Abstract
The coronavirus disease 2019 (COVID-19) pandemic has been associated with a declining volume of patients seen in the emergency department. Despite the need for seeking urgent care for conditions such as myocardial infarction, many people may not seek treatment. This study seeks to measure associations between the COVID-19 pandemic and location of death among individuals who died from ischemic heart disease (IHD). Data obtained from death certificates from the Arkansas Department of Health was used to conduct a difference-in-difference analysis to assess whether decedents of IHD were more likely to die at home during the pandemic (March 2020 through September 2020). The analysis compared location of death for decedents of IHD pre and during the pandemic to location of death for decedents from non-natural causes. Before the pandemic, 50.0% of decedents of IHD died at home compared to 57.9% dying at home during (through September 2020) the pandemic study period (p < .001). There was no difference in the proportion of decedents who died at home from non-natural causes before and during the pandemic study period (55.8% vs. 53.5%; p = .21). After controlling for confounders, there was a 48% increase in the odds of dying at home from IHD during the pandemic study period (p < .001) relative to the change in dying at home due to non-natural causes. During the study period, there was an increase in the proportion of decedents who died at home due to IHD. Despite the ongoing pandemic, practitioners should emphasize the need to seek urgent care during an emergency.
Keywords: COVID-19, Ischemic heart disease, Mortality
1. Introduction
By late-September 2021, more than 4.7 million people worldwide have died due to complications from the SARS-CoV-2 virus (“COVID-19”) (Dong et al., 2020). It has been well documented that the pandemic has had widespread effects on physical health as well as mental health and wellbeing (Carfì et al., 2020; Krendl and Perry, 2020; Salari et al., 2020; Struyf et al., 2020; Zacher and Rudolph, 2020). The pandemic has also been associated with changes in care-seeking behavior leading to reductions in preventative healthcare utilization, such as annual wellness visits and pediatric vaccinations, as well as declines in the use of hospital facilities for elective procedures (Chudasama et al., 2020; Santoli et al., 2020). These changes have been attributed to several factors including fear of contracting the virus and shelter-in-place orders (Czeisler et al., 2020). Changes in care-seeking behavior can have subsequent adverse effects in the future, such as late-stage cancer diagnosis or increased spread of vaccine-preventable diseases among unvaccinated children. Few studies have evaluated the consequences of behavioral changes due to the pandemic.
Previous evaluations have found large declines in emergency department use and inpatient admissions for acute conditions, such as myocardial infarction during the COVID-19 pandemic (Braiteh et al., 2020; Butt et al., 2020; Jeffery et al., 2020; Mantica et al., 2020). The consequence of such a change in care-seeking behavior may be an increased likelihood of death from AMI or at a minimum, an increased risk of out-of-hospital death (Lai et al., 2020; Sun et al., 2021; Wadhera et al., 2021). Acute diagnoses such as myocardial infarction and subsequent ST-elevation myocardial infarction (STEMI) require immediate medical attention and delays in seeking care may worsen outcomes. Previous studies have indicated that delaying treatment from symptom onset can significantly impact mortality (De Luca et al., 2003; Song et al., 2016). Therefore, the reluctance to seek care for these conditions due to the ongoing pandemic may impact where people die. Thus, the goal of this study is to estimate the association between the pandemic and location of death for decedents of ischemic heart disease under the hypothesis that the pandemic changed care-seeking behavior leading to an increased probability of out-of-hospital death. Using death certificate data from the state of Arkansas, we compared the proportion of deaths occurring at home among individuals who died from ischemic heart disease before and during the pandemic, relative to deaths at home among those who died from non-natural causes such as suicides, unintentional injuries, and other causes likely that are unrelated to care-seeking behavior.
2. Methods
2.1. Data source
This study used death certificates from the Arkansas Vital Statistics Database (AVSD) for all deaths that were recorded during the months of March through September for the years of 2016 through 2020, meaning each year would have seven months of data. Data from the months of January and February were excluded, as Arkansas had its first positive COVID-19 case on March 11, 2020. Data through September is the most recent data available given the time needed to process death certificate data. The AVSD collects all vital events occurring in the state of Arkansas, including deaths, and data are housed at the Arkansas Department of Health. The data used in this study was a de-identified decedent-level dataset containing demographics, primary cause of death, month of death, and location where the decedent was pronounced dead (i.e., at home, at the hospital, etc.).
2.2. Study population
The study population included deaths in Arkansas that were either from ischemic heart disease or a non-natural cause of death (Table 1 ). The certifier (e.g. medical examiner, coroner, attending physician) for the decedent adjudicates the cause of death. The International Classification of Diseases, 10th Revision, (ICD-10) codes obtained from the primary cause of death field on the death certificates were used to classify the cause of death. Ischemic heart disease-related deaths, which included acute myocardial infarction and ST-elevation myocardial infarction (STEMI), (ICD-10: I20-I25) were compared to non-natural causes of death (i.e., unintentional injuries, suicides, and homicides) (ICD - ICD-10 - International Classification of Diseases, Tenth Revision, 2020). Non-natural deaths were selected as a comparison group for the difference-in-difference (DID) analysis because the COVID-19 pandemic should have minimal impact on care-seeking behavior for these conditions resulting in no change for the locations of death. Non-natural causes of death were aggregated into one category to improve the stability of estimates associated with the relatively low numbers during the study period.
Table 1.
ICD-10 codes for ischemic heart disease and non-natural deaths.
| Cause of death | ICD-10 code |
|---|---|
| Ischemic heart disease | I20-I25 |
| Non-natural death | |
| Unintentional | V01-X59, Y85-Y86 |
| Homicide | X85-Y09, Y87.1, U01-U02 |
| Suicide | X60-X84, Y87.0, U03 |
Decedents who died in nursing homes or in hospice were excluded from the study. Additionally, decedents who died in January or February were excluded from the study because COVID-19 was not yet declared a global pandemic, and Arkansas did not have its first case until March 2020 (Timeline of WHO's response to COVID-19, 2020). To improve the comparison of the pre-pandemic time period to the pandemic time period, deaths occurring during the months of March through September were included for all study years.
2.3. Dependent variable
The primary outcome of interest was whether the decedent died at home and was measured using a dichotomous variable to indicate whether the decedent died at home or at a hospital (i.e., emergency department, inpatient, or dead on arrival to the hospital). The location of death was abstracted from the death certificate, which was completed by a medical certifier. Dead on arrival was included in the hospital category because this represented a death in which the decedent sought treatment (or a bystander sought treatment for the decedent) at a hospital facility prior to the decedent being pronounced dead.
2.4. Independent variable
The primary independent variable for this study was a dichotomous indicator of whether the death occurred prior to the time period when COVID-19 was declared a pandemic or whether it was after the pandemic was declared. The World Health Organization proclaimed COVID-19 as a global pandemic on March 11, 2020 (Timeline of WHO's response to COVID-19, 2020). Therefore, deaths occurring from March through September of 2020 are categorized as the pandemic period. The second independent variable is whether the death was an ischemic heart disease-related death or a death from non-natural causes.
2.5. Analysis
Descriptive statistics were assessed using chi-square tests for categorical variables and t-tests or Wilcoxon signed-rank test for continuous variables. To improve identification of treatment effects, the study used a DID analysis to estimate the association of the COVID-19 pandemic with dying at home among individuals who died from ischemic heart diseases compared to those who died from non-natural causes of death. A DID analysis is a quasi-experimental method that uses a control group (i.e., location of deaths for non-natural conditions) to serve as a counterfactual for what would have been expected to occur without a given treatment (i.e., the pandemic) (Wing et al., 2018). A primary assumption of the DID approach is that trends in outcomes (i.e., deaths at home) remained similar in the treatment (ischemic heart disease) and control (non-natural deaths) groups in the time period prior to the intervention (COVID pandemic). The primary coefficient of interest in the DID model was the interaction between ischemic heart disease and the pandemic study period. The parallel trends assumption was tested using a linear yearly time trend in the pre-pandemic time period, from 2016 through 2019. The DID analysis used multivariable logistic regression to estimate outcomes controlling for age (as categories), gender, race, and Hispanic ethnicity.
Statistical significance was assumed at less than 0.05. Data analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). The Institutional Review Board of the primary author's institution designated this study as non-human subjects research.
3. Results
A total of 15,231 deaths were included in the analysis, including 10,867 individuals who died from ischemic heart disease and 4364 individuals who died from non-natural causes. Table 2 provides demographic characteristics for decedents who died from heart disease in the pre-pandemic period (N = 8606) and after the pandemic was declared (N = 2261). There were no differences in age, gender, race, or Hispanic ethnicity for persons who died from heart disease before and after the pandemic was declared.
Table 2.
Decedent demographics from heart disease (N = 10,867).
| Variable | Pre-pandemic period, 2016–2019 |
During pandemic period, 2020 |
p-Value |
|---|---|---|---|
| (N = 8606) | (N = 2261) | ||
| Age in years, mean (std. dev.) | 71.4 (13.6) | 71.3 (14.0) | 0.79 |
| Age categories, N (%) | |||
| 0–34 years | 41 (0.5%) | 16 (0.7%) | 0.18 |
| 35–64 years | 2605 (30.3%) | 713 (31.6%) | 0.24 |
| 65+ years | 5959 (69.3%) | 1531 (67.7%) | 0.17 |
| Missing | 1 (0.01%) | 1 (0.04%) | – |
| Gender, N (%) | |||
| Male | 5303 (61.6%) | 1404 (62.1%) | 0.68 |
| Female | 3303 (38.4%) | 857 (37.9%) | |
| Race, N (%) | |||
| White | 7292 (84.7%) | 1896 (83.9%) | 0.31 |
| Black | 1153 (13.4%) | 325 (14.4%) | 0.23 |
| Other race | 156 (1.8%) | 39 (1.7%) | 0.78 |
| Missing | 5 (0.1%) | 1 (0.0%) | – |
| Ethnicity, N (%) | |||
| Hispanic | 96 (1.1%) | 29 (1.3%) | 0.50 |
| Location of death, N (%) | |||
| Home | 4306 (50.0%) | 1310 (57.9%) | <0.001 |
| Hospital | 4300 (50.0%) | 951 (42.1%) |
Table 3 provides demographic characteristics for decedents who died from non-natural causes in the pre-pandemic period (N = 3437) and the pandemic study period (N = 927). There was a greater proportion of decedents who were ≥ 65 years during the pandemic study period compared to the pre-pandemic period (23.7% vs. 28.1%; p = .007). There also were differences in race and ethnicity with a greater proportion of Black and Hispanic individuals dying from non-natural causes during the pandemic study period compared to the time period before the pandemic. Significant differences were noted in the intent of those who died from non-natural causes with a greater proportion of homicides (10.4% vs. 12.8%; p = .03) and a smaller proportion of suicides during the pandemic study period (31.9% vs. 27.8%; p = .02). However, there were no significant differences observed when examining the location of death for homicides, suicides, and unintentional intent; collectively or independently.
Table 3.
Decedent demographics from homicide, suicide, and unintentional deaths (n = 4364).
| Variable | Pre-pandemic period, 2016–2019 |
During pandemic period, 2020 |
p-Value |
|---|---|---|---|
| (N = 3437) | (N = 927) | ||
| Age in years, mean (std. dev.) | 48.4 (21.6) | 50.0 (21.9) | 0.05 |
| Age categories, N (%) | |||
| 0–34 years | 975 (28.4%) | 248 (26.8%) | 0.34 |
| 35–64 years | 1646 (47.9%) | 418 (45.1%) | 0.14 |
| 65+ years | 816 (23.7%) | 260 (28.1%) | 0.007 |
| Missing | 0 (0.0%) | 1 (0.1%) | – |
| Gender | |||
| Male | 2363 (68.8%) | 648 (69.9%) | 0.50 |
| Female | 1074 (31.3%) | 279 (30.1%) | |
| Race, N (%) | |||
| White | 2878 (83.9%) | 747 (80.6%) | 0.02 |
| Black | 451 (13.1%) | 149 (16.1%) | 0.02 |
| Other race | 101 (2.9%) | 31 (3.3%) | 0.53 |
| Missing | 7 (0.2%) | 0 (0.0%) | – |
| Ethnicity | |||
| Hispanic | 83 (2.4%) | 36 (3.9%) | 0.02 |
| Intent | |||
| Homicide | 356 (10.4%) | 119 (12.8%) | 0.03 |
| Death at home | 182 (51.1%) | 68 (57.1%) | 0.25 |
| Suicide | 1097 (31.9%) | 258 (27.8%) | 0.02 |
| Death at home | 918 (83.7%) | 212 (82.2%) | 0.56 |
| Unintentional | 1984 (57.7%) | 550 (59.3%) | 0.38 |
| Death at home | 819 (41.3%) | 216 (39.3%) | 0.40 |
| Location of death | |||
| Home | 1919 (55.8%) | 496 (53.5%) | 0.21 |
| Hospital | 1518 (44.2%) | 431 (46.5%) |
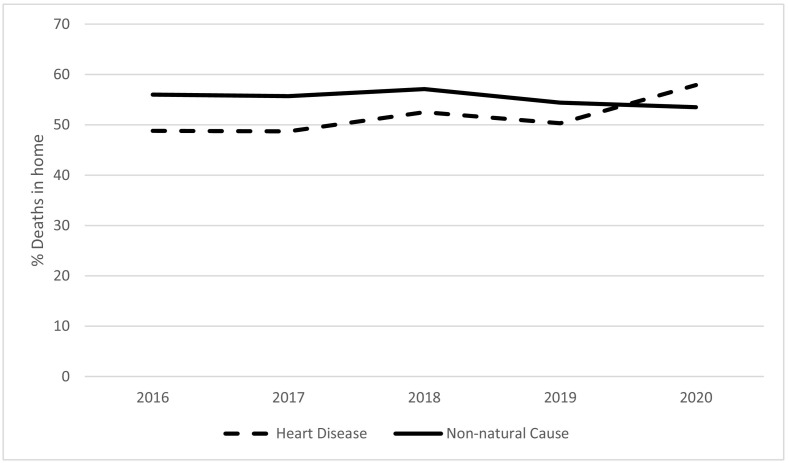
As seen in Fig. 1 , deaths due to ischemic heart disease and non-natural causes had similar trends prior to the pandemic (2016–2019), but the rate of deaths at home increased for heart disease only in 2020. In the time period before the pandemic, 50.0% of decedents from heart disease died at home compared to 57.9% dying at home during the pandemic study period (p < .001). No differences were observed in the decedents who died at home from non-natural causes as 55.8% did so before the pandemic compared to 53.5% during the pandemic study period (p = .21).
Fig. 1.
Proportion of deaths that occur in the home, 2016–2020.
The test for parallel trends during the pre-pandemic period was not significant (p = .46), suggesting similar trends among ischemic heart disease and non-natural causes of death in the pre-pandemic time period, an important assumption of DID analysis. Adjusted estimates using non-natural causes of death as the control group in the DID analysis presented in Table 4 indicate a 48% increase in the odds of dying at home from heart disease during the pandemic (p < .001).
Table 4.
Adjusted difference-in-difference logistic regression assessing the association of the COVID-19 pandemic and ischemic heart disease death on the odds of dying at home.
| Variable | Adjusted OR (95% CI) | p-Value |
|---|---|---|
| Age | ||
| 0–34 years (ref = 35–64 years) | 0.63 (0.55, 0.72) | <0.001 |
| 65+ years (ref = 35–64 years) | 0.72 (0.67, 0.77) | <0.001 |
| Male (ref = female) | 0.98 (0.92, 1.05) | 0.58 |
| Race | ||
| Black (ref = white) | 0.75 (0.69, 0.83) | <0.001 |
| Other race (ref = white) | 0.91 (0.71, 1.18) | 0.48 |
| Hispanic (ref = non-Hispanic) | 0.72 (0.54, 0.97) | 0.03 |
| COVID (ref = before COVID) | 0.93 (0.80, 1.08) | 0.34 |
| Ischemic heart disease (ref = non-natural deathsa) | 0.80 (0.73, 0.88) | <0.001 |
| Difference-in-difference interactionb | 1.48 (1.24, 1.76) | <0.001 |
Non-natural causes of death included deaths due to unintentional injuries, suicides, and homicides.
Interaction term (deaths from ischemic heart disease ∗ during pandemic period).
4. Discussion
Patients experiencing the signs and symptoms of heart disease, particularly a myocardial infarction must seek medical attention as soon as possible (De Luca et al., 2004). Administering life-saving therapies within the first hour of symptom onset is associated with a significant reduction in mortality (Boersma et al., 1996; Terkelsen et al., 2010). Generally, these therapies are administered in the emergency department. However due to the COVID-19 pandemic, many people may have been reluctant to seek treatment in the emergency department due to fear of contracting the disease (Barten et al., 2020; Mantica et al., 2020; Rosenbaum, 2020). There have been recent studies that brought attention to the decreased volume of patients presenting to the emergency department during the beginning of the pandemic (Barten et al., 2020; Garrafa et al., 2020; Jeffery et al., 2020; Mantica et al., 2020; Westgard et al., 2020). A review of patient volume for 24 emergency departments across the United States (US) found decreases that ranged between 41.5% to 63.5% (Jeffery et al., 2020). A study conducted in Italy highlighted the impact of “fear week,” a time period where lockdowns were implemented and daily press briefings regarding the pandemic were held (Garrafa et al., 2020). Garrafa et al., found that “fear week” was associated with a 31.8% decrease in emergency department visits for a large teaching hospital in Italy (Garrafa et al., 2020). Despite the decreases seen in emergency department visits during the pandemic, there is little evidence to suggest that the need for emergent care has decreased. In fact, Ciofani et al., found spikes in internet search volume related to chest pain during the pandemic (Ciofani et al., 2021). The consequences of such changes in care-seeking behavior may be widespread.
Non-natural deaths were selected as a comparison group for two reasons. First, while it has been documented that overall emergency department visits have decreased, trauma-related visits for severe injury were less impacted (Riuttanen et al., 2021). Additionally, a study examining the trend of trauma emergency department visits before and during the pandemic found that patients who were treated during the pandemic had higher injury severity scores when compared to patients treated prior to the pandemic (Ghafil et al., 2021). These studies indicate that despite the ongoing pandemic, people are still seeking treatment in the emergency department for severe injuries suggesting location of death for non-natural causes is a suitable control group to compare against location of death for IHD. It is possible that deaths from suicide or other non-natural causes could increase due to the pandemic, yet there would also be no change in the location of death from non-natural causes.
This study used death certificate data to assess whether there was a change in the location of death during the COVID-19 pandemic study period among individuals who died from ischemic heart disease relative to individuals who died from non-natural causes of death. The study findings indicate a drop in in-hospital deaths, with a 7.9 percentage point increase in deaths at home during the COVID-19 pandemic study period for decedents with ischemic heart disease. There was no significant difference in the percentage of patients who died from non-natural causes of death at home. The findings are consistent with a change in care-seeking behavior for ischemic heart disease, especially a reduction in care-seeking behavior at emergency departments.
The study findings are consistent with a change in patient care-seeking behaviors for IHD during the pandemic relative to what was observed in previous years. Policy considerations should include funding and resources for ensuring proper treatment protocols during public health emergencies to mitigate excess mortality. These resources may include the expansion of telehealth services and mobile health clinics to ensure proper care is sought and received. A prior analysis of excess mortality during the first two months of the pandemic found a 35% increase in deaths not attributed to COVID-19 (Woolf et al., 2020). The largest increases in excess mortality were attributed to heart disease (Woolf et al., 2020). Taken together with the current study findings, it is plausible that the increase in deaths due to heart disease may be related to changes in care-seeking behavior at emergency departments that led to the large increase in heart-related deaths at home.
This study used statewide data collected from death certificates to assess the impact of the COVID-19 pandemic for decedents from heart disease and the association of dying at home. Given that many heart-related deaths may be prevented with timely acute care, our study highlights the multifaceted impact of the COVID-19 pandemic on population health (Boersma et al., 1996; Lai et al., 2020; Sun et al., 2021). While COVID-19 has been directly associated with 4.7 M deaths worldwide and more than 690,000 deaths in the US alone, it is critical to understand the indirect impacts of COVID-19 (Dong et al., 2020). For example, the pandemic has been indirectly associated with large increases in poverty, insurance loss, and housing instability (Berkowitz and Basu, 2020; Han et al., 2020; Parolin et al., 2020). It has additionally been associated indirectly with adverse health outcomes, such as increased mental health disease (Salari et al., 2020). Our study adds to this literature by identifying the indirect contribution of COVID-19 to deaths due to ischemic heart disease.
There are several potential limitations of our study. First, the data come from vital statistics provisional death certificate data. While these data are used for multiple reporting and public health activities, including those by the National Center for Health Statistics, it is possible that some data records may be later adjusted. Additionally, these data lack several variables that could have been useful in this study, such as insurance status, being in the presence of someone during symptom onset, and marital status, which have been identified to impact the propensity to seek treatment (Goff et al., 1999). A final limitation is the lack of state-specific emergency department census data. These data would allow the researchers to examine the impact of the surges in COVID-19 cases, implementation of mask mandates, vaccination status, and other factors on the emergency department census within the state. Such data will not be available for research purposes for at least two years. Future studies should examine the impact of these factors on care-seeking behaviors during the pandemic.
5. Conclusion
While the U.S. and other parts of the world continue to address the COVID-19 pandemic, it is important that practitioners emphasize the need to seek medical care during an emergency. Although we are currently unable to evaluate the long-term impacts of missed preventative care and screening, our study provides a clear indication that the pandemic was associated with negative consequences for people with ischemic heart disease likely resulting from changes in care-seeking behavior. The findings are consistent with the well-documented finding that fewer patients sought urgent care in the emergency department during the COVID-19 pandemic. Continued efforts should be aimed at helping patients identify what signs and symptoms indicate the urgent need for medical help and stressing the importance of seeking that care immediately.
Author statement
-
•
Austin Porter contributed to the literature search, study design, data analyses, data interpretation, writing, and critical revision.
-
•
Clare Brown contributed to the literature search, study design, writing, data interpretation, and critical revision.
-
•
J. Mick Tilford contributed to the study design, data interpretation, and critical revision.
-
•
Michael Cima contributed to the writing and critical revision.
-
•
Namvar Zohoori contributed to the data interpretation and critical revision.
-
•
Donald McCormick contributed to the data interpretation and critical revision.
-
•
Michael P. Wilson contributed to the literature search, data interpretation, and critical revision.
-
•
Benjamin Amick contributed to the study design, data interpretation, and critical revision.
-
•
José Romero contributed to the study design, data interpretation, and critical revision.
The above-mentioned authors do not report any conflicts of interest.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors gratefully acknowledge the UAMS Clinician Scientist program, which generously supported Dr. Wilson's time during a portion of this work.
The views expressed in this article are solely those of the authors and do not necessarily represent the official views of the Arkansas Department of Health.
References
- Barten D.G., Latten G.H.P., van Osch F.H.M. Reduced emergency department utilization during the early phase of the COVID-19 pandemic: viral fear or lockdown effect? Disaster Med. Public Health Prep. 2020:1–4. doi: 10.1017/dmp.2020.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz S.A., Basu S. Unemployment insurance, health-related social needs, health care access, and mental health during the COVID-19 pandemic. JAMA Intern. Med. 2020 doi: 10.1001/jamainternmed.2020.7048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boersma E., Maas A.C., Deckers J.W., Simoons M.L. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet Lond. Engl. 1996;348:771–775. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- Braiteh N., Rehman W.U., Alom M., Skovira V., Breiteh N., Rehman I., Yarkoni A., Kahsou H., Rehman A. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am. Heart J. 2020;226:147–151. doi: 10.1016/j.ahj.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butt A.A., Azad A.M., Kartha A.B., Masoodi N.A., Bertollini R., Abou-Samra A.-B. Volume and acuity of emergency department visits prior to and after COVID-19. J. Emerg. Med. 2020;59:730–734. doi: 10.1016/j.jemermed.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carfì A., Bernabei R., Landi F., Gemelli Against COVID-19 Post-Acute Care Study Group Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chudasama Y.V., Gillies C.L., Zaccardi F., Coles B., Davies M.J., Seidu S., Khunti K. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabet. Metab. Syndr. 2020;14:965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciofani J.L., Han D., Allahwala U.K., Asrress K.N., Bhindi R. Internet search volume for chest pain during the COVID-19 pandemic. Am. Heart J. 2021;231:157–159. doi: 10.1016/j.ahj.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Marynak K., Clarke K.E.N., Salah Z., Shakya I., Thierry J.M., Ali N., McMillan H., Wiley J.F., Weaver M.D., Czeisler C.A., Rajaratnam S.M.W., Howard M.E. Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. Morb. Mortal. Wkly. Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Luca G., Suryapranata H., Zijlstra F., van't Hof A.W.J., Hoorntje J.C.A., Gosselink A.T.M., Dambrink J.H., de Boer M.J., ZWOLLE Myocardial Infarction Study Group Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J. Am. Coll. Cardiol. 2003;42:991–997. doi: 10.1016/s0735-1097(03)00919-7. [DOI] [PubMed] [Google Scholar]
- De Luca G., Suryapranata H., Ottervanger J.P., Antman E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrafa E., Levaggi R., Miniaci R., Paolillo C. When fear backfires: emergency department accesses during the Covid-19 pandemic. Health Policy Amst. Neth. 2020 doi: 10.1016/j.healthpol.2020.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghafil C., Matsushima K., Ding L., Henry R., Inaba K. Trends in trauma admissions during the COVID-19 pandemic in Los Angeles County, California. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff D.C., Feldman H.A., McGovern P.G., Goldberg R.J., Simons-Morton D.G., Cornell C.E., Osganian S.K., Cooper L.S., Hedges J.R. Prehospital delay in patients hospitalized with heart attack symptoms in the United States: the REACT trial. Rapid early action for coronary treatment (REACT) study group. Am. Heart J. 1999;138:1046–1057. doi: 10.1016/s0002-8703(99)70069-4. [DOI] [PubMed] [Google Scholar]
- Han J., Meyer B.D., Sullivan J.X. National Bureau of Economic Research; 2020. Income and Poverty in the COVID-19 Pandemic (No. w27729) [DOI] [Google Scholar]
- ICD - ICD-10 - International Classification of Diseases, Tenth Revision [WWW Document] 2020. https://www.cdc.gov/nchs/icd/icd10.htm URL. (accessed 11.15.20)
- Jeffery M.M., D’Onofrio G., Paek H., Platts-Mills T.F., Soares W.E., Hoppe J.A., Genes N., Nath B., Melnick E.R. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern. Med. 2020;180:1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krendl A.C., Perry B.L. The impact of sheltering-in-place during the COVID-19 pandemic on older adults’ social and mental well-being. J. Gerontol. B. Psychol. Sci. Soc. Sci. 2020 doi: 10.1093/geronb/gbaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai P.H., Lancet E.A., Weiden M.D., Webber M.P., Zeig-Owens R., Hall C.B., Prezant D.J. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantica G., Riccardi N., Terrone C., Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health. 2020;183:40–41. doi: 10.1016/j.puhe.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parolin Z., Curran M., Matsudaira J., Waldfogel J., Wimer C. Cent. Poverty Soc. Policy Columbia Univ.; 2020. Monthly Poverty Rates in the United States During the COVID-19 Pandemic; p. 24. [Google Scholar]
- Riuttanen A., Ponkilainen V., Kuitunen I., Reito A., Sirola J., Mattila V.M. Severely injured patients do not disappear in a pandemic: incidence and characteristics of severe injuries during COVID-19 lockdown in Finland. Acta Orthop. 2021;92:249–253. doi: 10.1080/17453674.2021.1881241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum L. The untold toll — the pandemic’s effects on patients without Covid-19. N. Engl. J. Med. 2020;382:2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor Shna, Mohammadi M., Rasoulpoor Shabnam, Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoli J.M., Lindley M.C., DeSilva M.B., Kharbanda E.O., Daley M.F., Galloway L., Gee J., Glover M., Herring B., Kang Y., Lucas P., Noblit C., Tropper J., Vogt T., Weintraub E. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration - United States, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:591–593. doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- Song F., Yu M., Yang J., Xu H., Zhao Y., Li W., Wu D., Wang Z., Wang Q., Gao X., Wang Y., Fu R., Sun Y., Gao R., Yang Y., China Acute Myocardial Infarction (CAMI) Registry Study Group Symptom-onset-to-balloon time, ST-segment resolution and in-hospital mortality in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention in China: from China acute myocardial infarction registry. Am. J. Cardiol. 2016;118:1334–1339. doi: 10.1016/j.amjcard.2016.07.058. [DOI] [PubMed] [Google Scholar]
- Struyf T., Deeks J.J., Dinnes J., Takwoingi Y., Davenport C., Leeflang M.M., Spijker R., Hooft L., Emperador D., Dittrich S., Domen J., Horn S.R.A., Van den Bruel A., Cochrane COVID-19 Diagnostic Test Accuracy Group Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID-19 disease. Cochrane Database Syst. Rev. 2020;7 doi: 10.1002/14651858.CD013665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun C., Dyer S., Salvia J., Segal L., Levi R. Worse cardiac arrest outcomes during the COVID-19 pandemic in Boston can be attributed to patient reluctance to seek care. Health Aff. Proj. Hope. 2021;40:886–895. doi: 10.1377/hlthaff.2021.00250. [DOI] [PubMed] [Google Scholar]
- Terkelsen C.J., Sørensen J.T., Maeng M., Jensen L.O., Tilsted H.-H., Trautner S., Vach W., Johnsen S.P., Thuesen L., Lassen J.F. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- Timeline of WHO'’s response to COVID-19 [WWW Document] 2020. https://www.who.int/news-room/detail/29-06-2020-covidtimeline URL. (accessed 7.3.20)
- Wadhera R.K., Shen C., Gondi S., Chen S., Kazi D.S., Yeh R.W. Cardiovascular deaths during the COVID-19 pandemic in the United States. J. Am. Coll. Cardiol. 2021;77:159–169. doi: 10.1016/j.jacc.2020.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westgard B.C., Morgan M.W., Vazquez-Benitez G., Erickson L.O., Zwank M.D. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann. Emerg. Med. 2020;76:595–601. doi: 10.1016/j.annemergmed.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing C., Simon K., Bello-Gomez R.A. Designing difference in difference studies: best practices for public health policy research. Annu. Rev. Public Health. 2018;39:453–469. doi: 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324:510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zacher H., Rudolph C.W. Individual differences and changes in subjective wellbeing during the early stages of the COVID-19 pandemic. Am. Psychol. 2020 doi: 10.1037/amp0000702. [DOI] [PubMed] [Google Scholar]