Abstract
Purpose
Dental implants are widely used for the rehabilitation of edentulous sites. This study investigated the occurrence of dental implant malpositioning as shown on post-implantation cone-beam computed tomography (CBCT) and to identify related factors.
Materials and Methods
Samples with at least 1 malpositioned dental implant were collected from a central radiology clinic in Tehran, Iran from January 2017 to January 2019. Variables such as demographic characteristics, length and diameter of implants, type of implant, sites of implant insertion, different types of implant malpositioning problems (cortical plate perforation, interference with anatomical structures), angulation of the implant, and the severity of malpositioning were assessed. In addition, the incidence of implant fracture and over-drilling was evaluated. Data were statistically analyzed using the chi-square test, 1-sample t-test, and Spearman correlation coefficients.
Results
In total, 252 patients referred for implant postoperative CBCT evaluations were assessed. The cases of implant malpositioning included perforation of the buccal cortical plate (19.4%), perforation of the lingual cortical plate (14.3%), implant proximity to an adjacent implant (19.0%), implant proximity to an adjacent tooth (3.2%), interference with anatomical structures (maxillary sinus: 18.3%, mandibular canal: 11.1%, nasal cavity: 6.3%, mental foramen: 5.6%, and incisive canal: 0.4%). Implant fracture and over-drilling were found in 1.6% and 0.8% of cases, respectively. Severity was categorized as mild (9.5%), moderate (35.7%), severe (37.7%), and extreme (17.1%), and 52.4% of implants had inappropriate angulation.
Conclusion
CBCT imaging is recommended for detecting dental implant malpositioning. The most common and severe type of malpositioning was buccal cortex perforation.
Keywords: Dental Implants, Cone-Beam Computed Tomography, Medical Errors, Anatomic Landmarks
Introduction
Dental implants have become increasingly popular for the rehabilitation of patients with edentulism. However, the increasing need for dental implants is accompanied by a growth in unwanted complications. Complications are expected and may lead to a number of poor treatment results.1 McDermott et al.2 reported the overall frequency of complications to be as high as nearly 14%; therefore, a thorough clinical and radiographic pre-surgical evaluation of patients' bone quality and quantity is imperative for successful implant treatment.3,4
Previous studies have indicated that better host bone results in a higher success rate.4,5 Esposito et al.6 claimed that the 3 most important factors resulting in implant failure are surgical trauma, bone quality, and bone quantity. In another study, implant failure complications were found to be mainly due to biomechanical overload, infection or inflammation, and invasion of adjacent anatomical structures.7 Recent studies have discussed a number of adverse events after implant placement, ranging from functional and esthetic problems to neurosensory disturbances and life-threatening complications including hematoma formation, upper airway obstruction, and profuse, pulsatile bleeding.5,8,9,10 Therefore, a profound knowledge of surgical anatomy and prerequisites are obligatory prior to dental implant insertion.
In order to insert implant fixtures into an edentulous site, cone-beam computed tomography (CBCT) is the modality of choice, as it can accurately define the shape, morphology, and quantity of bone.11,12 This imaging modality presents cross-sectional views that can precisely indicate ridge height and width, the location of the mental and incisive fora-mina, lingual concavity, and the degree of ridge angulation. Shelley et al. reported fewer perforations of the lingual cortical plate when CBCT was performed prior to implant placement.11 In addition, the application of a prosthetically driven approach and use of a surgical guide may reduce operator-related surgical complications.12 However, unexpected complications may occur, even in the hands of skilled surgeons.1
The aim of this survey was to assess the occurrence of different types of dental implant malpositioning on postoperative CBCT imaging and to identify factors that cause or may be associated with complications of implant insertion.
Materials and Methods
This study was approved by the research committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.RIDS.REC.1395.366).
This descriptive cross-sectional study was performed on all postoperative CBCT examinations from patients referred to an oral and maxillofacial radiology center in Tehran, Iran from January 2017 to January 2019. Patients were referred from various dental clinics in Tehran Province and the suburbs of Tehran. The main reason for requesting scans was patient discomfort or the initial detection of implant malpositioning through a 2-dimensional radiographic assessment by the surgical operator. In total, 252 CBCT scans were included for evaluation. Demographic characteristics, including age and sex, were recorded. According to Moy et al.,13 patients were categorized by age into the following 4 groups: 1: under 40 years old, 2: 40 to 59 years old, 3: 60 to 79 years old, and 4: more than 79 years old. In addition, the specialty of the referring doctor was registered.
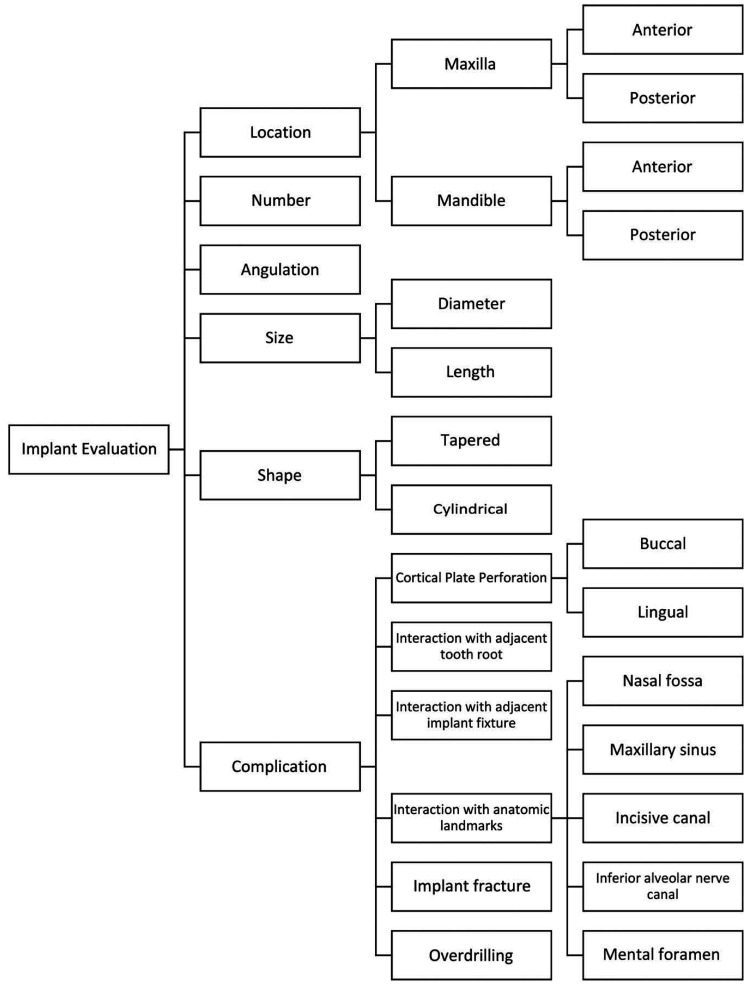
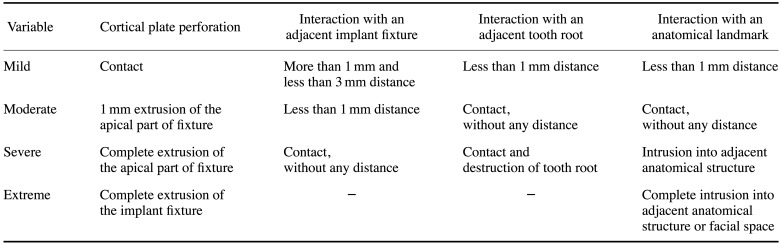
CBCT scans were taken with a Dentri device (HDXWILL, Seoul, Korea), with maximum peak kilovoltage of 100 kVp and variable fields of view suitable for each jaw. Images were evaluated using the OnDemand version No. 1.0.10 (CyberMed Inc, Seoul, Korea) 3-dimensional application with a standardized position for each jaw and sextant. On the selected cross-sectional images, containing implant, the following criteria were evaluated: implant location, number, size (diameter and length) and shape (tapered or cylindrical), angulation in degrees, and complications (including perforation of the cortical plates, interaction with an adjacent tooth or implant, interaction with anatomical landmarks, implant fracture, and over-drilling) (Fig. 1). The severity of implant malpositioning was categorized into 4 groups by a specialized periodontist (mild, moderate, severe, and extreme), as presented in Table 1. All assessments made based on the CBCT scans were made by an oral and maxillofacial radiologist with 10 years of experience.
Fig. 1. Flowchart shows the assessment of various criteria for each dental implant.
Table 1. Categorization of the severity of implant malpositioning.
All data were entered into a database system and evaluated using SPSS for Windows version 21 (IBM Corp., Armonk, NY, USA). Patients' data were analyzed anonymously. Every case was assigned a registration number before evaluation to allow explicit and anonymous attribution of the necessary information. Data analysis was performed with descriptive statistics, the chi-square test, the 1-sample t-test, and Spearman correlation coefficients. The level of significance was set at P=0.05.
Results
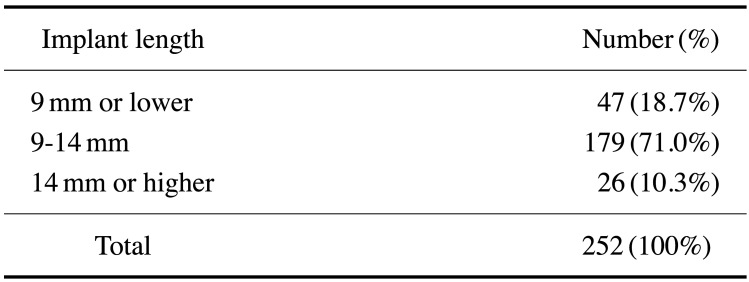
In total, 252 implants with malpositioning were evaluated from 113 patients, including 67 men (59.3%) and 46 women (40.7%). Each patient had at least 1 implant with malpositioning at the site of insertion. Patients' age ranged from 23 to 77 years (mean: 57.57±10.95 years). The prevalence of malpositioning was highest in the age range of 60 to 79 years. The relationship between age and severity of implant malpositioning was not statistically significant (P>0.05). The occurrence of implant malpositioning in various sites of the jaws was as follows: posterior mandible: 28.8%, anterior maxilla: 27.4%, posterior maxilla: 25.0%, and anterior mandible: 19.0%; however, these differences were not statistically significant (P>0.05). Regarding the implant type, 50.4% of implant fixations were cylindrical and 49.6% were tapered. There was a statistically significant relationship between the implant type and implant malpositioning (P<0.05), as malpositioning was more commonly detected with the cylindrical type. Over-drilling was only detected in 2 cases of tapered implants. Implant height varied between 5 mm and 16 mm (mean: 10.97±2.25 mm, Table 2). Implant diameter ranged from 3 mm to 5 mm (mean: 3.89±0.59 mm). No statistically significant relationship was found between implant height or width and the severity of implant malpositioning (P>0.05).
Table 2. Incidence of implant malpositioning according to length categorization.
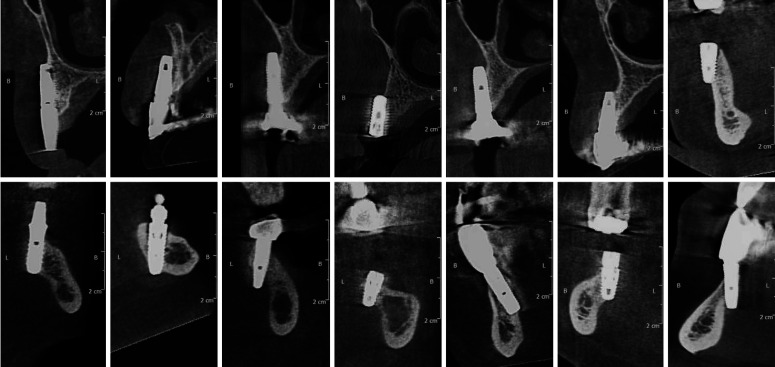
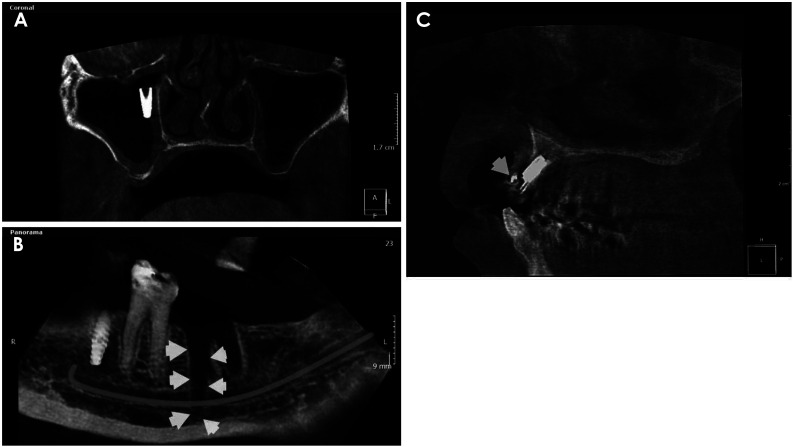
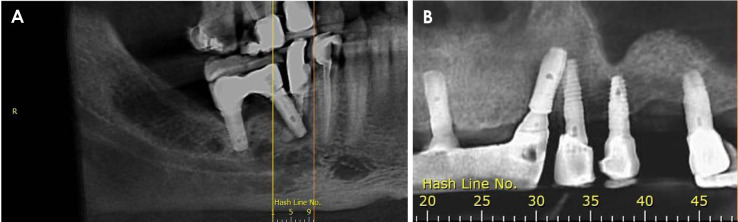
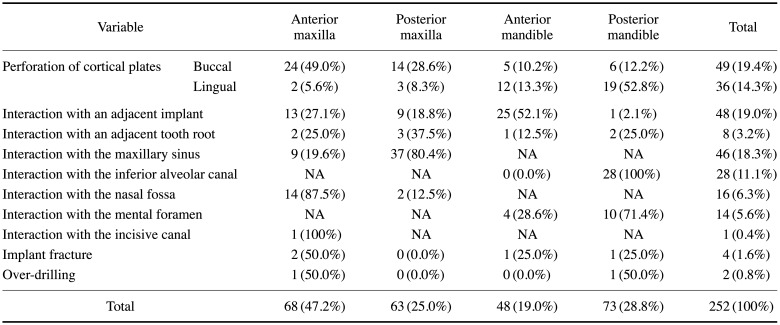
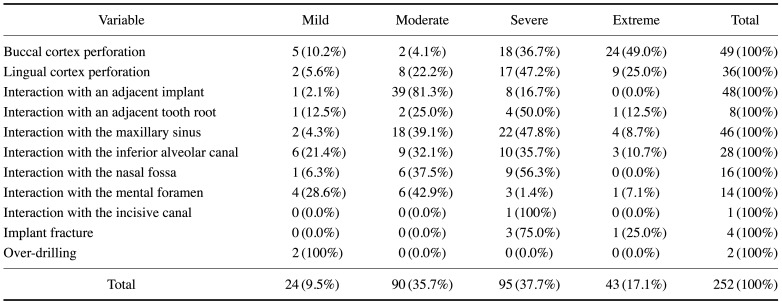
The distribution of types of implant malpositioning was as follows: interaction with anatomical structures: 41.7%, perforation of the buccal or lingual cortical plate: 33.7%, interaction with an adjacent implant: 19.0%, and interaction with an adjacent tooth root: 3.2%. Implant fracture was detected in 1.6% of cases. Two cases (0.8%) had over-drilling (Figs. 2, 3, 4, 5, 6). Buccal cortical plate perforations were more often seen in the anterior and posterior maxilla, while lingual cortical plate perforations were more often observed in the anterior and posterior mandible. Implant fixture interaction with another implant was more frequently observed in the anterior mandible and anterior maxilla. Implant interactions with the adjacent tooth root were more frequently seen in the posterior maxilla. No implants invaded the adjacent facial, pterygomandibular, or submandibular spaces (Table 3). The severity classification of implant malpositioning was as follows: severe, 37.7%; moderate, 35.7%; extreme, 17.1%; and mild, 9.5%. Table 4 shows the distribution of severity for each type of malpositioning.
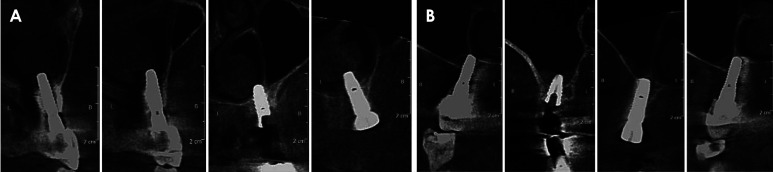
Fig. 2. Selected cross-sectional reformatted cone-beam computed tomographic images of the existing implants in different patients illustrate perforation of the buccal cortical plate (upper row) and lingual cortical plate (lower row).
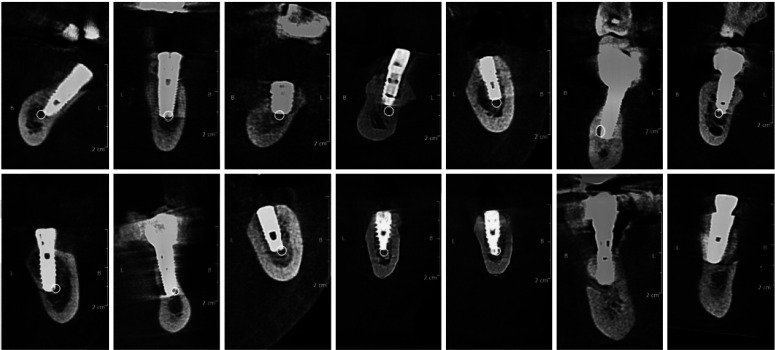
Fig. 3. Selected cross-sectional reformatted cone-beam computed tomographic images of the existing implants in different patients shows perforation of the cortical boundaries of the nasal floor (A) and sinus floor (B). There is mucosal thickening in the adjacent maxillary sinus.
Fig. 4. Selected cross-sectional reformatted cone-beam computed tomographic images of the existing implants in different patients indicates involvement of the inferior alveolar canal. White circles are the expected inferior alveolar canal outline.
Fig. 5. Various types of dental implant complications. A. Reformatted coronal cone-beam computed tomographic (CBCT) image shows displacement of a fixture into the right maxillary sinus. B. Low-thickness pseudo-panoramic image revealing over-drilling of the inferior alveolar canal in a patient with history of implant surgery 6 months ago and complaint of numbness of the lower left lip. The drilling hole is marked by arrows. C. Reconstructed cross-sectional CBCT image showing implant fracture (arrow).
Fig. 6. Cone-beam computed tomographic images show an implant crossing over the root of right mandibular second premolar (A), and contact of 2 implant fixtures in the maxilla (B).
Table 3. Incidence of implant malpositioning, fracture, and over-drilling at various sites of the jaw.
NA: not applicable
Table 4. Incidence of implant malpositioning, fracture, and over-drilling according to severity.
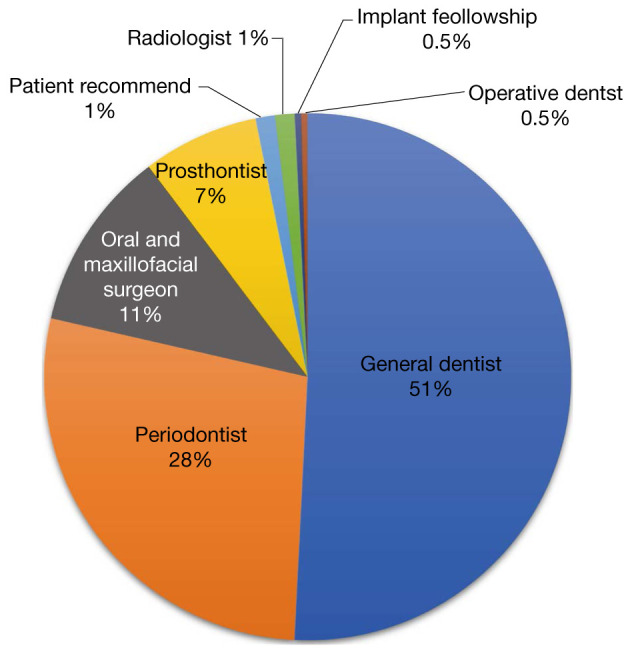
Regarding the implant angulation, 51.6% (n=130) of implants had proper angulation and 46.8% (n=118) had improper angulation. Four implants were completely displaced in the maxillary sinus; therefore, the angulation could not be assessed in those cases. There was a statistically significant relationship between implant malpositioning and implant angulation, as more complications occurred in cases of improper angulation (P<0.05). No statistically significant relationship was found between the implant site and angulation problems (P>0.05). Most of the post-implantation CBCT assessments were referred from general dentists (51.0%), followed in descending order by periodontists (28.0%), oral and maxillofacial surgeons (11.0%), prosthodontists (7.0%), and other clinicians (3.0%) (Fig. 7).
Fig. 7. Pie chart illustrating the prevalence of different specialties referring patients for post-implantation cone-beam computed tomographic assessment due to complications.
Discussion
The aim of this study was to assess the occurrence of various types of dental implant malpositioning and factors influencing malpositioning on post-implantation CBCT scans. The causes and mechanisms of implant failure depend on implant location, diameter, and length; bone quality and quantity; attention to the anatomical structures at each site; and the operator's technique and skills.14 Understanding the potential risk factors for early and late implant failure may help to decrease their frequency.15
In this study, no statistically significant relationship was detected between age and severity of malpositioning, which aligns with previous studies reporting no relationship between age and early implant failure.15,16,17 However, most cases of implant malpositioning were detected in patients aged 60 to 79 years. Due to the high prevalence of edentulism in this age category and the relatively high demand for implant placement, more frequent malpositioning may also be expected. Moy et al.13 also reported more implant failure in patients 60 years of age and above. This issue could be due to a reduction in bone quality and quantity, resulting in a lack of sufficient bony support for implant fixture and osseointegration. In addition, Sverzut et al.18 reported that the risk of implant failure increased by a factor of 1.07 for each additional year of patients' age and that more implant failures were detected men than in women.3 However, no significant relationship between sex and implant malpositioning was seen in the present study.
In this study, the majority of implants (71.0%) were 9 to 14 mm long. No statistically significant relationship was seen between implant length and the severity of malpositioning. It can therefore be assumed that with any implant length, a good success rate can be achieved when the implant is properly inserted. A prior study reported no significant difference in early implant failure according to whether the length was less than or more than 10 mm;15 however, another study showed higher rates of early failure in longer implants.14 Noguerol et al.19 also reported a higher risk of implant failure in implants less than 15 mm in length and over 4 mm in diameter.
In this study, it is thought that the shape of the implant had a significant relationship with treatment success. It is proposed that tapered implants are better for use in proximity to the sinus, nasal fossa, an adjacent tooth, or an adjacent implant fixture, whereas cylindrical implants are recommended in proximity to the inferior alveolar nerve canal and mental foramen. O'Sullivan et al.20 indicated better early implant stability with conical shapes. Mohajerani et al. detected more implant failures in tapered implants (7.8%) than in cylindrical implants (5.9%), although this difference was not statistically significant (P>0.05).15
In this study, more cases of implant malpositioning were detected in the maxilla than in the mandible, which is consistent with previous studies.3,21,22,23 In addition, more cases of malpositioning were detected in the posterior segment of jaw than at anterior sites. Van Steenberghe et al. found that half of early implant failures occurred in the maxilla.17 They reported that the implant success rate was 91.4% in the posterior maxilla, compared to 97.0% in the anterior maxilla. The success rates were 96.3% and 97.9% in the posterior and anterior mandible, respectively. Alsaadi et al. found significantly more implant failures in the posterior region of both jaws than in the anterior segment of the mandible.16 Misch et al.1 reported more lingual plate perforation in the posterior mandible due to the presence of lingual undercut. However, Safi et al. found that although the anterior mandible was considered safe for the insertion of dental implants, lingual undercut in the anterior mandible was estimated to be as much as 10.0%, implying that this factor needs to be assessed to prevent lingual plate perforation and subsequent bleeding.24 Other studies reported severe bleeding and hemorrhage following lingual perforation of the implant in the posterior mandible.9,25 Studies have also reported that implant placement in the posterior maxilla is complex due to the proximity of the sinus floor to the alveolar crest.26,27 In the present study, a total of 37.3% of the implants perforated the adjacent buccal or lingual cortices. Buccal plate perforation was more frequently seen in the maxilla, while lingual plate perforation was more frequent in the mandible. Abas et al.10 reported that implant positioning buccally of the alveolar process may result in a painless hard swelling and blue discoloration of the mucosa, which is an important issue, especially in esthetic zones. It has been suggested that the standard distances from an implant fixture to an adjacent tooth, adjacent implant fixture, and adjacent vital anatomical structure should be at least 1.5 mm, 3 mm, and 2 mm respectively.12 Implant angulation is another important determinant of implant success that should be determined according to the future prosthesis with consideration of the bucco-lingual, apico-coronal, and mesio-distal positions.1 Improper angulation was found in 46.8% of inserted implants. Implant fixture length or improper angulation may lead to invasion of the adjacent boundaries, cortex perforation, devitalization of adjacent teeth, and consequently implant failure. Surgical guides and proper treatment planning can alleviate angulation problems.1
In the present study, the prevalence of implant interactions with the inferior alveolar canal and mental foramen was 11.1% and 5.6% respectively. Trauma to the terminal branches of the mandibular nerve may occur during oral surgical insertion of the implant fixture, resulting in varying degrees of sensory alteration.28 One study found that the incidence of altered nerve sensation following implant placement in the atrophic posterior mandible was as high as 13.0%,29 which may be due to application of a long implant, improper angulation, and variations in anatomical structures. 30 Inferior displacement of implants in the posterior mandible may also be due to the presence of low-density bone, which may lead to inferior alveolar nerve injury and paresthesia.31
Implant displacement into the maxillary sinus often results from the presence of an atrophic posterior maxilla, subsequent pneumatization of the maxillary sinus into the alveolar ridge, and poor bone quality.32,33 The prevalence of implant interactions with the maxillary sinus was found to be 18.3%, with 8.7% of implants completely displaced into the sinus. Previous studies emphasized the need for maxillary sinus lifting before implant insertion in order to augment the atrophic posterior maxilla.27,34 In case of complete displacement of the implant into the maxillary sinus, an endoscopic method of removal may be suggested.35,36
Implant fracture was considered as a mechanical complication in this study and had a prevalence of 1.6%. This may be due to metal fatigue and adverse occlusal loading. Parein et al.21 also considered implant fracture to be an important factor in implant failure and suggested using more implant fixtures or implants with a larger diameter to address this issue. In order to better assess the severity of each variable, a classification was proposed consisting of mild, moderate, severe, and extreme groups. Other studies have used other categories to assess implant positioning problems.37 In this study, most cases of implant malpositioning were categorized as severe (37.7%). Buccal cortex perforation was the most common complication, with 49% of cases counted as extreme.
In this study, the incidence of implant malpositioning varied according to the referring specialty, and malpositioning was more common among patients referred from general dentists (51.0%) and periodontics (28.0%). Due to the cross-sectional nature of this study and lack of a thorough risk factor assessment, a conclusive explanation for this finding cannot be proposed, but some possibilities include a higher rate of implant insertion by these categories of clinicians or a higher accuracy of periodontists in detecting malpositioning and making a referral for CBCT evaluation. Two cases showed signs of over-drilling on post-surgical CBCT scans, which resulted in neurosensory disturbances in 1 patient with a posterior implant. Previous studies also have reported higher implant failures (by a factor of 2) in procedures performed by inexperienced dentists. Although an experienced surgeon can reduce the likelihood of malpositioning, unexpected implant problems can occur.31 To prevent these problems, surgeons and dentists should thoroughly assess the jaw clinically and radiographically.24 CBCT is the modality of choice for the pre-surgical phase of dental implants, as it allows a clear visualization of variations in ridge quality and quantity.38,39
Due to the nature of this cross-sectional analysis, information on preoperative radiographic assessments and imaging could not be obtained. In addition, not all cases of implant malpositioning could be evaluated on CBCT scans. Further studies can explore further potential associations of implant failure and complications with systemic diseases and medication use.
Dental implant-associated problems may not be apparent immediately, and CBCT imaging is the modality of choice for postoperative evaluations of dental implant malpositioning.40 In this study, the most common type of malpositioning was buccal plate perforation, and it was more commonly seen in the anterior maxilla than at other sites.
Footnotes
Conflicts of Interest: None
References
- 1.Misch K, Wang HL. Implant surgery complications: etiology and treatment. Implant Dent. 2008;17:159–168. doi: 10.1097/ID.0b013e3181752f61. [DOI] [PubMed] [Google Scholar]
- 2.McDermott NE, Chuang SK, Woo VV, Dodson TB. Complications of dental implants: identification, frequency, and associated risk factors. Int J Oral Maxillofac Implants. 2003;18:848–855. [PubMed] [Google Scholar]
- 3.Palma-Carrió C, Maestre-Ferrín L, Peñarrocha-Oltra D, Peñarrocha-Diago MA, Peñarrocha-Diago M. Risk factors associated with early failure of dental implants. A literature review. Med Oral Patol Oral Cir Bucal. 2011;16:e514–e517. doi: 10.4317/medoral.16.e514. [DOI] [PubMed] [Google Scholar]
- 4.Ko YC, Huang HL, Shen YW, Cai JY, Fuh LJ, Hsu JT. Variations in crestal cortical bone thickness at dental implant sites in different regions of the jawbone. Clin Implant Dent Relat Res. 2017;19:440–446. doi: 10.1111/cid.12468. [DOI] [PubMed] [Google Scholar]
- 5.Dubois L, de Lange J, Baas E, Van Ingen J. Excessive bleeding in the floor of the mouth after endosseus implant placement: a report of two cases. Int J Oral Maxillofac Surg. 2010;39:412–415. doi: 10.1016/j.ijom.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 6.Esposito M, Thomsen P, Ericson LE, Lekholm U. Histopathologic observations on early oral implant failures. Int J Oral Maxillofac Implants. 1999;14:798–810. [PubMed] [Google Scholar]
- 7.Liaw K, Delfini RH, Abrahams JJ. Dental implant complications. Semin Ultrasound CT MR. 2015;36:427–433. doi: 10.1053/j.sult.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Jaju P, Jaju S. Lingual vascular canal assessment by dental computed tomography: a retrospective study. Indian J Dent Res. 2011;22:232–236. doi: 10.4103/0970-9290.84293. [DOI] [PubMed] [Google Scholar]
- 9.Longoni S, Sartori M, Braun M, Bravetti P, Lapi A, Baldoni M, et al. Lingual vascular canals of the mandible: the risk of bleeding complications during implant procedures. Implant Dent. 2007;16:131–138. doi: 10.1097/ID.0b013e31805009d5. [DOI] [PubMed] [Google Scholar]
- 10.Abas I, Meijer GJ. Implant positioned buccally of the alveolar process; a complication. Ned Tijdschr Tandheelkd. 2016;123:79–81. doi: 10.5177/ntvt.2016.02.15143. [DOI] [PubMed] [Google Scholar]
- 11.Shelley AM, Ferrero A, Brunton P, Goodwin M, Horner K. The impact of CBCT imaging when placing dental implants in the anterior edentulous mandible: a before-after study. Dentomaxillofac Radiol. 2015;44:20140316. doi: 10.1259/dmfr.20140316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang E. In: White and Pharoah's oral radiology: principles and interpretation. 8th ed. Mallya SM, Lam EW, editors. St. Louis: Elsevier; 2019. Dental implants; pp. 248–270. [Google Scholar]
- 13.Moy PK, Medina D, Shetty V, Aghaloo TL. Dental implant failure rates and associated risk factors. Int J Oral Maxillofac Implants. 2005;20:569–577. [PubMed] [Google Scholar]
- 14.Chuang SK, Wei LJ, Douglass CW, Dodson TB. Risk factors for dental implant failure: a strategy for the analysis of clustered failure-time observations. J Dent Res. 2002;81:572–577. doi: 10.1177/154405910208100814. [DOI] [PubMed] [Google Scholar]
- 15.Mohajerani H, Roozbayani R, Taherian S, Tabrizi R. The Risk factors in early failure of dental implants: a retrospective study. J Dent (Shiraz) 2017;18:298–303. [PMC free article] [PubMed] [Google Scholar]
- 16.Alsaadi G, Quirynen M, Michiles K, Teughels W, Komárek A, van Steenberghe D. Impact of local and systemic factors on the incidence of failures up to abutment connection with modified surface oral implants. J Clin Periodontol. 2008;35:51–57. doi: 10.1111/j.1600-051X.2007.01165.x. [DOI] [PubMed] [Google Scholar]
- 17.van Steenberghe D, Jacobs R, Desnyder M, Maffei G, Quirynen M. The relative impact of local and endogenous patient-related factors on implant failure up to the abutment stage. Clin Oral Implants Res. 2002;13:617–622. doi: 10.1034/j.1600-0501.2002.130607.x. [DOI] [PubMed] [Google Scholar]
- 18.Sverzut AT, Stabile GA, de Moraes M, Mazzonetto R, Moreira RW. The influence of tobacco on early dental implant failure. J Oral Maxillofac Surg. 2008;66:1004–1009. doi: 10.1016/j.joms.2008.01.032. [DOI] [PubMed] [Google Scholar]
- 19.Noguerol B, Muñoz R, Mesa F, de Dios Luna J, O'Valle F. Early implant failure. Prognostic capacity of Periotest: retrospective study of a large sample. Clin Oral Implants Res. 2006;17:459–464. doi: 10.1111/j.1600-0501.2006.01250.x. [DOI] [PubMed] [Google Scholar]
- 20.O'Sullivan D, Sennerby L, Meredith N. Influence of implant taper on the primary and secondary stability of osseointegrated titanium implants. Clin Oral Implants Res. 2004;15:474–480. doi: 10.1111/j.1600-0501.2004.01041.x. [DOI] [PubMed] [Google Scholar]
- 21.Parein AM, Eckert SE, Wollan PC, Keller EE. Implant reconstruction in the posterior mandible: a long-term retrospective study. J Prosthet Dent. 1997;78:34–42. doi: 10.1016/s0022-3913(97)70085-4. [DOI] [PubMed] [Google Scholar]
- 22.Adell R, Eriksson B, Lekholm U, Brånemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5:347–359. [PubMed] [Google Scholar]
- 23.Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, Hirt H, et al. Long term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997;8:161–172. doi: 10.1034/j.1600-0501.1997.080302.x. [DOI] [PubMed] [Google Scholar]
- 24.Safi Y, Amid R, Vasegh Z, Ghazizadeh Ahsaie M. Anatomical variations in the interforaminal regions of candidates for implantassisted overdentures: a cross-sectional CBCT analysis. Gen Dent. 2020;68:11–16. [PubMed] [Google Scholar]
- 25.Kalpidis CD, Konstantinidis AB. Critical hemorrhage in the floor of the mouth during implant placement in the first mandibular premolar position: a case report. Implant Dent. 2005;14:117–124. doi: 10.1097/01.id.0000165028.89434.99. [DOI] [PubMed] [Google Scholar]
- 26.Kim SG, Mitsugi M, Kim BO. Simultaneous sinus lifting and alveo-lar distraction of the atrophic maxillary alveolus for implant placement: a preliminary report. Implant Dent. 2005;14:344–348. doi: 10.1097/01.id.0000188381.24406.35. [DOI] [PubMed] [Google Scholar]
- 27.Shin HI, Sohn DS. A method of sealing perforated sinus membrane and histologic finding of bone substitutes: a case report. Implant Dent. 2005;14:328–335. doi: 10.1097/01.id.0000188465.93052.cd. [DOI] [PubMed] [Google Scholar]
- 28.Ellies LG, Hawker PB. The prevalence of altered sensation associated with implant surgery. Int J Oral Maxillofac Implants. 1993;8:674–679. [PubMed] [Google Scholar]
- 29.Burstein J, Mastin C, Le B. Avoiding injury to the inferior alveo-lar nerve by routine use of intraoperative radiographs during implant placement. J Oral Implantol. 2008;34:34–38. doi: 10.1563/1548-1336(2008)34[34:AITTIA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Griffin TJ, Cheung WS. The use of short, wide implants in poste-rior areas with reduced bone height: a retrospective investigation. J Prosthet Dent. 2004;92:139–144. doi: 10.1016/j.prosdent.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 31.Doh RM, Pang NS, Kim KD, Park W. Implant displacement into the mandible: an unusual complication during implant surgery. Implant Dent. 2011;20:345–348. doi: 10.1097/ID.0b013e3182326813. [DOI] [PubMed] [Google Scholar]
- 32.Hürzeler MB, Kirsch A, Ackermann KL, Quiñones CR. Reconstruction of the severely resorbed maxilla with dental implants in the augmented maxillary sinus: a 5-year clinical investigation. Int J Oral Maxillofac Implants. 1996;11:466–475. [PubMed] [Google Scholar]
- 33.Jung JH, Choi BH, Zhu SJ, Lee SH, Huh JY, You TM, et al. The effects of exposing dental implants to the maxillary sinus cavity on sinus complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:602–605. doi: 10.1016/j.tripleo.2005.10.061. [DOI] [PubMed] [Google Scholar]
- 34.Misch C. Maxillary sinus augmentation for endosteal implants: organized alternative treatment plans. Int J Oral Implantol. 1987;4:49–58. [PubMed] [Google Scholar]
- 35.Raghoebar GM, Vissink A. Treatment for an endosseous implant migrated into the maxillary sinus not causing maxillary sinusitis: case report. Int J Oral Maxillofac Implants. 2003;18:745–749. [PubMed] [Google Scholar]
- 36.Lim D, Parumo R, Chai MB, Shanmuganathan J. Transnasal endoscopy removal of dislodged dental implant: a case report. J Oral Implantol. 2017;43:228–231. doi: 10.1563/aaid-joi-D-16-00172. [DOI] [PubMed] [Google Scholar]
- 37.Ribas BR, Nascimento EH, Freitas DQ, Pontual AD, Pontual ML, Perez DE, et al. Positioning errors of dental implants and their associations with adjacent structures and anatomical variations: a CBCT-based study. Imaging Sci Dent. 2020;50:281–290. doi: 10.5624/isd.2020.50.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shelley AM, Brunton P, Horner K. Subjective image quality assessment of cross sectional imaging methods for the symphyseal region of the mandible prior to dental implant placement. J Dent. 2011;39:764–770. doi: 10.1016/j.jdent.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 39.Quirynen M, Mraiwa N, Van Steenberghe D, Jacobs R. Morpho-logy and dimensions of the mandibular jaw bone in the interfora-minal region in patients requiring implants in the distal areas. Clin Oral Implants Res. 2003;14:280–285. doi: 10.1034/j.1600-0501.2003.140305.x. [DOI] [PubMed] [Google Scholar]
- 40.Safi Y, Amid R, Vasegh Z, Ahsaie MG. A new classification of anterior mandible edentulous ridge based on cone beam computed tomography. J Long Term Eff Med Implants. 2021;31:21–31. doi: 10.1615/JLongTermEffMedImplants.2020037061. [DOI] [PubMed] [Google Scholar]