INTRODUCTION
Among cancer survivors, mental health conditions are responsible for a significant financial burden, accounting for the highest healthcare costs relative to other comorbid conditions.1 Furthermore, mental illness is associated with worse cancer-specific outcomes.2 Therefore, interventions addressing mental health interventions could improve oncologic outcomes2 and their associated healthcare costs. As such, we examined contemporary patterns of psychological distress and affordability of mental health service (MHS) among cancer survivors in the USA.
METHODS
The National Health Interview Survey (NHIS) collects data on health indicators in noninstitutionalized civilian adults living in the USA. For this study, harmonized data of participants self-reporting a cancer diagnosis from 2009 to 2018 were used. Sample weight-adjusted estimates of psychological distress were defined by the self-reported 6-item Kessler Psychological Distress Scale (K6). Using this index, K6 ≥ 13 is a validated binary threshold associated with severe mental illness;3 a 5-category scale has also been validated as follows: 0, 1–6, 7–12, 13–18, and 19–24 points.3 Additionally, the survey queried participants regarding whether they needed but were unable to afford MHS over the past 12 months.
Multivariable logistic regression defined adjusted odds ratios (AOR) and 95% confidence intervals (95CI) for the odds of needing but not being able to afford MHS as the primary outcome and the five-level K6 psychological distress index as the primary independent variable of interest. The regression was repeated stratified by insurance status (insured vs. uninsured) and also stratified by socioeconomic status (defined as ratio of family income to poverty threshold (< 1.00 vs. 1.00–1.99 vs. 2.00–3.99 vs. > 4.00)). For these stratified analyses, the primary independent variable of interest was psychological distress as a binary variable (K6 ≥ 13 vs. K6 < 13). In each of the logistic regression models, additional relevant demographic variables included are shown in Table 1. A separate model included a psychological distress (K6< vs. ≥ 13)*insurance status (insured vs. uninsured) interaction term to assess whether the effect of psychological distress on MHS affordability varied by insurance coverage.
Table 1.
Baseline Characteristics and Multivariable Logistic Regression Models for Affordability of Mental Health Services
| Baseline Char. | Unable to afford MHS | ||||||
|---|---|---|---|---|---|---|---|
| N | % | AOR | 95% CI | p > |t| | % unable to afford MHS | ||
| 1A | |||||||
| Race | 14,655 | ||||||
| White | 12,703 | 88.77 | 1.00 | - | - | - | 2.57 |
| Non-white | 1952 | 11.23 | 1.27 | 0.84 | 1.94 | 0.260 | 3.14 |
| Age | 14,655 | ||||||
| 18–64 | 6799 | 51.80 | 1.00 | - | - | - | 4.6 |
| 65–74 | 4008 | 25.57 | 0.30 | 0.19 | 0.49 | < 0.001 | 0.8 |
| ≥ 75 | 3848 | 22.63 | 0.08 | 0.03 | 0.25 | < 0.001 | 0.22 |
| Sex | 14,655 | ||||||
| Male | 5881 | 42.24 | 1.00 | - | - | - | 1.54 |
| Female | 8774 | 57.76 | 1.58 | 1.12 | 2.25 | 0.010 | 3.44 |
| Kessler score | 14,655 | ||||||
| K6 = 0 | 6176 | 42.13 | 1.00 | - | - | - | 0.32 |
| K6 = 1–6 | 6203 | 42.71 | 3.50 | 1.74 | 7.02 | < 0.001 | 1.45 |
| K6 = 7–12 | 1637 | 10.98 | 15.78 | 8.03 | 31.01 | < 0.001 | 8.34 |
| K6 = 13–18 | 496 | 3.29 | 40.42 | 19.58 | 83.43 | < 0.001 | 21.83 |
| K6 = 19–24 | 143 | 0.89 | 54.58 | 22.09 | 134.88 | < 0.001 | 28.09 |
| Insurance status | 14,655 | ||||||
| Insured | 13,912 | 94.88 | 1.00 | - | - | - | 1.95 |
| Uninsured | 743 | 5.12 | 3.49 | 2.47 | 4.92 | < 0.001 | 15.45 |
| Socioeconomic status (SES) | 14,655 | ||||||
| SES < 1.00 | 649 | 3.71 | 1.00 | - | - | - | 9.51 |
| SES 1.00–1.99 | 3560 | 19.98 | 1.18 | 0.75 | 1.85 | 0.484 | 4.83 |
| SES 2.00–3.99 | 4814 | 32.47 | 0.85 | 0.53 | 1.38 | 0.517 | 2.55 |
| SES > 4.00 | 5632 | 43.84 | 0.51 | 0.29 | 0.89 | 0.018 | 1.12 |
| 1B | |||||||
| Insurance status | 14,655 | ||||||
| Insured | 13,912 | 94.88 | 1.00 | - | - | - | 1.95 |
| K6 ≥ 13 vs. K6 ≤ 13 | - | - | 7.20 | 4.77 | 10.86 | < 0.001 | 17.91 vs. 1.33 |
| Uninsured | 743 | 5.12 | 3.49 | 2.47 | 4.92 | < 0.001 | 15.45 |
| K6 ≥ 13 vs. K6 < 13 | - | - | 8.68 | 4.45 | 16.93 | < 0.001 | 50.49 vs. 10.15 |
| 1C | |||||||
| Socioeconomic status (SES) | 14,655 | ||||||
| SES < 1.00 | 649 | 3.71 | 1.00 | - | - | - | 9.51 |
| K6 ≥ 13 vs. K6 < 13 | - | 6.16 | 2.70 | 14.02 | < 0.001 | 26.67 vs. 5.93 | |
| SES 1.00–1.99 | 3560 | 19.98 | 1.18 | 0.75 | 1.85 | 0.484 | 4.83 |
| K6 ≥ 13 vs. K6 < 13 | - | - | 6.56 | 3.85 | 11.18 | < 0.001 | 26.39 vs. 3.07 |
| SES 2.00–3.99 | 4814 | 32.47 | 0.85 | 0.53 | 1.38 | 0.517 | 2.55 |
| K6 ≥ 13 vs. K6 < 13 | - | - | 12.31 | 6.53 | 23.22 | < 0.001 | 22.24 vs. 1.74 |
| SES ≥ 4.00 | 5632 | 43.84 | 0.51 | 0.29 | 0.89 | 0.018 | 1.12 |
| K6 ≥ 13 vs. K6 < 13 | - | - | 9.02 | 3.85 | 21.14 | < 0.001 | 15.12 vs. 0.88 |
1A represents the entire cohort. In addition to the variables shown, the model was also adjusted for highest education level attained (less than high school [referent] vs. some high school vs. high school diploma/GED vs. some college vs. college degree or greater), US geographic region (Northeast [referent] vs. Midwest vs. South vs. West), self-reported health status (excellent vs. very good vs. good vs. fair vs. poor [referent]), time from cancer diagnosis (≤ 5 years [referent] vs. ≥ 6 years), birth status (US born [referent] vs. non-US born), and comorbidity score (0 [referent] vs. 1 vs. 2 vs. 3 vs. 4 vs. 5 comorbid conditions), none of which was significant. 1B and 1C show the results of multivariable logistic regression stratified by insurance status and socioeconomic status, respectively. Each of these models was also adjusted for all of the demographic characteristics listed above
RESULTS
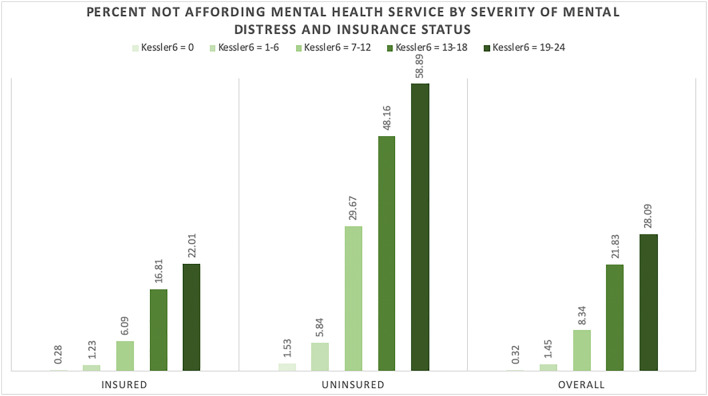
Among 14,655 survivors of cancer, factors associated with needing but inability to afford MHS included younger age, female sex, lower socioeconomic status, uninsured status, and psychological distress (Table 1). For example, uninsured cancer survivors were more likely than their insured counterparts to report needing but being unable to afford MHS (15.5% vs. 2.0%, AOR 3.49, 95CI 2.47–4.92, p < 0.001). Increasing K6 score was also associated with needing but being unable to afford MHS among cancer survivors (trend p < 0.001) (Table 1, Fig. 1). Time from cancer diagnosis was not associated with difference in affordability of MHS (p = 0.700).
Figure 1.
Rates of needing but inability to afford MHS among insured and uninsured adult cancer survivors by K6 score. *Survey question: “Have you needed but couldn’t afford mental health care in the past 12 months?” Respondents selected from “yes” and “no” for survey question. **Kessler 6 includes a self-reported questionnaire as follows: “How often you felt sad / worthless / nervous / hopeless / restless that felt everything was an effort in the past 30 days?” Respondents selected from 4 possible answers for each question: “none of the time,” “a little of the time,” “some of the time,” “most of the time,” and “all of the time.”
For both patients with and without insurance and across all SES groups, a K6 ≥ 13 score was associated with needing but being unable to afford MHS (Table 1). The interaction term psychological distress (K6< vs. ≥ 13)*insurance status (insured vs. uninsured) was not statistically significant (pinteraction = 1.0).
DISCUSSION
In this comprehensive nationwide analysis of cancer survivors in the USA, individuals with the highest need for MHS also appeared to be those least likely to be able to afford MHS. Limitations of our study include potential for reverse causality (i.e., being unable to afford MHS could lead to further psychological distress) and also lack of information on specific costs and types of MHS. Also, it is possible that individuals with higher psychological distress have greater and more costly MHS needs, leading to difficulty affording these services. However, the association persisted even among patients of higher socioeconomic status and those with health insurance, suggesting that out-of-pocket costs for MHS are high for most cancer survivors. Notably, while parity laws such as the Mental Health Parity and Addiction Equity Act of 2008 aimed to decrease financial barriers to mental health treatment,4 our study underscores the widespread barriers for access to MHS among the oncology population. Potential strategies to address these shortcomings include implementation of collaborative care models, comprised of multidisciplinary healthcare providers including mental health professionals, as these programs have demonstrated superior outcomes in treating mood disorders as compared with single disciplinary practices.5 Furthermore, incentives to improve adherence to existing standards such as those set in place by American College of Surgeons Commission on Cancer to screen patients’ level of psychological distress could lead to earlier identification and referral of cancer patients who may benefit from MHS.6
Compliance with Ethical Standards
Conflict of Interest
B.A.M. receives funding from the Prostate Cancer Foundation and (PCF) and the American Society for Radiation Oncology (ASTRO). P.L.N. receives support from Bayer, Astellas, Ferring, Dendreon, Blue Earth, Genome Dx, Augmenix, Boston Scientific, Janssen, and Cota Healthcare. M.A.A. receives funding from Sarepta Therapeutics.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rim SH, Guy GP, Yabroff KR, McGraw KA, Ekwueme DU. The impact of chronic conditions on the economic burden of cancer survivorship: a systematic review. Expert Rev Pharmacoeconomics Outcomes Res. Published online 2016. 10.1080/14737167.2016.1239533 [DOI] [PMC free article] [PubMed]
- 2.Sherrill C, Smith M, Mascoe C, Bigus E, Abbitt D. Effect of Treating Depressive Disorders on Mortality of Cancer Patients. Cureus. Published online 2017. 10.7759/cureus.1740 [DOI] [PMC free article] [PubMed]
- 3.Kessler RC, Green JG, Gruber MJ, et al. Screening for serious mental illness in the general population with the K6 screening scale: Results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. Published online 2010. 10.1002/mpr.310 [DOI] [PMC free article] [PubMed]
- 4.Mulvaney-Day N, Gibbons BJ, Alikhan S, Karakus M. Mental Health Parity and Addiction Equity Act and the Use of Outpatient Behavioral Health Services in the United States, 2005-2016. Am J Public Health. Published online 2019. 10.2105/AJPH.2019.305023 [DOI] [PMC free article] [PubMed]
- 5.Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. Published online 2012. 10.1002/14651858.cd006525.pub2 [DOI] [PMC free article] [PubMed]
- 6.Wagner L, Spiegel D, Pearman T. Using the science of psychosocial care to implement the new american college of surgeons commission on cancer distress screening standard. J Natl Compr Cancer Netw. 2013;11(2):214. doi: 10.6004/jnccn.2013.0028. [DOI] [PubMed] [Google Scholar]