Dear Editor,
We read with interest a Letter to the Editor by Xu et al. (1), in which they described no previous reported cavitation in patients with COVID-19 pneumonia to date, indicating the need to consider associated causes other than the virus infection determining the cavitary lesions. However, they reported the case of a 27-year-old man with confirmed COVID-19 infection who presented with a CT cavitation in the right lung. An extensive search revealed no secondary infectious agent, including tuberculosis. Even so, the patient was treated with multiple antimicrobial drugs, but after 5 days the symptoms improved, and the cavity enlarged. Henceforth, the patient was mainly treated with antiviral drugs, and the cavity gradually disappeared. Therefore, the authors suggested that the cavity was caused by COVID-19, although there was no pathological confirmation of that evidence.
The literature reflects consensus that lung injuries caused by COVID-19 do not cavitate, and that the finding of cavitation should direct the search for alternative diagnoses, or even overlap with other diseases, especially associated secondary infections (2). Recent studies have demonstrated that pulmonary co-infection by other agents is not uncommon in the COVID-19 context. Complications such as necrotizing pneumonia and subsequent cavitation of lung lesions may occur, and their imaging presentations are considered to be atypical of COVID-19 (3, 4). None of the published cases demonstrate adequately that the pulmonary cavitation is attributable to COVID-19 pneumonia.
We would like to report the case of a 66-year-old man admitted to the emergency room with COVID-19 pneumonia, requiring high FiO2. D-dimer level was 980 ng/mL (normal <500 ng/mL). The patient developed respiratory failure and his condition progressed slowly, with no oximetric improvement. A new D-dimer test showed values 10 times greater than normal. Angio-CT performed 23 days after the first examination demonstrated extensive pulmonary thromboembolism, with the simultaneous appearance of two cavitated lung lesions, with different morphological aspects, compatible with the evolutionary stages of pulmonary infarction cavitation (Fig.). The patient had an excellent evolution after full anticoagulation therapy.
Figure. a–d.
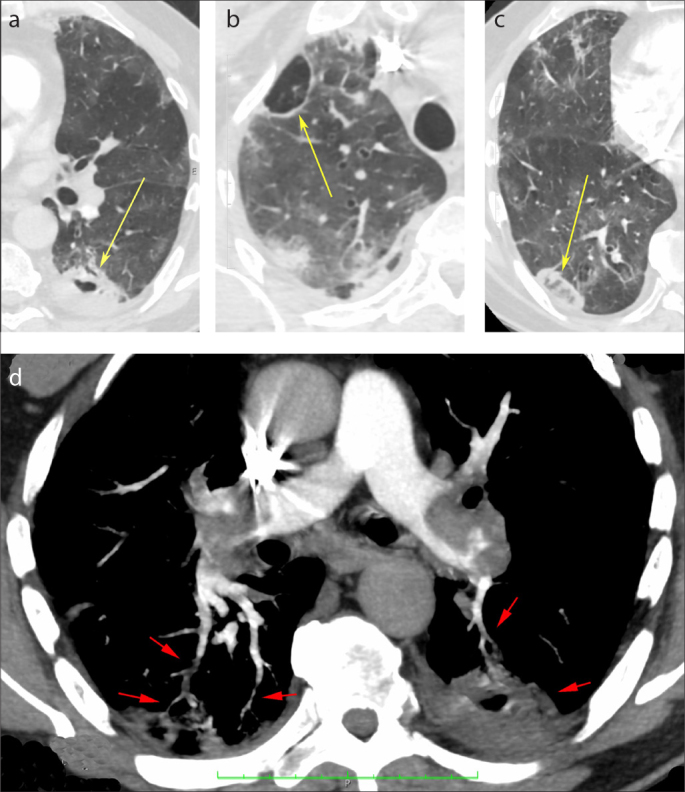
Axial chest CT images showing two cavitary lesions, one with thick walls on the left lung (a, yellow arrow), and the other with thin walls on the right lung (b, yellow arrow). A reversed halo sign in the right lung is visible (c, yellow arrow). Pulmonary angio-CT image (d) demonstrating bilateral large emboli in the pulmonary arteries, irregular and tortuous small peripheral vessels (red arrows) related to the reversed halo sign in the right lung, and the cavitary lesion on the left lung.
Lung cavitation following pulmonary embolism and infarction is an uncommon finding, described in patients with diseases other than COVID-19 (5). The two types of cavitary pulmonary infarction are bland infarction, caused by aseptic necrosis in the absence of infection, and septic infarction, caused by the superinfection of dead lung tissue. Infected pulmonary infarctions lead to cavitation more rapidly than do bland infarctions with aseptic necrosis, and infectious cavitary infarction has a higher mortality rate and requires an aggressive approach to improve the outcome (5).
Our patient had two cavitated lesions with different morphological characteristics (one with thick and irregular walls, the other with thin walls), in addition to a reticular reversed halo sign. The reticular reversed halo sign prompts differential diagnoses for angioinvasive fungal diseases, particularly in immunocompromised patients, and pulmonary infarctions (6). Our patient was not immunocompromised, and an angiographic study showed abnormal, partially occluded vessels passing to the reversed halo and the thick-walled cavity. Thus, we consider that the two cavitated lesions represent later stages of pulmonary infarction.
In conclusion, although the presence of cavitation is considered to be an atypical finding of COVID-19, suggesting alternative diagnoses, clinicians must consider that cavitation may be due to pulmonary infarctions caused directly by embolic/thrombotic vascular disease related to pulmonary involvement by COVID-19.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Xu Z, Pan A, Zhou H. Rare CT feature in a COVID-19 patient: cavitation. Diagn Interv Radiol. 2020;26:380–381. doi: 10.5152/dir.2020.20181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA - Secondary Publication. J Thorac Imaging. 2020;35:219–227. doi: 10.1097/RTI.0000000000000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amaral LTW, Beraldo GL, Brito VM, et al. Lung cavitation in COVID-19: co-infection complication or rare evolution? Einstein (Sao Paulo) 2020;18:eAI5822. doi: 10.31744/einstein_journal/2020AI5822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farias LP, Strabelli DG, Fonseca EK, Loureiro BM, Nomura CH, Sawamura MV. Thoracic tomographic manifestations in symptomatic respiratory patients with COVID-19. Radiol Bras. 2020;53:255–261. doi: 10.1590/0100-3984.2020.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koroscil MT, Hauser TR. Acute pulmonary embolism leading to cavitation and large pulmonary abscess: A rare complication of pulmonary infarction. Respir Med Case Rep. 2016;20:72–74. doi: 10.1016/j.rmcr.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mançano AD, Rodrigues RS, Menna Barreto M, Zanetti G, Moraes TC, Marchiori E. Incidence and morphological characteristics of the reversed halo sign in patients with acute pulmonary embolism and pulmonary infarction undergoing computed tomography angiography of the pulmonary arteries. J Bras Pneumol. 2019;45:e20170438. doi: 10.1590/1806-3713/e20170438. [DOI] [PMC free article] [PubMed] [Google Scholar]


