Abstract
Several antibiotics demonstrate both antibacterial and anti-inflammatory/immunomodulatory activities and are used to treat inflammatory pulmonary disorders. Lefamulin is a pleuromutilin antibiotic approved to treat community-acquired bacterial pneumonia (CABP). This study evaluated lefamulin anti-inflammatory effects in vivo and in vitro in a lipopolysaccharide-induced lung neutrophilia model in which mouse airways were challenged with intranasal lipopolysaccharide. Lefamulin and comparators azithromycin and dexamethasone were administered 30min before lipopolysaccharide challenge; neutrophil infiltration into BALF and inflammatory mediator induction in lung homogenates were measured 4h postchallenge. Single subcutaneous lefamulin doses (10‒140mg/kg) resulted in dose-dependent reductions of BALF neutrophil cell counts, comparable to or more potent than subcutaneous azithromycin (10‒100mg/kg) and oral/intraperitoneal dexamethasone (0.5/1mg/kg). Lipopolysaccharide-induced pro-inflammatory cytokine (TNF-α, IL-6, IL-1β, and GM-CSF), chemokine (CXCL-1, CXCL-2, and CCL-2), and MMP-9 levels were significantly and dose-dependently reduced in mouse lung tissue with lefamulin; effects were comparable to or more potent than with dexamethasone or azithromycin. Pharmacokinetic analyses confirmed exposure-equivalence of 30mg/kg subcutaneous lefamulin in mice to a single clinical lefamulin dose to treat CABP in humans (150mg intravenous/600mg oral). In vitro, neither lefamulin nor azithromycin had any relevant influence on lipopolysaccharide-induced cytokine/chemokine levels in J774.2 mouse macrophage or human peripheral blood mononuclear cell supernatants, nor were any effects observed on IL-8‒induced human neutrophil chemotaxis. These in vitro results suggest that impediment of neutrophil infiltration by lefamulin in vivo may not occur through direct interaction with macrophages or neutrophilic chemotaxis. This is the first study to demonstrate inhibition of neutrophilic lung infiltration and reduction of pro-inflammatory cytokine/chemokine concentrations by clinically relevant lefamulin doses. This anti-inflammatory activity may be beneficial in patients with acute respiratory distress syndrome, cystic fibrosis, or severe inflammation-mediated lung injury, similar to glucocorticoid (eg, dexamethasone) activity. Future lefamulin anti-inflammatory/immunomodulatory activity studies are warranted to further elucidate mechanism of action and evaluate clinical implications.
Introduction
Anti-inflammatory and immunomodulatory activities have been observed with various antibiotics, including macrolides (eg, azithromycin), tetracyclines (eg, minocycline), and sulfonamides (eg, trimethoprim-sulfamethoxazole). This has resulted in their use to treat a variety of disorders, including chronic inflammatory conditions (eg, pulmonary and skin disorders), gastrointestinal dysmotility, cancer, and rheumatoid arthritis [1]. In the context of chronic inflammatory pulmonary disorders, substantial evidence supports the use of macrolides to reduce the number of exacerbations and risk of mortality [1]. In cystic fibrosis with Pseudomonas aeruginosa infection, long-term azithromycin therapy reduces exacerbations by inhibiting virulence factors in P. aeruginosa [2–5]. Macrolides have also been used in non–cystic fibrosis bronchiectasis, diffuse panbronchiolitis, chronic obstructive pulmonary disease, chronic rhinosinusitis, and asthma [1, 2, 6]. In these contexts, the anti-inflammatory effects of macrolides are attributed to reductions in levels of interleukin (IL)-8, neutrophils, neutrophil elastase, and complement 5a and in reduced lymphocyte proliferation.
Inflammation is also observed in acute lung injury and its most severe form, acute respiratory distress syndrome (ARDS), which cause inflammatory damage to the alveolar capillary membrane and excessive uncontrolled pulmonary inflammation [7]. Acute lung injury and ARDS complicate pneumonia and contribute substantially to morbidity and mortality in these patients [7–9]. Systemic inflammation associated with ARDS is commonly treated for up to 3 weeks with corticosteroids such as methylprednisolone or dexamethasone [10]. Macrolide treatment has also been shown to improve clinical outcomes in patients with ARDS, accompanied by evidence that these effects resulted from the immunomodulatory, not the antimicrobial, effects of the macrolides [5, 11]. Lipopolysaccharide (LPS) administration can induce pathologic and biological changes similar to those seen in ARDS, including neutrophilic infiltration and increased intrapulmonary cytokines, which have been extensively studied in experimental models of acute lung injury [12]. Further, research has suggested that increased neutrophil recruitment to the lungs may contribute to tissue damage, particularly in chronic diseases [13].
Pleuromutilin antibiotics inhibit bacterial protein synthesis by binding to the peptidyl transferase center of the 50S ribosomal subunit [14], and lefamulin is the first pleuromutilin antibiotic approved for intravenous (IV) and oral use in humans [15]. Lefamulin has demonstrated potent in vitro activity against the pathogens that most commonly cause community-acquired bacterial pneumonia (CABP) [16–19] and, based on the results of two phase 3 clinical trials [20, 21], is approved in the United States and has received a positive opinion from the Committee for Medicinal Products for Human Use in the European Union for the treatment of adults with CABP [15]. The current investigations evaluated the anti-inflammatory effects of lefamulin in LPS-induced lung neutrophilia using in vivo and in vitro models. The antibiotic azithromycin and the glucocorticoid dexamethasone were included as comparators because of their known anti-inflammatory properties [1, 10].
Materials and methods
Pharmacokinetics of lefamulin and azithromycin treatment
Pharmacokinetic parameters were evaluated as previously described [22]. Briefly, female BALB/c mice (weight ~20 g, n = 3/time point; Charles River Deutschland GmbH, Sulzfeld, Germany) received a single subcutaneous (SC) injection of 35 mg/kg lefamulin (dissolved in 0.9% saline [Sigma-Aldrich Chemie GmbH]) or 35 mg/kg azithromycin (Pfizer Inc, New York, NY, USA; solubilized in 10% dimethyl sulfoxide [DMSO; Sigma-Aldrich Chemie GmbH]). Plasma and bronchoalveolar lavage fluid (BALF) samples were collected at 0.08, 0.25, 0.5, 0.75, 1.5, 3, 6, and 24 hours after lefamulin or azithromycin administration. Plasma samples were analyzed by liquid chromatography with triple quadrupole mass spectrometry (Q Exactive Plus; Thermo Fisher Scientific). Lefamulin and azithromycin concentrations in the epithelial lining fluid (ELF) were calculated from the BALF-to-plasma urea concentration ratio for samples collected at the same time point (BioAssay QuantiChromTM; Thermo Fisher Scientific). These experiments were conducted in Vienna, Austria, according to European Union directive 2010/63/EU and national legislation (GZ:461104/2018/13) regulating the use of laboratory animals in scientific research.
Measurement of LPS-induced neutrophils and cytokine/chemokine levels in murine lungs
Animals
These experiments were conducted in Zagreb, Croatia, according to European Union directive 2010/63/EU and national legislation (Official Gazette 55/13) regulating use of laboratory animals in scientific research, with oversight from an Institutional Committee on Animal Research Ethics (CARE-Zg), and all efforts were made to minimize suffering. Six-week-old male BALB/c mice (Charles River, Calco, Italy) were singly housed in a temperature-controlled (22°C±2°C) environment with a 12:12-hour light:dark cycle and free access to food and water. Mice were given ≥7 days for acclimation before all procedures. The study did not control for additional potential confounders. One day before the start of experimental procedures, all animals were randomized into 6 groups (n = 8/group). Animal group assignment was not blinded.
Reagents
LPS lyophilized powder (2 mg; Sigma-Aldrich Chemie GmbH, Munich, Germany) from Escherichia coli (O111:B4) was dissolved in 10 mL cold saline (0.9%; Pliva, Zagreb, Croatia), vortexed, and further diluted by mixing 2 mL of this solution with 2 mL saline to reach a final concentration of 5 μg LPS/50 μL saline. Dexamethasone (Sigma-Aldrich Chemie GmbH) was dissolved in carboxymethylcellulose (0.5% in water; Sigma-Aldrich Chemie GmbH) and dosed in a volume of 10 mL/kg per mouse. Lefamulin (BC-3781.Ac; Nabriva Therapeutics, Vienna, Austria) was weighed considering the “as is” purity of 89.3% and dissolved in 0.9% saline. For the lefamulin dose groups (free base: 10, 30, 35, 70, 100, and 140 mg/kg), corresponding lefamulin concentrations were 1.1, 3.4, 3.9, 7.8, 11.2, and 15.7 mg/mL (free base: 1.0, 3.0, 3.5, 7.0, 10.0, and 14.0 mg/mL), respectively. Azithromycin (BC-1024; Nabriva Therapeutics) was weighed using a correction factor of 1.08 and dissolved in 0.5% methylcellulose with 1.25 μL of 1 M citric acid (Alfa Aesar, Ward Hill, MA, USA) for each milligram of azithromycin. For the azithromycin dose groups (free base: 10, 30, and 100 mg/kg), corresponding azithromycin concentrations were 1.1, 3.2, and 10.8 mg/mL (free base: 1.0, 3.0, and 10.0 mg/mL). Lefamulin and azithromycin were each dosed in a volume of 10 mL/kg per mouse. Ketamine hydrochloride (Narketan 10) was acquired from Vetoquinol (Bern, Switzerland), and xylazine hydrochloride (Rompun, 2%) was acquired from Bayer (Leverkusen, Germany).
Induction of lung neutrophilia and treatments
Before the LPS challenge, dexamethasone (1 mg/kg intraperitoneal [IP] at 30 minutes before challenge or 0.5 mg/kg oral at 60 minutes before challenge) was administered; vehicle (0.9% saline), lefamulin, and azithromycin were administered SC. The dexamethasone doses and administration routes used (0.5 mg/kg oral or 1 mg/kg IP) produce reproducible effects in the LPS-induced neutrophilia model [23, 24]. Immediately before the LPS challenge, mice were anesthetized via IP injection of ketamine (2 mg/mouse) and xylazine (0.08 mg/mouse). To induce pulmonary neutrophilia, mice in the control group received intranasal (IN) 50 μL saline, and all other animals received 5 μg LPS/50 μL saline IN per mouse.
Bronchoalveolar lavage fluid collection and neutrophil analysis
Approximately 4 hours after LPS administration, mice were euthanized by an overdose of IP ketamine (200 mg/kg) and xylazine (16 mg/kg). Tracheostomy was performed, and a Buster cat catheter (1.0 × 130 mm; Kruuse, Langeskov, Denmark), shortened to 3 cm, was clamped into the trachea. The lungs were washed 3 times with cold phosphate-buffered saline (PBS; Sigma-Aldrich Chemie GmbH) in a total volume of 1 mL (0.4, 0.3, and 0.3 mL). The collected BALF samples were centrifuged (1303×g, 5 min, 4°C), and resulting cell pellets were each resuspended in 600 μL PBS. Samples were immediately analyzed for total and differential neutrophil cell counts via automated hematology analyzer (XT-2000iV; Sysmex, Kobe, Japan).
Lung tissue sampling
After bronchoalveolar lavage, lungs were removed, weighed, snap frozen, and stored at −80°C until analysis. To homogenize the tissue, the frozen lungs were thawed and placed in Precellys CK28 Hard Tissue tubes (BERTIN Instruments, Montigny-le-Bretonneux, France) in 1 mL PBS (Gibco, Life Technologies, Paisley, UK) supplemented with protease inhibitors (Halt™ Protease Inhibitor Cocktail [100×]; Thermo Fisher Scientific, Rockford, IL, USA). A Precellys homogenizer (BERTIN Instruments) was used, shaking at 6800 rpm for three 30-second pulses separated by 15-second pauses. After homogenization, samples were centrifuged at 18,000×g for 10 minutes at 4°C, and the supernatants were collected for analysis.
Measurement of TNF-α, IL-6, GM-CSF, CXCL-1, CXCL-2, and CCL-2 in lung tissue
Concentrations of tumor necrosis factor (TNF)-α, IL-6, granulocyte-macrophage colony-stimulating factor (GM-CSF), chemokine (C-X-C motif) ligand (CXCL)-1, CXCL-2, and chemokine (C-C motif) ligand (CCL)-2 in mouse lung homogenates were analyzed with the Mouse Premixed Multi-Analyte Kit (R&D Systems, Minneapolis, MN, USA) per the manufacturer’s protocol and using a Luminex 200 System (Luminex Corporation, Austin, TX, USA). Cytokine and chemokine concentrations were determined from blank-corrected median fluorescence intensity of each sample via xPONENT® software (Luminex Corporation), interpolating from standard curves generated with a 5-parameter logistic curve-fit.
Measurement of MMP-9 and IL-1β in lung tissue
Mouse Total MMP (matrix metalloprotease)-9 and IL-1β/IL-1F2 DuoSet ELISA (enzyme-linked immunosorbent assay) kits (R&D Systems) were used to measure concentrations of MMP-9 and IL-1β, respectively, in lung homogenates per the manufacturer’s protocols. Absorbance at 450 nm was measured using the SpectraMax i3 (Molecular Devices, San Jose, CA, USA). Concentrations of MMP-9 and IL-1β in samples were determined by interpolation from standard curves.
Chemotaxis of IL-8–activated human neutrophils
Neutrophil isolation from human blood
Buffy coat (blood sample fraction comprising white blood cells and platelets) from whole blood was obtained from a healthy adult volunteer at the Croatian Institute of Transfusion Medicine (CITM; Zagreb, Croatia). The CITM ethics committee approved the blood collection process, and the volunteer provided written informed consent prior to blood collection. Neutrophils were isolated from the buffy coat, an aliquot of which was used for cell counting via hematologic analyzer (X500i; Sysmex). The remainder of the buffy coat (7 mL) was diluted with 5 mL of 3% dextran (GE Healthcare, Chicago, IL, USA) and 1.5 mL of 0.18% glucose in PBS (Sigma-Aldrich Chemie GmbH). The diluted buffy coat was drawn into sterile 50-mL syringes and incubated for 30 minutes at RT. Following incubation, the upper layer of leukocyte-rich plasma (35 mL) was decanted into a new sterile 50-mL conical centrifuge tube, carefully layered onto 15 mL of Lymphoprep (Axis-Shield Diagnostics, Ltd., Dundee, UK) and centrifuged at 400×g (brake turned off) for 35 minutes at RT. The supernatant and mononuclear ring were discarded, and the pellet was resuspended in 10 mL of cold sterile MilliQ water. Erythrocyte lysis was stopped by adding 10 mL of 1.8% saline. Following lysis, neutrophils were centrifuged at 300×g for 5 minutes at RT, supernatants were removed, and neutrophils were resuspended in freshly prepared migration medium (Roswell Park Memorial Institute [RPMI] 1640 medium [Thermo Fisher Scientific] supplemented with 0.05% BSA-FAF [bovine serum albumin-fatty acid free; Sigma-Aldrich Chemie GmbH] and 0.2 μm filtered). Resuspended neutrophils were counted via Sysmex X500i hematologic analyzer. Cell concentrations were adjusted to 5.55 × 106 neutrophils/mL.
Preparation of compounds and neutrophil treatment
All test compounds were reconstituted in DMSO (Sigma-Aldrich Chemie GmbH) to 100-mM stock concentrations, taking into consideration and correcting for salt and purity. A 30-mM stock solution of reference compound Sch527123 (MedChemExpress, Monmouth Junction, NJ, USA) was diluted to 10 mM with DMSO.
Using DMSO as the diluent, 7 consecutive 3.16-fold dilutions were prepared from stock solutions for all compounds. Final working dilutions for all compounds were then prepared by further diluting the compounds 100-fold in migration medium (2 μL of compound was transferred to 198 μL of medium). DMSO was used as vehicle. Lefamulin and azithromycin were tested at concentrations of 0.03, 0.1, 0.3, 1, 3, 10, 30, and 100 μM. The reference compound was tested at concentrations of 0.003, 0.01, 0.03, 0.1, 0.3, 1, 3, and 10 μM. All compounds were tested in triplicate, and the final DMSO concentration was 0.1% per well.
To each well of a 96-well U-bottom plate, 180 μL of resuspended neutrophils (5.55 × 106 neutrophils/mL) was added. Test and reference compound working solutions were then added (20 μL/well) for a 10-fold dilution to final testing concentrations. Compounds and cells were mixed by gentle pipetting, and the plate was pre-incubated for 30 minutes at RT with gentle mixing by pipetting.
Chemotaxis assay and cytotoxicity evaluation
A 96-well transwell plate insert (Corning Life Sciences, Tewksbury, MA, USA) with donor (upper) wells was removed, and the receiver (lower) wells were filled with 180 μL of 22.22 ng/mL rhIL-8 solution in migration medium. Negative control wells received 180 μL of migration medium alone. To all wells, 20 μL of compound working solutions or DMSO vehicle was added. Once pre-incubation of cells with compounds was complete, the transwell inserts were carefully placed on the receiver plate, with caution to avoid air bubble formation, which could prevent cell migration. To the upper wells, 75 μL of cell suspension (375,000 cells/well) was added, taking care not to tear the membrane with pipette tips.
The plate was incubated in a CO2 incubator (37°C, 5% CO2, 95% humidity) for 1 hour. After incubation, the number of cells that migrated to the lower wells was quantified by removing the Transwell insert and adding 200 μL of CellTiter Glo reagent (CellTiter-Glo Luminescent Cell Viability Assay, Promega, Madison, WI, USA) to each lower well to quantify the amount of adenosine triphosphate (ATP) present, signaling the presence of metabolically active cells. The plate was incubated for 10 minutes in the dark at RT, followed by transferring 150 μL of solution into wells of a white 96-well plate (Lumitrac 200; Greiner Bio-One International GmbH, Kremsmunster, Austria). Luminescence was measured by use of EnVision 2104 Multilabel Plate Reader (PerkinElmer, Waltham, MA, USA), with exposition time of 0.1 seconds.
To evaluate cytotoxicity of human neutrophils, cells that were not used for the chemotaxis assay were incubated with compounds for an additional hour in the CO2 incubator (37°C, 5% CO2, 95% humidity), after which 125 μL of CellTiter Glo reagent was added to each well, and the plate was incubated for 10 minutes in the dark at RT. The solution (150 μL) was transferred into wells of a white 96-well plate (Lumitrac 200), and luminescence was measured by use of EnVision 2104 Multilabel Plate Reader, with an exposition time of 0.1 seconds.
Statistical analyses
The pharmacokinetic profiles of lefamulin and azithromycin were analyzed by the sparse sampling noncompartmental method (Phoenix WinNonlin 6, Certera, Princeton, NJ, USA) based on the nominal time points. Area under the curve (AUC) values were determined using the linear trapezoidal method.
For the lung neutrophilia analyses, statistical analyses were performed using GraphPad Prism (versions 5.04 and 8.1.1; GraphPad Software, Inc., La Jolla, CA, USA). Differences between treated versus vehicle groups were determined using the Mann-Whitney test and were considered statistically significant when P<0.05. Outliers in the analysis of cytokine and chemokine concentrations were identified using the Grubbs test. No criteria were set for inclusion/exclusion of animals during the experiment or data points during the analysis.
For the chemotaxis and cytotoxicity evaluations, average relative light unit values were calculated from all untreated vehicle samples and, for each sample, percentage of vehicle value was calculated. The tested compound was considered cytotoxic if reduction from untreated vehicle was ≥20%.
Additional Methods can be found in S1 Appendix.
Results
Pharmacokinetic analysis of lefamulin in mice
The pharmacokinetics of a single SC injection of 35 mg/kg lefamulin or azithromycin was assessed in mice. Plasma AUC from time 0 to 24 hours (AUC0-24h) values after 35 mg/kg SC lefamulin or azithromycin were 6.25±0.93 or 11.6±1.37 μg∙h/mL, respectively (Table 1). In terms of distribution from plasma to ELF in mice, both lefamulin and azithromycin showed rapid penetration into the lung compartment following a single SC dose, with comparable times to maximum concentration for both matrices. For each drug, the AUC ratio for ELF to plasma was approximately 2-fold.
Table 1. Pharmacokinetic profile in plasma and epithelial lining fluid of mice following a single subcutaneous dose of lefamulin or azithromycin 35 mg/kg.
| Matrix | tmax (h), | Cmax (μg/mL), | AUC0-24h (μg∙h/mL), | AUC0-24h/Dose (μg∙h/mL)/(mg/kg), | |
|---|---|---|---|---|---|
| mean | mean±SEM | mean±SEM | mean | ||
| Lefamulin | Plasma | 0.50 | 1.33±0.18 | 6.25±0.93 | 0.18 |
| ELF | 0.50 | 2.16±0.50 | 12.6±1.17 | 0.36 | |
| Azithromycin | Plasma | 0.08 | 2.33±0.83 | 11.6±1.37 | 0.33 |
| ELF | 0.25 | 2.35±1.45 | 26.7±5.78 | 0.76 |
AUC0-24h = area under the curve from time 0 to 24 hours; Cmax = maximum observed plasma concentration; ELF = epithelial lining fluid; tmax = time of maximum observed concentration.
Effects of lefamulin on LPS-induced lung neutrophilia in mice
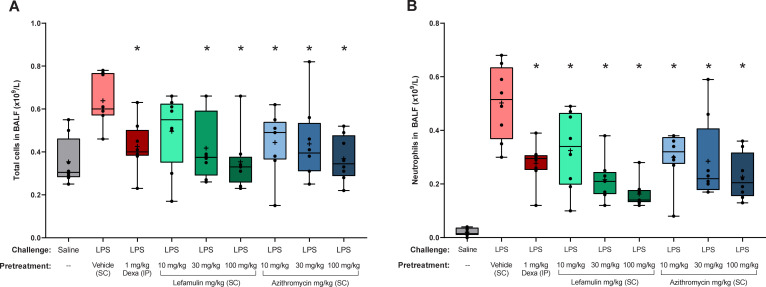
In the in vivo mouse lung neutrophilia model, lefamulin treatment at doses of 10, 30, and 100 mg/kg SC at 30 minutes before intranasal LPS challenge (30 minutes pretreatment) was associated with a dose-dependent reduction in total cell and neutrophil recruitment to the lungs (measured in BALF) at 4 hours postchallenge compared with the vehicle control group (no treatment; Fig 1). These reductions were comparable to those observed following treatment with 1 mg/kg IP dexamethasone, with a tendency toward more potent inhibition of total cell counts and neutrophil cell counts at the highest lefamulin dose of 100 mg/kg. Pretreatment with azithromycin at doses of 10, 30, and 100 mg/kg SC demonstrated significant dose-dependent reductions in total cell and neutrophil counts as well, although the effects on neutrophil counts in BALF were more pronounced with the 30- and 100-mg/kg lefamulin doses. Similar results were observed in an independent experiment using higher doses of lefamulin and azithromycin (35, 70, and 140 mg/kg; S1 Fig in S1 Appendix).
Fig 1.
(A) Total and (B) neutrophil cell counts in BALF after LPS induction. BALF, bronchoalveolar lavage fluid; Dexa, dexamethasone; IP, intraperitoneal; LPS, lipopolysaccharide; SC, subcutaneous. Box and whisker plots show 25% percentile, median, and 75% percentile in box, with minimum and maximum values shown with whiskers. Means are shown with “+” and raw data points with black circles. *P<0.05 vs LPS/vehicle via Mann-Whitney test.
Effects of lefamulin on cytokine production in vivo and in vitro
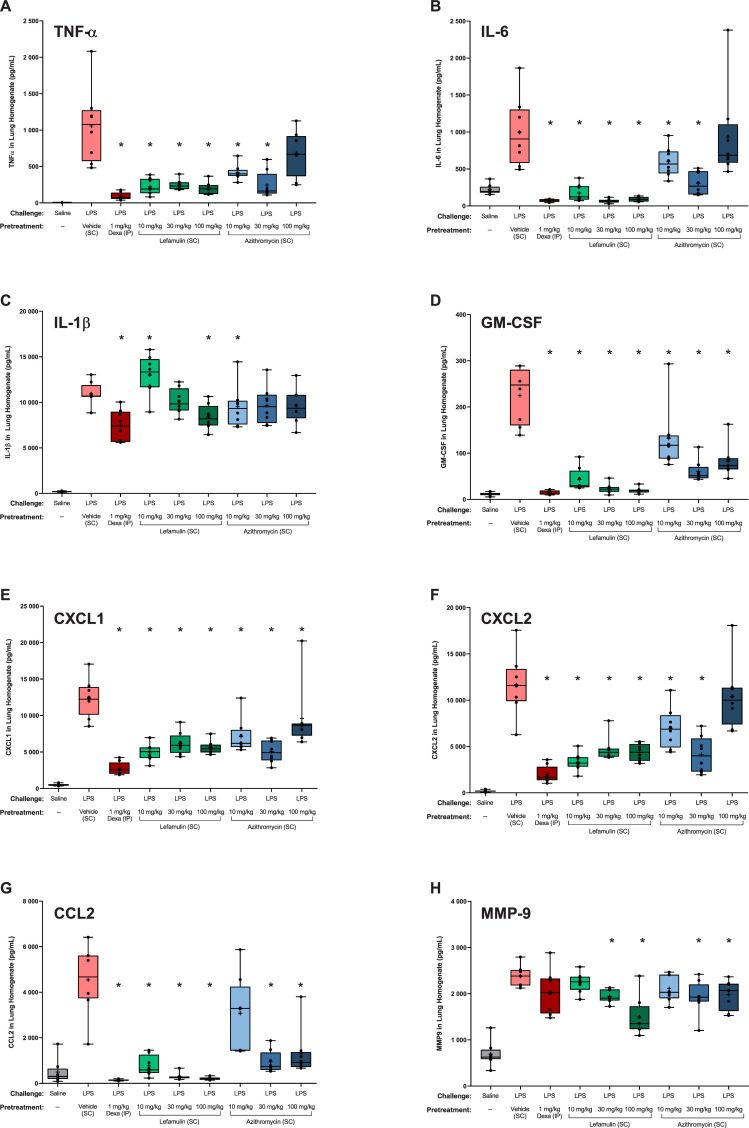
To assess the effects of lefamulin, azithromycin, and dexamethasone on LPS-induced pro-inflammatory cytokines, chemokines, and MMP-9, lungs from the mouse model of neutrophilia were homogenized and evaluated via Luminex immunoassay and ELISA. As observed with dexamethasone (1 mg/kg IP), lefamulin (10, 30, and 100 mg/kg SC) was generally associated with significantly reduced levels of all cytokines and chemokines assessed, as well as of MMP-9 (Fig 2). TNF-α and IL-6 concentrations were significantly reduced at all lefamulin doses tested compared with vehicle control. The reductions observed with lefamulin were similar to those observed with 1 mg/kg IP dexamethasone. In contrast, azithromycin was associated with significant reductions in TNF-α concentrations at 10 and 30 mg/kg, with no significant effect observed with 100 mg/kg, and IL-6 levels were reduced to a lesser extent with azithromycin than with lefamulin or dexamethasone.
Fig 2. LPS-induced cytokines and chemokines in mouse lung homogenate.
CCL, chemokine (C-C motif) ligand; CXCL, chemokine (C-X-C motif) ligand; Dexa, dexamethasone; GM-CSF, granulocyte-macrophage colony-stimulating factor; IL, interleukin; IP, intraperitoneal; LPS, lipopolysaccharide; MMP, matrix metalloprotease; SC, subcutaneous; TNF, tumor necrosis factor. Box and whisker plots show 25% percentile, median, and 75% percentile in box, with minimum and maximum values shown with whiskers. Means are shown with “+” and raw data points with black circles. *P<0.05 vs LPS/vehicle via Mann-Whitney test.
A dose-dependent effect on IL-1β concentrations was also observed with lefamulin; however, significant inhibition of IL-1β was observed only with the highest lefamulin dose (100 mg/kg), similar to that observed with dexamethasone 1 mg/kg. In contrast, azithromycin reduced IL-1β concentrations at all doses, although only the lowest dose showed a significant reduction similar to that of 100 mg/kg lefamulin. Significant reductions in MMP-9 levels were observed with 30 and 100 mg/kg lefamulin, with effects similar to those seen with dexamethasone, whereas reductions in MMP-9 levels with azithromycin (all doses) were not as pronounced as with lefamulin. Significant reductions in chemokines and GM-CSF were also observed with all lefamulin doses and dexamethasone, whereas reductions with azithromycin were significant but not as pronounced as those with lefamulin or dexamethasone.
To investigate further the mechanism of inhibition of LPS-induced pulmonary neutrophilia by lefamulin and azithromycin, cell viability and LPS-induced production of cytokines, chemokines, and MMP-9 were assessed in vitro in human neutrophils, J774.2 mouse macrophages, and human peripheral blood mononuclear cells (PBMCs). Cells were pretreated with lefamulin and azithromycin similarly as described for the in vivo experiment. In J774.2 cells, cell viability was reduced at 30 μM (15.2 μg/mL free base) and 100 μM (50.8 μg/mL free base) lefamulin and at 100 μM (74.9 μg/mL) azithromycin (S1 Table in S1 Appendix). In PBMCs, cell viability was reduced at 100 μM lefamulin, and no cytotoxic effects were observed with azithromycin ≤100 μM. Based on these results, data in J774.2 cells are not shown for the 30- and 100-μM doses of lefamulin and azithromycin, and data in PBMCs are not shown for 100 μM lefamulin or azithromycin.
Although treatment with dexamethasone resulted in dose-dependent reductions of TNF-α, IL-6, and IL-1β in J774.2 mouse macrophages (S2 Fig in S1 Appendix) and of all measured cytokines and chemokines in human PBMCs (S3 Fig in S1 Appendix), little to no reduction in levels of the measured LPS-induced cytokines, chemokines, or MMP-9 was observed in supernatants from either cell type at the concentrations of lefamulin or azithromycin tested. In J774.2 macrophages, however, IL-6 and IL-1β levels showed a trend toward reduction with lefamulin (S2 Fig in S1 Appendix).
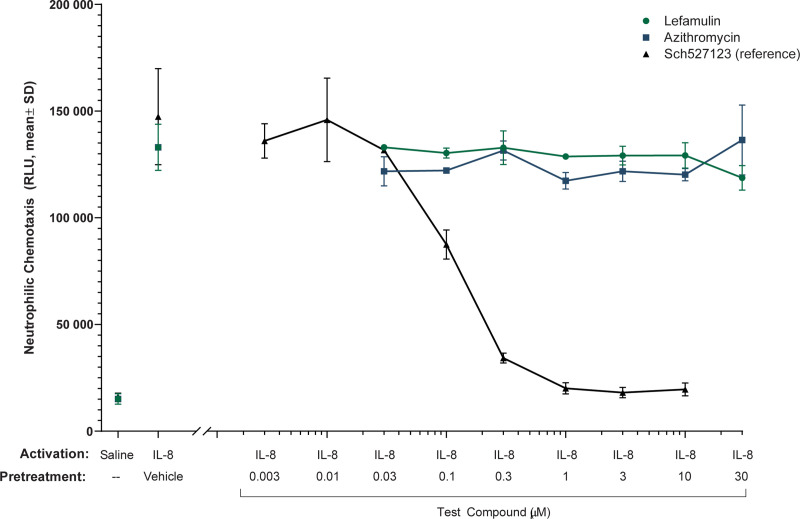
Effects of lefamulin and azithromycin on neutrophilic chemotaxis
The effects of lefamulin and azithromycin on IL-8–induced chemotaxis of human neutrophils were also assessed. Treatment with the reference compound Sch527123 (an antagonist of chemokine [C-X-C motif] ligand [CXCL]-1 and CXCL-2) resulted in dose-dependent inhibition neutrophilic chemotaxis (Fig 3), whereas treatment with 0.03 to 30 μM lefamulin (0.02‒15.2 μg/mL free base) or azithromycin (0.02‒22.5 μg/mL) had no effect on IL-8–induced chemotaxis of human neutrophils. In neutrophils, cell viability was reduced at 100 μM (50.8 μg/mL free base) lefamulin to 86% of vehicle control (S1 Table in S1 Appendix), whereas no cytotoxic effects were observed at 30 μM lefamulin or azithromycin ≤100 μM. Based on these results, data in neutrophils are not shown for 100 μM lefamulin or azithromycin.
Fig 3. Chemotaxis of IL-8–activated human neutrophils with lefamulin, azithromycin, and Sch527123 (reference compound).
IL, interleukin; RLU, relative light unit; SD, standard deviation.
Discussion
Previous research has demonstrated anti-inflammatory and immunomodulatory effects with antibiotics, including macrolides, tetracyclines, and fluoroquinolones, but for many, the higher dose and/or longer duration of antibiotic treatment that may be required for anti-inflammatory effects (compared with those required for anti-infective effects) must be balanced with both adverse effects and the risk of emerging microbial resistance [1]. In the context of acute infection, the timing of anti-inflammatory treatment may also need to be considered, as a required anti-pathogen immune response can be hindered by an anti-inflammatory treatment effect [25]. Therefore, an antibiotic able to exert anti-inflammatory effects at anti-infective doses would be of interest, particularly in chronic inflammatory pulmonary disorders or ARDS, in which neutrophilic lung infiltration is a key characteristic [7].
To our knowledge, these analyses are the first to investigate the anti-inflammatory activity of the pleuromutilin antibiotic lefamulin. In a mouse model of lung neutrophilia, pretreatment with lefamulin at doses of 10, 30, and 100 mg/kg SC was associated with almost complete reduction in LPS-induced recruitment of total cells and neutrophils to the lungs at 4 hours postchallenge compared with the vehicle control group (no treatment). Similar effects were observed with the same SC doses of the macrolide antibiotic azithromycin (although the exposures associated with these doses of azithromycin exceed those of the corresponding human clinical doses), as well as with 1 mg/kg IP dexamethasone, a known anti-inflammatory glucocorticoid. Levels of cytokines, chemokines, and MMP-9 in lung homogenates were reduced following pretreatment with lefamulin, dexamethasone, or azithromycin, although the reductions associated with 10 to 100 mg/kg lefamulin tended to be comparatively larger in magnitude and more consistent than those associated with 10 to 100 mg/kg azithromycin. The results observed here were generally consistent with previous anti-inflammatory effects seen with azithromycin [26–28], although some inconsistencies exist that may be related to a variety of methodologic differences between the studies, including LPS dose, azithromycin dose, and route of azithromycin administration.
The plasma AUC0-24h observed here for SC lefamulin was comparable to exposures seen in healthy volunteers following a single dose of 150 mg IV lefamulin [29], which is half of the daily dose approved for the treatment of CABP. Our data are also consistent with lefamulin pharmacokinetics previously described in mice administered 35 and 70 mg/kg SC lefamulin [22], which showed dose-AUC linearity; hence, a daily dose of 70 mg/kg in mice provides equivalent exposure to 300 mg IV lefamulin in humans, which is the recommended daily dose to treat CABP [15]. Thus, the in vivo data presented here (with lefamulin doses of 10‒100 mg/kg) indicate that lefamulin anti-inflammatory activity is seen with a plasma exposure that is lower than that achieved at the corresponding antimicrobial clinical dose (ie, at subtherapeutic concentrations). The plasma exposure observed here following a 35-mg/kg SC azithromycin dose (11.6 μg∙h/mL), however, was 2-fold higher than that following a 500-mg IV 3-hour infusion in healthy volunteers (5.0 μg∙h/mL) [30]. According to the label, the daily AUC following the first and fifth daily doses of 500 mg IV azithromycin showed only an 8% increase in maximum observed plasma concentration but a 61% increase in AUC [30]. These data suggest that azithromycin anti-inflammatory activity is seen with a plasma exposure that is achieved at doses higher than the approved daily clinical dose of 500 mg IV.
The robust anti-inflammatory effects observed within a range of clinically exposure-equivalent lefamulin doses (eg, 10‒100 mg/kg) in this mouse model of neutrophilic inflammation suggest that lefamulin inhibits either LPS-induced pro-inflammatory signaling, resulting in reduced neutrophil accumulation, or alternatively, directly inhibits neutrophil infiltration into the lung, resulting in reduced levels of neutrophil-contributed cytokines and chemokines. Both potential mechanisms are consistent with the dose-dependent anti-inflammatory effects observed in vivo following lefamulin pretreatment.
LPS activates macrophages and monocytes to release high amounts of pro-inflammatory cytokines, chemokines, and MMPs via toll-like receptor (TLR)-2 and TLR-4 signaling [31, 32]. To investigate whether lefamulin targets macrophages and monocytes, in vitro experiments were performed using LPS-activated J774.2 mouse macrophages. To investigate whether any effect was species specific, human PBMCs were also tested.
In contrast to the in vivo results, pretreatment of mouse macrophages and human PBMCs with lefamulin at doses of 0.03 to 10 μM had little to no effect on the levels of LPS-induced cytokines, chemokines, or MMP-9 in cell supernatants. At the azithromycin doses tested, these results were consistent with previous studies [27, 28]. We therefore concluded that macrophages/monocytes are not the target cells of lefamulin, or alternatively, the in vitro experiments do not appropriately mimic the in vivo situation.
As macrophages seemed to be unaffected by lefamulin, neutrophils were also evaluated as potential target cells. To examine possible effects of lefamulin on neutrophil recruitment to the lungs, lefamulin and azithromycin were tested in a model of IL-8–induced neutrophil chemotaxis. However, doses of 0.03 to 30 μM lefamulin or azithromycin did not affect IL-8–induced chemotaxis of human neutrophils. These findings therefore suggest that, although lefamulin may impede neutrophil chemotaxis based on the in vivo results, it does not do so by direct interaction with macrophages or neutrophils.
Other potential target cells of lefamulin are endothelial cells and type 2 pneumocytes. When activated by pro-inflammatory mediators such as TNF-α and IL-1, the endothelium becomes a major participant in the generation of the inflammatory response, increasing adhesion molecules and enabling leukocyte extravasation [33]. Type 2 pneumocytes also have TLRs and secrete cytokines and chemokines following activation by bacterial components like LPS [34]. However, the role of these cells in the lefamulin-induced anti-inflammatory effect is not yet known.
Notably, compared with the other cytokines and chemokines tested, significant reductions in levels of IL-1β, a key pro-inflammatory cytokine [35], were observed only at higher lefamulin concentrations. This may suggest that the anti-inflammatory effects observed with lefamulin proceed via a different mechanism than that of azithromycin and other macrolides, which inhibit the production of IL-1β by alveolar macrophages [27, 28]; the possibility that lefamulin acts via a different anti-inflammatory mechanism from azithromycin is further supported by the inability of lefamulin to reduce LPS-induced cytokines, chemokines, or MMP-9 in vitro in J774.2 mouse macrophages or human PBMCs.
In earlier investigations, the veterinary pleuromutilin antibiotic valnemulin showed in vitro and in vivo anti-inflammatory effects [36, 37]. LPS-induced pulmonary edema, accumulation of inflammatory cells in BALF (eg, neutrophils and macrophages), and increased inflammatory cytokines (eg, TNF-α and IL-6) were significantly attenuated in mice pretreated with valnemulin or dexamethasone compared with no-treatment control group, with histologic analysis suggesting a protective effect from valnemulin on LPS-induced acute lung injury [36]. Valnemulin treatment in murine RAW 264.7 macrophages also significantly inhibited LPS-induced production of inflammatory mediators, including nitric oxide, prostaglandin E2, TNF-α, and IL-6 [37]. Likewise, significantly reduced TNF-α, IL-6, and CCL-2 serum levels were observed in a methicillin-resistant Staphylococcus aureus wound infection mouse model following treatment with amphenmulin, a pleuromutilin derivative currently in development for veterinary use [38]; due to the model used, however, further studies are needed to determine if these effects were the direct result of anti-inflammatory activity, an indirect consequence of antimicrobial activity, or both.
Although further research into the anti-inflammatory mechanism of lefamulin is needed, these findings have clinical implications. Glucocorticoids such as dexamethasone have demonstrated benefits in reducing mortality in patients with severe inflammation-mediated lung injury [25]. Likewise, the immunomodulatory treatment tocilizumab has been shown to reduce mortality in similar patient populations [39, 40]. Inhibition of neutrophilic lung infiltration with lefamulin may be beneficial, for example, during the early phase of ARDS, which is characterized by disruption of alveolar epithelial and endothelial barriers as well as widespread neutrophilic alveolitis, leading to formation of protein-rich edema in interstitium and alveolar spaces [7, 41]. However, these data have some limitations. First, although endotoxin (eg, LPS) models are suitable for assessing acute inflammation and early immune response [42], they do not reproduce exactly the complex pathophysiology of human sepsis or ARDS [43]. Therefore, the findings presented here provide an incomplete picture of the immunomodulatory effects of lefamulin and further research is needed. Second, only a single time point, 4 hours following LPS challenge, was examined in the in vivo models; future evaluation of additional time points in this inflammatory response may provide valuable insight. Third, methodologic differences between the analyses presented here and previous studies of azithromycin make comparisons across studies difficult.
In conclusion, these results suggest that lefamulin has anti-inflammatory properties similar to, or more potent than, those of macrolide antibiotics, which are currently used as anti-inflammatory therapy for pulmonary disorders [44]. Like macrolides, lefamulin inhibits bacterial protein synthesis and demonstrates excellent tissue penetration, accumulation in macrophages, and immunomodulatory effects (eg, neutrophilic inflammation inhibition) [15, 22, 44, 45]. Moreover, azithromycin or clarithromycin pretreatment in LPS-induced acute lung injury models similarly resulted in significantly reduced neutrophil recruitment [27]. Further research on the anti-inflammatory and immunomodulatory properties of lefamulin and its potential as a treatment for inflammatory lung diseases is warranted.
Supporting information
(PDF)
(XLSX)
Acknowledgments
Editorial and medical writing support for manuscript development was provided by Lauriaselle Afanador, PhD, Michael S. McNamara, MS, and Morgan C. Hill, PhD, employees of ICON (North Wales, PA, USA).
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research and manuscript development were funded by Nabriva Therapeutics (https://www.nabriva.com), Fort Washington, Pennsylvania, USA, and Vienna, Austria. The funder provided support in the form of salaries for MH, SP, WWW, and SPG, as well as contract funding to Fidelta (Zagreb, Croatia), from which BH, MC, and IF receive salaries. In their respective roles as employees of Nabriva Therapeutics and Fidelta, all authors were involved in aspects of the study design, implementation, decision to publish, and manuscript preparation. The specific roles of these authors are articulated in the “Author Contributions” section. Editorial and medical writing support for manuscript development was provided by Lauriaselle Afanador, PhD, Michael S. McNamara, MS, and Morgan C. Hill, PhD, employees of ICON plc (North Wales, PA, USA), and funded by Nabriva Therapeutics.
References
- 1.Sadarangani SP, Estes LL, Steckelberg JM. Non-anti-infective effects of antimicrobials and their clinical applications: a review. Mayo Clin Proc. 2015;90(1):109–27. doi: 10.1016/j.mayocp.2014.09.006 . [DOI] [PubMed] [Google Scholar]
- 2.Garey KW, Alwani A, Danziger LH, Rubinstein I. Tissue reparative effects of macrolide antibiotics in chronic inflammatory sinopulmonary diseases. Chest. 2003;123(1):261–5. doi: 10.1378/chest.123.1.261 [DOI] [PubMed] [Google Scholar]
- 3.Mogayzel PJ Jr., Naureckas ET, Robinson KA, Mueller G, Hadjiliadis D, Hoag JB, et al. Cystic fibrosis pulmonary guidelines: chronic medications for maintenance of lung health. Am J Respir Crit Care Med. 2013;187(7):680–9. doi: 10.1164/rccm.201207-1160oe [DOI] [PubMed] [Google Scholar]
- 4.Suresh Babu K, Kastelik J, Morjaria JB. Role of long term antibiotics in chronic respiratory diseases. Respir Med. 2013;107(6):800–15. doi: 10.1016/j.rmed.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 5.Leroy AG, Caillon J, Caroff N, Broquet A, Corvec S, Asehnoune K, et al. Could azithromycin be part of Pseudomonas aeruginosa acute pneumonia treatment? Front Microbiol. 2021;12:642541. doi: 10.3389/fmicb.2021.642541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhuo GY, He Q, Xiang-Lian L, Ya-Nan Y, Si-Te F. Prolonged treatment with macrolides in adult patients with non-cystic fibrosis bronchiectasis: meta-analysis of randomized controlled trials. Pulm Pharmacol Ther. 2014;29(1):80–8. doi: 10.1016/j.pupt.2014.02.002 [DOI] [PubMed] [Google Scholar]
- 7.Matthay MA, Zemans RL. The acute respiratory distress syndrome: pathogenesis and treatment. Annu Rev Pathol. 2011;6:147–63. doi: 10.1146/annurev-pathol-011110-130158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bauer TT, Ewig S, Rodloff AC, Müller EE. Acute respiratory distress syndrome and pneumonia: a comprehensive review of clinical data. Clin Infect Dis. 2006;43(6):748–56. doi: 10.1086/506430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kojicic M, Li G, Hanson AC, Lee KM, Thakur L, Vedre J, et al. Risk factors for the development of acute lung injury in patients with infectious pneumonia. Crit Care. 2012;16(2):R46. doi: 10.1186/cc11247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meduri GU, Annane D, Chrousos GP, Marik PE, Sinclair SE. Activation and regulation of systemic inflammation in ARDS: rationale for prolonged glucocorticoid therapy. Chest. 2009;136(6):1631–43. doi: 10.1378/chest.08-2408 [DOI] [PubMed] [Google Scholar]
- 11.Simonis FD, de Iudicibus G, Cremer OL, Ong DSY, van der Poll T, Bos LD, et al. Macrolide therapy is associated with reduced mortality in acute respiratory distress syndrome (ARDS) patients. Ann Transl Med. 2018;6(2):24. doi: 10.21037/atm.2017.12.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matute-Bello G, Frevert CW, Martin TR. Animal models of acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2008;295(3):L379–99. Epub 2008/07/16. doi: 10.1152/ajplung.00010.2008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giacalone VD, Margaroli C, Mall MA, Tirouvanziam R. Neutrophil adaptations upon recruitment to the lung: new concepts and implications for homeostasis and disease. Int J Mol Sci. 2020;21(3):851. doi: 10.3390/ijms21030851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paukner S, Riedl R. Pleuromutilins: potent drugs for resistant bugs-mode of action and resistance. Cold Spring Harb Perspect Med. 2017;7(1):a027110. doi: 10.1101/cshperspect.a027110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xenleta™. lefamulin. King of Prussia, PA: Nabriva Therapeutics US, Inc.; 2019.
- 16.Sader HS, Paukner S, Ivezic-Schoenfeld Z, Biedenbach DJ, Schmitz FJ, Jones RN. Antimicrobial activity of the novel pleuromutilin antibiotic BC-3781 against organisms responsible for community-acquired respiratory tract infections (CARTIs). J Antimicrob Chemother. 2012;67(5):1170–5. doi: 10.1093/jac/dks001 [DOI] [PubMed] [Google Scholar]
- 17.Paukner S, Sader HS, Ivezic-Schoenfeld Z, Jones RN. Antimicrobial activity of the pleuromutilin antibiotic BC-3781 against bacterial pathogens isolated in the SENTRY Antimicrobial Surveillance Program in 2010. Antimicrob Agents Chemother. 2013;57(9):4489–95. doi: 10.1128/AAC.00358-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waites KB, Crabb DM, Duffy LB, Jensen JS, Liu Y, Paukner S. In vitro activities of lefamulin and other antimicrobial agents against macrolide-susceptible and macrolide-resistant Mycoplasma pneumoniae from the United States, Europe, and China. Antimicrob Agents Chemother. 2017;61(2):e02008–16. doi: 10.1128/AAC.02008-16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paukner S, Gelone SP, Arends SJR, Flamm RK, Sader HS. Antibacterial activity of lefamulin against pathogens most commonly causing community-acquired bacterial pneumonia: SENTRY antimicrobial surveillance program (2015–2016). Antimicrob Agents Chemother. 2019;63(4):e02161–18. doi: 10.1128/AAC.02161-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.File TM Jr, Goldberg L, Das A, Sweeney C, Saviski J, Gelone SP, et al. Efficacy and safety of intravenous-to-oral lefamulin, a pleuromutilin antibiotic, for the treatment of community-acquired bacterial pneumonia: the phase III Lefamulin Evaluation Against Pneumonia (LEAP 1) trial. Clin Infect Dis. 2019;69(11):1856–67. doi: 10.1093/cid/ciz090 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alexander E, Goldberg L, Das AF, Moran GJ, Sandrock C, Gasink LB, et al. Oral lefamulin vs moxifloxacin for early clinical response among adults with community-acquired bacterial pneumonia: the LEAP 2 randomized clinical trial. JAMA. 2019;322(17):1661–71. doi: 10.1001/jama.2019.15468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wicha WW, Strickmann DB, Paukner S. Pharmacokinetics/pharmacodynamics of lefamulin in a neutropenic murine pneumonia model with Staphylococcus aureus and Streptococcus pneumoniae. J Antimicrob Chemother. 2019;74(suppl 3):iii11–iii8. doi: 10.1093/jac/dkz086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saleh SM, Mann TS, Peters T, Betts RJ, Henry PJ. Influence of dexamethasone on protease-activated receptor 2-mediated responses in the airways. J Pharmacol Exp Ther. 2008;324(2):622–30. doi: 10.1124/jpet.107.132753 [DOI] [PubMed] [Google Scholar]
- 24.van den Brule S, Huaux F, Uwambayinema F, Ibouraadaten S, Yakoub Y, Palmai-Pallag M, et al. Lung inflammation and thymic atrophy after bleomycin are controlled by the prostaglandin D2 receptor DP1. Am J Respir Cell Mol Biol. 2014;50(1):212–22. doi: 10.1165/rcmb.2012-0520OC [DOI] [PubMed] [Google Scholar]
- 25.The RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704. doi: 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ivetic Tkalcevic V, Bosnjak B, Hrvacic B, Bosnar M, Marjanovic N, Ferencic Z, et al. Anti-inflammatory activity of azithromycin attenuates the effects of lipopolysaccharide administration in mice. Eur J Pharmacol. 2006;539(1–2):131–8. doi: 10.1016/j.ejphar.2006.03.074 [DOI] [PubMed] [Google Scholar]
- 27.Bosnar M, Bošnjak B, Čužić S, Hrvačić B, Marjanović N, Glojnarić I, et al. Azithromycin and clarithromycin inhibit lipopolysaccharide-induced murine pulmonary neutrophilia mainly through effects on macrophage-derived granulocyte-macrophage colony-stimulating factor and interleukin-1beta. J Pharmacol Exp Ther. 2009;331(1):104–13. doi: 10.1124/jpet.109.155838 . [DOI] [PubMed] [Google Scholar]
- 28.Bosnar M, Cuzic S, Bosnjak B, Nujic K, Ergovic G, Marjanovic N, et al. Azithromycin inhibits macrophage interleukin-1beta production through inhibition of activator protein-1 in lipopolysaccharide-induced murine pulmonary neutrophilia. Int Immunopharmacol. 2011;11(4):424–34. doi: 10.1016/j.intimp.2010.12.010 [DOI] [PubMed] [Google Scholar]
- 29.Zeitlinger M, Schwameis R, Burian A, Burian B, Matzneller P, Müller M, et al. Simultaneous assessment of the pharmacokinetics of a pleuromutilin, lefamulin, in plasma, soft tissues and pulmonary epithelial lining fluid. J Antimicrob Chemother. 2016;71(4):1022–6. doi: 10.1093/jac/dkv442 [DOI] [PubMed] [Google Scholar]
- 30.Zithromax®. azithromycin dihydrate. New York, NY: Pfizer Inc; 2019. [Google Scholar]
- 31.Rossol M, Heine H, Meusch U, Quandt D, Klein C, Sweet MJ, et al. LPS-induced cytokine production in human monocytes and macrophages. Crit Rev Immunol. 2011;31(5):379–446. doi: 10.1615/critrevimmunol.v31.i5.20 [DOI] [PubMed] [Google Scholar]
- 32.Zhou D, Huang C, Lin Z, Zhan S, Kong L, Fang C, et al. Macrophage polarization and function with emphasis on the evolving roles of coordinated regulation of cellular signaling pathways. Cell Signal. 2014;26(2):192–7. doi: 10.1016/j.cellsig.2013.11.004 [DOI] [PubMed] [Google Scholar]
- 33.Kadl A, Leitinger N. The role of endothelial cells in the resolution of acute inflammation. Antioxid Redox Signal. 2005;7(11–12):1744–54. doi: 10.1089/ars.2005.7.1744 [DOI] [PubMed] [Google Scholar]
- 34.Mason RJ. Biology of alveolar type II cells. Respirology. 2006;11suppl:S12–5. doi: 10.1111/j.1440-1843.2006.00800.x [DOI] [PubMed] [Google Scholar]
- 35.Kaneko N, Kurata M, Yamamoto T, Morikawa S, Masumoto J. The role of interleukin-1 in general pathology. Inflamm Regen. 2019;39:12. doi: 10.1186/s41232-019-0101-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen Z, Zhang X, Chu X, Zhang X, Song K, Jiang Y, et al. Preventive effects of valnemulin on lipopolysaccharide-induced acute lung injury in mice. Inflammation. 2010;33(5):306–14. doi: 10.1007/s10753-010-9186-3 . [DOI] [PubMed] [Google Scholar]
- 37.Zhang X, Li H, Feng H, Xiong H, Zhang L, Song Y, et al. Valnemulin downregulates nitric oxide, prostaglandin E2, and cytokine production via inhibition of NF-kappaB and MAPK activity. Int Immunopharmacol. 2009;9(7–8):810–6. doi: 10.1016/j.intimp.2009.02.018 . [DOI] [PubMed] [Google Scholar]
- 38.Zuo X, Fang X, Zhang Z, Jin Z, Xi G, Liu Y, et al. Antibacterial activity and pharmacokinetic profile of a promising antibacterial agent: 22-(2-amino-phenylsulfanyl)-22-deoxypleuromutilin. Molecules. 2020;25(4):878. doi: 10.3390/molecules25040878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Biran N, Ip A, Ahn J, Go RC, Wang S, Mathura S, et al. Tocilizumab among patients with COVID-19 in the intensive care unit: a multicentre observational study. Lancet Rheumatol. 2020;2(10):e603–e12. doi: 10.1016/S2665-9913(20)30277-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salama C, Han J, Yau L, Reiss WG, Kramer B, Neidhart JD, et al. Tocilizumab in patients hospitalized with Covid-19 pneumonia. N Engl J Med. 2021;384(1):20–30. doi: 10.1056/NEJMoa2030340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matthay MA, Ware LB, Zimmerman GA. The acute respiratory distress syndrome. J Clin Invest. 2012;122(8):2731–40. doi: 10.1172/JCI60331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Seemann S, Zohles F, Lupp A. Comprehensive comparison of three different animal models for systemic inflammation. J Biomed Sci. 2017;24(1):60. doi: 10.1186/s12929-017-0370-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Korneev KV. Mouse models of sepsis and septic shock. Mol Biol. 2019;53(5):704–17. doi: 10.1134/S0026898419050100 [DOI] [PubMed] [Google Scholar]
- 44.Robbins R. Antibiotics as anti-inflammatories in pulmonary diseases. Southwest J Pulm Crit Care. 2018;17:97–107. [Google Scholar]
- 45.Zimmermann P, Ziesenitz VC, Curtis N, Ritz N. The immunomodulatory effects of macrolides—a systematic review of the underlying mechanisms. Front Immunol. 2018;9:302. doi: 10.3389/fimmu.2018.00302 [DOI] [PMC free article] [PubMed] [Google Scholar]