Abstract
Background
Consumption of 1–2 alcoholic beverages daily has been associated with a lower risk of cardiovascular disease and all-cause mortality in middle-aged and older adults. Central blood pressure has emerged as a better predictor of cardiovascular risk than peripheral blood pressure. However, the effects of habitual alcohol consumption on central blood pressure particularly in young adults, who are among the largest consumers of alcohol in North America, have yet to be investigated.
Objective
We aimed to study the effect of alcohol consumption on central and peripheral blood pressure, and arterial stiffness in young adults.
Design
Cross-sectional observational study.
Main Measures
Using a standardized questionnaire, alcohol consumption (drinks/week) was queried; participants were classified as non- (< 2), light (2–6), moderate (women 7–9, men 7–14), and heavy drinkers (women > 9, men > 14). Central blood pressure and arterial stiffness were measured using applanation tonometry.
Key Results
We recruited 153 healthy, non-smoking, non-obese individuals. We found a U-shaped effect of alcohol consumption on blood pressure. Light drinkers had significantly lower central systolic and mean arterial blood pressure, but not peripheral blood pressure when compared to non- and moderate/heavy drinkers (P < 0.05). No significant associations with arterial stiffness parameters were noted.
Conclusions
A U-shaped relationship was found between alcohol consumption and central and mean arterial blood pressure in young individuals, which importantly, was shifted towards lower levels of alcohol consumption than currently suggested. This is the first study, to our knowledge, that examines the effect of alcohol consumption on central blood pressure and arterial stiffness exclusively in young individuals. Prospective studies are needed to confirm the relationships observed herein.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06665-0.
KEY WORDS: central blood pressure, peripheral blood pressure, arterial stiffness, alcohol consumption, young adults
INTRODUCTION
Young adults in their twenties and early thirties are among the largest consumers of alcohol in North America.1, 2 Given that the rates of alcohol consumption among young adults surpass those of all other age groups, it is especially important to examine the cardiovascular risks and benefits of alcohol consumption in this population.
Whereas excessive alcohol intake is known to be detrimental, light–moderate drinking has been shown to be cardioprotective in middle-aged adults. A U- or J-shaped relationship between alcohol consumption and cardiovascular risk,3–5 arterial stiffness,6–10 and peripheral blood pressure11, 12 in middle-aged adults has been found. Current guidelines suggest that if alcohol is consumed, it should be in moderation, limiting daily consumption to one alcoholic beverage in women and two in men.13, 14
There is a known disparity between central and peripheral blood pressure.15 Central blood pressure has been identified as a potentially superior predictor of cardiovascular risk when compared to peripheral blood pressure.15 However, there is limited evidence of the effect of alcohol consumption, particularly light–moderate drinking, on central hemodynamics especially in a young population.
The current study, therefore, aims to investigate the chronic effect of alcohol consumption on both peripheral and central hemodynamics, including the assessment of central pressure, wave reflection, pulse pressure amplification, and arterial stiffness.
METHODS
Participants
Participants were recruited as part of a larger study evaluating the effects of smoking on vascular health16; all available data from non-smoking participants were considered for this analysis. Advertisements for the study were posted widely on Montreal area and McGill University websites to recruit a representative sample of young adults. Eligible participants were healthy non-smokers, aged 18 to 45, with BMI < 30 kg/m2 (height and weight were measured on the day of the assessment). Subjects with cardiovascular disease or risk factors (i.e., diabetes mellitus, hypertension, dyslipidemia, and metabolic syndrome), renal disease, respiratory diseases, autoimmune diseases (i.e., rheumatoid arthritis, systemic vasculitis, systemic lupus erythematosus), or currently pregnant were excluded from the study. Subjects had to report feeling well and not taking any medications regularly (including cardioprotective agents, oral contraceptives, or antidepressants). The completed questionnaire was reviewed carefully by a member of the research team to confirm eligibility for the study.
Ethics
Written informed consent was obtained from all participants. The study was approved by the Research Ethics Board of the McGill University Health Centre (08-020 MP-CUSM-GEN).
Assessment of Alcohol Consumption
Alcohol consumption was assessed through a standardized written questionnaire. One drink was defined as 148 mL (5 oz) of wine, sherry or port, 355 mL (12 oz) of beer or ale, and 44 mL (1.5 oz) of spirits as per Center for Disease Control guidelines.14 Participants were categorized into the following 4 groups based on weekly alcohol consumption: non-drinkers (< 2 drinks/week), light drinkers (2–6 drinks/week), moderate drinkers (7–9 drinks per week for women, and 7–14 drinks/week for men), and heavy drinkers (> 9 drinks/week for women, and > 14 drinks per week for men). These cutoff points were chosen to mimic the recommendation for alcohol consumption in middle-aged adults.13, 14
Study Protocol
Subjects were instructed to abstain from all caffeine-containing beverages and flavonoid-containing foods for at least 12 h before the assessment. Strenuous exercise and alcohol consumption were also prohibited in the 24 h leading up to the assessment.
Immediately prior to the assessment, subjects were asked to lie in a supine position for 10 min in a temperature (22 ± 1 °C) and humidity (60 ± 5%) controlled room. Peripheral blood pressure was measured in triplicate using a cuff sphygmomanometer (HEM-705CP, Omron Healthcare, Kyoto, Japan). Following the Canadian Hypertension guidelines,14 the first measure was discarded, and the average of the subsequent two measures was reported. Pulse wave analysis (PWA), carotid-femoral pulse wave velocity (cfPWV), and carotid-radial pulse wave velocity (crPWV) measurements were performed using applanation tonometry (SphygmoCor, AtCor Medical, Sydney, Australia). Measurements were repeated until good-quality recordings were within 0.5 m/s, and the average value was reported. PWA was used to calculate augmentation index (AIx), central blood pressure, and heart rate. An average radial pressure waveform was generated from 10 s of sequential radial pressure waveforms. The system software used a previously validated generalized transfer function to translate the average radial artery waveform to a corresponding central pressure waveform which, in turn, was used to determine the central blood pressure and AIx.17 Measurements were repeated until two good-quality recordings had AIx values within 4%, and the average value of those two recordings was reported. Heart rate–corrected AIx was also calculated through the system software. Lastly, pulse pressure amplification, defined as the quotient between peripheral pulse pressure and central pulse pressure, was calculated [pulse pressure amplification = peripheral pulse pressure/central pulse pressure].
Statistical Analyses
Means, medians, and frequencies were used to summarize the demographic characteristics of the participants. Demographic characteristics of the different groups “non-,” light, moderate, and heavy drinkers were compared on age, body mass index (BMI), alcohol consumption, and years of alcohol consumption. Analysis of variance (ANOVA) and the chi-square test were used to test for between-group differences in continuous and categorical variables, respectively. Hemodynamic and arterial stiffness parameters were compared using analysis of covariance (ANCOVA), adjusting for relevant covariates such as age, sex, BMI, and duration of alcohol consumption. CfPWV, crPWV, AIx, and heart rate–corrected AIx were also adjusted for mean arterial pressure (MAP). The Tukey-Kramer method was applied to account for multiple pairwise comparisons. SAS version 9.4 software (SAS Institute, 100 SAS Campus Dr, Cary, NC) was used for all statistical analyses.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
RESULTS
We recruited 153 healthy non-smokers (79 male, 74 female), aged 25.2 ± 6.4 years, with a median of 3 [IQR 0.5, 5.0] drinks per week, and for 3 [IQR 0.8, 4.0] years. Due to the small number of participants in the heavy drinking category (3 women consumed > 9 drinks/week, 4 men consumed > 14 drinks per week), these participants were included with the moderate drinking group. However, it should be noted that hemodynamic and arterial stiffness parameters were comparable between the moderate and the heavy drinking groups (Appendix, Supplementary Table 1). For convenience, the combined group will be referred to as “moderate drinkers.” Therefore, participants were classified as non-drinkers (42%), light (40%), and moderate drinkers (18%). Descriptive statistics are reported in Table 1.
Table 1.
Baseline Characteristics of Participants
| Non-drinkers (n = 64) | Light drinkers (n = 61) | Moderate drinkers (n = 28) | P value | |
|---|---|---|---|---|
| Sex (% men) | 51.5 | 52.5 | 50.0 | 0.98 |
| Age (years) | 27.4 ± 7.7 | 23.5 ± 4.2 | 23.7 ± 5.8 | 0.001 |
| Body mass index (kg/m2) | 22.5 ± 2.9 | 22.0 ± 2.2 | 22.8 ± 2.7 | 0.35 |
| Ethnicity, N (%) | ||||
| White | 35 (55%) | 48 (79%) | 26 (93%) | < 0.001 |
| Black | 1 (2%) | 0 (0%) | 1 (4%) | 0.334 |
| Asian | 21 (33%) | 8 (13%) | 0 (0%) | 0.193 |
| Hispanic | 3 (5%) | 2 (3%) | 0 (0%) | 0.842 |
| Other | 4 (6%) | 3 (5%) | 1 (4%) | 1.000 |
| Alcohol consumption (drinks/week) | 0.2 [0.0, 1.0] | 4.0 [3.0, 5.0] | 9.0 [8.0, 12.0] | < 0.001 |
| Beer | 0.0 [0.0, 0.3] | 2.0 [1.0, 3.0] | 6.0 [4.0, 7.5] | < 0.001 |
| Spirits | 0.0 [0.0, 0.0] | 0.0 [0.0, 1.0] | 2.5 [0.0, 4.5] | < 0.001 |
| Wine | 0.0 [0.0, 0.1] | 1.0 [0,0, 2.0] | 1.0 [0.0, 2.5] | < 0.001 |
| Alcohol consumption (years) | 0.5 [0.0, 3.0] | 3.0 [2.0, 4.0] | 3.0 [2,0, 5.0] | < 0.001 |
Values are expressed as a percentage, mean ± standard deviation or median [interquartile range], as appropriate. Body mass index was missing for n = 1 participant in the non-drinking group, and n = 2 participants in the light drinking group. Categories outlined by the National Institute of Health were used for reporting ethnicity18
There were no differences between the groups in dietary habits and physical activity levels (based on the questionnaire, data not shown). Participants in the non-drinking group were older (27.4 ± 7.7 years) than the light and moderate groups (23.5 ± 4.2 and 23.7 ± 5.8 years, respectively), and analyses were adjusted for age to account for this. A weak relationship between the amount of alcohol consumption and years of consumption was noted, and accounted for by adjusting for the duration of drinking. A greater proportion of moderate/heavy drinkers were White when compared to the light and non-drinkers.
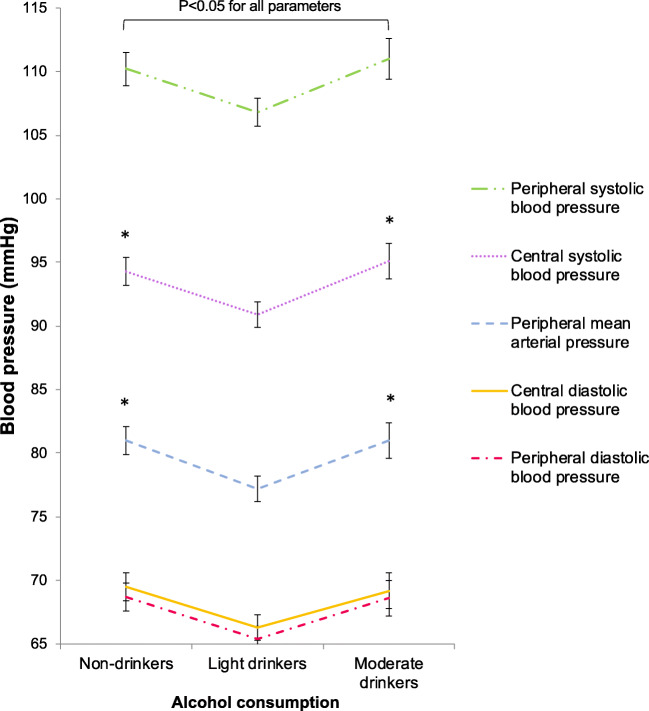
A U-shaped relationship was observed between alcohol consumption and measures of central and peripheral blood pressure (Fig. 1); a significant between-group difference was observed for all blood pressure indices. More specifically, light drinkers had significantly lower central systolic blood pressure (SBP) than both non-drinkers and moderate drinkers when adjusting for all covariates and considering multiple pairwise comparisons, as described in the statistical section. A similar pattern was observed for MAP (Table 2).
Figure 1.
The U-shaped relationship between alcohol consumption and blood pressure. *P < 0.05 vs. light drinkers after applying the Tukey-Kramer correction for multiple comparisons. Error bars reflect the standard error.
Table 2.
Comparing Hemodynamic Parameters Between Non-, Light, and Moderate Young Drinkers
| Non-drinkers | Light drinkers | Moderate drinkers | P value | |
|---|---|---|---|---|
| Peripheral SBP (mmHg) | 110.2 ± 1.1* | 106.8 ± 1.1 | 111.0 ± 1.6* | 0.03 |
| Peripheral DBP (mmHg) | 68.7 ± 1.0* | 65.4 ± 0.9 | 68.6 ± 1.4 | 0.04 |
| Central SBP (mmHg) | 94.3 ± 1.0*† | 90.9 ± 0.9 | 95.1 ± 1.4*† | 0.01 |
| Central DBP (mmHg) | 69.5 ± 1.0* | 66.3 ± 1.0 | 69.2 ± 1.4 | 0.05 |
| MAP (mmHg) | 81.0 ± 1.0*† | 77.2 ± 0.9 | 81.0 ± 1.3*† | 0.01 |
| Carotid-femoral PWV (m/s) | 6.1 ± 0.1 | 6.0 ± 0.1 | 5.8 ± 0.1 | 0.25 |
| Carotid-radial PWV (m/s) | 7.3 ± 0.1 | 7.6 ± 0.1 | 7.6 ± 0.2 | 0.26 |
| AIx (%) | − 1.9 ± 1.3 | − 1.5 ± 1.2 | 0.7 ± 1.8 | 0.48 |
| AIx heart rate corrected (%) | − 7.2 ± 1.3 | − 7.6 ± 1.3 | − 7.0 ± 1.8 | 0.96 |
| Pulse pressure amplification | 1.68 ± 0.02 | 1.67 ± 0.02 | 1.63 ± 0.02 | 0.22 |
| Heart rate (bpm) | 62.1 ± 1.1 | 61.3 ± 1.1 | 59.0 ± 1.6 | 0.29 |
SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; PWV, pulse wave velocity; AIx, augmentation index
Values are presented as mean ± standard error. All variables were adjusted for sex, age, body mass index, and years of alcohol consumption. PWV, AIx, and AIx heart rate corrected were adjusted for MAP in addition to the variables mentioned above. Central SBP/DBP was missing in n = 1 participant in the non-drinking group, and n = 2 in the light drinking group
*P < 0.05 vs. light drinkers
†P < 0.05 vs. light drinkers after applying the Tukey-Kramer correction for multiple comparisons
Peripheral SBP also followed a U-shaped relationship; light drinkers had lower SBP than non-drinkers and moderate drinkers, but this difference was not significant once multiple testing was accounted for. Similarly, both central and peripheral DBP were lowest in light drinkers, but not conclusively (Table 2). No significant differences were found for cfPWV, crPWV, AIx, AIx heart rate corrected, pulse pressure amplification, and heart rate between the three groups (Table 2). Unadjusted values of hemodynamic and arterial stiffness parameters are presented in the Appendix (Supplementary Table 2).
DISCUSSION
Our results demonstrated a U-shaped association between alcohol consumption and both central and peripheral blood pressure in a young population. After adjusting for possible confounders, we demonstrated that light drinkers had significantly lower central systolic and mean arterial blood pressures when compared to non-drinkers and moderate drinkers. In contrast, this effect was not seen with peripheral blood pressure. Importantly, a shift of the U-shaped curve towards lower levels of consumption was noted in this young population; light drinking (2–6 drinks/week) has more favorable effects on central systolic and mean arterial blood pressures when compared to non- or moderate drinking.
The results from the current study are particularly important since blood pressure in young adulthood is predictive of future cardiovascular events.19 Large prospective cohort studies have shown that even a small increase in blood pressure, within the upper limit of normal, early in life is associated with future adverse cardiovascular events.19
In our study, we specifically assessed central blood pressure in addition to peripheral blood pressures. This is important as discrepancies between these two measures have been shown, especially in young healthy individuals; for the same peripheral blood pressure, the central blood pressure might significantly vary between individuals.15 Furthermore, central blood pressure has been demonstrated to be an independent predictor of future CV events; a 10 mmHg increase in central systolic BP is associated with a 9% increased risk for CVD events.20 There is also evidence to suggest that central blood pressure is a better predictor of cardiovascular outcomes than peripheral blood pressure,21–25 and treatment regimens for hypertension have been shown to exert different effects on central blood pressure for the same effect on peripheral blood pressure.26 It is, therefore, relevant that in the current study of young individuals we examined the effect of alcohol not only on peripheral but also on central blood pressure. Interestingly, peripheral and central SBP were significantly lower in light drinkers when compared to non-drinkers and moderate drinkers, but this difference only persisted for central systolic and mean arterial BP once multiple testing was accounted for.
Previous studies in middle-aged and older adults have found that both central blood pressure and cfPWV are significantly lower in moderate drinkers.7–9 Furthermore, excessive alcohol consumption has been associated with higher cfPWV, brachial-ankle PWV, and central blood pressure.27–29 We also examined the effect of alcohol consumption on measures of arterial stiffness (cfPWV, crPWV) and wave reflection (AIx, AIx heart rate corrected) and did not find a U-shaped association in these parameters. This could be due to the absence of heavy drinkers, or at least for AIx and AIx heart rate corrected due to the fact that they were adjusted for peripheral MAP (which has a U-shaped effect). There is evidence from an earlier study in young men that AIx is higher in heavy drinkers when compared to light drinkers, but a higher threshold was set for heavy drinking (≥ 3 drinks/day).30 Importantly, no significant differences in AIx were observed when comparing moderate drinkers or non-drinkers to light drinkers. Another possible explanation could be the absence of a more permanent arterial damage due to unfavorable alcohol patterns at this early stage in young individuals. Taken together, the above data suggest that in a younger population light alcohol consumption reduced predominantly the total peripheral resistance rather than affected pressure wave reflections and aortic stiffness.
Potential mechanisms of a cardioprotective effect of alcohol have been identified in previous studies in the general adult population (but not specifically in youth). For example, an analysis of the Framingham Offspring Cohort showed that light-to-moderate alcohol use is associated with lower levels of fibrinogen, plasma viscosity, factor VII, and von Willebrand factor.31 Moderate alcohol intake (up to 1 drink per day for women and 2 drinks per day for men) is also associated with significantly increased circulating levels of high-density lipoprotein cholesterol, apolipoprotein AI, adiponectin, and significantly decreased fibrinogen levels.32 In addition, the resveratrol found in red wine is known to have potent antioxidant and anti-inflammatory effects.33
Although guidelines for alcohol consumption in the general adult population exist,13, 14 there are no specific studies and recommendations addressing alcohol consumption in young adults. Canadian and American surveys have shown that the rate of alcohol consumption peaks in the twenties and early thirties and drops in the later years.1, 2 Therefore, an evaluation of the chronic effect of alcohol consumption on both peripheral and central hemodynamics is relevant and few studies have addressed this population specifically. A sub-study of the Nurses’ Health Study II evaluated the association between alcohol consumption and subsequent hypertension risk in 70,891 young women (aged 25–42 years). They found that the relative risk of hypertension in this population according to alcohol consumption followed a J-shaped curve.34 Interestingly, the relative risk reached the lowest point among women who drank 0.25–0.50 drinks per day, and their risk was 14% lower than in non-drinkers.34 This translates to 1.75–3.5 drinks per week, which is consistent with our findings. However, the study included only women, the mean age was 35 and did not include subjects below the age of 25. Interestingly, there is also more recent data from a meta-analysis in older adults indicating that even moderate drinking (1–2 drinks per day), the current threshold adopted in alcohol consumption guidelines, is associated with an increased risk for hypertension in men.35 Therefore, a lower limit (2–6 drinks per week, i.e., light drinking) may support more optimal blood pressure in young adults and lower the risk of developing hypertension.
There are limitations to this study. The sample size is relatively small. Nevertheless, we were able to reach significance in several of our analyses even after adjusting for possible confounders. Assessment of alcohol consumption was determined by a self-administered questionnaire, which could generally be subject to recall bias and under-reporting. However, self-report is a standard method to assess alcohol consumption in the literature, and the reliability of this method is well-established,36 including among younger adults.37 Furthermore, lifestyle factors may differ between non-, light, and heavier drinkers and this could influence blood pressure levels.38 However, this is less likely in our study, given that there were no differences in dietary and physical activity habits. Furthermore, all participants had similar BMI, and they were all non-smokers and apparently healthy. A greater proportion of moderate/heavy drinkers were White when compared to the light and non-drinkers. This was mainly driven by a larger number of Asian participants in the non-drinking and light drinking groups. While we acknowledge that race and ethnicity have been shown to influence blood pressure and cardiovascular risk,39, 40 central systolic blood pressure was identical between Asian and White participants in our study (both 93 mmHg). Furthermore, peripheral systolic blood pressure was also very similar (109 mmHg and 108 mmHg in White and Asian participants, respectively).
The current study did not include a separate group of heavy drinkers. However, we specifically aimed to examine the effect of lighter drinking on vessel hemodynamics. Interestingly, increased alcohol consumption was shown to be associated with increasing hemodynamic parameters even at the level of moderate consumption. Additionally, our results are not necessarily generalizable to all young adults, including those who smoke or have other risk factors or cardiovascular disease. However, given the strong association between smoking and cardiovascular risk factors with blood pressure and arterial stiffness, we opted to study a population without these confounding variables in order to isolate the effect of alcohol alone.
Applanation tonometry is an operator-dependent technique. However, all measurements were in accordance with the SphygmoCor internal quality control system, and the operators underwent extensive training prior to the study. Furthermore, central blood pressures were not measured directly, but rather calculated non-invasively through PWA. However, this method has been validated extensively in the previous literature with intra-arterial catheterization.41–43 Moreover, central blood pressure data derived with the same method are closely associated with all-cause as well as cardiovascular mortality.20 Since this was a cross-sectional study, we were only able to find associations and not causation. Further prospective studies utilizing a longitudinal approach towards examining the effects of habitual alcohol consumption in young adulthood on cardiovascular outcomes are needed to establish causation. These studies should assess a wide variety of cardiovascular outcomes, ranging from central and peripheral blood pressures and arterial stiffness to hypertension, atherosclerosis, and vascular events with long-term follow-ups.
Lastly, more research, specifically examining the association between drinking patterns and central hemodynamic measurements, is needed. For example, binge drinking is consistently associated with increased risk for hypertension and cardiovascular disease in middle-aged and older adults. In younger adults, binge drinking has been associated with higher peripheral blood pressure.44 In our study, although questions were asked to capture binge drinking, the majority of participants were social drinkers; only one person consuming more than 11 units of alcohol per week reported drinking more than usual from time to time. Therefore, we were not able to assess the impact of binge drinking on central hemodynamics in our study.
To our knowledge, this is the first study to examine and provide support for a U-shaped effect of alcohol on central systolic and mean arterial blood pressure in young adults, which was not apparent when evaluating differences in peripheral SBP. Although previous studies in middle-aged and elderly populations have addressed this issue, no studies specific to young adults have been performed. In comparison to studies conducted in the general adult population, an interesting difference was observed. More specifically, it is light as opposed to moderate drinking that appears beneficial in younger populations. Prospective studies are needed to confirm the relationships observed herein.
Supplementary Information
(DOCX 140 kb)
Contributors
We would like to thank Yessica Gomez Sandoval, Andrew Mutter, Tania Giannone, Giordano Egiziano, Nahid Punjani, and Andrew Dawson for their valuable contribution in data collection.
Funding
This study was funded in part by a grant from the Canadian Institutes of Health Research (#102626). Dr. Daskalopoulou is supported by a senior clinician scientist award from the Fonds de la recherche en santé du Québec.
DECLARATIONS
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
REFERENCES
- 1.Canadian Centre on Substance Use and Addiction. CCSA Canadian Drug Summary Alcohol. 2019.
- 2.Delker E, Brown Q, Hasin DS. Alcohol consumption in demographic subpopulations: an epidemiologic overview. Alc Res. 2016;38:7–15. [PMC free article] [PubMed] [Google Scholar]
- 3.Bell S, Daskalopoulou M, Rapsomaniki E, et al. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ. 2017;356:j909. doi: 10.1136/bmj.j909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of alcohol consumption to all-cause, cardiovascular, and cancer-related mortality in U.S. adults. J Am Coll Cardiol. 2017;70:913–922. doi: 10.1016/j.jacc.2017.06.054. [DOI] [PubMed] [Google Scholar]
- 5.Bergmann MM, Rehm J, Klipstein-Grobusch K, et al. The association of pattern of lifetime alcohol use and cause of death in the European prospective investigation into cancer and nutrition (EPIC) study. Int J Epidemiol. 2013;42:1772–1790. doi: 10.1093/ije/dyt154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sierksma A, Lebrun CEI, Schouw YTVD, et al. Alcohol consumption in relation to aortic stiffness and aortic wave reflections: a cross-sectional study in healthy postmenopausal women. Arterioscler Thromb Vasc Biol. 2004;24:342–348. doi: 10.1161/01.ATV.0000110784.52412.8f. [DOI] [PubMed] [Google Scholar]
- 7.Hougaku H, Fleg JL, Lakatta EG, et al. Effect of light-to-moderate alcohol consumption on age-associated arterial stiffening. Am J Cardiol. 2005;95:1006–1010. doi: 10.1016/j.amjcard.2004.12.051. [DOI] [PubMed] [Google Scholar]
- 8.Mattace-Raso FU, van der Cammen TJ, van den Elzen AP, et al. Moderate alcohol consumption is associated with reduced arterial stiffness in older adults: the Rotterdam study. J Gerontol A Biol Sci Med Sci. 2005;60:1479–1483. doi: 10.1093/gerona/60.11.1479. [DOI] [PubMed] [Google Scholar]
- 9.Sierksma A, Muller M, van der Schouw YT, Grobbee DE, Hendriks HF, Bots ML. Alcohol consumption and arterial stiffness in men. J Hypertens. 2004;22:357–362. doi: 10.1097/00004872-200402000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Sasaki S, Yoshioka E, Saijo Y, et al. Relation between alcohol consumption and arterial stiffness: A cross-sectional study of middle-aged Japanese women and men. Alcohol. 2013;47:643–649. doi: 10.1016/j.alcohol.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Sesso HD, Cook NR, Buring JE, Manson JE, Gaziano JM. Alcohol consumption and the risk of hypertension in women and men. Hypertension. 2008;51:1080–1087. doi: 10.1161/HYPERTENSIONAHA.107.104968. [DOI] [PubMed] [Google Scholar]
- 12.Fuchs FD, Chambless LE, Whelton PK, Nieto FJ, Heiss G. Alcohol consumption and the incidence of hypertension: The Atherosclerosis Risk in Communities Study. Hypertension. 2001;37:1242–1250. doi: 10.1161/01.HYP.37.5.1242. [DOI] [PubMed] [Google Scholar]
- 13.United States Department of Health and Human Services. 2015-2020 Dietary Guidelines - Appendix 9 - Alcohol. 2020.
- 14.Nerenberg KA, Zarnke KB, Leung AA, et al. Hypertension Canada’s 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Can J Cardiol. 2018;34:506–525. doi: 10.1016/j.cjca.2018.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Protogerou AD, Papaioannou TG, Blacher J, Papamichael CM, Lekakis JP, Safar ME. Central blood pressures: do we need them in the management of cardiovascular disease? Is it a feasible therapeutic target? J Hypertens. 2007;25:265–272. doi: 10.1097/HJH.0b013e3280114f23. [DOI] [PubMed] [Google Scholar]
- 16.Doonan RJ, Hausvater A, Scallan C, Mikhailidis DP, Pilote L, Daskalopoulou SS. The effect of smoking on arterial stiffness. Hypertens Res. 2010;33:398–410. doi: 10.1038/hr.2010.25. [DOI] [PubMed] [Google Scholar]
- 17.Butlin M, Qasem A. Large Artery Stiffness Assessment Using SphygmoCor Technology. Pulse (Basel). 2017;4:180–192. doi: 10.1159/000452448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Institutes of Health. Racial and Ethnic Categories and Definitions for NIH Diversity Programs and for Other Reporting Purposes.
- 19.Sundstrom J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643. doi: 10.1136/bmj.d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vlachopoulos C, Aznaouridis K, O'Rourke MF, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31:1865–1871. doi: 10.1093/eurheartj/ehq024. [DOI] [PubMed] [Google Scholar]
- 21.Chirinos JA, Zambrano JP, Chakko S, et al. Relation between ascending aortic pressures and outcomes in patients with angiographically demonstrated coronary artery disease. Am J Cardiol. 2005;96:645–648. doi: 10.1016/j.amjcard.2005.04.036. [DOI] [PubMed] [Google Scholar]
- 22.London GM, Blacher J, Pannier B, Guerin AP, Marchais SJ, Safar ME. Arterial wave reflections and survival in end-stage renal failure. Hypertension. 2001;38:434–438. doi: 10.1161/01.HYP.38.3.434. [DOI] [PubMed] [Google Scholar]
- 23.Roman MJ, Devereux RB, Kizer JR, et al. Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart Study. Hypertension. 2007;50:197–203. doi: 10.1161/HYPERTENSIONAHA.107.089078. [DOI] [PubMed] [Google Scholar]
- 24.Safar ME, Blacher J, Pannier B, et al. Central pulse pressure and mortality in end-stage renal disease. Hypertension. 2002;39:735–738. doi: 10.1161/hy0202.098325. [DOI] [PubMed] [Google Scholar]
- 25.Waddell TK, Dart AM, Medley TL, Cameron JD, Kingwell BA. Carotid pressure is a better predictor of coronary artery disease severity than brachial pressure. Hypertension. 2001;38:927–931. doi: 10.1161/hy1001.096107. [DOI] [PubMed] [Google Scholar]
- 26.Williams B, Lacy PS, Thom SM, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113:1213–1225. doi: 10.1161/CIRCULATIONAHA.105.606962. [DOI] [PubMed] [Google Scholar]
- 27.Karatzi K, Papaioannou TG, Papamichael C, Lekakis J, Stefanadis C, Zampelas A. Red wine, arterial stiffness and central hemodynamics. Curr Pharm Des. 2009;15:321–328. doi: 10.2174/138161209787354195. [DOI] [PubMed] [Google Scholar]
- 28.Kurihara T, Tomiyama H, Hashimoto H, Yamamoto Y, Yano E, Yamashina A. Excessive alcohol intake increases the risk of arterial stiffening in men with normal blood pressure. Hypertens Res. 2004;27:669–673. doi: 10.1291/hypres.27.669. [DOI] [PubMed] [Google Scholar]
- 29.Nakanishi N, Kawashimo H, Nakamura K, et al. Association of alcohol consumption with increase in aortic stiffness: a 9-year longitudinal study in middle-aged Japanese men. Ind Health. 2001;39:24–28. doi: 10.2486/indhealth.39.24. [DOI] [PubMed] [Google Scholar]
- 30.van Trijp MJ, Beulens JW, Bos WJ, et al. Alcohol consumption and augmentation index in healthy young men: the ARYA study. Am J Hypertens. 2005;18:792–796. doi: 10.1016/j.amjhyper.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 31.Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002. J Am Coll Cardiol. 2010;55:1328–1335. doi: 10.1016/j.jacc.2009.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636. doi: 10.1136/bmj.d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weiskirchen S, Weiskirchen R. Resveratrol: How Much Wine Do You Have to Drink to Stay Healthy? Adv Nutr. 2016;7:706–718. doi: 10.3945/an.115.011627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thadhani R, Camargo CA, Jr, Stampfer MJ, Curhan GC, Willett WC, Rimm EB. Prospective study of moderate alcohol consumption and risk of hypertension in young women. Arch Intern Med. 2002;162:569–574. doi: 10.1001/archinte.162.5.569. [DOI] [PubMed] [Google Scholar]
- 35.Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e108–e120. doi: 10.1016/S2468-2667(17)30003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98(Suppl 2):1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- 37.Toner P, Böhnke JR, Andersen P, McCambridge J. Alcohol screening and assessment measures for young people: A systematic review and meta-analysis of validation studies. Drug Alcohol Depend. 2019;202:39–49. doi: 10.1016/j.drugalcdep.2019.01.030. [DOI] [PubMed] [Google Scholar]
- 38.Ruidavets JB, Bataille V, Dallongeville J, et al. Alcohol intake and diet in France, the prominent role of lifestyle. Eur Heart J. 2004;25:1153–1162. doi: 10.1016/j.ehj.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 39.Eastwood SV, Tillin T, Chaturvedi N, Hughes AD. Ethnic Differences in Associations Between Blood Pressure and Stroke in South Asian and European Men. Hypertension. 2015;66:481–488. doi: 10.1161/HYPERTENSIONAHA.115.05672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yano Y, Reis JP, Tedla YG, et al. Racial Differences in Associations of Blood Pressure Components in Young Adulthood With Incident Cardiovascular Disease by Middle Age: Coronary Artery Risk Development in Young Adults (CARDIA) Study. JAMA Cardiol. 2017;2:381–389. doi: 10.1001/jamacardio.2016.5678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen CH, Nevo E, Fetics B, et al. Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Validation of generalized transfer function. Circulation. 1997;95:1827–1836. doi: 10.1161/01.CIR.95.7.1827. [DOI] [PubMed] [Google Scholar]
- 42.O’Rourke MF, Pauca A, Jiang XJ. Pulse wave analysis. Br J Clin Pharmacol. 2001;51:507–522. doi: 10.1046/j.0306-5251.2001.01400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pauca AL, O'Rourke MF, Kon ND. Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension. 2001;38:932–937. doi: 10.1161/hy1001.096106. [DOI] [PubMed] [Google Scholar]
- 44.Piano MR, Burke L, Kang M, Phillips SA. Effects of Repeated Binge Drinking on Blood Pressure Levels and Other Cardiovascular Health Metrics in Young Adults: National Health and Nutrition Examination Survey, 2011-2014. J Am Heart Assoc. 2018;7:e008733. doi: 10.1161/JAHA.118.008733. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 140 kb)
Data Availability Statement
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.