Abstract
Outcomes following different types of surgical intervention for femoroacetabular impingement (FAI) are well reported individually but comparative data are deficient. The purpose of this study was to conduct a systematic review (SR) and meta-analysis to analyze the outcomes following surgical management of FAI by hip arthroscopy (HA), anterior mini open approach (AMO), and surgical hip dislocation (SHD). This SR was registered with PROSPERO. An electronic database search of PubMed, Medline, and EMBASE for English and German language articles over the last 20 years was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We specifically analyzed and compared changes in patient-reported outcome measures (PROMs), α-angle, rate of complications, rate of revision, and conversion to total hip arthroplasty (THA). A total of 48 articles were included for final analysis with a total of 4,384 hips in 4,094 patients. All subgroups showed a significant correction in mean α angle postoperatively with a mean change of 28.8° (95% confidence interval (CI) 21 to 36.5; p < 0.01) after AMO, 21.1° (95% CI 15.1 to 27; p < 0.01) after SHD, and 20.5° (95% CI 16.1 to 24.8; p < 0.01) after HA. The AMO group showed a significantly higher increase in PROMs (3.7; 95% CI 3.2 to 4.2; p < 0.01) versus arthroscopy (2.5; 95% CI 2.3 to 2.8; p < 0.01) and SHD (2.4; 95% CI 1.5 to 3.3; p < 0.01). However, the rate of complications following AMO was significantly higher than HA and SHD. All three surgical approaches offered significant improvements in PROMs and radiological correction of cam deformities. All three groups showed similar rates of revision procedures but SHD had the highest rate of conversion to a THA. Revision rates were similar for all three revision procedures.
Keywords: Femoroacetabular impingement, Surgical approach, Outcomes, femoroacetabular impingement, patient-reported outcome measures (PROMs), arthroscopic treatment, surgical hip dislocation, hips, cam deformities, surgical approaches, hip arthroscopy, total hip arthroplasty (THA), Medline
Article focus
Outcomes following different types of surgical intervention for femoroacetabular impingement (FAI) are well reported individually but comparative data are deficient.
The purpose of this study was to conduct a systematic review (SR) and meta-analysis to analyze the outcomes following surgical management of FAI by hip arthroscopy (HA), anterior mini open approach (AMO), and surgical hip dislocation (SHD).
Key messages
All three procedures showed a significant correction in mean α-angle postoperatively.
All three surgical approaches offered significant improvements in PROMs and radiological correction of cam deformities.
Revision rates were similar for all three revision procedures, but rate of complications following AMO was significantly higher than arthroscopy and SHD.
Strengths and limitations
Strengths include being the first SR and meta-analysis comparing different surgical treatment options for the management of FAI.
Limitations include the small number of included studies, especially for AMO and SHD, and the fact that different surgeons may have different thresholds for the different surgical techniques assessed in this review.
Introduction
Femoroacetabular impingement (FAI) was first described in 1999 by Myers et al1 as an abnormal abutment between the femoral head-neck junction and the acetabulum.1,2 It has two distinct forms: a pincer type with acetabular over-coverage; and a cam type with an abnormal contour of the femoral head-neck junction. In addition, FAI can also occur as a mixed type, having features of both the cam and pincer.3 These osseous abnormalities can lead to damage of the chondrolabral junction and eventually osteoarthritis (OA).4
The goal of surgical intervention in patients with symptomatic FAI is hip preservation. This is achieved by correcting the morphological abnormality and then addressing the resultant damage to the labrum and the articular cartilage. Ganz et al5 described the surgical treatment of FAI using the open surgical hip dislocation (SHD) approach via the trochanteric flip osteotomy in 2001. Advances in surgical technique led to the development of an anterior mini open (AMO) approach and eventually an arthroscopic approach, which has grown exponentially over the last decade.6,7 Additionally, some authors have also used a combined AMO and arthroscopic approach to address FAI.8
While SHD was once considered the gold-standard treatment for FAI, hip arthroscopy (HA) has caught up rapidly and is currently the preferred approach,9,10 being used more frequently around the world.6 The individual outcomes of these approaches have been reported but comparative data are limited. Matsuda et al11 and Botser et al12 have both published systematic reviews including SHD, AMO, and arthroscopic approaches but unfortunately a detailed meta-analysis on the outcomes was lacking in both these studies. Therefore, the purpose of our study was to perform a systematic review and meta-analysis to analyze the outcomes following the use of either SHD, AMO, or arthroscopy in the surgical management of primary FAI with follow-up of > 12 months.
Methods
Search strategy
This systematic literature review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.13 A protocol for this review was registered with PROSPERO: CRD42020206428. An electronic database search for English and German language articles from the last 20 years was carried out using PubMed, EMBASE (Ovid), and Medline (Ovid) on 8 June 2020. The following search terminology was used in each database: [FAI OR Femoroacetabular impingement] AND [surgical hip dislocation OR open hip surgery OR open surgical dislocation OR open dislocation OR arthroscop* OR mini anterior OR mini open OR hueter]. Bibliographies of past systematic reviews and included articles were also analyzed for further potential articles.
Identification of eligibility
Inclusion and exclusion criteria are outlined in Table I. Two authors independently screened articles for inclusion via the title and abstract initially before the screening of full-text articles. Any discrepancies were discussed in a consensus meeting.
Table I.
Inclusion and exclusion criteria.
| Inclusion criteria |
|---|
| Studies reporting surgical outcome for FAI Studies reporting complications after FAI surgery Original studies including retrospective and prospective cohort studies and RCTs Studies reported in English or German language Studies within the last 20 yrs Mean patient population age > 18 or < 60 yrs Average follow-up > 12 mths |
| Exclusion criteria |
| Non-FAI patient population Studies involving revision cases, secondary FAI (i.e. Perthes' disease, slipped capital femoral epiphysis), Tönnis grade > 2, or dysplasia Studies emphasizing periacetabular osteotomy or chondrolabral surgery without osteoplasty Case reports Studies that were not original (e.g. systematic reviews, narrative reviews, technical notes) Studies that were not reported in the English or German Language Average follow-up of < 12 mths Mean patient population age < 18 or > 60 yrs Duplicate cohorts |
FAI, femoroacetabular impingement; RCT, randomized controlled trial.
Data extraction and quality appraisal
The quality of each article was assessed by two independent authors (DA and JZ) using the methodological index for non-randomized studies (MINORS) with eight questions for cohort studies and a further four questions if the study was a comparative one.14 Any disagreements between reviewers were discussed in a consensus meeting and a third independent author (MP) was consulted if an agreement could not be met. Quality assessment of the studies was performed using the MINORS score, which is made up of eight items for non-comparative studies and an additional four items for comparative studies. Each item is given a score of 0 to 2, which helps in rating the studies as either very low quality, low quality, fair quality, or high quality.14,15 The scores for non-comparative studies were as follows: 0 to 4 very low quality; 5 to 8 low quality; 9 to 12 fair quality; and 13 to 16 high quality. For comparative studies, the scores were 0 to 6 very low quality; 7 to 12 low quality; 13 to 18 fair quality; and 19 to 24 high quality.15
The level of evidence was assessed by the criteria published by the Oxford Centre for Evidence-Based Medicine.16 Patient demographic details, surgical procedure, pre- and postoperative α angle and patient-reported outcome measures (PROMs), complication rates, reoperation rates, and rates of conversion to THA were extracted from each article to be included. Pooled estimates were calculated for these outcomes and were summarized in forest plots.
Data for continuous variables of interest were presented in an alternative format to mean and standard deviation (SD) in the studies. We estimated the SD following guidelines from the Cochrane handbook, and using equations from Wan et al.17
Meta-analysis
All meta-analyses were conducted using R 4.0.0 software (R Foundation for Statistical Computing, Austria). Mixed effects subgroup analysis was conducted. Data were pooled within groups using random effects meta-analysis, with restricted maximum likelihood estimation of between-study variance and the inverse variance weighting. Heterogeneity was assessed using I2. Heterogeneity was classified as either low (I2 < 25%), moderate (I2 25% to 75%), or high (I2 > 75%).18 Between group differences were identified using the Q test for heterogeneity.
Meta-analysis for patient-reported outcome measures
Primary analysis was of multidimensional PROMs in minimally important difference (MID) units. If PROMs were reported in individual dimensions as subscales, they were combined as described in the literature for an overall score. This precluded studies which reported the Copenhagen Hip and Groin Outcome Scores (HAGOS), as the individual subscales could not be combined into an overall score. Only PROMs validated for hip arthroscopy were included in this meta-analysis; a larger body of evidence is available regarding the outcomes of hip arthroscopy in young adults, additionally, scores validated for hip arthroscopy typically focus towards younger, more active patients, which reflects the population of interest.19 Conversion to MID units was achieved by dividing the PROM score by the most conservative minimum clinically important difference value (MCID) reported in the literature (Table II).20-24
Table II.
Minimum clinically important difference units used for each patient-reported outcome measure.
| PROM | MCID unit |
|---|---|
| HOS-ADL | 920 |
| HOS-SSS | 14.521 |
| mHHS | 8.221 |
| HOOS pain | 923 |
| HOOS symptoms | 923 |
| HOOS ADL | 623 |
| HOOS sport and recreation | 1023 |
| HOOS QoL | 1123 |
| iHOT-33 | 1221 |
| iHOT-12 | 922 |
| NAHS | 1024 |
HOOS-ADL, Hip disability and osteoarthritis outcome score - Activities of Daily Living; HOOS-QoL, Hip disability and osteoarthritis outcome score - Quality of Life; HOS-ADL, Hip Outcome Score - Activities of Daily Living; HOS-SSS, Hip Outcome Score - Sport Specific Subscales; iHOT, International Hip Outcome Tool; MCID, minimal clinically important difference; mHHS, modified Harris Hip Score; NAHS, Non Arthritic Hip Score; PROM, patient-reported outcome measure.
In studies which reported multiple PROMs, we chose to use the one most valid for the treatment of FAI. In accordance with the Warwick agreement, where iHOT and HOS scores are recommended, these scores were chosen to represent the study in the primary PROM analysis. If both the iHOT and HOS scores were used, for convenience the iHOT was prioritized.23 If none of these scores were present, we then chose to use the NAHS, mHHS, and HOOS scores respectively in order of preference due to their construct validity in measuring outcomes for FAI.22
Sensitivity analysis was conducted for MID meta-analyses using standardized mean difference (SMD) between preoperative and postoperative scores. Secondary analysis of PROMs in each dimension was not feasible, as the SHD group only reported multidimensional scores, and the AMO group only reported single-dimension PROMs in two studies. Meta-regression was conducted with mean follow-up period as a covariate to establish whether differing follow-up times had introduced heterogeneity or between group differences into the results.
Meta-analysis for the α angle
The mean difference between pre- and postoperative α angles was pooled and compared between groups. Sensitivity analysis was conducted using SMD to account for variation in α angle reported from the different radiological techniques employed in the included studies.24
Meta-analysis for rates of revision, complications, and conversion to total hip arthroplasty
The proportion of cases undergoing revision, complications, and conversion to THA were pooled and compared between groups. For pooling calculations, the proportional data were transformed using the Freeman–Tukey double-arcsine transformation, before transformation back to proportions for presentation. This approximates the data to a normal distribution and has an increased accuracy when handling zero events.25
Results
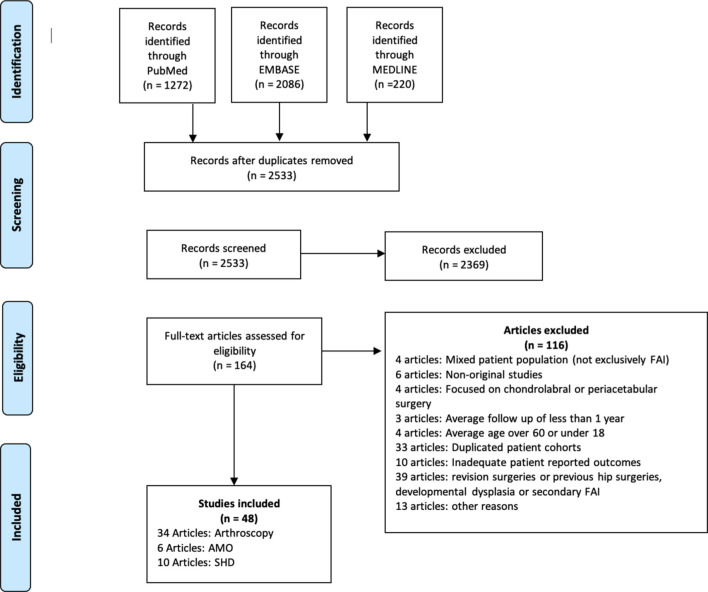
A total of 2,533 relevant titles were obtained after duplicate removal. No additional articles were found through bibliography searches. A thorough screening of title and abstracts was performed, leaving 164 articles suitable for full-text review. The PRISMA chart is shown in Figure 1. Only the most recent study was included where articles had potentially overlapping cohorts, and any article identified in German literature that was duplicated in English literature was not included for further analysis. A total of 48 articles met the inclusion criteria and were included for the final analysis (Table III). The individual MINORS scores for each study included are presented in Supplementary Tables i and ii. The levels of evidence and study characteristics are shown in Table III.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart of study selection process. AMO, anterior mini open approach; FAI, femoroacetabular impingement; SHD, surgical hip dislocation.
Table III.
Included studies.
| Study | Year | Time | Type of study | Level of evidence | Location | Patients, n | Hips, n | Male, n | Female, n | Mean age, yrs | Follow-up, mths |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Arthroscopy | |||||||||||
| Kunze et al26 | 2020 | Retrospective | Comparative trial | 3 | USA | 310 | 310 | 120 | 190 | 34 | 60 |
| Lindmann et al27 | 2020 | Prospective | Case series | 4 | Sweden | 64 | 84 | 52 | 12 | 24 | 60 |
| Öhlin et al28 | 2020 | Prospective | Case series | 4 | Sweden | 184 | 225 | 110 | 74 | 38 | 60 |
| Ortiz-Declet et al29 | 2020 | Prospective | Case series | 4 | USA | 34 | 34 | 15 | 19 | 20.8 | 47.4 |
| Bolia et al30 | 2019 | Retrospective | Comparative trial | 3 | USA | 99 | 126 | 72 | 54 | 38 | 87.6 (SD 32.4) |
| Hassebrock et al31 | 2019 | Retrospective | Comparative trial | 3 | USA | 133 | 133 | 47 | 86 | 31.96 | 24 |
| Kierkegaard et al32 | 2019 | Prospective | Cohort study with a cross-sectional comparison | 3 | Denmark | 56 | 72 | 24 | 32 | 36 | 12 |
| Perets et al33 | 2019 | Prospective | Case series | 4 | USA | 295 | 327 | 108 | 219 | 32.4 | 68.7 |
| de Girolamo et al34 | 2018 | Retrospective | Comparative trial | 3 | Italy | 109 | 109 | 64 | 54 | 39.3 and 38.3 | 96 |
| Kaldau et al35 | 2018 | Retrospective | Case series | 4 | Denmark | 84 | 84 | 45 | 39 | 40.4 | 82.9 |
| Mansell et al36 | 2018 | Prospective | RCT | 1 | USA | 66 | 66 | 39 | 21 | 30.3 | 24 |
| Tahoun et al37 | 2018 | Prospective | Case series | 4 | Egypt | 23 | 23 | 18 | 5 | 40.9 | 38.4 (SD 7.0) |
| Zimmerer et al38 | 2018 | Prospective | Case series | 4 | Germany | 43 | 43 | 31 | 12 | 25 | 24.4 |
| Menge et al39 | 2017 | Retrospective | Comparative trial | 3 | USA | 154 | 154 | 80 | 74 | 40.6 | 120 |
| Murata et al40 | 2017 | Retrospective | Comparative trial | 3 | Japan | 74 | 74 | 43 | 31 | 28.3 and 39.7 | 24 |
| Tjong et al41 | 2017 | Prospective | Case series | 4 | USA | 86 | 106 | 36 | 50 | 38.1 | 37.2 |
| Degen et al42 | 2016 | Retrospective | Case series | 4 | USA | 70 | 86 | 70 | 0 | 22.5 | 16.8 |
| Hufeland et al43 | 2016 | Retrospective | Case series | 4 | Germany | 44 | 44 | 24 | 20 | 34.3 | 66.3 (SD 14.5) |
| Joseph et al44 | 2016 | Prospective | Cohort study | 2 | USA | 64 | 64 | 19 | 45 | 31.6 and 31.1 | 24 |
| Dippmann et al45 | 2014 | Prospective | Case series | 4 | Denmark | 76 | 76 | 27 | 49 | 38 | 12 |
| Gicquel et al46 | 2014 | Prospective | Case series | 4 | France | 51 | 53 | 19 | 32 | 31 | 55.2 (50.4 to 66) |
| Gupta et al47 | 2014 | Prospective | Case series | 4 | USA | 47 | 47 | 28 | 19 | 37 | 28.32 (24 to 41) |
| Nielsen et al48 | 2014 | Prospective | Case series | 4 | Denmark | 117 | 117 | 48 | 69 | 37 | 40 (24 to 60) |
| Domb et al49 | 2013 | Prospective | Matched-pair comparative study | 2 | USA | 20 | 20 | 4 | 16 | 19.6 | 25.5 |
| Krych et al50 | 2013 | Prospective | RCT | 1 | USA | 36 | 36 | 0 | 36 | 38 and 39 | 32 (12 to 48) |
| Malviya et al51 | 2013 | Prospective | Case series | 4 | UK | 80 | 92 | 50 | 30 | 35.7 | 16.8 (12 to 21.6) |
| Zingg et al52 | 2013 | Prospective | Comparative trial | 3 | Switzerland | 23 | 23 | 18 | 5 | 27.6 | 12 |
| Larson et al53 | 2012 | Prospective | Cohort study | 3 | USA | 90 | 94 | 56 | 38 | 32 and 28 | 42 (24 to 72) |
| Palmer et al54 | 2012 | Prospective | Case series | 4 | USA | 185 | 201 | 99 | 102 | 40.2 | 46 |
| Philippon et al55 | 2012 | Prospective | Case series | 4 | USA | 153 | 153 | 72 | 81 | 57 | 35.7 (12 to 64) |
| Byrd and Jones56 | 2011 | Prospective | Case series | 4 | USA | 200 | 200 | 148 | 52 | 28.6 | 24 |
| Haviv et al57 | 2010 | Retrospective | Case series | 4 | Israel | 166 | 170 | 132 | 34 | 37 | 22 (12 to 72) |
| Horisberger et al58 | 2010 | Prospective | Case series | 4 | Switzerland | 88 | 105 | 60 | 28 | 40.9 | 27.6 (15.6 to 49.2) |
| Philippon et al59 | 2009 | Prospective | Case series | 4 | USA | 112 | 112 | 50 | 62 | 40.6 | 27.6 (24 to 34.8) |
| AMO approach | |||||||||||
| Skowronek et al60 | 2017 | Retrospective | Cohort study | 4 | Poland | 39 | 39 | 25 | 14 | 29.3 | 45 (24 to 55) |
| Ezechieli et al61 | 2016 | Prospective | Comparative trial | 3 | A - Germany B - Italy |
72 | 72 | 38 | 34 | A - 36 B - 28.5 |
15 (6 to 24) |
| Srinivasan et al62 | 2013 | Retrospective | Cohort study | 4 | UK | 25 | 26 | 11 | 15 | 31.3 | 22.3 |
| Chiron et al63 | 2012 | Prospective | Cohort study | 4 | France | 106 | 118 | 92 | 16 | 34.4 | 26.4 (12 to 54) |
| Ribas et al64 | 2010 | Prospective | Cohort study | 4 | Spain | 105 | 107 | 79 | 38 | 37 | 12 |
| Nepple et al65 | 2009 | Retrospective | Comparative trial | 3 | USA | 25 | 25 | 17 | 8 | 33 | 20.4 |
| SHD | |||||||||||
| Kockara et al66 | 2018 | Retrospective | Cohort study | 4 | Turkey | 33 | 34 | 19 | 14 | 34.5 | 72 |
| İnan et al67 | 2016 | Retrospective | Cohort study | 4 | Turkey | 21 | 22 | 7 | 14 | 33.8 | 48 |
| Hingsammer et al68 | 2015 | Retrospective | Cohort study | 4 | Switzerland | 23 | 30 | 18 | 5 | 24.3 | 19.2 (9.6 to 36) |
| Steppacher et al69 | 2014 | Retrospective | Cohort study | 4 | Switzerland | 75 | 97 | 55 | 42 | 32 | 72 (60 to 84) |
| Domb et al49 | 2013 | Prospective | Comparative trial | 3 | USA | 10 | 10 | 2 | 8 | 19 | 24.8 |
| Zingg et al52 | 2013 | Prospective | Comparative trial | 3 | Switzerland | 15 | 15 | 11 | 4 | 28.9 | 12 |
| Jäger et al70 | 2011 | Prospective | Cohort study | 4 | Germany | 21 | 21 | 7 | 15 | 36.3 | 12 |
| Naal et al71 | 2011 | Retrospective | Cohort study | 4 | Switzerland | 22 | 30 | 22 | 0 | 19.7 | 45.1 (12 to 79) |
| Yun et al72 | 2009 | Retrospective | Cohort study | 4 | South Korea | 14 | 15 | 12 | 2 | 35.8 | 27.6 (12 to 120) |
| Espinosa et al73 | 2006 | Retrospective | Comparative trial | 3 | Switzerland | 52 | 60 | 33 | 19 | 30 | 24 |
AMO, anterior mini open approach; RCT, randomized controlled trial; SD, standard deviation; SHD, surgical hip dislocation.
Patient characteristics
A total of 4,384 hips in 4,094 patients were included in this review. Patient characteristics for each treatment modality are presented in Table IV.
Table IV.
Patient characteristics.
| Variable, n | Arthroscopy | AMO approach | SHD |
|---|---|---|---|
| Articles | 34 | 6 | 10 |
| Patients | 3,436 | 372 | 286 |
| Hips | 3,663 | 387 | 334 |
| Male/female | 1,828/1,681 | 262/125 | 186/123 |
AMO, anterior mini open; SHD, surgical hip dislocation.
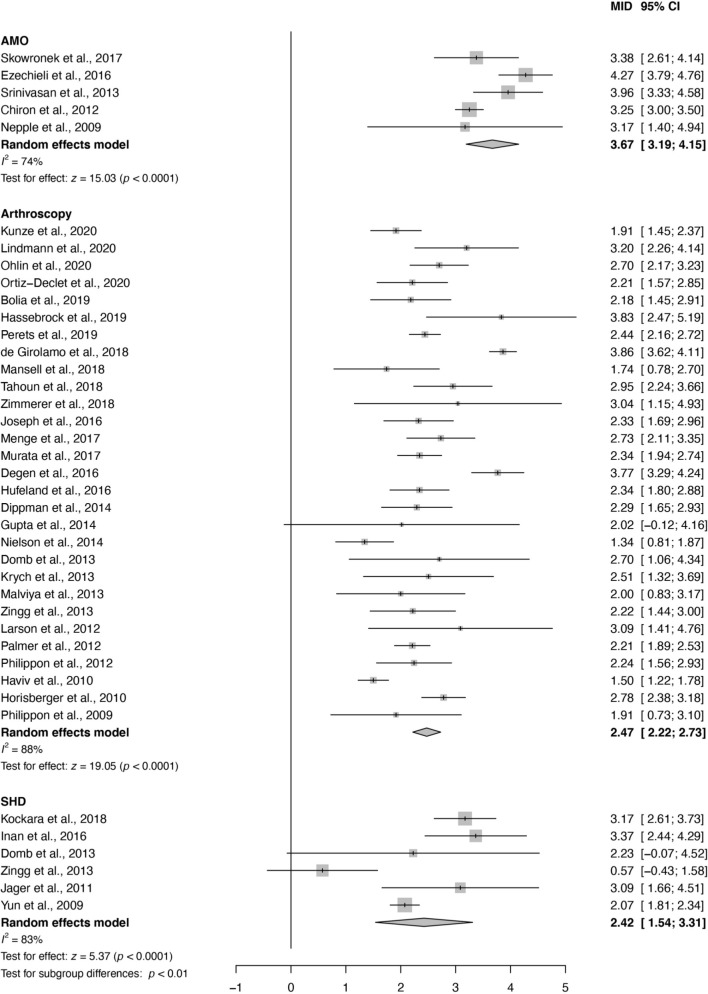
Patient-reported outcome measures
All subgroups reported a significant increase in PROMs. The AMO group showed a significantly higher increase in PROMs versus arthroscopy (Q 18.731, df 1, p < 0.001) and SHD (Q 5.893, df 1, p = 0.015) (Figure 2). This was most likely due to higher postoperative PROMs rather than to selection of patients with lower preoperative PROMs. No significant difference was observed between groups in post-hoc comparison of preoperative PROM values (Q 2.583, df 2, p = 0.275), although a significant difference between groups was found between postoperative PROMs (Q 9.690, df 2, p = 0.008). Individual preoperative and postoperative group comparisons are presented in Supplementary Table iii. Heterogeneity was high in arthroscopy and SHD groups, but moderate in the AMO group, despite normalization of PROMs to MCID units. Sensitivity analysis confirmed that there was a significant difference between the AMO and arthroscopy groups, although not between the AMO and SHD groups (Supplementary Table iv). This reflects the significant increase in postoperative PROMs between the AMO and arthroscopy groups (Supplementary Table iii).
Fig. 2.
Mean difference between pre- and postoperative patient-reported outcome measures (PROMs) expressed as minimally important difference (MID) units. AMO, anterior mini open approach; CI, confidence interval; SHD, surgical hip dislocation.
Furthermore, differing lengths of follow-up were investigated as a covariate within the PROM meta-analysis through post-hoc meta-regression. Follow-up period was not significantly associated with PROMs (p = 0.641; Supplementary Figure a).
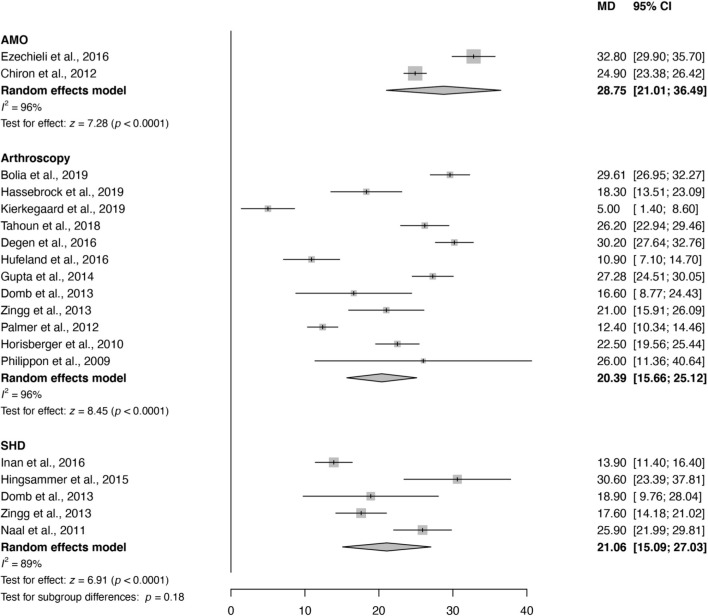
α angle
All subgroups showed a significant decrease in the mean α angle postoperatively. All subgroups showed high heterogeneity. There was no difference between groups in the amount of α angle correction (Figure 3) (Q 3.455, df 2, p = 0.178). Sensitivity analysis showed moderate rather than high heterogeneity in AMO and SHD groups, and showed that the AMO group had a higher standardized reduction in α angle than both the arthroscopy and the SHD groups (Supplementary Table v).
Fig. 3.
Change in α angle from pre- to postoperative. AMO, anterior mini open approach; CI, confidence interval; MD, mean difference in degrees; SHD, surgical hip dislocation.
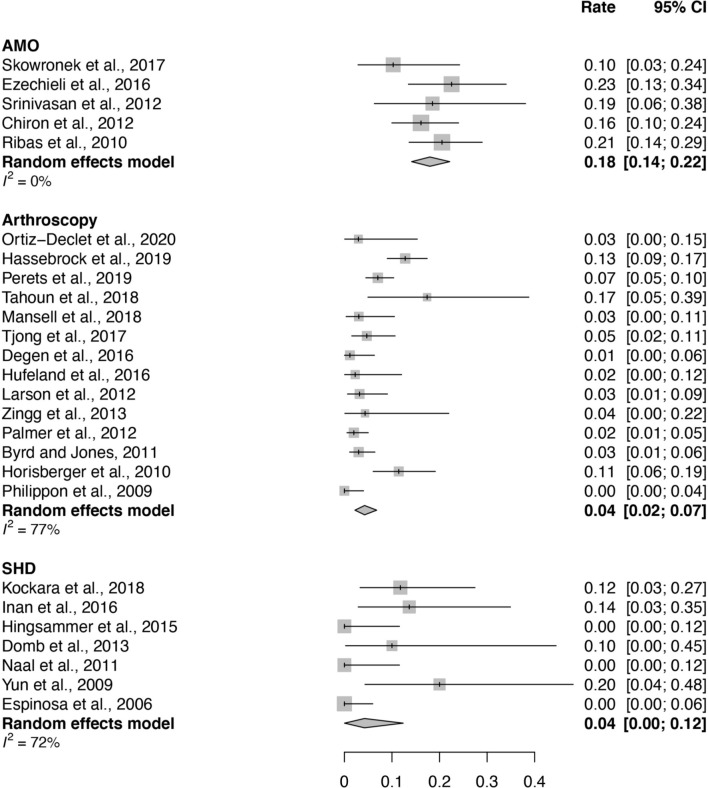
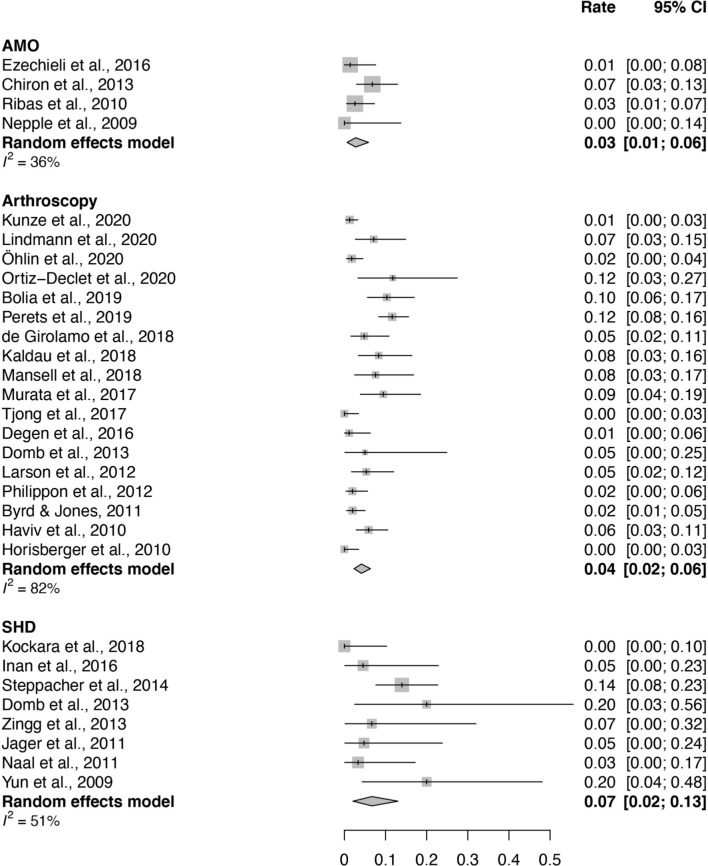
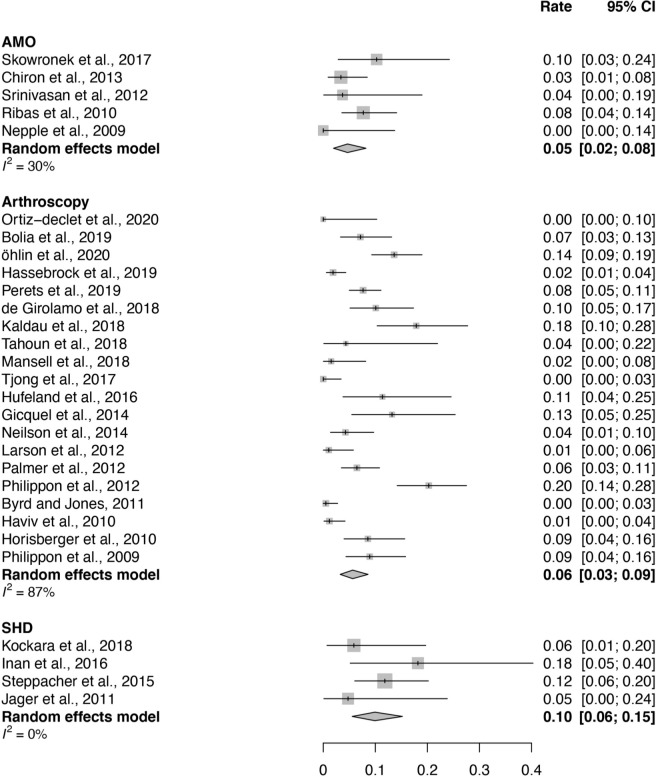
Rates of complications, revision, and conversion to total hip arthroplasty
The rate of complications following AMO was significantly higher in comparison to the rate of complications following arthroscopy and SHD, which both had similar overall rate of complications (Figure 4). The incidence of major complications was highest for SHD (0% to 21.4%) and lowest for AMO (0% to 4.8%). Incidence of moderate complications, including transient neuropraxia, symptomatic heterotopic ossification, infection, wound haematoma, or osteoarthritis progression, was 0% to 25.5% for HA, 16.7% to 24% for AMO, and 0% to 14.7% for SHD. Incidence of minor complications was 0% to 14.3% for HA, 0% to 30.5% for AMO, and 0% for SHD except for one study reporting an incidence of 45.5% (Table V). All procedures had similar rates of revision surgery (Figure 5). SHD has a high rate of conversion to THA, which was significant compared to AMO (Q 3.844, df 1, p = 0.049) and had a strong trend towards significance when compared to HA (Q 3.583, df 1, p = 0.058, Figure 6).
Fig. 4.
Pooled rate/proportion of all complications. AMO, anterior mini open approach; CI, confidence interval; SHD, surgical hip dislocation.
Table V.
Rates of major, moderate, and minor complications for each study including revision and conversion rates.
| Study | Patients, n |
THA conversion, n (%) |
Repeat procedures, n (%) | Major | Moderate | Minor |
|---|---|---|---|---|---|---|
| Arthroscopy | ||||||
| Kunze et al 202,04526 | 310 | NR | 4 revision arthroscopies Total: 4 (1.3) |
NR | NR | NR |
| Öhlin et al 202,04728 | 184 | 36 (19.6) | NR | NR | NR | NR |
| Ortiz-Declet et al 202,04829 | 34 | 0 (0) | 3 revision arthroscopies for adhesions; 1 revision arthroscopies for labral retear Total: 4 (11.8) |
0 (0) | 0 (0) | 1 temporary neuropraxia Total: 1 (2.9) |
| Bolia et al 201,94930 | 99 | 9 (9.1) | 10 evision arthroscopies for adhesions; 3 revision arthroscopies for adhesions and a small cam regrowth Total: 13 (13.1) |
3 cases of small cam regrowth Total: 3 (3.0) |
NR | NR |
| Hassebrock et al 201,95031 | 133 | 1 (0.8) | NR | 0 (0) | 1 infection Total: 1 (0.8) |
8 temporary neuropraxia; 2 heterotopic ossification;* 9 other‡
Total: 19 (14.3) |
| Perets et al 201,95233 | 295 | 25 (8.5) | 25 revision arthroscopies for persistent symptoms; 11 revision arthroscopies for hip reinjury; 3 revision arthroscopies for heterotopic ossification; 1 revision arthroscopy for femoral neck stress fracture Total: 40 (13.6) |
25 persistent hip symptoms; 1 femoral neck stress fracture Total: 26 (8.8) |
3 heterotopic ossification;†
3 cases of infection that resolved with antibiotics treatment Total: 6 (2.0) |
16 temporary neuropraxia Total: 16 (5.4) |
| de Girolamo et al 201,85334 | AMIC-59 MFx-50 |
AMIC -0 (0) MFx- 11 (22) |
5 revision arthroscopies for persistent or recurrent mechanical hip symptoms Total: 5 (4.6) |
5 persistent symptoms Total: 5 (4.6) |
0 (0) | 0 (0) |
| Kaldau et al 201,85435 | 84 | 15 (17.9) | 7 repeat arthroscopies (reasons unspecified) Total: 7 (8.3) |
0 (0) | 0 (0) | 0 (0) |
| Mansell et al 201,85536 | 66 | 1 (7.5) | 5 revision arthroscopies for persistent symptoms Total: 5 (7.6) |
1 hip fracture Total: 1 (7.5) |
7 postoperative diagnosis of hip osteoarthritis Total: 7 (10.6) |
1 heterotopic ossification* Total: 1 (7.5) |
| Tahoun et al 201,85637 | 23 | 1 (4.3) | NR | 0 (0) | 1 periarticular muscular pain and stiffness; 3 perineal hypoesthesia Total: 4 (17.4) |
0 (0) |
| Menge et al 201,75839 | 154 | 50 (32.5) | 7 repeat arthroscopies (reasons unspecified) Total: 7 (4.5) |
NR | NR | NR |
| Murata et al 201,75940 | 74 | NR | 7 revision arthroscopies due to persistent hip pain Total: 7 (9.5) |
NR | NR | NR |
| Tjong et al 201,76041 | 86 | 0 (0) | 0 (0) | 0 (0) | 5 superficial erythema that resolved with ABx Total: 5 (5.8) |
0 (0) |
| Degen et al 201,66142 | 70 | NR | 1 arthroscopy for irrigation and debridement of a subcutaneous wound infection Total: 1 (1.4) |
0 (0) | 1 subcutaneous wound infection Total: 1 (1.4) |
0 (0) |
| Hufeland et al 201,66243 | 44 | 5 (11.4) | 0 (0) | 0 (0) | 0 (0) | 3 temporary neuropraxia; 1 asymptomatic heterotopic ossifications Brooker type II Total: 4 (9.1) |
| Gicquel et al 201,43146 | 51 | 8 (15.7) | NR | NR | 13 Tönnis grade progression Total: 13 (25.5) |
NR |
| Nielsen et al 201,46648 | 117 | 5 (4.3) | NR | NR | NR | NR |
| Domb et al 201,36749 | 20 | NR | 1 iliopsoas release because of new-onset symptomatic internal snapping. Total: 1 (0.5) |
1 iliopsoas release because of new-onset symptomatic internal snapping. Total: 1 (0.5) |
NR | NR |
| Zingg et al 201,37052 | 23 | NR | 0 (0) | 0 (0) | 1 transient neuropraxia of LFCN Total: 1 (4.4) |
0 (0) |
| Larson et al 201,27153 | 94 | 1 (1.1) | 2 revision arthroscopies for HO; 2 revision femoral osteochondroplasty for inadequate initial decompression; 1 open surgical dislocation for a symptomatic posterior cam-type lesion Total: 5 (5.3) |
2 persistent symptoms Total: 2 (2.1) |
2 heterotopic ossifications†
Total: 2 (2.1) |
1 heterotopic ossification*
Total: 1 (1.1) |
| Palmer et al 201,27254 | 185 | 13 (7.0) | 0 (0%) | 1 case of symptomatic Brooker type 3 heterotopic ossification Total: 1 (0.5) |
1 case of Superficial phlebitis; 1 superficial portal infection; 1 transient foot paraesthesia; 2 Tönnis grade progression. Total: 4 (2.2) |
0 (0) |
| Philippon et al 201,27355 | 153 | 31 (20.3) | 2 revision arthroscopies before THA; 1 revision arthroscopy for adhesions Total: 3 (2.0) |
NR | NR | NR |
| Byrd and Jones 201,17456 | 200 | 1 (0.5) | 4 revision arthroscopies for persistent or recurrent mechanical hip symptoms Total: 4 (2.0) |
4 persistent or recurrent mechanical hip symptoms Total: 4 (2.0) |
5 transient neurapraxias 1 LFCN 1 Femoral nerve 1 Sciatic nerve 1 Pudendal nerve 1 Contralateral sciatic nerve (all resolved within a few days) Total: 5 (2.5%) |
1 heterotopic ossification Total: 1 (0.5) |
| Haviv et al 201,07557 | 166 | 2 (1.2) | 10 revision arthroscopies for repeat symptoms; 8 revision arthroscopies for osteochondroplasty; 4 revision arthroscopies for labral tears Total: 22 (13.3) |
10 repeat symptoms; 8 cam re-growths Total: 18 (10.8) |
0 (0) | 0 (0) |
| Horisberger et al 201,07658 | 88 | 9 (10.3) | 0 (0) | 0 (0) | 9 cases of dysesthesia/ hypesthesia of the pudendal nerve and LFCN; 2 transient neurapraxias of the sciatic nerve Total: 11 (12.5) |
1 superficial labia minora tear Total: 1 (1.1) |
| Philippon et al 200,97759 | 112 | 10 (8.9) | NR | 0 (0) | 0 (0) | 0 (0) |
| AMO approach | ||||||
| Skowronek et al60 | 39 | 4 (10.3) | 0 (0) | 0 (0) | 3 meralgia paresthetica, which resolved within 10 months; 4 osteoarthritis developments Total: 7 (17.9) |
1 heterotopic ossification (Brooker Type 2) Total: 1 (2.6) |
| Ezechieli et al 201,67961 | 72 | NR | 1 deep infection with Staphylococcus aureus that needed to be revised Total: 1 (1.4) |
1 deep infection with Staphylococcus aureus
Total: 1 (1.4) |
8 transient neuropraxia of LFCN; 4 hypercorrections Total: 12 (16.7) |
1 asymptomatic heterotopic ossification; 2 LFCN irritations Total: 3 (4.2) |
| Srinivasan et al 201,38062 | 25 | 1 (4.0) | 0 (0) | 1 perineal numbness and sciatic nerve paralysis with foot drop that resolved within 6 months Total: 1 (4.0) |
3 transient neuropraxia of LFCN; 3 patients had a slow recovery period and needed steroid injections to help with their rehabilitation Total: 6 (24.0) |
1 asymptomatic heterotopic ossification Brooker grade one Total: 1 (4.0) |
| Chiron et al 201,28163 | 106 | 4 (3.8) | 2 revision arthroscopies to complete the femoral neck plasty 2 revision arthroscopies for capsular adhesions and lengthening of the psoas tendon; 4 revision arthroscopies for drainage of painful haematomas Total: 8 (7.5) |
2 incomplete femoro osteoplasties Total: 2 (1.9) |
18 cases of osteoarthritis progression; 2 cases of complex regional pain syndrome which quickly improved with conservative treatment that included bisphosphonates; 4 postoperative painful haematomas Total: 24 (22.6) |
0 (0) |
| Ribas et al 201,03264 | 105 | 9 (8.6) | 2 revision arthroscopies for capsulolabral adhesions; 1 revision arthroscopy for persisting retrolabral ulceration Total: 3 (2.9) |
4 cases of permanent neuropraxia of LFCN; 1 retrolabral ulceration Total: 5 (4.8) |
2 postoperative haematomas; 18 transient neuropraxias of LFCN Total: 20 (19.0) |
32 cases of hypertrophic scar formation Total: 32 (30.5) |
| SHD | ||||||
| Kockara et al 201,88366 | 33 | 2 (6.1) | 0 (0) | 2 avascular necrosis; 1 DVT Total: 3 (9.1) |
1 superficial wound infection Total: 1 (3.0) |
0 (0) |
| İnan et al 201,63367 | 22 | 4 (18.2) | 1 revision arthroscopy for persistent symptoms Total: 1 (4.5) |
1 persistent symptom Total: 1 (4.5) |
0 (0) | 8 minor trochanteric irritation; 2 heterotopic ossification*
Total: 10 (45.5) |
| Hingsammer et al 201,58468 | 30 | NR | NR | 0 (0) | 0 (0) | 0 (0) |
| Steppacher et al 201,48569 | 75 | 11 (14.7) | 1 revision of iliotibial band dehiscence; 1 arthroscopic acetabular rim trimming; 2 refixations of greater trochanter; 6 arthroscopic adhesiolysis; 2 evacuations of wound haematoma; 1 irrigation and debridement for subcutaneous wound infection Total: 13 (17.3) |
1 iliotibial band dehiscence; 2 trochanteric nonunion Total: 3 (4.0) |
8 cases of osteoarthritis progression; 1 subcutaneous wound infection; 2 wound haematomas Total: 11 (14.7) |
0 (0) |
| Domb et al 201,36749 | 10 | NR | 1 patient underwent hip arthroscopy at the time of hardware removal where a microfracture was performed; 1 patient underwent revision arthroscopy for labral debridement, chondroplasty, and lysis of adhesions. Total: 2 (20.0) |
2 revision arthroscopies due to persisting symptoms Total: 2 (20.0) |
0 (0) | 0 (0) |
| Zingg et al 201,37052 | 18 | NR | 1 arthroscopic adhesiolysis Total: 1 (5.6) |
0 (0) | 0 (0) | 0 (0) |
| Naal et al 201,18771 | 22 | NR | NR | 0 (0) | 1 patient had osteoarthritis progression Total: 1 (4.5) |
0 (0) |
| Yun et al 200,93072 | 14 | NR | NR | 3 trochanteric nonunions Total: 3 (21.4) |
0 (0) | 0 (0) |
| Espinosa et al 200,63873 | 52 | NR | NR | 0 (0) | 0 (0) | 0 (0) |
Brooker grade 2 (minor) was assumed for studies that did not report Brooker grade.
Brooker grade 3 (moderate) was assumed for studies that did not report Brooker grade but reported arthroscopic treatment for heterotopic ossifications.
Complications stated as “other” were classed as minor complications.
Fig. 5.
Pooled rate/proportion of all revision surgery. AMO, anterior mini open approach; CI, confidence interval; SHD, surgical hip dislocation.
Fig. 6.
Pooled proportion of conversion to total hip arthroplasty. AMO, anterior mini open approach; CI, confidence interval; SHD, surgical hip dislocation.
Discussion
Our systematic review evaluated PROMs, α angle, complications, revision rates, and incidence of conversion to THA after SHD, AMO, or arthroscopic management for FAI. The gradual transition from SHD to arthroscopic management is evident in the literature over the past 20 years,74 and is reflected by the large proportion of the 48 articles analyzed which examined outcomes following HA. In 2011, the difference between the different procedures was not robust, which was reflected in the systematic review by Botser et al12 including eight articles for SHD, four articles for AMO, and 15 articles for HA. Since then, there has been an exponential increase in the use of HA for the treatment of FAI.
All surgical groups reported a significant increase in PROMs. We can conclude with a high degree of certainty that AMO has the highest PROM values, as this was significant in both primary and sensitivity analysis of arthroscopy versus AMO. We conducted meta-regression to establish whether follow-up period influenced PROM values. No association was found between follow-up period and PROM values, therefore differences in follow-up period could not explain the high heterogeneity and the higher PROM values reported in the AMO group, in which studies tended to have shorter follow-up. The high heterogeneity observed throughout all PROMs likely reflects the subjective nature of PROMs, and that the physicians delivering these measures may have different attitudes or variations in presentation which affect the patient’s interpretation. Again, there is an urgent need for uniformity of reporting PROMs and the Non-Arthroplasty Hip Registry in the UK seems to have managed that to an extent by using the iHot12 and EuroQol five-dimension (EQ-5D) scoring system in their minimum dataset.
All three surgical methods showed a significant decrease in mean α angle postoperatively, with no difference between each group in the amount of α angle correction. Sensitivity analysis revealed that AMO may provide a larger correction in α angle than both SHD and arthroscopy, and this may be because it allows easy access to the anterolateral aspect of the cam lesion. Nevertheless, the AMO group had only two studies with high heterogeneity and a wide confidence interval. More data are required for firm conclusions to be drawn regarding this difference. Additionally, the lower heterogeneity observed in the sensitivity analysis using standardized mean difference demonstrated that different α angle measurement techniques introduced heterogeneity within groups. In the future, studies should endeavour to use the same measurement technique for quantification of the α angle so that results are directly comparable, or multiple measurement techniques to enable comparison between studies. There is currently no consensus on the optimum measurement technique for quantification of the α angle, however the authors recommend the 45° radiological Dunn view, in the absence of MRI, due to its increased sensitivity for detection of femoral head asphericity.75,76
All procedures showed similar rates of revision. We used the classification provided by Clohisy et al77 for complications which are divided into major, moderate, or minor. The overall rate of complications after the AMO approach was significantly higher than the rate of complications after arthroscopy and SHD, which both had similar overall rate of complications. This was a consequence of consistently high reported rates of transient neuropraxia of the lateral femoral cutaneous nerve, which was the second most reported complication in this group. Interestingly, the incidence of major complications was lowest in AMO studies, while the highest incidence of major complications was reported in an early SHD study by Yun et al72 who reported a 21.4% rate of trochanteric nonunion. Progression of the Tönnis grade was mentioned in several articles including Gicquel et al,46 who reported the highest rate of progression of the Tönnis grade in the arthroscopic group. It is likely that these patients may not have been appropriate for hip preservation surgery if degenerative disease had progressed. Therefore, this finding may not be a true complication, but rather a failure of the procedure due to a failure in patient stratification and selection. Minor complications were reported to be between 0% and 10.8% in arthroscopic studies. In AMO studies, Ribas et al64 recorded the highest percentage of minor complications with 30.5% hypertrophic scar formations. The majority of SHD studies had no minor complications except for İnan et al,67 who reported 36.4% with minor trochanteric irritation. Additionally, SHD had the highest rate of conversion to THA which was significantly higher than the rate reported for AMO and displayed a strong trend towards significance against arthroscopy. Interestingly, heterogeneity was consistently higher in the arthroscopy group versus the AMO and SHD groups for complications, revision, and conversion. This may reflect the steep learning curve reported for arthroscopy, which was a relatively new technique at the time of authorship for many of the included papers, and the position of the surgeon or institution on the learning curve.78,79
Our results showed good qualitative agreement with the results of Matsuda et al11 and Botser et al.12 All three surgical approaches produce consistent positive outcomes for patients, and the arthroscopic approach has a lower incidence of major complications. In contradiction with Botser et al,12 we found that AMO shows the greatest improvement in PROMs at the latest follow-up. Additionally, we have reported similar rates of reoperation and clinical complications to Minkara et al80 who analyzed arthroscopic outcomes only. They report the rate of reoperation was 5.5%, and the risk of clinical complications was 1.7%.80 This may be due to the inclusion of minor complications, including transient neuropraxias, in our overall complication rate.
FAI is a widely recognized condition that occurs mostly in young adults and has been postulated to lead to degenerative changes of the hip joint.81 It is prudent to consider that all three surgical approaches may have valuable roles in the treatment of FAI. Generally, the Ganz technique of SHD is a safe surgical approach to the femoral head and the acetabulum without the risk of avascular necrosis and allows an almost 360° view of the hip joint.73,82 Nevertheless, it is an extensive procedure with more soft-tissue disruption.73,82 While SHD is the first described method of treatment of FAI and several studies have shown good outcomes following SHD, over the last decade the management of FAI has naturally evolved to favour more minimally invasive techniques such as arthroscopy.83 Current advances in surgical techniques combined with advances in our understanding of the native hip joint have incited a dramatic increase in the arthroscopic management of FAI.8 However, arthroscopy is a technically demanding procedure with a steep learning curve, which carries its own inherent risks and commonly requires traction to distract the hip joint for arthroscopic access.84,85 Similarly, the mini open approach demonstrates favourable outcomes after treatment for FAI, which minimizes muscle damage and reduces the traction necessary for assessing the hip joint when compared to arthroscopy.86 Nevertheless, caution must be applied to prevent damage to the LFCN, which was evident in all our AMO studies.
This systematic review employed strong statistical methodology, with sensitivity analyses, in order to synthesize data from 48 studies including 4,384 hips in 4,094 patients, and offers a higher statistical power and more robust conclusions than any individual study.87 We do, however, recognize several limitations that should be acknowledged. Firstly, although there were two RCTs in the arthroscopic group, most studies consisted of level 4 evidence. Secondly, most studies were of fair quality rather than high. Thirdly, in interpreting the data we were required to make some assumptions and estimate variance due to inconsistencies in reporting and study design. The between-study heterogeneity was also judged as moderate or high throughout our meta-analysis, which is likely a reflection of the nature of the included studies, which tend to report outcomes from a single surgeon or centre, and a reflection of our chosen outcome variables. Additionally, while SHD shows a higher rate of THA conversion, we were unable to account for the intuitively higher rate of conversions if starting age at surgery was older or if the length of follow-up was longer. Finally, our systematic review only included English and German language articles, which may not represent all literature published on this subject.
In conclusion, all three surgical approaches for the treatment of FAI offer significant improvements in PROMs and significant correction of the cam deformity. While AMO demonstrated the largest improvement in outcomes, there was a similar correction in α angle measurements across all groups. All three groups showed similar rates of revision procedures, but both arthroscopy and SHD had relatively low rates of complications. AMO had the highest incidence of complications, mostly due to the damage to the LFCN, and SHD had the highest rates of conversion to a THA. The widespread adoption of arthroscopy has not led to a decrease in the quality of PROMs or an increase in complications.
Author contributions
D. Addai: Investigation, Methodology, Writing – original draft, Writing – review & editing.
J. Zarkos: Methodology, Visualization, Writing – original draft, Writing – review & editing.
M. Pettit: Methodology, Formal analysis, Visualization, Writing – original draft, Writing – review & editing
K. H. Sunil Kumar: Methodology, Writing – original draft, Writing – review & editing, Project administration.
V. Khanduja: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Project administration.
Funding statement
No funding has been received or will be received relating directly or indirectly to the subject of this article.
ICMJE COI statement
All authors declare that they have no conflict of interest with this work and have received no funding for this work. V. Khanduja is an associate editor for The Bone & Joint Journal, and an educational consultant for Smith & Nephew and Arthrex.
Open access funding
Open access funding for this study was obtained from Addenbrooke's - Cambridge University Hospital NHS Foundation Trust.
Follow V. Khanduja @CambridgeHipDoc
Supplementary material
Sensitivity analyses, full between-group comparisons, and further meta-regression relating to the meta-analysis. Additionally, full Methodological Index for Non-randomized Studies assessment, patient-reported outcome measures, and alpha angle values extracted from the literature are quoted.
References
- 1.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. [PubMed] [Google Scholar]
- 2.Imam S, Khanduja V. Current concepts in the diagnosis and management of femoroacetabular impingement. Int Orthop. 2011;35(10):1427–1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palmer AJR, Ayyar Gupta V, Fernquest S, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: Multicentre randomised controlled trial. BMJ. 2019;364:l185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83-B(8):1119–1124. [DOI] [PubMed] [Google Scholar]
- 6.Griffin DR, Dickenson EJ, Wall PDH, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK fashion): a multicentre randomised controlled trial. Lancet. 2018;391(10136):2225–2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakano N, Lisenda L, Jones TL, Loveday DT, Khanduja V. Complications following arthroscopic surgery of the hip: a systematic review of 36 761 cases. Bone Joint J. 2017;99-B(12):1577–1583. [DOI] [PubMed] [Google Scholar]
- 8.Kuhns BD, Weber AE, Levy DM, Wuerz TH. The natural history of femoroacetabular impingement. Front Surg. 2015;2:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lynch TS, Terry MA, Bedi A, Kelly BT. Hip arthroscopic surgery: patient evaluation, current indications, and outcomes. Am J Sports Med. 2013;41(5):1174–1189. [DOI] [PubMed] [Google Scholar]
- 10.Griffin DR, Dickenson EJ, O'Donnell J, et al. The Warwick agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169–1176. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27(2):252–269. [DOI] [PubMed] [Google Scholar]
- 12.Botser IB, Smith TW, Nasser R, Domb BG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27(2):270–278. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. original article methodological index for non-Randomized studies (minors). 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 15.Sundemo D, Hamrin Senorski E, Karlsson L, et al. Generalised joint hypermobility increases ACL injury risk and is associated with inferior outcome after ACL reconstruction: a systematic review. BMJ Open Sport Exerc Med. 2019;5(1):e000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oxford Centre for Evidence-based Medicine . Levels of Evidence (March 2009). 2009. https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ (date last accessed20 August 2020).
- 17.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thorborg K, Roos EM, Bartels EM, Petersen J, Hölmich P, Validity HP. Validity, reliability and responsiveness of patient-reported outcome questionnaires when assessing hip and groin disability: a systematic review. Br J Sports Med. 2010;44(16):1186–1196. [DOI] [PubMed] [Google Scholar]
- 20.Harris JD, Brand JC, Cote MP, Dhawan A. Research pearls: the significance of statistics and perils of pooling. Part 3: pearls and pitfalls of meta-analyses and systematic reviews. Arthroscopy. 2017;33(8):1594–1602. [DOI] [PubMed] [Google Scholar]
- 21.Nwachukwu BU, Fields K, Chang B, Nawabi DH, Kelly BT, Ranawat AS. Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(3):612–619. [DOI] [PubMed] [Google Scholar]
- 22.Thomeé R, Jónasson P, Thorborg K, et al. Cross-Cultural adaptation to Swedish and validation of the Copenhagen hip and groin outcome score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):835–842. [DOI] [PubMed] [Google Scholar]
- 23.Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med. 2013;41(9):2065–2073. [DOI] [PubMed] [Google Scholar]
- 24.Ramisetty N, Kwon Y, Mohtadi N. Patient-Reported outcome measures for hip preservation surgery-a systematic review of the literature. J Hip Preserv Surg. 2015;2(1):15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kunze KN, Nwachukwu BU, Beck EC, et al. Preoperative duration of symptoms is associated with outcomes 5 years after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2020;36(4):1022–1029. [DOI] [PubMed] [Google Scholar]
- 27.Lindman I, Öhlin A, Desai N, et al. Five-Year outcomes after arthroscopic surgery for femoroacetabular impingement syndrome in elite athletes. Am J Sports Med. 2020;48(6):1416–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Öhlin A, Ahldén M, Lindman I, et al. Good 5-year outcomes after arthroscopic treatment for femoroacetabular impingement syndrome. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1311–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ortiz-Declet V, Yuen LC, Schwarzman GR, Chen AW, Perets I, Domb BG. Return to play in amateur soccer players undergoing hip arthroscopy: short- to mid-term follow-up. Arthroscopy. 2020;36(2):442–449. [DOI] [PubMed] [Google Scholar]
- 30.Bolia IK, Fagotti L, Briggs KK, Philippon MJ. Midterm outcomes following repair of capsulotomy versus Nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with Labral repair. Arthroscopy. 2019;35(6):1828–1834. [DOI] [PubMed] [Google Scholar]
- 31.Hassebrock JD, Krych AJ, Domb BG, Levy BA, Neville MR, Hartigan DE. Bilateral hip arthroscopy: can results from initial arthroscopy for femoroacetabular impingement predict future contralateral results? Arthroscopy. 2019;35(6):1837–1844. [DOI] [PubMed] [Google Scholar]
- 32.Kierkegaard S, Mechlenburg I, Lund B, Rømer L, Søballe K, Dalgas U. Is hip muscle strength normalised in patients with femoroacetabular impingement syndrome one year after surgery?: results from the HAFAI cohort. J Sci Med Sport. 2019;22(4):413–419. [DOI] [PubMed] [Google Scholar]
- 33.Perets I, Chaharbakhshi EO, Shapira J, Ashberg L, Mu BH, Domb BG. Hip arthroscopy for femoroacetabular impingement and Labral tears in patients younger than 50 years: minimum five-year outcomes, survivorship, and risk factors for reoperations. J Am Acad Orthop Surg. 2019;27(4):e173. [DOI] [PubMed] [Google Scholar]
- 34.de Girolamo L, Jannelli E, Fioruzzi A, Fontana A. Acetabular chondral lesions associated with femoroacetabular impingement treated by autologous matrix-induced chondrogenesis or Microfracture: a comparative study at 8-year follow-up. Arthroscopy. 2018;34(11):3012–3023. [DOI] [PubMed] [Google Scholar]
- 35.Kaldau NC, Brorson S, Hölmich P, Lund B. Good midterm results of hip arthroscopy for femoroacetabular impingement. Dan Med J. 2018;65(6). [PubMed] [Google Scholar]
- 36.Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG. Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: a randomized controlled trial with 2-year follow-up. Am J Sports Med. 2018;46(6):1306–1314. [DOI] [PubMed] [Google Scholar]
- 37.Tahoun MF, Tey M, Mas J, Abd-Elsattar Eid T, Monllau JC. Arthroscopic repair of acetabular cartilage lesions by Chitosan-Based Scaffold: clinical evaluation at minimum 2 years Follow-up. Arthroscopy. 2018;34(10):2821–2828. [DOI] [PubMed] [Google Scholar]
- 38.Zimmerer A, Bock M, Hoffmann M, Miehlke W, Sobau C. Return to work after arthroscopic surgery for femoroacetabular impingement in patients younger than 30 years. Sports Orthop Traumatol. 2018;34(1):31–37. [Google Scholar]
- 39.Menge TJ, Briggs KK, Dornan GJ, McNamara SC, Philippon MJ. Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement: Labral debridement compared with Labral repair. J Bone Joint Surg Am. 2017;99-A(12):997–1004. [DOI] [PubMed] [Google Scholar]
- 40.Murata Y, Uchida S, Utsunomiya H, Hatakeyama A, Nakamura E, Sakai A. A comparison of clinical outcome between athletes and Nonathletes undergoing hip arthroscopy for femoroacetabular impingement. Clin J Sport Med. 2017;27(4):349–356. [DOI] [PubMed] [Google Scholar]
- 41.Tjong VK, Gombera MM, Kahlenberg CA, et al. Isolated Acetabuloplasty and Labral repair for Combined-Type femoroacetabular impingement: are we doing too much? Arthroscopy. 2017;33(4):773–779. [DOI] [PubMed] [Google Scholar]
- 42.Degen RM, Fields KG, Wentzel CS, et al. Return-to-play rates following arthroscopic treatment of femoroacetabular impingement in competitive baseball players. Phys Sportsmed. 2016;44(4):385–390. [DOI] [PubMed] [Google Scholar]
- 43.Hufeland M, Krüger D, Haas NP, Perka C, Schröder JH. Arthroscopic treatment of femoroacetabular impingement shows persistent clinical improvement in the mid-term. Arch Orthop Trauma Surg. 2016;136(5):687–691. [DOI] [PubMed] [Google Scholar]
- 44.Joseph R, Pan X, Cenkus K, Brown L, Ellis T, Di Stasi S. Sex differences in self-reported hip function up to 2 years after arthroscopic surgery for femoroacetabular impingement. Am J Sports Med. 2016;44(1):54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dippmann C, Thorborg K, Kraemer O, Winge S, Palm H, Hölmich P. Hip arthroscopy with labral repair for femoroacetabular impingement: short-term outcomes. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):744–749. [DOI] [PubMed] [Google Scholar]
- 46.Gicquel T, Gédouin J-E, Krantz N, et al. Function and osteoarthritis progression after arthroscopic treatment of femoro-acetabular impingement: a prospective study after a mean follow-up of 4.6 (4.2-5.5) years. Orthop Traumatol Surg Res. 2014;100(6):651–656. [DOI] [PubMed] [Google Scholar]
- 47.Gupta A, Redmond JM, Stake CE, Finch NA, Dunne KF, Domb BG. Does the femoral CaM lesion regrow after osteoplasty for femoroacetabular impingement? two-year follow-up. Am J Sports Med. 2014;42(9):2149-55. [DOI] [PubMed] [Google Scholar]
- 48.Nielsen TG, Miller LL, Lund B, Christiansen SE, Lind M. Outcome of arthroscopic treatment for symptomatic femoroacetabular impingement. BMC Musculoskelet Disord. 2014;15(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Domb BG, Stake CE, Botser IB, Jackson TJ. Surgical dislocation of the hip versus arthroscopic treatment of femoroacetabular impingement: a prospective matched-pair study with average 2-year follow-up. Arthroscopy. 2013;29(9):1506–1513. [DOI] [PubMed] [Google Scholar]
- 50.Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46–53. [DOI] [PubMed] [Google Scholar]
- 51.Malviya A, Paliobeis CP, Villar RN. Do professional athletes perform better than recreational athletes after arthroscopy for femoroacetabular impingement? Clin Orthop Relat Res. 2013;471(8):2477–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zingg PO, Ulbrich EJ, Buehler TC, Kalberer F, Poutawera VR, Dora C. Surgical hip dislocation versus hip arthroscopy for femoroacetabular impingement: clinical and morphological short-term results. Arch Orthop Trauma Surg. 2013;133(1):69–79. [DOI] [PubMed] [Google Scholar]
- 53.Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40(5):1015–1021. [DOI] [PubMed] [Google Scholar]
- 54.Palmer DH, Ganesh V, Comfort T, Tatman P. Midterm outcomes in patients with CAM femoroacetabular impingement treated Arthroscopically. Arthroscopy. 2012 Nov 1;28(11):1671–1681. [DOI] [PubMed] [Google Scholar]
- 55.Philippon MJ, Schroder E Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28(1):59–65. [DOI] [PubMed] [Google Scholar]
- 56.Byrd JWT, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011;27(10):1379–1388. [DOI] [PubMed] [Google Scholar]
- 57.Haviv B, Singh PJ, Takla A, O’Donnell J. Arthroscopic femoral osteochondroplasty for CaM lesions with isolated acetabular chondral damage. J Bone Joint Surg Br. 2010;92-B(5):629–633. [DOI] [PubMed] [Google Scholar]
- 58.Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoroacetabular impingement of the hip: a new technique to access the joint. Clin Orthop Relat Res. 2010;468(1):182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Philippon MJ, Briggs KK, Yen Y-M, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91-B(1):16–23. [DOI] [PubMed] [Google Scholar]
- 60.Skowronek P, Synder M, Polguj M, Marczak D, Sibiński M. Treatment of femoroacetabular impingement with a Mini-open direct anterior approach. Indian J Orthop. 2017;51(6):677–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ezechieli M, De Meo F, Bellotti V, et al. Arthroscopic assisted mini-open approach of the hip: early multicentric experience. Technol Health Care. 2016;24(3):359–365. [DOI] [PubMed] [Google Scholar]
- 62.Srinivasan SCM, Hosny HAH, Williams MR. Combined hip arthroscopy and limited open osteochondroplasty for anterior femoroacetabular impingement: early patient reported outcomes. Hip Int. 2013;23(2):218–224. [DOI] [PubMed] [Google Scholar]
- 63.Chiron P, Espié A, Reina N, Cavaignac E, Molinier F, Laffosse J-M. Surgery for femoroacetabular impingement using a minimally invasive anterolateral approach: analysis of 118 cases at 2.2-year follow-up. Orthop Traumatol Surg Res. 2012;98(1):30–38. [DOI] [PubMed] [Google Scholar]
- 64.Ribas M, Ledesma R, Cardenas C, Marin-Peña O, Toro J, Caceres E. Clinical results after anterior mini-open approach for femoroacetabular impingement in early degenerative stage. Hip Int. 2010;20(Suppl 7):S36–42. [DOI] [PubMed] [Google Scholar]
- 65.Nepple JJ, Zebala LP, Clohisy JC. Labral disease associated with femoroacetabular impingement: do we need to correct the structural deformity? J Arthroplasty. 2009;24(6 Suppl):114–119. [DOI] [PubMed] [Google Scholar]
- 66.Kockara N, Sofu H, Issin A, Çamurcu Y, Bursali A. Predictors of the clinical outcome and survival without degenerative arthritis after surgical treatment of femoroacetabular impingement. J Orthop Sci. 2018;23(1):117–121. [DOI] [PubMed] [Google Scholar]
- 67.İnan U, Harmanşa S, Ömeroğlu H. Treatment of mixed type femoroacetabular impingement using safe surgical hip dislocation in adults. Eklem Hastalik Cerrahisi. 2016;27(3):160–166. [DOI] [PubMed] [Google Scholar]
- 68.Hingsammer AM, Lee CB, LaReau J, Kalish LA, Kim Y-J. Is acetabular osteoplasty always required in mixed impingement? Eur J Orthop Surg Traumatol. 2015;25(2):331–338. [DOI] [PubMed] [Google Scholar]
- 69.Steppacher SD, Huemmer C, Schwab JM, Tannast M, Siebenrock KA. Surgical hip dislocation for treatment of femoroacetabular impingement: factors predicting 5-year survivorship. Clin Orthop Relat Res. 2014;472(1):337–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jäger M, Bittersohl B, Zilkens C, et al. Surgical hip dislocation in symptomatic CaM femoroacetabular impingement: what matters in early good results? Eur J Med Res. 2011;16(5):217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Naal FD, Miozzari HH, Wyss TF, Nötzli HP. Surgical hip dislocation for the treatment of Femoroacetabular impingement in high-level athletes. Am J Sports Med. 2011;39(3):544–550. [DOI] [PubMed] [Google Scholar]
- 72.Yun H-H, Shon W-Y, Yun J-Y. Treatment of femoroacetabular impingement with surgical dislocation. Clin Orthop Surg. 2009;1(3):146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of Femoro-Acetabular impingement: preliminary results of Labral refixation. JBJS. 2006;88(5):925–935. [DOI] [PubMed] [Google Scholar]
- 74.Nakano N, Khanduja V. Femoroacetabular impingement: the past, current controversies and future perspectives. Phys Sportsmed. 2018;46(3):270–272. [DOI] [PubMed] [Google Scholar]
- 75.Smith KM, Gerrie BJ, McCulloch PC, Lintner DM, Harris JD. Comparison of MRI, CT, Dunn 45° and Dunn 90° alpha angle measurements in femoroacetabular impingement. Hip Int J Clin Exp Res Hip Pathol Ther. 2018;28(4):450–455. [DOI] [PubMed] [Google Scholar]
- 76.Saito M, Tsukada S, Yoshida K, Okada Y, Tasaki A. Correlation of alpha angle between various radiographic projections and radial magnetic resonance imaging for CaM deformity in femoral head-neck junction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):77–83. [DOI] [PubMed] [Google Scholar]
- 77.Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res. 2010;468(2):555–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hoppe DJ, de Sa D, Simunovic N, et al. The learning curve for hip arthroscopy: a systematic review. Arthroscopy. 2014;30(3):389–397. [DOI] [PubMed] [Google Scholar]
- 79.Nakano N, Khanduja V. Complications in hip arthroscopy. Muscles Ligaments Tendons J. 2016;6(3):402–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Minkara AA, Westermann RW, Rosneck J, Lynch TS, Review S. Systematic review and meta-analysis of outcomes after hip arthroscopy in femoroacetabular impingement. Am J Sports Med. 2019;47(2):488–500. [DOI] [PubMed] [Google Scholar]
- 81.Khanduja V, Villar RN. The arthroscopic management of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1035–1040. [DOI] [PubMed] [Google Scholar]
- 82.Peters CL, Erickson JA. Treatment of Femoro-Acetabular impingement with surgical dislocation and débridement in young adults. JBJS. 2006;88(8):1735–1741. [DOI] [PubMed] [Google Scholar]
- 83.Cadet ER. Historical Background of the Treatment of Femoroacetabular Impingement. : Ayeni OR, Karlsson J, Philippon MJ, Safran MR. . Diagnosis and Management of Femoroacetabular Impingement [Internet]. Cham: Springer International Publishing, 2017:1–4. [Google Scholar]
- 84.Bedi A, Kelly BT, Khanduja V. Arthroscopic hip preservation surgery. Bone Jt J. 2013;95-B(1):10–19. [DOI] [PubMed] [Google Scholar]
- 85.Griffiths EJ, Khanduja V. Hip arthroscopy: evolution, current practice and future developments. Int Orthop. 2012;36(6):1115–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chen AF, O’Toole P, Minori J, Parvizi J. Surgical Technique: Mini-Open Approach to the Hip. : Nho S, Leunig M, Kelly B, Bedi A, Larson C. . Hip Arthroscopy and Hip Joint Preservation Surgery [Internet]. New York NY: Springer New York, 2013:1–8. [Google Scholar]
- 87.Fagard RH, Staessen JA, Thijs L. Advantages and disadvantages of the meta-analysis approach. J Hypertens Suppl. 1996;14(2):S9–13. [DOI] [PubMed] [Google Scholar]