Abstract
In the early months of 2020, Europe was confronted by a pandemic that originated in China, which initially affected its territories in different ways. Parts of northern Italy were among the regions most affected. At the same time, Ticino, a small canton of Switzerland geographically wedged into Italian territory, had an incidence rate comparable to that of hard-hit Lombardy. Home to 350,000 inhabitants and separated from the rest of Switzerland by the Alps, Ticino had to face the first part of the pandemic with little available knowledge. The cantonal authorities decided to transform two active hospitals into COVID centres, concentrating all coronavirus patients there. Since the virus was new and there were no clear guidelines for managing it, the nutritional team on site had to reorganise to provide patient care, adapting their strategy to accommodate the evolution of the pandemic and growing medical knowledge. This paper explains how one of these teams developed a model to deal with the first wave of COVID, maintaining it during the second and current third wave of the pandemic.
Keywords: COVID-19, Pandemic, Nutritional risk score, Nutritional assessment, Bioelectrical impedance
Abbreviations: EOC, Ente Ospedaliero Cantonale; NRS 2002, Nutritional Risk Score 2002; ESPEN, European Society for Clinical Nutrition and Metabolism; BIVA, Bioimpedance vectorial phase angle
1. Introduction
For a long time, the world has struggled with a pandemic caused by an unknown viral agent. During the early months of 2020, Europe faced a pandemic that originated in China, which initially affected its various countries and territories in different ways. An initial lack of information on the global evolution of the virus, its morbidity/mortality, and the lack of effective therapies subjected the medical world to a severe test. This article describes the organisational process and nutritional approach adopted by a hospital in Switzerland to counteract SARS-CoV-2.
2. Methods
2.1. Setting
Towards the end of February 2020, some territories in Europe suddenly found themselves facing a new infectious disease, the new coronavirus, COVID 19, which originated in China and then spread rapidly to the rest of the world, becoming a pandemic [1]. Initially, scientific knowledge was scarce and there were no clear protocols for organising proper therapeutic care for hospitalised patients or managing patient flow within healthcare facilities. Northern Italy immediately became an epicentre of the pandemic in Europe [2,3]. During that initial period, Switzerland was unevenly affected. The Canton of Ticino, an Italian-speaking canton south of the Swiss Alps, was seriously affected [4] (Fig. 1 ), owing to its geographical position, wedged into Lombardia.
Fig. 1.
Geographical location of the Locarno Regional Hospital, a COVID centre in Switzerland.
In addition to geographical proximity, the two territories share a very high level of daily human contact. In fact, out of a resident population of around 350,000 inhabitants, more than 70,000 frontier workers enter Swiss soil every day [5,6]. Furthermore, the period in question coincided with the Canton of Ticino's Carnival school holidays (22 February to 1 March 2020), when contact between the populations of the two places normally increases, as people spend their holidays on the nearby peninsula.
Unsurprisingly, therefore, during the first wave of the pandemic, this territory had incidence and prevalence rates comparable to those of Lombardy and unlike the rest of Switzerland, as the Alps probably prevented the pandemic from spreading rapidly to the rest of the country. As there were no models available to cope with the pandemic, the cantonal political and health authorities had to restructure healthcare provision [7]. In particular, the clinical nutrition service had to reorganise itself to care for COVID patients at Locarno Regional Hospital, which became the reference hospital for patients suffering from SARS-Co19.
2.2. Description of the team structure in normal times
Switzerland has a federal health system, in which the federal central health authority leaves each canton ample room to handle inpatient care individually. Hospitals, whose cost coverage is guaranteed by compulsory health insurance (Lamal), are generally divided into public and private hospitals. In the pre-pandemic era, public-hospital healthcare in the Canton of Ticino was united within an institution (Ente Ospedaliero Cantonale-EOC), which incorporated several hospitals, spread out across the canton as a multisite hospital, with an overall capacity of 800 beds [8] (Fig. 1).
One of these hospitals, the Regional Hospital of Locarno, has an emergency room, an intensive-care service, and departments of internal medicine, geriatrics, surgery/traumatology, and gynaecology/obstetrics. There are also specific clinics for other specialties [8].
In 2017, a clinical and dietetic nutrition unit was created at the cantonal level and divided up among the various locations. In Locarno, the local nutrition team, which is part of the cantonal clinical nutrition service, is composed of a part-time doctor and three qualified dieticians, for a total work percentage of 270%.
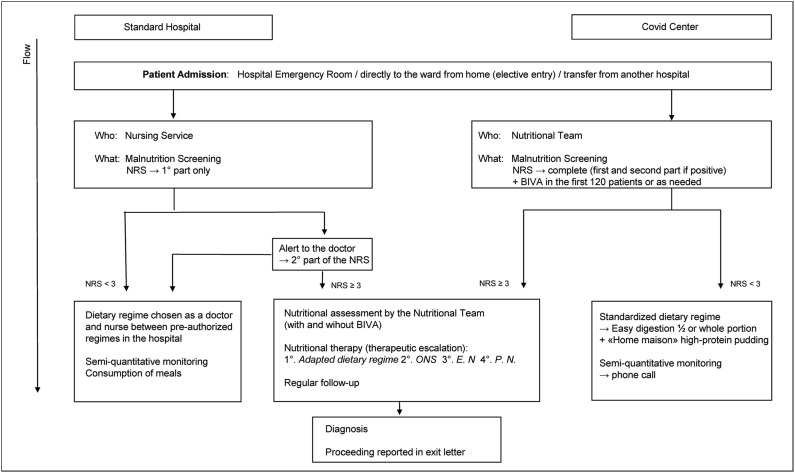
The nutrition team is responsible not only for supervising hospital dietetics through the catering service but also for caring for hospitalised patients. It actively intervenes in the care of malnourished patients, detected through Nutritional Risk Screening (NRS), which when the service was launched was made mandatory for all hospitalised patients. The tools were incorporated into each patient's computerised medical record [9]. The first part of each NRS screening is carried out by the patient's referral nurse; if the result is positive, the second part is completed by the doctor overseeing the patient. At the same time, if NRS ≥3, the nutrition service is automatically alerted, receiving the patient's computerised file (Fig. 2 ).
Fig. 2.
Flow of classic nutritional care compared to that implemented in the COVID Centre. Abbreviations: NRS, Nutritional Risk Score, BIVA, Bioimpedance Vectorial Phase Angle, O.N.S, Oral Nutritional Supplements, E. N., Enteral Nutrition, P.N. Parenteral Nutrition.
2.3. Changes made during the pandemic
As the pandemic advanced rapidly, the political and health authorities decided to convert an EOC public hospital in Locarno into a hospital entirely dedicated to SARS-CoV-2, with 250 beds and a private support hospital [5,7]. Maximum occupancy was reached on 30 March, with 415 patients hospitalised with SARS-CoV-2 throughout the Canton of Ticino, of whom 75 were in intensive care. Given the large number of hospitalisations and the need for patients to be invasively ventilated in intensive care, hybrid wards with designated “tracheostomised beds” were introduced during the first wave [5]. In Locarno hospital, equipment and medical and paramedical personnel were drawn from other hospitals as needed, expanding the number of intensive-care beds from the seven normally provided to a maximum of 45 beds during the first wave. Faced with the sudden reorganisation of an entire hospital, which, in just a few days, had found itself managing a new typology of cases with multiple unknowns (how to take charge and protect staff and patients, as well as many patients with serious anorexia, later found to be linked to SARS-CoV-2), the Nutrition Service was asked to take full responsibility for all nutritional care and to review operational protocols.
The initial problems detected by the Nutrition Service were as follows:
-
1.
The need to reduce the risk of infecting members of the nutrition team
-
2.
The need to overcome the fears of team members, who had to care for potentially infectious patients at their bedsides
-
3.
The need to care for a large number of new patients, admitted every day of the week (the maximum occupancy of the two hospitals in the canton was reached on 30 March 2020, with 415 patients hospitalised with SARS-CoV-2; 75 of these required intensive care) [7].
-
4.
The disruption of known and well-established care; the elimination of the physical bedside presence of catering personnel, offering patients a choice of menu. The nutrition team carried out malnutrition screening to relieve the nurses' workload.
-
5.
An initial lack of guidelines for medical nutrition treatment of SARS-CoV-2 patients
The approach adopted to address the problem.
-
1.
Operator safety management. The entire team received instructions on protective measures, based on the recommendations of Swissnoso and provided by the hospital hygiene service [10]. The training covered various topics, from the correct way to wear personal protective equipment (mask, goggles, gown, gloves, and hat) to methods of disinfecting both hands and materials (including writing implements and tablets).
-
2.
In the beginning, members of the team were worried and some raised doubts about the advisability of contact with infected patients while carrying out activities previously performed by others. To address this problem and prepare for cases of illness, given that the work had to be carried out seven days a week, the team brought in a doctor from another hospital in the network. This colleague spent time with the team, briefing members on up-to-date scientific knowledge and providing reassurance that their protective measures would be effective.
-
3.
Before the pandemic, the hospital cared for patients 24 h a day and seven days a week, with administrative services, outpatient activities, and dietary counselling closed on the weekend. To cope with the regular and significant influx of COVID patients, the hospital initiated a seven-day-a-week routine and increased the number of dieticians accordingly, as did the team.
-
4.
To reduce the risk of contagion, the physical bedside presence of a catering attendant was suspended. Inpatient dietetics were simplified and reduced to one default easy-to-digest regime for every patient. A member of the nutrition team visited each patient in his/her room, changing the patient's profile to accommodate allergies or intolerances, if necessary, and carrying out malnutrition screening. Patients who screened positive for malnutrition were monitored via telephone if they were able to cooperate (Fig. 2).
-
5.
Initially, the ESPEN guidelines were followed when caring for polymorphous or intensive-care patients. As soon as more specific guidelines were published, they were followed instead and handed down to different departments [11,12].
2.4. Intensive care
Initially, this service worked with the pharmacy to maintain a stock of artificial nutrients used under normal conditions. It looked for alternatives to specific enteral nutrient formulations that were running low or might not be supplied on a regular basis. As the pandemic evolved, various members of the intensive-care team were educated and informed about new nutritional guidelines, which were gradually published, making it possible to achieve a certain degree of autonomy in nutritional prescriptions. In particular, during the first wave of COVID, many patients suffered from diarrhoea, which made it difficult for them to reach the caloric targets established by the formulas. During the second and third waves, patients experienced hyperglycaemia, brought on by massive use of steroids. This was managed using enteral formulations adapted for diabetes. As soon as the ESPEN guidelines for patient care were published, they were forwarded to team members and other colleagues [13]. Given the unit's limited resources, the nutrition team provided support only for extremely needy individual patients at the explicit request of intensive-care colleagues.
2.5. Tracheostomy ward
To free up ICU beds while continuing to perform invasive ventilation, percutaneous tracheotomies were performed systematically by surgeons, supported by pneumologists [5]. In this department, the nutrition team visited daily to evaluate patients, initiate nutrition programmes, and modify or adapt those programmes as the illness evolved, following the weaning programme established by a team consisting of speech therapists, pulmonologists, and physiotherapists.
2.6. Care wards
Initially, as previously mentioned, unnecessary contact between the treatment team and patients was reduced to minimise the risk to staff members. Once it was noted that almost all patients experienced a significant lack of appetite, partly due to the disease and partly due to anosmia and ageusia, individual patients were no longer visited by catering staff but directly by members of the nutrition team. The decision was made to standardise the diet served to patients, creating one easy-to-digest regime (a half portion per patient) combined with a high-protein pudding made by the kitchen on site (12 g/protein).
Each new admission was seen by a member of the nutrition team, who made an initial assessment, including nutritional risk screening (NRS) for malnutrition, adapted the default regime if necessary, and instructed the patient to try to consume the energy/protein parts of the diet. The nutritionist informed patients who were not too seriously ill that their next consultations would take place by telephone. As most patients had little appetite, the NRS results were almost always positive, and many patients were subjected to a bioelectrical impedance vector analysis (BIVA) to better understand the problem. Although a post-hoc analysis showed that the results lacked usefulness in relation to the NRS score, it did show excellent specificity [14].
3. Discussion and teaching
During the first few weeks, when the nursing staff was overburdened and doctors were trying to understand how to treat patients who were rapidly deteriorating, the nutrition team was able to take complete, autonomous responsibility for the nutritional care of patients. The team found itself managing a massive number of patients and screening almost all of them for malnutrition. It is striking that despite direct contact with patients through the execution of more than 100 bio-impedances – as well as remote contact (collecting data in the patient's room, screening for malnutrition, and bedside re-consultations for some malnourished patients, depending on the course of the illness) – no member of the nutrition team developed COVID symptoms or required hospitalisation. This shows that with suitable protection and pre-knowledge, the dietary management of COVID patients can be carried out normally. It is also clear that body composition analyses using vector bio-impedance (BIVA) can be carried out without subjecting staff members to a high risk of infection, as long as the correct hygiene measures and appropriate protective materials are used. However, the usefulness of BIVA in COVID patients is yet to be proven. The team, faced with new case histories, initially carried out these analyses to see whether they could provide an extra parameter for determining which patients were getting worse and needed to be transferred to intensive care. It was immediately clear that BIVA was no better than NRS and did not provide added value; for this reason, it was discontinued [14].
The screenings carried by the team detected a high number of patients suffering from malnutrition, enabling the provision of essential care. Members of the team felt that they were an integral part of the patient-care process, alongside other professionals – a somewhat unusual situation. This sense of engagement motivated the team greatly, helping members cope with the enormous amount of work they had to undertake.
This study also shows that, in a crisis, patients will accept reduced levels of comfort, such as a less varied or appealing menu. As discussed, the meals provided to patients with no need for artificial nutrition were reduced to single, light, easy-to-digest regime that included a high-protein pudding, prepared in-house by cooks in the hospital's dietetics department. This simplified meal made it possible for catering staff to avoid entering patient rooms, thus reduced pressure on the kitchen. Although the pudding was slightly lower in protein than an oral supplement, it was highly appreciated by those patients who, in addition to being anorexic due to the disease, were often presented with anosmia, a previously unrecognised symptom that was later identified in the literature as specific to the COVID-19 infection [15]. The problem was reduced during the second wave when the massive use of corticosteroids reduced the presence of anorexia. Pandemic-related data drawn from other settings, such as palliative care, have not yet been well analysed [16].
Finally, this new pandemic has allowed us to test the readiness of bodies responsible for medical nutrition to issue guidelines for patient care. Surely, the test has been passed by a wide margin, both by ESPEN [12,17] and by national companies. Without dismissing others, it is worth noting the success of French medical bodies for their complete coverage of all aspects of SARS-CoV-2 [17].
4. Conclusion
During an acute overload of hospital facilities, a structured nutrition team was able to take complete and autonomous control of the management of hospital nutrition, screening for and resolving malnutrition, and relieving other health workers. Nutritional care can be delivered safely at patient bedsides with no restrictions, as long as team members use the necessary protection.
Funding
The authors did not receive any grants from funding agencies in the public, commercial, or not-for-profit sectors for this manuscript.
Author contributions
Rosamaria Turri Quarenghi, Massimo Quarenghi: Conceptualisation, Methodology, Draft Writing- Original draft preparation; Massimo Quarenghi: Supervision; Marta Gavazzoni, Dario Bertolotti, Nicola Ossola: Writing, reviewing, and editing.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
References
- 1.Liu Yen-Chin, Kuo Rei-Lin, Shih Shin-Ru. COVID-19: the first documented coronavirus pandemic in history. Biomed J. 2020;43(4):328–333. doi: 10.1016/j.bj.2020.04.007. ISSN 2319-4170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sebastiani G., Massa M., Riboli E. Covid-19 epidemic in Italy: evolution, projections and impact of government measures. Eur J Epidemiol. 2020 Apr;35(4):341–345. doi: 10.1007/s10654-020-00631-6. Epub 2020 Apr 18. PMID: 32306149; PMCID: PMC7165256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Romagnani P., Gnone G., Guzzi F., Negrini S., Guastalla A., Annunziato F., et al. The COVID-19 infection: lessons from the Italian experience. J Publ Health Pol. 2020 Sep;41(3):238–244. doi: 10.1057/s41271-020-00229-y. PMID: 32472024; PMCID: PMC7257358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Repubblica e Cantone del Ticino . 2020. Bollettino epidemiologico 05.06.2020.https://www4.ti.ch/dss/dsp/covid19/%20home/ [Google Scholar]
- 5.Forni R., Besana T., Amitrano A., Voinea C., Ogna A. Ventilatory weaning and early rehabilitation in COVID-19-related acute respiratory distress syndrome: the experience at Locarno hospital, canton of Ticino, Switzerland. Swiss Med Wkly. 2020 Nov 12;150:w20397. doi: 10.4414/smw.2020.20397. PMID: 33180953. [DOI] [PubMed] [Google Scholar]
- 6.Confederazione Svizzera Ufficio Federale di Statistica UST. https://www.bfs.admin.ch/bfs/it/home/statistiche/lavoro-reddito/attivita-professionale-orario-lavoro/occupati/svizzeri-stranieri/frontalieri.html
- 7.Republica e cantone Ticino, messaggio 7893. 2020. https://m3.ti.ch/COMUNICAZIONI/188762/M7893.%20pdf Published 2020. [Google Scholar]
- 8.Ente ospedaliero Cantonale . 2021. Ospedali e Istituti.https://www.eoc.ch/Ospedali-e-Istituti.html Published 2021. [Google Scholar]
- 9.Cederholm T., Barazzoni R., Austin P., Ballmer P., Biolo G., Bischoff S.C., et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49–64. doi: 10.1016/j.clnu.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Swissnoso Microsoft Word - 210329_Control of healthcare-associated COVID-19 outbreaks_V2.0 (swissnoso.ch).
- 11.Gomes Filomena, Schuetz Philipp, Bounoure Lisa, Austin Peter, Ballesteros-Pomar María, Cederholm Tommy, et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clin Nutr. 2018;37(Issue 1):336–353. doi: 10.1016/j.clnu.2017.06.025. ISSN 0261-5614. [DOI] [PubMed] [Google Scholar]
- 12.Barazzoni R., Bischoff S.C., Krznaric Z., Pirlich M., Singer P. Endorsed by the ESPEN Council, Espen expert statements and practical guidance for nutritional management of individuals with sars-cov-2 infection. Clin Nutr. 2020 doi: 10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singer Pierre, Blaser Annika Reintam., Berger Mette M., Alhazzani Waleed, Calder Philip C., Casaer Michael P., Hiesmayr Michael, Mayer Konstantin, Montejo Juan Carlos., Claude Pichard, Preiser Jean-Charles, Arthur R., van Zanten H., Simon Oczkowski, Szczeklik Wojciech, Bischoff Stephan C. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1) doi: 10.1016/j.clnu.2018.08.037. [DOI] [PubMed] [Google Scholar]
- 14.Del Giorno R., Quarenghi M., Stefanelli K., Capelli S., Giagulli A., Quarleri L., et al. Nutritional risk screening and body composition in COVID-19 patients hospitalized in an internal medicine ward. Int J Gen Med. 2020 Dec 23;13:1643–1651. doi: 10.2147/IJGM.S286484. PMID: 33380822; PMCID: PMC7767704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gori A., Leone F., Loffredo L., Cinicola B.L., Brindisi G., De Castro G., et al. COVID-19-Related anosmia: the olfactory pathway hypothesis and early intervention. Front Neurol. 2020;11:956. doi: 10.3389/fneur.2020.00956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Childs D.S., Jatoi A. A hunger for hunger: a review of palliative therapies for cancer-associated anorexia. Ann Palliat Med. 2019 Jan;8(1):50–58. doi: 10.21037/apm.2018.05.08. Epub 2018 May 24. PMID: 29860861; PMCID: PMC6252156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Recommandation, Avis d’experts Covid-19 de Société Francophone Nutrition Clinique et Métabolisme (SFNCM) https://www.sfncm.org/outils-education/recommandations/procedures-covid-19