Abstract
Background
Evidence suggests that the outbreak of the coronavirus disease 2019 (COVID-19) and the prevention/control measures for COVID-19 may cause insomnia during the acute phase of COVID-19 pandemic in China. However, it is unclear whether insomnia sustains during the later phases of the pandemic.
Methods
We searched PubMed/Medline, EMBASE, PsycINFO and China National Knowledge Infrastructure from the 27th December 2019 to the 2nd February 2021. As early stage studies on COVID-19 pandemic in China were defined as those conducted prior to April 1st, 2020, while late stage studies were those conducted after April 1st, 2020.
Results
A total of 98 studies with 193,889 participants were included. The pooled prevalence of insomnia symptoms among all populations was 39.1% (95% CI 36.2–42.0%); the pooled prevalence of insomnia symptoms during the early and late stages of COVID-19 in China were 37.0% (95% CI 34.1–39.9%) and 41.8% (95% CI 33.6–50.0%), respectively. Importantly, there was no significant difference regarding the prevalence of insomnia symptoms between the early and late stages of COVID-19. Meta-regression showed that healthcare workers, COVID-19 patients, patients with chronic medical conditions and patients with mental disorders had a higher prevalence of insomnia symptoms compared to the general population. This association remained significant in healthcare workers and patients with chronic medical conditions after adjusting for age, gender, areas of high or low prevalence of COVID-19 cases, anxiety and depression.
Conclusions
Over one third of our sample present insomnia symptoms during the early stage of COVID-19 pandemic in China. Interestingly, prevalence of insomnia symptoms sustains high during the late stage of the pandemic despite the control of the disease and the amelioration of its adverse effects. Our findings suggest that insomnia symptoms related to COVID-19 appear to persist of over time.
Keywords: COVID-19, Sleep, Insomnia, China
Abbreviations: 2019-nCoV/SARS-CoV-2, 2019 Novel Coronavirus; AHRQ, Agency for Healthcare Research and Quality; AIS, Athens Insomnia Scale; CI, Confidence Interval; CNKI, China National Knowledge Infrastructure; COVID-19, Coronavirus Disease 2019; ISI, Insomnia Severity Index; MERS, Middle East Respiratory Syndrome; PSQI, Pittsburgh Sleep Quality Index; SARS, Severe Acute Respiratory Syndrome; SRSS, Self-Rating Scale of Sleep
1. Introduction
Beginning in late December 2019, an outbreak of a highly contagious, novel coronavirus (2019-nCoV/SARS-CoV-2) that causes respiratory infections and pneumonia in humans was observed in Wuhan city, Hubei Province of China. Since then, the coronavirus disease 2019 (COVID-19) rapidly spread throughout China and worldwide, began January 27th, 2020 and maintained an upward trend until February 27th, 2020 in China [1]. On the 30th January 2020, the World Health Organization declared COVID-19 a Public Health Emergency of International Concern [2], and on 11th March 2020, a global pandemic [3].
During the acute phase of COVID-19 pandemic (January 23rd-February 21st, 2020), the Chinese government implemented a range of strict measures to control the COVID-19 pandemic [3]. For example, all COVID-19 patients were treated and quarantined in hospitals, whereas close-contacts and front-line healthcare workers were quarantined in hotels. Furthermore, residents were under home-quarantine during the peak of the pandemic, except those who were needed to guarantee the basic functions of a city. In addition, social distancing policies, wearing face masks in public, mandatory lockdowns, as well as work and school closings were implemented. Though these critical control measures changed normal life, they were one of the best ways to control the spread of the virus, since no successful treatments or vaccines were available. Fortunately, since mid-February 2020, the COVID-19 pandemic has been under control in China. Specifically, newly cured and discharged cases outnumbered newly confirmed ones since February 19th, 2020 with no new domestic cases confirmed on the Chinese mainland for the first time on March 18th, 2020 [3], and all temporary treatment centers for COVID-19 patients were closed on March 20th, 2020 [4]. Importantly, the daily mortality cases of COVID-19 in China have dropped to signal digits since March 18th, 2020 and no daily mortality cases were reported on most days after mid-March 2020 [1].
The outbreak of the disease and the mass lockdowns during the acute phase of COVID-19 pandemic caused fear of getting sick, disrupted thousands of lives and impacted commerce. It was also related to psychological distress and sleep disturbance such as insomnia symptoms. During the acute phase of the COVID-19 pandemic, our group conducted an online survey with a total of 3637 adults from all 31 provinces in mainland China [5]. In this nationwide survey based on self-reported data, we found that the prevalence of insomnia (Insomnia Severity Index [ISI]>7, 33.7% vs. 26.2%) and time in bed (531.5 ± 94.2 vs. 485.5 ± 72.6 minutes) were increased, while sleep efficiency (86.8% vs. 88.5%) was decreased during the pandemic compared to the pre-pandemic period. Also, delayed bedtime (25.6 ± 66.3 minutes) and wake-up time (71.7 ± 89.5 minutes) were observed.
Since mid-March 2020, work and daily life gradually returned to normal among most provinces in China, and the newly confirmed cases resulted mainly from inbound cases [3]. From the end of March 2020, China entered a new phase of COVID-19 since the pandemic has been basically under control, and the measures to control it have become less strict. For example, the government's effort has shifted to preventing inbound cases by domestic large-scale SARS-CoV-2 nucleic acid testing and hotel-quarantining of inbound arrivals at all points of entry. In addition, the government stressed the need to speedily resume commerce and normal life, as soon as possible.
The different stages of COVID-19 pandemic raise a fundamental question: was the impact of COVID-19 on insomnia different during the early and late stages of COVID-19 pandemic? To our knowledge, no review or meta-analysis has examined the impact of the pandemic on sleep during the early and late stages of COVID-19 pandemic in China. To address this gap in the literature, the aims of this study were (1) to conduct a systematic review and meta-analysis on the prevalence of insomnia symptoms during the early and late stages of the COVID-19 pandemic in China, and (2) to determine the prevalence of insomnia symptoms in specific populations during the pandemic.
2. Methods
2.1. Search strategy
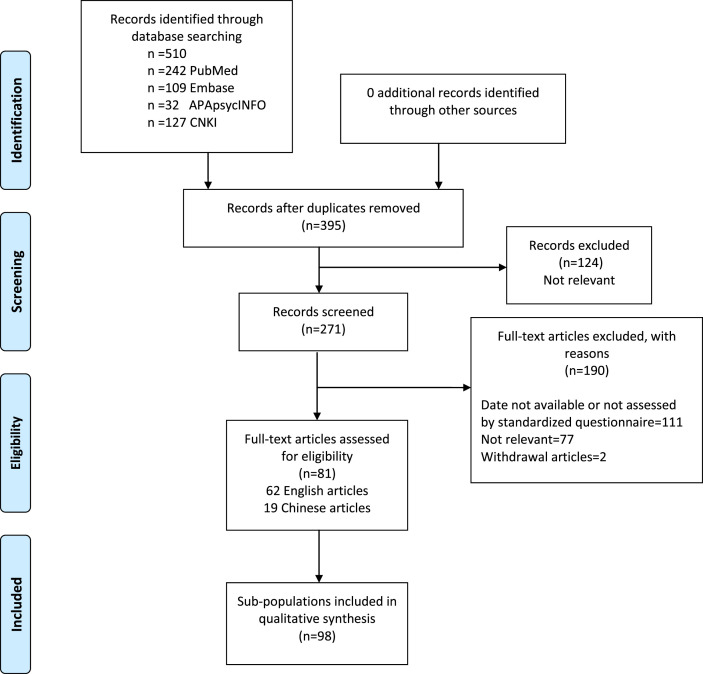
We conducted this review and meta-analysis according to Preferred Reporting Items for Systematic Review and Meta-analysis protocols (PRISMA-P) checklist [6]. This study was registered in the Prospective Register of Systematic Reviews (CRD 42021236518). We searched PubMed/Medline, EMBASE, PsycINFO and China National Knowledge Infrastructure (CNKI) form 27th December, 2019 (when China reported the first case of SARS-CoV-2 in Wuhan [3]) to the 2nd February, 2021 using following key terms (“sleep” OR “insomnia”) AND (“COVID-19″ OR “SARS-COV-2″) AND “China”. Reference lists of selected studies were searched to identify further papers. Fig. 1 depicts the study selection process.
Fig. 1.
PRISMA flow diagram of study inclusion. PRISMA=Preferred Reporting Items for Systematic Review and Meta-analysis protocols checklist.
Two researchers (Hong Z and Sun Q) independently assessed articles for eligibility for inclusion. Any disagreements were settled by the senior author (Li Y). The inclusion criteria were: 1) published or online in a peer-reviewed journal; 2) articles in the English or Chinese language; 3) population in China; 4) reported prevalence of insomnia symptoms after the 27th December, 2019 [3]; and 5) used well-established validated scales/questionnaires to measure sleep. In order to diminish the bias of prevalence of insomnia symptoms due to non-standardized scales/questionnaires, we did not include studies that used self-designed measures or a subsection or cluster of questions to measure sleep problems. The exclusion criteria were: 1) use of self-designed measures or a subsection or cluster of questions to report sleep problems; 2) abstracts; 3) articles that did not report insomnia data; 4) reviews or case reports.
2.2. Data extraction
To confirm the accuracy, two researchers (Chen B & Dai Y) independently extracted relevant variables (eg, first author's name, research date, population, sample size, age, prevalence of insomnia symptoms, anxiety symptoms, and depressive symptoms, measures of sleep, Supplementary Table 1). If the prevalence of insomnia symptoms was provided for subgroups rather than the total sample, they were considered as separate studies in the subsequent data extraction and analyses. If the prevalence of insomnia symptoms was provided for the total sample and subgroups simultaneously, the data of the total sample was extracted and used for analyzing the estimated pooled prevalence among the overall population, while the data of the subgroups was used for analyzing the estimated pooled prevalence in the corresponding subgroups.
2.3. Definitions of early and late stages of COVID-19 pandemic in China
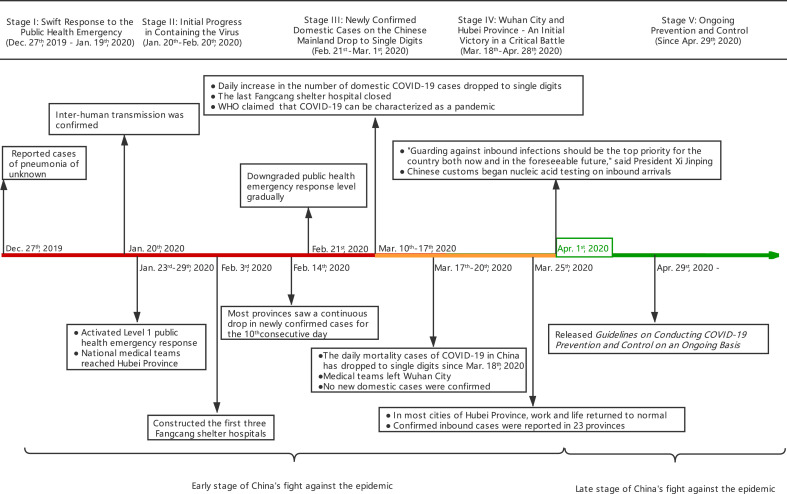
The “early stage” of COVID-19 pandemic in China was defined as the time between December 2019 and April 1st, 2020, and the “late stage” of COVID-19 pandemic in China was the time after April 1st, 2020 (see Fig. 2 ). The reasons for choosing April 1st, 2020 as the cut-off point were: 1) According to the official data from Chinese Center for Disease Control and Prevention [1], the daily mortality cases of COVID-19 in China have dropped to signal digits since March 18th, 2020. More importantly, no daily mortality cases of COVID-19 were reported on most days after mid-March, 2020; 2) no newly diagnosed domestic cases were confirmed in the Chinese mainland for the first time on March 18th, 2020 [3]; 3) all temporary treatment centers (ie, Fangcang shelter hospitals) were closed on March 20th, 2020 [4], and 4) the daily life and work of most people returned to normal since the end of March 2020 [3].
Fig. 2.
Milestone events of China during the outbreak and epidemic of COVID-19. These milestone events mainly refer to “Fighting Covid-19, China in Action”. Fangcang shelter hospitals: large-scale, temporary hospitals, rapidly built by converting existing public venues, such as stadiums and exhibition centers, into health-care facilities. Red color, acute phase of COVID-19 pandemic in China. Yellow color, transition period of COVID-19 pandemic in China. Both red and yellow periods indicate the early stage of COVID-19 pandemic in China; Green color depicts the period of COVID-19 under control in China (late stage of COVID-19 pandemic in China). The “early stage” of COVID-19 pandemic in China was defined as the time between December 2019 and April 1st, 2020, and the “late stage” of COVID-19 pandemic in China was the time after April 1st, 2020. WTO=World Trade Organization.
2.4. Definitions of insomnia symptoms
In this meta-analysis, insomnia symptoms were defined based on the well-established validated scales/questionnaires that assess insomnia symptoms from the original studies.
2.5. Assessment of study quality
The study quality was assessed using an 11-item checklist which was recommended by the Agency for Healthcare Research and Quality (AHRQ) [7]. An item would be scored ‘0’ if the answer was ‘NO’ or ‘UNCLEAR’; and “1” if the answer was ‘YES’, then the item would be scored ‘1’. Article quality was assessed as follows: low quality = 0–3; moderate quality = 4–7; high quality = 8–11. The total scores and detailed AHRQ checklist for each article were provided in Supplementary Table 2.
2.6. Statistical analysis
The pooled prevalence and 95% confidence intervals (95% CIs) of insomnia symptoms were calculated according to the Cochrane Handbook [8]. Since the I2, an indicator of heterogeneity, was greater than 50% in all meta-analyses, random effect was used for all models [8]. As the prevalence of insomnia symptoms may vary among different populations, subgroup meta-analyses were conducted to assess the pooled prevalence of insomnia symptoms in the general population, healthcare workers, COVID-19 patients, patients with chronic medical conditions and patients with mental disorders. Considering that the COVID-19 pandemic may have different effects on front-line and non-front-line healthcare workers, we also calculated the pooled prevalence of insomnia symptoms within the two subgroups, separately. In this study, “front-line healthcare worker” was defined as employees in healthcare provision who were in direct contact with COVID-19 patients. Moreover, subgroup analyses of different age groups (age ≥50 years vs. <50 years) and areas of high vs. low prevalence of COVID-19 cases (Hubei Province vs. non-Hubei Provinces or mixed samples) were also conducted.
Meta-regressions were conducted to examine the potential risk factors for insomnia symptoms in specific sub-populations (ie, general population, healthcare workers, COVID-19 patients, patients with chronic medical conditions, and patients with mental disorders). In the regression models, we always considered the general population as the reference, while the other four sub-populations were independent covariates. In model 1, we included four sub-populations in the meta-regression to examine the association of each sub-population with insomnia symptoms compared to the general population, while in model 2 we further adjusted for age and gender (male percentage). In model 3, we further adjusted for prevalence of depressive and anxiety symptoms and areas of high or low prevalence of COVID-19 cases, given the effect of these parameters as well as anxiety and depression may have effects on insomnia symptoms. Publication bias was only assessed by inspection of a funnel plot if there were 10 or more studies available for analysis [9]. Sensitivity analyses were used to test the stability of results. A p-value<0.05 was considered statistically significant. All statistical analyses were conducted by using Stata software (STATA 14.0, Stata Corp, College Station, Texas, USA) and R Project (R 3.4.2, R Foundation for Statistical Computing, Vienna, Austria).
3. Results
3.1. Characteristics of included studies
A total of 395 articles and abstracts were identified in the search strategy. Screening of titles and abstracts resulted in 271 articles for evaluation. Upon removing ineligible articles, 81 articles were included in this meta-analysis. Since the data were provided by different types of populations in 14 articles, they were considered as separate studies in the subsequent data analyses. Thus, 98 studies with 193,889 subjects were included in the final analyses. Among the 98 studies, 82 (83.6%) studies were conducted during the early stage and 8 (8.2%) were during the late stage of the COVID-19 pandemic in China, while 8 (8.2%) did not provide research dates. Regarding the study populations, 34 studies focused on the general population, 42 on healthcare workers, 6 on COVID-19 patients, 5 on patients with chronic medical conditions and 2 on patients with mental disorders. The main characteristics of the studies included are presented in Supplementary Table 1. The median scores of the AHRQ checklist were 6 points (Supplementary Table 2).
Among the 98 included studies, 56 (57.1%) assessed insomnia symptoms using the ISI, 37 (37.7%) using the Pittsburgh Sleep Quality Index (PSQI), 4 (4.0%) using the Athens Insomnia Scale (AIS), and one using the Self-Rating Scale of Sleep (SRSS). The cut-off points of sleep scales/questionnaires used to define insomnia symptoms in each study are shown in Supplementary Table 1.
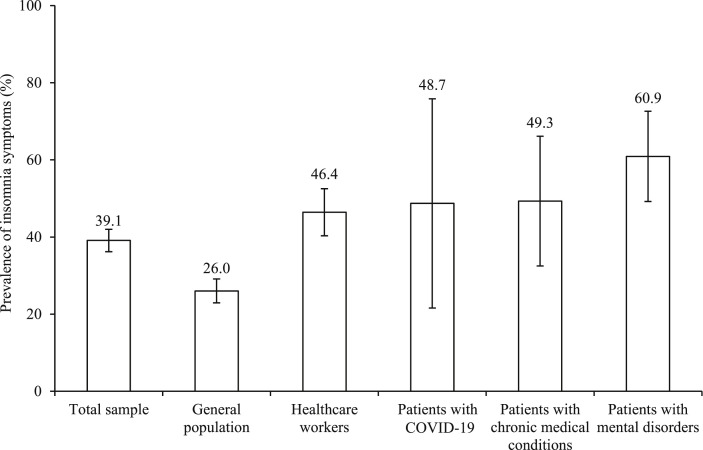
3.2. Insomnia symptoms among the overall sample during the COVID-19 pandemic
Among the 98 studies included with 193,889 participants, prevalence of insomnia symptoms ranged from 2.6% to 100% during the COVID-19 pandemic in China. Random-effects meta-analysis showed that the overall estimated pooled prevalence of insomnia symptoms was 39.1% (95% CI 36.2–42.0%, I2 = 99.5%, Fig. 3 and Supplementary Fig. 1). Inspection of funnel plot indicated no significant publication bias (Supplementary Fig. 2). Sensitivity analysis confirmed the stability of the result was not violated after omitting any particular study. Furthermore, the estimated pooled prevalence of insomnia symptoms was close (38.4%, 95% CI 35.3–41.4%, I2 = 99.5%) when the 83 studies with moderate-to-high quality were analyzed. The prevalence of insomnia symptoms in studies using different sleep scales is provided in Supplementary Fig. 1. Subgroup analyses showed that the studies with older adults (mean age ≥50 years: 49.7%, 95% CI 43.0–56.5%; mean age <50 years: 38.8%, 95% CI 35.7–42.0%; between group p = 0.033, Supplementary Fig. 3) and the people in high prevalence COVID-19 case areas (Hubei Province: 50.2%, 95% CI 42.6–57.7%; non-Hubei Province or mixed samples: 32.9%, 95% CI 30.0–35.8%, between group p < 0.001). had higher pooled prevalence of insomnia symptoms (Supplementary Fig. 4).
Fig. 3.
Prevalence of insomnia symptoms among specific sub-populations. Error bars indicate the 95% confidence interval.
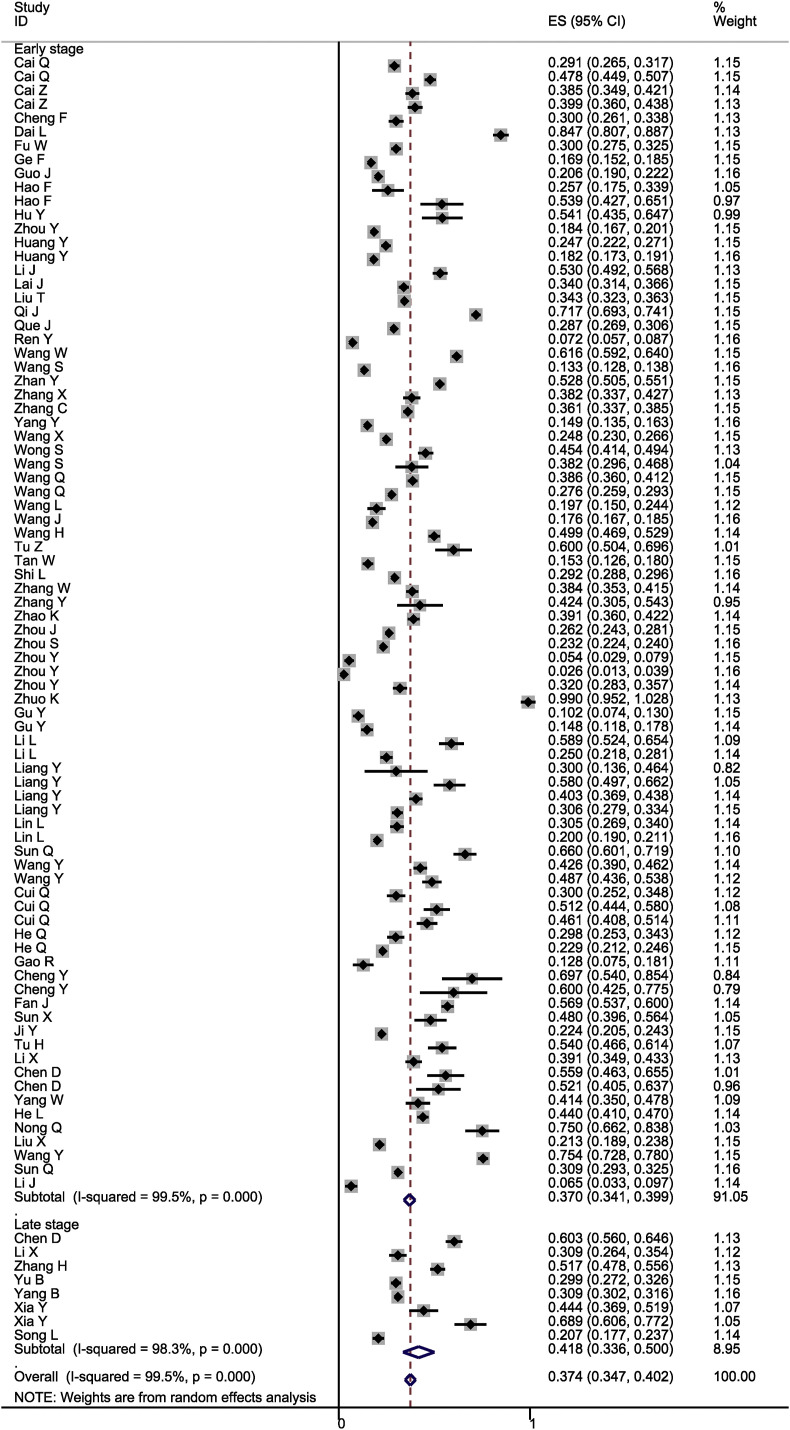
3.3. Insomnia symptoms during the early stage of COVID-19 pandemic
Among the 82 studies with 172,607 participants, prevalence of insomnia symptoms ranged from 2.6% to 100% during the early stage of the COVID-19 pandemic in China. Random-effects meta-analysis showed that the estimated pooled prevalence of insomnia symptoms during the early stage was 37.0% (95% CI 34.1–39.9%, I2 = 99.5%, Fig. 4 ). Inspection of the funnel plot indicated no significant publication bias (Supplementary Fig. 5), and sensitivity analysis confirmed that the stability of the result was not violated after omitting any particular study.
Fig. 4.
Forest plot of prevalence of insomnia symptoms during the early and late stages of COVID-19 pandemic in China. The “early stage” of COVID-19 pandemic in China was defined as the time between December 2019 and April 1st, 2020, and the “late stage” of COVID-19 pandemic in China was the time after April 1st, 2020.
3.4. Insomnia symptoms during the late stage of the COVID-19 pandemic
Among the eight studies with 18,663 participants, prevalence of insomnia symptoms ranged from 20.7% to 68.9% during the late stage of the COVID-19 pandemic in China. Random-effects meta-analysis showed that the estimated pooled prevalence of insomnia symptoms during the late stage was 41.8% (95% CI 33.6–50.0%, I2 = 98.3%, Fig. 4), and sensitivity analysis confirmed that the stability of the result was not violated after omitting any particular study. In comparing the estimated pooled prevalence of insomnia symptoms between the early (37.0%, 95% CI 34.1–39.9%) and the late stage (41.8%, 95% CI 33.6–50.0%) of the COVID-19 pandemic in China, no significant difference was observed (between-group p = 0.682, Fig. 4).
3.5. Insomnia symptoms in specific sub-populations
In order to examine the prevalence of insomnia symptoms in specific sub-populations during the COVID-19 pandemic in China, we conducted the following subgroup analyses among the overall samples.
3.5.1. General population
Among the 37 studies with 155,583 subjects including the general population samples, prevalence of insomnia symptoms ranged from 2.6% to 60.3% during the COVID-19 pandemic in China. Random-effects meta-analysis showed that the estimated pooled prevalence of insomnia symptoms was 26.0% (95% CI 23.0–29.1%, I2 = 99.5%, Fig. 3). No publication bias was observed based on the funnel plot (Supplementary Fig. 6), and sensitivity analysis confirmed that the stability of the result was not violated after omitting any particular study.
3.5.2. Healthcare workers
Among the 48 studies with 33,021 subjects including healthcare workers, prevalence of insomnia symptoms ranged from 14.2% to 100% during the COVID-19 pandemic in China. Random-effects meta-analysis showed that the estimated pooled prevalence of insomnia symptoms was 46.4% (95% CI 40.3–52.5%, I2 = 99.5%, Fig. 3). No publication bias was observed based on the funnel plot (Supplementary Fig. 7). Sensitivity analysis confirmed that the stability of the result was not violated after omitting any particular study.
Subgroup analysis by front-line vs. non-front-line healthcare workers was conducted. There were 25 studies with 13,021 front-line healthcare workers and 28 studies with 20,000 non-front-line or non-specified healthcare workers. Random-effects meta-analysis showed that the estimated pooled prevalence of insomnia symptoms was significantly higher in front-line healthcare workers (56.7%, 95% CI 45.9–67.5%, I2 = 99.5%) compared to that in non-front-line/non-specified healthcare workers (38.0%, 95% CI 33.8–42.2%, I2 = 97.6%, between-group p < 0.001, Supplementary Fig. 8).
3.5.3. COVID-19 patients
Among the 6 studies with 1780 COVID-19 patients, prevalence of insomnia symptoms ranged from 10.2% to 84.7% during the COVID-19 pandemic in China. Random-effects meta-analysis showed that the estimated pooled prevalence of insomnia symptoms was 48.7% (95% CI 21.6–75.8%, I2 = 99.5%, Fig. 3). Sensitivity analysis confirmed the stability of the result was not violated after omitting any particular study.
3.5.4. Patients with chronic medical conditions
Among the five studies with 3185 subjects with chronic medical conditions, two studies included patients with breast cancer and the three remaining studies focused on patients with diabetes, Parkinson's disease, and various chronic diseases, respectively. Prevalence of insomnia symptoms among patients with chronic medical conditions ranged from 26.2% to 68.9% during the COVID-19 pandemic in China. Random-effects meta-analysis showed that the estimated pooled prevalence of insomnia symptoms was 49.3% (95% CI 32.5–66.1%, I2 = 98.5%, Fig. 3). Sensitivity analysis confirmed the stability of the result was not violated after omitting any particular study.
3.5.5. Patients with mental disorders
Among the two studies with 320 subjects with mental disorders, the prevalence of insomnia symptoms was 53.9% and 66.0%, respectively. Random-effects meta-analysis showed that the estimated pooled prevalence of insomnia symptoms was 60.9% (95% CI 49.2–72.6%, I2 = 71.4%, Fig. 3).
As shown in Table 1 Model 1, meta-regression suggested that being a healthcare worker (coef. = 0.200, p < 0.001), COVID-19 patient (coef. = 0.223, p = 0.007), patient with a chronic medical condition (coef. = 0.229, p = 0.009) or patient with a mental disorder (coef. = 0.338, p = 0.013) was significantly associated with increased prevalence of insomnia symptoms. In model 2, after controlling for age and gender, healthcare workers (coef. = 0.298, p < 0.001), patients with chronic medical conditions (coef. = 0.295, p = 0.018) and patients with mental disorders (coef. = 0.379, p = 0.006) were significantly associated with increased prevalence of insomnia symptoms. In model 3, after controlling for age, gender, areas of high or low prevalence of COVID-19 cases, anxiety and depressive symptoms, healthcare workers (coef. = 0.202, p = 0.002) and patients with chronic medical conditions (coef. = 0.272, p = 0.045) were significantly associated with increased prevalence of insomnia symptoms.
Table 1.
Meta-regressions for prevalence of insomnia symptoms among specific sub-populations.
| Predictors | Model 1 |
Model 2 |
Model 3 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Coef. | P | 95% CI | Coef. | P | 95% CI | Coef. | P | 95% CI | |
| Population type (ref = general population) | |||||||||
| Healthcare workers | 0.200 | <0.001 | 0.122 to 0.279 | 0.298 | <0.001 | 0.197 to0.400 | 0.202 | 0.002 | 0.079 to 0.325 |
| Patients with COVID-19 | 0.223 | 0.007 | 0.063 to 0.382 | 0.147 | 0.148 | −0.053 to 0.349 | 0.156 | 0.207 | −0.090 to 0.404 |
| Patients with chronic medical conditions | 0.229 | 0.009 | 0.057 to 0.401 | 0.295 | 0.018 | 0.051 to 0.539 | 0.272 | 0.045 | 0.006 to 0.539 |
| Patients with mental disorders | 0.338 | 0.013 | 0.072 to 0.604 | 0.379 | 0.006 | 0.113 to 0.645 | 0.335 | 0.062 | −0.018 to 0.689 |
| Age (years) | – | – | – | 0.004 | 0.106 | −0.001 to 0.010 | 0.004 | 0.271 | −0.003 to 0.012 |
| Gender (male %) | – | – | – | 0.002 | 0.120 | −0.001 to 0.004 | 0.002 | 0.180 | −0.001 to 0.004 |
| Prevalence of anxiety symptoms (%) | – | – | – | – | – | – | 0.000 | 0.836 | −0.001 to 0.001 |
| Prevalence of depressive symptom (%) | – | – | – | – | – | – | 0.000 | 0.825 | −0.001 to 0.001 |
| Study areas (Hubei Province vs. non-Hubei Provinces or mixed sample) | 0.047 | 0.429 | −0.072 to 0.167 | ||||||
Because some covariates were not provided in some original articles, Model 1, model 2, and model 3 included 98, 77, 47 studies, respectively.
Characters in bold indicate p < 0.05.
4. Discussion
This systematic review and meta-analysis included 98 studies from 81 articles, with a total of 193,889 participants, and examined the prevalence of insomnia symptoms during early and late stages of the COVID-19 pandemic, as well as insomnia symptoms in different populations during the COVID-19 in China. The main findings of our study indicate that the prevalence of insomnia symptoms among all populations is rather high, raising up to 39.1%, and the pooled prevalence of insomnia symptoms does not differ between the early (37.0%) and late (41.8%) stages of the COVID-19 pandemic in China suggesting that this sleep complaint sustains high in the mid-term. Furthermore, our meta-regression analysis suggests that healthcare workers, COVID-19 patients, patients with chronic medical conditions and patients with mental disorders are more likely to have insomnia symptoms compared to the general population during the COVID-19 pandemic in China. This association remains significant in healthcare workers and patients with chronic medical conditions after adjusting for age, gender, areas of high or low prevalence of COVID-19 cases, anxiety and depressive symptoms.
In the current meta-analysis, the prevalence of insomnia symptoms among all populations is 39.1%. Our finding appears to be slightly higher compared to the prevalence of 35.7% reported in a recent meta-analysis for the pooled prevalence of insomnia symptoms in adults from 13 countries [10]. In this previous meta-analysis, subgroup analysis by country determined that the pooled prevalences of insomnia symptoms in China, Italy, France and Germany were 26.5%, 55%, 50.8% and 38.8%, respectively. The higher prevalence of insomnia symptoms in our study could be attributed to the methodological differences that we included more studies on healthcare workers (48.9% vs. 33.0%) that are known to present higher prevalence of insomnia symptoms compared to the general population due to increased workload and higher risk of being infected with COVID-19 [[11], [12], [13]].
Interestingly, we did not observe a significant difference in pooled prevalence of insomnia symptoms between the early and late stages, though the COVID-19 spread has been controlled in China and the daily life has returned to a relatively normal situation. These findings suggest that the effects of COVID-19 on insomnia symptoms may persist, suggesting long-term follow-up and interventions for sleep are needed. However, since the COVID-19 pandemic is still continuing in many other countries, our findings may not be generalized to these countries. Further prolongation of the COVID-19 pandemic may further worsen insomnia and insomnia-related psychological and medical issues. Thus, long-term follow-up for sleep disturbance is warranted.
Risk factors for insomnia symptoms during the early and late stages of the COVID-19 pandemic may differ. During the early stage, insomnia symptoms have been reported to be mainly associated with acute psychological reactions due to the rapid spread of the disease (ie, fear of getting SARS-CoV-2 infected) and the strict implementations for controlling the COVID-19 pandemic (ie, quarantine, social distancing, lockdown, school and factory shut-down, limited access to hospitals, and traffic restrictions) [14,15], as well as poor sleep hygiene [5,16]. During the late stage of the COVID-19 pandemic, insomnia symptoms are associated with long-term effects of the COVID-19 pandemic on economic stress [17,18] and mental health problems [[19], [20], [21]]. Before the COVID-19 pandemic, the prevalence of insomnia symptoms in China was 15% in the adult general population [22] and 35.9% among older adults [23]. In the current meta-analysis, prevalence of insomnia symptoms among the general population was 26.0%, which is higher than the prevalence in the adult general population [22] but lower than for older adults [23] before the COVID-19 pandemic in China. A recent meta-analysis [10] showed that, similar to our study, the pooled prevalence of sleep problems in China during the COVID-19 pandemic was 26.5%. In a previous study conducted by our group during the COVID-19 outbreak in China, we found that worsened insomnia during COVID-19 outbreak was significantly associated with stress, anxiety and depressive symptoms and prolonged time in bed [5]. It appears that psychological symptoms and insomnia symptoms may have a bidirectional relationship during the COVID-19 pandemic, suggesting that sleep specialists should consider psychiatric comorbidities and sleep hygiene education when treating sleep problems and vice versa. Compared to a recent meta-analysis evaluating the prevalence of insomnia symptoms during the COVID-19 from 13 countries [10], the pooled prevalence of insomnia symptoms was lower in our study (26% vs. 32%). Our findings of lower prevalence of insomnia symptoms in the general population in China during the COVID-19 pandemic is consistent with the subgroup analysis by country in this meta-analysis [10]. In this meta-analysis, the authors reported that the estimated pooled prevalence of insomnia symptoms in China is lower than in Italy, France and Germany [10].
Our findings show a very high – almost double compares to the general population-pooled prevalence of insomnia symptoms in healthcare workers that increased during the pandemic compares to the pre-pandemic period [24]. This may be due to increased COVID-19-related stress and workload during the pandemic. Importantly, the association remains significant even after adjusting for age, gender, areas of high or low prevalence of COVID-19 cases, anxiety and depressive symptoms, suggesting that insomnia symptoms may be independent of psychological symptoms. Other factors, ie, shift work, poor sleep environment and high-intensity work, may play a more important role in insomnia in healthcare workers during the COVID-19 pandemic. As expected, front-line healthcare workers had a higher prevalence of insomnia symptoms compared to non-front-line healthcare workers. This finding may be associated with direct contact with COVID-19 patients [[25], [26], [27]]. Thus, front-line healthcare workers may have a higher risk of being infected by COVID-19, more intensive work [28], isolation from their families [11,29] and higher levels of COVID-19-related stress, anxiety, depression [[30], [31], [32]]. In contrast to our study, two recent meta-analyses reported slightly lower prevalence of insomnia symptoms among healthcare workers [10,33]. The reasons for the discrepancy are not clear. Since insomnia symptoms are risk factors for the development of anxiety and depression, our findings emphasize the importance of intervening insomnia symptoms before it evolves into more complex and enduring psychological responses.
We also show that COVID-19 patients have higher prevalence of insomnia symptoms compare to the general population (48.7% vs. 26.0%). In meta-regression analyses, after adjusting for age, gender, areas of high or low prevalence of COVID-19 cases, anxiety and depressive symptoms, this association disappear, suggesting it may be moderated by these covariates. The higher prevalence of insomnia symptoms in COVID-19 patients could be directly associated with the symptoms of COVID-19 per se, such as cough, fever, difficulty in breathing and physical pain, all of which have been reported to be associated with disturbed sleep [34,35], the psychological effect of the disease or hospitalization, ie due to fears related to adverse outcomes of the infection, isolation in a ward, lack of stimulation of the 24-h circadian rhythm in the ward, extremely prolonged time in bed, and a poor sleep environment in the hospital. Finally it may relate to side effects of medications administered for the treatment of COVID-19, such as steroid medication, may also affect sleep. We found 48.7% of COVID-19 patients had insomnia symptoms, which is lower than the previous meta-analysis showing that of 75% COVID-19 patients had insomnia symptoms [10]. This difference may be due to methodological issues, such as smaller sample size, and different origin of the populations included, ie China vs. Europe. The latter may be related to different way of hospitalization payment, ie Public vs. individual and pressure to the health care system etc.
The pooled prevalence of insomnia symptoms in patients with chronic medical conditions during COVID-19 pandemic in China is 49.3%, which is within the range of 35.4%–88.1% reported in other countries [[36], [37], [38]]. This finding remains higher compare to the general population, even after controlling for age, gender, areas of high and low prevalence of COVID-19 cases, anxiety and depressive symptoms, and may be multifactorial. First, as previously demonstrated that the prevalence of insomnia symptoms is higher in patients with chronic medical conditions compared to healthy controls [[39], [40], [41]], independently of the pandemic. This may be related to the underlying symptoms of the disease per se, such as pain. Other factors may be restricted access to health care system due to increased medical care need [[44], [45], [46]], home quarantine, travel restrictions and fear of getting infected [48,49] associated with stress, anxiety and depression [36,[42], [43], [44], [45], [46], [47]]. More attention should be paid to such populations and effective measures such as modifications to standard treatment paradigms, establishing special clinics (ie, special clinics to care for central venous catheter patients weekly), and telemedicine are needed.
The pooled prevalence of insomnia symptoms in patients with mental disorders during COVID-19 pandemic in China is 60.9%, which is the highest among different populations. In a nationwide survey which was conducted during the acute phase of COVID-19 pandemic in China, we found that mental health disorder is a risk factor for developing worsened insomnia symptoms [5], which is consistent with the current study. In this current study, after controlling for areas of high and low prevalence of COVID-19 cases, anxiety and depression status, the association between mental disorders and insomnia symptoms becomes weaker and marginally significant, suggesting that insomnia symptoms in patients with mental disorders may be moderated by concerns to the high COVID-19 epidemic. The reasons for higher prevalence of insomnia symptoms among patients with mental disorders may be associated with increased vulnerability to stress among patients with mental disorders [[48], [49], [50], [51]], resulting in relapses or deterioration of an already existing mental issue. For example, in a nationwide survey which was conducted during the acute phase of the COVID-19 pandemic, we found that adults with mental disorders had higher odds for developing COVID-19 stress, worsened anxiety, and depressive and insomnia symptoms compared to individuals without mental disorders [21]. Furthermore, nationwide travel restrictions and quarantine during the acute phase of COVID-19 pandemic resulted in suspended hospital visits, which prevented patients with mental disorders from attending regular outpatient visits for evaluations and medication prescriptions. Based on a psychiatric and neurological outpatient-based survey during the acute phase of the COVID-19 pandemic in China, 22.0% of patients diagnosed with mental disorders could not receive routine psychiatric care because of the suspended hospital visits [52]. Cessation or irregular administration of medication could be another major reason for deterioration of emotional status and insomnia in mentally ill patients. Since this group of patients is often neglected following a disaster, our findings suggest that more attention, including timely psychological intervention and telemedicine, needs to be provided as soon as possible.
Subgroup analyses show that older adults have a higher prevalence of insomnia symptoms during the COVID-19 pandemic in China, which is consistent with previous studies [[53], [54], [55], [56]]. However, all of the studies in this subgroup are either healthcare workers or patients with chronic medical conditions, and the association between age and prevalence of insomnia symptoms after adjusting for different specific populations and gender is non-significant in meta-regression models, suggesting that the finding could be explained by the predisposition of insomnia in healthcare workers and patients with chronic medical conditions. Furthermore, subgroup analyses suggest that pooled prevalence of insomnia symptoms is higher in Hubei Province compared to other regions of China, which is consistent with previous studies reporting more frequent adverse psychological reactions and higher prevalence of insomnia symptoms in areas with a higher prevalence of COVID-19 cases [16,[57], [58], [59]].
4.1. Clinical implications and future research directions
The high prevalence and similar levels of insomnia symptoms during the early and late stages of COVID-19 pandemic suggest that sleep intervention services focusing on sleep improvement, such as sleep hygiene, cognitive behavior therapy, mindfulness-based therapy, and medications need to be considered. Furthermore, since insomnia symptoms persist after the acute phase of the pandemic and may persist for a relative long period, long-term sleep follow-up and intervention services should also be considered. Findings of the current study identify a range of directions for future research. First, longitudinal studies need to be conducted to better understand the short and long-term effects of COVID-19 on sleep in different populations. Second, COVID-19 effects on objective sleep need to be examined. Finally, since insomnia symptoms are risk factors for mental disorders [60,61] and cardiometabolic diseases [62], longitudinal studies should also examine the long-term effects of COVID-19-related insomnia symptoms on mental health problems (ie, post-traumatic stress disorder, obsessive compulsive disorder, depression and anxiety disorders) and cardiometabolic diseases.
4.2. Strengths and limitations
Our systematic review and meta-analysis has the following strengths: 1) it includes 98 studies from 81 articles with 193,889 participants; 2) careful selection of included studies that used standardized questionnaires/scales to assess insomnia symptoms; 3) is the first study to compare the prevalence of insomnia symptoms during the early and late stages of COVID-19 pandemic, and 4) is the first meta-analysis to include anxiety and depression as covariates in meta-regression analyses to examine the independent association of different populations with insomnia symptoms during the COVID-19 pandemic. However, some limitations should be acknowledged. First, the heterogeneity is high. However, findings of sensitivity analysis suggest our results are stable. Differences in the prevalence of insomnia symptoms in different populations may explain the high heterogeneity. Another possible explanation for the high heterogeneity may be associated with different sleep measures for assessing insomnia symptoms across different time frames (eg, PSQI and AIS assess symptoms during the past month, while the ISI assesses symptoms during the past 2 weeks). However, it has been reported that there is no significant difference regarding the sensitivity and specificity of the diagnostic accuracy among the PSQI, ISI and AIS for screening insomnia [63]. Second, the number of studies that were conducted during the late stage of COVID-19 pandemic in China is relatively small, which prevents further analyses of the prevalence of insomnia symptoms in different specific sub-populations during the late stage of the COVID-19 pandemic.
5. Conclusions
Over one third of our sample present insomnia symptoms during the early stage of COVID-19 pandemic in China. Interestingly, prevalence of insomnia symptoms sustains high during the late stage of the pandemic despite the control of the disease and the amelioration of its adverse effects. Our findings suggest that insomnia symptoms related to COVID-19 appear to persist of over time. Healthcare workers, patients with COVID-19, patients with chronic medical conditions and patients with mental disorders have higher prevalence of insomnia symptoms compare to the general population. Future studies may examine the long-term effects of COVID-19 on sleep and its adverse effects on health in different populations.
Credit author statement
Yun Li contributed to the ideas of this study, data interpretation and revised the manuscript; Baixin Chen contributed in variables extraction, statistical analyses, data interpretation and the first draft of this manuscript; Zhuoting Hong contributed to search articles, assess articles and crate tables and figures; Qimeng Sun contributed in articles assessment, interpret data and first draft of this manuscript; Yanyuan Dai contributed in variables extraction, interpreting data and first draft of this study; Maria Basta contributed in interpreting data and revising the manuscript; Xiangdong Tang contributed in interpreting data; Qingsong Qin contributed in interpreting data and revising the manuscript.
Funding/support
This study was supported by National Natural Science Foundation of China (No.81970087), Special funding for Science and Technology of Guangdong Province in 2020 (SKJZX202001) and 2020 Li Ka Shing Foundation Cross-Disciplinary Research Grant (2020LKSFG05B).
Role of the sponsors
The supporters had no role in the design, analysis, interpretation, or publication of this study.
Previous presentation
None.
Acknowledgments
The authors thank Prof. Stanley Lin, a native English-speaking scientist proof-read this manuscript before submission.
Footnotes
All authors have seen and approved the manuscript.
Yun Li, Baixin Chen, Zhuoting Hong, Qimeng Sun, Yanyuan Dai, Maria Basta, Xiangdong Tang and Qingsong Qin have no conflicts of interest to disclose.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.09.014.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleep.2021.09.014.
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Distribution of COVID-19 outbreaks. http://2019ncov.chinacdc.cn/2019-nCoV/ [Internet]. [cited 2021 Feb 1]. Available from:
- 2.Statement on the second meeting of the international health regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) 2020. https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [Internet] [cited 2021 Feb 1]. Available from: [Google Scholar]
- 3.Full Text: Fighting COVID-19: China in Action. http://www.chinatoday.com.cn/ctenglish/2018/zdtj/202006/t20200608_800209101.html [Internet]. [cited 2021 Feb 1]. Available from:
- 4.All temporary treament centers were closed. http://www.gov.cn/xinwen/2020-03/11/content_5489757.htm [Internet]. [cited 2021 Feb 1]. Available from:
- 5.Li Y., Qin Q., Sun Q., et al. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med [Internet] 2020;16(8):1417–1418. doi: 10.5664/jcsm.8524. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamioka H. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Jpn Pharmacol Ther. 2019;47(8):1177–1185. [Google Scholar]
- 7.Rostom A., Dube C., Cranney A., et al. Agency for Healthcare Research and Quality (US); Rockville (MD): 2004 Sep. Celiac disease.http://www.ncbi.nlm.nih.gov/books/NBK35156, oks/NBK35156 (Evidence Reports/Technology Assessments, No. 104.) Appendix D. Quality Assessment Forms. [Internet]. [cited 2021 Feb 1]. Available from: [Google Scholar]
- 8.Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for systematic reviews of interventions. 2nd ed. Chichester (UK): John Wiley & Sons.
- 9.Cochrane Collaboration, Cochrane Handbook for systematic reviews of interventions. https://training.cochrane.org/handbook/archive/v5.1/ [Internet]. [cited 2021 Feb 1]. Available from:
- 10.Jahrami H., BaHammam A.S., Bragazzi N.L., et al. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang W., Song W., Xia Z., et al. Sleep disturbance and psychological profiles of medical staff and non-medical staff during the early outbreak of COVID-19 in Hubei province, China. Front Psychiatr. 2020;11(July):1–8. doi: 10.3389/fpsyt.2020.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang L.-Q., Zhang M., Liu G.-M., et al. Psychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: a multicenter study. J Psychiatr Res. 2020;129:198–205. doi: 10.1016/j.jpsychires.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang W.R., Wang K., Yin L., et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China - PubMed. Psychother Psychosom [Internet] 2020 Dec 7;89(4):242–250. doi: 10.1159/000507639. https://pubmed.ncbi.nlm.nih.gov/32272480/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burtscher J., Burtscher M., Millet G.P. (Indoor) isolation, stress and physical inactivity: vicious circles accelerated by Covid-19? Scand J Med Sci Sports [Internet] 2020;30(8):1544–1545. doi: 10.1111/sms.13706. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiao C. A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: structured letter therapy. Psychiatry Investig [Internet] 2020;17(2):175–176. doi: 10.30773/pi.2020.0047. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qimeng S., Qingsong Q., Baixin C., et al. Stress, anxiety, depression and insomnia in adults outside Hubei province during the COVID-19 pandemic. Natl Med J China (Peking) 2020;100(43):3419–3424. doi: 10.3760/cma.j.cn112137-20200302-00557. [DOI] [PubMed] [Google Scholar]
- 17.Li X., Lu P., Hu L., et al. Factors associated with mental health results among workers with income losses exposed to COVID-19 in China. Int J Environ Res Publ Health. 2020;17(15):5627. doi: 10.3390/ijerph17155627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Song L., Wang Y., Li Z., et al. Mental health and work attitudes among people resuming work during the COVID-19 pandemic: a cross-sectional study in China. Int J Environ Res Publ Health. 2020;17(14):5059. doi: 10.3390/ijerph17145059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang B.X., Xia L., Huang R., et al. Relationship between eHealth literacy and psychological status during COVID-19 pandemic: a survey of Chinese residents. J Nurs Manag. 2021 May;29(4):805–812. doi: 10.1111/jonm.13221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu B.Y.-M., Yeung W.-F., Lam J.C.-S., et al. Prevalence of sleep disturbances during COVID-19 outbreak in an urban Chinese population: a cross-sectional study. Sleep Med. 2020;74(January):18–24. doi: 10.1016/j.sleep.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun Q., Qin Q., Basta M., et al. Psychological reactions and insomnia in adults with mental health disorders during the COVID-19 outbreak. BMC Psychiatr. 2021;21(1):19. doi: 10.1186/s12888-020-03036-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cao X.L., Wang S Bin, Zhong B.L., et al. The prevalence of insomnia in the general population in China: a meta-analysis. PloS One. 2017;12(2):1–11. doi: 10.1371/journal.pone.0170772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu L., Wang S Bin, Rao W., et al. The prevalence of sleep disturbances and sleep quality in older Chinese adults: a comprehensive meta-analysis. Behav Sleep Med. 2019;17(6):683–697. doi: 10.1080/15402002.2018.1469492. [DOI] [PubMed] [Google Scholar]
- 24.Qiu D., Yu Y., Li R.Q., et al. Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Med. 2020;67:258–266. doi: 10.1016/j.sleep.2019.01.047. [DOI] [PubMed] [Google Scholar]
- 25.Cai Q., Feng H., Huang J., et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J Affect Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cai Z., Cui Q., Liu Z., et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. 2020;131:132–137. doi: 10.1016/j.jpsychires.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lai J., Ma S., Wang Y., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou Y., Wang W., Sun Y., et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in China under the COVID-19 epidemic: workload should be concerned. J Affect Disord. 2020;277:510–514. doi: 10.1016/j.jad.2020.08.059. January. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feng Z., Xu L., Cheng P., et al. The psychological impact of COVID-19 on the families of first-line rescuers. Indian J Psychiatr. 2020;62(Suppl 3):S438–S444. doi: 10.4103/psychiatry.IndianJPsychiatry_1057_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng F.-F., Zhan S.-H., Xie A.-W., et al. Anxiety in Chinese pediatric medical staff during the outbreak of Coronavirus Disease 2019: a cross-sectional study. Transl Pediatr. 2020;9(3):231–236. doi: 10.21037/tp.2020.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang L., Lei W., Liu H., et al. Nurses' sleep quality of “Fangcang” hospital in China during the COVID-19 pandemic. Int J Ment Health Addiction. 2020 Oct 26:1–11 doi: 10.1007/s11469-020-00404-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tu Z.-H., He J.-W., Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine (Baltim) 2020;99(26) doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pappa S., Ntella V., Giannakas T., et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun [Internet] 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu Y., Chen Y., Zheng Y., et al. Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behav Immun [Internet] 2020;89:587–593. doi: 10.1016/j.bbi.2020.07.016. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang H., Qin S., Zhang L., et al. A psychological investigation of coronavirus disease 2019 (COVID-19) patients in mobile cabin hospitals in Wuhan. Ann Transl Med. 2020;8(15):941. doi: 10.21037/atm-20-4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.HØrmann Thomsen T., Wallerstedt S.M., Winge K., et al. Life with Parkinson's disease during the COVID-19 pandemic: the pressure is “OFF. J Parkinsons Dis. 2021:1–5. doi: 10.3233/JPD-202342. [DOI] [PubMed] [Google Scholar]
- 37.Kumar N., Gupta R., Kumar H., et al. Impact of home confinement during COVID-19 pandemic on sleep parameters in Parkinson's disease. Sleep Med [Internet. 2021;77:15–22. doi: 10.1016/j.sleep.2020.11.021. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Massicotte V., Ivers H., Savard J. COVID-19 pandemic stressors and psychological symptoms in breast cancer patients. Curr Oncol. 2021;28(1):294–300. doi: 10.3390/curroncol28010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stefani A., Högl B. Sleep in Parkinson's disease. Neuropsychopharmacology. 2020;45(1):121–128. doi: 10.1038/s41386-019-0448-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ogilvie R.P., Patel S.R. The epidemiology of sleep and diabetes. Curr Diabetes Rep. 2018;18(10):82. doi: 10.1007/s11892-018-1055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Medysky M.E., Temesi J., Culos-Reed S.N., et al. Exercise, sleep and cancer-related fatigue: are they related? Neurophysiol Clin [Internet] 2017;47(2):111–122. doi: 10.1016/j.neucli.2017.03.001. Available from: [DOI] [PubMed] [Google Scholar]
- 42.Juanjuan L., Santa-Maria C.A., Hongfang F., et al. Patient-reported outcomes of patients with breast cancer during the COVID-19 outbreak in the epicenter of China: a cross-sectional survey study. Clin Breast Canc. 2020;20(5):e651–e662. doi: 10.1016/j.clbc.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cui Q., Cai Z., Li J., et al. The psychological pressures of breast cancer patients during the COVID-19 outbreak in China — a comparison with frontline female nurses. Front Psychiatr. 2020;11:559701. doi: 10.3389/fpsyt.2020.559701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xia Y., Kou L., Zhang G., et al. Investigation on sleep and mental health of patients with Parkinson's disease during the Coronavirus disease 2019 pandemic. Sleep Med. 2020;75:428–433. doi: 10.1016/j.sleep.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sun Xiaoxu, Shi Fanghong, Ma jing, et al. Study on glycemic profiles and emotional scales in diabetic patients after the outbreak of COVID-19. Chin J Endocrinol Metab. 2020;36(8):673–677. [Google Scholar]
- 46.Yu J., Ouyang W., Chua M.L.K., et al. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in wuhan, China. JAMA Oncol. 2020;6(7):1108–1110. doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liang W., Guan W., Chen R., et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Phillips L.J., Francey S.M., Edwards J., et al. Strategies used by psychotic individuals to cope with life stress and symptoms of illness: a systematic review. Hist Philos Logic. 2009;22(4):371–410. doi: 10.1080/10615800902811065. [DOI] [PubMed] [Google Scholar]
- 49.Berry K., Barrowclough C., Byrne J., et al. Coping strategies and social support in old age psychosis. Soc Psychiatry Psychiatr Epidemiol [Internet] 2006;41(4):280–284. doi: 10.1007/s00127-005-0023-1. Available from: [DOI] [PubMed] [Google Scholar]
- 50.Phillips L.J., Francey S.M., Edwards J., et al. Stress and psychosis: towards the development of new models of investigation. Clin Psychol Rev [Internet] 2007;27(3):307–317. doi: 10.1016/j.cpr.2006.10.003. Available from: [DOI] [PubMed] [Google Scholar]
- 51.Hao F., Tan W., Jiang L., et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou J., Liu L., Xue P., et al. Mental health response to the COVID-19 outbreak in China. Am J Psychiatry [Internet] 2020;177(7):574–575. doi: 10.1176/appi.ajp.2020.20030304. Available from: [DOI] [PubMed] [Google Scholar]
- 53.Wang Y., Zhu L.-Y., Ma Y.-F., et al. Association of insomnia disorder with sociodemographic factors and poor mental health in COVID-19 inpatients in China. Sleep Med. 2020;75:282–286. doi: 10.1016/j.sleep.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jiang Z., Zhu P., Wang L., et al. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. J Psychiatr Res. 2021 Apr;136:595–602. doi: 10.1016/j.jpsychires.2020.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhou Y., Yang Y., Shi T., et al. Prevalence and demographic correlates of poor sleep quality among frontline health professionals in liaoning province, China during the COVID-19 outbreak. Front psychiatry. 2020;11:520. doi: 10.3389/fpsyt.2020.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jing W., Gong Y., Chen Z., et al. Sleep disturbances among Chinese residents during the Coronavirus Disease 2019 outbreak and associated factors. Sleep Med. 2020;74(January):199–203. doi: 10.1016/j.sleep.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cullen W., Gulati G., Kelly B.D. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Heal Artic [Internet] 2020;17(5):1729. doi: 10.1093/qjmed/hcaa110. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhu Z., Liu Q., Jiang X., et al. The psychological status of people affected by the COVID-19 outbreak in China. J Psychiatr Res [Internet. 2020;129 doi: 10.1016/j.jpsychires.2020.05.026. April):1–7. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guo J., Feng X.L., Wang X.H., et al. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int J Environ Res Publ Health. 2020;17(11):3857. doi: 10.3390/ijerph17113857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ford D.E., Kamerow D.B. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? J Am Med Assoc. 1989;262(11):1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 61.Bernert R.A., Kim J.S., Iwata N.G., et al. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatr Rep. 2015;17(3):554. doi: 10.1007/s11920-015-0554-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cappuccio F.P., Miller M.A. Sleep and cardio-metabolic disease. Curr Cardiol Rep. 2017;19(11):110. doi: 10.1007/s11886-017-0916-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chiu H.Y., Chang L.Y., Hsieh Y.J., et al. A meta-analysis of diagnostic accuracy of three screening tools for insomnia. J Psychosom Res [Internet. 2016;87:85–92. doi: 10.1016/j.jpsychores.2016.06.010. Available from: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1