Abstract
Objective
This study aimed to evaluate how social distancing measures affected physical activity (PA) patterns in adults from Rio Grande do Sul, Brazil.
Methods
Participants were recruited from social and local media campaigns, contacts with private and public universities, as well as research personal contacts across the state. PA was assessed before (retrospectively) and during social distancing. Frequency (days per week) and time (minutes per day) were asked to those participants who practiced PA. Two PA variables were built to each time-frame (before and during social distancing): 1) any PA (yes/no question), and 2) sufficient PA (based on the 150 min/week cut-off point).
Results
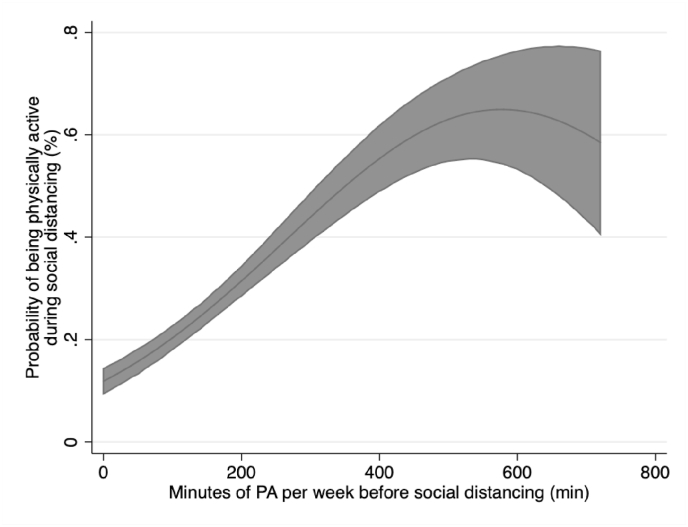
Overall, 2321 participants answered the questionnaire. Any and sufficient PA decreased from before to during social distancing (22.3% and 17.0%, respectively). A linear increase of activity during social distancing was observed in participants who practiced up to 400 min or less of PA per week before social distancing. Regarding associated factors, female, overweight/obese and diagnosed chronic disease participants were less likely to practice any or sufficient PA during social distancing when compared to the period before.
Conclusion
PA practice (both any and sufficient) decreased in Southern Brazil in the first months of social distancing. Women, overweight/obese and chronic diseased participants showed a higher decrease in PA compared to other groups. Finally, those participants who practiced PA before social distancing were more likely to continue practicing during COVID-19 pandemic.
Keywords: Cohort studies, Physical activity, Coronavirus disease 2019
1. Introduction
The coronavirus disease (COVID-19) pandemic strongly impacted several health systems around the world. Even countries with robust health systems, such as England and Germany were challenged by the virus.1 Unlike other countries, which are up ahead in their vaccine plan, Brazil is at a slow pace staying behind other countries, such as Chile.2 Health workers and at-risk groups (e.g. elderly) were vaccinated first, as stated by the Brazilian national plan, which foresees to immunize all population by 2022.3
During the pandemic, governments have adopted other strategies to avoid the virus spread, such as social distancing. This strategy is defined when people keep a safe space (about 2 arms lengths) between them and others who do not share the same household, in indoor and outdoor spaces.4 Although social distancing has shown to be an effective alternative to reduce the virus spread, other health consequences might be expected due to prolonged time spent at home. Indirect pandemic effects such as psychological and economic issues, as well as a decrease in physical activity (PA) levels might be expected.5
Regular PA is important for health, as it decreases the risk of several chronic conditions and premature death.6 Data from European and other Western countries, such as USA, showed a decrease in PA levels, as well as an increase in screen time activities.7,8 Furthermore, maintaining or increasing PA levels during pandemic times might prevent and aid in the treatment of other health issues (ie obesity, diabetes), which helps avoiding additional deaths due to pandemic indirect effects.7,8
At the beginning of the year 2020, when the pandemic was declared by the World Health Organization (WHO), people were encouraged to be physically active.9 General recommendation states that adults should practice at least 30 min of moderate intensity activity every day, or 150 min per week, however they can, since every minute counts.9, 10, 11 Staying at home may increase screen time (TV, smartphones, etc.) or hours spent in another sedentary pastime. Thus, our study aimed to evaluate how social distancing affected PA patterns in the first months of COVID-19 pandemic, in the adult population of Rio Grande do Sul state, Brazil.
2. Methods
2.1. Study design and sample
A longitudinal observational study in Rio Grande do Sul, a state in southern Brazil, is being carried out to gather data on mental and physical health, as well as healthcare access. Four timepoints were stablished: 1) pre-COVID-19 social distancing, 2) during COVID-19 social distancing, 3) 6 months and 4) 12 months after baseline assessments. Baseline covered pre-COVID-19 timepoint, which was assessed retrospectively, and the first months of social distancing in the region, which took place between June and July of 2020 (three months after the beginning of social restrictions).12 In this study, data from the first and second time point assessments of the PAMPA cohort (Prospective Study About Mental and Physical Health) were used. The study was approved by the local ethics institutional board (CAAE: 31906920.7.0000.5313). Details regarding study design and methods can be found elsewhere.13
In Brazil, states and cities governments have autonomy to define their actions against COVID-19. A controlled social distancing system was adopted by Rio Grande do Sul state. The state has seven macroregions (names in Portuguese): Vales, Sul, Serra, Metropolitana, Norte, Missioneira and Centro-Oeste. In this system, each macroregion is evaluated according to the following items on a weekly basis: the availability of intensive care unit (ICU) beds, infection incidence rates, and spreading velocity. Until may 2021, the severity of social restrictions measures was delimitated according to the scenario in each region, and every week the state government evaluated how the status was in each region, thus establishing a flag color (black, red, orange or yellow). During the first wave data collection, most of the state (73.4%) was classified as high risk (red flag), which means high level of social restriction (e.g. gyms, theaters, commercial centers closed).
Sample size was calculated considering the three main outcomes of this cohort (low back pain, mental health and healthcare access). Mental health outcomes required the highest sample size (n = 1359). After accounting for follow-up losses (30%) and multivariable analyzes, a final sample size of 1767 adults was required.13
A four-arm approach was used to achieve the target sample size as described elsewhere.13 In brief, a standardized message including information about the survey and a link to access the questionnaire was created. Further, this message was spread along as follows: 1) Contacts with private and public universities in the state; 2) social media campaigns (e.g. Facebook); 3) Local media; 4) Personal contacts across the state. The recruitment phase lasted four weeks. We have developed a self-administered online-based questionnaire using the Google Forms platform. The first question was related to the participant's acceptance to participate in the study. If participants answered “No”, the form was automatically uploaded without any participant's information. If participants answered “Yes”, the definitive questionnaire was prompted to participant's screen in the next page. The time needed to fill in the survey was around 10 min.
2.2. Physical activity
PA was estimated before and during social distancing using similar questions. The time frame was the only difference between the questions. The first question was related to PA engagement, as follows: “Before (During) social distancing, were you engaged in physical activity on a regular basis?”.14 “For those participants who answered “yes”, frequency (“How many days in the week do you practice these activities?”) and duration (“On the days that you practice these activities, how many minutes on average do they last?”) of their PA were also asked. Household chores and work-related physical activities were not considered.
Participants were also asked about the types of PA practiced at home or out of home. At home PA was considered as any activity performed within participant's household, and out of home as activities performed external to participants' household (e.g. parks, shared gyms). A list of activities was provided for the participants where they could indicate what activities they usually performed in each setting. Participants could indicate as many activities they performed.”
For analysis purposes, two PA variables were built. The first (any PA) was based solely on the first question (i.e. Yes or No PA practice, regardless of the volume). The second variable (sufficient PA) followed the WHO recommendation for PA9, and participants were categorized in inactive (less than 150 min per week) or active (150 min or more per week).
2.3. Covariates
Sociodemographic (gender, age, marital status and educational level), nutritional (body mass index [BMI]), self-reported diagnosis of chronic disease, as well as variables related to COVID-19 pandemic (economic impact and social distancing adherence) were used as exposure variables.
Body weight (kg) and height (m) was self-reported and BMI was calculated using the following formula: body weight/height.2 A question based on the Brazilian Surveillance System of Risk Factors for Chronic Diseases by Telephone Interviews (VIGITEL) was used to assess the diagnostic of chronic diseases such as hypertension, diabetes, depression, and others.15
The economic impact of pandemic on income was assessed by the following question: “Did social distancing affect your monthly income?”. The response options were: “yes, it reduced; yes, it increased or, no. For analysis purposes this variable was dichotomized in yes (reduced) or no.
Participants attitudes toward social distancing measures were asked by the question: “Regarding the social distancing that is being guided by health authorities, that is, staying home and avoiding contact with other people, how much of it do you think you are managing to do?”. There were five response options, as follows: “very little”, “little”, “somewhat”, “very much” and “totally isolated”. For analysis purposes participants were classified into four categories: “little”, “somewhat”, “very much” and “totally isolated”.
2.4. Statistical analysis
Due to a higher number of respondents from the South mesoregion (N = 1247 [53.7%]), all analyzes were weighted by the number of respondents in each region. An equality of proportions test was used to compare prevalence of any and sufficient PA in both time points, as well as the proportion of practiced PA's types. Minutes of PA are presented as median and interquartile range (IQR).
We also calculated the probability of being physically active during the pandemic based on pre-Covid-19 weekly volume of PA. To do this, PA volume before the pandemic (minutes per week) was adjusted for all covariates and then used to estimate the probability of reaching the WHO's recommendation (i.e., 150 min of PA per week) during the pandemic.
We performed univariable and multivariable Poisson regression to identify the determinants of any and sufficient PA. Gender, age, educational level, BMI, marital status, reduced monthly income, social distancing adherence and chronic diseases were used as covariate in both models (for any and sufficient PA). All variables from the univariable analysis were added in the multivariable model, and a p-value≤0.20 was set to determine whether variables were kept in the model. We adopted a p-value lower than 0.05 as the level of significance. All analyzes were conducted in Stata 15.1 (StataCorp, College Station, Texas).
3. Results
Most participants were female (76.6% [95%CI 74.4; 78.7]), aged 37.6 ± 13.5 years, had a college degree (44.9% [95%CI 42.3; 47.47]) or a higher graduation (40.2% [95%CI 37.7; 42.7]), lived with a partner (61.6 [95%CI 59.1; 64.1]) and were classified as overweight/obese (33.1% [95%CI 30.7; 35.5)] and (20.1% [95%CI 18.1; 22.2], respectively) regarding their BMI. In addition, most participants were not economically affected by pandemic (54.7% [95%CI 52.1; 57.2]), complied with social restrictions measures (51.8% [95%CI 49.2; 54.3]) and reported at least one chronic disease (56.7% [95%CI 54.3; 59.4%]).
A sharp decrease in the prevalence of any (from 69.0% [95%CI 66.6–71.4] to 46.7% [95%CI 44.2–49.3]; p < 0.001) and sufficient PA (from 40.5% [95%CI 37.9–42.9] to 23.5% [95%CI 21.4–25.7]; p < 0.001) from before to during social distancing was observed. This reduction was noticed regardless of gender, age, educational level, BMI, marital status, reduced monthly income, social distancing adherence and diagnosed chronic diseases (Table 1). Also, the median minutes of PA decreased from 45 (IQR 0–60 before) to 0 (IQR 0–50 during pandemic).
Table 1.
Prevalence (95% confidence interval) of physically active participants in both time points, by gender, age, educational level, BMI, marital status, reduced monthly income, social distance adherence and chronic disease. Rio Grande do Sul, Brazil, 2020.
|
Any PA |
Sufficient PA |
|||
|---|---|---|---|---|
| Gender (n = 2319) | Before | During | Before | During |
| Male | 77.4 (72.6; 81.6) | 49.8 (44.6; 55.1) | 52.8 (47.5; 57.9) | 27.2 (22.9; 32.1) |
| Female | 66.5 (63.6; 69.2) | 45.7 (42.8; 48.6) | 36.7 (33.9; 39.5) | 22.3 (19.9; 24.8) |
| Age(n = 2300) | ||||
| 18-30 | 71.8 (67.9; 75.5) | 47.4 (43.3; 51.6) | 50.5 (46.4; 54.7) | 25.9 (22.4; 29.8) |
| 31-59 | 66.1 (62.7; 69.4) | 46.7 (43.3; 50.2) | 34.5 (31.3; 37.8) | 21.9 (19.2; 24.9) |
| 60+ | 73.9 (65.2; 81.1) | 45.1 (36.5; 54.1) | 34.7 (26.8; 43.6) | 23.4 (16.8; 30.0) |
| Educational level(n = 2321) | ||||
| High school or less | 58.2 (51.5; 64.5) | 35.3 (29.4; 41.7) | 33.9 (28.1; 40.3) | 20.6 (15.9; 26.1) |
| College degree | 66.9 (63.1; 70.4) | 45.1 (41.3; 48.9) | 40.8 (37.0; 44.6) | 22.3 (19.2; 25.7) |
| Postgraduate | 75.5 (71.8; 78.7) | 52.7 (48.7; 56.7) | 42.5 (38.6; 46.5) | 25.8 (22.5; 29.4) |
| BMI(n = 2315) | ||||
| Normal | 74.9 (71.6; 78.1) | 53.8 (50.1; 57.6) | 45.4 (41.7; 49.1) | 28.8 (25.5; 32.3) |
| Overweight | 71.0 (66.8; 74.8) | 43.7 (39.4; 48.1) | 42.5 (38.2; 46.9) | 20.7 (17.4; 24.4) |
| Obese | 52.4 (46.6; 58.2) | 35.1 (29.8; 40.9) | 25.9 (21.3; 31.2) | 15.6 (11.9; 20.3) |
| Marital status(n = 2321) | ||||
| With partner | 66.9 (63.8; 69.9) | 45.1 (41.9; 48.4) | 36.9 (33.8; 40.0) | 21.5 (18.9; 24.3) |
| Without partner | 72.5 (68.6; 76.1) | 49.3 (45.2; 53.4) | 46.3 (42.2; 50.4) | 26.6 (23.2; 30.4) |
| Reduced monthly income(n = 2321) | ||||
| No | 67.2 (63.9; 70.4) | 46.6 (43.2; 50.1) | 37.3 (34.1; 40.7) | 22.2 (19.5; 25.1) |
| Yes | 71.3 (67.7; 74.6) | 46.8 (42.9; 50.7) | 44.3 (40.5; 48.1) | 24.9 (21.8; 28.4) |
| Social distancing adherence(n = 2321) | ||||
| Little | 71.3 (62.8; 78.5) | 43.1 (34.9; 51.8) | 46.8 (38.4; 55.5) | 24.9 (18.3; 32.9) |
| Somewhat | 67.6 (61.9; 72.8) | 50.5 (44.8; 56.3) | 42.3 (36.7; 48.0) | 27.4 (22.6; 32.8) |
| Very much | 71.4 (68.0; 74.4) | 48.3 (44.8; 51.9) | 40.5 (37.0; 43.9) | 22.8 (19.9; 23.8) |
| Totally isolated | 63.3 (57.6; 68.6) | 40.3 (34.9; 46.0) | 35.7 (30.5; 41.3) | 20.8 (16.6; 25.7) |
| Chronic disease(n = 2321) | ||||
| No | 74.1 (70.5; 77.3) | 50.1 (46.2; 53.9) | 47.4 (43.5; 51.3) | 25.4 (22.2; 28.8) |
| Yes | 65.2 (61.9; 68.4) | 44.1 (40.7; 47.5) | 35.2 (32.0; 38.5) | 22.0 (19.3; 24.9) |
Regarding the types of PA practiced at home, a significant increase was observed in activities such as walking/running (p = 0.016), rope jump (p < 0.001), strength (p < 0.001), flexibility (p < 0.001), yoga (p = 0.013) and dance (p = 0.015). On the other hand, climbing stairs showed a significant decrease from before to during social distancing (p < 0.001). On activities performed out of home, a significant decrease was observed in the following activities: walking/running (p < 0.001), rope jump (p < 0.001), bicycling (p < 0.001), strength (p < 0.001), flexibility (p < 0.001), climbing stairs (p < 0.001), dance (p = 0.002), functional training (p = 0.032), swim (p = 0.018), volleyball (p < 0.001), racquet sports (p = 0.019) and soccer (p < 0.001) (Table 2).
Table 2.
Prevalence (95% confidence interval) of PA types practiced at and out of home, before and during social distancing. Rio Grande do Sul, Brazil, 2020.
|
Activities performed at home |
||
|---|---|---|
| Activity | Before social distancing | During social distancing |
| Walk/run | 11.0 (9.6; 12.8) | 12.4 (10.9; 14.2) |
| Rope jump | 4.8 (3.8; 5.9) | 8.4 (7.1; 9.8) |
| Ride bike | 4.9 (3.9; 6.1) | 4.6 (3.7; 5.8) |
| Strength | 16.8 (14.9; 18.7) | 28.8 (27.0; 31.1) |
| Flexibility | 15.1 (13.4; 17.0) | 22.4 (20.4; 24.6) |
| Stairs | 13.7 (12.1; 15.5) | 11.4 (9.8; 13.1) |
| Dance | 0.6 (0.3; 1.0) | 1.1 (0.7; 1.7) |
| Pilates | 0.4 (0.2; 0.8) | 0.5 (0.3; 1.1) |
| Stretching | 0.4 (0.2; 0.8) | 0.5 (0.3; 1.0) |
| Yoga | 0.5 (0.3; 1.1) | 1.3 (0.8; 1.9) |
| Functional Training | 0.5 (0.2; 1.1) | 0.8 (0.4; 1.4) |
| Fights/martial arts | 0.3 (0.1; 0.7) | 0.6 (0.3; 1.1) |
| Activities performed outdoors | ||
| Activity | Before social distancing | During social distancing |
| Walk/run | 47.7 (45.2; 50.3) | 24.1 (21.9; 26.4) |
| Rope jump | 4.0 (3.0; 5.0) | 1.8 (1.3; 2.7) |
| Ride bike | 19.6 (17.7; 21.7) | 8.9 (7.6; 10.5) |
| Strength | 22.4 (20.3; 24.5) | 8.5 (7.1; 10.0) |
| Flexibility | 13.2 (11.6; 15.1) | 4.8 (3.8; 6.1) |
| Stairs | 9.0 (7.5; 10.5) | 3.5 (2.7; 4.6) |
| Dance | 0.6 (0.3; 1.0) | 0.1 (0.03; 0.5) |
| Pilates | 0.6 (0.3; 1.1) | 0.2 (0.1; 0.5) |
| Yoga | 0.3 (0.1; 0.8) | – |
| Functional Training | 0.5 (0.2; 1.0) | 0.3 (0.1; 0.9) |
| Fights/martial arts | 0.3 (0.1; 0.8) | 0.2 (0.1; 0.6) |
| Swim | 0.6 (0.3; 1.1) | 0.1 (0.02; 0.2) |
| Volley | 0.9 (0.5; 1.6) | 0.1 (0.01; 0.2) |
| Racquet sports | 0.8 (0.5; 1.3) | 0.5 (0.3; 1.0) |
| Soccer | 1.1 (0.7; 1.9) | 0.1 (0.01; 0.7) |
| Group classes | 1.5 (0.03; 0.7) | – |
Fig. 1 shows an association between PA before social distancing and PA during social distancing. A linear increase in the likelihood of being active during social distancing was observed, as more minutes of PA the participants practiced before this time point. However, our findings suggest that this linear increase was observed for participants who achieved 400 min or less of PA per week. For those who reported higher volume, no additional increase in the probability of being active during social distancing was observed.
Fig. 1.
Dose-response relationship between the amount of PA practiced before the COVID-19 social distancing and the probability of being physically active (i.e., ≥ 150 minutes of moderate-to-vigorous physical activity per week) during the COVID-19 social distancing. Rio Grande do Sul, Brazil.
The associated factors of any and sufficient PA are shown in Table 3, Table 4, respectively. Female (PR 0.83; 95%CI 0.78–0.89), overweight/obese (PR 0.87; 95%CI 0.82–0.93 and PR 0.69; 95%CI 0.62–0.76, respectively), as well as those participants with some chronic disease (PR 0.93; 95%CI 0.88–0.98) were less likely to practice any PA during social distancing, compared to the period before. On the other hand, participants with university or postgraduate degree (PR 1.15; 95%CI 1.04–1.28 and PR 1.37; 95CI 1.24–1.53, respectively) and those who lived without a partner (PR 1.10; 95%CI 1.03–1.16) were more likely to practice any PA (Table 3).
Table 3.
Crude and adjusted analyzes between co-variates and any PA. Rio Grande do Sul, Brazil, 2020.
|
Crude |
p-value |
Adjusted |
p-value |
|
|---|---|---|---|---|
| Gender | PR (95%CI) | <0.001 | PR (95%CI) | <0.001 |
| Male | – | – | ||
| Female | 0.88 (0.83; 0.94) | 0.83 (0.78; 0.89) | ||
| Age | 0.338 | 0.224 | ||
| 18-30 | – | – | ||
| 31-59 | 0.95 (0.88; 1.01) | 0.99 (0.92; 1.06) | ||
| 60+ | 0.99 (0.89; 1.11) | 1.11 (0.99; 1.24) | ||
| Educational level | <0.001 | <0.001 | ||
| High school or less | – | – | ||
| College degree | 1.19 (1.08; 1.33) | 1.15 (1.04; 1.28) | ||
| Postgraduate | 1.37 (1.23; 1.52) | 1.37 (1.24; 1.53) | ||
| BMIa | <0.001 | <0.001 | ||
| Normal | – | – | ||
| Overweight | 0.89 (0.83; 0.94) | 0.87 (0.82; 0.93) | ||
| Obese | 0.67 (0.61; 0.75) | 0.69 (0.62; 0.76) | ||
| Marital status | 0.007 | 0.003 | ||
| With partner | – | – | ||
| Without partner | 1.09 (1.02; 1.15) | 1.10 (1.03; 1.16) | ||
| Reduced monthly income | 0.238 | 0.140 | ||
| No | – | – | ||
| Yes | 1.04 (0.97; 1.10) | 1.05 (0.98; 1.10) | ||
| Social distancing adherence | 0.188 0.0107a |
0.218 0.0371a |
||
| Little | – | – | ||
| Somewhat | 1.03 (0.91; 1.16) | 1.02 (0.90; 1.14) | ||
| Very much | 1.04 (0.93; 1.16) | 1.03 (0.92; 1.14) | ||
| Totally isolated | 0.91 (0.79; 1.03) | 0.91 (0.79; 1.03) | ||
| Chronic disease | <0.001 | 0.016 | ||
| No | – | – | ||
| Yes | 0.88 (0.83; 0.93) | 0.93 (0.88; 0.98) |
∗BMI – Body mass index.
p for heterogeneity.
Table 4.
Crude and adjusted analyzes between co-variates and sufficient PA. Rio Grande do Sul, Brazil, 2020.
|
Crude |
p-value |
Adjusted |
p-value |
|
|---|---|---|---|---|
| Gender | PR (95%CI) | <0.001 | PR (95%CI) | <0.001 |
| Male | – | – | ||
| Female | 0.74 (0.66; 0.82) | 0.70 (0.62; 0.77) | ||
| Age | <0.001 | 0.050 | ||
| 18-30 | – | – | ||
| 31-59 | 0.74 (0.66; 0.82) | 0.83 (0.74; 0.93) | ||
| 60+ | 0.76 (0.62; 0.94) | 0.92 (0.75; 1.14) | ||
| Educational level | 0.006 | <0.001 | ||
| High school or less | – | – | ||
| College degree | 1.16 (0.98; 1.36) | 1.08 (0.92; 1.27) | ||
| Postgraduate | 1.06 (1.06; 1.48) | 1.34 (1.14; 1.59) | ||
| BMI | <0.001 | <0.001 | ||
| Normal | – | – | ||
| Overweight | 0.85 (0.76; 0.95) | 0.84 (0.75; 0.94) | ||
| Obese | 0.56 (0.47; 0.66) | 0.58 (0.49; 0.69) | ||
| Marital status | <0.001 | <0.001 | ||
| With partner | – | – | ||
| Without partner | 1.25 (1.13; 1.38) | 1.21 (1.09; 1.35) | ||
| Reduced monthly income | 0.004 | 0.014 | ||
| No | – | – | ||
| Yes | 1.16 (1.05; 1.29) | 1.14 (1.03; 1.26) | ||
| Social distancing adherence | 0.007 0.0434a |
0.030 0.1673a |
||
| Little | – | – | ||
| Somewhat | 0.97 (0.80; 1.17) | 0.95 (0.78; 1.14) | ||
| Very much | 0.88 (0.74; 1.05) | 0.86 (0.73; 1.02) | ||
| Totally isolated | 0.78 (0.64; 0.96) | 0.84 (0.69; 1.02) | ||
| Chronic disease | <0.001 | 0.029 | ||
| No | – | – | ||
| Yes | 0.78 (0.71; 0.87) | 0.89 (0.52; 0.65) |
∗BMI – Body mass index.
p for heterogeneity.
The likelihood of complying with PA recommendation was lower in female (PR 0.70; 95%CI 0.62–0.77), overweight/obese (PR 0.84; 0.75–0.94 and PR 0.58; 95%CI 0.49–0.69, respectively), and diagnosed chronic disease (PR 0.89; 95%CI 0.52–0.65) participants. On the other hand, participants with postgraduate degree (PR 1.34; 95%CI 1.14–1.59), who lived without a partner (PR 1.21; 95%CI 1.09–1.35) and reported reduced monthly income (PR1.14; 95%CI 1.03–1.26) were more likely to comply with the PA recommendations (Table 4).
4. Discussion
Our study revealed a decrease in PA of approximately 20% in the adult population of southern Brazil, from before to the first months of social distancing. Furthermore, the reduction in PA was higher among female, overweight/obese and diagnosed chronic disease participants. As expected, participants practiced more PA at and less PA out of home. Participants who practiced up to 400 min/week of PA before social distancing were more likely to practice PA during this timepoint. However, an increase in the likelihood of being active during social distancing was not observed in participants who practiced 400 min/week or more.
The recent PA guidelines launched by WHO state that people should practice from 150 to 300 min per week of moderate-intensity activities, however they can, with the idea that “every move counts”.9,16 A recent systematic review showed that higher levels of PA in any intensity (light, moderate or vigorous) can reduce the risk of premature death.17 Then, during COVID-19 pandemic the recent notion that “some activity is better than none” should be emphasized, as many people might not be able to achieve 150 min/week of PA.
During pandemic there was a remarkable downtrend on PA levels. Many people had to change from outdoor and sports activities to home-based workouts to remain physically active.18 Also, an increase in activities lasting less than 30 min per session was observed.19 This might be explained by a shift in the types of activities performed. Outdoors activities such as walking/practicing sports have been replaced by activities practiced at home, with shorter duration.19
A recent study reported large reductions in PA practice among participants who met PA recommendations before social distancing.20 On the other hand, our study showed a linear relationship between minutes of PA before social distancing and the likelihood of being active during this period. This pattern was observed even if participants practiced less than 150 min per week before this timepoint. Furthermore, it is also known that people who are inactive might achieve health benefits driven by small increases in PA.21 Prior PA levels have shown to be an important factor during the pandemic. Data from the UK Biobank study found that participants who were physically inactive before the pandemic were 32% more likely to be hospitalized due to COVID-19.22
The COVID-19 pandemic brought many changes to people's daily life, such as an increased time at home. Data from a 2019 telephone-based national survey conducted in Brazil, pointed out Porto Alegre, the state capital of Rio Grande do Sul, as one of the capitals with the lowest prevalence of sufficient PA (37.7%).23 We revealed a prevalence of 40.5% (95%CI 37.9–42.9) of sufficient PA before, and of 23.5% (95%CI 21.4–25.7) during social distancing. A decrease in PA levels was expected due to the measures adopted by the state and municipal governments to control the virus spread. Thus, PA promotion plans should be thought by the state's health organs to avoid health issues related to physical inactivity. Promoting PA is important in any time, especially during a pandemic. Our findings highlight the importance of PA promotion programs in southern Brazil.
The relationship between PA and associated factors found in our study are similar to those previously reported.24,25 It has been widely acknowledged that women are less active than men, especially in the leisure domain.24 However, during social distancing and prolonged homestay, women might have accumulated household tasks, paid work and child care, increasing their workday routine, which can be determinant for a more pronounced decline in PA among women compared to men.
People diagnosed with chronic conditions report several barriers to practice PA.26,27 These people are in the high-risk group; therefore, they are recommended to stay home, even when social restrictions are relaxed. However, at the same time that staying home is protecting this population from being infected, they might have disease-related complications due to physical inactivity. This is a concern and can have several impacts on health systems.28,29 Even though there are structural issues related to PA practice at home (e.g. lack of equipment or not suitable space), such people should find a way to exercise, always taking into account the specific characteristics of their disease condition.
Educational level is a proxy variable for income. It is known that high schooling and income group shows increased PA levels compared to their counterparts (i.e. lower schooling and income).24,25 Thus, it is plausible that participants with higher schooling were the least affected economically. In addition, this population is aware of the beneficial effects of PA on health, and are more likely to keep practicing PA at home through online classes, for example. This might explain why highly educated participants were more likely to practice PA during social distancing.
Participants who lived without a partner were more likely to practice PA, which corroborates with previous studies indicating that starting cohabitation or getting married were associated with reduced PA.30,31 Furthermore, due to social restrictions, people who lived without a partner might experience loneliness, and PA practice can be an alternative for their free time.
The limitations of our study should be acknowledged. Even though COVID-19 pandemic has an unprecedent impact on people's life improving their ability to make comparisons between the present and past time points, recall bias cannot be discarded. Also, since face-to-face research approaches are limited by ethics boards in Brazil at COVID-19 pandemic period, data collection was carried out online and there was an overrepresentation of some subgroups in our sample. As expected, our sample is younger and more schooled than the sate population25, and selection bias was a concern. Using this strategy to gather the data, a misrepresentation of the state population was expected, since many individuals do not have internet access in Brazil yet. However, this is a limitation observed in most studies during this pandemic time. In addition, richer individuals usually have higher levels of PA than their counterparts in Brazil, thus, we believe that if our sample had more participants from lower economic levels, the PA levels would be even lower than those reported here. Finally, this is a first report from an ongoing cohort study and data from future follow ups will be important to monitor and guide actions in this population.
5. Conclusions
In conclusion, our study reports a sharply decrease on the practice of any and sufficient PA in Southern Brazil, in the first months of social distancing. Specific groups, such as women, overweight/obese participants, as well as those diagnosed with some chronic disease had their PA patterns more affected by the pandemic, hence demanding more actions to promote PA in these groups in order to avoid other health issues in the future. Also, our study shows that participants with higher PA levels before the pandemic remained with the highest PA levels during this period. Future studies should evaluate PA tracking over time during COVID-19 pandemic.
Practical implications
-
•
The first months of social distancing showed an important impact in physical activity pattern;
-
•
People should stay active during the COVID-19 pandemic, regardless their physical activity practice before this event;
-
•
Specific groups such as women and chronic disease participants need more attention of public policies to increase their physical activity level during social distancing.
Funding
Not applied.
Disclosure statement
No potential competing interest was reported by the authors.
CRediT authorship contribution statement
Eduardo L. Caputo: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. Natan Feter: Formal analysis, Writing – original draft, Writing – review & editing. Igor R. Doring: Data curation, Writing – review & editing. Jayne S. Leite: Data curation, Writing – review & editing. Júlia Cassuriaga: Data curation, Writing – review & editing. Airton J. Rombaldi: Supervision, Writing – original draft, Writing – review & editing. Marcelo C. da Silva: Supervision, Writing – original draft, Writing – review & editing. Felipe F. Reichert: Supervision, Writing – original draft, Writing – review & editing.
Declaration of competing interest
None.
Acknowledgments
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
References
- 1.Sohrabi C., Alsafi Z., O'Neill N. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus (COVID-19) vaccinations - statistics and research - our World in data. https://ourworldindata.org/covid-vaccinations
- 3.Brasil. Plano Nacional de Operacionalização Da Vacinação Contra a COVID-19 Brasil.; 2020. [Google Scholar]
- 4.Social Distancing https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
- 5.Paules C.I., Marston H.D., Fauci A.S. Coronavirus infections-more than just the common cold. JAMA, J Am Med Assoc. 2020;323(8):707–708. doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 6.Zhao M., Veeranki S.P., Magnussen C.G., Xi B. Recommended physical activity and all cause and cause specific mortality in US adults: prospective cohort study. BMJ. 2020;370:2031. doi: 10.1136/bmj.m2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kovacs V., Starc G., Brandes M. Physical activity, screen time and the COVID-19 school closures in Europe - an observational study in 10 countries. Eur J Sport Sci. Published online. 2021 doi: 10.1080/17461391.2021.1897166. [DOI] [PubMed] [Google Scholar]
- 8.Karageorghis C., Bird J., Hutchinson J. Physical activity and mental well-being under COVID-19 lockdown: a cross-sectional multination study. BMC Publ Health. 2021;21(1) doi: 10.1186/S12889-021-10931-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO WHO guidelines on physical activity and sedentary behaviour. 2020. https://www.who.int/publications/i/item/9789240015128 [PubMed]
- 10.ACSM. Staying active during the coronavirus pandemic. 2020. https://www.exerciseismedicine.org/assets/page_documents/EIM_Rx for Health_ Staying Active During Coronavirus Pandemic.pdf
- 11.Chen P., Mao L., Nassis G.P., Harmer P., Ainsworth B.E., Li F. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Heal Sci. 2020;9(2):103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.COVID-19 Map - Johns Hopkins coronavirus Resource center. https://coronavirus.jhu.edu/map.html
- 13.Feter N., Caputo E.L., Doring I.R. Cold Spring Harbor Laboratory Press; 2020. Longitudinal Study about Low Back Pain, Mental Health, and Access to Healthcare System during COVID-19 Pandemic: Protocol of an Ambispective Cohort Short Title: PAMPA Cohort: Study Protocol. [DOI] [Google Scholar]
- 14.Milton K., Bull F.C., Bauman A. Reliability and validity testing of a single-item physical activity measure. Br J Sports Med. 2011;45(3):203–208. doi: 10.1136/bjsm.2009.068395. [DOI] [PubMed] [Google Scholar]
- 15.Enes C.C., Nucci L.B. A telephone surveillance system for noncommunicable diseases in Brazil. Public Health Rep. 2019;134(4):324–327. doi: 10.1177/0033354919848741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ding D., Mutrie N., Bauman A., Pratt M., Hallal P.R.C., Powell K.E. Physical activity guidelines 2020: comprehensive and inclusive recommendations to activate populations. Lancet. 2020;396(10265):1780–1782. doi: 10.1016/S0140-6736(20)32229-7. [DOI] [PubMed] [Google Scholar]
- 17.Ekelund U., Tarp J., Steene-Johannessen J. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019;366 doi: 10.1136/bmj.l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garmin The effect of the global pandemic on active lifestyles. https://www.garmin.com/en-US/blog/general/the-effect-of-the-global-pandemic-on-active-lifestyles/
- 19.Sánchez-Sánchez E., Ramírez-Vargas G., Avellaneda-López Y., Orellana-Pecino J.I., García-Marín E., Díaz-Jimenez J. Eating habits and physical activity of the Spanish population during the COVID-19 pandemic period. Nutrients. 2020;12(9):2826. doi: 10.3390/nu12092826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meyer J., McDowell C., Lansing J. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Public Health. 2020;17(18) doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Powell K.E., Paluch A.E., Blair S.N. Physical activity for health: what kind? how much? how intense? on top of what? Annu Rev Public Health. 2011;32:349–365. doi: 10.1146/annurev-publhealth-031210-101151. [DOI] [PubMed] [Google Scholar]
- 22.Hamer M., Kivimaki M., Gale C.R., Batty G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK. Brain Behav Immun. 2020. Published online. [DOI] [PMC free article] [PubMed]
- 23.Brazil. Vigilância de Fatores de Risco e Proteção Para Doências Crônicas Por Inquérito Telefônico. 2019. https://portalarquivos.saude.gov.br/images/pdf/2020/April/27/vigitel-brasil-2019-vigilancia-fatores-risco.pdf
- 24.Florindo A.A., Guimarães V.V., Cesar C.L.G., De Azevedo Barros M.B., Alves M.C.G.P., Goldbaum M. Epidemiology of leisure, transportation, occupational, and household physical activity: prevalence and associated factors. J Phys Act Heal. 2009;6(5):625–632. doi: 10.1123/jpah.6.5.625. [DOI] [PubMed] [Google Scholar]
- 25.Zanchetta L.M., Barros MB. de A., César C.L.G., Carandina L., Goldbaum M., Alves M.C.G.P. Physical inactivity and associated factors in adults, São Paulo, Brazil. Rev Bras Epidemiol. 2010;13(3) doi: 10.1590/S1415-790X2010000300003. [DOI] [PubMed] [Google Scholar]
- 26.Mulligan H.F., Hale L.A., Whitehead L., David Baxter G. Barriers to physical activity for people with long-term neurological conditions: a review study. Adapt Phys Act Q (APAQ) 2012;29(3):243–265. doi: 10.1123/apaq.29.3.243. [DOI] [PubMed] [Google Scholar]
- 27.Barker J., Smith Byrne K., Doherty A. Physical activity of UK adults with chronic disease: cross-sectional analysis of accelerometer-measured physical activity in 96 706 UK Biobank participants. Int J Epidemiol. 2019;48(4):1167–1174. doi: 10.1093/ije/dyy294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1
- 29.Caetano R., Silva A.B., Guedes A.C.C.M. Challenges and opportunities for telehealth during the COVID-19 pandemic: ideas on spaces and initiatives in the Brazilian context. Cad Saúde Pública. 2020;36(5) doi: 10.1590/0102-311X00088920. [DOI] [PubMed] [Google Scholar]
- 30.van Houten J.M., Kraaykamp G., Breedveld K. When do young adults stop practising a sport? An event history analysis on the impact of four major life events. Int Rev Sociol Sport. 2017;52(7):858–874. doi: 10.1177/1012690215619204. [DOI] [Google Scholar]
- 31.Bell S., Lee C. Emerging adulthood and patterns of physical activity among young Australian Women. Int J Behav Med. 2005;12(4):227–235. doi: 10.1207/s15327558ijbm1204_3. [DOI] [PubMed] [Google Scholar]