Abstract
Background
The COVID-19 pandemic has caused disruption to healthcare delivery worldwide including in the delivery of surgical services. The introduction of mRNA COVID vaccines and the significant reactogenicity seen with vaccination has caused an unanticipated impact on the operating room workforce via unanticipated paid time off after employee vaccination.
Methods
A retrospective cross-sectional survey was made available to approximately 33,000 front-line healthcare workers, students and volunteers who were offered voluntary vaccination in a state-wide healthcare system during phase one of the state's vaccine roll-out. The primary study aim was to determine the frequency of unanticipated paid time off, and the secondary study aim was to identify any demographic determinants influencing the need for unanticipated time off work secondary to adverse effects.
Results
4009 responses were received, a 12.15% response rate. When looking specifically at individuals who did not proactively schedule themselves for time off after vaccination, we determined that unanticipated paid administrative leave was required for 4.9% and 19.79% of individuals after the first and second doses of vaccine, respectively. The average lengths of absence were 1.66 days and 1.39 days for the first and second doses, respectively. There were no statistically significant differences found in the need for unanticipated leave when compared by vaccine manufacturer, gender, age, ethnicity, or job description. However, individuals with a bachelor's degree demonstrated a significantly higher unanticipated leave requirement than respondents who reported other educational backgrounds.
Conclusions
The ability to staff operating rooms and other critical healthcare services may be negatively affected as a result of COVID-19 mRNA vaccination reactogenicity and subsequent unanticipated paid administrative leave. For future COVID-19 boosters or during other pandemics in which mRNA vaccination is recommended, employees should proactively schedule their vaccination(s) in conjunction with their work schedules to minimize the impact of reactogenicity and unanticipated time off on the operating room schedule and patient care.
Keywords: COVID-19, Staffing, Vaccination, Reactogenicity, Work-related absences
Abbreviations
- WHO
World Health Organizaton
- NTW
Not to work
- PAL
Paid administrative leave
1. Introduction
On December 31, 2019, the World Health Organization (WHO) was first informed of a series of cases of pneumonia of unknown etiology in the city of Wuhan, China1, 2. On February 11, 2020, the WHO officially announced that the causative agent for this novel illness was a coronavirus. The disease vector, formally named SARS-CoV-2 and the disease it causes, COVID-19, has become responsible for over 4 million deaths world-wide at the time of this writing3, rapidly becoming the worst public health crisis since the influenza pandemic of 19184.
In addition to the unparalleled effect on public health and the economy, there was widespread impact on routine and urgent surgical services early in the pandemic5. Operating room facilities in the authors’ hospital system were impacted in a fashion consistent with that previously reported by other authors—elective procedures were abruptly limited, staffing levels were directly impacted by employee infections, staff were redeployed to unfamiliar locations, supplies were rationed and the COVID patient census limited surgical capacity5, 6. Wohler et al. stated, “Resuming elective surgical cases in the face of a global pandemic is a complex issue with unanticipated complicating factors”7. Operating room services at the authors’ hospital were reestablished pre-vaccination in the summer of 2020 using a gradual and tiered approach, but this approach did not initially consider provisions for team member absences due to vaccination reactogenicity.
A vaccine, using novel mRNA technology and manufactured by Pfizer BioNTech (BNT162) against SARS-CoV-2 was approved for clinical use under emergency use authorization from the Food and Drug Administration (FDA) on December 11, 2020. A week later, a second similar mRNA vaccine manufactured by Moderna (mRNA-1273) was also given emergency use authorization. Common reactions seen with the mRNA vaccinations in preclinical trials included local reactions at the injection site and systemic reactions like those seen with seasonal influenza infections—tiredness, headache, muscle pain, chills, fever and nausea8, 9. When associated with seasonal flu, staff with similar symptoms occasionally require paid administrative leave (PAL).
In the United States, the initial target population for vaccination was deemed to be patient-facing healthcare personnel11. While it was anticipated that vaccination would allow the return of operational normality in the healthcare industry, the direct impact of vaccination itself and vaccine related side effects on the ability of individuals to participate in their day-to-day work expectations was underappreciated and had unanticipated effects10. Shortly after mRNA vaccines by Pfizer12 and Moderna13 became available in December 2020, it was anecdotally observed that a non-trivial number of operating room staff in the authors’ operating suites required unanticipated PAL due to adverse effects following vaccination. This resulted in a real and impactful effect on operating room throughput, with cases being delayed or canceled due to the unanticipated impact of vaccination on staff availability. Other medical units in the health system reported similar observations of unanticipated PAL after employee vaccination14. In response, on March 16, 2021, the authors’ health system published a provision for special COVID-PAL, allowing PAL for vaccine reactogenicity, with provisions for retroactive claiming of COVID-PAL to January 1, 202115.
A literature search done at the time of the conception of this project did not find any previous publications highlighting the relationships between COVID-19 vaccination and work-related absences. A single story reported in the lay media outlined the concerns of nursing home staff regarding the role of vaccination reactogenicity on the provision of care, specifically in relation to the impact of vaccination reactogenicity on nurses and their ability to cover their shifts after vaccination16. This project was created to evaluate the adverse effects of mRNA COVID-19 vaccination among operating room staff and the general healthcare workforce in a large, multi-site, state-wide, tertiary medical system and to identify unexpected PAL and any significant demographic determinants of individuals more likely to require reactogenicity associated PAL.
2. Materials and methods
After receiving Institutional Review Board (IRB) review and exempt status from The University of North Carolina at Chapel Hill (IRB# 21-0354), a retrospective cross-sectional survey was made available to employees, healthcare providers, and volunteers of a state-wide tertiary care system—those with patient-facing responsibilities who had been deemed eligible for phase one vaccination—through a series of links published in staff, volunteer, and medical provider electronic newsletters. Individuals who opted to participate in the study were directed via the published links to a Qualtrics web-based survey which was used to collect their anonymous responses to the survey questions. Software, using IP addresses to screen for duplicate entries, which was offered by Qualtrics was employed to prevent individuals from entering multiple responses. Even though the IRB had waved the requirement for informed consent, the electronic survey included a summation of the study goals and a participant release which required acknowledgement as part of the entry into the evaluation portal. Those individuals who were not eligible for phase one vaccination who attempted to participate in the study were screened out of responding as part of the consent process preceding the survey on the Qualtrics website.
Vaccination for the target population began December 14, 2020 and continued through March 2021. The retrospective data collection began on March 16, 2021 and continued through May 4, 2021.
The target population was approximately 33,000 individuals with patient-facing responsibilities who received the electronic newsletters and who were eligible for voluntary COVID-19 vaccination with the aforementioned mRNA vaccines during the early vaccination period.
Applying a cross-sectional study design and following the STROBE observational study guidelines, a self-reporting questionnaire (Appendix 1) was used to collect anonymous information regarding patient demographics, enthusiasm for vaccination, type of vaccination received, the reactogenicity experienced, the intensity and duration of symptoms for each shot of the two-shot mRNA vaccine regimen and the impact on the ability to work post-vaccination. The enthusiasm for vaccination was gauged on a modified Likert scale where zero was “totally unenthusiastic” and ten was “thrilled.” The symptoms queried were based on a modified version of the list published by the FDA on the websites describing mRNA vaccines8, 9. Patients reported severity on a similarly modified Likert scale where zero indicated they did not experience the symptom and ten was considered incapacitating. Specific information was collected on individual planning for reactogenicity by questioning: whether they intentionally scheduled their inoculations to have off the following day, whether they modified their work schedule to take a planned PAL day after inoculation, and how much PAL they required after each inoculation. These responses were used to determine which individuals required unanticipated PAL and the amount of unanticipated PAL needed. Individuals who were offered vaccination but declined were also solicited and were asked to comment on their reason for refusing vaccination via a free text response.
Regarding side effects, the incidence and duration of any adverse effects as well as each kind of specific adverse reaction were reported, and the mean and standard deviation of the duration of symptoms were calculated for each type of vaccine after each dose. Additionally, the percentage of individuals with systemic side effects (any adverse reaction except for injection site pain, swelling or redness) was calculated.
The mean and standard deviation of enthusiasm scores and percentages of people reporting that they would not receive the vaccine were calculated. Kendall's tau test was used to estimate and test the association between vaccination enthusiasm and time off work requirements.
For each vaccine administration, we calculated the percentages of individuals scheduled to work post-shot and of individuals who either were not scheduled to work post-shot or modified their work or vaccination schedule in anticipation of potential side effects. The average length of absence was calculated for each vaccine type after each dose for all individuals as well as for the sub-population requiring non-scheduled absences. Wilcoxon rank-sum tests were used to test the association between vaccination types and the length of absence for the sub-population with non-scheduled absences after each dose.
Subgroup analyses were employed to ascertain whether the enthusiasm and the impact of vaccination differed according to the demographic groups including gender, age, education, job or ethnicity. For binary variables, Fisher's exact tests were employed to test the differences of percentages between males and females. Chi-squared tests of independence were employed to test the potential effects of age, education, job or ethnicity. For continuous variables, Kruskal-Wallis tests were employed to test the potential effect of various demographic factors including gender, age, education, job and ethnicity. P-values of the tests were reported. For all tests, complete cases were used in the cases of missing values.
3. Results
A total of 4009 responses were recorded out of approximately 33,000 eligible individuals, a 12.15% response rate. A complete data set is available by request from the corresponding author Not all respondents answered all questions. The demographic information of the respondents is noted in Table 1 .
Table 1.
Respondent demographic information.
| Gender | |
| Female | 3418 (86%) |
| Male | 534 (13%) |
| Other | 5 (0.1%) |
| Unknown | 52 |
| Age | |
| 18 - 24 | 156 (4.0%) |
| 25 - 34 | 839 (21%) |
| 35 - 44 | 920 (23%) |
| 45 - 54 | 1032 (26%) |
| 55 - 64 | 828 (21%) |
| 65 - 74 | 169 (4.3%) |
| 75 - 84 | 2 (<0.1%) |
| Unknown | 63 |
| Education | |
| Associate degree (e.g. AA, AS) | 663 (17%) |
| Bachelor's degree (e.g. BA, BS) | 1323 (34%) |
| Doctorate or professional degree (e.g. MD, DDS, PhD) | 551 (14%) |
| High school degree or equivalent (e.g. GED) | 142 (3.6%) |
| Less than a high school diploma | 2 (<0.1%) |
| Master's degree (e.g. MA, MS, MEd) | 765 (20%) |
| Some college, no degree | 477 (12%) |
| Unknown | 86 |
| Job | |
| Advanced Practice Provider | 201 (5.1%) |
| Attending Physician | 197 (5.0%) |
| Nurse | 1137 (29%) |
| Other | 1147 (29%) |
| Resident or Fellow Physician | 102 (2.6%) |
| Student | 73 (1.9%) |
| Support Staff | 718 (18%) |
| Technician | 341 (8.7%) |
| Volunteer | 4 (0.1%) |
| Unknown | 89 |
| American Indian or Alaska Native | 67 (1.7%) |
| Asian | 238 (5.9%) |
| Black or African American | 434 (11%) |
| Hispanic or Latino | 148 (3.7%) |
| Native Hawaiian or Pacific Islander | 6 (0.1%) |
| White | 3113 (78%) |
| Other | 55 (1.4%) |
1Statistics presented: n (%).
Of the 4009 respondents, 3638 (90.74%) reported to have opted for vaccination. For Pfizer (N = 3119), 90.8% of individuals had a minimum of one adverse reaction after the first dose and 86.4% of individuals experienced a minimum of one adverse reaction after second dose. The most common reactions for both the first and the second dose of the Pfizer vaccine were injection site pain, fatigue, and headache. For Moderna (N = 519), 93.4% of individuals had a minimum of one adverse reaction after the first dose and 83.8% of individuals had a minimum of one adverse reaction after the second dose. The most common reactions after the first dose of the Moderna vaccine were injection site pain, fatigue, and injection site redness. After the second dose, the most common reactions were injection site pain, fatigue, and muscle pain. The percentages of individuals reporting side effects can be visualized in Figs. 1 and 2 .
Fig. 1.
Side effects seen with Pfizer vaccination.
Fig. 2.
Side effects seen with Moderna Vaccination.
When the data was pooled for both vaccine manufacturers and the complaints related solely to the injection site (injection site pain, swelling and redness) were removed, we were able to determine the degree of systemic side effects. For the first dose, 52% of individuals reported systemic effects, while 70% reported systemic reactogenicity after the second injection. There were statistically significant associations between the percentages of systemic side effects and the queried demographics after both doses of the vaccine. Statistically significant associations were found for gender, age, ethnicity and education, as subsequently detailed. Female respondents were more inclined to report having systemic side effects than their male counterparts. Individuals who reported their age in the 25–44 cohort had the highest reported incidence of systemic reactogenicity with both doses. Those who described themselves as Hispanics or Latinos, and those who described themselves as Native Hawaiian or Pacific Islander, had the highest percentage of systemic side-effects after the first dose, while those who self-described as Asian or White had the highest systemic reactogenicity after the second dose of vaccine. Fifty seven percent of the individuals who described their education as having spent some time in college but not having earned a degree reported the highest incidence of systemic side-effects after the first injection, while those with a doctorate or professional degree reported the highest incidence of systemic effects after the second injection at 75%. Finally, when local side effects were removed, the Moderna vaccine was statistically more likely to cause systemic reactions than the Pfizer vaccine, but only with the first dose.
The overall mean of duration of symptoms was 1.8 days (SD = 1.59) after first dose of vaccination and 1.7 days (SD = 1.74) after second dose. There was a statistically significant association between the duration of symptoms after the first dose and vaccination type (p < 0.001), such that participants who received the Moderna vaccine had a longer duration of symptoms compared to those individuals who received the Pfizer vaccine. There were also statistically significant associations between the duration of symptoms after each dose and gender. Females tended to have a longer duration of symptoms compared to males after each dose of the vaccines. There was also a significant association between age and the first dose duration of symptoms, whereby the participants aged 35–54 tended to have a longer duration of symptoms after the first dose of vaccine.
Regarding education level, there was a significant association between the reported educational level and the second dose duration of symptoms, in which people with an associate degree tended to have a longer duration of symptoms. No statistically significant associations were seen between the duration of symptoms and either the self-reported job description or ethnicity.
The overall mean (SD) of enthusiasm for vaccination was 7.7 (2.8) on the 10-point Likert scale. There were statistically significant associations between the enthusiasm for vaccination and gender, age, education, job, and ethnicity. For gender, the male participants showed a higher enthusiasm for vaccination than the female participants. Older people tended to have a higher enthusiasm for vaccination and participants older than 65 showed the highest enthusiasm. Regarding education, people with a higher level of education tended to show a higher enthusiasm for vaccination. The mean enthusiasm of participants with a doctorate or a professional degree was the highest at 9.0 (1.87) and the mean enthusiasm of those with a master's degree was the second highest at 8.3 (2.42). In so far as job description, those that reported themselves as volunteers, attending physicians, physicians-in-training (resident or fellow physicians) and students showed a prominent level of enthusiasm for vaccination. Finally, regarding ethnicity, those who classified themselves as Native Hawaiian or Pacific Islander, as Asian or as White individuals had a high level of enthusiasm for vaccination.
By employing Kendall's tau test, it was determined that there was a statistically significant negative correlation between the enthusiasm for vaccination reported and the time off work required. Participants who reported a greater enthusiasm for vaccination tended to take less time off work. The calculated correlation coefficient was −0.0938 with associated 95% CI (−0.1526, 0.0344).
The data were further analyzed for any associations between the demographic classifications and the proclivity for individuals to schedule themselves to work post vaccination. For the individuals who received the Pfizer vaccine, the overall percentage of participants who were scheduled to work post-shot was 59% for the first dose and 57% for the second dose. There were statistically significant associations with both reported gender and ethnicity relative to the percentage of people who scheduled themselves to work immediately after their second dose of vaccine. More males were scheduled to work after their second dose compared to the female respondents. Regarding self-reported ethnicity, Black or African Americans and White individuals showed the highest percentage of scheduling themselves to work after the second dose. There were also statistically significant associations between age, education and the jobs reported and the percentage of participants who scheduled themselves to work after both doses of vaccine. For age, individuals aged 18–24 were the least likely to schedule themselves to work post vaccination, while individuals aged 55–64 were the most likely to schedule themselves to work after being vaccinated. Regarding education level, individuals with a high school degree or less were the most likely to schedule themselves to work post-vaccination, and people with a bachelor's degree were the least likely to schedule themselves to work after vaccination. When sorted by job description, nurses and students were the least likely to schedule themselves to work post vaccination and physicians-in-training (residents or fellows) were the most likely to schedule themselves to work after their shot was received.
When specifically looking at individuals who received the Moderna vaccine, the overall percentage scheduled to work post-shot was 65% for the first dose and 61% for the second dose. There was a statistically significant association between the reported education level and the percentage of respondents who were scheduled to work after the first dose of vaccination. People with a high school degree or less were the most likely to be scheduled to work post-vaccination and individuals with an associate degree were the least likely to have proactively scheduled themselves to work post vaccination. There was also a significant association between the reported job description and the percentage of individuals scheduled to work after both doses. Students were the least likely to be scheduled to work and physicians-in-training were the most likely to work after Moderna vaccination. No statistically significant associations were found between the percentage of individuals scheduled to work post-shot and gender, age or ethnicity.
The term “Not to Work” (NTW) was used to identify individuals who were either scheduled not to work or who actively modified their schedule not to work in anticipation of vaccine reactogenicity. This contrasts with the subset of individuals who required unanticipated PAL, which will be discussed subsequently in this section.
For the Pfizer vaccine recipients, the overall percentage of participants identified as NTW was 44% for first dose and 50% for second dose. There was a statistically significant association between gender and the percentage of people NTW for the second dose of Pfizer vaccine. Female participants were more likely to be NTW in anticipation of reactogenicity than their male counterparts. There were also statistically significant associations between age, education level and job and the percentage of NTW. For age, participants aged 55–64 had the lowest percentage of NTW and 18–24-year-old individuals had the highest percentage of NTW, 58% and 71% for the first and second doses, respectively. When asked regarding education, participants with a high school degree or less reported the lowest percentage NTW and those with a bachelor's degree reported the highest at 49% and 55% for the first and second doses, respectively. When reporting their self-described job, physicians-in-training had the lowest percentage of NTW while students had the highest percentage NTW for both doses. Additionally, there was demonstrated a statistically significant correlation between NTW and ethnicity, where Black or African Americans and White people had the lowest percentage of NTW.
The overall percentage of participants receiving the Moderna vaccine who were NTW in anticipation of potential side effects was 38% for the first dose and 49% for the second dose. Statistically significant associations were found between the percentage of NTW individuals after the second dose when stratified by age and by job. Regarding age and job status respectively, individuals aged 18–24 and students had the highest percentage of NTW, while technicians had the lowest. No statistically significant associations were found between the proportion of NTW and self-reported gender, education or ethnicity.
For Pfizer vaccine recipients, the overall mean (SD) length of absence was 0.1 days (0.61) for the first dose and 0.3 days (0.79) for the second dose. The maximum length reported was 10 days for both doses. Of note, the scale maximum was limited to 10 days and longer absences were not solicited. There was no statistically significant association between average length of absence and gender. However, significant associations were found between age and average length of absence after both doses. The age group 18–24 reported the longest average time off after vaccination. There were also statistically significant associations between education level, job and ethnicity and the average length of absence after both doses. For education, individuals with Doctorate or professional degrees and those with master's degrees tended to take fewer days off after vaccination than other participants. Regarding job descriptions, volunteers, attending physicians and physicians-in-training had the lowest average lengths of absence. For ethnicity, Native Hawaiian or Pacific Islander and White respondents reported the lowest average lengths of absence.
For Moderna recipients, the overall mean (SD) length of absence was 0.1 days (0.58) for the first dose and 0.4 days (0.81) for the second dose. The maximum length reported was 10 days and 9 days for the first and second doses, respectively. No statistically significant associations between average length of absence and gender, age, ethnicity, education or job description were found.
When controlled for systemic reactogenicity, using Wilcoxon rank-sum test, there were statistically significant differences in the average length of absence identified between those who reported systemic reactogenicity and those who reported only injection site complaints after both doses. The average length of absence was higher for those who reported systemic side effects compared to those who reported only an injection site effect.
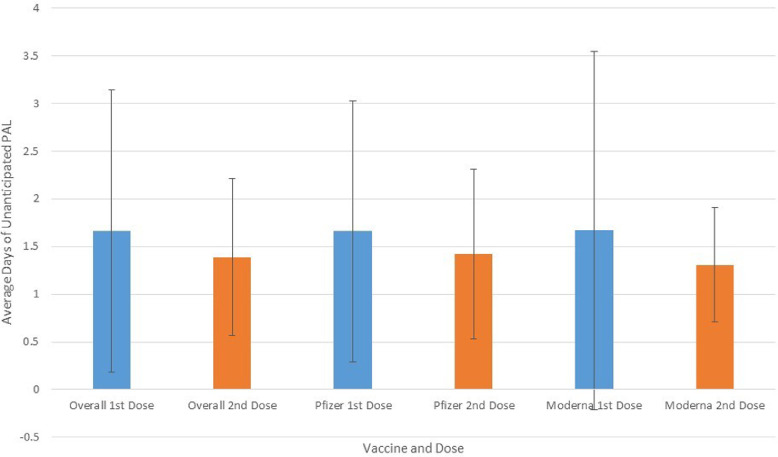
The data were then analyzed for the subgroup of individuals who were scheduled to work post vaccination yet required unanticipated PAL. After the first vaccination dose, there were 82 individuals who required non-scheduled PAL, constituting 4.9% of the 1673 individuals who chose to vaccinate but did not schedule, or modify their schedule, to allow their vaccine to coincide with leave afterwards. The average length of absence for this subpopulation was 1.66 days (SD = 1.48). After the second dose, a total of 360 individuals out of 1819 who were scheduled to work, or 19.79%, reported needing unscheduled PAL. The average length of absence was 1.39 days (SD = 0.82) for this cohort. There was no statistically significant difference in the average length of unanticipated PAL when stratified by vaccine manufacturer. A graphic representation of the results comparing vaccine manufacturers and the unscheduled PAL required is shown in Fig. 3 .
Fig. 3.
Unanticipated PAL seen by vaccine and dose.
There were no statistically significant associations found between the length of unexpected absence and gender, age, job or ethnicity. There was, however, a significant association between education level and the length of unanticipated PAL after the second dose, whereby individuals with a bachelor's degree had the highest average length of unanticipated PAL at 1.55 days (SD = 1.12).
Finally, 4.5% of the participants reported that they would not receive the vaccine. There were statistically significant associations between the cohort opting not to vaccinate and subgroups of gender, age, ethnicity, education, and job description. Female individuals were more likely not to vaccinate than their male counterparts. Younger people were more likely to opt out of vaccination than older individuals. None of the respondents greater than 65 years old refused COVID vaccination. The percentage of individuals refusing vaccination was highest, at 6.1%, in the 25–34-year-old cohort. Individuals with a lower level of education tended to show a stronger preference not to vaccinate. Those individuals with a higher education, i.e., at a master's or Doctor's levels, demonstrated the highest proclivity to vaccinate. When sorted by type of employment, those who self-described their employee status as technician or support staff were the least likely to vaccinate. Additionally when sorted by ethnicity, American Indian or Alaska Native and Black or African American individuals had relatively higher percentages of choosing not to vaccinate.
The free-text responses to the query “please tell us why you chose not to vaccinate” were analyzed with a word and phrase count algorithm for common themes and phrases and by hand for patterns of similar phrases. The most common phrases mentioned included:
-
•
“Side effects” or “long-term effects”—37 times
-
•
“Trust”, “Skeptic”, “Fear” or “comfort”—34 times
-
•
“Not approved”, “Made too fast”, “short trial”, or “experimental”—26 times
-
•
“Lack of research” or “Safety”—20 times
-
•
“Pregnancy”, “Childbearing”, “Breast feeding”, or “Conceive”—15 times
-
•
“Had COVID”—10 times
-
•
“Medical advice”—6 times
4. Discussion
In December 2020, the CDC Advisory Committee on Immunization Practices recognized that COVID-19 vaccination was expected to elicit systemic reactogenicity that may lead to healthcare personnel absenteeism and related acute staffing deficiencies17. This is the first known attempt to correlate vaccine adverse effects, enthusiasm, and the amount of unexpected personal leave required for vaccinated individuals.
The anecdotal observation that was the genesis for this project was made when approximately one fifth of the team members of the operating room staff at the authors’ hospital unexpectedly called out sick a day or so after their second Pfizer vaccination. Recognizing that time was of the essence, to limit recall bias, and to reach as many respondents as quickly and easily as possible, the decision was made to employ an advertisement placed in emailed employee and staff newsletters to recruit participants. When potential participants opened the electronic newsletter, they found a short recruitment statement to “Participate in a 5-minute survey on the side effects of COVID-19 vaccination” and a link that they were asked to click to join the study. This methodology is similar to that employed by email marketers, where the reader is asked to “click-through” using a link on the email to a specific site to take the survey18. Furthermore, it was recognized that limiting our participation to those who worked in the operating room may affect our ability to collect a statistically meaningful sample population size. As such, we targeted all individuals in the health system who would have been eligible for phase one vaccination, without predetermining the sample size required for statistical power. Additionally, we anticipated that a shot gunned direct marketing approach would produce a response rate which would provide an adequate sample size for statistical significance and that the targeted phase-one vaccination eligible individuals would provide a suitable surrogate population to represent the operating room staff.
According to direct marketing data collected by Constant Contact, an industry leader in direct email marketing, the overall average click-through rate, defined as the percentage of individuals who “click to enter” a proffered link, is 8.74% across all industries and 6.20% for the Health and Wellness subindustry19. As such, by these standards, our response rate of 12.15% should be considered quite robust. Unfortunately, although our recruitment goals included also soliciting non-vaccinated participants, the newsletter advertisement and the link to recruited individuals did not specifically mention this, a clear survey design oversight. This verbiage appears to have dissuaded some individuals who were not vaccinated from participating and may account for the 90% vaccination rate for all respondents, a rate considerably higher than the 71% vaccination rate reported in a contemporaneous study20.
The incidence of general side effects that we reported with the Pfizer vaccine of 90.8% on individuals having a minimum of one adverse reaction after the first dose and 86.4% after the second dose is consistent with the 87.1% reported by Klugar and colleagues in a similar retrospective cross-sectional study of COVID-19 vaccine reactogenicity completed in Germany21. Similarly, our data on type and duration of adverse reactions is similar to that seen in preclinical and clinical trials of both of the mRNA COVID-19 vaccines12, 13, 22, 23. However, the percentage of individuals who reported adverse effects in this study was higher across the board than that reported via the CDC V-Safe Surveillance System24, which tracks reactogenicity prospectively and in real-time. We attribute this to the selection bias created by our retrospective study design as well as a potential for recall bias also inherent in our retrospective study design.
How patients self-report adverse effects of vaccination is a multifactorial process and can be impacted by many interdependent intrinsic and extrinsic factors, including age, gender, general health, ethnicity, vaccine formulation, route of administration, injection technique and individual psychological stresses, as outlined in an excellent paper by Herve and colleagues. (Fig. 4 )25 As such, it is very challenging to assess the direct impact of any individual demographic factor on the severity and duration of vaccine reactogenicity, and those of our findings that showed statistical significance should be appreciated carefully within the complex and multifactorial nature of reactogenicity. Although not mentioned by Herve in her review, our data supports adding educational level to the intrinsic determinants of reactogenicity.
Fig. 4.
Summary of vaccination and host factors that can influence reactogenicity. With permission of the author25.
The CDC V-Safe Surveillance Reporting System for COVID-19 vaccinations has documented that local and systemic symptoms secondary to COVID vaccination are generally greater for younger adults as compared to those who are older26. Additionally, biological differences associated with gender can affect the severity and duration of the response to vaccination, with females historically reporting a greater degrees of fever, inflammation and pain than their male counterparts to vaccines directed towards viruses such as influenza, yellow fever and hepatitis27. While a number of authors have reported that female patients are more likely to report higher levels of injection site pain than men25, 27, our finding that female respondents reported statistically higher levels of systemic reactogenicity after mRNA vaccination than males was unexpected and would benefit from further validation, especially given that the Pfizer and Moderna COVID-19 vaccines are the first commercially available vaccines using mRNA technology. Our finding that the Moderna vaccination produces greater systemic reactogenicity than the Pfizer vaccine is supported elsewhere in the literature24, 28. While the statistical analysis demonstrates a number of demographic descriptors that have statistically significant associations with planned work schedule modifications and unexpected PAL, the clinical impact of these associations is multifactorial and requires additional research.
The duration of reactogenicity which we reported for both vaccines was consistent with the duration of symptoms reported by other researchers8, 9. While the reactions can last over a week, they typically resolve within 7 days, and generally peak on the second day post vaccination29.
A survey conducted in November and December of 2020, just prior to the emergency authorization of the COVID-19 vaccines, was published with a similar study population by Kuter et al.30. They reported that 63.7% of those surveyed planned to receive a COVID-19 vaccine, 26.3% were unsure, and that 10.0% did not plan to be vaccinated. Kuter's research also documented those individuals willing to be vaccinated were more likely male, older, better educated, and White or Asian, consistent with our findings regarding enthusiasm for COVID-19 vaccination. The mean enthusiasm for vaccination, which we measured at 7.7 out of 10, suggests an improved overall degree of enthusiasm since the study by Kuter was published in February 2021 using data collected in the 2-month window previously mentioned.
Similarly, the acceptance rate of vaccination within our study population was improved from the pre-vaccination group noted above. Optimistically, our 4.5% vaccination refusal rate suggests that education, public relation efforts and time have made the healthcare population less resistant to vaccination. However, the bias inherent in our sampling methodologies may cloud this optimistic conclusion. Additionally, our results corroborate the demographics noted by Kuter, confirming that individuals less likely to vaccinate were female, of a younger age, with a lower education level and either American Indian, Alaskan, Black or Native American.
The negative correlation between enthusiasm for vaccination and reactogenicity which we found was also unexpected and may also be secondary to the sampling methods employed for this project. However, if this trend were to be validated with prospective research, it suggests that the vaccine hesitant portion of the population, presumed to be those with lower enthusiasm, are more prone to appreciate adverse symptoms and at increased risk for work absences. Should this negative correlation hold true, as the vaccine hesitant portion of the population gradually become vaccinated, we would expect that the impact on work related absence for this sub-population would be higher than the early-adopting enthusiastic individuals. Furthermore, we would expect a higher subjectively reported symptoms and a greater need for scheduled and unscheduled vaccination reactogenicity-associated PAL.
Several interesting observations may be appreciated from the data regarding individuals planning to schedule themselves to work post vaccination. Older individuals, specifically those in the 55–64 age group, were the most likely to schedule themselves to work after vaccination, while younger individuals, ages 18–24 were the most likely to proactively schedule time off. While the age groups used for our survey do not clearly parallel the traditional generational demarcations, there is a similarity between our older respondents and the traditional Baby Boomer “work comes first” mentality. Similarly, the “work-life balance” credo of the Millennials and Generation Z cohorts is exhibited in the statistics documenting that the younger individuals in the 18–24-year-old cohort were the most likely to postpone returning to work after inoculation.
A similar socioeconomic observation can be made regarding educational level, in that those with a high school degree or less are most likely to schedule themselves to work post vaccination with both vaccine manufacturers’ products. Although no clear explanation is offered from the data, it may be that these individuals represent those with the lowest income and would be financially impacted most by missing a day or two due to simply the anticipation of reactogenicity. In a similar vein, the data for both producers, when sorted by job description, demonstrates that doctors in training are most likely to work post vaccination. This data point may speak to the cultural expectations of long work hours and a “pay your dues” mentality still widely present in medical training.
When individuals were either scheduled for time off after vaccination or proactively modified their individual schedule in anticipation of reactogenicity, they did not require significant and unexpected PAL. However, when vaccine related reactogenicity was not anticipate by either the scheduler or the individual employee, a significant amount of unexpected down time was seen after vaccination for a non-trivial amount of respondents. For the second vaccination, nearly one out of every 5 individuals reported requiring unanticipated PAL, a situation which could create significant staffing issues for any surgical, nursing or medical unit.
The impact of this should be clear to the reader: should a COVID-19 mRNA booster/third shot be necessary, as many are suggesting31, staff scheduling in operating suites and other critical locations must proceed in a proactive and thoughtful manner with anticipation of an impact of vaccine related side effects on staff availability. Similarly, as Pfizer's and Moderna's COVID-19 vaccines are the first widely administered vaccines using this technology, it is likely that subsequent mRNA vaccine approaches to other pandemic or endemic disease vectors could produce similar reactogenicity on par with that reported here requiring similar levels of PAL. Additionally, mRNA technology is a promising candidate for cancer immunotherapy32, 33. Similar or worse reactogenicity may be expected with this population due to both the vaccines and the potential immunosuppressed nature of this population. Thankfully, the operating room should not be significantly impacted by the individual mRNA treatment for oncological patients.
In addition to an ongoing pandemic, the US is currently experiencing acute shortages of physicians, nurses and trained operating room personnel34, 35. Personnel costs, including wages and benefits, have been estimated to account for up to 40% of the total cost of running an operating room36. As such, it is of critical importance to be able to anticipate the impact of vaccine reactogenicity on operating room staffing, and to be able to coordinate vaccination scheduling and the anticipated work absences with operating room demand and personnel scheduling.
The free-text key-word response analysis revealed several words and phrases which suggest that further progress can be made in decreasing the number of individuals choosing not to vaccinate. Even though the data collection method we designed was biased to recruiting those who chose to vaccinate, much can still be gained from the free text responses of those who chose not to vaccinate. Since this project was conceived, the CDC has released recommendations stipulating that pregnant and lactating individuals should receive the COVID vaccination, hopefully addressing one of the hesitation factors cited by our non-vaccinated respondents37.
This study has a number of strengths as well as some weaknesses and limitations. The anecdotal observation which lead to this study necessitated a retrospective data collection methodology, where significant recall bias could be expected. However, the total number of responses received was very robust and we have documented that a direct-marketing strategy can work well to collect medical research data at an expedited pace. Unfortunately, the study methodology may have created a non-response/participation bias that limited the participation of the number of individuals who refused vaccination or those who did not experience reactogenicity. This bias may have accounted for the larger overall percentage of those reporting reactogenicity than those in prospective research12, 13. Additionally, the anecdotal observation that led to the study necessitated a rapid roll out of the survey to capture as much timely data as possible. Although the survey methodology used proven and validated techniques such as Likert scales, the content validity was not formally tested as part of the surveying process for fear of increasing the non-response and recall biases by delaying the survey further for formal validation.
Furthermore, as the population of operating room personnel available in system was deemed too small to provide statistical power, it was decided to collect data from all healthcare system individuals who were eligible for early vaccination, as opposed to just operating room individuals. This expansion of the sample population makes extrapolation necessary when the goal was to reflect to the operating room staff population, but we feel that the impact of this extrapolation is negligible as the survey participants were part of the same cohort of stage one vaccination eligible individuals as the operating room staff.
Finally, the sampling method, which relied on emailed newsletters, biased the respondent sample to those who read the newsletters and furthermore to those who chose to “click through”. This sampling bias, as well as the preponderance of nurses responding, may account for the overwhelming of number of female respondents and those who describe their job type as “other”.
5. Conclusions
Local and systemic reactogenicity are known and expected occurrences after vaccination, including with the Pfizer and Moderna mRNA COVID-19 vaccinations. Vaccine reactogenicity is a complex and multifactorial subject with interdependent determining factors, including education level. Statistically, enthusiasm for vaccination has an inverse relationship with the amount of time off required after COVID-19 mRNA vaccination, and this knowledge may prove valuable in the future as additional mRNA vaccinations and doses are recommended. Managers should encourage employees to receive vaccination in a fashion that coordinates with operating room scheduling, allowing for reactogenicity with non-scheduled time after injection. When scheduled and proactive paid administrative leave is not anticipated to the individual team member, it should be anticipated up to 5 and 20 percent of vaccine recipients will require unanticipated time off for the first and second inoculation respectively. Although speculation, it is assumed that reactogenicity for a booster dose would be similar that of the second scheduled dose and a similar impact on unscheduled PAL would be anticipated. This unanticipated PAL has the potential to have significant and direct impact on operating room staffing and patient care, especially considering the current physician and nursing shortages.
Author statement
Marc Levi: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Management, Methodology, Supervision, Writing-original draft, Writing-review and editing, Visualization. Daniel McMillan: Writing-review and editing. Vishal Dhandha: Writing-review and editing. Jennifer Allan: Writing-review and editing, Data analysis. Fran D'Ercole: Conceptualization, Writing-review and editing.
Funding source
Funded by an internal department grant from the University of North Carolina at Chapel Hill Department of Anesthesiology.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank Wanting Jin and Quefeng Li of the UNC Department of Biostatistics for their statistical analysis expertise as well as Kari Balfanz, RN for her help in the conceptualization of this project.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.pcorm.2021.100220.
Appendix. Supplementary materials
References
- 1.World Health Organization. [Online] 2020. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/.
- 2.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China s.l. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ritchie H., Ortiz-Ospina E., Beltekian D., et al. 2021. Our world in data. Coronavirus (COVID-19) deaths.https://ourworldindata.org/covid-deaths [Online] April 19. [Google Scholar]
- 4.Burkle F.M., Bradt D.A., Ryan B.J. Global public health database support to population-based management of pandemics and global public health crises, part I: the concept s.l. Prehosp Disaster Med. 2021;36(1):95–104. doi: 10.1017/S1049023x20001351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soreide K., Hallet J., Matthews J.B., et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services s.l. Br J Surg Soc. 2020;107(10) doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papagiannopoulos P., Ganti A., Kim Y.J., et al. Impact of COVID-19 pandemic on ambulatory and operating room Rhinology practice in the US. Chicago : Am J Rhinol Allergy. 2020;35(4):441–448. doi: 10.1177/1945892420961962. [DOI] [PubMed] [Google Scholar]
- 7.Wohler A.D., Kneisl J.S., Macknet D.M., et al. Surgical re-entry strategy following COVID-19 pandemic s.l. Med Care. 2021;59(3):220–227. doi: 10.1097/MLR.0000000000001471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Food and Drug Administration . 2021. Pfizer-BioNTech COVID-19 Vaccine.https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine [Online] April 9[Cited: April 14, 2021.] [Google Scholar]
- 9.U. S . 2021. Food and Drug Administration. Moderna COVID-19 Vaccine.https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/moderna-covid-19-vaccine [Online] April a[Cited: April 14, 2021.] [Google Scholar]
- 10.Verger P., Dube E. Restoring confidence in vaccines in the COVID-19 era s.l. Expert Rev Vaccines. 2020;11:991–993. doi: 10.1080/14760584.2020.1825945. [DOI] [PubMed] [Google Scholar]
- 11.K Dooling ACIP COVID-19 Vaccines Work Group. Phase 1 allocation COVID-19 vaccine: Work Group Considerations. 9. 2020:22. [Online] Center for Disease Control [Cited: 3 25, 2021] https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-09/COVID-07-Dooling.pdf.
- 12.Fernando P, Polack M.D., Stephen J, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine s.l. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baden L.R., El Sahly H.M., Essink B., et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 Vaccine s.l. N Engl J Med. 2021;384(5):403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Unpublished personal communication. 02 2, 2021.
- 15.COVID-19 Leave Information-UNC Human Resources . Vol. 3. 2021. https://hr.unc.edu/benefits/covid-leave/ (University of North Carolina Health System). [Online] [Cited: 4 5, 2021.] [Google Scholar]
- 16.Weisman R. Boston Globe Meddia Partners; Boston: 2020. COVID Vaccines Could Reach Senior Care Sites this Month, but Daunting Logistical Challenges Lie Ahead.http://www.proquest.com/newspapers/covid-vaccines-could-reach-senior-carethis/docview/2468064616/se2?accountid=14244 [Online Article]LLC09 Dec. [Google Scholar]
- 17.Center for Disease Control and Prevention. Interim considerations for COVID-19 vaccination of healthcare personnel and long-term care facility residents. [Online] December 3, 2020. [Cited: June 14, 2021.] https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19/clinical-considerations.html.
- 18.A., Hayes. Click-through rate (CTR) definition. investopedia. [Online] Investopedia, August 26, 2020. [Cited: September 13, 2021.] https://www.investopedia.com/terms/c/clickthroughrates.asp.
- 19.Constant Contact . 2021. Average Industry Rates for Email as of.https://knowledgebase.constantcontact.com/articles/KnowledgeBase/5409-average-industry-rates?lang=en_US#compare AugustConstant Contact. [Online] Constant Contact, September 9, 2021. [Cited: September 13, 2021.] [Google Scholar]
- 20.Fossen M., Bethany M., Modak S., Parris S., Modak R. Who’s vaccinated? A closer look at healthcare workers’ coronavirus disease 2019 (COVID-19) COVID-19 vaccine hesitancy and demographics s.l. Infect Control Hosp Epidemiol. 2021;1-2 doi: 10.1017/ice.2021.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klugar M., Riad A., Mekhemar M., et al. Side effects of mRNA-based and viral vector-based COVID-19 vaccines among German healthcare workers Basel. Biology (Basel) 2021;10(8):752. doi: 10.3390/biology10080752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathioudakis A.G., Ghrew M., Ustianowski A., et al. Self-reported real-world safety and reactogenicity of COVID-19 vaccines: a vaccine recipient survey. Basel, Switzerland : Life. 2021;11(3):249. doi: 10.3390/life11030249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackson L.A., et al. An mRNA vaccine against SARS-CoV-2–preliminary report 20, s. N Engl J Med. 2020;383 doi: 10.1056/NEJMoa2022483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chapin-Bardales J., Gee J., Myers T. Reactogenicity following receipt of mRNA-based COVID-19 vaccines 21, s.l. JAMA Insights. 2021;325(21):2201–2202. doi: 10.1001/jama.2021.5374. [DOI] [PubMed] [Google Scholar]
- 25.Herve C., Laupeze B., Giudice G.D., Am Didierlaurent, Tavares Da Silva F. The how’s and what’s of vaccine reactogenicity s.l. npj Vaccines. 2019;4:39. doi: 10.1038/s41541-019-0132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gee J., marquez P., et al. CDC weekly. CDC Wkly Rep. 2021;8:70. [Google Scholar]
- 27.Klein S.L., Jedlicka A., Pekosz A. The Xs and Y of immune response to viral vaccines May, Baltimore. Lancet Infect Dis. 2010;10(5):338–349. doi: 10.1016/S1473-3099(10)70049-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meo S.A., Bukhari I.A., Akram J., Meo A.S., Klonoff D.C. COVID-19 vaccines: comparison of biological, pharmacological characteristics and adverse effects of Pfizer/BioNTech and Moderna vaccines s.l. Eur Rev Med Pharmacol Sci. 2021;25:1663–1669. doi: 10.26355/eurrev_202102_24877. [DOI] [PubMed] [Google Scholar]
- 29.Kadali R.A.K., Janagama R., Peruru S., et al. Non-life-threatening adverse effects with COVID-19 mRNA-1273 vaccine: a randomized, cross-sectional study on healthcare worker with detailed self-reported symptoms. Lillington : J Med Virol. 2021;93:4420–4429. doi: 10.1002/jmv.26996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuter B., Brown S., Momplaisir F.M., et al. Perspectives on the receipt of a COVID-19 vaccine: A survey of employees in two large hospitals in Philadelphia Offit P. 1693-1700, s.l. Vaccine. 2021;39 doi: 10.1016/j.vaccine.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Briefing Daily. The Advisory Board; 2021. When Will You Need a Covid-19 Booster Shot? Here's What Experts Say.https://www.advisory.com/daily-briefing/2021/05/20/booster-shot [Online] The Advisory Board, May 20[Cited: June 21, 2021.] [Google Scholar]
- 32.Yue Yin, Li Xiaoyang, Ma Haixia, et al. In situ transforming RNA nanovaccines from polyethylenimine functionalized graphene oxide hydrogel for durable cancer immunotherapy. Nano Lett : Am Chem Soc. 2021;21(5):2224–2231. doi: 10.1021/acs.nanolett.0c05039. [DOI] [PubMed] [Google Scholar]
- 33.Ball P. The lightening-fast quest for COVID vaccines - and what it means for other diseases s.l. Nature. 2021;589(7840):16–18. doi: 10.1038/d41586-020-03626-1. [DOI] [PubMed] [Google Scholar]
- 34.IHS Markit Ltd. The Complexities of Physician Supply and Demand: Projections From 2019 to 2034 . 2021. Washington : American Association of Medical Colleges.https://www.aamc.org/data-reports/workforce/data/complexities-physician-supply-and-demand-projections-2019-2034 [Google Scholar]
- 35.Mehdaova E. MD : Walden University Scholar Works; 2017. Strrategies to Overcome the Nursing Shortage. Minneapolis.https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=5933&context=dissertations [Google Scholar]
- 36.Childers C.P., Maggard-Gibbons M. Understanding costs of care in the operating room 4, s.l. JAMA Surg. 2018;153 doi: 10.1001/jamasurg.2017.6233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Center for Disease Control and Prevention . 2021. Center for Disease Control and Prevention–COVID-19. COVID-19 Vaccines While Pregnant or Breastfeeding.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html [Online] June 16[Cited: June 21, 2021.] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.