Abstract
Background
Evolving medical technology, advancing biomedical and drug research, and changing laws and legislation impact patients’ healthcare options and influence healthcare practitioners’ (HCPs’) practices. Conscientious objection policy confusion and variability can arise as it may occasionally be unclear what underpins non-participation. Our objective was to identify, analyze, and synthesize the factors that influenced HCPs who did not participate in ethically complex, legally available healthcare.
Methods
We used Arksey and O’Malley’s framework while considering Levac et al.’s enhancements, and qualitatively synthesized the evidence. We searched Medline, CINAHL, JSTOR, EMBASE, PsychINFO, Sociological Abstracts, and ProQuest Dissertations and Theses Global from January 1, 1998, to January 15, 2020, and reviewed the references of the final articles. We included articles written in English that discussed the factors that influenced physicians and registered nurses (RNs) who did not participate in end-of-life (EOL), reproductive technology and health, genetic testing, and organ or tissue donation healthcare areas. Using Covidence, we conducted title and abstract screening, followed by full-text screening against our eligibility criteria. We extracted the article’s data into a spreadsheet, analyzed the articles, and completed a qualitative content analysis using NVivo12.
Results
We identified 10,664 articles through the search, and after the screening, 16 articles were included. The articles sampled RNs (n = 5) and physicians (n = 11) and encompassed qualitative (n = 7), quantitative (n = 7), and mixed (n = 2) methodologies. The care areas included reproductive technology and health (n = 11), EOL (n = 3), organ procurement (n = 1), and genetic testing (n = 1). One article included two care areas; EOL and reproductive health. The themed factors that influenced HCPs who did not participate in healthcare were: (1) HCPs’ characteristics, (2) personal beliefs, (3) professional ethos, 4) emotional labour considerations, and (5) system and clinical practice considerations.
Conclusion
The factors that influenced HCPs’ who did not participate in ethically complex, legally available care are diverse. There is a need to recognize conscientious objection to healthcare as a separate construct from non-participation in healthcare for reasons other than conscience. Understanding these separate constructs will support HCPs’ specific to the underlying factors influencing their practice participation.
Keywords: Conscientious objection, Medical ethics, Refusal to treat, Abstention, Care provision, Non-participation, Non-involvement
Background
Evolving medical technology, advancing biomedical and drug research, and changing laws and legislation impact patients’ healthcare options and influence healthcare practitioners’ (HCPs’) practices. In June 2016, Bill C-14 became law in Canada, which supported eligible patients’ right to access medical assistance in dying (MAID) [1]. This newly available end-of-life (EOL) healthcare option, cultivated interest at the convergence of HCPs’ care participation, conscientious objection, and patients’ access to care.
HCPs consider their care participation within the greater systems in which they practice. Healthcare delivery systems are regulated by federal and provincial law, influenced by local, regional, and national culture, and guided by employer policies. HCPs also practice within their professional codes of ethics and standards, and their individual moral values [2], and moral imperatives [3]. When navigating these considerations, some HCPs find their practices do not align with the care a patient requests and have a conscientious objection to care.
HCPs engage in conscientious objection (CO) when they decline to provide care because their participation is incompatible with their ethical, religious, or core moral beliefs [4]. Conscientious objection is a complex and sometimes polarizing topic of debate. Schuklenk (2015) noted that patients are “entitled” to receive care from HCPs because they became HCPs by voluntary choice [5]. Others contend that CO is unethical and constitutes an abandonment of professional obligation [6]. Weinstock (2014), however, posits that there are reasons to support a “limited right” CO in healthcare [7]. These reasons include that conscientious objection (1) provides HCPs the opportunity to reflect on their practice demands relative to their sense of self, (2) allows HCPs to deliberate complex moral issues and reflect on the laws, rules, and codes that regulate their practice, (3) accommodates the moral agency of HCPs with alternative views, and (4) fosters the examination of the underlying reasons for dissent [7]. Canadian HCPs’ professional codes of ethics address CO and non-abandonment of patients [8, 9]. However, a pan-Canadian review of CO policies noted “considerable potential for practitioner confusion exists based on the bewildering array of policies existing in many provinces and territories” and further noted significant variability in how to address conscience conflicts [10].
Conscientious objection policy confusion and variability can arise as it may occasionally be unclear what underpins non-participation. Dean [11] noted that HCPs’ non-participation may not always be precipitated by conscience, and Lachman [12] highlighted the need to distinguish conscience claims from non-participation influenced by cowardice, dislike, self-interest, discrimination, or prejudice. For instance, claims of conscience were noted in some care refusals that were based on HCPs' convenience, irrational fear, or reluctance to treat patients because of the patient’s unhealthy lifestyle choices [10]. Card [5] proposed that HCPs be required to declare their reasons for the objection. He explained this evaluation would assess the objection's reasonability and would ensure the non-participation (1) did not result in unreasonable harm to patients, (2) respected the power inequality between HCPs and patients, (3) was non-discriminatory, and (4) did not violate the duty of care. Shaw and Downie (2014) noted that confusion and variability surrounding CO could result in inconsistent patient care options and outcomes, increased healthcare costs, friction within the care team, and patient and provider uncertainty regarding care [10].
Our research project used a scoping review methodology. Scoping methodologies are useful for charting the relevant literature in an area of interest and exploring broad topics with multiple study designs [13]. Specifically, scoping reviews (1) examine the nature of the research activity in a given field, (2) determine the potential value of undertaking a full systematic review, (3) summarize and disseminate research findings, and (4) identify gaps in the existing research [13]. Using this methodology, we identified, analyzed, and synthesized the factors that influenced HCPs who do not participate in ethically complex, legally available care and further identified the research gaps to inform future areas of inquiry. The Arksey and O’Malley methodology framework [13], Levac et al.’s enhancements [14], and the PRISMA Scoping Review Checklist [15] were used to guide the research and its reporting. A protocol was published [16], and this paper reflects the final project.
This scoping review explored factors of conscience and non-conscience origins that influenced HCPs’ who do not participate in ethically complex, legally available healthcare. We considered ethically complex care as the care available in a morally pluralistic, evolving context with significant physical, mental, emotional, and social implications for patients, families, and healthcare providers. Specifically, our research question was, “What is known regarding the factors that influence physicians and registered nurses who do not participate in the ethically complex and legally available care areas of EOL (including assisted death), reproductive health and technology, genetic testing, and organ or tissue donation?” A team of five researchers conducted this project.
Methods
Identifying the relevant articles
The search protocol was developed by the team librarian and included MeSH, keywords, and synonyms (Appendix A). We chose these terms to capture the concepts broadly related to care non-participation. We accessed the Medline, CINAHL, JSTOR, EMBASE, PsychINFO, Sociological Abstracts, and ProQuest Dissertations and Theses Global databases and searched the period from January 1, 1998, to January 15, 2020. Our STARLITE [17] search strategy summary is in Table 1.
Table 1.
STARLITE [17] literature search strategy summary
| Sampling strategy | Comprehensive survey |
| Type of study | Any article that might contribute to answering the research question |
| Approaches | Electronic database searching and manually reviewing the reference lists of the articles that eventually met all inclusion/exclusion criteria |
| Range of Years | January 1, 1998, to January 15, 2020 |
| Limits | Excluded grey literature and non-English articles |
| Inclusion/exclusion criteria | Per Table 2: Eligibility criteria for article selection |
| Terms used | Appendix A for initial literature search protocol |
| Electronic Databases | Medline, CINAHL, JSTOR, PsycINFO, ProQuest Dissertations and Theses Global, EMBASE and Sociological Abstracts |
We completed a second search of the databases inclusive of non-English articles to thoroughly account for all articles relative to our project, which resulted in 1537 non-English articles. Given the abundance of identified articles, we did not search beyond our initial article inclusion date, and grey literature and non-English articles were excluded. We also reviewed their reference lists of the articles identified through the selection process to identify other potentially relevant articles.
Article selection
Seeking to balance reasonable project boundaries within an extensive array of ethically complex, legally available care areas, we used our clinical and research experience to outline the article selection criteria and specify the included care areas (Table 2). We used Covidence [18] to organize and facilitate the article selection process. First, two team members evaluated each article’s title and abstract against the eligibility criteria. After screening a minimum of 30 studies, we cross-checked the screening results to support reliability in our understanding and application of the criteria. When we were satisfied with our cross-checking, we continued screening the articles. Articles with conflicted screening results were identified in Covidence, and subsequently, two team members determined their inclusion or exclusion by consensus. We refined the eligibility criteria prior to the full text-screening to support the exposition of the research question. Two team members then assessed the articles’ full-text, and again, the conflicted articles were discussed by two team members to determine their inclusion or exclusion by consensus. Article quality was not assessed, which was consistent with a scoping review methodology [13].
Table 2.
Eligibility criteria for article selection
| Title and abstract eligibility criteria | |
| Inclusion | Exclusion |
| Physicians and/or RNs in the sample, AND | Non-English studies, OR |
| Must include reasons or factors that precipitate or influence individual non-participation in legally available care, AND | Studies that included other health professional groups, OR |
| Must be within one of these healthcare areas: end-of-life care, reproductive technology, and health, genetic testing, organ or tissue donation, OR | Studies included nursing or medical students |
| The article speaks to the physician or RN CO in one of the identified healthcare areas | |
| Additional full-text eligibility criteria | |
| Additional inclusion | Additional exclusion |
| Must be a research study (as opposed to a theoretical discussion of constructs), AND | Conference abstract, OR |
| Care must be legally available where the study was conducted | The findings had aggregate results that included students or individuals other than RNs or physicians in the sample, OR |
| The study included multiple jurisdictions, and the care is not legally available in all areas identified in the study, OR | |
| The care area was not identified | |
Charting the data
As this scoping review formed part of a doctoral dissertation, the first author, supported by the second and third authors, led the data extraction, collation, and analysis. We populated the article’s information (including year, authors’ names, country, and journal), the article’s design (including methodology, objectives, care area, sample profession, and size), and the article’s findings into our data extraction spreadsheet. This spreadsheet was shared with all the research team members for cross-checking. With the support of NVivo 12 [19], the first author qualitatively analyzed the articles through open-coding and content analysis. Subsequently, through a process of code combining and refining, we developed a codebook and conducted thematic analysis [20]. All the team members had the opportunity to discuss and refine the interim and final findings.
Patient and public participation
We did not involve patients or families in this research. However, as we are able, knowledge translation activities will occur to disseminate findings to knowledge users.
Results
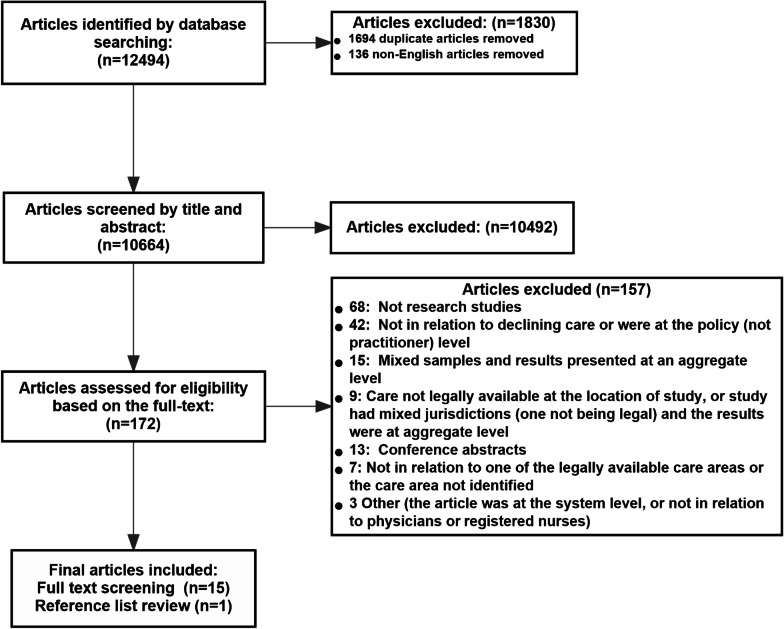
Include and excluded articles
Through our literature search strategy, we identified 12,494 articles. In Covidence, we removed the duplicate and non-English articles that were not excluded through the database searches. Consequently, we had 10,664 articles available for the title and abstract screening. One hundred and seventy-two (172) articles remained after we applied our initial eligibility criteria, and 15 articles remained after we conducted the full-text screening against our refined eligibility criteria. We located one additional article by reviewing the reference lists of the included articles (Fig. 1).
Fig. 1.
Study selection flow diagram
Analyzing the articles
The articles summary and contextual information are provided in Table 3 to frame our thematic findings. The included articles were published between 2000 and 2019, and eleven studies included physicians, and five included RNs. The articles originated in the United States (n = 8), Australia (n = 2), South Africa (n = 1), Brazil (n = 1), Norway (n = 1), Switzerland (n = 1), and Canada (n = 1). One article compared findings from the United States and the Netherlands. The articles comprised qualitative (n = 7), quantitative (n = 7), and mixed (n = 2) methodologies. The articles spanned multiple care areas and included reproductive health (n = 10), EOL care (including physician-assisted dying and medical assistance in dying) (n = 3), genetic testing (n = 1), and organ procurement (n = 1). One article included two care areas; EOL and reproductive health.
Table 3.
Summary of included studies
| First author | Year | Country | Methodology | Legally available care area | Profession | Sample size |
|---|---|---|---|---|---|---|
| Botes [29] | 2000 | South Africa | Qualitative | Reproductive health | RN | n = 1200 (open-ended questionnaire) and 22 focus groups |
| Bouthillier [34] | 2019 | Canada | Qualitative | Medical assistance in dying | Physician | n = 22 individual interviews |
| Clymin [32] | 2012 | Washington, USA | Mixed Methods (qualitative analysis of open text responses) | Physician-assisted dying | RN | n = 582 |
| Curlin [31] | 2008 | Illinois, USA | Qualitative | Reproductive health | Physician | n = 19 |
| Dawson [27] | 2017 | South Wales, Australia | Qualitative | Reproductive health | Physician | n = 28 and one focus group |
| Diniz [33] | 2014 | Brazil | Mixed Methods | Reproductive health | Physician | n = 1690 quantitative |
| n = 50 qualitative | ||||||
| Escher [36] | 2000 | Switzerland | Quantitative | Genetic testing | Physician | n = 259 (response rate of 64%) |
| Harris [23] | 2011 | USA | Quantitative | Reproductive health | Physician | n = 1154 (response rate of 66%) |
| Holt [22] | 2017 | USA | Quantitative | Reproductive health | Physician | n = 744 (response rate of 29%) |
| Marek [24] | 2004 | California, USA | Quantitative | Reproductive health | RN | n-75 (response rate of 49%) |
| Nordberg [21] | 2014 | Norway | Qualitative | Reproductive health | Physician | n = 7 individual interviews |
| Seelig [25] | 2006 | USA | Quantitative | Reproductive health | Physician | n = 419 (response rate 53%) |
| Smith [35] | 2017 | Australia | Qualitative | Organ procurement | RN | n = 35 individual interviews |
| Stevens [28] | 2017 | Massachusetts, USA | Quantitative | End-of-Life, Physician-assisted dying, reproductive health | RN | n-297 (response rate 42%) |
| Tilburt [30] | 2013 | USA | Quantitative | Reproductive healtha | Physician | n = 1032 (response rate 54%) |
| Willems [26] | 2000 | Oregon (USA) & Netherlands | Qualitative | End-of-Life, Physician-assisted dying, Euthanasia | Physician | n = 152 in Oregon |
| n = 67 in the Netherlands |
aStudy included two care areas: Reproductive health and Euthanasia. As euthanasia is not legal in all US jurisdictions, data used from the reproductive health findings only
Thematic findings
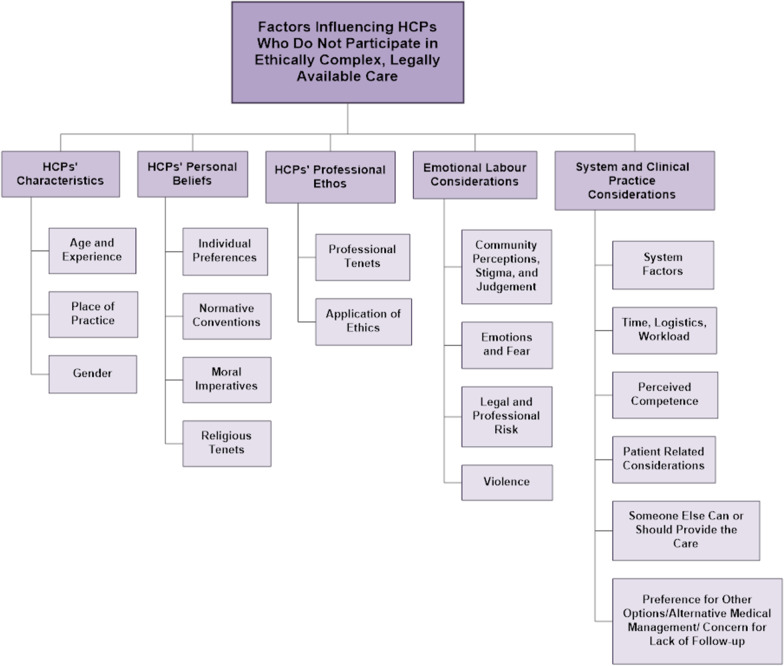
We categorized the factors that influence HCPs who do not participate in ethically complex, legally available care into five themes. These themes are (1) HCPs' characteristics, (2) HCPs' personal beliefs, (3) HCPs' professional ethos (4), emotional labour considerations, and (5) system and clinical practice considerations (insert Fig. 2). Table 4 outlines the content-coding matrix, including the themed factors, the content codes, and the articles where the content code was applied.
Fig. 2.
Thematic findings
Table 4.
Included study content coding and themes
| Themed factors | Content codes | The number of times the content code was applied | The article where the code was applied (by the first author) |
|---|---|---|---|
| HCPs’ characteristics | Age and experience | 4 | Harris, Holt, Marek, Nordberg |
| Gender | 3 | Willems, Holt, Harris | |
| Place of practice | 3 | Harris, Holt, Seelig | |
| HCPs’ personal beliefs | Individual preferences | 6 | Botes, Dawson, Stevens, Marek, Holt |
| Normative conventions | 3 | Botes, Tilburt, Curlin | |
| Moral imperatives and conviction | 8 | Bouthillier, Clymin, Dawson, Tilburt, Nordberg, Marek, Smith, Diniz | |
| Religious tenets | 13 | Botes, Bouthillier, Clymin, Diniz, Harris, Holt, Nordberg, Tilburt, Willems, Curlin, Stevens, Smith, Dawson | |
| HCPs’ professional ethos | Professional tenets | 3 | Botes, Bouthillier, Curlin |
| Application of ethics | 6 | Escher, Holt, Nordberg, Curlin, Smith, Marek | |
| Emotional labour considerations | Community perception, stigma, and judgement | 4 | Dawson, Smith, Bouthillier, Diniz |
| Emotions and fear | 3 | Bouthillier, Dawson, Clymin | |
| Legal and professional risk | 4 | Bouthillier, Clymin, Diniz, Willems | |
| Violence | 1 | Seelig | |
| System and clinical practice considerations | Perceived competence/lack of knowledge | 5 | Bouthillier, Clymin, Dawson, Holt, Smith |
| Time, workload and logistics | 3 | Bouthillier, Dawson, Smith | |
| Preference for other care options, concern for lack of available follow-up care, alternative medical management | 4 | Escher, Harris, Bouthillier, Clymin | |
| Someone else can or should provide the care | 6 | Seelig, Botes, Clymin, Dawson, Holt, Nordberg | |
| System factors | 4 | Clymin, Dawson, Holt, Smith | |
| Patient-related considerations | 6 | Diniz, Harris, Holt, Marek, Willems, Curlin |
HCPs’ characteristics
Age, years of experience, location of practice (including geographical region or clinical practice area), and gender were the identified characteristics of HCPs who do not participate in ethically complex, legally available care. One article highlighted that some HCPs developed opposition to care participation over time [21]. Conversely, other articles identified HCPs who had more experience [22], and HCPs who identified as “older” [23] were less likely to object to ethically complex, legally available care. Additionally, HCPs’ previous work experience specific to the care area influenced their care non-participation [24].
Non-participation in ethically complex, legally available care was more likely among HCPs who practiced in rural settings [23], and among HCPs who were located in the South or Midwest of the United States [22, 23]. Private practices (compared to hospital-based settings) [22, 25], and religiously affiliated practices (compared to non-religiously affiliated practices) [22] were associated with non-participation in ethically complex, legally available care, and non-participation was more likely among male HCPs [22, 23, 26].
HCPs’ personal beliefs
Personal beliefs influenced HCPs who did not participate in ethically complex, legally available care, and we coded these as individual preferences, normative conventions, moral imperatives or convictions, and religious tenets. HCPs' individual preferences were noted in the articles as “personal beliefs,” [27] “personal objections,” [22] “attitudes”, [24] “non-religious reasons”, [28] as care being an “unpleasant service”, [27] or as a “waste of taxpayers’ money”. [29] Normative conventions, or the socially and culturally shared notions about the way things are usually done [3], influenced HCPs’ non-participation in ethically complex, legally available care and were noted as HCPs’ consideration of rights and responsibilities [29], fairness [30], and if the request was counter to a “widely held societal norm” [31].
Non-participation was also influenced by a belief that the ethically complex, legally available care was fundamentally right or wrong [3], and we coded these as moral imperatives or convictions. Moral imperatives included “moral objections”, [27] “moral convictions”, [32] “moral duty”, [33] “moral beliefs”, [24, 34, 35] “sanctity”, [30] and that care refusal allowed HCPs “to be themselves” in care participation [21]. Lastly, some HCPs expressed care participation was counter to their religious tenets [21, 26–28, 30, 32–35], and identified that their participation would be “judged by God” [29] or would result in tensions between the HCPs’ beliefs and the patient’s care requests [31]. Specifically, HCPs who identified as Catholic, Protestant, Christian, Muslim, or who communicated the importance of religion were more likely to object to participation in ethically complex, legally available care [22, 23].
HCP’s professional ethos
Professional ethos influenced HCPs who do not participate in care. Some HCPs believed the care conflicted with the tenets of medicine [34] or the Hippocratic Oath [31]. Other HCPs noted the care misaligned with the promotion of health or the Nurses’ Pledge [29]. HCPs frequently noted that care participation was counter to their application of professional ethics [21, 22, 24, 31, 35, 36]. Specifically, this included beliefs that the care would “do more harm than good” [36], that the care would “harm the patient’s health” [22], and that HCPs had a “commitment to the patients medical good” [31].
Emotional labour considerations
Emotional labour, or the management of feelings [37], was considered by HCPs who do not participate in ethically complex, legally available care. Fear was documented as a primary emotional response in multiple articles [27, 32, 34]. Expressly HCPs: (1) feared the emotional aspects of care provision and its sequelae for the care provider [34]; (2) feared a potential backlash from others if they participated in care [27]; (3) feared patient death [34]; and/or (4) feared potential job loss [32]. Additionally, HCPs contemplated the risk of violence [25], the risk of medicolegal and/or professional repercussions [26, 32–34], and considered the stigma and judgment from their colleagues and the greater community [27, 33–35].
System and clinical practice considerations
System considerations influenced HCPs' non-participation in ethically complex, legally available care, including (1) “uncertainty about facility or professional policies” [32], (2) practices that “would not permit” the care option (i.e., employers believed the care to be outside the HCPs’ scope of practice) [27], (3) practices that restricted referrals [22], and (4) availability of alternative care providers [35]. Clinical practice considerations that influenced non-participation in ethically complex, legally available care included time, workload, and logistical concerns [27, 34, 35]. HCPs also considered their participation in care relative to their self-assessed competency and lack of knowledge [22, 27, 32, 34, 35], and considered whether another care provider could or should provide the care [21, 22, 25, 27, 29, 32]. This non-participation was explicitly noted in some articles as due to a lack of interest in the care area [25, 27], a lack of a desire to participate in care [29], or a belief that a specialist could provide better care [27]. Also influencing non-participation in ethically complex, legally available care was HCPs’ preference for other care options [32, 34], and their assessment that the precipitating condition could be managed in alternative ways [23]. Lastly, HCPs’ considered the circumstances that precipitated the patient’s care request [22–26, 33], and the availability of adequate care follow-up relative to their care participation [36].
Discussion
Main findings
While conscientious objection frequently dominates the discourse regarding HCPs’ non-participation in ethically complex, legally available care, the findings of this scoping review make clear that multiple factors beyond ethical, religious, or core moral beliefs [4] also influence HCPs’ non-participation. Non-participation in legally care available in a morally pluralistic, evolving care context that has significant physical, mental, emotional, and social implications was influenced by the emotional labour of care, the consideration of patient factors, HCPs' care preferences, practice logistics, and complexities, as well as the larger system within which HCPs work. Our findings align with a systematic review of nurses’ and midwives’ reasons for declining to participate in pregnancy termination [38], which identified moral, practical, religious, or legal reasons for objecting to care. Collectively, this highlights a need to distinguish between conscientious objection to care (when an HCP does not participate in care because doing so would be against “one or more of his deepest commitments” [39]) and non-participation in care due to reasons other than conscience (i.e., non-participation due to self-interest or professional integrity) [4]. This delineation is critical as the practice implications are different within each construct.
Non-participation in legally available care in a morally pluralistic, evolving care context with significant physical, mental, emotional and social implications that culminates in a conscientious objection is complicated. Existing codes of ethics frequently do not adequately capture the complex realities of practice, and the processes to disengage from care are ambiguous [40]. Nurses who had a conscientious objection reported feeling alone, uncertain, and stigmatized and that their objection felt futile due to a lack of meaningful professional support [41]. Thus, healthcare systems must mitigate the confusion and variability in conscientious objection policies [10] and address the disconnect between having a policy in situ, and the pragmatic, practical realities of enacting an objection [40]. The importance of this is paramount, considering the continuous advancements in healthcare and the resultant shifts in HCPs’ roles and responsibilities [42].
Non-participation in ethically complex, legally available care for reasons other than conscience requires authentic and continuous discussions among healthcare regulators, leadership, administrators, unit managers, and HCPs. These discussions will illuminate HCPs’ practice realities and support an enriched and nuanced understanding of the myriad of factors that are influencing non-participation. Self-assessed inadequate competence [22, 27, 32, 34, 35], time, workload and logistical concerns [27, 34, 35], uncertain policies [32], workplace practice limits [22, 27], and patient-related practice considerations [22–24, 26, 31, 33] all influenced HCPs’ non-participation in ethically complex, legally available care. Thus, policy clarification, removal of practice barriers and workplace practice limits, providing time and logistical support for care provision, and continuing education opportunities may positively support HCPs' participation. Additionally, professional regulators and associations must elucidate HCPs’ roles and obligations where duty, abandonment, and non-participation for reasons other conscience intersect. Elucidating these roles and responsibilities is crucial for all HCPs. However, this clarification is more acutely required for HCPs who practice in rural, remote, single-provider practices or in areas with limited referral options.
Strengths and limitations
The inclusion of two of the largest practicing groups of healthcare providers (physicians and RNs) and the inclusion of multiple care areas were project strengths. An additional strength was the inclusion of articles where the care was legally available, thus removing the hypothetical factors influencing potential non-participation in care. Eight countries were represented in the included articles, and it was not possible to account for the diversity and impact of culture. Additionally, there may be different non-participation factors in different care areas or among the professional groups that were excluded from the project. Inclusion of specific ethically complex, legally available care areas may have excluded other care areas where care non-participation occurs. Further, utilization of identified databases may result in the exclusion of articles indexed in other databases, and the use of English only articles could have resulted in the exclusion of relevant articles in other languages.
Areas of future research
With our article search and identification strategy, we discovered a significant body of literature (n = 10,664). However, when the results were limited to research articles of physicians and RNs within defined ethically complex, legally available care areas, the final number of articles markedly decreased. This suggests that although conscientious objection is frequently debated, explored, and deconstructed in the literature, there is significantly less research into the precipitating factors or underpinnings of HCPs’ care non-participation in ethically complex, legally available care. Equally important, as the discourse opens between conscientious objection and non-participation for reasons other than conscience, additional research into non-participation for reasons other than conscience is warranted. Of the included articles, the majority (14 out of 16) were concerning EOL and reproductive health (pregnancy termination and birth control) care areas. This suggests that research into the care areas of genetic testing, reproductive health and technology, and organ procurement may be underexplored. Lastly, future research could explore differences in the factors influencing HCP participation where care is legally available to those where it is illegal to distill the anticipated or hypothetical influencers of non-participation.
Conclusion
As healthcare evolves and patient care options change, a robust understanding of the factors that influence HCPs’ who do not participate in ethically complex, legally available care is imperative. This understanding of the factors will further delineate conscientious objection and non-participation for reasons other than conscience as separate constructs such that HCPs are supported in a manner that is specific to the underlying factor influencing their participation.
Acknowledgements
Not applicable.
Abbreviations
- HCPs
Healthcare practitioners
- RNs
Registered nurses
- EOL
End-of-LIFE
- MAID
Medical assistance in dying
- CO
Conscience objection
Authors' contributions
JB is the guarantor, and led the project. JB, DG, and LT participated in the refinement of the research question. MC developed and refined the search strategies, inclusion, and exclusion criteria in collaboration with JB and DG and LT. JB, DG, LT, and AH participated in the screening of articles. All authors participated in data analysis, and all authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations within three years of beginning the submitted work that could inappropriately influence, or be perceived to influence, their work.
Protocol
Brown, J., Goodridge, D., Thorpe, L., & Chipanshi, M. (2018). Factors contributing to practitioner choice when declining participation in legally available care: A scoping protocol. BMJ Open, 8(8), e023901. 10.1136/bmjopen-2018-023901.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Janine Brown, Email: janine.brown@uregina.ca.
Donna Goodridge, Email: donna.goodridge@usask.ca.
Lilian Thorpe, Email: lilian.thorpe@usask.ca.
Alexandra Hodson, Email: Alexandra.hodson@uregina.ca.
Mary Chipanshi, Email: Mary.chipanshi@uregina.ca.
References
- 1.Government of Canada. Statutes of Canada 2016: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying) [Internet]. Government of Canada; 2016 [cited 2017 Dec 29]. http://laws-lois.justice.gc.ca/eng/AnnualStatutes/2016_3/FullText.html
- 2.Kinnier R, Kernes J, Dautheribes T. A short list of universal moral values. Couns Values. 2000;45(1):4–16. doi: 10.1002/j.2161-007X.2000.tb00178.x. [DOI] [Google Scholar]
- 3.Skitka LJ. The psychology of moral conviction. Soc Pers Psychol Compass. 2010;4(4):267–281. doi: 10.1111/j.1751-9004.2010.00254.x. [DOI] [Google Scholar]
- 4.Wicclair MR. Conscientious objection in health care: an ethical analysis. Cambridge: Cambridge University Press; 2011. p. 252. [Google Scholar]
- 5.Card RF. Reasonability and conscientious objection in medicine: a reply to marsh and an elaboration of the reason-giving requirement: reasonability and conscientious objection in medicine. Bioethics. 2014;28(6):320–326. doi: 10.1111/bioe.12022. [DOI] [PubMed] [Google Scholar]
- 6.Fiala C, Gemzell Danielsson K, Heikinheimo O, Guðmundsson JA, Arthur J. Yes we can! Successful examples of disallowing “conscientious objection” in reproductive health care. Eur J Contracept Reprod Health Care Off J Eur Soc Contracept. 2016;21(3):201–206. doi: 10.3109/13625187.2016.1138458. [DOI] [PubMed] [Google Scholar]
- 7.Weinstock D. Conscientious refusal and health professionals: Does religion make a difference? Bioethics. 2014;28(1):8–15. doi: 10.1111/bioe.12059. [DOI] [PubMed] [Google Scholar]
- 8.Canadian Nurses Association . Code of ethics for registered nurses. Ottawa: Canadian Nurses Association; 2017. [Google Scholar]
- 9.Canadian Medical Association. CMA Code of Ethics and Professionalism [Internet]. 2018. https://policybase.cma.ca/documents/policypdf/PD19-03.pdf.
- 10.Shaw J, Downie J. Welcome to the wild, wild north: Conscientious objection policies governing Canada’s medical, nursing, pharmacy, and dental professions. Bioethics. 2014;28(1):33–46. doi: 10.1111/bioe.12057. [DOI] [PubMed] [Google Scholar]
- 11.Deans Z. Might a conscience clause be used for non-moral or prejudiced reasons? J Med Ethics. 2016;42(2):76–77. doi: 10.1136/medethics-2015-102798. [DOI] [PubMed] [Google Scholar]
- 12.Lachman V. Conscientious objection in nursing: definition and criteria for acceptance. MEDSURG Nurs. 2014;23(3):196–198. [PubMed] [Google Scholar]
- 13.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 14.Levac D, Colquhoun H, O’Brien KK. Scoping studies: Advancing the methodology. Implement Sci. 2010 doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 16.Brown J, Goodridge D, Thorpe L, Chipanshi M. Factors contributing to practitioner choice when declining involvement in legally available care: a scoping protocol. BMJ Open. 2018;8(8):e023901. doi: 10.1136/bmjopen-2018-023901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Booth A. “Brimful of STARLITE”: toward standards for reporting literature searches. J Med Libr Assoc. 2006;94(4):421e205–9e205. [PMC free article] [PubMed] [Google Scholar]
- 18.Covidence. Better systematic review management [Internet]. 2020 [cited 2020 Apr 16]. https://www.covidence.org/home.
- 19.QST International. NVivo, Software that supports qualitative and mixed methods research [Internet]. Available from: http://www.qsrinternational.com/nvivo/what-is-nvivo
- 20.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 21.Nordberg EMK, Skirbekk H, Magelssen M. Conscientious objection to referrals for abortion: pragmatic solution or threat to women’s rights? BMC Med Ethics. 2014 doi: 10.1186/1472-6939-15-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holt K, Janiak E, McCormick MC, Lieberman E, Dehlendorf C, Kajeepeta S, et al. Pregnancy options counseling and abortion referrals among US primary care physicians: results from a national survey. Fam Med. 2017;49(7):527–536. [PubMed] [Google Scholar]
- 23.Harris LH, Cooper A, Rasinski KA, Curlin FA, Lyerly AD. Obstetrician–gynecologistsʼ objections to and willingness to help patients obtain an abortion. Obstet Gynecol. 2011;118(4):905–12. doi: 10.1097/AOG.0b013e31822f12b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marek MJ. Nurses’ attitudes toward pregnancy termination in the labor and delivery setting. J Obstet Gynecol Neonatal Nurs. 2004;33(4):472–479. doi: 10.1177/0884217504266912. [DOI] [PubMed] [Google Scholar]
- 25.Seelig MD, Gelberg L, Tavrow P, Lee M, Rubenstein LV. Determinants of physician unwillingness to offer medical abortion using mifepristone. Womens Health Issues. 2006;16(1):14–21. doi: 10.1016/j.whi.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Willems DL, Daniels ER, van der Wal G, van der Maas PJ, Emanuel EJ. Attitudes and practices concerning the end of life: a comparison between physicians from the United States and from the Netherlands. Arch Intern Med. 2000;160(1):63–68. doi: 10.1001/archinte.160.1.63. [DOI] [PubMed] [Google Scholar]
- 27.Dawson AJ, Nicolls R, Bateson D, Doab A, Estoesta J, Brassil A, et al. Medical termination of pregnancy in general practice in Australia: a descriptive-interpretive qualitative study. Reprod Health. 2017;14(1):39. doi: 10.1186/s12978-017-0303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stevens L. Conscientious objection by Massachusetts Registered Nurses [Thesis]. [USA]: University of Massachusetts; 2018.
- 29.Botes A. Critical thinking by nurses on ethical issues like the termination of pregnancies. Curationis. 2000;23(3):26–31. doi: 10.4102/curationis.v23i3.686. [DOI] [PubMed] [Google Scholar]
- 30.Tilburt JC, James KM, Jenkins SM, Antiel RM, Curlin FA, Rasinski KA. “Righteous minds” in health care: measurement and explanatory value of social intuitionism in accounting for the moral judgments in a sample of U.S. physicians. PLoS ONE. 2013;8(9):e73379. doi: 10.1371/journal.pone.0073379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Curlin FA, Dinner SN, Lindau ST. Of more than one mind: obstetrician-gynecologists’ approaches to morally controversial decisions in sexual and reproductive healthcare. J Clin Ethics. 2008;19(1):11–21 . [PubMed] [Google Scholar]
- 32.Clymin J, Jacobson D, Jablonski A, Feldt KS. Washington State Death With Dignity Act: a survey of nurses’ knowledge and implications for practice part 2. J Hosp Palliat Nurs. 2012;14(2):141–148. doi: 10.1097/NJH.0b013e31823cc77a. [DOI] [Google Scholar]
- 33.Diniz D, Madeiro A, Rosas C. Conscientious objection, barriers, and abortion in the case of rape: a study among physicians in Brazil. Reprod Health Matters. 2014;22(43):141–148. doi: 10.1016/S0968-8080(14)43754-6. [DOI] [PubMed] [Google Scholar]
- 34.Bouthillier M-E, Opatrny L. A qualitative study of physicians’ conscientious objections to medical aid in dying. Palliat Med. 2019;33(9):1212–1220. doi: 10.1177/0269216319861921. [DOI] [PubMed] [Google Scholar]
- 35.Smith Z. Duty and dilemma: Perioperative nurses hiding an objection to participate in organ procurement surgery. Nurs Inq. 2017;24(3):66. doi: 10.1111/nin.12173. [DOI] [PubMed] [Google Scholar]
- 36.Escher M, Sappino AP. Primary care physicians’ knowledge and attitudes towards genetic testing for breast-ovarian cancer predisposition. Ann Oncol Off J Eur Soc Med Oncol. 2000;11(9):1131–1135. doi: 10.1023/A:1008319114278. [DOI] [PubMed] [Google Scholar]
- 37.Grandey AA. Emotional regulation in the workplace: a new way to conceptualize emotional labor. J Occup Health Psychol. 2000;5(1):95–110. doi: 10.1037/1076-8998.5.1.95. [DOI] [PubMed] [Google Scholar]
- 38.Fleming V, Frith L, Luyben A, Ramsayer B. Conscientious objection to participation in abortion by midwives and nurses: a systematic review of reasons. BMC Med Ethics. 2018;19(1):66. doi: 10.1186/s12910-018-0268-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kassner J, Lefkowitz D. Conscientious Objection. In: Chadwick RF, Callahan D, Singer P, editors. Encyclopedia of applied ethics. 2. ed. Amsterdam: Elsevier [u.a.]; 2012. p. 594–601.
- 40.Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood KW. Conscience, conscientious objection, and nursing: a concept analysis. Nurs Ethics. 2019;26(1):37–49. doi: 10.1177/0969733017700236. [DOI] [PubMed] [Google Scholar]
- 41.Lamb C, Babenko-Mould Y, Evans M, Wong CA, Kirkwood KW. Conscientious objection and nurses: results of an interpretive phenomenological study. Nurs Ethics. 2019;26(5):1337–1349. doi: 10.1177/0969733018763996. [DOI] [PubMed] [Google Scholar]
- 42.Ford N, Fraser K, Marck P. Conscientious objection: A call to nursing leadership. Nurs Leadersh. 2010;23(3):46–55. doi: 10.12927/cjnl.2010.21941. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.