Abstract
Study Objectives:
Post-9/11 veterans are particularly vulnerable to insomnia disorder. Having accurate prevalence rates of insomnia disorder in this relatively young, diverse population, is vital to determine the resources needed to identify and treat insomnia disorder. However, there are no accurate prevalence rates for insomnia disorder in post-9/11 veterans enrolling in the VA Healthcare System (VHA). We present accurate prevalence of insomnia disorder, and correlates, in a large sample of post-9/11 veterans enrolling in a VHA.
Methods:
This was an observational study of 5,552 post-9/11 veterans newly enrolling for health care in a VHA. Data were collected using VA eScreening. Insomnia diagnosis was determined using a clinical cutoff score of ≥ 11 on the Insomnia Severity Index. Measures also included sociodemographic, service history, posttraumatic stress disorder (PTSD), depression, suicidal ideation, alcohol misuse, military sexual trauma, traumatic brain injury (TBI), and pain intensity.
Results:
About 57.2% of the sample population had insomnia disorder. Our sample was nationally representative for age, sex, ethnicity, branch of the military, and race. The sample also was at high-risk for a host of clinical disorders, including PTSD, TBI, and pain; all of which showed higher rates of insomnia disorder (93.3%, 77.7%, and 69.6%, respectively).
Conclusions:
The findings suggest alarmingly high rates of insomnia disorder in this population. Examining and treating insomnia disorder, especially in the context of co-occurring disorders (e.g. PTSD), will be a necessity in the future.
Keywords: insomnia, prevalence rates, co-occurring disorders
Introduction
Chronic insomnia disorder is a behavioral sleep disorder characterized as dissatisfaction with sleep quantity or quality, marked by complaints of difficulty falling or staying asleep, waking up earlier than desired, and significant sleep-related daytime impairment [1]. Insomnia is linked to reduced quality of life [2], increased risk for morbidity [3–7], premature mortality [8, 9], and elevations in health care utilization [10, 11]. Insomnia is associated with impaired functioning across multiple life areas, including cognitive, emotional, social, and physical domains [12–15], with societal cost estimated at $100 billion per year [16].
Veterans are particularly vulnerable to insomnia [17–21], with rates double and even triple those of civilian populations [22], due to the irregularity of their sleep/wake schedules during active duty, harsh living conditions, combat stress, higher rates of physical and psychological injury, and issues associated with post-deployment reintegration [22–26]. Insomnia disorder among veterans Health Administration (VHA) users is expected to continue rising as post-9/11 troops leave military service and begin accessing VHA healthcare [25, 27]. Having accurate prevalence rates of insomnia disorder in this relatively young, diverse set of veterans, along with a better understanding of the demographic and clinical correlates, is vital for VHA to determine the resources needed to identify and treat insomnia disorder using evidence-based care. Unfortunately, there are no accurate prevalence rates of insomnia disorder in post-9/11 veterans seeking services.
A confounding issue of estimating insomnia prevalence is the inconsistent use of insomnia terminology throughout the literature. The gold standard for diagnosing insomnia disorder is a weekly sleep diary and an in-depth clinician interview [28]. However, due to the assessment being time consuming, diagnostic criteria for insomnia disorder are rarely assessed outside of research trials [29]. Therefore, most prior studies only examined insomnia symptoms. To ensure clarity, we use “insomnia disorder” herein when diagnosis was established, “insomnia symptoms” when diagnosis was not established, and “insomnia” when the prior literature is unclear on this point.
Rates of insomnia for veterans range from 3.4% based on medical records [30] to 90% of veterans with posttraumatic stress disorder (PTSD) reporting “sleep difficulties” [18]. These rates depend on the definition of insomnia (e.g. “trouble sleeping,” insomnia disorder), data source (e.g. chart review, self-report questionnaire), sample characteristics (e.g. treatment seeking, community), objective/subjective measurement (e.g. self-report questionnaire, sleep diary), measure (e.g. sleep items from mental health [MH] questionnaires, validated sleep questionnaire), co-occurring disorders (e.g. depression, PTSD), gender, and age.
Several studies have reported prevalence rates of insomnia symptoms using “trouble falling or staying sleep” assessed from other MH questionnaires. They found rates of insomnia symptoms of 24.7%–30.5% [31, 32] in a general military/veteran population to upwards of 100% in Vietnam veterans with PTSD [33]. However, a single item about sleep is not a validated measure of insomnia diagnosis, may be anchored to other items in the questionnaire, and may be overly influenced by external factors [34].
Two studies used ICD-9 diagnostic codes from large national VHA databases to estimate prevalence rates of insomnia disorder and found 2.5% of 9,786,778 US veterans seeking VA healthcare from 2000 to 2010 had an insomnia diagnosis recorded in their medical record [23]; the one-year (2010) prevalence rate of insomnia diagnosis was 3.4% in veterans [30]. PTSD was associated with the highest prevalence of insomnia (16%) [23] and deployments to Iraq or Afghanistan conflicts along with anxiety and depressive disorders were also strongly related to insomnia [30]. Unfortunately, using medical records does not provide accurate prevalence of insomnia disorder. Only 53% of VA primary care providers indicated routinely documenting insomnia disorder and 39% routinely included it in the problem list [35–37]. Given the community insomnia rates of 6%–10%, reports of shorter sleep durations, longer sleep onset latencies, more wake after sleep onset, and lower sleep efficiencies in veterans [38–40], along with the well-known problems with obtaining prevalence rates from medical records [29, 35], the rates suggested by these large studies severely underrepresent the true prevalence of insomnia disorder in veterans.
There are three generalizable insomnia disorder prevalence studies that used validated measures of insomnia with clinical cutoff scores on a general sample of post-9/11 veterans. They found rates of insomnia disorder of 59.1% in 375 post-9/11 veterans [41], 53.1% of veterans without military sexual trauma (MST) and 60.8% of veterans with MST (using a subset of the current study sample) [36], and 52.3% of veterans in 660 female veterans receiving services at VA primary care facilities [42]. While these studies used validated measures of insomnia, the samples were relatively small and need follow-up with larger samples.
The existing literature on the prevalence of insomnia disorder is limited by assessing insomnia using non-validated questionnaires or single items, using medical record chart review, small sample sizes, and non-generalizable samples. Accurate estimates of the insomnia disorder rates in post-9/11 veterans is critical to better target and prioritize healthcare resources. This study aimed to addresses these gaps by including an independent sleep questionnaire validated against insomnia diagnostic criteria [43] to (1) obtain prevalence estimates of insomnia disorder in a large sample of post-9/11 veterans enrolling in a VHA and (2) examine the relationship between insomnia disorder and sociodemographics and other clinical symptoms.
Methods
Participants and procedures
The data examined was obtained through standard clinical screening processes of newly enrolling post-9/11 veterans at the VA San Diego Healthcare System between March 2012 and April 2019. Self-reported data was collected electronically using the VA eScreening program or using paper-and-pencil assessment. eScreening is a computer-based, self-screening program that efficiently and effectively collects mental and physical health information [44]. Screening was conducted in the Transition Care Management program, which coordinates healthcare for newly enrolling post-9/11 veterans. Veterans with complete data from the insomnia severity index (ISI; N = 5,552) were included in the study; 768 veterans in the database did not have an ISI. There were no differences between those with and without an ISI by gender, race/ethnicity, combat exposure, PTSD, depression, suicidal ideation, education level, marital status, or pain (p > 0.05); individuals with ISI data had higher rates of alcohol misuse. All research was approved by the Institutional Review Board and the Research and Development Committee.
Measures
Sociodemographic and service history
Age, gender, ethnicity, race, highest level of education, and relationship status was captured by an investigator-created self-report questionnaire. History related to service era, branch of service, number of deployments, and combat exposure was also assessed.
Insomnia
Insomnia severity over the past 2 weeks was measured using the ISI [45]. The ISI consists of seven items, assessing severity of insomnia as well as satisfaction with sleep, effect of sleep on daytime and social functioning, and concern about current sleep. The ISI ranges from 0 to 28, with higher scores indicating more severe insomnia symptoms. Research compared insomnia symptoms assessed with the ISI to weekly sleep diaries and overnight polysomnography for insomnia disorder and found a total score of ≥11 on the ISI indicates insomnia disorder in clinical samples with 97.2% sensitivity and 100% specificity [43]. Internal consistency was excellent for community and clinical sample [43] and for the current sample (α = 0.94).
Posttraumatic stress disorder
The 17-item PTSD Checklist—Civilian Version (PCL-C) [46] measured the degree to which respondents were bothered by PTSD symptoms within the past month. Scores range from 17 to 85, with higher scores indicating greater severity. Cutoff scores of >44 for presumed PTSD diagnosis were chosen based on research involving military and veteran samples [47]. The PCL-C showed strong internal consistency in a military population [46] and for the current sample (α = 0.96).
The 20-item PCL-5 (PTSD Checklist–DSM-5) was subsequently used following the release of the DSM-5 [47]. Items correspond to the DSM-5 diagnostic criteria, and respondents rate how much they are bothered by PTSD symptoms over the past month. Scores range from 0 to 80; cutoff scores of >33 for presumed PTSD diagnosis on the PCL-5 were used based on research involving military and veteran samples [47]. Internal consistency for the current sample was strong (α = 0.98).
Depression
The Patient Health Questionnaire 9-Item Depression Module (PHQ-9) [48] measured depression symptoms occurring within the past 2 weeks; with scores ranging from 0 to 27. Higher scores indicate greater severity. The PHQ-9 is a reliable and valid measure of depression with a cutoff score of ≥15 indicates moderate to severe depression [48]. Internal consistency for the current sample was strong (α = 0.93).
Suicidal ideation
To assess suicidal ideation, we used the PHQ-9 suicide/self-harm item, “Thoughts that you would be better off dead, or thoughts of hurting yourself in some way?,” to indicate presence/absence of suicidal ideation. “0 = Not at all” was coded as negative suicidal ideation and “1 = Several days” or greater was coded as positive.
Alcohol misuse
The Alcohol Use Disorders Identification Test (AUDIT-C) [49] was used to screen hazardous alcohol consumption. Scores range from 0 to 12; scores of ≥4 and ≥3 suggest alcohol misuse in men and women, respectively [50]. This instrument has high internal consistency in the literature [51] and in the current sample (α = 0.80).
Traumatic brain injury (TBI)
History of TBI with concurrent related symptoms was assessed using the four-item VA TBI screen. A positive TBI screen required one or more positive responses in each of the following categories: a list of events in which an injury could have occurred, immediate symptoms following the event, new or worsening symptoms, and current symptoms. The VA TBI screen has high-internal consistency and test–retest reliability, high sensitivity, and moderate specificity [52].
Military sexual trauma
MST was assessed by two VA created questions: “When you were in the military, did you ever receive uninvited and unwanted sexual attention (i.e. touching, pressure for sexual favors, verbal remarks)?” and “When you were in the military, did anyone ever use force or the threat of force to have sex with you against your will?” A positive screen required an affirmative answer to either of these questions [53].
Pain
Pain intensity over the past four weeks was assessed using a numerical rating scale from 0 to 10, anchored at “no pain at all” and “worst pain ever,” respectively. A rating of ≥4 was considered to be clinically significant pain [54].
Statistical analyses
Data were analyzed using descriptive statistics and frequencies. Chi-squares examined insomnia by grouped categories; follow-up 2 × 2 chi-squares examined significant omnibus results with the largest group being the comparison group. Cramer’s V examined effect sizes of all chi-squares, (.1 is a small effect, .3 is a medium effect, and .5 or larger is considered a large effect) and Cohen’s d for t-tests (.2 is a small effect, .5 is a medium effect, and .8 is a large effect size) [55]. Data were analyzed using Statistical Package for Social Sciences 26 (IBM, Inc.). p < 0.05 level was used to indicate significance.
Results
Sociodemographic and service history
Table 1 presents the means and standard deviations of the sociodemographic and service history variables for the entire sample (N = 5,552). Consistent with national cohorts of veterans’ demographics, our sample was approximately 35 years old (M = 34.8, SD = 9.10), primarily male (82.8%), with nearly a quarter (24.2%) Hispanic, and more than half (53.6%) White [56]. There was an average of 1.93 deployments (SD = 1.23) and most (52.4%) deployed to the operations in Iraq and Afghanistan. Consistent with the characteristics of the region, the sample had proportionally more veterans of the Navy (51.2%) and Marines (30.5%) compared to the Active Duty Personnel Data (Army: 36.6%; Navy: 24.8%; Air Force: 24.3%; Marines: 14.2%) [56].
Table 1.
Demographic characteristics of post-9/11 veterans (N = 5,552)
| Demographic variable | Total %/M (SD) | Demographic variable | Total %/M (SD) |
|---|---|---|---|
| Age | 34.8 (9.10) | Service/branch | |
| Sex | Army | 13.2% | |
| Men | 82.8% | Air Force | 3.8% |
| Women | 17.2% | Marines | 30.5% |
| Marital status | National Guard | 0.9% | |
| Single | 31.8% | Navy | 51.2% |
| Married | 50.9% | Coast Guard | 0.5% |
| Divorced/Separated | 17.3% | ||
| Education | Service operation | ||
| High school/GED | 21.4% | Bosnia | <1% |
| Some college | 43.9% | Djbouti | 2.8% |
| College graduate | 22.8% | Gulf War | 3.1% |
| Associates Degree | 11.9% | Global War on Terror | 11.0% |
| Ethnicity | Kosovo | 1.1% | |
| Hispanic | 24.2% | Latin America | 1.6% |
| Non-Hispanic | 69.2% | Libya | <1% |
| Declined Answer | 6.7% | Somalia | 1.8% |
| Race | OEF | 24.6% | |
| White | 53.6% | OIF | 25.4% |
| Black | 14.7% | OND | 2.4% |
| Pacific Islander/Asian | 13.3% | Other | 3.7% |
| Bi/Multi-Racial | 6.9% | None | 21.5% |
| American Indian/Alaskan | 1.5% | Combat exposure | 53.7% |
| Other | 2.9% | Number of Deployments | 1.93 (1.23) |
| Declined to Answer | 7.1% |
OEF, operation enduring freedom; OIF, operation Iraqi freedom; OND: operation new dawn.
Prevalence of insomnia disorder and clinical characteristics
Table 2 shows the sample sizes and percentages of veterans screening positive for insomnia disorder, PTSD, depression, suicidal ideation, alcohol misuse, TBI, MST, and clinically significant pain. We found 57.2% of the sample had insomnia disorder using clinical cutoff scores (ISI ≥ 11) versus 40.5% who screened positive when using a more conservative cutoff ISI ≥ 15; 31.5% of the sample showed no insomnia (ISI ≤ 9). The rates in women and men were 59.6% and 56.6%, respectively. Up to 69.6% of the sample were above the cutoff for other clinically significant conditions including PTSD, depression, alcohol misuse, TBI, MST, and clinically significant pain.
Table 2.
Prevalence of insomnia disorder and clinical characteristics (N = 5,552)
| Variable (n = sample size) | Total %*/M (SD) |
|---|---|
| ISI ≥ 11 (N = 5,552) | 57.2% |
| ISI ≥ 15—Moderate to Severe | 40.5% |
| PCL-C (n = 3,918) | 36.57 (19.29) |
| PCL-C ≥ 44 | 32.2% |
| PCL-5 (n = 1,480) | 25.44 (22.62) |
| PCL-5 ≥ 33 | 35.8% |
| Combined PCL above cutoff | 33.2% |
| PHQ-9 ≥ 15 (N = 5,552) | 23.3% |
| Suicidal ideation > 0 (n = 5,532) | 14.6% |
| Audit C | |
| Male (n = 3,982) | 3.53 (2.71) |
| % ≥ 4 | 44.9% |
| Female (n = 827) | 2.47 (2.34) |
| % ≥ 3 | 39.4% |
| TBI positive (n = 5,366) | 25.14% |
| MST positive (n = 3,423) | 11.7% |
| Pain ≥ 4 | 69.6% |
ISI, insomnia severity index; MST, military sexual trauma; PTSD, posttraumatic stress disorder; PCL, PTSD clinician checklist; TBI, traumatic brain injury; PHQ9, patient health questionnaire 9-Item depression module; Audit, alcohol use disorders identification test.
Percentages based on the clinical cutoffs for each of the measures.
Demographic correlates
Table 3 shows the percentages and statistics of insomnia disorder by demographic categories. The percentages of veterans screening positive for insomnia disorder did not differ by sex or ethnicity. However, there were differences by marital status, race, and branch of service. While older age showed statistically higher insomnia, the effect size was very small. Married or separated veterans had higher rates of insomnia disorder than individuals who were single, although effect sizes were small. Veterans of all other races showed higher rates of insomnia disorder compared to White veterans, with small effect sizes. Veterans of the Air Force endorsed lower levels of insomnia disorder compared with veterans of the Navy, with a very small effect size.
Table 3.
Demographic characteristics by insomnia disorder
| Characteristics | ISI < 11 | ISI ≥ 11 | Stats | Effect size Cohen’s d/Cramer’s V |
|---|---|---|---|---|
| Age | 34.32 (9.35) | 35.17 (8.84) | t = −3.43 (p < 0.001)* | r = 0.09 |
| Sex | X2 = 2.70 (p = 0.10) | V = 0.02 | ||
| Men | 43.4% | 56.6% | ||
| Women | 40.4% | 59.6% | ||
| Marital status | X2 = 94.58 (p < 0.001)* | V = 0.14 | ||
| Single† | 51.7% | 48.3% | ||
| Married | 40.9% | 59.1% | X2 = 48.65 (p < 0.001)* | V = 0.11 |
| Separated | 32.8% | 67.2% | X2 = 84.13 (p < 0.001)* | V = 0.18 |
| Ethnicity | X2 = 0.612 (p = 0.737) | V = 0.01 | ||
| Hispanic | 41.7% | 58.3% | ||
| Non-Hispanic | 43.0% | 57% | ||
| Race | X2 = 72.26 (p < 0.001)* | V = 0.12 | ||
| White† | 47.3% | 52.7% | ||
| Black | 34.2% | 65.8% | X2 = 43.74 (p < 0.001)* | V = 0.11 |
| Pacific Islander | 30.2% | 69.8% | X2 = 6.11 (p = 0.01)* | V = 0.01 |
| Asian | 42.2% | 57.8% | X2 = 5.59 (p = 0.02)* | V = 0.04 |
| Bi/Multi-Racial | 33.5% | 66.5% | X2 = 25.30 (p < 0.001)* | V = 0.09 |
| American | 32.9% | 67.1% | X2 = 9.21 (p = 0.002)* | V = 0.06 |
| Indian/Alaskan | ||||
| Service/branch | X2 = 17.95 (p = 0.003)* | V = 0.06 | ||
| Navy† | 43.4% | 56.6% | ||
| Army | 41.3% | 58.7% | X2 = 1.05 (p = 0.31) | V = 0.02 |
| Air Force | 55.0% | 45.0% | X2 = 10.63 (p < 0.001)* | V = 0.06 |
| Marines | 40.9% | 59.1% | X2 = 2.63 (p = 0.11) | V = 0.02 |
| National Guard | 35.3% | 64.7% | X2 = 1.35 (p = 0.25) | V = 0.02 |
| Coast Guard | 50.0% | 50.0% | X2 = 0.46 (p = 0.50) | V = 0.01 |
Significant p < .05.
Comparison group for all analyses.
Clinical correlates
Figure 1 shows percentages of insomnia disorder by clinical correlates and Table 4 shows percentages and statistics. Neither the number of deployments, nor screening positive for alcohol misuse showed differences in screening positive for insomnia disorder. Veterans who screened positive for PTSD, depression, suicidal ideation, TBI, MST, clinically significant pain, or having exposure to combat showed higher rates of insomnia disorder. Screening positive for PTSD or MST showed large effect sizes, depression, suicidal ideation, and pain showed medium effects, while TBI and combat exposure showed small effect sizes. PTSD and depression scores were highly correlated (r (5,481) = .85, p < 0.001) suggesting they may be overlapping constructs or disorders.
Figure 1.
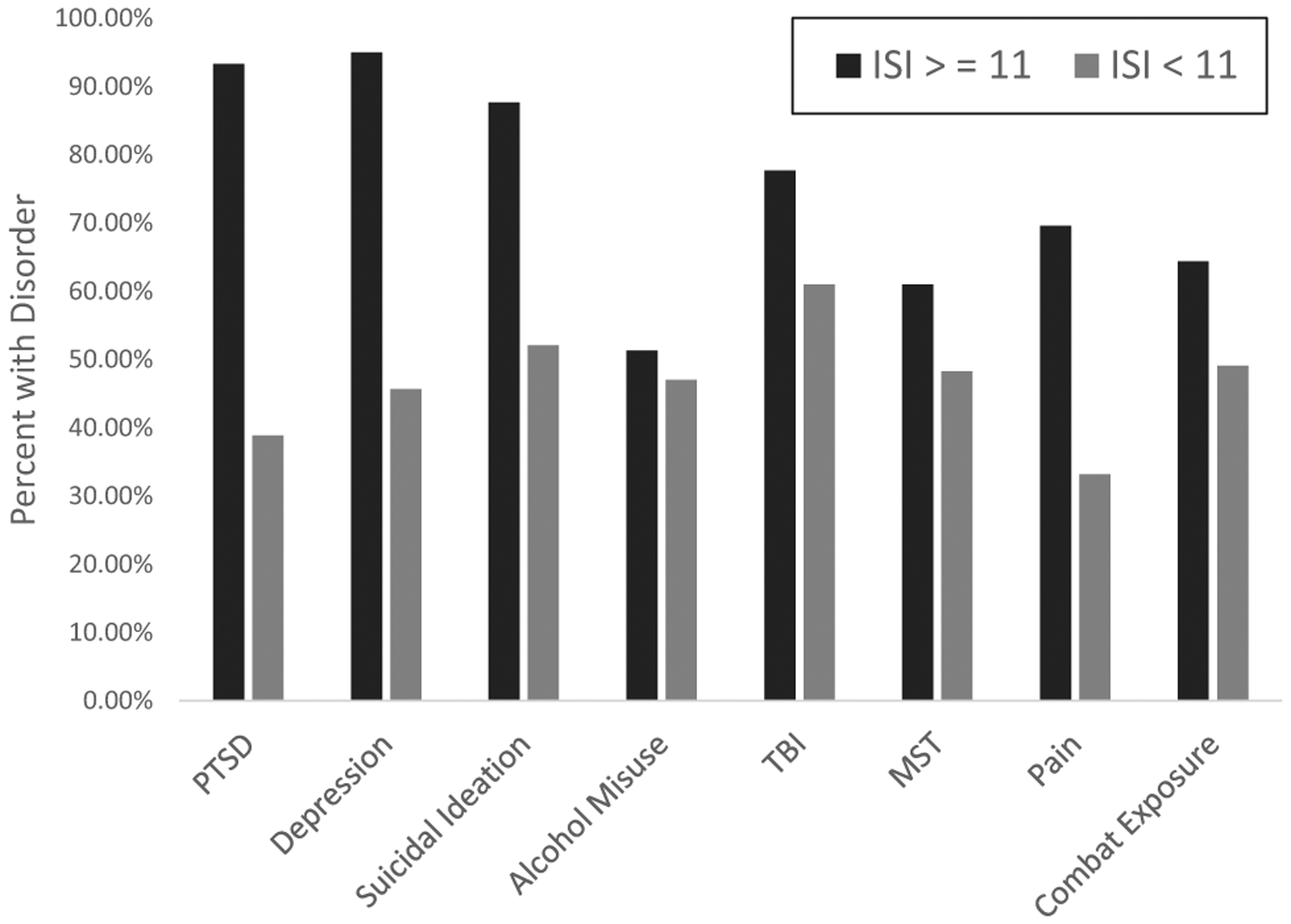
Percentage of clinical correlates by insomnia disorder.
Table 4.
Clinical correlates by insomnia disorder
| Characteristics | ISI < 11 | ISI ≥ 11 | Stats | Effect size Cohen’s d/Cramer’s V |
|---|---|---|---|---|
| # of Deployments | 1.89 (1.21) | 1.96 (1.24) | t = −1.47 (p = 1.41) | r = 0.06 |
| Combat exposure | X2 = 132.06 (p < 0.001)* | V = 0.16 | ||
| Yes | 35.6% | 64.4% | ||
| No | 50.9% | 49.1% | ||
| PTSD | X2 = 1,445.16 (p < 0.001)* | V = 0.52 | ||
| PCL+ | 6.7% | 93.3% | ||
| PCL− | 61.1% | 38.9% | ||
| Depression | X2 = 970.37 (p < 0.001)* | V = 0.42 | ||
| PHQ9+ | 5.0% | 95.0% | ||
| PHQ9− | 54.3% | 45.7% | ||
| Suicidal ideation | X2 = 356.98 (p < 0.001)* | V = 0.25 | ||
| Ideation+ | 12.3% | 87.7% | ||
| Ideation− | 47.9% | 52.1% | ||
| Alcohol misuse | X2 = 1.89 (p = 0.17) | V = 0.04 | ||
| Audit+ | 48.7% | 51.3% | ||
| Audit− | 53.0% | 47.0% | ||
| TBI | X2 = 57.58 (p < 0.001)* | V = 0.16 | ||
| TBI+ | 22.3% | 77.7% | ||
| TBI− | 39.0% | 61.0% | ||
| MST | X2 = 4.87 (p = 0.02)* | V = 0.70 | ||
| MST+ | 39.9% | 61.0% | ||
| MST− | 51.7% | 48.3% | ||
| Pain | X2 = 489.70 (p < 0.001)* | V = 0.35 | ||
| Pain+ | 29.5% | 69.6% | ||
| Pain− | 66.8% | 33.2% |
Significant p < 0.05.
ISI, insomnia severity index; MST, military sexual trauma; PTSD, posttraumatic stress disorder; PCL, PTSD checklist; TBI, traumatic brain injury; PHQ9, patient health questionnaire 9-Item depression module; Audit, alcohol use disorders identification test.
Discussion
We found that 57.2% of a large sample of post-9/11 veterans entering the VHA screened positive for insomnia disorder, which suggests insomnia disorder is alarmingly common in this population. Given the size of our sample, its sociodemographic representativeness, and the use of an independent, validated, standardized measure of insomnia [43], the prevalence rates reported are the most accurate in post-9/11 veterans using VHA care. Confidence in our findings is further supported with comparison to previous generalizable research that found between 52.3% and 59.1% of veterans seeking care had insomnia disorder [36, 41, 42].
Insomnia is predictive of the development and recurrence of mood disorders [57, 58] and suicidality [59, 60], and is associated with the severity of psychiatric conditions (e.g. PTSD) [36]. Collectively, insomnia disorder is a risk factor for the most common medical and MH conditions seen in veterans, yet, insomnia disorder often goes unscreened and untreated in the VHA. The need to increase insomnia screening using independent measures for all veterans and offer evidence-based treatment is critical and is consistent with recommendations made by VA clinical practice guidelines [61].
The discrepancy between actual prevalence rates of insomnia disorder and what providers are documenting is larger than previously thought. Medical record codes have found rates 2.5% and 3.4% [23, 30], while we found 57.2% using an independent measure of insomnia. This confirms and expands on the finding that fewer than half of VHA providers routinely include insomnia in the encounter problem list [35]. Grandner and Chakravorty [29] suggest that many providers consider insomnia a symptom or secondary condition of a “primary disorder” rather than a comorbid diagnosis. Providers often focus on treating the “root cause” of insomnia (e.g. PTSD, pain) instead of targeting perpetuating factors (e.g. conditioned arousal), which is necessary for effective insomnia treatment.
The prevalence rates in this study were also markedly different than studies that used a single questionnaire item of “trouble falling or staying asleep” [18, 31–33]. The differences could be based on different samples (e.g. military vs. veteran or Vietnam era vs. post-9/11), co-occurring disorders, and age. However, a single item about sleep is not a validated measure, misses the chronic relationship between sleep and dissatisfaction, interference with daily life, and cognitive shift or anxiety involved with insomnia disorder [34]. As such, the use of insomnia or even insomnia symptoms when using a single sleep item can be misleading when trying to assess prevalence rates in various populations. We suggest regular use of validated insomnia questionnaires, as well as clearer guidelines on insomnia language in peer-reviewed publications.
Veterans who screened positive for MH disorders, increased combat exposure, positive for TBI and MST, and higher pain had considerably higher rates of insomnia disorder, consistent with previous literature [19, 41, 62, 63]. Interestingly, neither the number of deployments, nor screening positive for alcohol misuse, showed differences in screening positive for insomnia disorder. Our study also found that screening positive for suicidal ideation was strongly associated with insomnia disorder. Further, screening positive for PTSD and depression was associated with incredibly high rates of insomnia disorder. There are several possibilities for this finding. First, the higher prevalence of insomnia reported here, as compared to previous papers, may reflect high rates of combat exposure (53.7%) in our sample. Second, the co-occurrence of high PTSD and depression may have an additive effect in insomnia prevalence. Third, it is possible that while the ISI ≥ 11 is a reliable cutoff for a clinical sample, the cutoff for a more complex PTSD veteran sample needs to be higher (e.g. ≥15).
Our study suggests a critical need to increase evidence-based treatments for insomnia, especially in individuals with co-occurring disorders; this may be especially pertinent to help combat suicidal ideation in veterans [64, 65]. Cognitive behavioral therapy for insomnia (CBT-I) is considered the front-line treatment for insomnia [66] and is better than pharmacological interventions [67] with longer lasting positive outcomes [68]. Despite clear recommendations in the Department of Veterans Affairs/Department of Defense (VA/DOD) Clinical Practice guidelines [61], access to CBT-I as the standard of care for insomnia disorder is limited [69]. There is even increasing evidence in support of integrated treatment, providing CBT-I plus evidence-based treatment for the primary presenting disorder [70]. Together examining and treating insomnia disorder in the context of co-occurring disorders, especially PTSD, depression, and suicidal ideation in the VHA system is a necessity.
This study has several limitations. First, this sample of post-9/11 veterans may not be representative of veterans of all ages and eras using the VHA, or veterans who choose to receive their healthcare outside the VHA. Second, data were collected at time of registration for VA healthcare and not in specific clinics, limiting knowledge of what type of care veterans sought or our ability to address differences in veterans seeking mental versus physical health care. It is possible that not everyone presenting for enrollment was screened, meaning our findings may be impacted by self-selection bias. Finally, we were unable to screen for obstructive sleep apnea (OSA), which is highly co-occurring with insomnia as well as physical and MH correlates we examined, even in younger healthier veterans [71]. As such, the presence of OSA may influence insomnia prevalence rates, especially with co-occurring disorders [34].
While our sample was comprised only of post-9/11 veterans, the relevance of our cohort characteristics will only increase as they increasingly represent the veteran population using the VHA system in the future. The prevalence rates suggest that a considerable proportion of veterans enrolling in VA healthcare have clinically significant levels of insomnia. Despite clear recommendations in the VA/DOD Clinical Practice guidelines [61], access to CBT-I as the standard of care for insomnia disorder alone or with co-occurring disorders is limited [69]. Our findings, suggest heightened need for insomnia screening, documentation, and access to independent and direct interventions for insomnia in veterans entering the VHA system. Targeted efforts to increase veteran access to CBT-I, and behavioral sleep medicine, are essential in forestalling the array of adverse health consequences of chronic insomnia disorder.
Statement of Significance.
In an observational study of 5,552 post-9/11 veterans enrolling in the VA Healthcare System (VHA), 57.2% of the veterans were at high risk for insomnia disorder. Veterans with posttraumatic stress disorder, traumatic brain injury, and pain showed highest rates of insomnia disorder (93.3%, 77.7%, and 69.6%, respectively). Given the size of our sample, its sociodemographic representativeness, and the use of an independent, validated, standardized measure of insomnia, the prevalence rates reported are the most accurate in post-9/11 veterans using VHA care. Rates of insomnia disorder in post-9/11 veterans is alarmingly high and requires increased attention and direct treatment, especially in the context of co-occurring disorders.
Acknowledgments
The views expressed in this article are those of the authors only and do not reflect the official policy or position of the institutions with which the authors are affiliated, the Department of Veteran’s Affairs, nor the United States Government.
Funding
This material is the result of work supported by Department of Veterans Affairs (VA) Center of Excellence for Stress and Mental Health (CESAMH) and the VA Center for Innovation. This material also is the result of work supported with resources of the VA San Diego Healthcare System and the Durham Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), (CIN 13-410) at the Durham VA Health Care System. Dr. Peter Colvonen is partly funded by VA RR&D CDA Grant #1lK2Rx002120-01. Dr Jessica Tripp is funded by a fellowship in VA Interprofessional Advanced Fellowship in Addiction Treatment supported by the office of academic affiliations.
Footnotes
Disclosure Statement
Financial disclosures: None declared.
Non-Financial disclosure: None of the authors have any competing financial interests to disclose.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed.Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Katz DA, et al. The relationship between insomnia and health-related quality of life in patients with chronic illness. J Fam Pract. 2002;51(3):229–235. [PubMed] [Google Scholar]
- 3.Knutson KL, et al. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buxton OM, et al. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–1036. [DOI] [PubMed] [Google Scholar]
- 5.Xi B, et al. Short sleep duration predicts risk of metabolic syndrome: a systematic review and meta-analysis. Sleep Med Rev. 2014;18(4):293–297. [DOI] [PubMed] [Google Scholar]
- 6.Calhoun DA, Harding SM. Sleep and hypertension. Chest. 2010;138(2):434–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li M, et al. Insomnia and risk of cardiovascular disease: a meta-analysis of cohort studies. Int J Cardiol. 2014;176(3):1044–1047. [DOI] [PubMed] [Google Scholar]
- 8.Dew MA, et al. Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65(1):63–73. [DOI] [PubMed] [Google Scholar]
- 9.Kripke DF, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. [DOI] [PubMed] [Google Scholar]
- 10.Vgontzas AN, et al. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17(4):241–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez-Mendoza J, et al. Insomnia and its impact on physical and mental health. Curr Psychiatry Rep. 2013;15(12):418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Killgore WD, et al. Impaired decision making following 49 h of sleep deprivation. J Sleep Res. 2006;15(1):7–13. [DOI] [PubMed] [Google Scholar]
- 13.Killgore WD, et al. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Med. 2008;9(5):517–526. [DOI] [PubMed] [Google Scholar]
- 14.Pilcher JJ, et al. Effects of sleep deprivation on performance: a meta-analysis. Sleep. 1996;19(4):318–326. [DOI] [PubMed] [Google Scholar]
- 15.Szentkirályi A, et al. Sleep disorders: impact on daytime functioning and quality of life. Expert Rev Pharmacoecon Outcomes Res. 2009;9(1):49–64. [DOI] [PubMed] [Google Scholar]
- 16.Léger D, et al. Societal costs of insomnia. Sleep Med Rev.2010;14(6):379–389. [DOI] [PubMed] [Google Scholar]
- 17.Bramoweth AD, et al. Deployment-related insomnia in military personnel and veterans. Curr Psychiatry Rep. 2013;15(10):401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seelig AD, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33(12):1615–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McLay RN, et al. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in US service members returning from military deployments. Mil Med. 2010;175(10):759–762. [DOI] [PubMed] [Google Scholar]
- 20.Hughes J, et al. Insomnia and symptoms of post-traumatic stress disorder among women veterans. Behav Sleep Med. 2013;11(4):258–274. [DOI] [PubMed] [Google Scholar]
- 21.Fung CH, et al. Prevalence and symptoms of occult sleep disordered breathing among older veterans with insomnia. J Clin Sleep Med. 2013;9(11):1173–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Med. Clin 2013;8(3):281–297. [DOI] [PubMed] [Google Scholar]
- 23.Alexander M, et al. The national veteran sleep disorder study: descriptive epidemiology and secular trends, 2000– 2010. Sleep. 2016;39(7):1399–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ford ES, et al. Trends in insomnia and excessive daytime sleepiness among U.S. adults from 2002 to 2012. Sleep Med. 2015;16(3):372–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hughes JM, et al. Insomnia in United States military veterans: an integrated theoretical model. Clin Psychol Rev. 2018;59:118–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roth T Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 Suppl):S7–10. [PMC free article] [PubMed] [Google Scholar]
- 27.Mysliwiec V, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schutte-Rodin S, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4(5):487–504. [PMC free article] [PubMed] [Google Scholar]
- 29.Grandner MA, et al. Insomnia in primary care: misre-ported, mishandled, and just plain missed. J Clin Sleep Med. 2017;13(8):937–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hermes E, et al. Prevalence, pharmacotherapy and clinical correlates of diagnosed insomnia among Veterans Health Administration service users nationally. Sleep Med. 2014;15(5):508–514. [DOI] [PubMed] [Google Scholar]
- 31.Hoge CW, et al. Mild traumatic brain injury in US soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–463. [DOI] [PubMed] [Google Scholar]
- 32.Seelig AD, et al. Sleep and health resilience metrics in a large military cohort. Sleep. 2016;39(5):1111–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neylan TC, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929–933. [DOI] [PubMed] [Google Scholar]
- 34.Colvonen PJ, et al. Recent advancements in treating sleep disorders in co-occurring PTSD. Curr Psychiatry Rep. 2018;20(7):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ulmer CS, et al. Veterans affairs primary care provider perceptions of insomnia treatment. J Clin Sleep Med. 2017;13(8):991–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jenkins MM, et al. Prevalence and mental health correlates of insomnia in first-encounter veterans with and without military sexual trauma. Sleep. 2015;38(10):1547–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Araújo T, et al. Qualitative studies of insomnia: current state of knowledge in the field. Sleep Med Rev. 2017;31:58–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Faestel PM, et al. Perceived insufficient rest or sleep among veterans: behavioral Risk Factor Surveillance System 2009. J Clin Sleep Med. 2013;9(6):577–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cepeda MS, et al. Clinical relevance of sleep duration: results from a cross-sectional analysis using NHANES. J Clin Sleep Med. 2016;12(6):813–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ulmer CS, et al. A comparison of sleep difficulties among Iraq/Afghanistan theater veterans with and without mental health diagnoses. J Clin Sleep Med. 2015;11(9):995–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Plumb TR, et al. Sleep disturbance is common among servicemembers and veterans of operations enduring Freedom and Iraqi Freedom. Psychol Serv. 2014;11(2):209–219. [DOI] [PubMed] [Google Scholar]
- 42.Martin JL, et al. Estimated prevalence of insomnia among women veterans: results of a postal survey. Womens Health Issues. 2017;27(3):366–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morin CM, et al. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pittman JOE, et al. VA eScreening program: technology to improve care for post-9/11 veterans. Psychol Serv. 2017;14(1):23–33. [DOI] [PubMed] [Google Scholar]
- 45.Bastien CH, et al. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. [DOI] [PubMed] [Google Scholar]
- 46.Weathers FW, et al. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at Annual Convention of the International Society for Traumatic Stress Studies; 1993; San Antonio, TX. [Google Scholar]
- 47.Weathers FW, et al. The PTSD Checklist for DSM-5 (PCL-5). 2013. [Google Scholar]
- 48.Kroenke K, et al. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saunders JB, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. [DOI] [PubMed] [Google Scholar]
- 50.Meneses-Gaya C, et al. The fast alcohol screening test (FAST) is as good as the AUDIT to screen alcohol use disorders. Subst Use Misuse. 2010;45(10):1542–1557. [DOI] [PubMed] [Google Scholar]
- 51.Reinert DF, et al. The alcohol use disorders identification test: an update of research findings. Alcohol Clin Exp Res. 2007;31(2):185–199. [DOI] [PubMed] [Google Scholar]
- 52.Donnelly KT, et al. Reliability, sensitivity, and specificity of the VA traumatic brain injury screening tool. J Head Trauma Rehabil. 2011;26(6):439–453. [DOI] [PubMed] [Google Scholar]
- 53.Kimerling R, et al. The Veterans Health Administration and military sexual trauma. Am J Public Health. 2007;97(12):2160–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haskell SG, et al. Gender differences in rates of depression, PTSD, pain, obesity, and military sexual trauma among Connecticut War Veterans of Iraq and Afghanistan. J Womens Health (Larchmt). 2010;19(2):267–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cohen J Statistical Power for the Social Sciences. Hillsdale, NJ: Laurence Erlbaum and Associates; 1988. [Google Scholar]
- 56.Reynolds G, Shendruk A. Demographics of the U.S. Military. 2018, 2019. [Google Scholar]
- 57.Armitage R Sleep and circadian rhythms in mood disorders. Acta Psychiatr. Scand 2007;115:104–115. [DOI] [PubMed] [Google Scholar]
- 58.Manber R, et al. Insomnia and depression: a multifaceted interplay. Curr Psychiatry Rep. 2009;11(6):437–442. [DOI] [PubMed] [Google Scholar]
- 59.Taylor DJ, et al. Insomnia as a health risk factor. Behav Sleep Med. 2003;1(4):227–247. [DOI] [PubMed] [Google Scholar]
- 60.Sjöström N, et al. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30(1):91–95. [DOI] [PubMed] [Google Scholar]
- 61.VA/DOD. Clinical Practice Guideline for the Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea. 2019. https://www.healthquality.va.gov/guidelines/CD/insomnia/VADoDSleepCPGFinal508.pdf.
- 62.Ouellet MC, et al. Insomnia following traumatic brain injury: a review. Neurorehabil Neural Repair. 2004;18(4):187–198. [DOI] [PubMed] [Google Scholar]
- 63.Mahmood O, et al. Neuropsychological performance and sleep disturbance following traumatic brain injury. J Head Trauma Rehabil. 2004;19(5):378–390. [DOI] [PubMed] [Google Scholar]
- 64.Trockel M, et al. Effects of cognitive behavioral therapy for insomnia on suicidal ideation in veterans. Sleep. 2015;38(2):259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Manber R, et al. Dissemination of CBTI to the non-sleep specialist: protocol development and training issues. J Clin Sleep Med. 2012;8(2):209–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Qaseem A, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–133. [DOI] [PubMed] [Google Scholar]
- 67.Sateia MJ, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(2):307–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Morin CM, et al. Nonpharmacologic treatment of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 1999;22(8):1134–1156. [DOI] [PubMed] [Google Scholar]
- 69.Koffel E, et al. Increasing access to and utilization of cognitive behavioral therapy for insomnia (CBT-I): a narrative review. J Gen Intern Med. 2018;33(6):955–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Colvonen PJ, et al. Piloting cognitive behavioral therapy for insomnia integrated with prolonged exposure. Psychol Trauma. 2019;11(1):107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Colvonen PJ, et al. Obstructive sleep apnea and posttraumatic stress disorder among OEF/OIF/OND veterans. J Clin Sleep Med. 2015;11(5):513–518. [DOI] [PMC free article] [PubMed] [Google Scholar]


