Abstract
Emotion dysregulation mediates the effects of stress on drinking among individuals with co-occurring emotional and alcohol use disorders (AUD). The current study examined the effects of cognitive reappraisal (CR), an adaptive emotion regulation strategy, on mechanisms that contribute to drinking (alcohol craving, inhibitory control) among 50 women veterans. In session one, participants were randomized to one of two 50-min “microinterventions”, either to learn a CR coping strategy or receive non-therapeutic psychoeducation control. In session two, all participants underwent a personalized stress induction, after which women in the experimental condition were instructed to use CR to reduce stress, while those in the control group were instructed to sit quietly. Craving and inhibitory control were measured at post-stress induction and after using CR/sitting quietly. Moderating effects of AUD, depression, and PTSD severity were assessed. Craving and inhibitory control improved among women in both conditions (CR or sitting quietly), with no main effect of condition. Condition by AUD severity had a significant interaction effect (b = 0.018, p = .013), whereby women with more severe AUD had greater decreases in craving after sitting quietly, and women with less severe AUD had greater decreases in craving after CR. The opposite pattern was observed for inhibitory control (b = 6.45, p = .004), with women with less severe AUD having greater decreases in inhibitory control after sitting quietly, and women with more severe AUD having greater decreases in inhibitory control after CR. Results highlight CR’s immediate effects on alcohol-related outcomes and the important role of symptom severity.
Keywords: Women, Veterans, Alcohol, Emotion regulation, Cognitive reappraisal, Stress, Posttraumatic stress disorder
1. Introduction
The national prevalence rate of alcohol use disorder (AUD) among women increased by 84% between 2000 and 2013 (Grant et al., 2016). Heightened rates of AUD among women are also found for military veterans, with lifetime rates of AUD at 27% for both men and women veterans (Evans, Upchurch, Simpson, et al., 2018), despite historically higher rates for men. Additionally, among Army service members, 9.1% of women who use alcohol tend to drink at unhealthy levels compared to 5.1% of men who use alcohol (where unhealthy drinking is defined as 7 or more drinks per week for women, 14 or more for men) (Lande, Marin, Chang, et al., 2007). Clinically, female military service members and veterans have unique life experiences and symptoms (e.g., high rates of trauma, posttraumatic stress disorder/PTSD, depression, and daily stressors) that require a tailored treatment approach (Timko et al., 2017).
Indeed, stress and negative emotion (broadly referred to as negative affect) and trauma exposure are more consistently associated with drinking and the development of AUD among veteran and civilian women compared to men (Peltier et al., 2019), and these effects of negative affect on drinking are mediated by various factors (Guinle & Sinha, 2020). After personalized stress inductions, women who use substances have been shown to experience more craving compared to men who use substances (Rubonis et al., 1994; Saladin et al., 2012). Cognitively, stress and strong emotion deplete inhibitory control, which is one facet of executive functioning that reflects the ability to suppress ongoing or planned cognitive or behavioral processes (Hartmann, Sallard, & Spierer, 2016). Women who drink heavily have particularly low baseline (i.e., at a resting state) levels of inhibitory control compared to men who drink heavily and to non-drinking men or women (Weafer, De Arcangelis, & de Wit, 2015). Thus, alcohol craving and inhibitory control are two mechanisms that mediate the effect of negative affect on alcohol use for women (Guinle & Sinha, 2020).
Clinically, therefore, targeting negative affect may be an important treatment element for women veterans with unhealthy alcohol use. Improving a patient’s ability to tolerate and regulate emotional states (via improving emotion regulation skills) may directly and indirectly reduce the risk for unhealthy drinking, and this may be especially true for those with co-occurring emotional disorders. Emotion dysregulation has been posited as a transdiagnostic construct that helps explain the cooccurrence of PTSD, depression, and AUD (Fairholme, Nosen, Nillni, et al., 2013; Westphal, Aldao, & Jackson, 2017), and such co-occurring conditions are more prevalent among women (civilian and veteran) than men with AUD (Goldstein, Dawson, Chou, & Grant, 2012; Kalpakci, Sofuoglu, Petrakis, & Rosenheck, 2019; Karpyak et al., 2016). Among individuals with substance use disorders, emotion dysregulation has been shown to mediate the associations of negative affect with drinking to cope (Veilleux, Skinner, Reese, & Shaver, 2014) and substance cravings (Weiss, Sullivan, & Tull, 2015). Compared to those with substance use disorder only, individuals with substance use disorders and PTSD demonstrate greater difficulty engaging in goal-directed behavior and impulse control difficulties when distressed (Fairholme et al., 2013; N.H. Weiss, Tull, Viana, Anestis, & Gratz, 2012). Likewise, individuals with depression are less likely to use adaptive emotion regulation strategies and more likely to use maladaptive strategies such as rumination or emotional suppression (Eftekhari, Zoellner, & Vigil, 2009; Nolen-Hoeksema, 2012). Explicitly teaching adaptive emotion regulation strategies may be an important intervention for the growing population of women veterans with unhealthy alcohol use, especially those with co-occurring conditions.
Cognitive reappraisal (CR) is one adaptive emotion regulation strategy in which an individual generates alternative interpretations of (i.e., reappraises) an emotion-eliciting situation to down-regulate negative affect. The positive effects of CR on negative affect have been studied extensively (Beadman et al., 2015; Buhle et al., 2014; Denny, Inhoff, Zerubavel, Davachi, & Ochsner, 2015; Koch et al., 2007; Naqvi et al., 2015; Ray, McRae, Ochsner, & Gross, 2010), with CR diminishing the effects of negative affect at the physiological, subjective, and neurological level. These studies have provided brief instructions to participants on how to use CR, in order to examine its acute effect. For example, these studies have provided brief, five-sentence instructions on how to use CR (e.g., “think about the picture in a way that decreases your negative response to it”) or have provided instructional booklets to participants on using CR. Participants then execute these strategies in the lab and the acute effects are examined. In addition to decreasing negative emotion, CR has been found to improve inhibitory control in non-clinical samples (Buhle et al., 2014; Ray et al., 2010). Indeed, CR has strong evidence for its acute, immediate effects on negative emotion and related outcomes. CR is also an antecedent-focused emotion regulation strategy (Gross, 2001), meaning that it can be used before a behavioral response to a stressful stimulus is fully activated. Alternatively, a response-focused emotion regulation skill (e.g., distracting oneself, using relaxation skills) is an attempt at regulating emotion after the emotion is already underway (Gross, 2001). This distinction is important, as use of antecedent-focused emotion regulation has been shown to more effectively decrease negative emotion states and more effectively reduce behavioral expression of emotion (e.g., fighting, yelling, drinking) (Gross, 2001). To our knowledge, the effect of CR of negative emotion (distinct from cognitive reappraisal of alcohol-related thoughts) has not be experimentally studied in relation to alcohol use or alcohol-related outcomes. While stress and emotion regulation interventions have more recently been formally incorporated into AUD treatments (e.g., Epstein, McCrady, Hallgren, et al., 2018; Stasiewicz et al., 2013), patients are often taught how to avoid drinking in response to stress (Larimer & Palmer, 1999), with less focus on antecedent-focused emotion regulation strategies that down-regulate negative affect. Additionally, the mechanisms by which emotion regulation interventions may work have not been established or examined among women veterans or individuals with unhealthy or problematic alcohol use.
The current study used a microintervention design to examine the effects of CR on two mediators of the stress-drinking association, inhibitory control and alcohol craving, among women veterans. A microintervention design is an example of micro-analysis in which a therapeutic strategy is isolated in order to examine its acute effects on relevant outcomes (Strauman et al., 2015). Strauman et al. (2015) used a microintervention design to test effects of interventions for individuals with anxiety and dysphoria symptoms. In one proof-of-concept paper reporting two studies, participants were trained during one session to use skills to reduce dysphoric and anxious symptoms and affect was measured before and after; the second study provided brief instructions on these skills and then tested the acute effect of using that skill in the lab. Both studies found differing patterns of distress reduction that were consistent with hypotheses. Another study used a microintervention design to test the effects of cognitive restructuring (compared to two control groups) on affect and event-related potentials in frontal lobe regions among participants with low versus high severity of dysphoria (Zaunmüller, Lutz, & Strauman, 2014). They found no main condition effects on affect but did show differential effects of condition on frontal lobe region activity that were dependent on dysphoria severity. Additional studies with non-substance using samples have used micro-interventions (targeting anxiety and teaching mindfulness) to examine clinical severity as a moderating factor (Kivity & Huppert, 2016; Van Cappellen, Catalino, & Fredrickson, 2020). Thus, microintervention designs have been used in depression and anxiety treatment research (e. g., T. J. Strauman et al., 2013) but have not been utilized among patients with alcohol-related problems. While the term microintervention is relatively new, many studies (including those described above: Beadman et al., 2015; Naqvi et al., 2015; Ray et al., 2010; Szasz, Szentagotai, & Hofmann, 2012) have examined the acute, immediate impact of CR and cognitive restructuring in the laboratory using instructions that are briefer than a microintervention, the latter of which is typically the length of a therapy session (i.e., 45–60 min). Even with briefer training, those randomized controlled studies have demonstrated psychological and biological effects of using CR in the lab.
The current study tests the following hypotheses: Hypothesis 1: Following a personalized stress/negative emotion induction, participants in the CR experimental condition will report more reductions in alcohol cravings (hypothesis 1a) and increases in inhibitory control (hypothesis 1b), compared to a control of sitting quietly; Hypothesis 2: Severity of clinical symptoms – AUD, depression, and PTSD – will serve as moderators of CR’s effect on outcomes; specifically, CR will have greater therapeutic effect (compared to the control condition) on alcohol craving (hypothesis 2a) and inhibitory control (hypothesis 2b) for women veterans with more severe AUD, depression, and/or PTSD baseline symptoms.
2. Methods and materials
2.1. Participants
Fifty women veterans participated in the study (Fig. 1). Inclusion criteria included: (1) Age 18 or older; (2) Current unhealthy alcohol use, defined as scoring 3 or higher on the Alcohol Use Disorders Identification Test – Concise (AUDIT-C) [note: women veterans with AUDIT-C scores of 3+ have been found to have increased rates of alcohol-related consequences and blackouts, tolerance, and self-reported need to cut down on use (Chavez, Williams, Lapham, & Bradley, 2012)]; the average full AUDIT score for this sample was 15.80 (SD = 10.25)]; (4) If using other illicit substances, identify alcohol as their primary substance of choice (to reduce variability in terms of baseline craving); (5) Alcohol use in the past 45 days; (6) Able to write and speak in English; and (7) Served in the U.S. Military. Exclusion Criteria were: (1) Severe mental illness (psychotic symptoms and/or uncontrolled bipolar disorder); (2) Brain injury or physical limitation that affected ability to complete the computerized task; (3) Current suicidal ideation or intent; (4) Pregnancy.
Fig. 1.
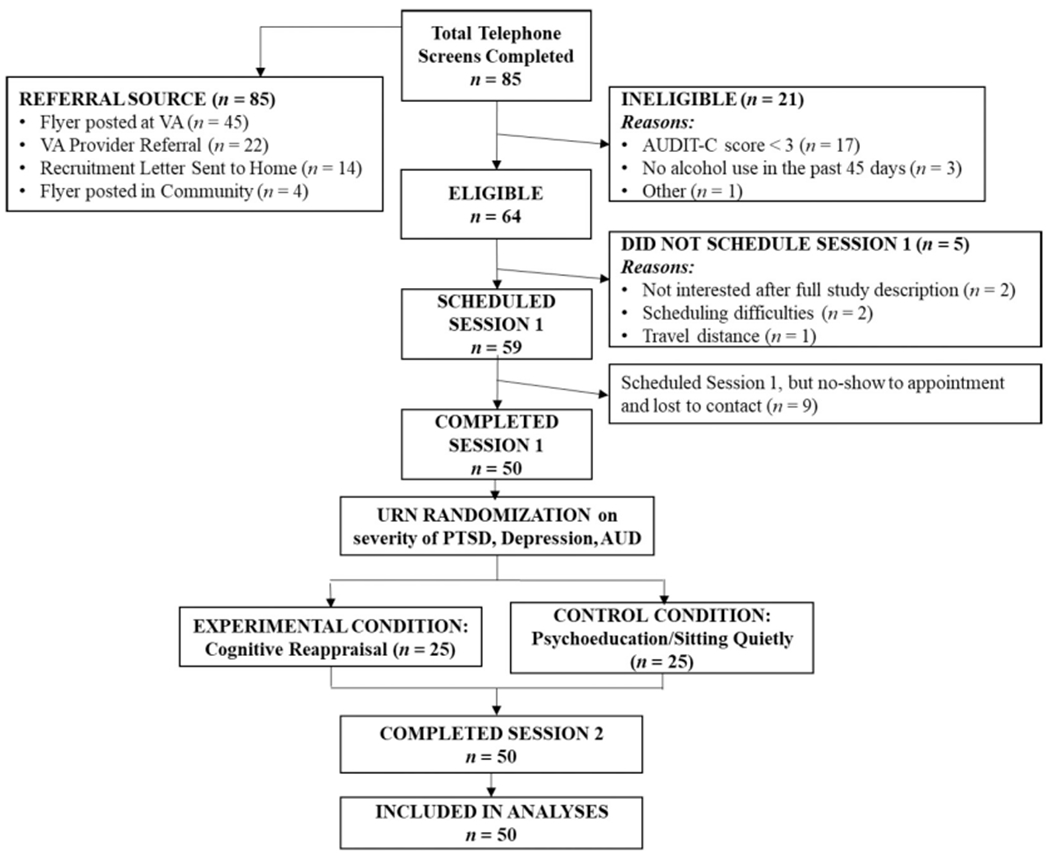
CONSORT table.
2.2. Procedures
See Fig. 2 for procedure outline. The study took place over two research sessions, scheduled approximately three days apart. Flyers, provider referrals, and letters sent to potentially eligible women (as indicated by report of regular alcohol use in their VA medical records) were used to recruit women veterans. An initial phone screen was then completed, and any eligible participants were scheduled for research session 1. During research session 1, the participant signed informed consented and completed self-report measures, including the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996) and PTSD Checklist (PCL-5; Weathers et al., 2013), and a baseline behavioral measure of inhibitory control. The participant then developed, with a study clinician, a personalized negative emotion script by describing the details of a recent, day-to-day stressful experience (using a manualized stress induction procedure by Sinha & Tuit, 2012). Consistent with the protocol, the stressful experience must be rated by the participant as an 8 or higher on a scale of 0 (not at all stressful) – 10 (the most stressful event you have experienced). The story is told to the clinician by the participant in detail, so that study staff can then re-write the story into an audio script that is played to the participant in research session 2, in order to induce negative emotion and stress. Traumatic events were not allowed to be used as the stressful experience for several reasons: (1) Not all participants had PTSD or equivalent trauma exposure; (2) Responses to non-traumatic stressors are qualitatively different than responses to traumatic stressors, with the focus of the study being on the former; (3) Given the high rates of traumatic exposure and PTSD in this population, we did not want to evoke a traumatic memory as this was not a treatment study; (4) It is also part of the protocol (Sinha & Tuit, 2012) that traumatic events not be allowed. (See the preliminary results section for details about stressful events chosen by participants in this study.)
Fig. 2.
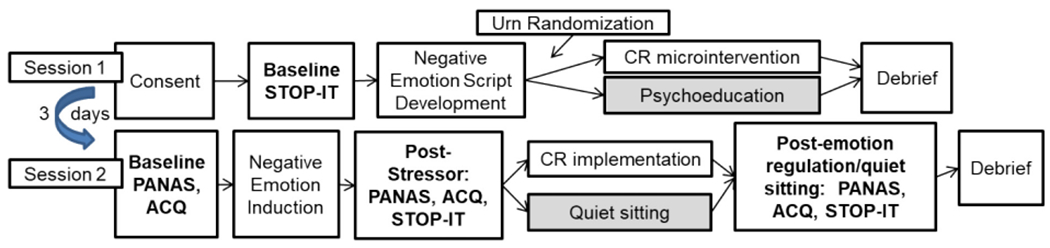
Study procedures
Note: Bolded items indicate measurement of outcome variables, including STOP-IT (behavioral measure of inhibitory control), and ACQ (self-report alcohol craving). PANAS, a self-report measure of negative affect, administered as well. See Methods for details. CR = Cognitive Reappraisal. Grey boxes = control group.
At the end of research session 1, the participant was randomized to receive either the CR microintervention (if in the experimental condition) or the control psychoeducation condition (see below for details regarding the session material). Urn randomization was implemented using R package randomizeR based on BDI, PCL, and AUDIT total score, to allow for balanced symptom severity between groups in order to analyze hypothesis 2; participants were stratified based on established clinical cut-offs for each measure: BDI (<20 no/low depression; 20+ moderate-high depression), PCL (<33 no/low PTSD, 33+ moderate-high PTSD), and AUDIT (<8 low AUD, 8+ high AUD). Once stratified, the urn randomization program performed independent randomization, with replacement, within each stratum as participants were recruited to the study.
During research session 2, each participant in both conditions listened to her personalized stress script and then completed measures of alcohol craving and inhibitory control (referred to as “post-stressor”). Each participant in both conditions then listened to the stress induction once again. Study staff then asked women in the experimental condition (n = 25) to implement the CR strategy for six minutes. During these six minutes, women in the CR condition completed a worksheet as they were taught in session 1 CR microintervention to assist them in applying CR to reduce stress. After the second stress induction, staff instructed women in the control condition (n = 25, who did not receive the CR microintervention in session 1) to sit quietly for six minutes. After the second presentation of the personalized stress induction and subsequent implementation of CR (in the experimental condition) or “sitting quietly” (in the control condition), participants completed the measures of inhibitory control and alcohol craving once more (this assessment wave is referred to as “post-CR/sitting quietly”).
2.3. Study conditions
Both microintervention protocols delivered in session 1 were manualized, lasted 50 min, and were delivered by one of four therapists who had graduate level (MA or doctoral) training in clinical psychology. All therapists were cross-trained by the first author to deliver both study conditions’ manuals. The first author also attended each therapist’s first two sessions for each condition for training and feedback.
2.3.1. Cognitive reappraisal microintervention (research session 1)
The cognitive reappraisal session in Barlow et al.’s (2011) Unified Protocol for the Treatment of Emotional Disorders was adapted for use in the study. CR is a strategy that emphasizes the importance of attending to one’s automatic appraisals of a stressful situation and identifying potential “thinking traps” (e.g., catastrophizing, overestimation). The reappraisal entails generating, or allowing for, alternative, less negative, appraisals. For example, after a fight with a significant other one may have the automatic, catastrophic appraisal of, “the relationship is over”; a reappraisal in this case may be “arguments are normal, it doesn’t necessarily mean that the relationship is over”. The session content includes: (1) Introduction to CR as a strategy one can use to regulate negative emotion after a stressful or distressing experience, and setting an agenda for the next 50 min; (2) Introducing “thinking traps” that prevent reappraisal and maintain negative emotion; (3) Teaching CR as an adaptive emotion regulation strategy; (4) Teaching the CR process (identifying: situation→ negative appraisal→ negative emotion→ thinking trap→ CR /generate alternative appraisals); (5) Having participants practice CR using a structured worksheet, focused on their personalized stress story. Participants are given copies of the CR workbook, including the worksheet, and were encouraged to read over the material again before their next session. However, this “homework” was not an emphasis or monitored in anyway as it was expected the participant would have a full understanding of how to use CR by the end of the microintervention so that she would be able to use it during session 2.
2.3.2. Attention-control psychoeducation condition (research session 1)
In order to control for potential effects of study staff attention during the session 1 CR microintervention in the experimental group, the control group (which ultimately sits quietly during session 2) received 50 min of psychoeducation during session 1, at the time when the experimental group would be learning CR. The psychoeducation protocol was derived from two sources: (1) Session 1 of the Women’s Health Education Manual (Miller, Pagan, & Tross, 1998), providing education about the main body systems and their functions, and (2) Fact sheets published by the American College of Obstetricians and Gynecologists American College of Obstetricians and Gynecologists, 2017, providing information about gender and health, female-specific health education, and making the most of primary care visits. None of this information discussed alcohol or other substance use. The content of the session was the review of basic body systems and discussing the effects of gender on health (e.g., discussing the influence of gender and sex differences in terms of physical health). Participants received worksheets to take home regarding topics to discuss at well-woman visits and information about when certain health screenings (e.g., mammography) should occur; as with the CR group, they were not explicitly provided any homework.
2.3.3. Cognitive reappraised implementation (research session 2)
In research session 2, participants in the CR condition were given six minutes to implement the CR strategy after the stress induction. As reviewed, past research has demonstrated that very brief use of CR has acute effects on various physiological, neural, and subjective outcomes (Beadman et al., 2015; Naqvi et al., 2015; Ray et al., 2010; Szasz et al., 2012). However, the current study procedures required participants to complete a worksheet to help them use CR and also to track the quality of how well they executed reappraisal; therefore, a longer time was needed for participants to execute the CR strategy in the experimental session. Six minutes was selected to match the stress induction timeframe outlined in Sinha and Tuit (2012), a timeframe which was established based on objective neuro-chemical (e.g., in salivary cortisol, plasma measurements) and neurobiological activation during emotion induction procedures. Participants were provided a blank worksheet that walks them through the process of CR (described above) and asked to use their CR skills that they learned in the previous session with regard to the script they just listened to, writing down their thoughts as they work through the thought chain. This was intended to focus them on CR and allowed researchers to check appropriate use of the strategy (as used in previous CR research; Beadman et al., 2015; Naqvi et al., 2015). The quality of participants’ uses of CR (via worksheet completion) was independently rated by two clinicians. Specifically, each of five “steps” of the CR process was scored on a three-point Likert scale as to whether the participant achieved that step (coded 1, 2, 3 as all participants provided some information for each step; anchors varied for each step); thus, the potential range of total CR quality scores was 4–12. The two clinicians gave the same rating on 78% of all scored items, across participants; on any items not scored the same, the mean difference in rating was 1.0 (SD = 1.2). For the items with disagreement, an average score (average of the two scoring clinicians) was used to generate the participant’s total score. These CR quality scores were used as a check of the microintervention, whether participants were able to use the strategy after one session.
2.4. Baseline measures
2.4.1. Timeline follow-back (Sobell & Sobell, 1996; TLFB)
The TLFB uses a calendar and other memory aids to determine an individual’s drinking over a specified time. At baseline, participants were interviewed about their alcohol use on each of the 45 days prior session 1. The TLFB has excellent reliability (Sobell & Sobell, 1992) and validity for alcohol use (Sobell et al., 1992). TLFB data were used to calculate baseline percentage of days drinking (PDD, used as a covariate) and mean drinks per drinking day (MDPDD).
2.4.2. PTSD Checklist for DSM-5 with Criterion A and Life Events Checklist (Weathers et al., 2013; PCL-5/LEC)
The PCL-5 is a 20-item self-report measure of DSM-5 PTSD symptoms. Participants rate each item on a scale of 0–4 for each symptom, reflecting whether they experience the symptom on a range from “Not at all” to “Extremely.” On the Life Events Checklist for DSM-5 (LEC-5) participants check whether they have experienced a number of potentially traumatic events; the Criterion A assessment asks questions regarding their most difficult life event, in order to determine whether the event meets Criterion A of the DSM-5 PTSD diagnosis. The PCL is scored by totaling each item (range 0–80), reflecting severity of PTSD symptoms. A PCL-5 cutoff score between 31 and 33 is indicative of probable PTSD. A provisional PTSD diagnosis can be assessed using the PCL, Criterion A questions, and LEC. Cronbach alpha for the PCL in this sample was 0.93.
2.4.3. Alcohol use disorders identification test (Saunders, Aasland, Babor, et al., 1993; AUDIT)
The AUDIT is a 10-item tool developed by the World Health Organization to assess alcohol consumption, drinking behaviors, and alcohol-related problems. The first three questions comprise the AUDIT-C, used in eligibility screening for this study. Items are scored on a scale of 0–4, reflecting the frequency or intensity of alcohol use and alcohol-related problems. A summed total score for the full AUDIT is calculated with a range of 0–40; a total of 8 or more indicates hazardous or harmful alcohol use and 15 or more of moderate-severe AUD. The Cronbach alpha for the current sample was 0.90.
2.4.4. Beck Depression Inventory-II (Beck et al., 1996; BDI)
The BDI-II is a 21-item measures that assess the severity of depressive symptoms in the last two weeks. Each item is rated on a scale from 0 (non-presence of symptom) to 3 (worst severity of symptom) and total scores range from 0 to 63. Total scores of 20 or higher are considered moderate-to-severe depression. Cronbach alphas in the current sample was 0.92.
2.5. Repeated/outcome measures
2.5.1. Positive affect negative affect schedule (Watson, Clark, & Tellegen, 1988; PANAS)
The PANAS is a brief, 20-item measure used to assess positive and negative affect. Participants were instructed to complete the questionnaire based on how they felt then, in that moment, which could change during a short period of time. Each emotion (e.g., enthusiastic, irritable, nervous) is rated on a 5-point Likert scale ranging from “very slightly or not at all” to “extremely”. Answers are summed to create positive affect and negative affect scores, each comprising 10 items and ranging from 10 to 50. Cronbach alphas were 0.87 and 0.90 for negative affect at post-stressor and post-CR/sitting quietly, respectively.
2.5.2. Alcohol craving questionnaire short-form revised (Singleton, Henningfield, & Tiffany, 1994; ACQ-SF)
The ACQ-SF comprises 12 items and is used to assess alcohol cravings in the current moment. Participants are asked to rate how much they agree or disagree with each statement, each regarding how they feel or think about alcohol in the moment (e.g., “If I used alcohol, I would feel less tense”). Each item is scored on a 7-point Likert scale that ranges from “strongly disagree” to “strongly agree”. The total score was used in the current study. The Cronbach alpha for post-stressor and post-CR/sitting quietly were 0.75 and 0.74, respectively.
2.5.3. STOP-IT (Verbruggen, Logan, & Stevens, 2008)
The STOP-IT is a stop-signal task used to measure inhibitory control and is completed by participants on a laptop. A horizontal block arrow is presented on the screen, prompting participants to hit a button on the keyboard corresponding to the arrow’s direction. On 25% of trials, the arrow suddenly turns blue, representing a “stop” signal that is presented at varying times. When this stop signal is presented, participants must withhold their learned response of pressing the key in response to arrows. Participants’ stop signal reaction time (SSRT) reflects varying levels of inhibitory control (lower SSRT reflects better inhibitory control). The integration method of calculating SSRT is used in the STOP-IT (Logan, 1981; G.D. Logan & Cowan, 1984).
2.6. Data analytic plan
2.6.1. Preliminary analyses/manipulation check
A priori power analyses demonstrated that a total sample size of 36 (18 per condition) provided power of 0.95, based on past studies’ effect sizes reflecting the impact of CR on inhibitory control and craving (Beadman et al., 2015; Szasz et al., 2012). Descriptive statistics were computed to characterize the sample, and variable distribution and missing data were examined. Conditions were compared to ensure successful randomization. Data on participants’ use of CR, as described above (using CR quality score), were examined and the effectiveness of the stress induction procedure was also checked.
2.6.2. Hypothesis testing
Linear Mixed Model Analysis was conducted with maximum likelihood estimation. SSRT (inhibitory control) and ACQ total score (alcohol craving) at two time points – post-stressor and post-CR/sitting quietly - were entered as the dependent variables in two separate models. Percent Days Drinking (PDD) at baseline was entered as a control variable. Condition, BDI, PCL, and AUDIT total scores (continuous measures of depression, PTSD, and AUD symptoms, respectively) were entered as fixed effects for all participants. Models included a random intercept with an identity covariance structure to control and test for individual differences in the outcome variables at baseline. Time point [post-stressor, post-CR/sitting quietly (SQ)] was entered as the repeated variable and as a fixed effect, given the manipulations associated with these time points. Main effects of condition, BDI, PCL, AUDIT, and time point were estimated, as well as two-way condition by time point interaction and three-way interaction of condition and time point by each continuous predictor (BDI, PCL, AUDIT). Simple effects of significant interaction effects were examined. Continuous scores on the BDI, PCL, and AUDIT scores were used in analyses; however, for visual graphing purposes (Fig. 2), estimates were calculated for low and high values (one standard deviation below/above the mean) of our continuous moderators. Although the same model tested hypotheses 1 and 2 for each outcome, results are reported by hypothesis.
3. Results
3.1. Preliminary analyses & descriptive statistics
See Table 1 and Fig. 1 for demographics and baseline sample descriptive statistics. There were no missing data in the variables of interest. There were no significant differences between study conditions in terms of demographics (Table 1), baseline alcohol use, or treatment for alcohol use at the time of study participation. Despite urn randomization, the control group had slightly higher PCL total scores; however, any potential effects of randomization error were mitigated given that the PCL was well-above the clinical cut-off score (31–33) in both groups (control M = 46, CR M = 37) and all models included total PCL score as a predictor.
Table 1.
Participant demographics and descriptive statistics, by condition.
| Cognitive Reappraisal (n = 25) |
Psychoeducation Control (n = 25) |
Total (n = 50) |
||||
|---|---|---|---|---|---|---|
| M/N | (SD)/% | M/N | (SD)/% | M/N | (SD)/% | |
| Age | 45.20 | (10.98) | 46.16 | (12.28) | 45.68 | (11.54) |
| Education (years) | 16.38 | (3.77) | 15.97 | (2.84) | 16.17 | (3.30) |
| Race | – | – | – | – | – | – |
| White | 22 | 88% | 20 | 80% | 42 | 84% |
| Black | 1 | 4% | 2 | 8% | 3 | 6% |
| Othera | 2 | 8% | 3 | 12% | 5 | 10% |
| Hispanic ethnicity | 2 | 8% | 4 | 16% | 6 | 12% |
| Sexual Orientation | – | – | – | – | – | – |
| Heterosexual/Straight | 17 | 68% | 20 | 80% | 37 | 74% |
| Homosexual/Gay | 4 | 16% | 3 | 12% | 7 | 14% |
| Bisexual | 2 | 8% | 2 | 8% | 4 | 8% |
| Other | 2 | 8% | 0 | – | 2 | 4% |
| Employment | – | – | – | – | – | – |
| Full-time or Part-time | 11 | 44% | 9 | 36% | 20 | 40% |
| Retired or Disabled | 8 | 32% | 7 | 28% | 15 | 30% |
| Unemployed | 6 | 24% | 7 | 28% | 13 | 26% |
| Other | 0 | – | 2 | 8% | 2 | 4% |
| Days between Sessions | 2.92 | (1.85) | 3.60 | (3.56) | 3.26 | (2.83) |
| Provisional PTSD (PCL-5) | 13 | 52% | 17 | 68% | 30 | 60% |
| Military Sexual Trauma History b | 6 | 25% | 12 | 48% | 18 | 36% |
| In AUD treatment during study | 8 | 32% | 8 | 32% | 16 | 32% |
| PCL total score* | 36.92 | (17.82) | 46.48 | (15.22) | 41.70 | (17.09) |
| AUDIT | 14.52 | (9.72) | 17.08 | (10.80) | 15.80 | (10.25) |
| BDI | 18.92 | (12.56) | 24.40 | (10.89) | 21.66 | (11.96) |
| Psychotropic Medicationc | 16 | 64% | 19 | 76% | 35 | 70% |
| Craving Medicationc | 3 | 12% | 4 | 16% | 7 | 14% |
| Drinking at Baseline | – | – | – | – | – | |
| Percent Days Drinking | 48.18 | (32.11) | 45.07 | (33.50) | 46.62 | (32.51) |
| Mean Drinks per Drinking Day | 5.16 | (7.28) | 4.16 | (2.78) | 4.66 | (5.47) |
| Descriptive Statistics for Outcome Measures, by Session 2 Time Point: | ||||||
| SSRT, post-stress induction | 244.29 | (94.90) | 252.45 | (95.25) | 248.29 | (95.15) |
| SSRT, post-CR/SQ | 219.60 | (72.40) | 206.49 | (75.92) | 212.91 | (75.72) |
| ACQ total, post-stress induction | 3.60 | (0.93) | 3.65 | (1.14) | 3.63 | (1.11) |
| ACQ total, post-CR/SQ | 3.35 | (0.94) | 3.36 | (1.03) | 3.36 | (1.04) |
Note:
p = .047 between conditions. PCL total score was the only variable in this table that differed significantly between conditions, with all chi-square or independent t-tests yielding p > .05. SSRT = stop-signal reaction time; post-CR/SQ = post-Cognitive Reappraisal/Sitting Quietly; ACQ = alcohol craving questionnaire, total score.
5 “other” = 2 multiracial, 1 American Indian/Alaskan Native, 1 Native Hawaiian/Pacific Islander, 1 Asian.
For MST history, n = 49, did not have information for one participant in cognitive reappraisal condition.
Number of women reporting taking psychotropic or anti-craving medication at time of study participation. Craving medication included any that may be expected to impact craving, regardless of whether it was prescribed for craving (medications reported: Gabapentin, Topiramate, Naltrexone).
While participants needed only to score ≥ 3 on the AUDIT-C to be eligible, the average full AUDIT score was 15.80 (SD = 10.25), with 52% (n = 26) scoring between 8 and 14 (suggesting harmful/hazardous use) and 44% (n = 22) scoring ≥15 (suggesting moderate-severe AUD). Additionally, 78% (n = 39) scored ≥20 on the BDI-II (indicating moderate-severe depression) and 70% (n = 35) met criteria for a provisional PTSD diagnosis based on the PCL-5/LEC. Sixty percent (n = 30) met the respective clinical cut-off for at least one co-occurring condition - unhealthy alcohol use plus depression and/or PTSD - and 32% (n = 16) met clinical cut-offs on all three measures. There was a strong correlation of BDI with PCL scores (r = 0.78, p < .01), and moderate correlation of AUDIT score with BDI (r = 0.34, p < .05) and PCL (r = 0.38, p < .01).
For the personalized stress induction, 72% of the focal stressors chosen by participants was relational in nature (e.g., argument with loved one), 13% were medical (e.g., family illness), 11% achievement (e. g., loss of employment), and 4% environmental (e.g., homelessness). Ninety-two percent (92%, n = 46) of participants had an increase in negative affect score on the PANAS negative affect subscale in response to the induction procedure in research session 2, suggesting successful stress induction. All analyses reported below were also run without the four participants who did not have any increase in negative affect score in response to the stress induction and the overall results remained the same. In terms of whether participants were able to successfully implement CR, 17 of the 25 participants (68%) in the CR condition were rated as having a perfect score (12) on the CR quality rating. There was variation in quality of CR use, with scores ranging from 7.5–12, with a mean score of 10.56 (SD = 1.42). There were no effects of therapist on the quality ratings of participants’ use of CR (F = 1.24, p = .32). Post-hoc paired samples t-tests showed significant decrease in both outcomes (SSRT and craving) after the six minutes in which they were sitting quietly or using CR (t = 4.24, p < .001, Cohens d = 0.60 for craving; t = 4.21, p < .001, Cohens d = 0.61 for SSRT). This test, conducted across condition, demonstrated that participants had significantly increased inhibitory control and decreased craving in response to the CR or sitting quietly. (See Section 3.2 for results on main effects, by condition. Mean scores for each outcome variable at each time point can be found in Table 1.)
3.2. Main and interaction effects
3.2.1. Hypothesis 1a: testing main effects of condition (using CR vs. sitting quietly) on alcohol craving (ACQ toted)
There was not a main effect of study condition on reported alcohol craving after CR or sitting quietly following the stress induction (F = 1.1, p = .321). The model included baseline PDD, AUDIT, PCL, and BDI scores as independent predictors. PDD, AUDIT, and PCL were not significantly associated with change in craving from post-stressor to post-CR/sitting quietly (SQ) (all p > .05); there was, however, a near-significant main effect of BDI (F = 3.34, p = .074), with higher depression being associated with higher alcohol craving overall. The random intercept, reflecting individual differences in craving at post-stressor, accounted for significant variance (Wald Z = 4.61, p < .001).
3.2.2. Hypothesis 2a: testing interaction effects of condition by clinical symptoms (PCL, BDI, AUDIT) on alcohol craving
There was a significant three-way interaction of condition and time (post-stressor and post-CR/SQ) with AUDIT (F = 4.14, p = .011) but not BDI (F = 1.14, p = .341) or PCL (F = 2.29, p = .089). Estimated R2 showed that 5.7% of the variance in craving was accounted for by the interaction of AUDIT, time, and condition. Simple effects were examined for the significant interaction of AUDIT score with the two fixed factors, condition and timepoint (post-stressor and post-CR/SQ). Results showed differences in craving change from post-stressor to post-sitting quietly in the control group, which was further moderated by AUDIT (b = 0.018, p = .013). Specifically, in the control condition, participants with more severe AUD reported decreased craving after sitting quietly while participants with less severe AUD experienced no change in craving after sitting quietly (Table 2, Fig. 3). Although it was only at a trend-level of significance, the opposite effect was found for women in the CR condition (b = −0.018, p = .055) which contributed to the significant interaction; in the CR condition, participants with less severe AUD reported decreased craving after using CR while participants with more severe AUD did not experience change in craving after CR. (Table 2, Fig. 3).
Table 2.
Mixed models analysis results – estimates of fixed effects.
| Alcohol Craving | Stop Signal Reaction Time (SSRT) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Fixed Effects | Est | SE | t | p |
95% CI
|
Est | SE | t | p |
95% CI
|
||
| LL | UL | LL | UL | |||||||||
| Intercept | 2.68 | 0.41 | 6.60 | 0.000 | 1.87 | 3.50 | 212.33 | 36.39 | 5.84 | 0.000 | 139.21 | 285.45 |
| Baseline Percent Days Drinking | −0.53 | 0.33 | −1.59 | 0.117 | −1.19 | 0.14 | 5.20 | 30.51 | 0.17 | 0.865 | −56.12 | 66.51 |
| Depression Severity | 0.02 | 0.02 | 0.83 | 0.410 | −0.03 | 0.06 | −0.38 | 2.04 | −0.19 | 0.854 | −4.47 | 3.72 |
| PTSD Severity | 0.02 | 0.02 | 1.07 | 0.292 | −0.02 | 0.05 | 1.37 | 1.47 | 0.93 | 0.356 | −1.58 | 4.31 |
| AUD Severity | −0.01 | 0.02 | −0.31 | 0.756 | −0.04 | 0.03 | −3.00 | 1.61 | −1.86 | 0.068 | −6.23 | 0.23 |
| Time: Post-Stressor/Post-CR/ sitting quietly (SQ) | 0.23 | 0.20 | 1.15 | 0.256 | −0.17 | 0.63 | 8.08 | 29.60 | 0.27 | 0.786 | −51.42 | 67.59 |
| Condition | −0.64 | 0.63 | −1.02 | 0.311 | −1.91 | 0.62 | −69.13 | 55.98 | −1.24 | 0.223 | −181.64 | 43.38 |
| Condition*Time | 0.07 | 0.33 | 0.22 | 0.826 | −0.59 | 0.74 | 4.63 | 48.78 | 0.10 | 0.925 | −93.46 | 102.72 |
| AUDIT interactions: | ||||||||||||
| Post-Stressor*Control | 0.04 | 0.02 | 1.82 | 0.074 | −0.00 | 0.09 | 5.47 | 2.48 | 2.20 | 0.031 | 0.51 | 10.42 |
| Post-CR/SQ* Control | 0.02 | 0.02 | 1.03 | 0.308 | −0.02 | 0.07 | 6.45 | 2.16 | 3.00 | 0.004 | 2.12 | 10.77 |
| Post-Stressor*CR | −0.02 | 0.01 | −1.96 | 0.055 | −0.04 | 0.00 | 1.96 | 1.41 | 1.40 | 0.168 | −0.86 | 4.79 |
| Post-CR/SQ*CR (ref) | – | – | – | – | – | – | – | – | – | – | – | – |
| BDI interactions: | ||||||||||||
| Post-Stressor*Control | 0.03 | 0.03 | 0.90 | 0.374 | −0.03 | 0.09 | −0.64 | 3.06 | −0.21 | 0.836 | −6.75 | 5.48 |
| Post-CR/SQ* Control | 0.02 | 0.03 | 0.68 | 0.501 | −0.04 | 0.08 | −0.05 | 2.68 | −0.02 | 0.986 | −5.42 | 5.33 |
| Post-Stressor*CR | −0.02 | 0.01 | −1.35 | 0.184 | −0.04 | 0.01 | 2.08 | 1.77 | 1.18 | 0.245 | −1.47 | 5.64 |
| Post-CR/SQ*CR (ref) | – | – | – | – | – | – | – | – | – | – | – | – |
| PCL interactions: | ||||||||||||
| Post-Stressor*Control | −0.02 | 0.02 | −1.02 | 0.311 | −0.06 | 0.02 | 0.25 | 2.18 | 0.11 | 0.91 | −4.11 | 4.61 |
| Post-CR/SQ* Control | −0.01 | 0.02 | −0.53 | 0.599 | −0.05 | 0.03 | −1.10 | 1.91 | −0.58 | 0.568 | −4.94 | 2.74 |
| Post-Stressor*CR | 0.02 | 0.01 | 1.83 | 0.074 | −0.00 | 0.03 | −1.25 | 1.28 | −0.98 | 0.331 | −3.82 | 1.31 |
| Post-CR/SQ*CR (ref) | – | – | – | – | – | – | – | – | – | – | – | – |
Note:Bolded values represent simple effects interpreted due to significant interactive fixed effects in the mixed model analysis.
Depression severity assessed with BDI-II; PTSD severity with PCL-5; AUD severity with AUDIT (see Methods for details); Cond = Condition [Control vs. Cognitive Reappraisal/CR (CR Reference)].
Est = Beta Estimate, SE = Parameter Standard Error, CI = Confidence Interval, LL = Lower Limit, UL = Upper Limit.
Fig. 3.
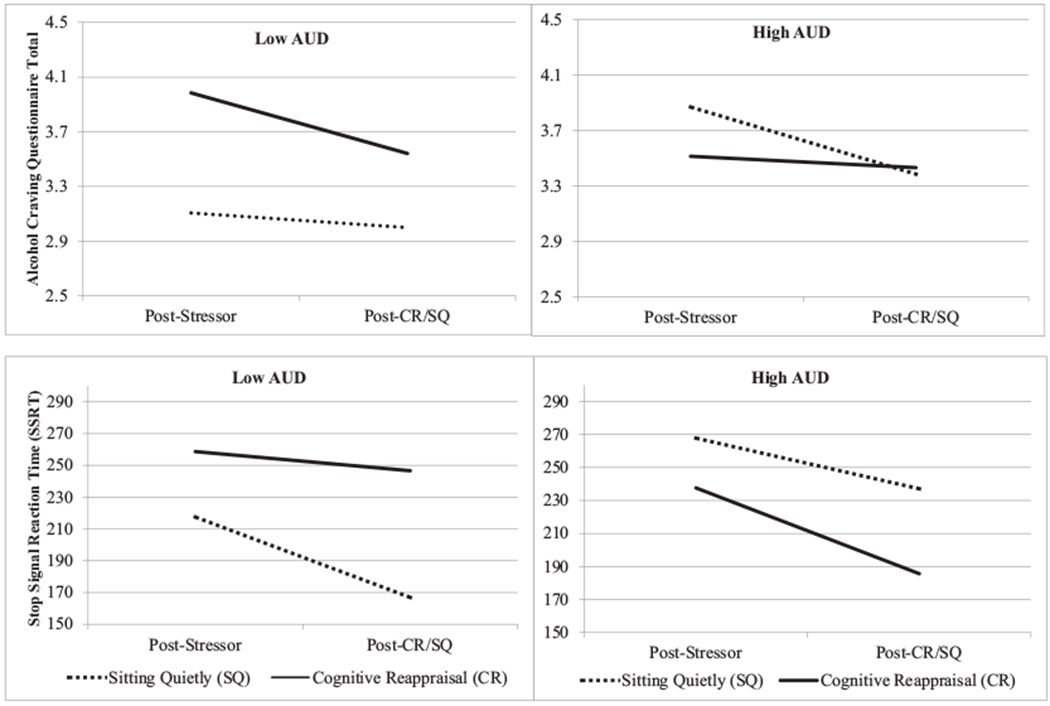
3-Way interaction effects on main study outcomes
Note: Lower scores are “better” for both outcomes. AUD reflects high (mean + 1SD) and low (mean −1SD) scores on the full AUDIT. AUDIT scores were entered in analyses as a continuous variable and graphed here as dichotomous for visualization purposes only.
For craving, the significant interaction was driven by differences at the post-stressor time point and differences within each group across time. Within the control group, the change from post-stressor to post-CR/SQ is significantly different based on severity of AUD. Within the cognitive reappraisal group, the change from post-stressor to post-CR/SQ is near-significant (p = .055) different based on severity of AUD. For SSRT, the significant interaction was driven by differences between groups at the post-CR/SQ time point.
3.2.3. Hypothesis 1b: testing main effects of condition (using CR vs. sitting quietly) on inhibitory control [STOP-IT, stop-signal reaction time (SSRT)]
There was not a main effect of study condition on SSRT after CR or sitting quietly following the stress induction (F = 1.22, p = .274). The model included baseline PDD, AUDIT, PCL, and BDI scores as independent predictors. PDD, AUDIT, BDI, and PCL were not significantly associated with change in craving from post-stressor to post-CR/SQ (all p > .05). The random intercept, reflecting individual differences in SSRT at post-stressor, accounted for significant variance (Wald Z = 4.19, p < .001).
3.2.4. Hypothesis 2b: testing interaction effects of condition by clinical symptoms (PCL, BDI, AUDIT) on inhibitory control [STOP-IT, stop-signal reaction time (SSRT)]
As with alcohol craving, there was a significant three-way interaction of condition and timepoint with AUDIT (F = 3.57, p = .020) but not BDI (F = 0.51, p = .675) or PCL (F = 0.93, p = .431). Estimated R2 found that 6.4% of the variance in SSRT was accounted for by the interaction of AUDIT, time, and condition.
There was a significant between-condition difference in SSRT at the post-CR/sitting quietly time point, moderated by AUDIT (b = 6.45, p = .004). Among women in the CR condition, those with higher baseline AUD severity had better inhibitory control (lower SSRT) after implementing CR, compared to participants in the control group who had sat quietly. Women in the control group with lower baseline AUD severity had better inhibitory control after sitting quietly, compared to all participants in CR. (Table 2, Fig. 3).
4. Discussion
The current study examined the proximal effects of cognitive reappraisal of negative emotion (CR), after a stress induction, among women veterans with unhealthy alcohol use. This is the first study to our knowledge to examine the acute effects of CR within this population, using a microintervention approach to test the acute effects of CR. Participants effectively used CR; however, there was no main effect of condition (CR compared to sitting quietly) on outcomes. Instead, women who sat quietly after a stress induction procedure demonstrated equivalent overall improvements in alcohol craving and inhibitory control to women who used the CR (the experimental condition). Therefore, there was a significant improvement in craving and inhibitory control during the six-minute period for women in both conditions. Whether it is sitting quietly or using CR, provider attention/contact, or the passing of time that precipitated the decrease is unclear and requires further research.
Alternatively, examining moderators of the main condition effect demonstrated that these two approaches – using CR versus sitting quietly – did work differently for individuals based on severity of AUD. Specifically, women had increases in craving and reductions in inhibitory control in response to the stress induction; afterward, women who simply sat quietly had greater reductions in craving if they had more severe AUD, while those with less severe AUD benefitted more from using CR. Alternatively, women in the CR condition had improved inhibitory control if they had more severe AUD, while women with less severe AUD had greater improvements in inhibitory control if they sat quietly. These results from testing hypothesis 2a and 2b are consistent with previous research finding that clinical severity moderates the impact of therapeutic strategies in other populations, using a micro-intervention design (e.g., Zaunmüller et al., 2014), but requires further research. The model included severity of co-occurring depression and PTSD as predictors, but they did not have significant effects on the outcomes.
These results suggest nuanced effects of CR in this population, and effects that may vary based on outcome of interest. CR was less effective for women with more severe AUD in reducing craving, with craving being a cardinal symptom of AUD. For those women, sitting quietly worked well. Others have also found that relaxation and distracting oneself can be effective emotion regulation strategies (albeit, typically in the short-term; Gross, 2001) that are often taught to patients receiving AUD treatment to cope with stress or cravings (Larimer & Palmer, 1999). Additionally, sitting quietly is cognitively less taxing than employing CR, especially given that CR was a newly acquired skill. Cognitive theories of treatment for depression (which rely heavily on cognitive restructuring/reappraisal) posit that gradually strengthening prefrontal regulatory brain mechanisms is an important mechanism of change (DeRubeis, Siegle, & Hollon, 2008) and a recently published study found that executive control was associated with CR ability in the lab (Quinn & Joormann, 2020). Women in the current study who were coping with more severe AUD may have had more difficulty recruiting executive control required to effectively execute CR. If one is experiencing an intense craving (expected for those with more severe AUD), the high need for downregulation of that craving may, simultaneously, be especially difficult to implement. For women with more severe AUD symptoms, sitting quietly may be easier than executing a cognitively taxing, newly learned skill. However, while sitting quietly may be effective at immediately reducing negative affect and/or craving, emotion regulation research has shown that strategies focused on cognitive change, such as CR, are more effective in the long-run than those that focus on response modulation (such as sitting quietly, deep breathing, etc.) (Gross, 2001). These findings may extend to the effect of CR and other emotion regulation strategies on alcohol cravings. For instance, while immediate coping and reduction of craving states is important especially in early treatment for AUD, the use of response-focused strategies (e.g., distraction, deep breathing, urge surfing) may be related to greater likelihood of continued cravings in response to triggers. Alternatively, more stable changes in cognitive schemas (e.g., decreased expectations about the positive effects of alcohol in relieving negative affect) may be more likely to reduce frequency and intensity of future cravings.
In examining the effects of CR on a cognitive outcome measure, inhibitory control, an opposite pattern of results emerged. Specifically, women with more severe AUD had better inhibitory control (lower stop-signal reaction time) if in the CR group, while women with less severe AUD performed better after sitting quietly. These were between-group differences, at the post-CR /sitting quietly time point while controlling for post-stressor levels (which did not differ between groups). These findings were consistent with hypotheses, in that teaching and having participants use CR resulted in increased inhibitory control after a stress induction procedure among women with more severe AUD. However, the finding that sitting quietly also improved inhibitory control, albeit for women with less severe AUD, was not expected. As described above, these results suggest that different strategies for regulating emotion work differently for women based on the severity of their AUD. Zaunmüller et al. (2014) found that the effects of cognitive restructuring on frontal lobe activity was dependent on severity of participant dysphoria. This finding was interpreted to reflect an intensified utilization of prefrontal regulatory brain mechanisms that could serve to dampen emotional arousal among participants with higher dysphoria/clinical symptoms. Similarly, the greater effect of CR on inhibitory control (but not cravings) for women with more severe AUD may reflect an intensified utilization of cognitive mechanisms that could – but do not necessarily (or acutely) – dampen cravings for alcohol. This is speculative, however, and continued research is needed to better understand and compare both the proximal and long-term effects of CR on affect and alcohol-related outcomes.
4.1. Limitations
Despite its findings, this study has limitations. First, we did not assess potential emotion regulation strategies that control group participants may have been using while sitting quietly between the stress induction and final (post-CR/sitting quietly) outcome assessment. Using a structured control in which participants are specifically instructed to use a different strategy from that of the experimental group or assessing for use of relevant strategies after experimental sessions among the control group would enhance study design moving forward. Second, the study was not designed to examine causal associations between outcomes of interest, allowing us only to examine the effects of CR directly on alcohol craving and inhibitory control and not the associations between those outcome measures. While the sample was clinically complex, as indicated by scores on valid self-report measures including the PCL-5, BDI-II, and AUDIT, we did not do structured clinical interviews with the participants. Therefore, we are unable to interpret findings based on clinical diagnoses. Relatedly, the unequal PTSD severity (measured with total PCL-5 score) across conditions was a failure of the study’s randomization procedures and is important to note. Third, research should examine these findings with larger samples, which could also allow for direct gender comparisons.
4.2. Conclusions and future directions
The current study suggests that CR, a commonly taught emotion regulation strategy, has different effects based on type of outcome examined and severity of clinical symptoms among women veterans. Continued experimental research on the immediate and long-term effects of isolated, individual therapeutic strategies could provide information on the efficacy of strategies for subgroups of patients, and, importantly, provide information about how those strategies have their effects. Women – both veterans and civilians – are one such population of under-researched individuals with high prevalence rates of alcohol use disorders and unhealthy alcohol use more generally. While characteristics of a given population (e.g., based on sex and gender, presence and severity of clinical symptoms) are likely to moderate the efficacy of specific treatment interventions (C.G. Holzhauer, Cucciare, & Epstein, 2020; McCrady, Epstein, & Fokas, 2020), examining these effects using a clinical trial design can be difficult (e.g., by requiring very large, diverse samples or by testing the efficacy of a treatment over multiple studies with specific sub-populations). Alternatively, a microintervention design allows for empirically based examination of moderators of an intervention, providing information about for whom, or in what context, a given therapeutic strategy work best.
Acknowledgements
Work supported by Dept of Veterans Affairs, Veterans Health Administration CSR&D grant CX001951 (PI: Holzhauer) and VA VISN 1 Career Development Award (PI: Holzhauer). The opinions expressed here are those of the authors and do not represent the official policy or position of the U.S. Department of Veterans Affairs or the U.S. government.
Footnotes
Declaration of competing interest
The authors do not have any competing financial or personal interests to disclose.
References
- American College of Obstetricians and Gynecologists. Patient Fact Sheets, Women’s Health [Internet]. 2017. [cited 1/13/2017]
- Barlow DH, Ellard KK, Fairholme CP, Farchione TJ, Boisseau CL, Allen LB, & Ehrenreich-May JT (2011). Unified protocol for transdiagnostic treatment of emotional disorders. New York, NY: Oxford University Press. [Google Scholar]
- Beadman M, Das RK, Freeman TP, Scragg P, West R, & Kamboj SK (2015). A comparison of emotion regulation strategies in response to craving cognitions: Effects on smoking behaviour, craving and affect in dependent smokers. Behaviour Research and Therapy, 69, 29–39. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, TX: Psychological Corp. [Google Scholar]
- Buhle JT, Silvers JA, Wager TD, Lopez R, Onyemekwu C, Kober H, … Ochsner KN (2014). Cognitive reappraisal of emotion: A meta-analysis of human neuroimaging studies. Cerebral Cortex, 24(11), 2981–2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez LJ, Williams EC, Lapham G, & Bradley KA (2012). Association between alcohol screening scores and alcohol-related risks among female veterans affairs patients. Journal of Studies on Alcohol and Drugs, 73(3), 391–400. [DOI] [PubMed] [Google Scholar]
- Denny BT, Inhoff MC, Zerubavel N, Davachi L, & Ochsner KN (2015). Getting over it: Long-lasting effects of emotion regulation on amygdala response. Psychological Science, 26(9), 1377–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRubeis RJ, Siegle GJ, & Hollon SD (2008). Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nature Reviews Neuroscience, 9(10), 788–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eftekhari A, Zoellner LA, & Vigil SA (2009). Patterns of emotion regulation and psychopathology. Anxiety, Stress, & Coping, 22(5), 571–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein EE, McCrady BS, Hallgren KA, et al. (2018). Individual versus group female-specific cognitive behavior therapy for alcohol use disorder. Journal of Substance Abuse Treatment, 88, 27–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans EA, Upchurch DM, Simpson T, et al. (2018). Differences by veteran/civilian status and gender in associations between childhood adversity and alcohol and drug use disorders. Social Psychiatry and Psychiatric Epidemiology, 53(4), 421–435. [DOI] [PubMed] [Google Scholar]
- Fairholme CP, Nosen EL, Nillni YI, et al. (2013). Sleep disturbance and emotion dysregulation as transdiagnostic processes in a comorbid sample. Behaviour Research & Therapy, 51(9), 540–546. doi: 10.1016/j.brat.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Dawson DA, Chou SP, Grant BF. (2012). Sex differences in prevalence and comorbidity of alcohol and drug use disorders: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Studies on Alcohol and Drugs, 73(6): 938–950. doi: 10.15288/jsad.2012.73.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, … Hasin DS. (2016). Epidemiology of DSM-5 drug use disorder: Results from the National Epidemiologic Survey on alcohol and related conditions–III. JAMA Psychiatry, 73(1), 39–47. 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ (2001). Emotion regulation in adulthood: Timing is everything. Current Directions in Psychological Science, 10(6), 214–219. [Google Scholar]
- Guinle MIB, & Sinha R (2020). The role of stress, trauma, and negative affect in alcohol misuse and alcohol use disorder in women. Alcohol Research: Current Reviews, 40(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann L, Sallard E, & Spierer L (2016). Enhancing frontal top-down inhibitory control with Go/NoGo training. Brain Structure and Function, 221(7), 3835–3842. doi: 10.1007/s00429-015-1131-7. [DOI] [PubMed] [Google Scholar]
- Holzhauer CG, Cucciare M, & Epstein EE (2020). Sex and gender effects in recovery from alcohol use disorder. Alcohol Research: Current Reviews, 40(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalpakci A, Sofuoglu M, Petrakis I, & Rosenheck RA (2019). Gender differences among veterans with alcohol use disorder nationally in the Veterans Health Administration. Journal of Addictive Diseases, 1–10. 10.1080/10550887.2019.1653739. [DOI] [PubMed] [Google Scholar]
- Karpyak VM, Biernacka JM, Geske JR, Abulseoud OA, Brunner MD, Chauhan M, … Onsrud DA (2016). Gender-specific effects of comorbid depression and anxiety on the propensity to drink in negative emotional states. Addiction, 111(8), 1366–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivity Y, & Huppert JD. (2016). Does cognitive reappraisal reduce anxiety? A daily diary study of a micro-intervention with individuals with high social anxiety. Journal of Consulting and Clinical Psychology, 84(3), 269. [DOI] [PubMed] [Google Scholar]
- Koch K, Pauly K, Kellermann T, Seiferth NY, Reske M, Backes V, … Schneider F (2007). Gender differences in the cognitive control of emotion: An fMRI study. Neuropsychologia, 45(12), 2744–2754. [DOI] [PubMed] [Google Scholar]
- Lande RG, Marin BA, Chang AS, et al. (2007). Gender differences and alcohol use in the US Army. Journal of the American Osteopathic Association, 107(9), 401. [PubMed] [Google Scholar]
- Larimer ME, & Palmer RS (1999). Relapse prevention: An overview of Marlatt’s cognitive-behavioral model. Alcohol Research and Health, 23(2), 151–160. 403. doi: 10.1037/cou0000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan GD (1981). Attention, automaticity, and the ability to stop a speeded choice response. In Long J, & Baddeley AD (Eds.), Attention and performance IX (pp. 205–222). Hillsadale: Erlbaum. [Google Scholar]
- Logan GD, & Cowan WB (1984). On the ability to inhibit thought and action A theory of an act of control. Psychological Review, 91(3), 295–327. [DOI] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, & Fokas KF (2020). Treatment interventions for women with alcohol use disorder. Alcohol Research: Current Reviews, 40(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S, Pagan D, & Tross S (1998). Women’s health education: Peer activism for female partners of injection drug users. Columbia University, New York: Unpublished treatment manuscript. [Google Scholar]
- Naqvi NH, Ochsner KN, Kober H, Kuerbis A, Feng T, Wall M, & Morgenstern J (2015). Cognitive regulation of craving in alcohol-dependent and social drinkers. Alcoholism: Clinical and Experimental Research, 39(2), 343–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S (2012). Emotion regulation and psychopathology: The role of gender. Annual Review of Clinical Psychology, 8, 161–187. [DOI] [PubMed] [Google Scholar]
- Peltier MR, Verplaetse TL, Mineur YS, Petrakis IL, Cosgrove KP, Piceiotto MR, & McKee SA (2019). Sex differences in stress-related alcohol use. Neurobiology of Stress, 10, 100–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn ME, & Joormann J (2020). Executive control under stress: Relation to reappraisal ability and depressive symptoms. Behaviour Research and Therapy, 103, 634–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray RD, McRae K, Ochsner KN, & Gross JJ (2010). Cognitive reappraisal of negative affect: Converging evidence from EMG and self-report. Emotion, 10(4), 587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubonis AV, Colby SM, Monti PM, Rohsenow DJ, Gulliver SB, & Sirota AD (1994). Alcohol cue reactivity and mood induction in male and female alcoholics. Journal of Studies on Alcohol, 55(4), 487–494. [DOI] [PubMed] [Google Scholar]
- Saladin ME, Gray KM, Carpenter MJ, LaRowe SD, DeSantis SM, & Upadhyaya HP (2012). Gender differences in craving and cue reactivity to smoking and negative affect/stress cues. The American Journal on Addictions, 21(3), 210–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, et al. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Singleton EG, Henningfield JE, & Tiffany SE (1994). Alcohol craving questionnaire: ACQ-now: Background and administration manual. Baltimore: NIDA Addiction Research Centre. [Google Scholar]
- Sinha R, & Tuit KL (2012). Imagery script development procedures. New Haven, CT: Yale University School of Medicine. [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline follow-back. In Measuring alcohol consumption (pp. 41–72). Totowa, NJ: Humana Press. [Google Scholar]
- Sobell LC, & Sobell MB (1996). Timeline followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Ontario, Canada: Addiction Research Foundation. [Google Scholar]
- Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, & Bole CW (2013). Affect regulation training (ART) for alcohol use disorders: Development of a novel intervention for negative affect drinkers. Journal of Substance Abuse Treatment, 45(5), 433–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauman TJ, Goetz EL, Detloff AM, MacDuffie KE, Zaunmüller L, & Lutz W (2013). Self-regulation and mechanisms of action in psychotherapy: A theory-based translational perspective. Journal of Personality, 81(6), 542–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauman TJ, Socolar Y, Kwapil L, Cornwell JF, Franks B, Sehnert S, & Higgins ET (2015). Microinterventions targeting regulatory focus and regulatory fit selectively reduce dysphoric and anxious mood. Behaviour Research and Therapy, 72, 18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szasz PL, Szentagotai A, & Hofmann SG (2012). Effects of emotion regulation strategies on smoking craving, attentional bias, and task persistence. Behaviour Research and Therapy, 50(5), 333–340. [DOI] [PubMed] [Google Scholar]
- Timko C, Hoggatt KJ, Wu FM, Tjemsland A, Cucciare M, Rubin A, & Simpson TL (2017). Substance use disorder treatment services for women in the Veterans Health Administration. Women’s Health Issues, 27(6), 639–645. [DOI] [PubMed] [Google Scholar]
- Van Cappellen P, Catalino LI, & Fredrickson BL (2020). A new micro-intervention to increase the enjoyment and continued practice of meditation. Emotion, 20(8), 1332–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veilleux JC, Skinner KD, Reese ED, & Shaver JA (2014). Negative affect intensity influences drinking to cope through facets of emotion dysregulation. Personality and Individual Differences, 59, 96–101. [Google Scholar]
- Verbruggen F, Logan GD, & Stevens MA (2008). STOP-IT: Windows executable software for the stop-signal paradigm. Behavior Research Methods, 40(2), 479–483. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen L (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Weafer J, De Arcangelis J, & de Wit H (2015). Sex differences in behavioral impulsivity in at-risk and non-risk drinkers. Frontiers in Psychiatry, 6, 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD checklist for DSM-5 (PCL-5) – LEC-5 and extended criterion a [measurement instrument]. [Google Scholar]
- Weiss NH, Sullivan TP, & Tull MT (2015). Explicating the role of emotion dysregulation in risky behaviors: A review and synthesis of the literature with directions for future research and clinical practice. Current Opinion in Psychology, 3, 22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, & Gratz KL (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westphal M, Aldao A, & Jackson C (2017). Emotion dysregulation in comorbid posttraumatic stress disorder and substance use disorders: A narrative review. Military Psychology, 29(3), 216–233. [Google Scholar]
- Zaunmüller L, Lutz W, & Strauman TJ (2014). Affective impact and electrocortical correlates of a psychotherapeutic microintervention: An ERP study of cognitive restructuring. Psychotherapy Research, 24(5), 550–564. [DOI] [PubMed] [Google Scholar]


