M, Anderson RA, Ballantyne E, Joffe H, Kerr M, Pawsey S. Effects of NT-814, a dual neurokinin 1 and 3 receptor antagonist, on vasomotor symptoms in postmenopausal women: a placebo-controlled, randomized trial. Menopause (N Y, NY) 2020;27(5):498–505. doi: 10.1097/GME.0000000000001500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gold EB, Colvin A, Avis N, Bromberger J, Greendale GA, Powell L, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women's health across the nation. Am J Public Health. 2006;96(7):1226–1235. doi: 10.2105/AJPH.2005.066936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research. Guidance for industry—estrogen and estrogen/progestin drug products to treat vasomotor symptoms and vulvar and vaginal atrophy symptoms—recommendations for clinical evaluation [Internet]. 2003. https://www.fda.gov/media/71359/download. Accessed 28 Feb 2021.
- 37.Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient compliance with paper and electronic diaries. Control Clin Trials. 2003;24(2):182–199. doi: 10.1016/S0197-2456(02)00320-3. [DOI] [PubMed] [Google Scholar]
- 38.Regestein QR. Hot flashes and sleep. Menopause. 2006;13(4):549–552. doi: 10.1097/01.gme.0000227395.30321.ff. [DOI] [PubMed] [Google Scholar]
- 39.Electronic medicines compendium [Internet]. 2021. https://www.medicines.org.uk/emc/. Accessed 11 Aug 2021.
- 40.Archer DF, Pinkerton JV, Guico-Pabia CJ, Hwang E, Cheng RFJ. Cardiovascular, cerebrovascular, and hepatic safety of desvenlafaxine for 1 year in women with vasomotor symptoms associated with menopause. Menopause. 2013;20(1):47–56. doi: 10.1097/gme.0b013e3182775fe9. [DOI] [PubMed] [Google Scholar]
- 41.Vasan RS, Larson MG, Leip EP, Evans JC, O'Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345(18):1291–1297. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 42.Jaafari N, Hua G, Adélaïde J, Julé Y, Imbert J. Expression of the tachykinin receptor mRNAs in healthy human colon. Eur J Pharmacol. 2008;599(1–3):121–125. doi: 10.1016/j.ejphar.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 43.Ratti E, Carpenter DJ, Zamuner S, Fernandes S, Squassante L, Danker-Hopfe H, et al. Efficacy of vestipitant, a neurokinin-1 receptor antagonist, in primary insomnia. Sleep. 2013;36(12):1823–1830. doi: 10.5665/sleep.3208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schulz KF, Grimes DA. Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet. 2002;359(9308):781–785. doi: 10.1016/S0140-6736(02)07882-0. [DOI] [PubMed] [Google Scholar]
- 45.Cvetkovic V, Poncet F, Fellmann D, Griffond B, Risold PY. Diencephalic neurons producing melanin-concentrating hormone are influenced by local and multiple extra-hypothalamic tachykininergic projections through the neurokinin 3 receptor. Neuroscience. 2003;119(4):1113–1145. doi: 10.1016/S0306-4522(03)00146-5. [DOI] [PubMed] [Google Scholar]
- 46.Wichniak A, Wierzbicka A, Walęcka M, Jernajczyk W. Effects of antidepressants on sleep. Curr Psychiatry Rep. 2017;19(9):63. doi: 10.1007/s11920-017-0816-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ratti E, Bettica P, Alexander R, Archer G, Carpenter D, Evoniuk G, et al. Full central neurokinin-1 receptor blockade is required for efficacy in depression: evidence from orvepitant clinical studies. J Psychopharmacol. 2013;27(5):424–434. doi: 10.1177/0269881113480990. [DOI] [PubMed] [Google Scholar]
- 48.Hunter MS. Cognitive behavioral therapy for menopausal symptoms. Climacteric. 2021;24(1):51–56. doi: 10.1080/13697137.2020.1777965. [DOI] [PubMed] [Google Scholar]
- 49.Lessard A, Campos MM, Neugebauer W, Couture R. Implication of nigral tachykinin NK3 receptors in the maintenance of hypertension in spontaneously hypertensive rats: a pharmacologic and autoradiographic study. Br J Pharmacol. 2003;138(4):554–563. doi: 10.1038/sj.bjp.0705042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Brito GH, Couture R. Blockade of tachykinin NK3 receptor reverses hypertension through a dopaminergic mechanism in the ventral tegmental area of spontaneously hypertensive rats. Br J Pharmacol. 2010;161(8):1868–1884. doi: 10.1111/j.1476-5381.2010.01008.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pineda R, Sabatier N, Ludwig M, Millar RP, Leng G. A direct neurokinin B projection from the arcuate nucleus regulates magnocellular vasopressin cells of the supraoptic nucleus. J Neuroendocrinol. 2016;28:4. doi: 10.1111/jne.12342. [DOI] [PubMed] [Google Scholar]
- 52.Pal S, Wu J, Murray JK, Gellman SH, Wozniak MA, Keely PJ, et al. An antiangiogenic neurokinin-B/thromboxane A2 regulatory axis. J Cell Biol. 2006;174(7):1047–1058. doi: 10.1083/jcb.200603152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Prague JK. Neurokinin 3 receptor antagonists—prime time? Climacteric. 2021;24(1):25–31. doi: 10.1080/13697137.2020.1834530. [DOI] [PubMed] [Google Scholar]