Abstract
The current study visualized ADHD symptom networks in a longitudinal sample of participants across childhood and adolescence with exploratory examination of age and gender effects. 836 children ages 7–13 years were followed annually for eight years in total. Across parent and teacher report, results suggested is easily distracted and difficulties sustaining attention as central symptoms across three testing points (i.e., Year 1, Year 3, and Years 5–8 collapsed). Difficulties following instructions and intrudes/interrupts also emerged as parent-reported central symptoms. Assessment of network structure across the three testing points suggested global robustness of relations among ADHD symptoms from mid-childhood into early adolescence. However, relations among symptoms that cause problems in school settings (i.e., being easily distracted) were stronger in teacher-reported than parent-reported networks. When aggregated into a sum score, central symptoms during Year 1 predicted total difficulties related to mental health problems five years later just as well as all 18 symptoms. Central symptoms of ADHD may be useful as screeners of future emotional and behavioral difficulties.
Keywords: Childhood and Adolescent ADHD, Network Analysis, Longitudinal, Predictive Validity
General Scientific Summary
This study suggested that a subset of ADHD symptoms (i.e., is easily distracted; difficulties sustaining attention; difficulties following instructions, and intrudes/interrupts) may be particularly informative when screening for ADHD and assessing risk for future total difficulties throughout childhood and adolescence.
Attention-deficit/hyperactivity disorder (ADHD) is a relatively common yet highly impairing neurodevelopmental disorder that begins in childhood and often continues into adulthood with serious secondary complications (Faraone, 2000; Kessler et al., 2006; Polanczyk et al., 2007). As conceived in the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5; APA 2013), ADHD has two symptom domains, inattention and hyperactivity-impulsivity, with nine symptoms in each domain. As a result, its criteria set is one of the largest of any disorders in the DSM-5 (APA, 2013).
When conceptualizing the structure of ADHD symptoms, most prior research has relied on common cause models, which assume that symptoms of ADHD co-occur due to a common underlying cause or vulnerability, such as behavioral disinhibition or emotion dysregulation (Barkley, 1997; Shaw et al., 2014). Yet, as seen with other mental health conditions (Kendler, 2005; Nolen-Hoeksema & Watkins, 2011; Caspi & Moffit, 2018), this approach may be insufficient for capturing the massively multifactorial etiology and expression of ADHD (Thapar, Cooper, Eyre, & Langley, 2016). Additionally, ADHD is characterized by a great degree of heterogeneity, as symptom presentation often presents quite differently across individuals and across development (Lahey et al., 2005; Olson, 2002). Such facts are difficult to fit conceptually to a single causal framework and suggest the need for innovative approaches to model such complexity at the symptom level.
An alternative conceptualization is that symptoms, and the relationships among them, are constitutive of psychological disorders. This is a different set of conceptual assumptions than latent variable analysis or the DSM-5, which both assume that symptoms are reflective of underlying disorders or latent constructs (e.g., ADHD). Conversely, a network approach is designed to be conceptually compatible with a complex dynamic system. It entails a different meta-assumption: a process wherein the activation of one symptom may be strongly associated with the activation of other symptoms, potentially leading to increased dysfunction via mutually reinforcing interactions among symptoms (see Supplemental Material; for more elaboration see Borsboom et al., 2017; Fried, van Borkulo, Cramer, Boschloo, Schoevers, & Borsboom, 2017; McNally, 2016). In other words, disorders may arise from symptoms and the relations among them, rather than the other way around.
This perspective can be modeled using a computational method called network analysis. While not necessarily precluding the existence of latent traits or disorders, the network approach facilitates an investigation of the role of individual symptoms in a network of diagnostic criteria and easily accommodates developmental change in the importance of symptoms over time. Hence, it can provide clues regarding symptoms as mechanisms of developmental change.
In relation to ADHD, this approach might mean that, for example, symptoms of hyperactivity make children impulsive which, in turn, makes it more difficult for them to concentrate, with this process operating particularly during early childhood (versus later childhood and adolescence). Or, we might identify a process wherein the symptoms being forgetful in daily activities and experiences difficulties organizing tasks and activities may demonstrate a mutually reinforcing interaction such that the presence of one symptom is highly likely to co-occur with the presence of the other, with this process being particularly striking during later childhood and adolescence (versus early childhood). Overall, the network approach and accompanying network analysis techniques may be crucial for expanding our understanding of ADHD by suggesting that co-occurrence among symptoms may not solely reflect underlying common causes or overlapping variation among symptoms, but may also emerge from direct interactions among symptoms themselves.
One major question regarding any multivariate characterization of structure within ADHD concerns the robustness of the characterization over time. For network symptom structure, this question is largely unexplored across the field of psychopathology. Thus, additional research is needed pertaining to the stability of cross-sectional complex networks relevant to psychopathology particularly during development. Examination of both robustness and developmental change in networks of ADHD over time could advance understanding of the temporal dynamics of the symptoms of ADHD.
To our knowledge, only one study has applied the network approach to ADHD across multiple age ranges to examine development (Martel, Levinson, Langer, & Nigg, 2016). This study utilized cross-sectional samples from preschool to adulthood, with results suggesting that ADHD symptom structure became more differentiated over development. Additionally, two symptoms: often easily distracted and difficulty sustaining attention, emerged as central symptoms across all age groups. Yet, due to the use of cross-sectional samples, this study was unable to assess change within individuals, nor was it able to fully assess the predictive validity of central symptoms. More recently, Silk and colleagues (2019) assessed ADHD symptom networks cross-sectionally in children. They identified interrupts, loses things, and does not follow instructions as central symptoms; weighted symptom counts created by taking symptoms’ centrality into account exhibited concurrent and predictive validity comparable to that of traditional symptom count scores. Further, Preszler et al. (2020) found three symptom communities (i.e., a cluster of symptoms that exhibit many connections within the cluster but fewer connections with symptoms outside of it) of inattention, hyperactivity, and hyperactivity/impulsivity in a large sample of first graders, rated by mothers and fathers, that were largely invariant across a six-week period.
The Current Study
We report here the first use of network modeling across three testing points of a multi-year, longitudinal sample to evaluate stability and development of ADHD symptoms within a well-characterized sample of children with ADHD. Data for each testing point was collected between two and five years apart to facilitate an examination of three networks (i.e., one network for each testing point) during somewhat distinct age ranges across childhood and adolescence. Evidence of stability of network findings across independent samples is crucial, but has been lacking for ADHD. The study was designed therefore to build on the findings described above.
Consistent with past network studies of ADHD (i.e., Martel et al., 2016; Silk et al., 2019), it was hypothesized that often easily distracted and difficulty sustaining attention, along with interrupts, loses things, and does not follow instructions, would emerge as central symptoms across all networks. Further, replicating Martel and colleagues’ findings, it was hypothesized that although networks would feature consistent relations among symptoms across testing points, symptoms would become less related (i.e., more differentiated) from childhood to adolescence. We additionally sought to compare the predictive validity of central symptoms during the first testing point, as compared to all ADHD symptoms, with respect to total difficulties five years later. It was hypothesized that central symptoms, together, would account for equal variance in total difficulties five years later compared to all symptoms. Lastly, we explored possible effects of age and sex of the child on network structure (Howard et al., 2017).
Methods
Study Overview
Participants were drawn from the Oregon ADHD Cohort, a well-characterized child cohort with a planned missingness design for which the community-based recruitment, enrollment, and multi-informant assessment procedures for ADHD diagnosis have been published in detail elsewhere (Musser et al., 2016; Karalunas et al., 2017). Ethics approval was obtained from the Institutional Review Board at Oregon Health & Science University. A parent/legal guardian provided written informed consent and children provided written assent. 836 children were followed annually over 8 years. Data for the current study was drawn from 836 children from Year 1 (i.e., testing point 1; aged 7–13 years), 499 children in Year 3 (i.e., testing point 2; 9–15 years), and 411 children in Years 5–8 (i.e., testing point 3; 11–18 years). Regarding Years 5–8, the current study utilized each participant’s most recently provided data from these years in the larger study. This methodology was used to ensure a large enough sample size for an examination of ADHD networks while maintaining some distinction in age ranges between testing points. Testing points were selected to facilitate an investigation of ADHD networks across the important developmental transition from middle childhood into adolescence. Across all testing points, between 57 and 61% of participants met criteria for ADHD.
Sample Characterization
Volunteers were recruited via mass mailings, using commercial mailing lists, to all families with children in the target age range within the geographic radius of 50 miles from the University. The mailing made clear that we were looking for children with possible or definite ADHD, as well as for healthy, typically developing children with no history of learning or attention problems. In response to mailings to parents of all children in the target age range in our catchment area, we received 2144 inquiries. (A response rate of about 1% for non-ADHD participants and about 30% for ADHD participants.)
An initial screening phone call served to establish eligibility (below) and interest. Nearly half were ruled out at this stage due to medications, other illnesses (e.g. autism), or lack of interest. Those who were excluded at this stage did not differ reliably from the final sample on sex ratio (p = .11) or non-white race (p = .22), but were marginally lower income (p = .06) and slightly younger (p = .06).
For those remaining (n = 1,449), an in-person “diagnostic” visit was then scheduled. Here, a parent completed the Conners’ Rating Scales-3rd Edition short form (Conners’-3), Strengths and Difficulties Questionnaire long form (SDQ), the ADHD Rating Scale (ADHD-RS), and a semi-structured clinical interview administered by a Master’s-degree level clinician (i.e., Kiddie Schedule for Affective Disorders and Schizophrenia; KSADS). Children completed a brief unstructured clinical interview with the same clinician. Teachers were contacted and completed the Conners’-3, SDQ, and ADHD-RS.
All clinical interviewers were trained to reliability of kappa >.80 for all diagnoses seen at ≥ 5% base rate in this sample on the KSADS to a master interviewer and had videotapes viewed by a supervisor and reviewed periodically to prevent procedural drift. Psychometric testers were trained to an accuracy standard prior to beginning work and also had videotapes viewed periodically to prevent drift.
Diagnostic Assignment
All materials were scored and presented to a clinical diagnostic team comprising board certified child psychiatrist with over 25 years of experience and a licensed child neuropsychologist with over 10 years of experience. Blind to one another’s ratings, they formed a diagnostic opinion based on all available information. Their agreement rate for all diagnoses discussed in this paper was satisfactory (ADHD, kappa = .88; ADHD subtype, k > .80, all other disorders with at least 5% base rate, k > .68). Disagreements were conferenced and consensus reached. Cases where consensus was not achieved for ADHD diagnosis were excluded.
Using a best estimate procedure, DSM-IV diagnoses were made independently by each clinician. To count symptoms, the clinicians used the following rule: If both parent and teacher ratings exceeded a t-score of 60 on at least one ADHD scale and both rated at least 3 symptoms as “often” or “very often” on the ADHD rating scale (or for parents, were counted present on the KSADS), the “or” algorithm could be employed. When either informant fell below this mark, and clinicians judged that this was not explained by successful medication treatment during the school day, then the case was rejected as failing to meet the DSM requirement of substantial symptoms present in more than one setting. In addition, it was required that all other DSM criteria were met, including (a) impairment (determined through clinical interview and questionnaires), (b) onset prior to age 7 (current at the time we began enrollment), (c) sustained impairing symptoms > 1 year, and (d) symptoms of ADHD were not better accounted for by comorbid conditions, trauma history, or other confounds.
Longitudinal Retention
Participants included 836 children in Year 1, from whom n = 610 were selected for long term follow up study. They were followed annually for eight sequential years. With regard to retention, of those 610, resource limitations mandated a planning missing design from among those youth such that the target N was 535 at Year 3 and to be determined for Years 5–8. In actuality, we saw 527 children in Year 3 and up to 413 each year from Years 5–8 (data collection for these years is still ongoing, with some children excluded from the current study because of incomplete data). Those selected for follow up were chosen because their ADHD and non-ADHD status was clear and unambiguous. Those not followed included those with parent-teacher disagreement or sufficient comorbidity to reduce confidence that they were clear cases or non-cases by our criteria.
Measures
ADHD Symptoms
For the network analyses in this study, parent- and teacher-report versions of the ADHD-Rating Scale for DSM-IV1 (ADHD-RS; DuPaul et al., 1998; Puig-Antich & Ryan, 1986) were used as the measure of ADHD symptomatology. Parents (Year 1: α = .93; Year 3: α = .94; Years 5–8: α = .94) and teachers (Year 1: α = .97; Year 3: α = .97; Years 5–8: α = .96) responded to all 18 items on a 0 (rarely or never) to 3 (always or very often) scale. Items in each symptom domain were alternated on the rating scale, and all symptoms were included in network models. Among the parent raters, 79% were women in the primary caregiving role (most were biological mothers who chose to participate due to availability Year 1: age range 25–66 years, average age = 40 years). Informant demographic information was not available on teachers. Teacher response rate was 100% at Year 1 (required for inclusion) and > 80% for Years 3 and 5–8. Of note, a positive skew was identified for several ADHD symptom variables.
Total Difficulties
Total Difficulties were assessed using the self-reported version of the Strength and Difficulties Questionnaire (SDQ; Goodman, Meltzer, & Bailey, 1998). The SDQ is a 25-item behavioral questionnaire that assesses various psychopathology or functional domains. These items are scored on a three-point Likert scale (i.e., 0 = “Not True”, 1 = “Somewhat True”, 2 = “Certainly True”; some items are reverse coded), with scores on these items added to form Emotional Symptoms, Conduct Problems, Hyperactivity, Peer Problems, and Prosocial Scales. Emotional Symptoms, Conduct Problems, Hyperactivity, and Per Problems scale scores can then be added together to form a Total Difficulties score ranging from 0–40, with higher scores indicating greater difficulty. The Total Difficulties score was used in analyses to compare the predictive validity of central ADHD symptoms versus all symptoms. Past work has provided support for the validity of scores on the SDQ in school-aged populations (Van Roy, Veenstra, & Clench-Aas, 2008), and the internal consistency of scores within the Total Difficulties scale was adequate for inclusion in the current study (α ≥ .71).
Statistical Analyses
The R package qgraph was used to construct networks (Epskamp, Cramer, Waldorp, Schmittman, & Borsboom, 2012) using Graphical Gaussian Models with the Least Absolute Shrinkage Operator (GLASSO; Friedman et al., 2008; Epskamp et al., 2018) and extended Bayesian Information Criterion (EBIC) model selection (Foyget & Drton, 2010). A gamma (γ) hyperparameter of 0.5 was selected for the GLASSO to ensure high specificity in networks. Three networks were created to represent the three testing points included in the current study. Each network depicted regularized partial Spearman correlations among ADHD symptoms (Epskamp & Fried, 2018). Network structure was examined through the specification of symptom communities (i.e., strong relations among symptoms within the community compared to those outside of it) within each network using the R package igraph (Csardi & Nepusz, 2006). Communities were identified using the spinglass algorithm (Reichardt and Bornholdt, 2006), with the algorithm being run 1000 times and the median number of communities selected as the most stable.
Symptom Centrality
Expected Influence (i.e., the sum of the absolute edges attached to a node while accounting for negative edges) was used to determine central symptoms that exerted a strong influence on other symptoms within ADHD networks (Epskamp et al., 2012; Boccaleeti, Laotra, Moreno, Chavez, & Hwang, 2006; Robinaugh et al., 2016), with higher values suggesting greater centrality. Central items were specified as those that had Expected Influence values at least 1 standard deviation above the average value in at least two testing points. Bootstrapped difference tests comparing the Expected Influence of symptom pairs were also utilized to determine central symptoms. These tests are described in the Supplemental Material. Stability of centrality indices was assessed using the correlation-stability coefficient (CS) as calculated within the R-package bootnet. This index indicated the proportion of participants that could be eliminated from analyses while retaining a correlation of at least 0.7 between the revised and original centrality estimates within a 95% confidence interval (Epskamp et al., 2017). CS values range from 0–1; values above .25 are interpreted as adequate stability and above .5 as good stability (Epskamp & Fried, 2018).
Comparing Networks across Testing Points.
As a preliminary analysis of the robustness of network structure, we assessed correlations between respective edges in each pair of networks (i.e., Year 1 versus Year 3; Year 1 versus Years 5–8; Year 3 versus Years 5–8). All pairs of networks were compared using the R-package NetworkComparisonTest (NCT, van Borkulo, Boschloo, Kossakowski, Tio, Schoevers, Borsboom, & Waldorp, 2017). Each comparison only included participants who had complete data available in both years as required by the dependent comparison test within NCT (see below for exact sample sizes). Two tests of invariance were conducted (Borkulo et al., 2017): the first assessed the difference between networks’ global strength estimates (S), or the sum of all absolute edge values in each network. The second explored whether network pairs contained generally consistent relations among symptoms by assessing the maximum difference in corresponding relations among symptoms (M).
Predictive Validity of Central Symptoms.
Hierarchical regression analyses were conducted post-hoc to assess the ability of central symptoms in Year 1 for predicting Total Difficulties scores in Year 6 of the larger study. Analyses were conducted separately for parent- and teacher-report. Within each reporter-type, two models were tested: in the first model, the SDQ Total Difficulties score was regressed onto the Year 1 Total ADHD Sum Score. In the second model, the Total Difficulties score was regressed onto the Year 1 Central Sum Score, which was created by adding Year 1 scores on central symptoms. The R2 between these two models was qualitatively compared to determine whether central symptoms of ADHD accounted for future Total Difficulties to a different degree than all symptoms.
Statistical Power
For network comparison tests, 493 children had data available for the Year 1 versus Year 3 comparison, 409 children had data available for Year 3 versus Years 5–8, and 370 children had data available for Year 1 versus Years 5–8. Pertaining to statistical power, consensus guidelines concerning statistical power when conducted network studies have yet to be determined. Yet, prior work based on simulation studies has recommended three participants per parameter estimated as a “rule-of-thumb” (Epskamp & Fried, 2018). Given that the 153 parameters estimated in these networks equates to 459 required participants, it is likely that the current study had adequate power for creating networks in Year 1, although statistical power may have been more limited in Years 3 and 5–8.
Results2
Detailed demographic data of participants in each testing point are available in Table 1. Parent-reported networks in Years 1, 3, and 5–8 are depicted in Figure 1, while teacher-reported networks are depicted in Figure 2. Symptom centrality values in each year are depicted in Figure 3. Regularized partial correlation matrices and results of tests comparing the Expected Influence of symptoms in each year is available in the Supplemental Material. Approximately 37% of participants were girls and 84% identified as White. The average age of participants was 9.6 years in Year 1, 11.4 years in Year 3, and 15.5 years in Years 5–8.
Table 1.
Sample Demographic Information Across Years
| Variable | Year 1 | Year 3 | Years 5–8 |
|---|---|---|---|
| N = 836 | n = 499 | n = 411 | |
| Sex (n [%] Girls) | 317 (37.9) | 188 (37.7) | 151 (36.7) |
| Age (M [SD]) | 9.6 (1.51) | 11.4 (1.48) | 15.5 (0.8) |
| Race (n [%] White) | 709 (84.8) | 419 (84.0) | 348 (84.7) |
| Family Incomea (n [%]) | |||
| 0 – 50,000 | 204 (24.4) | 123 (24.6) | 114 (27.7) |
| 50,001 – 100,000 | 345 (41.3) | 210 (42.1) | 174 (42.3) |
| 100,001 – 150,000 | 164 (19.6) | 103 (20.6) | 80 (19.5) |
| > 150,001 | 66 (8.5) | 35 (7.0) | 25 (6.1) |
| Estimated Full Scale IQ [M(SD)] | 110.7 (13.86) | 111.4 (13.99) | 112 (13.97) |
| ADHD Total Sum Score | 19.6 (14.32) | 17.6 (13.69) | 15.9 (12.29) |
| ADHD (n [%] Positive) | 500 (59.8) | 302 (60.5) | 234 (56.9) |
Note.
57 participants at Year 1, 28 in Year 3, and 18 in Years 5–8 did not have data available for Family Income (i.e., declined to answer or did not know). Year 1 = aged 7–13 years, Year 3 = 9–15 years, and Years 5–8 was created by including each participant’s most recently provided data from Years 5–8 of the larger study (11–18 years). The methodology of collapsing Years 5–8 ensured a large enough sample size to create networks while maintaining some distinction between ages within each testing point.
Figure 1.
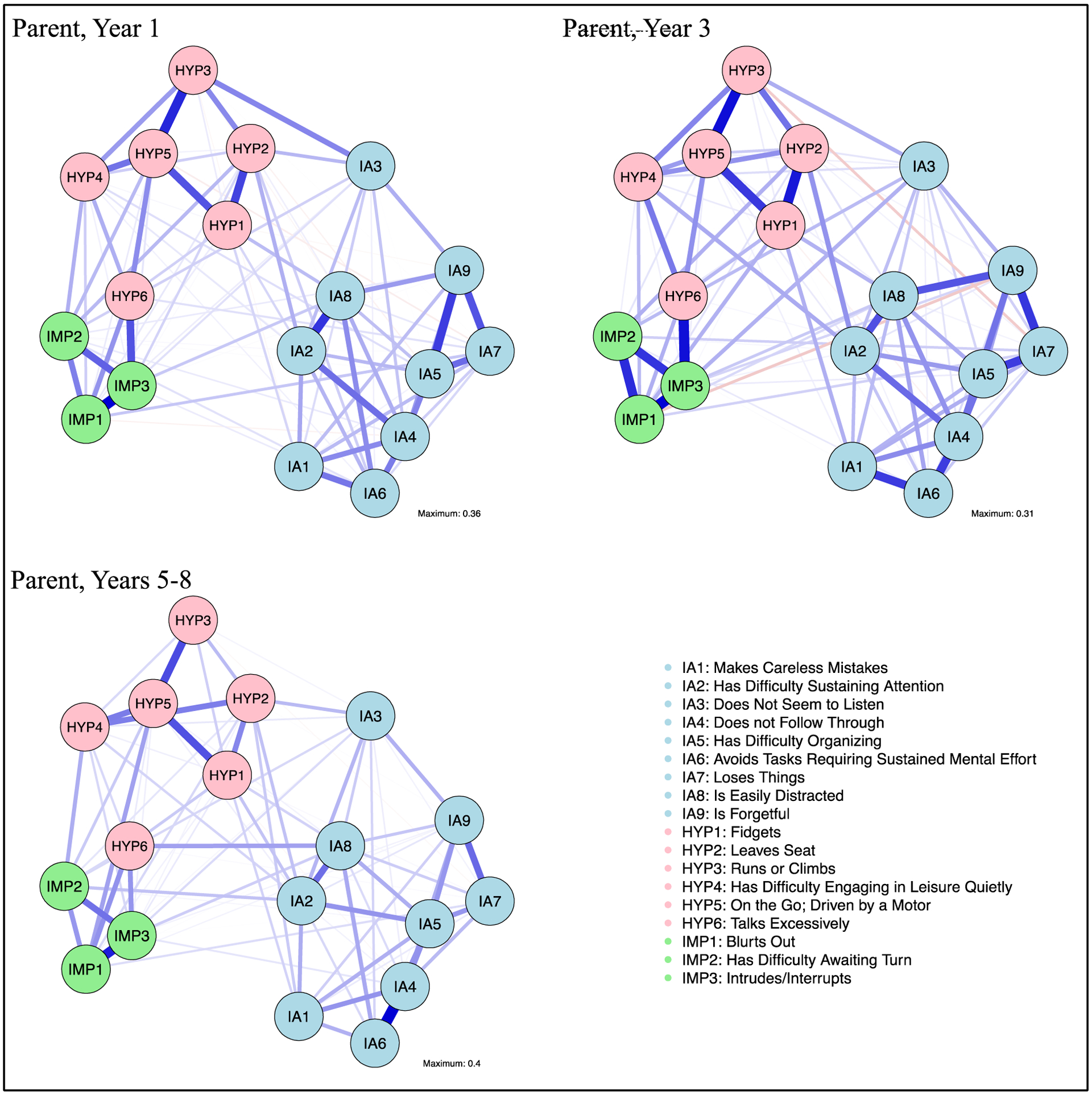
Parent-reported ADHD symptom networks (based on the ADHD Rating Scale-IV) across three longitudinal years of a larger study (Year 1 = 7–13 years; Year 3 = 9–15 years; Years 5–8 = 11–18 years). Networks were created using data from children with and without ADHD. Symptoms are depicted as nodes, with edges connecting these nodes depicting regularized partial Spearman correlations. Edge thickness represents the strength of the relation. Solid edges indicate positive relations and dashed edges indicate negative relations. IA = inattentive symptoms, HYP = hyperactive-impulsive symptoms, IMP = impulsive symptoms. A detailed figure depicting all edges labeled with their strength is available in the Supplemental Material.
Figure 2.
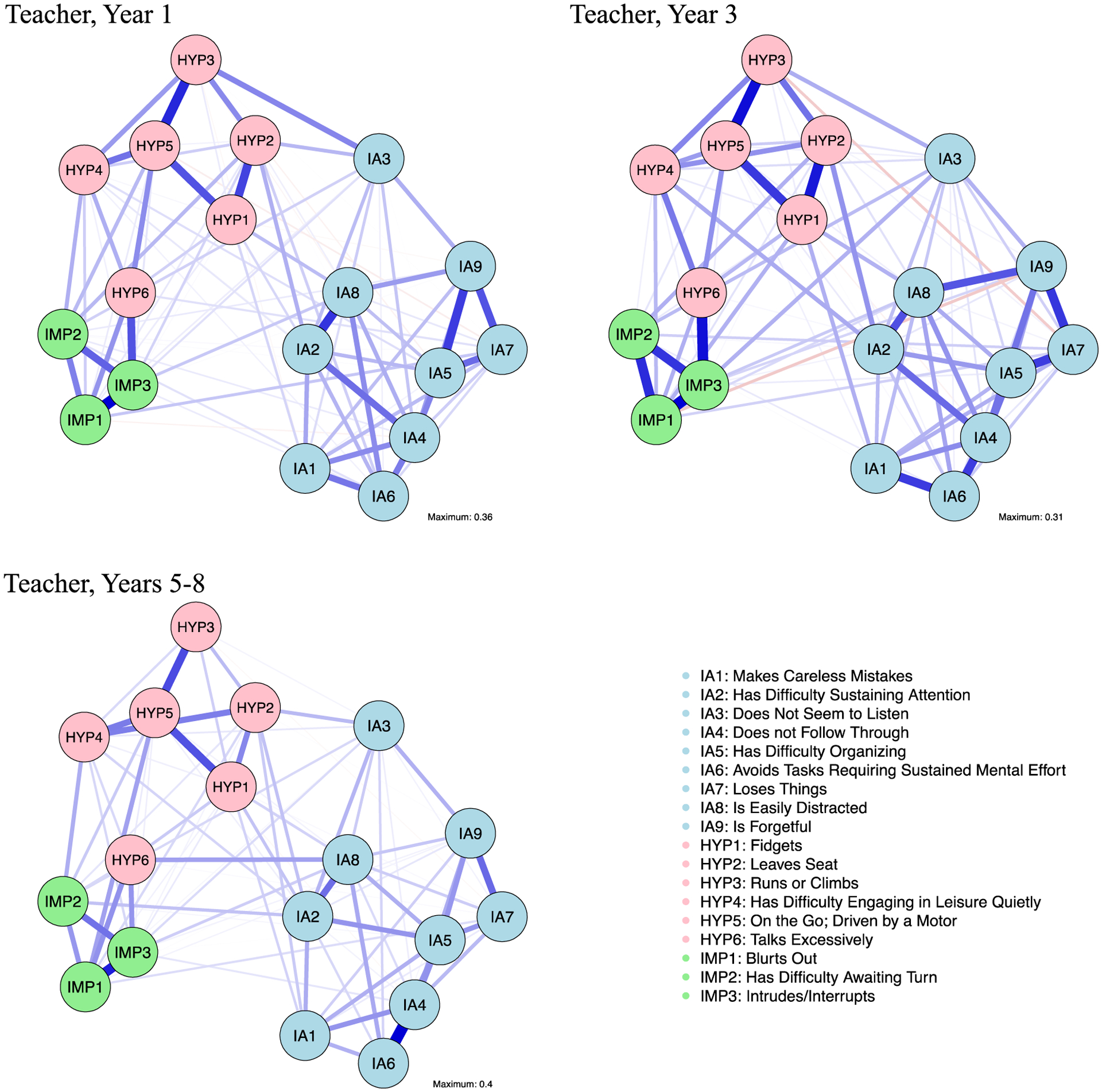
Teacher-reported ADHD symptom networks (based on the ADHD Rating Scale-IV) across three longitudinal years of a larger study (Year 1 = 7–13 years; Year 3 = 9–15 years; Years 5–8 = 11–18 years). Networks were created using data from children with and without ADHD. Symptoms are depicted as nodes, with edges connecting these nodes depicting regularized partial Spearman correlations. Edge thickness represents the strength of the relation. Solid edges indicate positive relations and dashed edges indicate negative relations. IA = inattentive symptoms, HYP = hyperactive-impulsive symptoms, IMP = impulsive symptoms. A detailed figure depicting all edges labeled with their strength is available in the Supplemental Material.
Figure 3.
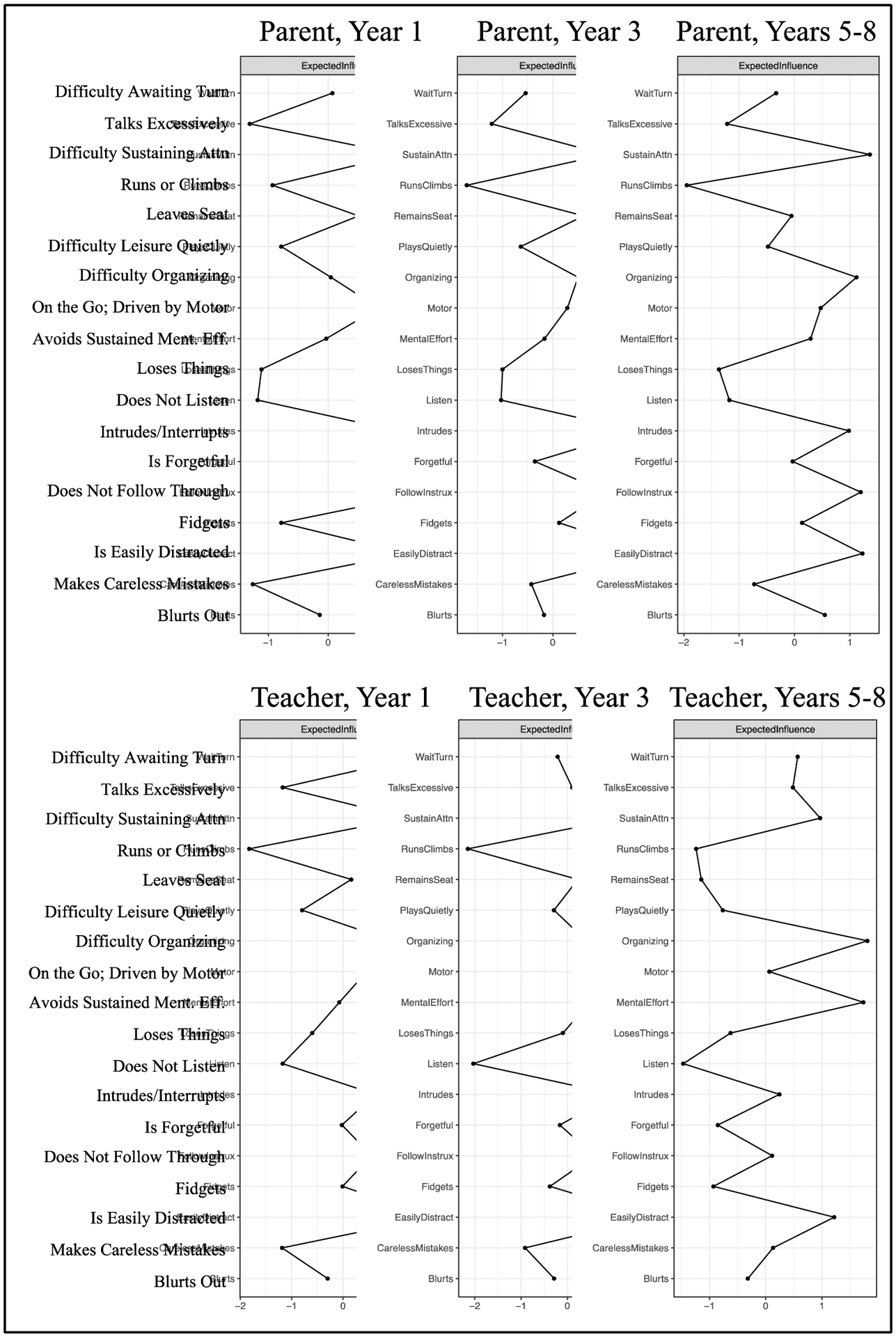
Plot denoting Expected Influence metrics for ADHD symptoms. Symptoms are depicted on the y-axis, and z-scores for bridge Expected Influence are depicted on the x-axes. Values farther to the right indicate higher Expected Influence values, thus implying that the respective symptom demonstrated more robust relations with other symptoms in the network. In the current study, central symptoms were specified as those with an Expected Influence > 1 standard deviation above the average value in at least two years.
Preliminary checks suggested no significant differences between those with and without complete data across years based on sex (X2[1, N = 836] = .43, p = .51). No differences were identified between those with (M = 18.55) and without (M = 16.23) complete data on teacher-reported Total ADHD Sum Scores at Year 1(F[1, 789] = 1.42, p = .23, partial η2 = .002). Those without complete data across all three years (M = 20.77) had significantly higher parent-reported Total ADHD Sum Scores at Year 1 than those with complete data (M = 18.09), although the effect size of this difference was negligible (F[1, 834] = 7.27, p = .01, partial η2 = .01). No differences were found between those with and without full data on SDQ Total Difficulties (F[1, 310] = 1.62, p = .21, partial η2 = .01).
Parent-Reported ADHD Symptom Networks
Across the three resulting networks, the spinglass algorithm, in general, suggested three communities of ADHD symptoms that fell in line with inattentive, hyperactive, and impulsive symptom domains (Figures 1–3). Talks excessively clustered with impulsive symptoms in all networks. Preliminary stability analyses suggested edges within each network were generally robust, with the strength of several edges being significantly different from zero (see Supplemental Material for a detailed description and results of these analyses).
Central Symptoms
Centrality stability analyses suggested stability in Expected Influence (CSs ≥ .67) across all networks. Assessment of Expected Influence revealed three central symptoms across testing points. These symptoms were as follows, with symptom domain (IA = inattentive, HYP = hyperactive, IMP = impulsive) and a subset of correlated symptoms across years included in parentheses: (1) difficulties sustaining attention (IA; has difficulties organizing; is easily distracted; has difficulty remaining in one’s seat); (2) difficulty following instructions (IA; makes careless mistakes; difficulties sustaining attention; difficulties with sustained mental effort; is easily distracted; is forgetful); (3) is easily distracted (IA; difficulties sustaining attention; difficulties with sustained mental effort). Intrudes/interrupts (IMP; talks excessively; blurts; difficulties waiting one’s turn) emerged as a central symptom in Years 1 and 3.
In sum, difficulties sustaining attention; difficulties following instructions; and is easily distracted emerged as central symptoms across all testing points in parent-reported networks due to robust associations with other symptoms characterized by difficulties with sustained concentration and organization. Additionally, intrudes/interrupts also emerged as a central symptom in Year 1 and Year 3.
Longitudinal Stability and Change in Network Structure of Parent-Reported Symptoms
Assessment of correlations between corresponding edges in network pairs suggested generally robust similarities in edges within networks across years (rs ≥ .72). Regarding network structure, omnibus tests suggested stability in network edges across years, with significant differences (ps < .001) emerging only with regard to two edges in Year 1 versus 3 comparisons (difficulties sustaining attention – difficulty following instructions; difficulties following instructions – difficulties with sustained mental effort) and one edge (difficulties following instructions – difficulties with sustained mental effort) in Year 3 versus 5–8 comparisons. No significant differences emerged in global strength across any comparisons (ps ≥ .38; Year 1: global strength = 8.76; Year 3: global strength = 8.65; Years 5–8: global strength = 8.54). Overall, results of network comparisons suggested that the structure of ADHD symptom networks was generally robust.
Teacher-Reported ADHD Networks Across Years
Results were generally consistent with those including parent-reported ADHD symptoms. Across years, the spinglass algorithm, in general, suggested three communities of ADHD symptoms consistent with inattentive, hyperactive, and impulsive symptom domains, although hyperactive and impulsive items were combined into one community in Year 3. Talks excessively clustered with impulsive symptoms in all networks.
Central Symptoms
Centrality stability analyses suggested adequate stability in Expected Influence (CSs ≥ .44) in all three networks. Assessment of Expected Influence suggested is easily distracted as a central symptom in all networks (IA; difficulty sustaining attention; difficulty staying organized; talks excessively). Additionally, difficulty sustaining attention (IA; fidgets; has difficulty remaining in one’s seat; is easily distracted) emerged as a central symptom in Years 1 and 3. Recall that these were two of the three central symptoms in the parent report.
Longitudinal Stability and Change in Network Structure of Teacher-Reported Symptoms
Based on the NCT, omnibus tests suggested no significant differences in global network structure (ps ≥ .17). Similarly, no significant differences in networks’ global strength emerged across testing points (ps ≥ .44; Year 1: strength = 9.03; Year 3: strength = 9.02; and Years 5–8: strength = 8.32). Of note, Year 3 was not compared to Years 5–8 due to the low number of overlapping participants with teacher ratings in both years (n = 53). Overall, results pertaining to teacher-reported networks were largely consistent with parent-reported networks, as network structure appeared to be robust.
Predictive Validity of Central Sum Scores
In analyses including parent-report, Central Sum Scores were created from responses on difficulties following instructions, is easily distracted, intrudes/interrupts, and difficulties sustaining attention. Conversely, Total Sum Scores were computed by adding together responses on all 18 parent-reported ADHD symptoms. Regression analyses suggested that Year 1 Total Sum Scores accounted for 18% of variance in Total Difficulties five years later (F[1, 310] = 67.24, p < .001, partial η2 = .18). Conversely, Central Sum Scores accounted for 18% of variance in Total Difficulties five years later (F[1, 310] = 68.84, p < .001, partial η2 = .18).
In analysis including teacher-report, Central Sum Scores were created from responses on is easily distracted and has difficulty sustaining attention. Conversely, Total Sum Scores were computed by adding together responses on all 18 teacher-reported ADHD symptoms. Regression analyses suggested that Year 1 Total Sum Scores accounted for 13% of variance in Total Difficulties five years later (F[1, 300] = 44.29, p < .001, partial η2 = .13). Conversely, Central Sum Scores accounted for 14% of variance in Total Difficulties five years later (F[1, 300] = 47.11, p < .001, partial η2 = .14). In sum, four parent-reported symptoms, or two teacher-reported symptoms, appeared to account for generally as much variance in Total Difficulties five years after Year 1 as all 18 symptoms when summed into a single total score.
Comparing Parent- and Teacher-Reported Networks
As a supplemental analysis, we compared parent- and teacher-reported networks during Year 1 using the NCT. Network structure was generally consistent across parent- and teacher-reported symptoms of ADHD, although three edges were found to be stronger in parent-reported networks than teacher-reported networks (i.e., blurts – has difficulty waiting one’s turn; easily distracted – talks excessively; difficulty waiting one’s turn – intrudes/interrupts; ps < .001). Regarding networks’ overall connectivity, comparison tests suggested no differences in overall strength of edges in parent- and teacher-reported networks (p = .46).
Exploration of Network Differences Based on Child Sex and Age
Supplemental analyses revealed that boys had significantly higher Total ADHD Sum Scores than girls across years and reporters (ps ≤ .01; partial η2s ≥ .02), except Years 5–8 teacher-report (p = .11; partial η2 = .03). Hence, to explore whether this impacted network structure, we used the NCT to compare Year 1 network structure in boys versus girls (Year 1 was selected to ensure statistical power). Across parent- and teacher-report, omnibus tests suggested no differences in the relations among symptoms in networks including males versus those including females (parent-report: maximum difference in respective relations = .16; p = .56; teacher-report: difference = .15; p = .81). No differences were found with respect global strength (parent-report: p = .20; teacher-report: p = .41) across networks including boys (parent-report: strength = 8.60; teacher-report: strength = 8.78) versus girls (parent-report: strength = 8.83; teacher-report: strength = 8.48). Overall, results in Year 1 suggested robustness in structure of networks across boys and girls.
In order to try to ascertain developmental differences with more sensitivity, we also reconstructed parent- and teacher-reported networks in the younger half of the sample from Year 1 (n = 477; M = 8.51 years, SD = .65), with Year 1 being used to ensure statistical power. This sample was obtained using a mean split strategy (mean age = 9.63 years). Results were generally consistent with those in primary analyses. Specifically, the spinglass algorithm suggested four communities of ADHD symptoms in parent-reported networks (i.e., hyperactive, impulsive, and two communities representing encompassing primarily inattentive symptoms), as well as three communities in teacher-reported networks consistent with DSM-5 symptom domains.
Assessment of Expected Influence suggested is easily distracted (IA) as a central symptom across reporter. In parent-reported networks, intrudes/interrupts (HYP) and difficulties sustaining attention (IA) also emerged as central symptoms. In teacher-reported networks, difficulty waiting one’s turn (IMP), driven by a motor (HYP), and difficulty following instructions (IA) emerged as additional central symptoms. Detailed results of these analyses are available upon request.
Lastly, to facilitate a direct comparison of the youngest and oldest children available, the NCT was used to compare parent-reported networks in the sample of young children described above versus the older half of the sample in Years 5–8 (also derived from a mean-split strategy). This older sample (n = 159) had an average age of 16.25 years. Results suggested no significant differences in global network structure and global strength across the two samples (ps ≥ .19). Teacher-reported networks were not compared due to low numbers of participants in Years 5–8. In sum, more intensive supplemental tests provided further support for the robustness of the ADHD network across childhood and adolescence.
Discussion
Symptoms of ADHD and other mental disorders have long been conceptualized as reflective of underlying common causes (e.g., emotion dysregulation, behavioral inhibition) or a latent disorder or trait (i.e., ADHD). As a result of this theoretical approach, prior work has generally combined all ADHD symptoms into a small number of composite scores or latent factors via confirmatory or exploratory factor analysis. Although parsimonious, techniques consistent with this approach (e.g., subtypes, continuous modifiers; APA, 2013; Lahey & Wilcutt, 2010) have largely precluded an exploration of symptom-to-symptom relations that may help explain the nature of ADHD persistence over time. Across three years in a longitudinally collected dataset, the current study sought to examine the utility of an innovative network approach for providing an additional explanation for the nature of ADHD: it derives from a complex network of interactions among observable symptoms, with each symptom providing differential clinical relevance and utility with respect to disorder expression and possibly remediation. Such an approach, if successful, might suggest useful screening items that are core to the developmental progression of ADHD, as well as perhaps personalized intervention targets.
Stable Communities of ADHD Symptoms in Line with Symptom Domains
Across all three years, community detection analyses suggested symptoms of ADHD appeared to form inattentive, hyperactive, and impulsive communities (similar to Preszler et al., 2020), largely in line with previously identified symptom domains, but notably distinct from the usual conclusion of only two symptom domains using factor analysis (Willcutt et al., 2012). Notably, this structure was consistent not only across testing points in the current sample, but also replicated across reporter, suggesting robustness in specific symptom communities across this important developmental period. Past work has suggested that ADHD phenotypes may change throughout development (i.e., hyperactive/impulsive symptoms decreasing and inattentive symptoms increasing; Lahey et al., 2005; Olson, 2002) and that parent and teacher-report ADHD symptoms may be only weakly to moderately correlated (Martel, Markon, & Smith, 2017; Narad et al., 2014). Although not necessarily contradicting these studies, results of the current study suggested that the propensity for certain symptoms of ADHD to theoretically be accompanied by other specific symptoms may, in general, be robust across development and reporter.
Central Symptoms
Across parent and teacher-report, results suggested difficulties sustaining attention and is easily distracted as central symptoms across all or most years. Additionally, intrudes/interrupts and difficulties following instructions emerged as central symptoms across parent-reported networks. Together, findings suggested these symptoms may play key roles in the development, characterization, and maintenance of ADHD. Often easily distracted and difficulty sustaining attention were two of the core symptoms, consistent with prior work (Martel et al., 2016). Also notable was that more hyperactive/impulsive symptoms were central symptoms as rated by teachers in the younger children.
Those who exhibit difficulties following instructions may also be at elevated risk for making careless mistakes, having difficulties with sustained mental effort, and being forgetful. These symptoms may exhibit reciprocal and robust relations with each other, strengthening these types of problems over time. Such items should be evaluated for their utility for screening purposes in time-limited settings such as pediatrician offices.
Robustness of Network Structure Across the Three Years
Assessment of the networks’ structure across the three years suggested stability of ADHD networks from middle childhood to early adolescence, both in terms of individual symptom-to-symptom relations in general as well as the sum of the strength of all relations among symptoms. Results appeared to provide support for the robustness of networks’ structure, as well as (indirectly) the Expected Influence centrality index, by suggesting that relations among symptoms as conceptualized through networks, as a whole, may be relatively generalizable over time. Importantly, these results also held in analyses where networks from the youngest participants available were compared with those from the oldest available. This work may thus indirectly contribute to the ongoing debate regarding the stability of complex networks (e.g., Borsboom et al., 2017; Contreras, Nierto, Valiente, Espinosa, & Vazquez, 2019; Fried et al., 2017; Jones et al., 2017). Results of the current study suggested that the structure of relations among ADHD symptoms may persist throughout childhood and adolescence.
Replication Across Parent- and Teacher-Report
Importantly, ADHD symptom networks largely replicated across parent and teacher report. Not only did the network structure hold, but is easily distracted and difficulty sustaining attention emerged as central items across reporter. However, it should be noted that some nuanced differences in network structure also appeared based on reporter, with stronger associations emerging in teacher-reported networks among specific symptoms that commonly cause problems in school settings (i.e., blurting out of turn, being easily distracted, talking excessively, and intruding on others). This could indicate that, in school settings, these mostly impulsive symptoms may be more likely to be accompanied by one another and contribute to more generalized dysfunction, perhaps suggesting that clinicians should place extra attention on addressing these symptoms in school settings.
The robustness of the ADHD network structure is also compelling when considering the fact that while parent-raters were generally the same across the three testing points, teachers were likely to have changed. Hence, although past studies have suggested differences in ADHD symptom trajectories across the elementary school years (Murray, Booth, Ribeaud, & Eisner, 2018; Lahey et al., 2005; Olson, 2002), results of the current study suggested that relations among ADHD symptoms may not only be robust across reporters in different environments (i.e., parent versus teacher), but also across reporters in similar environments (i.e., teachers within schools).
Predictive Validity of Central Symptoms Compared to Sum Scores
It also should be noted that the small number of central symptoms appeared to demonstrate predictive validity, as these symptoms accounted for generally as much variance in Total Difficulties five years later as all 18 symptoms considered together. Prior work on the role of central symptoms in providing valid information has suggested conflicting results, with some studies providing support for the role of central nodes as highlighting primary intervention targets (Elliot, Jones, & Schmidt, 2019; Olatunji, Levinson, & Calebs, 2018; McNally et al., 2015; Ruzzano et al., 2015; Rodebaugh et al., 2018). Conversely, other work has suggested caution in interpreting and using centrality indices (Hallquist et al., 2019, Burns et al., 2019; Bringmann et al., 2013). Results of the current study were in line with the former list of studies: central symptoms of ADHD appeared to have particular clinical utility in predicting future difficulties. Thus, although further study is needed in this area, difficulties following instructions, is easily distracted, intrudes/interrupts, and difficulties sustaining attention may ultimately prove useful for informing the development of more efficient screening tools aimed at assessing ADHD with useful prediction of associated Total Difficulties across the important developmental transition from childhood to adolescence. Further, these symptoms may form the core of the ADHD construct in this age range and thus warrant targeted intervention upon initial identification.
Additionally, although the nature of the data precludes any causal interpretation of results, prior work has suggested that intervening on a central symptom may facilitate a downstream cascade of benefits to other related symptoms (McNally et al., 2016). More concretely, results are in line with the idea that focusing ADHD-related interventions first on children’s distractibility, difficulty following instructions, and intrusive behaviors, perhaps through behavioral modification techniques, may provide benefits to other symptoms within the ADHD network. Instead, results appeared to provide support for central items as core to the ADHD construct, as well as – more speculatively-- key targets for assessment and intervention. Such ideas merit replication and attention in future work.
Limitations
The current study is not without limitations. First, the current sample was a community-recruited sample in the Northwest enriched for ADHD to constitute a case-control design. This was a strength in that we had more cases of ADHD than prior studies of this nature. Yet, one important area for further work includes testing networks in a wider age range, particularly in younger samples to more directly assess the potential central role of hyperactive/impulsive symptoms. Further, prior work has cautioned against making causal interpretations based on the connectedness of elements in cross-sectional networks (Bringmann et al., 2019). Hence, any directional conclusions remain speculative, with additional rigorous testing needed using more intensive longitudinal measurement techniques (e.g., experience sampling method) needed to confirm the directionality (or bidirectionality) of relations among items. We were also likely underpowered in Years 5–8 to detect differences in symptom relations. Additionally, possible ethnic/racial differences (among raters and among children) in symptom inter-relations are critically neglected (Howard et al., 2017, DuPaul et al., 2020; Kang et al., 2020; Vitoratou et al., 2019). Unfortunately, our sample had insufficient numbers of different ethnic/racial groups to enable evaluation of such differences. Further, power may have been limited given the positive skew of our symptom variables and smaller sample size in teacher-reporter networks. Testing in larger samples, along with further assessment regarding the generalizability of network structure across various demographic groups and reporter characteristics (i.e., reporter age, sex, race/ethnicity; DuPaul et al., 2020) and with more objective outcomes (e.g., GPA) is needed to help shed light on more nuanced differences over time.
Inclusion of a wider array of features will also be of interest in the future; for example, the DSM-IV and DSM-5 ADHD symptom lists provide poor coverage of contemporary measures of impulsivity (Nigg, 2017), as well as of the growing interest in emotional dysregulation in ADHD (Martel, 2009; Goh et al., 2020). On a related note, we relied on DSM-IV symptoms; although these are very similar to DSM-5, DSM-5 does include additional parenethetical examples that help translate child-oriented symptoms to be more appropriate for adolescents. Given recent work suggesting this difference may contribute to higher numbers of endorsed DSM-5 symptoms in adolescence (Sibley & Kuriyan, 2016), additional research is needed to confirm findings using DSM-5 criteria. Finally, methodological limitations related to network analysis, including the lack of effect size statistics, missingness bias, confounding related to tautological overlap among symptoms, and differential variability of symptoms distorting conclusions about node centrality (e.g., Terluin, de Boer, & de Vet, 2016) require further attention to fully elucidate the role of symptom measurement in determining centrality and prognostic utility.
Supplementary Material
Acknowledgments
Support was provided by NIH R37-MH-59105 (PI: Joel T. Nigg). Sarah L. Karalunas’ time was also supported by NIH K23-MH-108656 (PI: Sarah L. Karalunas).
Footnotes
Conflicts of Interest: All authors declare that they have no conflict of interest related to this paper.
The study was initiated in 2009 before DSM-5 was completed.
As a supplemental analysis, we also constructed networks for only participants diagnosed with ADHD. Results were somewhat consistent with the overall sample with some exceptions (see Supplemental Material for detailed results). Yet, including participants exhibiting the full range of ADHD symptoms was critical for an examination of ADHD’s structure, particularly in light of dimensional models supporting ADHD as existing on a continuum (Haslam et al., 2006; Marcus & Barry, 2011).
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Barkley RA (1997). Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological bulletin, 121, 65. [DOI] [PubMed] [Google Scholar]
- Boccaletti S, Latora V, Moreno Y, Chavez M, & Hwang DU (2006). Complex networks: Structure and dynamics. Physics reports, 424, 175–308. [Google Scholar]
- Borsboom D (2017). A network theory of mental disorders. World psychiatry, 16, 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Fried EI, Epskamp S, Waldorp LJ, van Borkulo CD, van der Maas HL, & Cramer AO (2017). False alarm? A comprehensive reanalysis of “Evidence that psychopathology symptom networks have limited replicability” by Forbes, Wright, Markon, and Krueger (2017). [DOI] [PubMed]
- Bringmann LF, Elmer T, Epskamp S, Krause RW, Schoch D, Wichers M, Wigman JTW, & Snippe E (2019). What do centrality measures measure in psychological networks? Journal of Abnormal Psychology, 128, 892–903. doi: 10.1037/abn0000446 [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Vissers N, Wichers M, Geschwind N, Kuppens P, Peeters F, … & Tuerlinckx F (2013). A network approach to psychopathology: new insights into clinical longitudinal data. PloS one. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, 175, 831–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contreras A, Nieto I, Valiente C, Espinosa R, & Vazquez C (2019). The study of psychopathology from the network analysis perspective: a systematic review. Psychotherapy and Psychosomatics, 88, 71–83. doi: 10.1159/000497425 [DOI] [PubMed] [Google Scholar]
- Csardi G, & Nepusz T (2006). The igraph software package for complex network research. International Journal of Complex Systems, 1695, 1–9. [Google Scholar]
- DuPaul GJ (2020). Adult ratings of child ADHD symptoms: importance of race, role, and context. Journal of Abnormal Child Psychology, 48, 673–677. doi: 10.1007/s10802-019-00615-5 [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, Fu Q, Anastopoulos AD, Reid R, Power TJ (2020). ADHD parent and teacher symptom ratings: differential item functioning across gender, age, race, and ethnicity. Journal of Abnormal Child Psychology, 48, 679–691. doi: 10.1007/s10802-020-00618-7 [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, & Reid R (1998). ADHD Rating Scale—IV: Checklists, norms, and clinical interpretation. Guilford Press. [Google Scholar]
- Elliott H, Jones PJ, & Schmidt U (2019). Central symptoms predict posttreatment outcomes and clinical impairment in anorexia nervosa: a network analysis. Clinical Psychological Science. doi: 10.1177/2167702619865958 [DOI] [Google Scholar]
- Epskamp S, Borsboom D, & Fried EI (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50, 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD, & Borsboom D (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48, 1–18. [Google Scholar]
- Epskamp S, & Fried EI (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23, 617–634. doi: 10.1037/met0000167 [DOI] [PubMed] [Google Scholar]
- Epskamp S, Rhemtulla M, & Borsboom D (2017). Generalized network psychometrics: Combining network and latent variable models. Psychometrika, 82, 904–927. [DOI] [PubMed] [Google Scholar]
- Fair DA, Cohen AL, Dosenbach NU, Church JA, Miezin FM, Barch DM, … & Schlaggar BL (2008). The maturing architecture of the brain’s default network. Proceedings of the National Academy of Sciences, 105, 4028–4032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV (2000). Genetics of childhood disorders: XX. ADHD, part 4: Is ADHD genetically heterogeneous?. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 1455–1457. [DOI] [PubMed] [Google Scholar]
- Foygel R, & Drton M (2010). Extended Bayesian information criteria for Gaussian graphical models. In Advances in neural information processing systems (pp. 604–612). [Google Scholar]
- Fried EI, Eidhof MB, Palic S, Costantini G, Huisman-van Dijk HM, Bockting CLH, … Karstoft K (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: a cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6, 335–351. doi: 10.1177/2167702617745092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Cramer AO, Boschloo L, Schoevers RA, & Borsboom D (2017). Mental disorders as networks of problems: a review of recent insights. Social Psychiatry and Psychiatric Epidemiology, 52, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, Hastie T, & Tibshirani R (2008). Sparse inverse covariance estimation with the graphical lasso. Biostatistics, 9, 432–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R, Meltzer H, & Bailey V (1998). The strengths and difficulties questionnaire: a pilot study on the validity of the self-report version. European Child & Adolescent Psychiatry, 7, 125–130. doi: 10.1007/s007870050057 [DOI] [PubMed] [Google Scholar]
- Goh PK, Lee CA, Martel MM, Karalunas SL, & Nigg JT (2020). Subgroups of childhood ADHD based on temperament traits and cognition: concurrent and predictive validity. Journal of Abnormal Child Psychology. Advance online publication. 10.1007/s10802-020-00668-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallquist MN, Wright AG, & Molenaar PC (2019). Problems with centrality measures in psychopathology symptom networks: Why network psychometrics cannot escape psychometric theory. Multivariate behavioral research, 1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam N, Williams B, Prior M, Haslam R, Graetz B, & Sawyer M (2006). The latent structure of attention-deficit/hyperactivity disorder: a taxometric analysis. Australian and New Zealand Journal of Psychiatry, 40, 639–647. doi: 10.1080/j.1440-1614.2006.01863.x [DOI] [PubMed] [Google Scholar]
- Heeren A, Jones P, & McNally RJ (2018). Mapping network connectivity among symptoms of social anxiety and comorbid depression in people with social anxiety disorder. Journal of Affective Disorders, 228, 75–82. doi: 10.1016/j.jad.2017.12.003 [DOI] [PubMed] [Google Scholar]
- Howard LM Ehrlich AM Gamlen F & Oram S (2017). Gender-neutral mental health research is sex and gender biased. The Lancet Psychiatry, 4, 9–11. [DOI] [PubMed] [Google Scholar]
- Jones PJ, Heeren A, & McNally RJ (2017). Commentary: A network theory of mental disorders. Frontiers in psychology, 8, 1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S, Harvey EA (2020). Racial differences between black parents’ and white teachers’ perceptions of attention-deficit/hyperactivity disorder behavior. Journal of Abnormal Child Psychology, 8,661–672. doi: 10.1007/s10802-019-00600-y [DOI] [PubMed] [Google Scholar]
- Karalunas SL, Gustafsson HC, Dieckmann NF, Tipsord J, Mitchell SH, & Nigg JT (2017). Heterogeneity in development of aspects of working memory predicts longitudinal attention deficit hyperactivity disorder symptom change. Journal of abnormal psychology, 126, 774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karalunas SL, Gustafsson HC, Fair D, Musser ED, & Nigg JT (2019). Do we need an irritable subtype of ADHD? Replication and extension of a promising temperament profile approach to ADHD subtyping. Psychological Assessment, 31(2), 236–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempe D, Kleinberg J, & Tardos É (2003, August). Maximizing the spread of influence through a social network. In Proceedings of the ninth ACM SIGKDD international conference on Knowledge discovery and data mining (pp. 137–146). ACM. [Google Scholar]
- Kendler KS (2005). “A gene for…”: the nature of gene action in psychiatric disorders. American Journal of Psychiatry, 162, 1243–1252. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, … & Spencer T. (2006). The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. American Journal of psychiatry, 163, 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, & Willcutt E (2005). Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry, 62, 896–902. [DOI] [PubMed] [Google Scholar]
- Lahey BB, & Willcutt EG (2010). Predictive validity of a continuous alternative to nominal subtypes of attention-deficit/hyperactivity disorder for DSM–V. Journal of Clinical Child & Adolescent Psychology, 39, 761–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus DK, & Barry TD (2011). Does attention-deficit/hyperactivity disorder have a dimensional latent structure? A taxometric analysis. Journal of Abnormal Psychology, 120, 427–442. doi: 10.1037/a0021405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM (2009). Research review: A new perspective on attention-deficit/hyperactivity disorder: Emotion dysregulation and trait models. Journal of Child Psychology and Psychiatry, 50(9), 1042–1051. [DOI] [PubMed] [Google Scholar]
- Martel MM, Levinson CA, Langer JK, & Nigg JT (2016). A network analysis of developmental change in ADHD symptom structure from preschool to adulthood. Clinical Psychological Science, 4, 988–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Markon K, & Smith GT (2017). Research review: Multi-informant integration in child and adolescent psychopathology diagnosis. Journal of Child Psychology and Psychiatry, 58, 116–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Von Eye A, & Nigg J (2012). Developmental differences in structure of attention-deficit/hyperactivity disorder (ADHD) between childhood and adulthood. International Journal of Behavioral Development, 36, 279–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ (2016). Can network analysis transform psychopathology? Behaviour Research and Therapy, 86, 95–104. doi: 10.1016/j.brat.2016.06.006 [DOI] [PubMed] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GW, Wang L, Deserno MK, & Borsboom D (2015). Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science, 3, 836–849. [Google Scholar]
- Mõttus R, & Allerhand M (2017). Why do traits come together? The underlying trait and network approaches. SAGE handbook of personality and individual differences, 1, 1–22. [Google Scholar]
- Murray AL, Booth T, Ribeaud D, & Eisner M (2018). Disagreeing about development: an analysis of parent-teacher agreement in ADHD symptom trajectories across the elementary school years. International Journal of Methods in Psychiatric Research, 27, e1723. 10.1002/mpr.1723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musser ED, Karalunas SL, Dieckmann N, Peris TS, & Nigg JT (2016). Attention-deficit/hyperactivity disorder developmental trajectories related to parental expressed emotion. Journal of abnormal psychology, 125, 182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narad ME, Garner AA, Peugh JL, Tamm L, Antonini TN, Kingery KM, … Epstein JN (2015). Parent-teacher agreement on ADHD symptoms across development. Psychological Assessment, 27, 239–248. doi: 10.1037/a0037864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT (2017). Annual Research Review: On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry, 58(4), 361–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, & Watkins ER (2011). A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6, 589–609. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Levinson C, & Calebs B (2018). A network analysis of eating disorder symptoms and characteristics in an inpatient sample. Psychiatry research, 262, 270–281. [DOI] [PubMed] [Google Scholar]
- Olson SL Developmental perspectives. In: Sandberg S, editor. Hyperactivity and attention disorders of childhood: Cambridge monographs in child and adolescent psychopathology. 2nd ed.Cambridge, UK: Cambridge University Press; 2002. pp. 149–183. [Google Scholar]
- Polanczyk G, De Lima MS, Horta BL, Biederman J, & Rohde LA (2007). The worldwide prevalence of ADHD: a systematic review and metaregression analysis. American journal of psychiatry, 164, 942–948. [DOI] [PubMed] [Google Scholar]
- Preszler J, Burns GL, Becker SP, & Servera M (2020). Multisource longitudinal Network and latent variable model analyses of ADHD symptoms in children. Journal of Clinical Child & Adolescent Psychology, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puig-Antich J, Ryan N (1986). Kiddie Schedule for Affective Disorders and Schizophrenia, Present State Version. Pittsburgh, PA: Western Psychiatric Institute and Clinic. [Google Scholar]
- Reichardt J, & Bornholdt S (2006). Statistical mechanics of community detection. Physical Review E, 74, 016110. doi: 10.1103/PhysRevE.74.016110 [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, Millner AJ, & McNally RJ (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125, 747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodebaugh TL, Tonge NA, Piccirillo ML, Fried E, Horenstein A, Morrison AS, … & Blanco C (2018). Does centrality in a cross-sectional network suggest intervention targets for social anxiety disorder? Journal of consulting and clinical psychology, 86, 831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruzzano L, Borsboom D, & Geurts HM (2015). Repetitive behaviors in autism and obsessive–compulsive disorder: New perspectives from a network analysis. Journal of autism and developmental disorders, 45, 192–202. [DOI] [PubMed] [Google Scholar]
- Santos HP Jr, Kossakowski JJ, Schwartz TA, Beeber L, & Fried EI (2018). Longitudinal network structure of depression symptoms and self-efficacy in low-income mothers. PloS one, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw P, Stringaris A, Nigg J, & Leibenluft E (2014). Emotion dysregulation in attention deficit hyperactivity disorder. American Journal of Psychiatry, 171, 276–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Kuriyan AB (2016). DSM-5 changes enhance parent identification of symptoms in adolescents with ADHD. Psychiatry Research, 242,180–185. DOI: 10.1016/j.psychres.2016.05.036. [DOI] [PubMed] [Google Scholar]
- Silk TJ, Malpas CB, Beare R, Efron D, Anderson V, Hazell P, … Sciberras E (2019). A network analysis approach to ADHD symptoms: more than the sum of its parts. PLoS ONE, 14, e0211053. doi: 10.1371/journal.pone.0211053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terluin B, De Boer MR, & De Vet HC (2016). Differences in connection strength between mental symptoms might be explained by differences in variance: Reanalysis of network data did not confirm staging. PloS ONE, 11, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A, Cooper M, Eyre O, & Langley K (2013). Practitioner review: what have we learnt about the causes of ADHD?.Journal of Child Psychology and Psychiatry, 54, 3–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Roy B, Veenstra M, & Clench-Aas J (2008). Construct validity of the five-factor strengths and difficulties questionnaire (SDQ) in pre-, early, and late adolescence. The Journal of Child Psychology and Psychiatry, 49, 1304–1312. doi: 10.1111/j.1469-7610.2008.01942.x [DOI] [PubMed] [Google Scholar]
- Van Borkulo CD (2015). Network comparison test: permutation-based test of differences in strength of networks.
- Van Borkulo CD, Boschloo L, Kossakowski J, Tio P, Schoevers RA, Borsboom D, & Waldorp LJ (2017). Comparing network structures on three aspects: A permutation test. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Vitoratou S, Garcia-Rosales A, Banaschewski T, Sonuga-Barke E, Buitelaar J, Oades RD, Rothenberger A, Steinhausen HC, Taylor E, Faraone SV, & Chen W (2019). Is the endorsement of the attention deficit hyperactivity disorder symptom criteria ratings influenced by informant assessment, gender, age, and co-occurring disorders? A measurement invariance study. International Journal of Methods in Psychiatric Research, 28, e1794. doi: 10.1002/mpr.1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, … & Lahey BB (2012). Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. Journal of abnormal psychology, 121, 991–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


