Abstract
PURPOSE
We aimed to determine the prevalence rate and radiological characteristics of intra-atrial right coronary artery (IARCA) in an adult population undergoing computed tomography coronary angiography (CTCA) on a dual-source CT scanner.
METHODS
Overall, 7114 consecutive CTCAs acquired using a dual-source CT scanner in a high-volume, specialized cardiac care facility were retrospectively analyzed for the presence of IARCA. We scrutinized the CTCA datasets to determine the prevalence rate of IARCA and also to characterize its various imaging features including its length, depth from right atrial wall, segment involved, and presence and absence of atherosclerosis within the involved segment and in the rest of the right coronary artery (RCA).
RESULTS
The prevalence of IARCA was 0.29% (21/7114) in our study population. The mean length and depth of the intra-atrial segment was 14.85 mm and 2.57 mm, respectively. The mid-RCA was the most common segment to be involved, and no significant atherosclerosis was noted either in the intra-atrial segment or the rest of the RCA.
CONCLUSION
The prevalence rate of the incidental IARCA in the adult subjects undergoing CTCA is higher than previously reported for anatomical series, as seen in our study using a dual-source scanner. This under-reported anomaly must be explicitly assessed in patients undergoing ablative and other electrophysiological procedures, where it can have important implications.
Intra-atrial, intracameral or intracavitary right coronary artery (IARCA) is a rare anomaly in which a segment of the right coronary artery (RCA) courses through the right atrial chamber. Radiologically, IARCA is defined as a segment of RCA that is entirely surrounded by intracavitary contrast in all phases of the cardiac cycle. It was initially described only in post mortem specimens and during cardiac surgeries with an incidence varying between ~0.1% and 1.8% (1, 2). Although current evidence points to it being a benign and incidental anomaly, its importance lies in its identification prior to ablative procedures for arrhythmias, catheterization of the right-sided chambers, and pacemaker implantation. With the indications for patients requiring the above procedures expanding rapidly, it is imperative to identify this anomaly pre-procedurally, as the risk of injury to the intracavitary coronary arterial segment is high. The injury can be thermal damage due to proximity to the ablation tip or due to entanglement during catheterization. IARCA can be detected reliably by using computed tomography coronary angiography (CTCA) and recent studies using CTCA have consistently detected a relatively higher prevalence rate as opposed to earlier studies due to its superior and improved image resolution (3, 4). As we increasingly shift from invasive coronary angiographies to non-invasive cross-sectional modalities, their diagnosis is bound to increase. The advent of dual-source CT scanners has led to tremendous developments in the field of cardiac imaging due to their higher temporal and spatial resolution. The purpose of this study was to identify the prevalence and characteristics of IARCA in the adult population undergoing CTCA on a dual-source CT scanner.
Methods
Study population
This study is a single-center retrospective observational study, conducted at a specialized cardiac facility at a tertiary level hospital performing over 1500 CTCAs annually. Consenting patients above 18 years of age who had undergone a CTCA for any indication between January 2015 and December 2018 were included in the study. Since this was a retrospective study involving only a review of CTCA images, the requirement of formal consent from the institutional review board (IRB) and the need for informed patient consent were waived.
CTCA acquisition
All CTCAs were acquired using either a dual-source 128 slice (Siemens Somatom Definition) or a dual-source 384 (192×2) slice CT (Siemens Somatom Force). The increased speed and advanced dose reduction techniques are important characteristics of these scanners which help both in the reduction of radiation dose and superior image quality in terms of both spatial and temporal resolution (88 and 66 ms, respectively) enabling us to delineate the course of the RCA accurately. All scans were ECG-gated and performed after intravenous injection of 1 mL/kg of non-ionic iodinated contrast media from a power injector. A bolus tracking method was used to trigger the scanning when the attenuation at the descending thoracic aorta reached 100 HU. Depending on the patient’s baseline heart rate (HR), the patient underwent either a prospectively gated scan (HR <80 bpm) or a retrospective gated scan (HR >80 bpm). Automatic exposure control was active, enabling the adjustment of the tube current (CARE DOSE, Siemens) based on the topogram.
CTCA analysis
All CTCA reports were retrieved from the institutional database, and the images were retrieved and scrutinized for the presence of IARCA. The evaluation was done using a dedicated workstation (Siemens Syngo.via VB 10B) using multiplanar or curved planar reconstructions as required. Reconstruction of the images was performed using a B36f convolution kernel, a matrix size of 512 × 512 and 0.6 mm slice thickness with 0.4 or 0.6 mm increment. The image quality was good for all the CTCAs for the purpose of our interpretation. Two cardiothoracic radiologists (with 3.5 and 2.5 years of sub-specialty experience) interpreted the images independently and reported the following parameters: 1) confirmation of diagnosis; 2) location of the intra-atrial segment; 3) length of the intra-atrial segment; 4) distance of the RCA from the right atrial wall; 5) presence of disease within the intra-atrial segment; and 6) presence of disease in the rest of the RCA. Both radiologists reviewed all the images. In case of doubtful diagnosis, both radiologists resolved the issue consensually by discussion.
Statistical analysis
Continuous variables were reported as mean values, and categorical variables were reported as frequency and percentage. The correlations between continuous variables were evaluated using Spearman’s rank correlation (ρ) or Pearson’s correlation coefficient (r), wherever appropriate.
Results
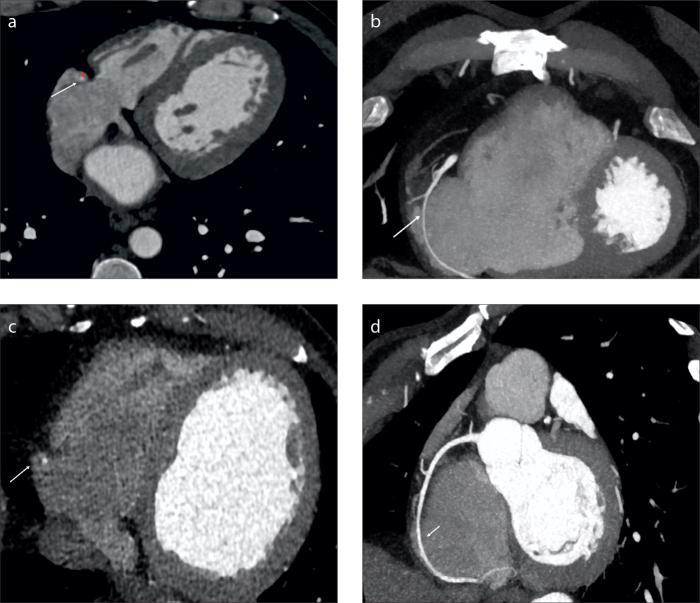
A total of 7114 CTCAs were scrutinized from the institutional database (Table). Overall, 4783 investigations were performed on the 384 slice CT, and the rest were performed on the 128 slice CT. IARCA was present in 21 patients (0.29%) (Fig.). No discrepancy was noted between the radiologists for the diagnosis of IARCA. All datasets of these 21 patients were adequate for analysis and devoid of any significant artifacts which could hamper the diagnosis or analysis of IARCA. Of the 21 patients with IARCA, 17 had retrospective scans (mean dose, 6.75 mSv), and 5 had prospective scans (mean radiation dose, 1.8 mSv).
Table.
Prevalence and characteristics of intra-atrial right coronary artery
| Variables | Total number (n=21) |
|---|---|
| Prevalence rate of IARCA, n (%) | 21 (0.29) |
|
| |
| Age (years) | 53.7 |
|
| |
| Sex ratio (Male: Female) | 1.3:1 |
|
| |
| Segment of RCA involved, n (%) | |
| • Proximal | 0 (0) |
| • Mid | 16 (76.2) |
| • Distal | 5 (42.9) |
|
| |
| Length of IARCA (mm), mean (range) | 14.85 (3.5–29) |
|
| |
| Depth of IARCA (mm), mean (range) | 2.57 (1.2–8) |
|
| |
| Prevalence of IARCA with luminal atherosclerosis, n (%) | 0 (0) |
|
| |
| Prevalence of IARCA with disease in the rest of RCA, n (%) | 2 (9) |
|
| |
| Coronary dominance, n (%) | Right, 17 (81); Left, 4 (19) |
|
| |
| Other coronary anomaly, n (%) | 1 (4.7) (anomalous origin of left circumflex artery from the right sinus) |
IARCA, intra-atrial right coronary artery; RCA, right coronary artery.
Figure.
Axial (a, c) and oblique coronal (b, d) CT images show the intra-atrial course of the distal right coronary artery (RCA) (arrow). Red line depicts the depth of RCA from the atrial wall (a).
The mean age of the patients with IARCA was 53.7 years with male: female ratio of 12:9 patients (1.3:1). Other coronary anomalies were observed in only one patient (4.7%) in the IARCA subset, which was an anomalous origin of left circumflex from the right coronary sinus. No patient with an IARCA had other anomalies involving the RCA. Overall, 17 patients (81%) had a right dominant coronary circulation.
Mid-RCA was the most common segment (16 patients, 76.2%) to have an intra-atrial course followed by the distal RCA (5 patients, 23.8%). Proximal RCA was not involved in any of the patients. None of the patients had an RCA with two intra-luminal segments. The average involved segment measured 14.85 mm (range, 3.5–29 mm). The longest intra-atrial segment was noted involving the mid-RCA. The average distance of the IARCA from the outer wall of the right atrium was 2.57 mm (range, 1.2–8 mm).
None of the intra-atrial segments of RCA had any significant disease. Mild stenosis was noted in the rest of the RCA in 2 patients (9.5%). No significant disease was noted in the RCA in any of the patients with IARCA.
There was no significant correlation between any of the characteristics of IARCA and age and sex of the patients (all p > 0.05).
Discussion
This is a large single-center study to identify the prevalence and characterization of IARCA in adult patients undergoing CTCA in a dual-source scanner. Identifying IARCA is essential due to the growing use of ablative therapies and intracardiac pacing devices. Ablation, especially at the cavotricuspid isthmus, has a risk of causing injury to RCA, which increases with the presence of an intra-atrial course, with few case reports suggesting a causal relationship (4–6). Ablation therapies and pacemaker insertion are rapidly growing with an increase in both expertise and affordability and projected to rise significantly in the near future (7, 8). IARCA is also at risk of injury during catheter manipulations, right heart catheterizations, and possibly surgeries involving the tricuspid valve (9). The increasing use of CTCA has helped in the identification of this rare anomaly more often and is a useful tool as it is usually performed before ablative procedures for pre-procedural planning. The utility of dual-source CTCA in identifying IARCA has been previously reported (10, 11). The purpose of this study was to identify the prevalence and characteristics of IARCA in the adult population undergoing CTCA on a dual-source CT scanner.
The significance of CTCA grows more critical, considering that conventional angiography cannot demonstrate IARCA. CTCA, however, is not without fallacy as RCA must be evaluated in both systolic and diastolic phases to prevent a false diagnosis of IARCA. IARCA will have a segment that is entirely surrounded by intracavitary contrast in all phases of the cardiac cycle. On searching the literature, we could find 2 CTCA studies and 3 autopsy studies reporting the prevalence of IARCA (1–4, 12). Opolski et al. (4) had established the utility of CTCA in the identification of IARCA and reported a prevalence rate of 0.15% of IARCA in their study population of 9284 patients. The higher prevalence rate in our study of 0.29% is closer to that established by Hossain et al. (3) who reported it as 0.4% in their cohort of 464 patients. The increased prevalence rate in our study may be attributable to the increased temporal and spatial resolution of current-generation scanners. While our study was performed on either a 128-slice or a 384-slice CT, the other studies have utilized either a 128-slice CT or 264/64-slice CT. While we report no significant sex predilection similar to the study by Opolski et al. (4), it was detected more commonly in men in the Hossain et al. (3) study. The autopsy or surgical series reported lower IARCA prevalence rates (2, 12). MacAlpine et al. (2) reported a prevalence rate of 0.1% out of 1000 postmortem examinations for intracavitary RCA. Ochsner et al. (12) reported a surgical prevalence rate of 0.09% for the same. A recent anatomical study by Krishnan et al. (1) demonstrated a high prevalence of 1.8%, which suggests that this anomaly is more common and almost undoubtedly under-reported on cross-sectional imaging.
The most commonly involved segment in previous studies was distal RCA compared with the mid-RCA in this study. No atherosclerotic disease was noted in the intra-atrial segment underscoring its similarity to intramuscular left anterior descending (LAD) artery, which is also associated with protection from atherosclerosis. We also did not identify any significant atherosclerosis in the rest of the RCA in this subset of patients concordant with Opolski et al. (4) and Krishnan et al. (1). However, an anatomical study by Kolodziej et al. (13) in a subset of three patients with IARCA demonstrated mild atherosclerosis involving this intra-atrial segment. Further histological studies will be required to resolve the presence or absence of predilection of the intra-atrial segment to atherosclerosis. The average depth of the RCA from the outer wall was 2.57 mm in this study. The electrode-to-artery distance determines the susceptibility of the coronary arteries to thermal damage during ablation. With ablation known to cause thermal damage to tissues within a 3–5 mm vicinity, it puts the IARCA at risk for post-ablation injury (14). Majority of the patients had a right-sided dominance (17/21, 81%). Although the RCA in case of a left dominant circulation supplies a smaller proportion of myocardium, it is nevertheless capable of being injured during the above procedures.
Although IARCA is thought to be a benign entity and mostly incidental, there is no definitive evidence to completely exonerate it from being a cause of electrical disturbances in the heart which will require a prospective follow-up study in these patients. However, the presence of IARCA adds an additional source of complication for electrophysiological procedures and right heart catheterization and must be considered when assessing procedure risk score as well as its planning.
We are limited by single-center data, which may not be truly representative of the general population. Nevertheless, it allows us to draw inference because of the large sample size. The statistical fallacy lies in the fact that CTCA is indicated only in patients with low or intermediate probability of coronary heart disease, as the rest of the patients undergo conventional angiography which does not identify the anomaly. Furthermore, even in the CTCA group, patients are not absolutely asymptomatic as they visited the hospital for some cardiac complaint for which CTCA was ordered. Clinico-radiological correlation with RCA/RCA territory symptom and pathology or correlation with intramyocardial/cavitary LAD would have been ideal but was not the objective of this study. However, our prevalence rates firmly establish that IARCA is more common than earlier realized; concordant with the more recent studies.
In conclusion, IARCA may be present in up to 0.3% of the adult population, a relatively higher rate than previous population reports. It is largely incidental and benign, but its presence may have significant implications for electrophysiological procedures, right heart catheterization, and possibly for surgeries of the tricuspid valve. CTCA is safe and reliable for identifying this anomaly. Radiologists must specifically assess and report consistently in all CTCAs, primarily prior to the invasive procedures so as to prevent potentially catastrophic perioperative complications.
Main points.
Intra-atrial right coronary artery (IARCA) is a rare and benign anomaly.
It assumes clinical importance prior to cardiac catheterization.
IARCA can be detected by using computed tomography coronary angiography (CTCA).
Recent CTCA studies have detected a relatively higher prevalence rate.
We have described the prevalence and characteristics of IARCA on CTCA.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Krishnan B, Cross C, Dykoski R, et al. Intra-atrial right coronary artery and its ablation implications. JACC Clin Electrophysiol. 2017;3:1037–1045. doi: 10.1016/j.jacep.2017.02.025. [DOI] [PubMed] [Google Scholar]
- 2.McAlpine W. Heart and coronary arteries Anatomical atlas for clinical diagnosis, radiological investigation and surgical treatment. New York: Springer; 1975. pp. 186–187. [Google Scholar]
- 3.Hossain R, Chelala L, Amin SB, et al. Intracavitary coronary artery: an unusual coronary anomaly. J Thorac Imaging. 2019;34:121–124. doi: 10.1097/RTI.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 4.Opolski MP, Pregowski J, Kruk M, et al. The prevalence and characteristics of intra-atrial right coronary artery anomaly in 9,284 patients referred for coronary computed tomography angiography. Eur J Radiol. 2014;83:1129–1134. doi: 10.1016/j.ejrad.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Tint D, Ortan FO, Ursu ME, Micu S. Right coronary artery spasm-a complication of cardiac pacemaker implantation. Anadolu Kardiyol Derg. 2013;13:815–818. doi: 10.5152/akd.2013.4984. [DOI] [PubMed] [Google Scholar]
- 6.Bertram H, Bökenkamp R, Peuster M, Hausdorf G, Paul T. Coronary artery stenosis after radiofrequency catheter ablation of accessory atrioventricular pathways in children with Ebstein’s malformation. Circulation. 2001;103:538–543. doi: 10.1161/01.CIR.103.4.538. [DOI] [PubMed] [Google Scholar]
- 7.Mond HG, Proclemer A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009--a World Society of Arrhythmia’s project. Pacing Clin Electrophysiol. 2011;34:1013–1027. doi: 10.1111/j.1540-8159.2011.03150.x. [DOI] [PubMed] [Google Scholar]
- 8.Shenthar J, Bohra S, Jetley V, et al. A survey of cardiac implantable electronic device implantation in India: By Indian Society of Electrocardiology and Indian Heart Rhythm Society. Indian Heart J. 2016;68:68–71. doi: 10.1016/j.ihj.2015.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krivoshchekov EV, Ackerman JP, Yanulevich OS, et al. Modified cone reconstruction of the tricuspid valve for Ebstein anomaly as performed in Siberia. Tex Heart Inst J. 2017;44:39–42. doi: 10.14503/THIJ-16-5832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ganga KP, Ojha V, Shaw M, Kumar S. Intra-atrial course of the right coronary artery: depiction of a potentially hazardous entity on dual-source CT. BMJ Case Rep. 2019;12:e228345. doi: 10.1136/bcr-2018-228345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christopher J, Duraikannu C. Case report: Intra-atrial course of right coronary artery: Evaluation by dual-source CT. Indian J Radiol Imaging. 2011;21:57–59. doi: 10.4103/0971-3026.76057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ochsner JL, Mills NL. Surgical management of diseased intracavitary coronary arteries. Ann Thorac Surg. 1984;38:356–362. doi: 10.1016/S0003-4975(10)62285-0. [DOI] [PubMed] [Google Scholar]
- 13.Kolodziej AW, Lobo FV, Walley VM. Intra-atrial course of the right coronary artery and its branches. Can J Cardiol. 1994;10:263–267. [PubMed] [Google Scholar]
- 14.Yan S, Gu K, Wu X, Wang W. Computer simulation study on the effect of electrode-tissue contact force on thermal lesion size in cardiac radiofrequency ablation. Int J Hyperthermia. 2020;37:37–48. doi: 10.1080/02656736.2019.1708482. [DOI] [PubMed] [Google Scholar]