Abstract
Ankylosis of the temporomandibular joint (TMJ) is a disabling disease resulting from fibrous or bony fusion of the mandibular condyle and the glenoid fossa. Early diagnosis and surgical treatment are essential to prevent facial deformity and other complications. Conventional radiography has limitations in demonstrating the true extent of ankylosis. It is important for surgeons to be aware of the size and degree of bony ankylosis in order to perform complete resection of the ankylotic mass. In addition, a detailed evaluation of the relationship with adjacent vital structures such as the internal maxillary artery, inferior alveolar nerve canal, external auditory canal, and skull base are crucial to avoid iatrogenic injury. Multidetector computed tomography (MDCT) is the current imaging modality of choice for preoperative assessments. Herein, the authors propose a structured CT reporting template for TMJ ankylosis to strengthen the value of the preoperative imaging report and to reduce the rates of intraoperative complications and recurrence.
Keywords: Temporomandibular Joint, Multidetector Computed Tomography, Ankylosis, Wounds and Injuries
Introduction
The term “ankylosis” refers to a stiff joint, and temporomandibular joint (TMJ) ankylosis involves fusion between the mandibular condyle and glenoid fossa. It can be fibrous, fibro-osseous, or osseous in nature, with changes occurring sequentially.1 TMJ ankylosis often occurs secondary to trauma (73.2%), systemic or local infections (17%), and unknown causes(7.3%).2 In systemic diseases, such as ankylosing spondylitis, the TMJ is involved in approximately 3–20% of cases, but cases of TMJ ankylosis (2–4%) in ankylosing spondylitis are reported sporadically.3 Infection is the commonest cause in the pediatric age group, whereas post-traumatic ankylosis predominates in adults.4 The clinical features of TMJ ankylosis vary depending on the age of onset, and facial deformities are frequently seen in children. This condition often presents as difficulty in speech, mouth opening, and mastication. Imaging plays a pivotal role in diagnosing TMJ ankylosis and in planning surgery. Conventional radiography was the mainstay of diagnostic imaging before the advent of computed tomography.5 The limitations of conventional radiography include poor spatial resolution, inadequate assessment of the extent of the ankylotic mass, and the need for multiple views of the joint leading to more radiation exposure to the patient.6 MDCT is the current imaging modality of choice for an accurate preoperative demonstration of the ankylotic mass and other surgically important findings.5,7 However, surgically relevant findings on preoperative CT imaging are often inconsistently documented in the radiology report, which may result in intraoperative complications or inadequate resection.
The TMJ is a hinge synovial joint formed between the mandibular condyle, glenoid fossa, and articular eminence (Fig. 1A). Medially, the TMJ is related to the skull base and numerous foramina transmitting vital neurovascular structures. In particular, the foramen ovale and foramen spinosum lie medially to the TMJ and transmit the mandibular nerve and middle meningeal artery, respectively (Fig. 1B). Posterosuperiorly, the mastoid part of the temporal bone is related to the TMJ (Fig. 2A). Other surgically important neurovascular bundles related to the TMJ include the inferior alveolar neurovascular bundle, which lies inferiorly to the TMJ, and the maxillary artery, which is located medially to the TMJ (Figs. 2B-D). The most widely accepted hypothesis for the pathogenesis of TMJ ankylosis is that a fracture leads to activation of molecular pathways (e.g., tumor growth factor) and bone morphogenic proteins, which subsequently activate osteoblasts. Sequentially, fibrosis and ossification of intraarticular hematoma ensue, leading to the formation of an ankylotic mass.8,9
Fig. 1. Anatomy and relationships of the temporomandibular joint (TMJ). A. A sagittal computed tomographic (CT) image of the TMJ shows the mandibular condyle and articular fossa. B. An axial CT image of the skull base shows the foramen ovale and spinosum lying medial to the TMJ and carotid canal and jugular foramen posteromedially. GF: glenoid fossa, FO: foramen ovale, FS: foramen spinosum, CH: condylar head, CC: carotid canal, JF: jugular foramen.
Fig. 2. Temporomandibular joint relationships. A. Coronal computed tomographic (CT) image shows the mastoid part of the temporal bone lying posterosuperiorly. B. Coronal CT image shows the mandibular foramen (MF), which continues as the inferior alveolar nerve canal (IAC) lying inferiorly. Sagittal reformatted CT (C) and panoramic (D) images show the course of the IAC.
This pictorial review highlights the surgically relevant anatomical relationships of the TMJ, the pathogenesis of TMJ ankylosis, and a proposed structured CT reporting template of TMJ ankylosis.
Case Findings and Structured Reporting Format
The MDCT imaging technique involved supine positioning of the patient on the CT table. The patient was instructed not to swallow or move while scanning the area between the inferior orbital margin and tip of chin with a closed mouth. The image acquisition protocol at our institution included a peak kilovoltage of 120 kVp, current of 75–80 mA, 1-mm collimation, and 1-mm pitch. Sections measuring 3 mm in thickness were acquired and reconstructed into 1-mm-thick sections in the soft tissue window (H30s kernel) and in the bone window (H60s kernel). CT angiography was performed when appropriate to assess the relationship of the internal maxillary artery (IMA) with the ankylotic mass. Multiplanar reconstructions were performed in the coronal oblique plane (parallel to the long axis of the mandibular condyle) and sagittal oblique plane (perpendicular to the long axis of the mandibular condyle). Various measurements were made on thick multiplanar (MPR), maximum intensity projection (MIP), volume rendering technique (VRT), and panoramic reconstruction images.
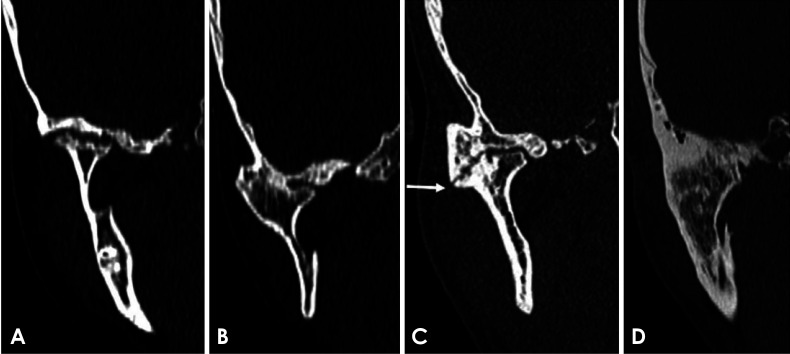
The imaging appearance of TMJ ankylosis on CT has been variably described depending on age and the duration of the injury. Xia et al.10 proposed a classification of TMJ ankylosis corresponding to the stages of TMJ ankylosis on CT, as follows: stage 1, in which the glenoid fossa and condyle are clearly seen with no bony ankylosis and scattered callus can be seen (Fig. 3A); stage 2, in which lateral bony ankylosis of the joint is seen and the condyle is displaced medially, forming pseudoarthrosis with the glenoid fossa (Fig. 3B); stage 3, in which there is complete bony ankylosis with no recognizable condyle and fossa and a radiolucent zone is seen in the fused area (Fig. 3C); and stage 4, which has extensive bony ankylosis with loss of the radiolucent zone (Fig. 3D).
Fig. 3. Stages of temporomandibular joint ankylosis on computed tomographic images. A. Stage 1: glenoid fossa and condyles are visible with no bony ankylosis. B. Stage 2: lateral bony ankylosis of the joint is seen. C. Stage 3: complete bony ankylosis of the joint with a radiolucent line inside (arrow). D. Stage 4: extensive bony ankylosis with no visible radiolucent line.
An ankylotic mass is an abnormal chunk of bone bridging the glenoid fossa and mandibular condyle that may variably extend to involve the zygomatic arch, ramus or other parts of the mandible, and skull base.11 In addition to the ankylotic mass, TMJ ankylosis results in bony and structural changes such as distorted mandibular structures (micrognathia/retrognathia) along with reduced ramus height, a deepened antegonial notch, and an elongated coronoid process.12
The preoperative imaging of TMJ ankylosis consists of evaluating the ankylotic mass, its relationship to vital structures, and the bony changes secondary to ankylosis. Surgical procedures for TMJ ankylosis have been previously described in various studies.13,14,15 The proposed structured reporting format includes all the surgically relevant components(Table 1) based on the authors' previous experiences. The individual subheadings are discussed below. The type of ankylotic mass(fibrous or bony) was assessed and staging of ankylosis was done as described above.
Table 1. Temporomandibular joint ankylosis reporting template.
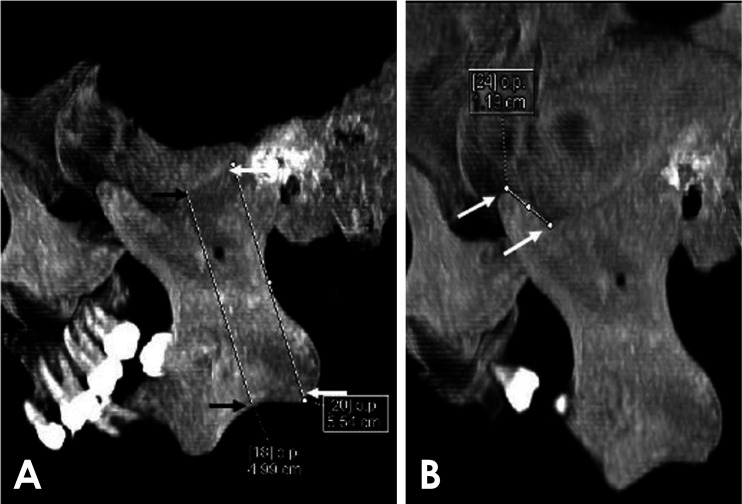
Measurements of the ankylotic mass were made in the anteroposterior, mediolateral, and superoinferior dimensions, which helped in assessing the complete removal of the ankylotic mass and in estimating the amount of autogenous and alloplastic material required for interpositional gap arthroplasty.7 The mediolateral dimension was measured on an axial section, and the maximum dimension of the ankylotic mass was measured (Fig. 4A). The superoinferior dimension was best evaluated in the coronal plane (Fig. 4B). The anteroposterior dimension was measured in the sagittal plane (Fig. 4C).
Fig. 4. Measurement of ankylotic mass dimensions. A. The mediolateral dimension is measured in the axial plane (arrows). B. The superoinferior dimension is measured in the coronal plane (arrows). C. The anteroposterior dimension is measured in the sagittal plane (arrows). Maximum intensity projection images are used to delineate the margins.
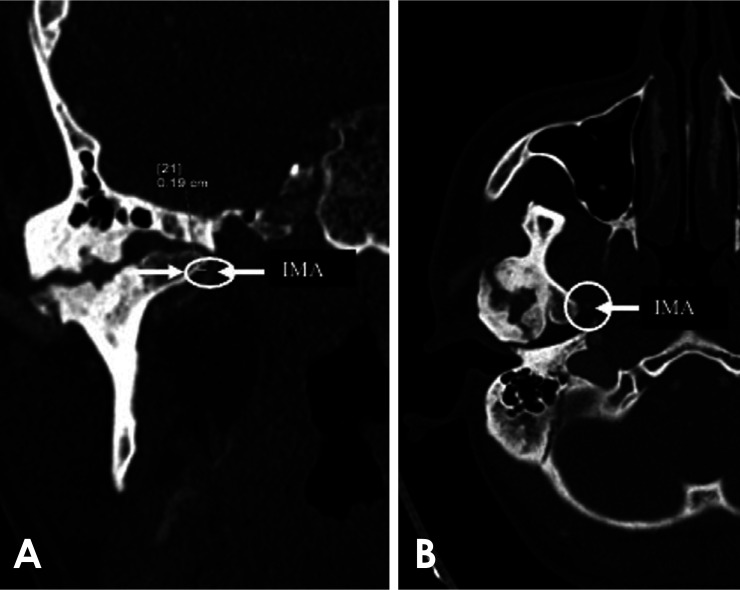
The distance of the IMA from the ankylotic mass is surgically relevant. The IMA is the terminal branch of external carotid artery, and courses between the ramus of the mandible and sphenomandibular ligament and reaches the pterygopalatine fossa, coursing either superficial or deep to the lateral pterygoid muscle. Along its course between the ramus and sphenomandibular ligament, it lies in a close relationship to the ankylotic mass and can be injured intraoperatively, leading to torrential bleeding. Hence, CT angiography was necessary to assess the distance of IMA from the ankylotic mass to avoid intraoperative injury; this measurement was made in the coronal plane (Fig. 5).
Fig. 5. Relationship of an ankylotic mass to the surrounding vital structures. A. Computed tomographic (CT) angiography shows a measurement of the distance of the ankylotic mass (arrow) from the internal maxillary artery (arrow). B. An axial CT image shows that the ankylotic mass is abutting the internal maxillary artery (arrow).
The distance of the inferior alveolar nerve canal (IAC) from the base of ankylotic mass was measured. The IAC begins from the mandibular foramen, located in the ramus of the mandible below the sigmoid notch on the medial aspect. The inferior alveolar nerve, artery, and vein traverse through it and exit at the mental foramen. The basic tenet of osteoarthrectomy is to create a 1.5- to 2-cm bony gap for the treatment of TMJ ankylosis. This frequently meant that plating the osteotomy near the lingula, where the inferior alveolar nerve enters the mandible, would cause intraoperative bleeding and sensory damage to the inferior alveolar nerve. This was mostly seen in cases with a very short ramus of the mandible. It is advisable for the surgeon to have prior information about the distance of the lingula for inferior osteotomy. IAC can be damaged intraoperatively when an ankylotic mass adjoins the IAC, leading to neurovascular injury. Distance from the inferior margin of the ankylotic mass to the IAC was best evaluated in the coronal plane (Fig. 6).
Fig. 6. Relationship of ankylotic masses to the mandibular foramen and inferior alveolar nerve canal. The distance of the ankylotic mass from the inferior alveolar nerve canal is measured in the coronal plane. A. A case of early fibrous ankylosis. B and C. The advanced stage of ankylosis shows reduced distance.
In some cases, termed as skull base fibrosis, the ankylotic mass fuses with the lateral pterygoid plate and adequate mouth opening cannot be restored unless the fusion is released.12 Therefore, the distance of the ankylotic mass from the lateral pterygoid plate was measured in the coronal plane as the minimum distance between the medial margin of the ankylotic mass and the lateral pterygoid plate (Fig. 7).
Fig. 7. Relationship of ankylotic masses to the lateral pterygoid plate. The distance between the lateral pterygoid plate and medial margin of ankylotic mass is measured in the coronal plane. A. Early stage of ankylosis. B and C. Advanced stage of ankylosis, showing ankylotic masses in close proximity to the lateral pterygoid plate in the advanced stage of ankylosis.
The external auditory canal (EAC) is S-shaped, first curving posterosuperiorly and then anteroinferiorly. It is fibrocartilaginous in the lateral one-third and bony in the medial two-thirds. Its anterior wall and floor are formed by the tympanic part of the temporal bone, and it is related to the TMJ anteriorly. Damage to the EAC may occur if the surgeon is mistakenly guided or the ankylotic mass is in the vicinity of the EAC(Fig. 8). In addition, the aggressive use of instrumentation such as a chisel and a hammer can cause trauma to the related areas. The surgeon should have preoperative anatomic guidance when approaching an area of ankylosis that extends adjacent to the EAC.16 The distance between the ankylotic mass and the anterior wall of the external auditory canal was measured in the sagittal plane.
Fig. 8. Relationship of an ankylotic mass to the external auditory canal. The distance between the ankylotic mass(arrow) and the anterior wall of the external auditory canal (arrow) is measured in the sagittal plane. (A) Normal temporomandibular joint (TMJ). The circle shows the measurement in a normal TMJ. (B) An ankylosed TMJ with the ankylotic mass closely abutting the external auditory canal, as shown by the circle in B. CH: condylar head, EAC: external auditory canal.
The glenoid fossa, which consists of the squamous part of the temporal bone, forms the cranial component of the TMJ. When the ankylosis involves the glenoid fossa, as in stages 3 and 4, intraoperative iatrogenic perforation through the glenoid fossa into the middle cranial fossa can occur (Figs. 3C and D). This may lead to dural tear, cerebrospinal fluid leak, and exposure of the temporal lobe, for which a neurosurgical consultation is necessary.16 It may also result in unrecognized extradural hemorrhage from the middle meningeal artery. Glenoid fossa involvement was mentioned as part of the staging of ankylosis.
An assessment of the mandibular ramus and coronoid process is essential for surgical planning. TMJ ankylosis is associated with a reduced vertical height of the ramus secondary to arrested growth. Therefore, it is crucial to measure the ramus height when assessing the extent of shortening. The ramus height was measured in the sagittal plane on thick multiplanar images displaying the entire ramus along the posterior margin of ramus and in the region of the deepest antegonial notch (Fig. 9A).
Fig. 9. Measurement of the height of the ramus and coronoid process. A. Sagittal reformatted image shows a measurement of the vertical height of the ramus along its posterior margin (white arrows) and in the region of the deepest antegonial notch (black arrows). B. Sagittal reformatted image shows a measurement of coronoid process length, corresponding to the distance from the tip of the coronoid process to the mandibular incisura.
When the coronoid process projects superiorly beyond the inferior margin of the zygomatic arch, it is termed an enlarged coronoid process.17 An enlarged coronoid process leads to restricted mouth opening. Therefore, coronoid process length is measured to assess the need for coronoidectomy. This measurement was made in the sagittal plane, as the vertical distance from the tip of the coronoid process to the mandibular incisura (Fig. 9B).
A preoperative assessment of the skull base is required to avoid intraoperative injury. As mentioned above, skull base bones such as the sphenoid and temporal bones have a close anatomic relationship with the TMJ and transmit vital neurovascular structures via various foramina. When the ankylotic mass is in close relation with the foramen ovale, foramen spinosum, jugular foramen, and carotid canal; there is a risk of intraoperative injury to these structures during resection of an ankylotic mass(Fig. 10). In addition, the extent of bony fusion with the mastoid is estimated to evaluate the magnitude of drilling required to release the ankylotic mass(Fig. 11). There is an increased risk of dural perforation and iatrogenic brain injury when the skull base thickness is less than 3 mm.18 The relationships of the neural foramen were evaluated on axial sections and mastoid involvement was assessed on coronal sections.
Fig. 10. Skull base assessment. Mastoid involvement is assessed on a coronal section. A. Mild/early stage of ankylosis in which the mastoid is not involved. B. Advanced stage of ankylosis in which the mastoid is involved with the ankylotic mass(arrow).
Fig. 11. Skull base assessment. Mastoid involvement is assessed on a coronal section. A. Mild/early stage of ankylosis in which the mastoid is not involved. B. Advanced stage of ankylosis in which the mastoid is involved with the ankylotic mass(arrow).
The aforementioned measurements were performed bilaterally, even if the other side was normal, in order to enable comparisons with the ankylosed site.
Discussion
TMJ ankylosis refers to fibrous or bony fusion between the mandibular condyle and the glenoid fossa. It usually presents with progressive difficulty in mouth opening and facial deformity. Trauma, infection, and systemic diseases such as ankylosing spondylitis or rheumatoid arthritis are the common underlying etiologies.19 The etiopathogenesis of the development of ankylosis in cases of trauma is complex, with hypoxia and a pro-coagulant or hypofibrinolytic state playing a key role in stimulation of chondrogenesis or osteogenesis.20 As previously explained, TMJ ankylosis is classified into 4 stages(stages 1–4) depending on the degree of bony ankylosis. The commonly performed surgical procedures for TMJ ankylosis include osteoarthrectomy of the ankylosis with adequate gap creation.21,22,23 This is followed by ramus-condyle unit reconstruction.9,24 Additionally, coronoidectomy and fat grafting are performed to increase mouth opening and to reduce heterotopic bone formation, respectively.13,14,15
The authors have observed that a detailed preoperative assessment is of significant value prior to surgery. This can easily be done using MDCT, which can accurately assess the extent of an ankylotic mass and its relationship to adjacent vascular and bony structures. The various multiplanar reconstructions provide a complete evaluation of the joint and surrounding key anatomic landmarks. Structured radiological reporting of TMJ ankylosis is essential for preoperative planning to reduce the risk of intraoperative complications or inadequate resection. This includes an assessment of the extent of fibrous or bony ankylosis and staging according to the classification proposed by Xia et al.10 Measurement of the ankylotic mass on MDCT provides an estimate of the amount of material required for interpositional gap arthroplasty. Vascular injury to the IMA can be avoided by knowing the distance between the ankylotic mass and the IMA. Similarly, the distance of the ankylotic mass and key anatomic structures in the vicinity, such as the IAC, lateral pterygoid plate, glenoid fossa, and external auditory canal, can be depicted on the reconstructed images. This is essential for planning the surgical incision and can serve as a preoperative anatomic guide.
The length of the mandibular ramus and the coronoid process is also measured. Coronoidectomy is required in cases of an elongated coronoid process, the length of which can be easily measured on a preoperative scan. A skull base thickness less than 3 mm predisposes to dural perforation and brain injury. The magnitude of bone drilling varies with the extent of bony fusion with the mastoids, which can be easily assessed on the reformatted images. A detailed view of the condylar head, glenoid fossa, sphenoid bone, and temporal bone, along with the skull base foramina, can help in the safe resection of the ankylotic mass without any intraoperative damage to these key structures.
In conclusion, MDCT can provide an accurate assessment of the extent of an ankylotic mass, its relationship to adjacent vital structures, and other bony abnormalities. Structured reporting of TMJ ankylosis is essential to provide a roadmap for operating surgeons.
Footnotes
Conflicts of Interest: None
References
- 1.Rowe NL. Ankylosis of the temporomandibular joint. J R Coll Surg Edinb. 1982;27:67–79. [PubMed] [Google Scholar]
- 2.Roychoudhury A, Yadav P, Alagarsamy R, Bhutia O, Goswami D. Outcome of stock total joint replacement with fat grafting in adult temporomandibular joint ankylosis patients. J Oral Maxillofac Surg. 2021;79:75–87. doi: 10.1016/j.joms.2020.07.214. [DOI] [PubMed] [Google Scholar]
- 3.Li JM, Zhang XW, Zhang Y, Li YH, An JG, Xiao E, et al. Ankylosing spondylitis associated with bilateral ankylosis of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e478–e484. doi: 10.1016/j.oooo.2012.02.036. [DOI] [PubMed] [Google Scholar]
- 4.Chidzonga MM. Temporomandibular joint ankylosis: review of thirty-two cases. Br J Oral Maxillofac Surg. 1999;37:123–126. doi: 10.1054/bjom.1997.0089. [DOI] [PubMed] [Google Scholar]
- 5.El-Hakim IE, Metwalli SA. Imaging of temporomandibular joint ankylosis. A new radiographic classification. Dentomaxillofac Radiol. 2002;31:19–23. doi: 10.1038/sj/dmfr/4600660. [DOI] [PubMed] [Google Scholar]
- 6.Görgü M, Erdoğan B, Aköz T, Koşar U, Dağ F. Three-dimensional computed tomography in evaluation of ankylosis of the temporomandibular joint. Scand J Plast Reconstr Surg Hand Surg. 2000;34:117–120. doi: 10.1080/02844310050159963. [DOI] [PubMed] [Google Scholar]
- 7.Kavin T, John R, Venkataraman SS. The role of three-dimensional computed tomography in the evaluation of temporomandibular joint ankylosis. J Pharm Bioallied Sci. 2012;4(Suppl 2):S217–S220. doi: 10.4103/0975-7406.100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deckers MM, van Bezooijen RL, van der Horst G, Hoogendam J, van Der Bent C, Papapoulos SE, et al. Bone morphogenetic proteins stimulate angiogenesis through osteoblast-derived vascular endothelial growth factor A. Endocrinology. 2002;143:1545–1553. doi: 10.1210/endo.143.4.8719. [DOI] [PubMed] [Google Scholar]
- 9.Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145–1152. doi: 10.1016/0278-2391(90)90529-b. [DOI] [PubMed] [Google Scholar]
- 10.Xia L, An J, He Y, Xiao E, Chen S, Yan Y, et al. Association between the clinical features of and types of temporomandibular joint ankylosis based on a modified classification system. Sci Rep. 2019;9:10493. doi: 10.1038/s41598-019-46519-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salins PC. New perspectives in the management of craniomandibular ankylosis. Int J Oral Maxillofac Surg. 2000;29:337–340. [PubMed] [Google Scholar]
- 12.Bhave SM, Mehrotra D, Singh P, Shukla A. Extensive temporomandibular joint ankylosis involving medial pterygoid plates and the maxillary tuberosity - a case report. J Oral Biol Craniofac Res. 2019;9:218–221. doi: 10.1016/j.jobcr.2019.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roychoudhury A, Yadav P, Alagarsamy R, Bhutia O, Goswami D. Outcome of stock total joint replacement with fat grafting in adult temporomandibular joint ankylosis patients. J Oral Maxillofac Surg. 2021;79:75–87. doi: 10.1016/j.joms.2020.07.214. [DOI] [PubMed] [Google Scholar]
- 14.Kaur K, Roychoudhury A, Bhutia O, Bhalla AS, Yadav R, Pandey RM. Evaluation of success of transport disc distraction osteogenesis and costochondral graft for ramus condyle unit reconstruction in pediatric temporomandibular joint ankylosis. J Oral Maxillofac Surg. 2020;78:1–16. doi: 10.1016/j.joms.2020.01.029. [DOI] [PubMed] [Google Scholar]
- 15.Roychoudhury A, Acharya S, Bhutia O, Seith Bhalla A, Manchanda S, Pandey RM. Is there a difference in volumetric change and effectiveness comparing pedicled buccal fat pad and abdominal fat when used as interpositional arthroplasty in the treatment of temporomandibular joint ankylosis? J Oral Maxillofac Surg. 2020;78:1100–1110. doi: 10.1016/j.joms.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman D, Puig L. Complications of TMJ surgery. Oral Maxillofac Surg Clin North Am. 2015;27:109–124. doi: 10.1016/j.coms.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 17.Munk PL, Helms CA. Coronoid process hyperplasia: CT studies. Radiology. 1989;171:783–784. doi: 10.1148/radiology.171.3.2717752. [DOI] [PubMed] [Google Scholar]
- 18.Schmelzeisen R, Gellrich NC, Schramm A, Schön R, Otten JE. Navigation-guided resection of temporomandibular joint ankylosis promotes safety in skull base surgery. J Oral Maxillofac Surg. 2002;60:1275–1283. doi: 10.1053/joms.2002.35724. [DOI] [PubMed] [Google Scholar]
- 19.Nagori SA, Jose A, Bhutia O, Roychoudhury A. Undiagnosed mandibular condylar fractures causing temporomandibular joint ankylosis: a problem in northern India. Natl Med J India. 2014;27:251–255. [PubMed] [Google Scholar]
- 20.Bhatt KV, Roychoudhury A, Bhutia O. Pathogenesis of temporomandibular joint ankylosis: a perspective. Natl J Maxillofac Surg. 2020;11:154–155. doi: 10.4103/njms.NJMS_91_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajgopal A, Banerji PK, Batura V, Sural A. Temporomandibular ankylosis: a report of 15 cases. J Maxillofac Surg. 1983;11:37–41. doi: 10.1016/s0301-0503(83)80009-5. [DOI] [PubMed] [Google Scholar]
- 22.Roychoudhury A, Parkash H, Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: a report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:166–169. doi: 10.1016/s1079-2104(99)70267-2. [DOI] [PubMed] [Google Scholar]
- 23.Bhatt K, Roychoudhury A, Bhutia O, Pandey RM. Functional outcomes of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 2014;72:2434–2439. doi: 10.1016/j.joms.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 24.Mercuri LG, Ali FA, Woolson R. Outcomes of total alloplastic replacement with periarticular autogenous fat grafting for management of reankylosis of the temporomandibular joint. J Oral Maxillofac Surg. 2008;66:1794–1803. doi: 10.1016/j.joms.2008.04.004. [DOI] [PubMed] [Google Scholar]