Abstract
Background
The novel SARS-CoV-2 (COVID-19) pandemic has dramatically altered the delivery of healthcare services, resulting in significant referral pattern changes, delayed presentations, and procedural delays. Our objective was to determine the effect of the COVID-19 pandemic on all-cause mortality in patients awaiting commonly performed cardiac procedures.
Methods
Clinical and administrative data sets were linked to identify all adults referred for: (1) percutaneous coronary intervention; (2) coronary artery bypass grafting; (3) valve surgery; and (4) transcatheter aortic valve implantation, from January 2014 to September 2020 in Ontario, Canada. Piece-wise regression models were used to determine the effect of the COVID-19 pandemic on referrals and procedural volume. Multivariable Cox proportional hazards models were used to determine the effect of the pandemic on waitlist mortality for the 4 procedures.
Results
We included 584,341 patients who were first-time referrals for 1 of the 4 procedures, of whom 37,718 (6.4%) were referred during the pandemic. The pandemic period was associated with a significant decline in the number of referrals and procedures completed compared with the prepandemic period. Referral during the pandemic period was a significant predictor for increased all-cause mortality for the percutaneous coronary intervention (hazard ratio, 1.83; 95% confidence interval, 1.47-2.27) and coronary artery bypass grafting (hazard ratio, 1.96; 95% confidence interval, 1.28-3.01), but not for surgical valve or transcatheter aortic valve implantation referrals. Procedural wait times were shorter during the pandemic period compared with the prepandemic period.
Conclusions
There was a significant decrease in referrals and procedures completed for cardiac procedures during the pandemic period. Referral during the pandemic was associated with increased all-cause mortality while awaiting coronary revascularization.
Résumé
Contexte
La nouvelle pandémie de SRAS-CoV-2 (COVID-19) a radicalement modifié la prestation des services de soins de santé, entraînant des changements importants dans l'orientation du parcours de soin des patients, des présentations retardées et des retards dans les procédures. Notre objectif était de déterminer l'effet de la pandémie de la COVID-19 sur la mortalité, toutes causes confondues, chez les patients en attente de procédures cardiaques courantes.
Méthodes
Des collections de données cliniques et administratives ont été réunies pour identifier tous les adultes ayant été orientés vers: (1) une intervention coronarienne percutanée; (2) un pontage coronarien; (3) une chirurgie valvulaire; et (4) une implantation valvulaire aortique par cathéter, de janvier 2014 à septembre 2020 en Ontario, Canada. Des modèles de régression par segments ont été utilisés pour déterminer l'effet de la pandémie de COVID-19 sur les renvois et le volume de procédures. Des modèles à risques proportionnels multivariables de Cox ont été utilisés pour déterminer l'effet de la pandémie sur la mortalité des patients en liste d'attente pour les quatre procédures.
Résultats
Nous avons inclus 584 341 patients qui étaient orientés pour la première fois pour l'une des quatre procédures, dont 37 718 (6,4 %) ont été orientés pendant la pandémie. La période de pandémie a été associée à une baisse significative du nombre d'orientations et de procédures réalisées par rapport à la période prépandémique. Le niveau d'orientation pendant la période pandémique était un facteur prédictif significatif de l'augmentation de la mortalité toutes causes confondues pour l'intervention coronarienne percutanée (rapport de risque, 1,83; intervalle de confiance à 95 %, 1,47-2,27) et le pontage aorto-coronarien (rapport de risque, 1,96; intervalle de confiance à 95 %, 1,28-3,01), mais pas pour les orientations pour une valve chirurgicale ou une implantation valvulaire aortique par cathéter. Les temps d'attente pour les interventions chirurgicales étaient plus courts pendant la période pandémique que pendant la période prépandémique.
Conclusions
Il y a eu une diminution significative des orientations et des procédures réalisées pour les interventions cardiaques pendant la période pandémique. Le niveau d'orientation pendant la pandémie a été associée à une augmentation de la mortalité toutes causes confondues en attendant une revascularisation coronarienne.
The novel SARS-CoV-2 (COVID-19) pandemic has dramatically affected and altered the delivery of health care services.1 In several jurisdictions, a consequence of the health policy countermeasures for the first wave of the pandemic was a significant change in referral patterns, delayed presentation of diseases, and delays in the provision of procedures and surgical interventions.1 Although these volume reductions in procedures have been well documented from several regions globally, their effect on morbidity and mortality is not well known. Issues in wait list management, while not new for publicly funded health care systems, have become a more complex and pressing problem globally during the pandemic. Because of the association of longer wait times with increased mortality in patients with life-threatening cardiovascular disease, a reduction in clinical activity might therefore lead to increased morbidity and mortality while awaiting procedures.2 However, this association has yet to be confirmed across the spectrum of cardiovascular conditions.
Accordingly, we addressed this knowledge gap by examining the effect of the COVID-19 pandemic on clinical outcomes in patients awaiting common cardiovascular procedures or surgeries. Our specific objectives were twofold: first we explored the effect of the pandemic on the number of patients referred and the actual number of procedures completed. Second, we explored the effect of the pandemic period on all-cause mortality and all-cause hospitalization for those awaiting these cardiac procedures.
Methods
The use of data in this retrospective cohort study was authorized under section 45 of Ontario's Personal Health Information Protection Act, which does not require review by a research ethics board. The need for individual patient consent was waived. We adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement for reporting of observational studies.
Context
Ontario is the largest province in Canada with a population of 14.2 million. All residents have universal access to health care through a publicly funded health care program administered by a single third-party payer, the Ontario Ministry of Health and Long-Term Care (MOHLTC).
Data sources
Our study used data constructed through linkages of multiple population and clinical databases housed at ICES (previously known as the Institute of Clinical Evaluative Sciences) in Toronto, Ontario, Canada. ICES is Canada's largest health services research institute and holds multiple population-based health databases of the Ontario population. ICES is a prescribed entity under Ontario's Personal Health Information Protection Act, which allows for researchers to link together encoded population-based administrative databases and clinical registries for conducting approved research studies under strict privacy and security policies, procedures, and practices (see link to Data and Privacy at www.ices.on.ca). We made use of the CorHealth Registry, which is a mandatory repository of data from patients who are referred or undergo cardiac procedures in Ontario; it contains data on demographic, comorbidity, and procedural variables including referral dates. Data elements have been validated through selected chart abstractions and core laboratory analyses.3 , 4 This data set was linked using unique encoded identifiers to the following administrative data sets held at ICES. The Canadian Institute of Health Information (CIHI) Discharge Abstract Database (DAD) was used to supplement baseline comorbidity and procedural data. Sociodemographic information, including postal code, was obtained from the Ontario Registered Persons Database, which was linked to Statistics Canada's census data to obtain median neighbourhood income of individuals to serve as a proxy for socioeconomic status.
Study population
Our study population was identified in the CorHealth Registry as patients older than the age of 18 years, who were referred for the following commonly performed cardiac procedures: percutaneous coronary intervention (PCI), isolated coronary artery bypass grafting (CABG), valve surgery (aortic, mitral, or tricuspid), or transcatheter aortic valve implantation (TAVI) from January 1, 2014 to September 30, 2020. This time period was chosen because it reflected a contemporary cohort yet provided sufficient number of time points to adjust for secular and seasonality trends in our regression model described later in the Statistical Analysis section. These patients were followed until one of the following occurred: procedure completed, death while awaiting procedure, or offlisting/removal from waitlist for another reason. Each episode of care represented the length of time a patient remained on the waitlist and was defined as the referral date to the removal date (procedure date, death, or offlisting).
Main exposure
The primary exposure was the COVID-19 pandemic start. Although the World Health Organization declared the COVID-19 pandemic on March 11, 2020, we considered the start of the pandemic as of March 15, 2020, when the Ontario MOHLTC directive took effect that cancelled elective surgical procedures including cardiac procedures and surgeries.5
Outcome definitions
The primary outcome for the referral cohort was death while awaiting procedure, ascertained through either the Registered Persons Database or the CIHI DAD. The secondary outcome for the referral cohort was all-cause hospitalization while awaiting procedure, ascertained from the CIHI DAD. This was only evaluated in patients who were referred and initially put on the wait list as outpatients. As such, those who were initially referred, put on the wait list, and had the procedure of interest, all during the same hospital admission, were not at risk for this outcome.
Statistical analysis
Baseline characteristics were compared between those who were referred before the pandemic (January 1, 2014 to March 14, 2020) and during the pandemic (March 15, 2020 to September 30, 2020). The Student t test was used for normally distributed continuous variables whereas the Wilcoxon rank sum test was used for non-normally distributed continuous variables. The χ2 test was used for categorical variables. Standardized mean differences were calculated.
To first better understand the potential effect of the COVID-19 pandemic on referral trends, piece-wise regression models were developed to estimate the difference in volumes over time during the pandemic compared with a counterfactual scenario of no pandemic. Using linear regression models, referral volume for different procedures were regressed by time, seasonality (weekly), an indicator for the pandemic start, and time since pandemic start. In the counterfactual model, the same models were constructed but the indicator for the pandemic start and time since pandemic start were set to 0.
For the outcome analysis, cumulative incidence function curves were derived to describe the probability of the primary outcome (all-cause mortality) or the secondary outcome (all-cause hospitalization) in the presence of competing risk events (receiving the procedure or being off-listed). Patients were followed from the date of referral to time of death or procedure or censoring at the end of the follow-up period. Cause-specific hazard competing risk models were constructed to account for the competing risks previously described, while adjusting for all patient-level baseline characteristics and the exposure of waiting during the pandemic period. Because of our objectives, we chose a cause-specific hazards model because it is well suited for etiological purposes to understand the effect of covariates on an outcome of interest while accounting for competing risks. We also included an interaction term for pandemic period and presentation type (stable coronary artery disease, acute coronary syndrome [ACS], or emergent) as well as pandemic period and sex.
Scenario analysis
To provide context on the effect of referrals, we constructed a second cohort of patients who underwent one of the procedures of interest from January 1, 2014 to September 30, 2020 and repeated the time series analyses previously described.
Categorical missing values that were < 5% were imputed to median or mode. Categorical variables with missing values ≥ 5% were placed in a “missing” category. As per privacy rules, any variable with < 5 cases were suppressed to prevent patient identity. All data analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC) and RStudio (2016, RStudio: Integrated Development for R. RStudio, Inc, Boston, MA). Statistical significance was considered to be 2-sided P values of < 0.05.
Results
Cohort derivation and baseline characteristics
Cohort derivation is shown in Supplemental Figure S1 and included 584,341 patients referred for the first time for 1 of the 4 procedures, of whom 37,718 (6.4%) were referred during the pandemic. In the PCI and CABG cohorts, although age, sex, and distribution of cardiac comorbidities were similar (as denoted by a standardized mean difference < 0.10), patients referred for procedures during the pandemic period were more likely to be urgent patients presenting with ACS (Supplemental Table S1). In those who underwent PCI, more patients underwent same-sitting PCI (ie, date of PCI was the same as referral date) during the pandemic period compared with the prepandemic period (30.7% vs 27.4%; P < 0.001). For surgical valve and TAVI patients, those referred in the pandemic period were slightly younger than those who were referred in the prepandemic period whereas other comorbidities were similar in both time periods (Supplemental Table S2).
Time series analysis
Piecewise regression showed a significant decline in the number of referrals at the pandemic onset for all procedures of interest (Supplemental Figs. S2-S5). The greatest change was for PCI (−970 weekly referrals; 95% confidence interval [CI], −1068 to −871), followed by CABG (−109 weekly referrals; 95% CI, −127 to −90), surgical valves (−35 weekly referrals; 95% CI, −45 to −25), and TAVI (−35 weekly referrals, 95% CI, −43 to −26) after accounting for secular trends and weekly seasonality. The numbers steadily increased with time after the pandemic start for all procedures (P < 0.001; Supplemental Table S3) except for surgical valves. The counterfactual scenario suggested that there would have been a year-on-year increase in the number of referrals for all procedures of interest with the exception of CABG surgery (Supplemental Table S4).
Using the procedure-completed cohort (Supplemental Fig. S1), we examined if similar effects were seen in procedural volume. A significant reduction was seen for all procedures completed (Supplemental Figs. S6-S9). In general, the recovery in procedures completed was greater in magnitude compared with referrals (Supplemental Table S4).
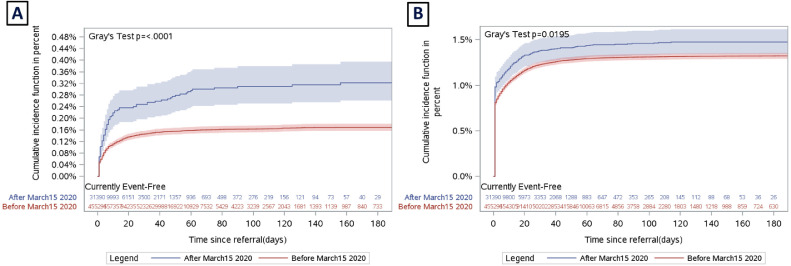
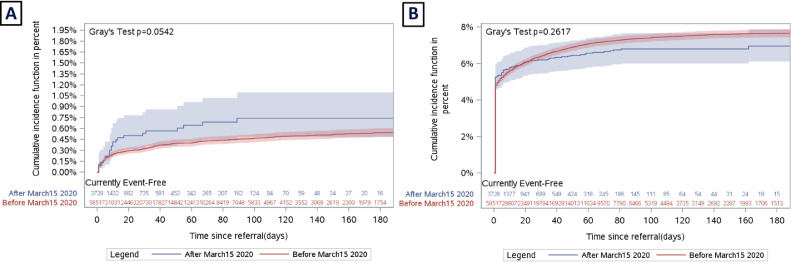
PCI and CABG waitlist morbidity and mortality: referred cohort
Unadjusted
In the PCI group, the cumulative incidence of waitlist mortality was significantly higher during the pandemic period compared with the prepandemic period (Fig. 1 A; 0.29% vs 0.17%; P < 0.001). The cumulative incidence of waitlist mortality in the CABG cohort was numerically higher in the pandemic period compared with the prepandemic period (Fig. 2 A; 0.64% vs 0.59%; P = 0.054). When restricted to patients referred while outpatients, rates of all-cause hospitalization while waiting was higher during the pandemic compared with the prepandemic period for PCI patients (Fig. 1B; 1.4% vs 1.3%; P < 0.05). There was no difference in unadjusted all-cause hospitalization during the pandemic compared with the prepandemic period for CABG for patients who were referred as outpatients (Fig. 2B; 6.5% vs 7.8%; P = 0.26).
Figure 1.
(A) Cumulative incidence of death while awaiting percutaneous coronary intervention before the pandemic (red) and after the pandemic start (blue) accounting for competing risk of receiving the procedure and being off-listed. (B) Cumulative incidence of hospital admission while awaiting percutaneous coronary intervention before the pandemic (red) and after the pandemic start (blue) accounting for competing risk of receiving the procedure, death, and being off-listed.
Figure 2.
(A) Cumulative incidence of death while awaiting coronary artery bypass grafting before the pandemic (red) and after the pandemic start (blue) accounting for competing risk of receiving the procedure and being off-listed. (B) Cumulative incidence of hospital admission while awaiting coronary artery bypass grafting before the pandemic (red) and after the pandemic start (blue) accounting for competing risk of receiving the procedure, death, and being off-listed.
The median wait times to procedure and mortality while waiting procedure for CABG and PCI during and before the pandemic are provided in Supplemental Table S5. Wait times to receiving CABG and PCI were shorter during the pandemic. The incidence of all events (including off-listing) for PCI and CABG are provided in Supplemental Table S6.
Adjusted
In the adjusted analysis, referral during the pandemic period was a significant predictor for increased all-cause mortality for the PCI (hazard ratio [HR], 1.83; 95% CI, 1.47-2.27) and CABG (HR, 1.96; 95% CI, 1.28-3.01) groups (Table 1 ). In patients referred for PCI, there was no significant interaction between ACS (P = 0.721) or emergent (P = 0.947) referral status and pandemic status. Similarly, among those who were referred for CABG, there was no significant interaction between ACS (P = 0.265) and emergent (P = 0.234) status and pandemic status. Similarly there was no interaction between sex and pandemic status for PCI patients (P = 0.839) and CABG patients (P = 0.170). When restricted to outpatients, referral during the pandemic period was not a significant predictor for all-cause hospitalization while on the wait list for CABG patients (HR, 0.90; 95% CI, 0.79-1.02) or PCI patients (HR, 1.06; 95% CI, 0.96-1.17). Full cause-specific models for mortality and all-cause hospitalization while awaiting PCI and CABG are shown in Supplemental Tables S7 and S8, respectively.
Table 1.
Summary of cause-specific HR point estimates and 95% CIs for mortality and unplanned hospital admission competing risk models and pandemic status
| Procedure | Mortality HR estimate (95% CI) | Unplanned hospital admission HR estimate (95% CI) |
|---|---|---|
| PCI | 1.83 (1.47-2.27) | 1.06 (0.96-1.17) |
| CABG | 1.96 (1.28-3.01) | 0.90 (0.79-1.02) |
| Valve surgery | 1.56 (0.85-2.89) | 0.86 (0.64-1.16) |
| TAVI | 1.43 (0.99-2.04) | 0.65 (0.53-0.81) |
CABG, coronary artery bypass grafting; CI, confidence interval; HR, hazard ratio; PCI, percutaneous coronary intervention; TAVI, transcatheter aortic valve implantation.
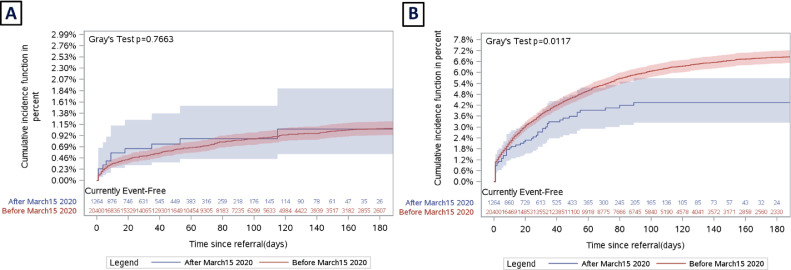
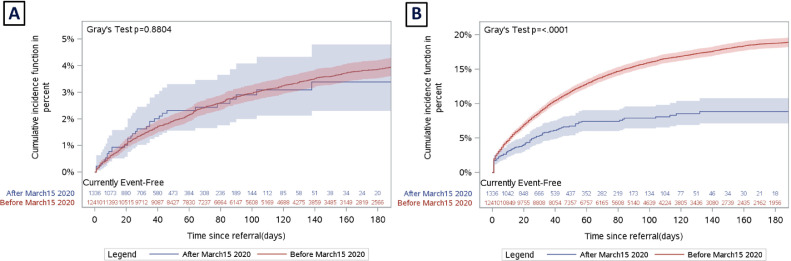
Surgical valve and TAVI waitlist morbidity and mortality: referred cohort
Unadjusted
In the surgical valve group, there was no difference in the cumulative incidence of waitlist mortality during the pandemic and prepandemic periods (Fig. 3 A; 0.87% vs 1.2%; P = 0.766). Similarly, in TAVI patients, there was no difference in the cumulative incidence of waitlist mortality during the pandemic and prepandemic periods (Fig. 4 A; 2.5% vs 4.9%; P = 0.880). Before adjustment, the incidence of all-cause hospitalization while awaiting valve surgery was lower during the pandemic (Fig. 3B; 3.8% vs 7.4%; P < 0.05). Similar findings were seen for TAVI patients before adjustment for baseline characteristics (Fig. 4B; 7.0% vs 20.6%; P < 0.001).
Figure 3.
(A) Cumulative incidence of death while awaiting valve surgery before the pandemic (red) and after the pandemic start (blue) accounting for competing risk of receiving the procedure and being off-listed. (B) Cumulative incidence of hospital admission while awaiting valve surgery before the pandemic (red) and after the pandemic start (blue) accounting for competing risk of receiving the procedure, death, and being off-listed.
Figure 4.
(A) Cumulative incidence of death while awaiting transcatheter aortic valve implantation before the pandemic (red) and after the pandemic start (blue) accounting for competing risk of receiving the procedure and being off-listed. (B) Cumulative incidence of hospital admission while awaiting transcatheter aortic valve implantation surgery before the pandemic (red) and after the pandemic start (blue) accounting for competing risk of receiving the procedure, death, and being off-listed.
The median wait times to procedure and mortality while waiting for procedures for surgical valves and TAVI during and before the pandemic are provided in Supplemental Table S5. Wait times to receiving valve surgery and TAVI were shorter during the pandemic. The incidence of all events (including off-listing) for surgical valves and TAVI are provided in Supplemental Table S6.
Adjusted
In adjusted analysis, referral during the pandemic period was not a statistically significant predictor for all-cause waitlist mortality for the surgical valve and TAVI groups (Table 1). Overall, there was no association in pandemic status and risk for all-cause hospitalization in outpatients while awaiting the procedure for surgical valve patients (HR, 0.86; 95% CI, 0.64-1.16) whereas pandemic status was associated with a lower risk of all-cause hospitalization for TAVI patients (HR, 0.65; 95% CI, 0.53-0.81) while on the wait list. There was no interaction between pandemic status and sex for patients referred for valve surgery (P = 0.165) and TAVI (P = 0.293). The complete cause-specific models for mortality and hospital admission while awaiting surgical valve and TAVI procedures are shown in Supplemental Tables S9 and S10, respectively.
Discussion
This study has several important findings. As expected, we noted a decline in the number of patients referred for commonly performed cardiovascular procedures in Ontario at the onset of the pandemic, although these numbers steadily increased throughout the pandemic period. Similarly, we also saw an initial decline in the number of procedures performed at the start of the pandemic after the issue of a government memorandum to halt elective cardiac procedures in the province. Our analysis of wait times and waitlist-related mortality suggested that the pandemic period was associated with increased waitlist mortality for those who were referred for coronary revascularization procedures despite surprisingly, a shorter time to procedure during the pandemic period. Taken together, these findings have important clinical implications. The increase in waitlist mortality for patients who required revascularization is novel—although overall wait times have not increased, this suggests that those referred might potentially have higher-acuity presentations, or at a later point in their disease progression, compared with patients before the pandemic. In our analysis on the interaction between urgency of referral and pandemic status, this increase in waitlist mortality for revascularization procedure was consistent among those with stable coronary artery disease, ACS, and emergency referral status. Coupled with the observation that referral levels remain below that historically expected, this raises concerns of a care deficit, due to upstream delays in patients being diagnosed and actually getting on the wait list. This suggests that the increased mortality we observed might be dramatically underestimated.
There might be a myriad of factors that explain the decline in referrals during the immediate pandemic period. Disruption of the referral pathways, such as reduced outpatient noninvasive testing for coronary artery disease during the pandemic might have led to a decreased detection of advanced coronary artery disease that would require further invasive imaging, might be partly responsible.6 It is also well documented in the literature that a decrease in ACS hospitalizations occurred, partly related to patients’ reluctance to present to the hospital for fear of contracting COVID-19.7 , 8 This led to public awareness campaigns in multiple jurisdictions to encourage patients with chest pain to attend the emergency department for further evaluation. Globally, the effect of COVID-19 on non-COVID-related morbidity and mortality is likely underestimated because most studies do not account for the “vanishing patient”—those that have not been referred into the health care system. Indeed, an analysis of vital statistic data from the US National Center for Health Statistics suggests that between March and July 2020, there was an increase in deaths by 20%, of which only two-thirds could be accounted for by COVID-19 and data suggesting a large increase in heart disease-related deaths.9 This care deficit warrants further research.
Additional causes for higher morbidity and mortality rates might be related to logistical challenges in obtaining timely care. Although subtle, in one British study increased door to balloon time was reported for patients with ST-elevation myocardial infarction in the COVID-19 era compared with the pre-COVID-19 era.10 There might be several factors for these delays, from decreased availability of emergency medical services, stretched thin from attending to COVID-19 cases, to more time required to properly take precautions before treating patients with chest pain, to fewer available beds in PCI centres that might be overwhelmed with critically ill COVID-19 patients.11 Similar findings have been observed in the stroke literature in a cohort study of 21 stroke centres in Northern California.12 In California, the decrease in volume of weekly stroke alerts coincided with early shelter-in-place orders during the pandemic. Those who did present with stroke presented with more severe strokes and more large vessel occlusions, despite having an overall lower comorbidity score, implying delays in diagnosis and patient avoidance of the health care system.12 , 13 Although overall wait times were not longer in the pandemic, our registries do not capture the onset of symptomatology; thus, it is possible that patients waited longer before being initially evaluated and referred for interventions. As such, patients are arriving on the wait list at a more advanced stage of their disease, and thus the increased mortality despite a shorter time on the wait list.
Overall, there are important health policy implications that must be addressed because of the possibility of subsequent waves during the COVID-19 pandemic. First, any reduction in cardiac procedural capacity to accommodate critically ill COVID-19 patients must be balanced against the real risk for waitlist mortality, which we observed for coronary revascularization procedures. We found that in the pandemic period, although overall wait times did not increase, there was increased mortality on the waitlist. Thus, any reduction in capacity might further negatively affect mortality because it reduces the ability of the system to respond nimbly to acute patients who require urgent cardiac procedures. In valve disease, previous literature suggests that the relationship between morbidity, mortality, and wait times is complex. Although we did not observe an increase in waitlist mortality for TAVI patients, previous work from our group showed that waitlist mortality for TAVI was 2% at 80 days and that event rates increased linearly with increasing wait times.2 In addition, increased capacity for TAVI was associated with lower morbidity and mortality while waiting.14 Overall, this suggests that any reduction in capacity to treat severe aortic stenosis might lead to incremental harm—whether this applies to other valve lesions is less certain and warrants further investigation. Second, maintaining timely access to outpatient and inpatient cardiac investigations will be paramount in limiting delays in referral of patients for cardiac procedures and prevent further progression of disease for those with higher-acuity presentations. Although all-cause hospitalizations while awaiting procedures did not increase during the pandemic, this might be partly explained by the shorter wait-times secondary to fewer referrals during the pandemic. Interestingly, we found that more PCI patients referred during the pandemic period underwent same-sitting PCI compared with the prepandemic period. This modest increase in same-sitting PCI during the pandemic might have occurred to reduce hospital length of stay or obviate the need for future visits.
This study must be interpreted in the context of some important limitations. Because of the retrospective observational nature of the study design, there were differences in baseline characteristics in the 2 time periods that might have biased the results. Although multivariable regression was used to account for some of these differences, including the urgent and emergent status of the patient, unmeasured or unknown confounders remain. The reason for offlisting from the waitlist is not known but it is possible that patients chose to delay their procedures because of fear of contracting COVID-19 while hospitalized for their procedure. Furthermore, we hypothesize that the true effect of the pandemic on mortality and morbidity while awaiting cardiac procedures might be underestimated because of the decline in referrals during this time period. In our analysis, we did not examine the COVID-19 status of our patients; it is possible that the higher mortality seen for patients awaiting revascularization could be associated with a positive COVID-19 status. There is evidence in the literature to suggest worse outcomes in those with COVID-19 and ACS due to the highly inflammatory nature of the virus.15 Unfortunately, we were unable to provide cause of death (ie, cardiovascular vs noncardiovascular causes) because of delay in cause of death reporting in administrative data sets. The surgical valve cohort was a heterogenous group of patients with aortic, mitral, and tricuspid disease, and because of the smaller sample of patients, we were unable to delineate the pandemic status on each individual valve type. Those who required mitral valve surgery might be likely elective patients, particularly if asymptomatic—this might explain why surgical valve procedure numbers did not increase as quickly as other procedures in the pandemic period. Finally, future work should be undertaken to understand the effect of the pandemic on postprocedural outcomes.
In conclusion, we observed a significant decrease in referrals for commonly performed cardiac procedures along with a significant decrease in number of procedures completed during the pandemic period. The potential effect of the COVID-19 pandemic on waitlist mortality and morbidity is likely underestimated and highlights the importance of continued timely recognition of symptoms and treatment of these high-risk patients with cardiovascular disease.
Acknowledgments
Acknowledgements
The authors acknowledge that the clinical registry data used in this publication is from participating hospitals through CorHealth Ontario, which serves as an advisory body to the Ontario MOHLTC, is funded by the MOHLTC, and is dedicated to improving the quality, efficiency, access, and equity in the delivery of the continuum of adult cardiac, vascular, and stroke services in Ontario, Canada.
Funding Sources
This study was funded by a grant from the Canadian Cardiovascular Society (COVID-19 Challenge for Canada Initiative) and a grant in aid from the Heart and Stroke Foundation of Canada. This study was supported by ICES, which is funded by an annual grant from the Ontario MOHLTC. The opinions, results and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are on the basis of data and/or information compiled and provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors, and not necessarily those of CIHI. Dr Wijeysundera is supported by a Phase 2 Clinician Scientist Award from the Heart and Stroke Foundation of Canada, Ontario office.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See editorial by Graham and Simpson, pages 1502–1503 of this issue.
See page 1553 for disclosure information.
To access the supplementary material accompanying this article, visit the online version of the Canadian Journal of Cardiology at www.onlinecjc.ca and at doi:10.1016/j.cjca.2021.05.008.
Appendix. Supplementary materials
References
- 1.Katz JN, Sinha SS, Alviar CL, et al. COVID-19 and disruptive modifications to cardiac critical care delivery: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;76:72–84. doi: 10.1016/j.jacc.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elbaz-Greener G, Masih S, Fang J, et al. Temporal trends and clinical consequences of wait-times for trans-catheter aortic valve replacement: a population based study. Circulation. 2018;138:483–493. doi: 10.1161/CIRCULATIONAHA.117.033432. [DOI] [PubMed] [Google Scholar]
- 3.Tu JV, Chu A, Donovan LR, et al. The Cardiovascular Health in Ambulatory Care Research Team (CANHEART): using big data to measure and improve cardiovascular health and healthcare services. Circ Cardiovasc Qual Outcomes. 2015;8:204–212. doi: 10.1161/CIRCOUTCOMES.114.001416. [DOI] [PubMed] [Google Scholar]
- 4.Wijeysundera HC, Qiu F, Koh M, et al. Comparison of outcomes of balloon-expandable versus self-expandable transcatheter heart valves for severe aortic stenosis. Am J Cardiol. 2017;119:1094–1099. doi: 10.1016/j.amjcard.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 5.Tam DY, Naimark D, Natarajan MK, et al. The use of decision modelling to inform timely policy decisions on cardiac resource capacity during the COVID-19 pandemic. Can J Cardiol. 2020;36:1308–1312. doi: 10.1016/j.cjca.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wosik J, Clowse MEB, Overton R, et al. Impact of the COVID-19 pandemic on patterns of outpatient cardiovascular care. Am Heart J. 2021;231:1–5. doi: 10.1016/j.ahj.2020.10.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Filippo O, D'Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woolf SH, Chapman DA, Sabo RT, et al. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. 2020;324:1562–1564. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdelaziz HK, Abdelrahman A, Nabi A, et al. Impact of COVID-19 pandemic on patients with ST-segment elevation myocardial infarction: insights from a British cardiac center. Am Heart J. 2020;226:45–48. doi: 10.1016/j.ahj.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roffi M, Guagliumi G, Ibanez B. The obstacle course of reperfusion for ST-segment-elevation myocardial infarction in the COVID-19 pandemic. Circulation. 2020;141:1951–1953. doi: 10.1161/CIRCULATIONAHA.120.047523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen-Huynh MN, Tang XN, Vinson DR, et al. Acute stroke presentation, care, and outcomes in community hospitals in Northern California during the COVID-19 pandemic. Stroke. 2020;51:2918–2924. doi: 10.1161/STROKEAHA.120.031099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teo KC, Leung WCY, Wong YK, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51:2228–2231. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henning KA, Ravindran M, Qiu F, et al. Impact of procedural capacity on transcatheter aortic valve replacement wait times and outcomes: a study of regional variation in Ontario. Canada. Open Heart. 2020;7 doi: 10.1136/openhrt-2020-001241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu PP, Blet A, Smyth D, Li H. The science underlying COVID-19: implications for the cardiovascular system. Circulation. 2020;142:68–78. doi: 10.1161/CIRCULATIONAHA.120.047549. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.