INTRODUCTION
The classification of elevated cardiac troponin levels has expanded with the advent of high sensitivity troponin assays over the last decade.1, 2 A type 2 myocardial infarction (T2MI) is defined by an ischemic event due to myocardial oxygen supply-demand mismatch. Clinically, T2MI events are accompanied by ischemic findings, including chest pain and electrocardiogram changes. In contrast, patients with myocardial injury do not display evidence of ischemia. Despite their descriptive differences, both conditions are associated with short- and long-term increases in morbidity and mortality.2, 3 The timing and value of preventive medical therapy and secondary risk stratification remain largely undefined for these entities.4 The aim of this study was to investigate how patients with elevated troponin levels are managed in the hospital, with a focus on titration of cardiac medications, cardiac testing, and recommendations for outpatient evaluation.
METHODS
We retrospectively reviewed all patients between ages 55 and 65 admitted with ≥ 2 elevated cardiac troponin I (cTnI) levels suggestive of either T2MI or acute myocardial injury at three hospitals within the largest healthcare system in Rhode Island over one year. We collected data on demographics, cardioprotective medication decisions, inpatient testing, discharge summary descriptions of elevated troponin levels, and recommendations for further outpatient evaluation. Our primary outcome was the proportion of patients initiated on cardioprotective medications or whose existing regimen was intensified.
RESULTS
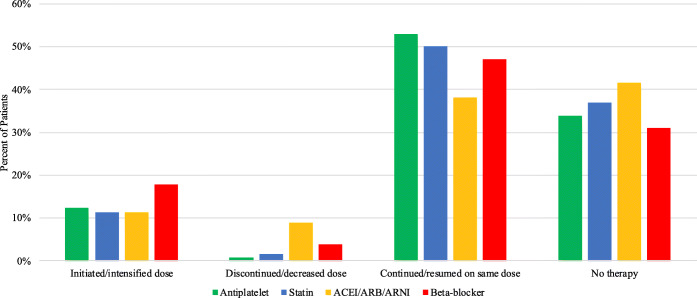
A total of 257 patients were included in the sample (Table 1). Among the sample, 33% had any cardioprotective medication initiated or intensified (Fig. 1). Approximately 41% of the sample underwent any cardiovascular testing. Two-thirds of discharge summaries (64%) included documentation of an elevated troponin and 19% recommended further outpatient evaluation.
Table 1.
Patient characteristics, inpatient management, and discharge information (N = 257)
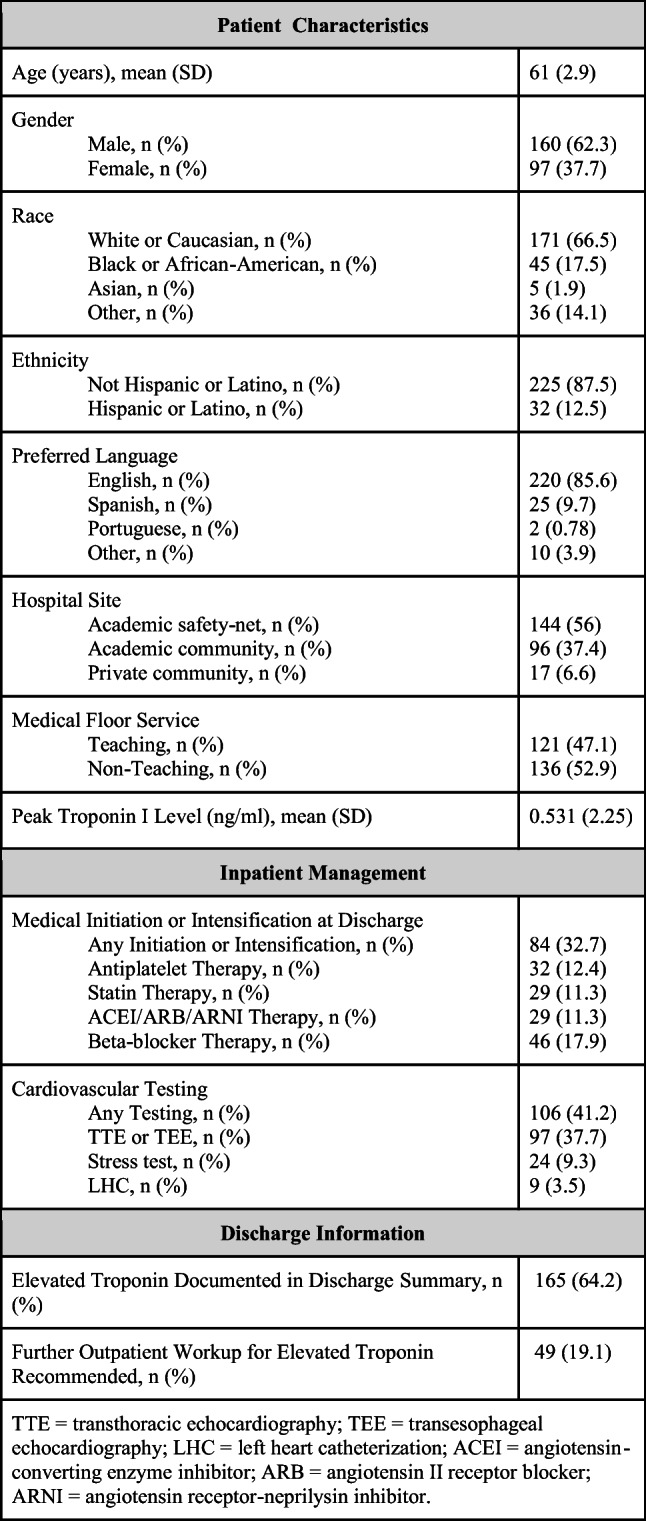
TTE, transthoracic echocardiography; TEE, transesophageal echocardiography; LHC, left heart catheterization; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ARNI, angiotensin receptor-neprilysin inhibitor
Fig. 1.
Proportions of patients with suspected type 2 myocardial infarction and acute myocardial injury who were medically initiated or intensified on, dose-reduced or discontinued, maintained without change on, or discharged without therapy for major cardioprotective medication classes at hospital discharge. ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ARNI, angiotensin receptor-neprilysin inhibitor
DISCUSSION
Overall, we found wide variation in the management of inpatients with suspected T2MI or acute myocardial injury. About a third were initiated or intensified on cardioprotective medications, and fewer than half underwent cardiovascular testing by hospital discharge. Our findings might reflect physician uncertainty about preventive medication strategies or the timing and value of secondary risk stratification in this patient population.
Medication titration and cardiac risk stratification might have been deferred for several reasons. First, patients managed in higher acuity settings were excluded; troponin elevations can be challenging to interpret and manage in the critically ill population, and these patients might warrant lower thresholds for cardioprotective medication titration, cardiovascular testing, and/or cardiology consultation compared with their medical floor counterparts. Second, more modest troponin elevations might be interpreted and acted on differently than higher levels, and—in the absence of established best practices—the cutoff prompting further management likely varies among clinicians. Patients with known coronary artery disease, marked electrocardiographic changes, and/or higher absolute troponin concentrations might be managed more aggressively. Finally, clinicians caring for patients on the general medicine ward are likely weighing competing priorities in their patients, such as the timing of initiating aspirin in a patient with a gastrointestinal bleed or an ACEI in a patient with acute kidney injury.
Our findings are consistent with observational studies which have compared inpatient management of patients with T1MI versus T2MI. Patients with T2MI are referred less often for both non-invasive and invasive testing—including coronary interventions—and less often receive guideline-directed medical therapies.5, 6
There are several limitations to this study. First, patients were identified from a single institutional database, which may limit generalizability to other regions of the country with different practice patterns. Second, the age restriction may preclude extrapolation to older adults. Third, cases were not adjudicated and therefore we could not draw conclusions on whether T2MI or acute myocardial injury patients were managed differently. Finally, we did not report on adverse cardiovascular or non-cardiovascular outcomes in this patient population.
We found substantial variability in practice patterns of hospital clinicians caring for patients with troponin elevations. While the optimal management strategies of patients with T2MI and acute myocardial injury remain uncertain, it is evident that these patients have poor short- and long-term outcomes3–6 and they might benefit from interventions to prevent future cardiovascular morbidity. Best practice guidelines for inpatient medication titration and risk stratification, in addition to studies looking at the impact of elevated troponin levels on adverse outcomes in this patient population, are urgently needed. Furthermore, complete and accurate discharge information might improve management after the patient leaves the hospital.
Acknowledgments
We appreciate the contribution of Steven Reinert, MS, Lifespan Research Analyst, who assisted with data abstraction.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018) J Am Coll Cardiol. 2018;72(18):2231–2264. doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 2.Sandoval Y, Thygesen K. Myocardial Infarction Type 2 and Myocardial Injury. Clin Chem. 2017;63(1):101–107. doi: 10.1373/clinchem.2016.255521. [DOI] [PubMed] [Google Scholar]
- 3.Sandoval Y, Jaffe AS. Type 2 Myocardial Infarction: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73(14):1846–1860. doi: 10.1016/j.jacc.2019.02.018. [DOI] [PubMed] [Google Scholar]
- 4.Christopher J, King MD, Andrew E, Levy MD, Jeffrey C, Trost MD. Clinical Progress Notes: Updates from the 4th Universal Definition of Myocardial Infarction. J. Hosp. Med. 2019;9:555–556. doi: 10.12788/jhm.3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stein GY, Herscovici G, Korenfeld R, et al. Type-II myocardial infarction--patient characteristics, management and outcomes. PLoS One. 2014;9(1):e84285. doi: 10.1371/journal.pone.0084285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baron T, Hambraeus K, Sundström J, et al. Type 2 myocardial infarction in clinical practice. Heart. 2015;101(2):101–106. doi: 10.1136/heartjnl-2014-306093. [DOI] [PubMed] [Google Scholar]