Abstract
Purpose.
To investigate whether life satisfaction and optimism might reduce the risk of suicidal thoughts and behaviors among adolescents with depressive symptoms.
Methods.
Participants were 1,904 youth from the NEXT Generation Health Study, a national sample of U.S. adolescents followed over 7 years from 2009/2010 to 2015/2016. Longitudinal latent profile analysis and logistic regressions were conducted.
Results.
We identified three subgroups of adolescents with different patterns of depressive symptoms across the first six waves: “Low” (40%), “Mild” (42%), and “Moderate to Severe” (18%). The Moderate to Severe (OR = 14.47, 95% CI [6.61, 31.66]) and Mild (OR = 3.90, 95% CI [2.22, 6.86]) depression profiles had significantly higher odds of developing suicidality than the Low depression profile. Both life satisfaction and optimism moderated the association between depressive symptom profile and suicidality. The difference in suicidality risk between the Mild and Low depression profiles was significantly attenuated at high versus low levels of life satisfaction, with a difference of −0.08, 95% CI [−0.14, −0.03]. In addition, the difference in suicidality risk between the Moderate to Severe and Low depression profiles was attenuated at high versus low levels of optimism, with a difference of −0.11, 95% CI [−0.21, −0.01].
Conclusions.
For adolescents transitioning to young adulthood, resilience factors such as life satisfaction and optimism may buffer against suicidality risk in the face of mild or moderate to severe depressive symptoms.
Keywords: Depression, life satisfaction, optimism, risk factor, resilience factor, suicidal ideation, suicide plan, suicide attempt
Suicide is the second leading cause of death in people aged 15–29 years [1]. Prevention of this important public health problem relies on accurate identification of risk and protective factors [2]. Depression is one of the strongest risk factors for suicide and routine depression screening at health maintenance visits is recommended for adolescents aged 11 to 21 years [3]. Though depression assessed at a single point in time is predictive of later risk for suicide, modeling the changing or persistent patterns of depressive symptoms across multiple time points may provide additional predictive value [4]. However, few studies have examined how longitudinal trajectories of adolescent depression are associated with subsequent suicidality. In one study, Kerr, Reinke and Eddy [5] used linear growth curve modeling and found that on average there were no increases in adolescents’ depressive symptoms from grades 5 to 10 but the level of depressive symptoms at grade 5 prospectively predicted suicidal ideation and attempts in young adulthood. Several studies used person-centered approaches to identify subgroups of children who had different comorbidity patterns of internalizing (e.g., depression, anxiety) and externalizing (e.g., aggression, delinquency) problems and their suicidal behaviors [6, 7], but these studies did not focus specifically on depression. Therefore, it remains unclear how different profiles of depressive symptoms (e.g., persistently high depression or intermittent patterns) in adolescents predict suicidality during their transition to young adulthood, which would be examined in this study.
Even among adolescents with high levels of depressive symptoms, suicidal thoughts and behaviors might be diminished by having perceptions or beliefs that act as buffers in the face of vulnerability, referred to as the buffering hypothesis of resilience to suicidality [8]. An improved understanding of potential resilience factors that could protect adolescents with depression from developing suicidality may have implications for suicide prevention and intervention efforts. However, the role of resilience factors that may disrupt the negative developmental cascade from depression to suicidality has rarely been examined longitudinally. Several cross-sectional studies have explored resilience to suicidality in the context of depression and found that positive cognitive interpretations of the world, self, and future [9], hope [2], subjective well-being [10], and gratitude [11] buffered the association between depression and suicidality in adolescents or adults. One longitudinal study found that the impact of depression on subsequent suicidal ideation was attenuated among young adults with higher subjective well-being [12].
Here we examine life satisfaction and optimism as potential resilience factors. Life satisfaction is the cognitive component of subjective well-being [13] and optimism reflects positive expectations about one’s future, similar to hope [14]. Both life satisfaction [15] and optimism [16] have been associated with lower risk of suicidality and were found by cross-sectional studies to mitigate the associations of other adversities such as cyberbullying [17] and negative life events [18] with suicidality in adolescents and adults. Thus, even in the context of depression, positive attributes such as life satisfaction and optimism may be beneficial for well-being, including being protective against suicidality; however, their buffering roles in the depression-suicidality link have not been extensively studied using longitudinal designs [19].
Accordingly, the present study examined patterns of adolescents’ depressive symptoms over time using longitudinal latent profile analysis (LLPA) and tested whether specific patterns conferred different risk for suicidality (i.e., suicidal thoughts, plans, or attempts) in young adulthood. LLPA identified groups of adolescents with similar patterns of depressive symptoms across six time points. Subsequent logistic regression analyses examined risks of suicidality within each group, and whether this risk was attenuated if adolescents in each depressive symptom profile had higher levels of life satisfaction and optimism.
Methods
Sample and Data
Data were from the NEXT Generation Health Study, a longitudinal study that enrolled 2,783 U.S. high school students in 10th grade (Mage = 16.31 years; SD = 0.56; range = 14–20) and followed them annually for 7 years (2009/2010 to 2015/2016). The national sample of adolescents was recruited from 81 high schools stratified by nine U.S. census divisions. We conducted the LLPA analysis in the full sample to identify the longitudinal profiles of adolescent depressive symptoms. Questions about suicidal thoughts, plans, and attempts were introduced into the study at Wave 7; thus, only participants at Wave 7 (Mage = 22.61 years; SD = 0.57; range = 20–26) were eligible for the suicidality analysis (n = 2,321). In the Wave 7 sample, 1904 had complete data on all study variables and comprised the final analytic sample for the logistic regression analyses. Participants included in the final sample were similar to those of participants in the Wave 7 or full NEXT sample on all study variables except that the final sample had a relatively lower representation of males (40% vs 42% at Wave 7 and 45% at baseline) and adolescents with low family affluence (22% vs 24% at Wave 7 and 25% at baseline). Informed consent was obtained from parents with adolescent assent and from adolescents after they turned 18 years old. The study was approved by the Institutional Review Board of NICHD.
Measures
Suicidality
Suicidality was measured at Wave 7. Participants were asked whether they had seriously thought about committing suicide, made a plan for committing suicide, and attempted suicide in the past 12 months. Questions were adapted from the World Mental Health Survey Version of the World Health Organization Composite International Diagnostic Interview [20]. Suicidality was defined as positive endorsement of any suicidal thought or behavior (1 = yes; 0 = no).
Depressive symptoms
Depressive symptoms were measured using the 6-item Modified Depression Scale (MDS) [21] at Wave 1 (α = .81) and 8-item Patient-Reported Outcomes Measurement Information System scale (PROMIS) [22] at Waves 2 through 6 (α = .94 to .96) on a 5-point response scale from never to always or almost always. Examples of the MDS items included “How often were you very sad” and “How often were you grouchy or irritable, or in a bad mood.” Examples of the PROMIS items included “I could not stop feeling sad” and “I felt everything in my life went wrong.” PROMIS scores were transformed to T scores according to published norms [23] and MDS scores were standardized to the same mean and standard deviation as the PROMIS T scores (M = 50, SD = 10).
Life satisfaction
Life satisfaction was measured using one item at Wave 6: “In general, how happy are you with how your life is going?” The item was rated on a scale of 0 (I am very unhappy with my life) to 10 (I am very happy with my life) and was standardized in the analysis.
Optimism
Optimism was measured using the Life Orientation Test-Revised [24], which assesses a general positive attitude about the future and a tendency to anticipate favorable outcomes to life situations at Wave 6 (α = .74). Three positively worded items (e.g., “I am always optimistic about my future”) and three negatively worded (reverse-coded) items (e.g., “I hardly ever expect things to go my way”) were each rated on a scale of 1 (Strongly disagree) to 5 (Strongly agree). The standardized mean scores of the six items were used in the analysis.
Sociodemographic covariates.
Participants’ sex, race/ethnicity, age at Wave 7, parental education, and family affluence were included as demographic covariates. Race/ethnicity was categorized as White, Black, Hispanic, and Other (i.e., Asian, American Indians, Native Hawaiian and Pacific Islander, and Multiracial). Parental education was reported by the consenting parent and defined by the highest education level of the participant’s mother or father. Responses included 1 (high school or lower), 2 (some college or associate’s degree), and 3 (bachelor’s degree or higher). Family affluence was measured by adolescents’ perceptions of family wealth or socioeconomic status through the sum of items about family car (range = 0–2) and computer ownership (range = 0–3), whether participants had their own bedrooms (0 or 1), and frequency of family holidays (range = 0–3) [25] and the composite score was then categorized into three levels: low (score = 0–2), medium (score = 3–5), and high (score = 6–9).
Analysis Plan
LLPA was conducted to identify subgroups of adolescents with similar depressive symptom trajectories across the first six waves of the study in Mplus Version 8. This approach is advantageous because it does not impose a specific functional form on the trends in depressive symptoms over time (e.g., linear, quadratic) [26]. Missing data were handled by full information maximum likelihood estimation. LLPA solutions were evaluated for model fit and classification quality. Better model fit was indicated by lower values of model fit statistics [27]: Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and sample-adjusted BIC (SABIC). The Lo-Mendell-Rubin likelihood ratio test (LMR LRT) was used to test whether there was a statistically significant improvement in model fit with the inclusion of each additional class/profile. BIC and SABIC were given priority in determining the optimal number of classes given their better performance compared to other fit indices, particularly given the uncertainty of the LMR LRT test in complex designs as in this study [27]. The posterior probabilities of profile membership and entropy were used to assess the quality of membership classification, with values closer to 1 indicating better classification. The posterior probabilities were also used to assign each individual to their best-fitting longitudinal profile of depressive symptoms.
Next, we used the results of the LLPA to investigate the association between longitudinal depressive symptoms and suicidality. This was done by fitting a logistic regression model of suicidality with depressive symptom profile as the primary exposure. We then extended this model to investigate the potential buffering effects of life satisfaction and optimism by adding their interactions with depressive symptom profile. The regression coefficients from the logistic model were used to derive probabilities of suicidality for each depressive symptom profile across the range of scores on life satisfaction and optimism, thereby enabling us to formally test the interaction effects on the probability scale using the approach described by Mize [28]. Specifically, by plotting the resulting probabilities (and differences between them) using the margins commands in Stata Version 16, we can visualize how the risk of suicidality varies for each depressive symptom profile when life satisfaction or optimism is low or high. Moreover, using the mlincom command in Stata, we further compared differences in the risk of suicidality across depressive symptom profiles at low and high levels of life satisfaction and optimism to infer the significance of interactions on the probability scale. All analyses accounted for the study’s clustered sampling design and incorporated its sampling and nonresponse weights.
Results
In the final analytic sample, 60% were female with an average age of 22.58 (SD = 0.56, range = 20–26). The race/ethnic groups were White (41%), Black (21%), Hispanic (30%), and Other (7%). The highest parental education levels were high school or lower (36%), some college or associate’s degree (38%), and bachelor’s degree or higher (26%). About 30% of the adolescents had low, 48% had medium, and 22% had high family affluence. The correlation between life satisfaction (M = 7.53, SD = 2.04, range = 0–10) and optimism (M = 3.39, SD = 0.71, range = 1–5) was r = .42. Adolescents’ past-year suicidality prevalence was 8%, largely consisting of suicidal thoughts (7.5%) but also representing plans (0.4%) and attempts (1.6%).
Longitudinal Profiles of Depressive Symptoms
Model fit statistics from the five LLPA models are shown in Table 1. From the 1-class to 3-class models, decreases in AIC, BIC, and SABIC values were relatively large, but decreases from the 3-class to 5-class models were negligible and did not justify greater model complexity. The LMR LRT was significant for the 2-class model but not significant for 3-class to 5-class models. However, we prioritized BIC and SABIC and selected the 3-class LLPA model for further analysis. The minimum probability of correct classification of profile membership was adequate (.83) and entropy was medium to high (.71) for the 3-class LLPA model.
Table 1.
Model Fit Statistics from the Longitudinal Latent Profile Analyses of Depressive Symptoms Across the First Six Waves.
| AIC | BIC | SABIC | LMR LRT p value | Entropy | Minimum Probabilities | |
|---|---|---|---|---|---|---|
| 1-Class | 106765.66 | 106836.83 | 106798.70 | N/A | N/A | N/A |
| 2-Class | 103393.39 | 103506.07 | 103445.70 | < .001 | 0.76 | 0.91 |
| 3-Class | 102740.69 | 102894.88 | 102812.27 | .153 | 0.71 | 0.83 |
| 4-Class | 102662.98 | 102858.69 | 102753.83 | .052 | 0.72 | 0.80 |
| 5-Class | 102362.23 | 102599.45 | 102472.36 | .055 | 0.72 | 0.67 |
Note: AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; SABIC = Sample-Adjusted Bayesian Information Criterion. LMR LRT = Lo-Mendell-Rubin Likelihood Ratio Test. Lower AIC, BIC, and SABIC are considered fit. Significant LMR LRT indicates the k+1 model fits the data better than the k model. Entropy and probabilities closer to 1 are considered better quality of profile classification. Classification probabilities >= .70 are considered acceptable. There is no clear cut-off point for the value of entropy to ensure a minimum level of good classification but a value of 0.80 is considered high, 0.60 is considered medium, and 0.40 is considered low entropy.
The three depression profiles are shown in Figure 1. The average levels of depressive symptoms in each profile were relatively stable over time, but there were slightly different patterns of fluctuations, which might not be captured with imposition of a linear or quadratic trend on the data. Based on the clinical cutoff values for PROMIS and other depressive symptom measures [23], the profiles were best characterized as having “Low” (n = 868; 40%), “Mild” (n = 962; 42%), and “Moderate to Severe” (n = 401; 18%) depressive symptoms. Adolescents’ mean levels of depressive symptoms (T scores) across time were 40 to 45 for the Low profile, 51 to 54 for the Mild profile, and 61 to 64 for the Moderate to Severe profile.
Figure 1.
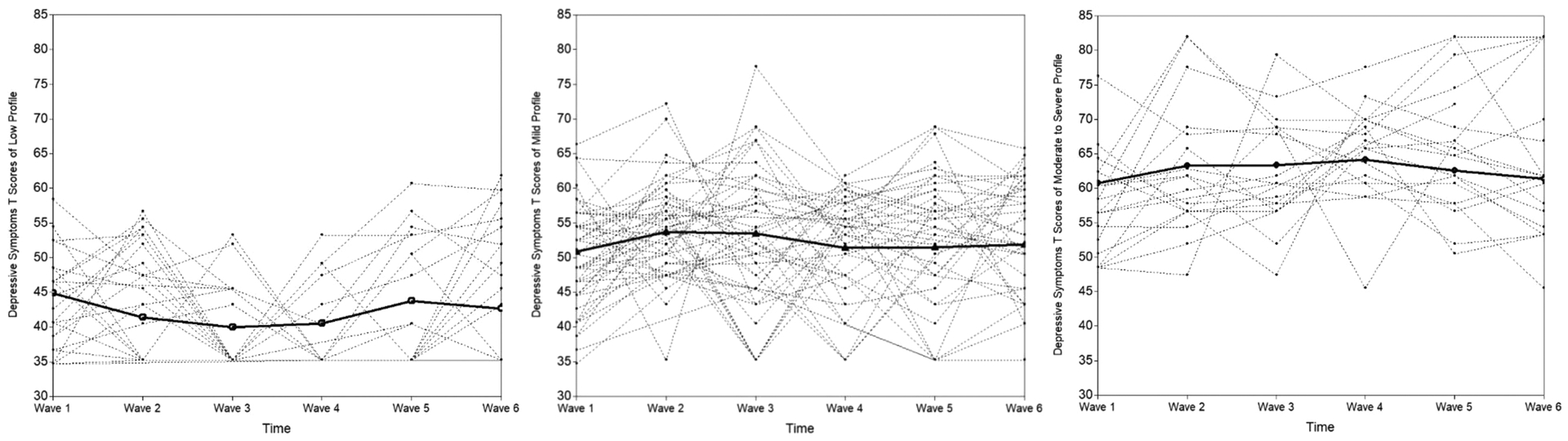
Longitudinal profiles of adolescents’ depressive symptoms from Wave 1 to Wave 6.
Note: The plot was based on 100 randomly selected individuals, specifically, about 30 individuals in the Low depression profile (1a), 47 individuals in the Mild depression profile (1b), and 23 individuals in the Moderate to Severe depression profile (1c).
Depressive Symptom Profiles and Risk of Suicidality
The past-year prevalence of suicidality for the three depression profiles was 2% among participants in the Low profile, 7% among participants in the Mild profile, and 20% among participants in the Moderate to Severe profile. In a logistic regression model adjusting for demographic factors (Table 2), adolescents in the Moderate to Severe (OR = 14.47, 95% CI [6.61, 31.66]) and Mild (OR = 3.90, 95% CI [2.22, 6.86]) profiles had higher odds of suicidality than adolescents in the Low profile. The odds ratios for suicidality were not substantially changed after satisfaction and optimism were added to the model (Table 2).
Table 2.
Results of Logistic Regression Models Predicting Wave 7 Suicidality.
| Model 1: Depression and Covariates | Model 2: Moderators Added | Model 3: Interactions Added | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| Depression Profile | Mild | 3.90*** | 2.22 | 6.86 | 5.04** | 1.93 | 13.14 | 4.24** | 1.47 | 12.24 |
| Moderate to Severe | 14.47*** | 6.61 | 31.66 | 14.45*** | 4.38 | 47.70 | 16.30*** | 4.88 | 54.53 | |
| Ref: Low | 1 | 1 | 1 | |||||||
| Adolescent Sex | Female | 0.92 | 0.43 | 1.96 | 1.25 | 0.63 | 2.50 | 1.21 | 0.62 | 2.37 |
| Ref: Male | 1 | 1 | 1 | |||||||
| Race/Ethnicity | Black | 0.49 | 0.17 | 1.44 | 0.68 | 0.22 | 2.11 | 0.69 | 0.23 | 2.09 |
| Hispanic | 0.83 | 0.62 | 1.11 | 0.84 | 0.61 | 1.16 | 0.93 | 0.67 | 1.28 | |
| Other | 0.53 | 0.15 | 1.85 | 0.63 | 0.20 | 1.96 | 0.62 | 0.19 | 2.01 | |
| Ref: White | 1 | 1 | 1 | |||||||
| Adolescent Age | 1.14 | 0.70 | 1.86 | 1.31 | 0.80 | 2.13 | 1.25 | 0.76 | 2.06 | |
| Parental Education | Some college | 0.62 | 0.29 | 1.35 | 0.54 | 0.23 | 1.26 | 0.56 | 0.25 | 1.25 |
| >=Bachelor’s degree | 0.73 | 0.32 | 1.65 | 0.57 | 0.24 | 1.38 | 0.56 | 0.24 | 1.29 | |
| Ref: <=High school | 1 | 1 | 1 | |||||||
| Family Affluence | Medium | 1.39 | 0.74 | 2.61 | 1.62 | 0.93 | 2.84 | 1.62 | 0.92 | 2.86 |
| High | 2.04 | 0.65 | 6.39 | 2.39 | 0.82 | 6.95 | 2.41 | 0.88 | 6.66 | |
| Ref: Low | 1 | 1 | 1 | |||||||
| Life Satisfaction | 0.75 | 0.53 | 1.06 | 0.61* | 0.42 | 0.88 | ||||
| Optimism | 0.76* | 0.58 | 1.00 | 0.95 | 0.32 | 2.89 | ||||
| Life Satisfaction × Mild Depression | 0.71 | 0.39 | 1.30 | |||||||
| Life Satisfaction × Moderate to Severe | 1.63* | 1.06 | 2.51 | |||||||
| Optimism × Mild Depression | 0.94 | 0.29 | 3.03 | |||||||
| Optimism × Moderate to Severe | 0.73 | 0.23 | 2.30 | |||||||
Note: Ref = Reference group. OR = Odds Ratio. CI = Confidence Intervals.
p < .05.
p < .01.
p < .001.
Life satisfaction and optimism were standardized (Mean = 0, SD = 1).
Moderators in the Depression-Suicidality Link
We fit the final logistic model by adding interactions of the depression profiles with life satisfaction and optimism to the model (Table 2). There was a significant interaction on the logit scale between depression profile and life satisfaction in predicting suicidality, F (2, 19) = 4.54, p = .024. Figure 2a shows that the suicidality risk of the Mild profile decreased as the level of life satisfaction increased, in contrast to suicidality risk in Low and Moderate to Severe profiles, which did not change substantially. As a result, as the level of life satisfaction increased the difference in the suicidality risk between Mild and Low profiles became smaller (Figure 2b), showing a stronger buffering effect at higher versus lower levels of life satisfaction. Specifically, at lower levels of life satisfaction (−1 SD), the Mild depression profile had significantly higher probability of suicidality (0.12) than the Low profile (0.02), with a difference of 0.10, p = .001, 95% CI [0.05, 0.15]; but at higher levels of life satisfaction (+1 SD), adolescents in the two profiles had similar probability of suicidality (0.03 versus 0.01), with a difference of 0.02, p = .114, 95% CI [−0.01, 0.04]. The association of Mild (vs Low) depression with suicidality risk was significantly weaker at high versus low levels of life satisfaction, with a difference of −0.08, p = .004, 95% CI [−0.14, −0.03]. However, the Moderate to Severe profile had significantly higher probability of suicidality than the Low profile, even at very high levels (e.g., +2 SD) of life satisfaction (Figure 2).
Figure 2.
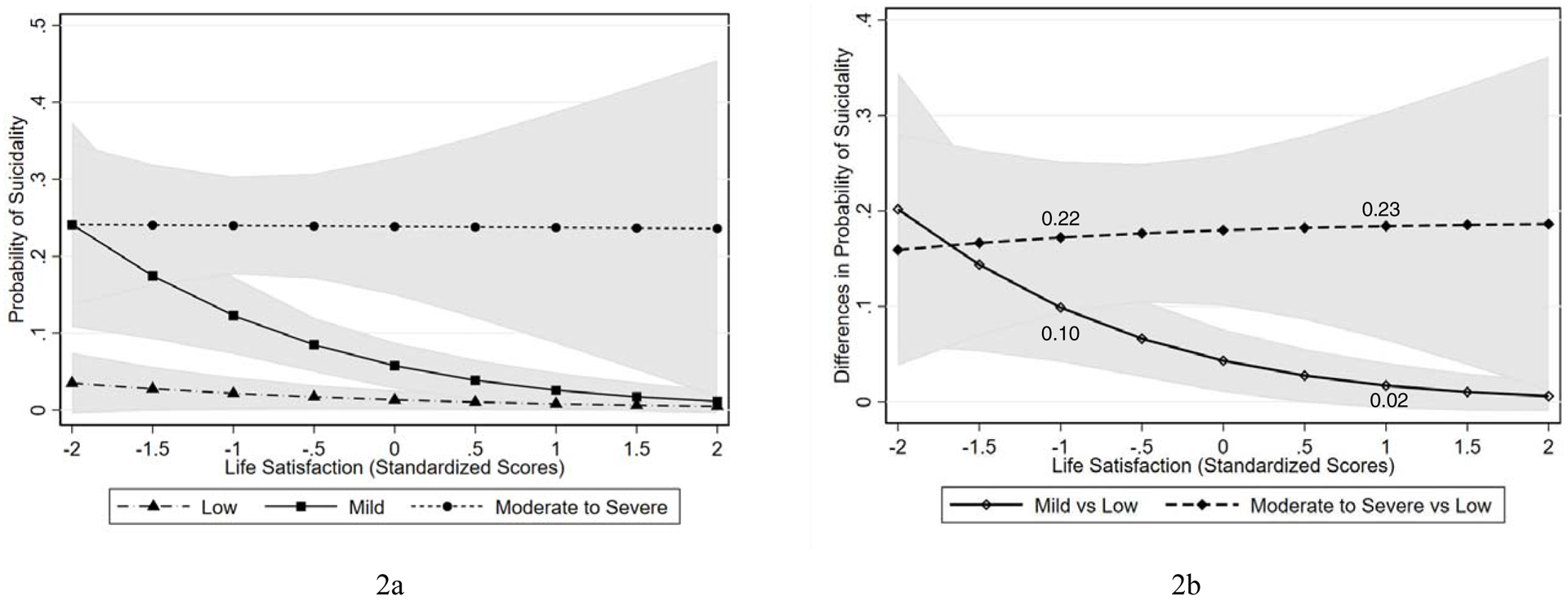
Risk of suicidality across depressive symptom profiles at different levels of life satisfaction
Note: Results of the logistic regression analysis, converted into probabilities, were used to evaluate the buffering effect of life satisfaction in the association between depressive symptom profile and risk of suicidality. Figure 2a shows that the risk of suicidality in the Mild depression profile decreased as the level of life satisfaction increased, whereas the suicidality risk of the Moderate to Severe and Low depression profiles did not change appreciably as the level of life satisfaction increased. Figure 2b shows that differences in the suicidality risk between the Mild and Low depression profiles decreased (i.e., a stronger buffering effect) as the level of life satisfaction increased, whereas risk differences between the Moderate to Severe and Low depression profiles did not change much as the level of life satisfaction increased.
There was not significant interaction between depression profile and optimism on the logit scale, F (2, 19) = 0.50, p = .617, but on the probability scale, there was evidence supporting effect modification. Figure 3a shows that the suicidality risk of the Moderate to Severe profile decreased as the level of optimism increased and Figure 3b shows that the buffering effect became stronger (i.e., differences in the suicidality risk between the Moderate to Severe and Low profiles became smaller) as the level of optimism increased. Specifically, at lower levels of optimism (−1 SD), the Moderate to Severe profile (0.25) had significantly higher probability of suicidality than the Low profile (0.01), with a difference of 0.23, 95% CI [0.16, 0.31]. At higher levels of optimism (+1 SD), the Moderate to Severe profile (0.138) also had higher probability of suicidality than the Low profile (0.01), with a difference of 0.13, 95% CI [0.04, 0.22]; however, the association of Moderate to Severe (vs Low) depression with suicidality was weaker at high versus low levels of optimism, with a difference of −0.11, 95% CI [−0.21, −0.01]. Moreover, at very high levels (e.g., +2 SD) of optimism, the three depression profiles did not differ in their risk for suicidality (Figure 3).
Figure 3.
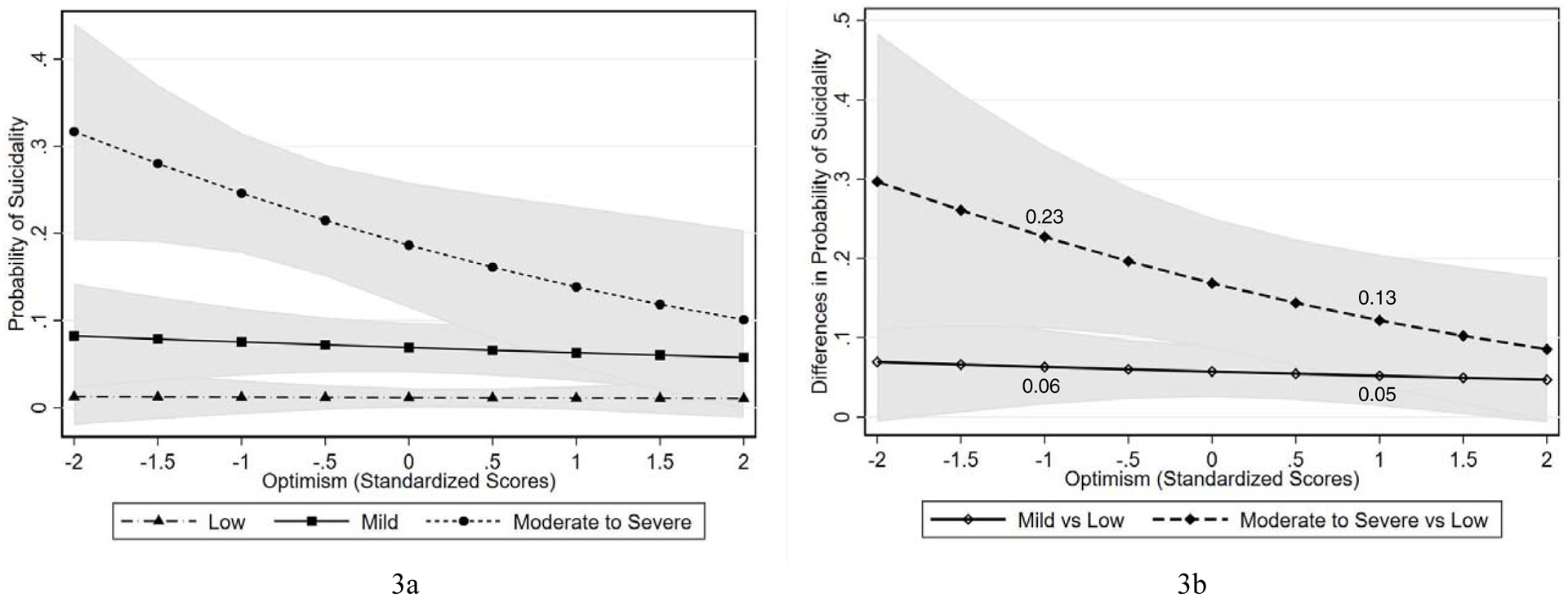
Risk of suicidality across depressive symptom profiles at different levels of optimism
Note: Results of the logistic regression analysis, converted into probabilities, were used to evaluate the buffering effect of optimism in the association between depressive symptom profile and risk of suicidality. Figure 3a shows that risk of suicidality of the Moderate to Severe depression profile decreased as the level of optimism increased, whereas the suicidality risk of the Mild and Low depression profiles did not change much as the level of optimism increased. Figure 3b shows that differences in the suicidality risk between the Moderate to Severe and Low depression profiles decreased (i.e., a stronger buffering effect) as the level of optimism increased, whereas risk differences between the Mild and Low depression profiles did not change much as the level of optimism increased.
Discussion
In a large nationally representative sample of adolescents followed between the ages of 16 and 22, we found three distinct patterns of adolescent depressive symptoms using the person-centered approach of longitudinal latent profile analysis. Adolescents with Mild and Moderate to Severe depressive symptoms had significantly higher risk of past-year suicidality at age 23 years than those with Low depressive symptoms. Moreover, based on the interaction results on the probability scale, high levels of life satisfaction and optimism conferred considerable resilience to suicidality for adolescents with Mild and Moderate to Severe depression, respectively. Specifically, the risk difference between Mild and Low depression profiles was diminished at higher versus lower levels of life satisfaction and the risk difference between Moderate to Severe and Low depression profiles was significantly reduced at higher versus lower levels of optimism. In addition, with very high levels of optimism, adolescents in all depression profiles were at similarly low suicidality risk. The results suggest the protective roles of life satisfaction and optimism by reducing the probability that adolescents with mild or moderate to severe depressive symptoms will develop suicidality.
A recent meta-analysis [4] identified 3 to 11 depression trajectory groups, based on 20 studies published between 2002 and 2015 on longitudinally modeled depressive symptoms in nonclinical populations (average baseline age 12 years). They reported that 56% of the sampled children and adolescents (N = 41,236) on ‘No or low’ depressive symptom trajectories, 26% on a ‘Moderate’ (similar to our Mild profile) trajectory, and less than 12% on ‘High’ (similar to our Moderate to Severe profile) depressive symptom trajectories. The percentages of our higher depressive symptom profiles especially the Moderate to Severe profile were larger perhaps because our data reflected historical trends of increasing mental health problems in adolescents after 2010 and our sample was assessed in middle to late adolescence, when depressive symptoms are more prevalent than in younger children [29].
Extending previous studies that used a variable-centered approach [5], our person-centered analysis also suggested that depression is a strong risk factor for suicidality. That is, adolescents in the Mild and Moderate to Severe depressive symptom profiles had much higher risk of suicidality than those in the Low depression profile. The close depression-suicidality link may be explained by the interpersonal psychological theory of suicide [30] such that adolescents with more depressive symptoms perceive higher burdensomeness to others and lack of belongingness to a social group which in turn lead to their desire to die by suicide. It is also possible that dysfunctional interpersonal relationships (e.g., parental rejection) result in both depression and suicidality among adolescents and young adults [31].
Although depression plays a significant role in suicidality, not every depressed individual develops suicidal thoughts and behavior. Suicidality can also occur in the absence of depression [32]. Importantly, we found evidence suggesting that the depression-suicidality link can be attenuated by resilience factors such as life satisfaction and optimism. Life satisfaction is a core component of subjective well-being and important predictor of hopeful thinking, both of which were found to moderate the depression-suicidality link [2, 12]. Optimism is conceptually related to hope and associated with active and adaptive coping strategies such as attempting to overcome adversity and persisting toward the accomplishment of goals [33]. Optimism is also related to increased attention to positive information and less sustained attention to dysphoric and threatening information [34]. The presence of these positive cognitive, emotional, and behavioral processes may neutralize or cancel some of the deleterious effects of depression, leading to a lower risk of suicidality [2]. Therefore, in addition to treating depression, improving positive well-being in the domains of life satisfaction and optimism may be worthy of including in research on suicide prevention.
On average, adolescents with higher depressive symptoms tended to have lower life satisfaction and optimism, but even in the Moderate to Severe depression group, there were individuals who had relatively high levels (above the mean) of life satisfaction and optimism in our sample. Resilience factors can be strengthened using positive psychology interventions (e.g., mindfulness training, best possible self for optimism intervention). A recent study [35] showed promise in integrating positive psychology interventions with cognitive behavioral therapy to optimize care by addressing depression and supporting psychological strengths and positive emotionality. Examples of their positive psychology intervention strategies included writing gratitude journal, recalling past successes, using personal strengths in new ways, performing acts of kindness, imaging one’s best possible self and starting to work for the future [35]. These practices have the potential to help individuals develop gratitude for the good in their lives, get more connected to family and friends, and develop more positive perceptions of their self-competence, which may in turn improve their overall satisfaction with the current life and their optimistic thinking towards the future [36, 37].
The limitations of this study include insufficient cases to allow separate examinations of suicidal thoughts, plans, and attempts. There may be different etiological processes underlying different manifestations of suicidality [38] which should be addressed by future studies to better inform prevention strategies. In addition, we measured life satisfaction with a single item and its comparability to widely used life satisfaction measures is unknown. It is also a measure for overall life satisfaction without detailed information on specific domains (e.g., satisfaction with family, friends, and work and school performance) which may have differential roles in conferring resilience to suicidality [17]. Having better measures would facilitate a nuanced understanding of specific aspects of life satisfaction and also the study of potentially distinct buffering levels of life satisfaction and optimism. Relatedly, our study relied on self-report scales and the examined relations may be inflated because of same reporter biases. However, the main constructs (suicidality, depressive symptoms, life satisfaction, and optimistic thinking) are self-perceptions usually measured by self-reports and there may not be a better way to capture them. Finally, we had to use posterior probabilities to classify each individual into a depression profile in order to estimate the buffering effects on the probability scale in Stata. This approach did not allow us to account for the uncertainty in class/profile membership.
The buffering hypothesis of resilience to suicidality [8] provided a useful framework for the study of suicide risk and resilience factors. However, most previous studies testing the buffering hypothesis relied on small sample sizes and/or cross-sectional designs. By following the best practices in estimating and interpreting interactions from the logistic regression analysis in terms of probabilities [28], our study provided proper empirical evidence for the buffering roles of the two resilience factors in the developmental cascade from depression to suicidality. Our study replicated the consistent observation that depression is a strong predictor of suicidal thoughts and behaviors, and provided support for the hypothesis that the presence or absence of positive psychological attributes plays a role in determining whether adolescents with higher depressive symptoms will ultimately escalate to exhibit suicidal thoughts or behaviors. These findings may have implications for prevention and intervention efforts. Supporting the emerging field of positive suicidology [39], our findings are consistent with the idea that positive psychology interventions may complement existing evidence-based approaches such as cognitive behavioral therapy to reduce suicidality. If found to be effective, interventions designed to improve positive attributes like optimism and life satisfaction could also be attractive because they could be implemented more broadly than interventions tailored to individuals with high levels of symptoms and would not rely on implementation by practitioners in clinical settings. Further work is needed to evaluate if they should be incorporated into existing population-based strategies for suicide prevention particularly among young people [40].
Implications and Contribution.
This study identified three longitudinal patterns of adolescent depressive symptoms over a 6-year period which subsequently predicted their suicidal thoughts or behaviors in young adulthood. Findings also provided empirical support for the importance of evaluating resilience factors (life satisfaction and optimism) in suicide prevention and intervention studies.
Acknowledgement
This research (contract number HHSN275201200001I) was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and the National Heart, Lung and Blood Institute (NHLBI), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and Maternal and Child Health Bureau (MCHB) of the Health Resources and Services Administration (HRSA), with supplemental support from the National Institute on Drug Abuse (NIDA).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical trials registration: NCT01031160, http://www.clinicaltrials.gov
There are no potential conflicts of interest associated with this article.
Reference
- [1].Organization WH. Suicide in the world: global health estimates. World Health Organization; 2019. Available at: https://apps.who.int/iris/handle/10665/326948 [Google Scholar]
- [2].Hirsch JK, Visser PL, Chang EC, et al. Race and ethnic differences in hope and hopelessness as moderators of the association between depressive symptoms and suicidal behavior. J Am Coll Health 2012;60:115–125. DOI: 10.1080/07448481.2011.567402 [DOI] [PubMed] [Google Scholar]
- [3].Shain B. Suicide and suicide attempts in adolescents. Pediatr 2016;138. DOI: 10.1542/peds.2016-1420 [DOI] [PubMed] [Google Scholar]
- [4].Shore L, Toumbourou JW, Lewis AJ, et al. Review: Longitudinal trajectories of child and adolescent depressive symptoms and their predictors - a systematic review and meta-analysis. Child Adolesc Ment Health 2018;23:107–120. DOI: 10.1111/camh.12220 [DOI] [PubMed] [Google Scholar]
- [5].Kerr DC, Reinke WM, Eddy JM. Trajectories of depressive symptoms and externalizing behaviors across adolescence: associations with histories of suicide attempt and ideation in early adulthood. Suicide Life Threat Behav 2013;43:50–66. DOI: 10.1111/j.1943-278X.2012.00127.x [DOI] [PubMed] [Google Scholar]
- [6].Hart SR, Van Eck K, Ballard ED, et al. Subtypes of suicide attempters based on longitudinal childhood profiles of co-occurring depressive, anxious and aggressive behavior symptoms. Psychiatry Res 2017;257:150–155. DOI: 10.1016/j.psychres.2017.07.032 [DOI] [PubMed] [Google Scholar]
- [7].Duprey EB, Oshri A, & Liu S Developmental pathways from child maltreatment to adolescent suicide-related behaviors: The internalizing and externalizing comorbidity hypothesis. Dev Psychopathol 2019; 1–15. DOI: 10.1017/S0954579419000919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Johnson J, Wood AM, Gooding P, et al. Resilience to suicidality: The buffering hypothesis. Clin Psychol Rev 2011;31:563–591. DOI: 10.1016/j.cpr.2010.12.007 [DOI] [PubMed] [Google Scholar]
- [9].Chang H-J, Lin M-F, Lin K-C. The mediating and moderating roles of the cognitive triad on adolescent suicidal ideation. Nurs Res 2007;56:252–259. DOI: 10.1097/01.NNR.0000280611.00997.0e [DOI] [PubMed] [Google Scholar]
- [10].Siegmann P, Teismann T, Fritsch N, et al. Resilience to suicide ideation: A cross-cultural test of the buffering hypothesis. Clin Psychol Psychother 2018;25:e1–e9. DOI: 10.1002/cpp.2118 [DOI] [PubMed] [Google Scholar]
- [11].Kleiman EM, Adams LM, Kashdan TB, et al. Grateful individuals are not suicidal: Buffering risks associated with hopelessness and depressive symptoms. Pers Individ Dif 2013;55:595–599. DOI: 10.1016/j.paid.2013.05.002 [DOI] [Google Scholar]
- [12].Teismann T, Forkmann T, Brailovskaia J, et al. Positive mental health moderates the association between depression and suicide ideation: A longitudinal study. Int J Clin Health Psychol 2018;18:1–7. DOI: 10.1016/j.ijchp.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol 2009;65:467–487. DOI: 10.1002/jclp.20593 [DOI] [PubMed] [Google Scholar]
- [14].Alarcon GM, Bowling NA, Khazon S. Great expectations: A meta-analytic examination of optimism and hope. Pers Individ Dif 2013;54:821–827. DOI: 10.1016/j.paid.2012.12.004 [DOI] [Google Scholar]
- [15].Kamali M, Reilly-Harrington NA, Chang WC, et al. Bipolar depression and suicidal ideation: Moderators and mediators of a complex relationship. J Affect Disord 2019;259:164–172. DOI: 10.1016/j.jad.2019.08.032 [DOI] [PubMed] [Google Scholar]
- [16].Huffman JC, Boehm JK, Beach SR, et al. Relationship of optimism and suicidal ideation in three groups of patients at varying levels of suicide risk. J Psychiatry Res 2016;77:76–84. DOI: 10.1016/j.jpsychires.2016.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Chang Q, Xing J, Ho RTH, et al. Cyberbullying and suicide ideation among Hong Kong adolescents: The mitigating effects of life satisfaction with family, classmates and academic results. Psychiatry Res 2019;274:269–273. DOI: 10.1016/j.psychres.2019.02.054 [DOI] [PubMed] [Google Scholar]
- [18].Hirsch JK, Wolford K, LaLonde SM, et al. Dispositional optimism as a moderator of the relationship between negative life events and suicide ideation and attempts. Cognit Ther Res 2007;31:533–546. DOI: 10.1007/s10608-007-9151-0 [DOI] [Google Scholar]
- [19].O’Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry 2014;1:73–85. DOI: 10.1016/s2215-0366(14)70222-6 [DOI] [PubMed] [Google Scholar]
- [20].Kessler RC, Üstün TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004;13:93–121. DOI: 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Dunn EC, Johnson RM, Green JG. The Modified Depression Scale (MDS): A brief, no-cost assessment tool to estimate the level of depressive symptoms in students and schools. School Ment Health 2011;4:34–45. DOI: 10.1007/s12310-011-9066-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Yeatts KB, Stucky B, Thissen D, et al. Construction of the Pediatric Asthma Impact Scale (PAIS) for the Patient-Reported Outcomes Measurement Information System (PROMIS). J Asthma 2010;47:295–302. DOI: 10.1007/s12310-011-9066-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Choi SW, Schalet B, Cook KF, et al. Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychol Assess 2014;26:513–527. DOI: 10.1037/a0035768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994;67:1063–1078. DOI: 10.1037/0022-3514.67.6.1063 [DOI] [PubMed] [Google Scholar]
- [25].Currie C, Molcho M, Boyce W, et al. Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med 2008;66:1429–1436. DOI: 10.1016/j.socscimed.2007.11.024 [DOI] [PubMed] [Google Scholar]
- [26].Hartl AC, Laursen B, Cantin S, et al. A test of the bistrategic control hypothesis of adolescent popularity. Child Dev 2019;91. DOI: 10.1111/cdev.13269 [DOI] [PubMed] [Google Scholar]
- [27].Wang J, Wang X. Structural equation modeling: applications using Mplus. Chichester, West Sussex England ; Hoboken, N.J.: John Wiley/Higher Education Press, 2012. [Google Scholar]
- [28].Mize T Best Practices for estimating, interpreting, and presenting nonlinear interaction effects. Sociol Sci 2019;6:81–117. DOI: 10.15195/v6.a4 [DOI] [Google Scholar]
- [29].Twenge JM, Joiner TE, Rogers ML, et al. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among U.S. adolescents after 2010 and links to increased new media screen time. Clin Psychol Sci 2017;6:3–17. DOI: 10.1177/2167702617723376 [DOI] [Google Scholar]
- [30].Kleiman EM, Liu RT, Riskind JH. Integrating the interpersonal psychological theory of suicide into the depression/suicidal ideation relationship: A short-term prospective study. Behav Ther 2014;45:212–221. DOI: 10.1016/j.beth.2013.10.007 [DOI] [PubMed] [Google Scholar]
- [31].Sobrinho AT, Campos RC, Holden RR. Parental rejection, personality, and depression in the prediction of suicidality in a sample of nonclinical young adults. Psychoanal Psychol 2016;33:554–570. DOI: 10.1037/pap0000051 [DOI] [Google Scholar]
- [32].Batterham PJ, Spijker BAJ, Mackinnon AJ, et al. Consistency of trajectories of suicidal ideation and depression symptoms: Evidence from a randomized controlled trial. Depress Anxiety 2018;36:321–329. DOI: 10.1002/da.22863 [DOI] [PubMed] [Google Scholar]
- [33].Hirsch JK, Conner KR. Dispositional and explanatory style optimism as potential moderators of the relationship between hopelessness and suicidal ideation. Suicide Life-Threat 2006;36:661–669. DOI: 10.1521/suli.2006.36.6.661 [DOI] [PubMed] [Google Scholar]
- [34].Kelberer LJA, Kraines MA, Wells TT. Optimism, hope, and attention for emotional stimuli. Pers Individ Dif 2018;124:84–90. DOI: 10.1016/j.paid.2017.12.003 [DOI] [Google Scholar]
- [35].Mira A, Bretón-López J, Enrique Á, et al. Exploring the incorporation of a positive psychology component in a cognitive behavioral internet-based program for depressive symptoms. Results throughout the intervention process. Front Psychol 2018; 9: 2360. DOI: 10.3389/fpsyg.2018.02360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Celano CM, Gomez-Bernal F, Mastromauro CA, et al. A positive psychology intervention for patients with bipolar depression: a randomized pilot trial. J Ment Health 2020;29: 60–68. DOI: 10.1080/09638237.2018.1521942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Yu J, Putnick DL, Hendricks C, & Bornstein MH Long-term effects of adolescent self-competence and parenting for dispositional optimism and neuroticism. J Youth Adolesc 2019;48:1544–1554. DOI: 10.1007/s10964-018-0980-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Klonsky ED, Saffer BY, Bryan CJ. Ideation-to-action theories of suicide: a conceptual and empirical update. Curr Opin Psychol 2018;22:38–43. DOI: 10.1016/j.copsyc.2017.07.020 [DOI] [PubMed] [Google Scholar]
- [39].Rabon JK, Chang EC, & Hirsch JK (2019). Positive psychology and suicide prevention: An introduction and overview of the literature. In Hirsch JK, Change EC, & Rabon JK (Eds.), A positive psychological approach to suicide (pp. 1–15). Springer. [Google Scholar]
- [40].Zalsman et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry 2016;3:646–659. DOI: 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]


