Abstract
Background
Concerns exist about the ability of safety net health care organizations to participate in US health care reform. Primary care practices are key to several efforts, but little is known about how capabilities of primary care practices serving a high share of disadvantaged patients compare to other practices.
Objective
To assess capabilities around access to and quality of care among primary care practices serving a high share of Medicaid and uninsured patients compared to practices serving a low share of these patients.
Design
We analyzed data from the National Survey of Healthcare Organizations and Systems (response rate 46.8%), conducted 2017–2018.
Participants
A total of 2190 medical practices with at least three adult primary care physicians.
Main Measures
Our key exposures are payer mix and federally qualified health center (FQHC) designation. We classified practices as safety net if they reported a combined total of at least 25% of annual revenue from uninsured or Medicaid patients; we then further classified safety net practices into those that identified as an FQHC and those that did not.
Key Results
FQHCs were more likely than other safety net practices and non-safety net practices to offer early or late appointments (79%, 55%, 62%; p=0.001) and weekend appointments (56%, 39%, 42%; p=0.03). FQHCs more often provided medication-assisted treatment for opioid use disorders (43%, 27%, 25%; p=0.004) and behavioral health services (82%, 50%, 36%; p<0.001). FQHCs were more likely to screen patients for social and financial needs. However, FQHCs and other safety net providers had more limited electronic health record (EHR) capabilities (61%, 71%, 80%; p<0.001).
Conclusion
FQHCs were more likely than other types of primary care practices (both safety net practices and other practices) to possess capabilities related to access and quality. However, safety net practices were less likely than non-safety net practices to possess health information technology capabilities.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06746-0.
KEY WORDS: Safety net, primary care, Medicaid, FQHC, federally qualified health centers, physician practices, access to care, quality of care
INTRODUCTION
A spate of initiatives over the past decade have emphasized improving the quality and value of primary care, such as Medicare’s Merit-based Incentive Payment System, an array of medical home models, State Innovation Models, and broader accountable care and population health-based models. At the same time, major concerns have been raised about how safety net organizations are incorporated into these programs, including that these provider organizations may either be unfairly punished for patient severity1–3 or truly disadvantaged in terms of resources and capabilities needed for success,4–6 and as a result these organizations may suffer either inability to participate7–9 or difficulty succeeding1,2,10 under new models.
Work on other health care organizations, such as hospitals, has shown that safety net hospitals often have difficulty investing in quality-related capabilities11. Patterns may be similar for primary care practices. Despite these concerns, little work has comprehensively examined capabilities associated with high-quality care, either among primary care practices generally12 or safety net practices more specifically. Without a clear understanding of the capabilities of primary care practices, the success of efforts to improve performance will likely be dulled by the inability to sufficiently account for safety net practices’ strengths and weaknesses.13,14
Existing work on safety net primary care has largely focused on federally qualified health centers (FQHCs). FQHCs are primary care clinics that qualify for enhanced public reimbursements and grants through meeting a variety of requirements, including offering a sliding fee scale, having a quality assurance program, and community governance. Prior research has shown that FQHCs deliver care of comparable or perhaps higher quality than other primary care practices,15–17 but face challenges in areas such as recruiting staff or implementing health information technology.18,19 Of course, federally qualified health centers likely represent a fraction of practices caring for disadvantaged patients, and little research has examined the primary care safety net more broadly.
In this paper, we analyze new, nationally representative survey data to compare the organizational characteristics and capabilities of primary care practices serving a high share of Medicaid and uninsured patients with primary care practices serving low shares of these patients. We examine an array of organizational characteristics and capabilities thought to promote high-quality care,20 including capabilities in care management, health information technology, quality improvement, and access to care. We further compare safety net practices with a FQHC designation to practices with a high share of Medicaid and uninsured patients without that designation. Our paper provides a foundation for understanding the strengths and weaknesses of the primary care safety net, necessary to best develop and target initiatives focused on improving primary care for socioeconomically vulnerable populations.
METHODS
We use data from the National Survey of Healthcare Organizations and Systems (NSHOS) primary care practice survey, conducted June 2017 through August 2018. The NSHOS practice survey was created as part of a multi-center collaborative of health care researchers. At each practice, the survey targeted a single respondent, such as a practice manager, administrator, or chief physician. The survey included questions addressing domains such as organizational attributes, practice culture, quality of care, care coordination, and information systems, and both cognitive and pilot testing were employed to ensure high-quality data collection. More details on survey methodology are available in the Appendix.
To develop the sample frame, IQVIA’s OneKey database was used. The OneKey data are commercially available from IQVIA and describe relationships among clinicians, practices, hospitals, and health care systems. IQVIA develops the data using the American Medical Association’s physician Masterfile, publicly available sources, and proprietary data collection strategies, which have been used previously by researchers,21–24 including as a sample frame for national survey efforts.15,25–27 The NSHOS sample frame included all medical practices (defined as a group of clinicians delivering care at a single location) with at least three primary care specialty physicians, defined as family medicine, internal medicine, geriatrics, and general practice. A stratified-cluster sampling design was used to select practices operating different organizational structures, including independent practices and practices, while maintaining a nationally representative sample through survey weights that account for sampling probabilities.
The survey response rate was 48.6%, resulting in an analytic sample of 2190 practice responses. We conducted thorough analysis of non-response across available measures from the OneKey data, including practices’ size, specialty mix, geography, ownership, and, for practices within systems, characteristics of the systems they were in. In general, respondents and non-respondents looked statistically similar across nearly all of these measures; the only statistically significant predictor of non-response was region, with those in the Midwest being slightly more likely to have responded and those in the South being slightly less likely to have responded.
Our key exposures of interest were payer mix (across commercial, Medicare, Medicaid, self-pay, and other) of the practice and the designation of the practice as a FQHC. We classified practices as “safety net” if they reported a combined total of at least 25% of their annual revenue came from uninsured or Medicaid patients; in sensitivity analysis, we also examined varying this threshold to 30% or 50%, but substantive results were unchanged (tables available in the Appendix). We further classified safety net practices as those with FQHC designation (as assessed by self-report in our survey) and those without. We included five practices that identified as FQHC look-alikes in the FQHC category. We then compared differences between FQHCs, other safety net practices, and non-safety net practices across organizational characteristics and capabilities. We used the Pearson chi2 test to examine differences between groups for categorical variables and Bonferroni-adjusted Wald tests to evaluate differences in means for each group for continuous variables. All results were calculated using survey weights.
We first examined differences in organizational characteristics, including practice size, ownership, payer mix, and participation in payment and delivery reforms. Next, we examined differences across capabilities including enhanced patient appointment access, care management coordination, health information technology (HIT), behavioral health access, and screening for social needs. Our measures included two composites related to health information technology capabilities: Advanced HIT was defined as having at least 4 of the following capabilities: patients can access medical15–18 records, patients can comment on medical records, physicians/patients communicate via secure email, physicians know when patients fill prescriptions, system uses advanced analytic systems. HIT communication tool was defined as having at least 4 of the following capabilities: notification that a patient was admitted to a local hospital, notification that a patient visited an ED at a local hospital, receipt of discharge summaries from local hospitals, receipt of labs/test results, and information from groups that are not using the same EHR. Details on specific survey questions are available in the Appendix.
Our payer mix questions had approximately 21% missing data, which is relatively high for item non-response. We examined organizational features associated with item non-response to the payer mix question. We found that practices who did and did not respond to this question were similar across the measures in Table 1, showing similar means and no statistically significant differences in the number of employed clinicians, specialty mix of clinicians, and ownership, or most measures of payment reform participation. The only significant difference was on pay-for-performance participation; practices who were missing on the payer mix question were less likely to have participated in pay-for-performance (64% among non-response vs 72% among response, p=− 0.019).
Table 1.
Organizational Characteristics of Federally Qualified Health Centers, Other Safety Net Primary Care Practices, and Practices That Are Not Safety Net
| FQHC (N=164)* | Safety net not FQHC (N=425)* | Non-safety net (N=1141)* | p value | |
|---|---|---|---|---|
| Number of employed clinicians, mean (SE) | 19.0 (2.9) | 27.4 (4.4) | 29.3 (4.7) | 0.11 |
| Primary care physicians | 12.9 (2.8) | 13.6 (1.8) | 13.3 (1.6) | 0.97 |
| Specialist physicians | 2.1 (0.3) | 12.8 (3.3) | 16.0 (3.9) | <0.001 |
| Nurse practitioners | 3.6 (0.4) | 4.3 (0.7) | 6.0 (1.4) | 0.24 |
| Physician assistants | 2.5 (0.4) | 3.1 (0.7) | 3.5 (0.7) | 0.34 |
| Ownership, % (N) | ||||
| A hospital | 3.9 (12) | 26.2 (232) | 16.8 (356) | <0.001 |
| A health care system | 37.0 (112) | 54.6 (483) | 49.1 (1040) | |
| Non-hospital or health care system | 59.1 (178) | 19.2 (170) | 34.1 (722) | |
| Member of Independent Practice Association, % (N) | 32.1 (95) | 16.4 (145) | 17.8 (369) | 0.007 |
| Delivery reform participation, % (N) | ||||
| Primary care improvement program, e.g., PCMH† | 80.9 (239) | 54.6 (471) | 61.1 (1270) | <0.001 |
| ACO participation (any payer) | 59.9 (181) | 60.0 (532) | 56.4 (1201) | 0.61 |
| Payer mix, mean % (SE) | ||||
| Private | 17.0 (2.0) | 29.0 (0.9) | 49.5 (0.8) | <0.001 |
| Medicare | 19.5 (1.5) | 27.0 (0.8) | 35.7 (0.8) | <0.001 |
| Medicaid | 49.0 (2.6) | 31.7 (1.0) | 7.5 (0.3) | <0.001 |
| Self-pay | 11.2 (1.2) | 8.6 (0.7) | 3.7 (0.2) | <0.001 |
| Region, % (N) | ||||
| Northeast | 25.7 (78) | 16.3 (145) | 17.9 (604) | <0.001 |
| Midwest | 20.4 (62) | 43.3 (383) | 31.5 (1117) | |
| South | 12.8 (39) | 21.7 (193) | 27.5 (817) | |
| West | 41.1 (124) | 18.7 (166) | 23.1 (781) | |
| Rural, % (N) | 9.1 (28) | 22.6 (200) | 7.9 (397) | <0.001 |
*The number of observations in the table rows is greater than the number of respondents listed in the header because we conducted all analyses using survey weights which approximates the population level estimate
†In the survey, a primary care improvement program was defined to include the comprehensive primary care initiative (CPC), CPC+, and patient-centered medical homes
RESULTS
Organizational Characteristics and Payers
FQHCs, other safety net practices, and non-safety net practices employed similar numbers of primary care physicians, nurse practitioners, and physician assistants (Table 1). However, on average, FQHCs employed significantly fewer specialist physicians (FQHC=2.1, other safety net=12.8, non-safety net=16.0; p<0.001). FQHCs were less likely than other safety net practices and non-safety net practices to be owned by a hospital (3.9%, 26.2%, 16.9%) or health care system (37.0%, 54.6%, 49.1%). However, they were more likely to be part of an Independent Practice Association (32.1%, 16.4%, 17.8%; p<0.001). FQHCs were more likely than other safety net practices and non-safety net practices to participate in primary care improvement programs like patient-centered medical homes (80.9%, 54.6%, 61.1%; p<0.001), and had similar levels of participation in accountable care organizations.
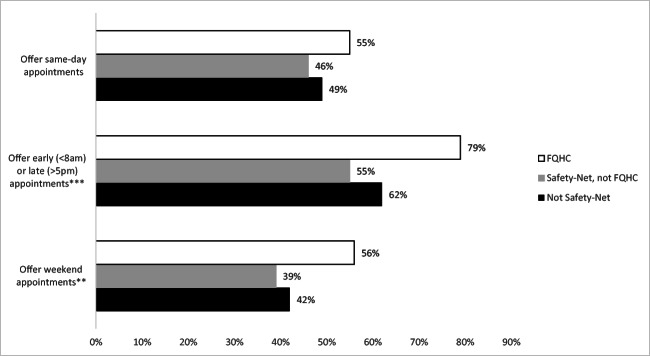
Access to Care
In terms of access to care (Fig. 1), FQHCs were more likely than other safety net practices and non-safety net practices to offer patients early (before 8 am) or late (after 5 pm) appointments (78.5%, 55.2%, 62.1%; p=0.001) and weekend appointments (56.1%, 38.9%, 42.3%; p=0.03) (Fig. 1).
Figure 1.
Enhanced appointment access strategies by practice type. Significance indicated as *p<0.05, **p<0.01, and ***p<0.001.
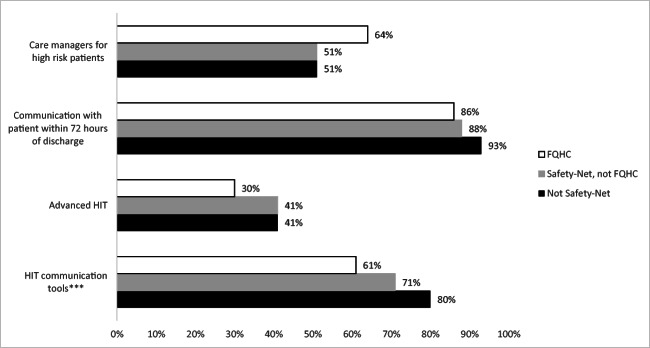
Care Management and Coordination
Safety net and other practices were similar in their care management coordination abilities (Fig. 2). FQHCs were marginally more likely to report using care managers for high-risk patients (64.1%, 50.5%, 51.4%; p=0.08), although this relationship was marginally significant. After discharging complex patients, FQHCs were less likely than other safety net practices and non-safety net practices to communicate with patients within 72 h of discharge (86.0%, 88.1%, 92.7%; p=0.05).
Figure 2.
Care management and coordination capabilities by practice type. Significance indicated as *p<0.05, **p<0.01, and ***p<0.001.
We measured two aspects of health information technology capabilities (Fig. 2). The first focused on the use of the electronic health record internal to the clinic. Specifically, if the practice's EHR had the following capabilities: patients access medical records, patients comment on medical records, patients and physicians communicate via email, physicians know when patients fill prescriptions, the system use advanced analytics. FQHCs were less likely to possess at least four out of these five internal EHR capabilities (30.3%, 41.1%, 41.3%; p=0.18), although this relationship was not significant. The second measures the ability of the EHR to connect externally. Specifically, if the EHR did the following: notify that a patient was admitted to a local hospital, notify that a patient visited an ED at a local hospital, receive discharge summaries from local hospitals, receive labs/test results, and receive information from groups that are not using the same EHR. FQHCs were less likely to possess at least four out of these five external EHR capabilities (60.9%, 71.2%, 80.3%; p<0.001)
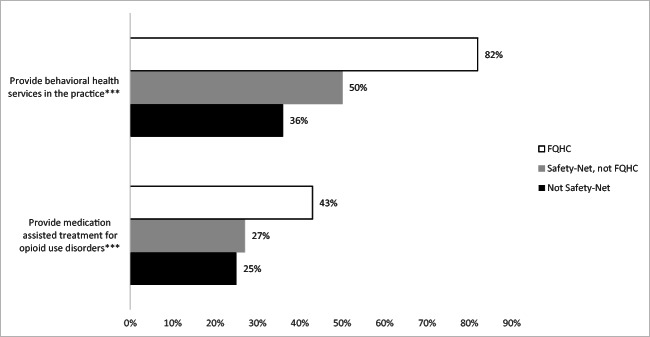
Access to Mental and Behavioral Health Services
Regarding access to mental and behavioral health treatments (Fig. 3), FQHCs were more likely than other safety net practices and non-safety net practices to provide medication-assisted treatment for opioid use disorders (42.6%, 26.8%, 25.1%; p=0.004) and behavioral health services (81.6%, 50.1%, 35.8%; p<0.001) (Fig. 3). FQHCs also reported less difficulty accessing treatment for patients with opioid use disorders (26.0%, 40.7%, 33.7%; p=0.04).
Figure 3.
Behavioral health services access across practice type. Significance indicated as *p<0.05, **p<0.01, and ***p<0.001.
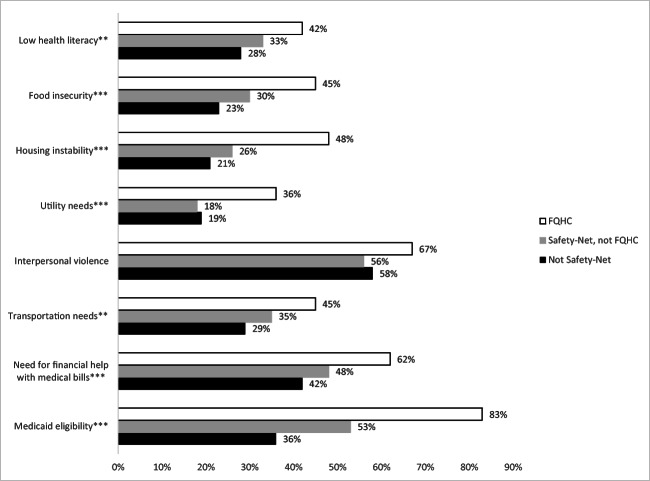
Screening for Patient Needs
FQHCs were more likely than other safety net practices and non-safety net practices to screen patients for a variety of social and financial needs (Fig. 4), including low health literacy (42.2%, 33.1%, 28.2%; p=0.03), food insecurity (44.8%, 29.9%, 23.2%; p<0.001), housing instability (48.0%, 25.6%, 21.0%; p<0.001), utility needs (35.7%, 17.6%, 18.9%; p=0.001), transportation needs (45.2%, 35.1%, 29.1%; p=0.01), need for financial assistance with medical bills (61.5%, 48.4%, 41.7%; p=0.002), and Medicaid eligibility (82.7%, 53.2%, 35.9%; p<0.001).
Figure 4.
Routine screening for social and financial needs by practice type. Significance indicated as *p<0.05, **p<0.01, and ***p<0.001.
DISCUSSION
Using new national data on primary care practices, we find that practices serving a high share of Medicaid and uninsured patients differ in key ways. First, primary care safety net practices include both practices designated as FQHCs and practices without such designation, and this distinction is quite important. FQHCs exhibited strengths and weaknesses that were distinct from safety net practices without the FQHC designation. FQHCs had more advanced capabilities than other practices in care management, patient access, and behavioral health. FQHCs and other safety net practices, however, were both less “wired” with other health care provider organizations.
Our results have critical implications for policy and practice and suggest that policymakers should carefully consider the benefits of expanding the FQHC program. Despite a challenging payer mix, FQHCs stand out across many features that may facilitate higher quality, patient-centered care. These results may be a function of several mechanisms. First, the grants and higher reimbursement received through the program may facilitate practices investing in and developing greater access and quality capabilities. Second, the FQHC program requires clinics engage in a number of activities that may facilitate performance on the variables included in our study. For example, regulations stipulate that FQHCs must have a quality assurance program, have scheduled hours of operation responsive to patient needs, and provide enabling services (such as interpreters or transportation) to assist patients in accessing care. Although these requirements leave autonomy and flexibility to individual health centers (for example, on their specific operating hours), they may promote greater capabilities as measured in our study. Additionally, the FQHC program has other incentives that might contribute to their quality capabilities. This includes Quality Improvement Awards that reward health centers for improving access to care, clinical performance, or use of health information technology. Finally, because clinics must apply for and be accepted into the FQHC program, the program may select for high-quality practices likely to invest in access and quality capabilities. Regardless of the mechanism, our data suggest that expanding the FQHC program could result in improved capabilities among safety net practices. A deeper understanding of which aspects of the program promote greater capabilities through additional research would be beneficial to further explicate our findings.
Second, health information technology may require particular support for safety net provider organizations. Outpatient physicians have long discussed the difficulty of obtaining data on patients from outside one’s practice. In particular, the importance of receiving timely notifications of hospital and emergency department visits and discharges has risen as models like accountable care organizations have become prominent. Additionally, this is particularly salient given work has shown that better communication between primary care and hospitals is associated with greater care integration between safety net primary care practices and hospitals (e.g., joint quality improvement, clinical guideline alignment).28
Our work has important limitations. Most notably, we have studied only practice capabilities, without patient outcome data. While practice capabilities are important, a more in-depth understanding of how these capabilities influence patient outcomes, particularly in the safety net, is necessary in future work. Second, as noted above, because our work is descriptive and focused on high level differences between practices, we are unable to distinguish the mechanism through which FQHC designation is associated with greater practice capabilities. While our analysis is valuable to understanding broad differences, further in-depth work is necessary to better inform policymakers and stakeholders on what aspects of the FQHC program promote greater capabilities. Finally, our data do not include practices with only one or two physicians, which face unique challenges.5,25,26,29
Overall our results suggest that initiatives aimed at improving the efficiency and quality of the health care system may require nuanced consideration of the safety net. Evidence suggests that Americans with primary care have better access and experience,12 and that primary care practices vary in capabilities around quality and coordination.30 Our paper highlights important variation across safety net status as well. National discourse on improving care has largely overlooked the safety net, often focusing instead on large, integrated systems. In contrast, our data suggest that FQHCs have many strengths commonly accepted as important for improving health care, such as robust care management, better access to care, and consideration of the whole patient (including non-medical issues) when treating medical needs. Health centers as such may have valuable insights about improving primary care capabilities that could be valuable to the larger US health care delivery system. Better calibrating quality, payment, and delivery initiatives to include or even promote FQHCs may result in more improvement in US health care.
CONCLUSION
Federally qualified health centers stand out among primary care practices in having strong capabilities around primary care access and quality, although all safety net primary care practices have difficulty in health information exchange with other provider organizations. Our results underscore the importance of existing initiatives such as the FQHC program for strengthening US primary care, as well as the need for continued work to improve data sharing and exchange between health care providers.
Supplementary Information
(DOCX 60 kb)
Acknowledgements
AMA is the source for the raw physician data; statistics, tables, or tabulations were prepared by the authors using AMA Masterfile data.
Funding
This work was supported by the National Institute on Aging Grant #5K01AG049914 and the Agency for Healthcare Research and Quality’s (AHRQ’s) Comparative Health System Performance Initiative under Grant #1U19HS024075 which studies how health care delivery systems promote evidence-based practices and patient-centered outcomes research in delivering care.
Declarations
Conflict of Interest
The authors have received funding that supported this work in part from the National Institutes on Aging (Lewis) and the Agency for Healthcare Research and Quality (Lewis and Rodriguez).
Disclaimer
The statements, findings, conclusions, views, and opinions contained and expressed in this article are based in part on data obtained under license from IQVIA information services: OneKey subscription information services 2010–2017, IQVIA incorporated all rights reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IQVIA Incorporated or any of its affiliated or subsidiary entities. AMA is the source for the raw physician data; statistics, tables or tabulations were prepared by the authors using AMA Masterfile data.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Joynt KE, Jha AK. Characteristics of Hospitals Receiving Penalties Under the Hospital Readmissions Reduction Program. JAMA. 2013;309(4):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 2.Chen LM, Epstein AM, Orav EJ, Filice CE, Samson LW, Joynt Maddox KE. Association of Practice-Level Social and Medical Risk With Performance in the Medicare Physician Value-Based Payment Modifier Program. JAMA. 2017;318(5):453–461. doi: 10.1001/jama.2017.9643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roberts ET, Zaslavsky AM, McWilliams JM. The Value-Based Payment Modifier: Program Outcomes and Implications for Disparities. Ann Intern Med. 2018;168(4):255–265. doi: 10.7326/M17-1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis VA, Larson BK, McClurg AB, Boswell RG, Fisher ES. The Promise and Peril of Accountable Care for Vulnerable Populations: a Framework for Overcoming Obstacles. Health Aff Proj Hope. 2012;31(8):1777–1785. doi: 10.1377/hlthaff.2012.0490. [DOI] [PubMed] [Google Scholar]
- 5.Hearld LR, Alexander JA, Shi Y, Casalino LP. Pay-for-Performance and Public Reporting Program Participation and Administrative Challenges Among Small- and Medium-Sized Physician Practices. Med Care Res Rev. 2014;71(3):299–312. doi: 10.1177/1077558713509018. [DOI] [PubMed] [Google Scholar]
- 6.Chien AT, Chin MH, Davis AM, Casalino LP. Pay for Performance, Public Reporting, and Racial Disparities in Health Care. Med Care Res Rev. 2007;64(5 suppl):283S–304S. doi: 10.1177/1077558707305426. [DOI] [PubMed] [Google Scholar]
- 7.Lewis VA, Colla CH, Carluzzo KL, Kler SE, Fisher ES. Accountable Care Organizations in the United States: Market and Demographic Factors Associated with Formation. Health Serv Res. 2013;48(6pt1):1840–1858. doi: 10.1111/1475-6773.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yasaitis LC, Pajerowski W, Polsky D, Werner RM. Physicians’ Participation In ACOs Is Lower In Places With Vulnerable Populations Than In More Affluent Communities. Health Aff (Millwood) 2016;35(8):1382–1390. doi: 10.1377/hlthaff.2015.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fraze TK, Fisher ES, Tomaino MR, Peck KA, Meara E. Comparison of Populations Served in Hospital Service Areas With and Without Comprehensive Primary Care Plus Medical Homes. JAMA Netw Open. 2018;1(5). 10.1001/jamanetworkopen.2018.2169 [DOI] [PMC free article] [PubMed]
- 10.Lewis VA, Fraze T, Fisher ES, Shortell SM, Colla CH. ACOs Serving High Proportions Of Racial And Ethnic Minorities Lag In Quality Performance. Health Aff Proj Hope. 2017;36(1):57–66. doi: 10.1377/hlthaff.2016.0626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bazzoli GJ, Clement JP, Lindrooth RC, et al. Hospital Financial Condition and Operational Decisions Related to the Quality of Hospital Care. Med Care Res Rev. 2007;64(2):148–168. doi: 10.1177/1077558706298289. [DOI] [PubMed] [Google Scholar]
- 12.Levine DM, Linder JA, Landon BE. Characteristics and Disparities among Primary Care Practices in the United States. J Gen Intern Med. 2018;33(4):481–486. doi: 10.1007/s11606-017-4239-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friedberg MW, Safran DG, Coltin KL, Dresser M, Schneider EC. Readiness for the Patient-Centered Medical Home: Structural Capabilities of Massachusetts Primary Care Practices. J Gen Intern Med. 2009;24(2):162–169. doi: 10.1007/s11606-008-0856-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friedberg MW, Coltin KL, Safran DG, Dresser M, Zaslavsky AM, Schneider EC. Associations between structural capabilities of primary care practices and performance on selected quality measures. Ann Intern Med. Published online 2007. [DOI] [PubMed]
- 15.Wright B, Potter AJ, Trivedi A. Federally Qualified Health Center Use Among Dual Eligibles: Rates Of Hospitalizations And Emergency Department Visits. Health Aff Proj Hope. 2015;34(7):1147–1155. doi: 10.1377/hlthaff.2014.0823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldman LE, Chu PW, Tran H, Romano MJ, Stafford RS. Federally Qualified Health Centers and Private Practice Performance on Ambulatory Care Measures. Am J Prev Med. 2012;43(2):142–149. doi: 10.1016/j.amepre.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rothkopf J, Brookler K, Wadhwa S, Sajovetz M. Medicaid Patients Seen at Federally Qualified Health Centers Use Hospital Services Less than Those Seen by Private Providers. Health Aff Proj Hope. 2011;30(7):1335–1342. doi: 10.1377/hlthaff.2011.0066. [DOI] [PubMed] [Google Scholar]
- 18.Doty MM, Abrams MK, Hernandez SE, Stremikis K, Beal AC. Enhancing the capacity of community health centers to achieve high performance. The Commonwealth Fund; 2010.
- 19.Abrams MK, Doty MM, Ryan J, Hall D, Riley P. Ready or not? How community health centers view their preparedness to care for newly insured patients. The Commonwealth Fund; 2014.
- 20.Fisher ES, Shortell SM, Kreindler SA, Citters ADV, Larson BK. A Framework For Evaluating The Formation, Implementation, And Performance Of Accountable Care Organizations. Health Aff (Millwood) 2012;31(11):2368–2378. doi: 10.1377/hlthaff.2012.0544. [DOI] [PubMed] [Google Scholar]
- 21.Furukawa MF, Machta RM, Barrett KA, et al. Landscape of Health Systems in the United States. Med Care Res Rev. Published online 2019:1077558718823130. [DOI] [PMC free article] [PubMed]
- 22.Cohen GR, Jones DJ, Heeringa J, et al. Leveraging Diverse Data Sources to Identify and Describe U.S. Health Care Delivery Systems. eGEMs. 5(3). 10.5334/egems.200 [DOI] [PMC free article] [PubMed]
- 23.Tang Y, Chang C-CH, Lave JR, Gellad WF, Huskamp HA, Donohue JM. Patient, Physician and Organizational Influences on Variation in Antipsychotic Prescribing Behavior. J Ment Health Policy Econ. 2016;19(1):45–59. [PMC free article] [PubMed] [Google Scholar]
- 24.Marcum ZA, Bellon JE, Li J, Gellad WF, Donohue JM. New Chronic Disease Medication Prescribing by Nurse Practitioners, Physician Assistants, and Primary Care Physicians: a Cohort Study. BMC Health Serv Res. 2016;16(1):312. doi: 10.1186/s12913-016-1569-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rittenhouse DR, Casalino LP, Shortell SM, et al. Small And Medium-Size Physician Practices Use Few Patient-Centered Medical Home Processes. Health Aff (Millwood) 2011;30(8):1575–1584. doi: 10.1377/hlthaff.2010.1210. [DOI] [PubMed] [Google Scholar]
- 26.Rittenhouse DR, Ramsay PP, Casalino LP, McClellan S, Kandel ZK, Shortell SM. Increased Health Information Technology Adoption and Use Among Small Primary Care Physician Practices Over Time: a National Cohort Study. Ann Fam Med. 2017;15(1):56–62. doi: 10.1370/afm.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shortell SM, McClellan SR, Ramsay PP, Casalino LP, Ryan AM, Copeland KR. Physician Practice Participation in Accountable Care Organizations: the Emergence of the Unicorn. Health Serv Res. 2014;49(5):1519–1536. doi: 10.1111/1475-6773.12167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Timbie JW, Kranz AM, Mahmud A, Setodji CM, Damberg CL. Federally Qualified Health Center Strategies for Integrating Care with Hospitals and Their Association with Measures of Communication. Jt Comm J Qual Patient Saf. 2019;45(9):620–628. doi: 10.1016/j.jcjq.2019.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Casalino LP, Wu FM, Ryan AM, et al. Independent Practice Associations And Physician-Hospital Organizations Can Improve Care Management For Smaller Practices. Health Aff (Millwood) 2013;32(8):1376–1382. doi: 10.1377/hlthaff.2013.0205. [DOI] [PubMed] [Google Scholar]
- 30.Levine DM, Landon BE, Linder JA. Quality and Experience of Outpatient Care in the United States for Adults With or Without Primary Care. JAMA Intern Med. 2019;179(3):363–372. doi: 10.1001/jamainternmed.2018.6716. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 60 kb)