Abstract
Since the second half of the 20th century, our knowledge about the biology of cancer has made extraordinary progress. Today, we understand cancer at the genomic and epigenomic levels, and we have identified the cell that starts neoplastic transformation and characterized the mechanisms for the invasion of other tissues. This knowledge has allowed novel drugs to be designed that act on specific molecular targets, the immune system to be trained and manipulated to increase its efficiency, and ever more effective therapeutic strategies to be developed. Nevertheless, we are still far from winning the war against cancer, and thus biomedical research in oncology must continue to be a global priority. Likewise, there is a need to reduce unequal access to medical services and improve prevention programs, especially in countries with a low human development index.
Keywords: cancer, cell therapy, epidemiology, epigenomics, genomics, immunotherapy, metastasis, stem cells, targeted therapy
Introduction
During the last one hundred years, our understanding of the biology of cancer increased in an extraordinary way.1-4 Such a progress has been particularly prompted during the last few decades because of technological and conceptual progress in a variety of fields, including massive next-generation sequencing, inclusion of “omic” sciences, high-resolution microscopy, molecular immunology, flow cytometry, analysis and sequencing of individual cells, new cell culture techniques, and the development of animal models, among others. Nevertheless, there are many questions yet to be answered and many problems to be solved regarding this disease. As a consequence, oncological research must be considered imperative.
Currently, cancer is one of the illnesses that causes more deaths worldwide.5 According to data reported in 2020 by the World Health Organization (WHO), cancer is the second cause of death throughout the world, with 10 million deaths.6 Clearly, cancer is still a leading problem worldwide. With this in mind, the objective of this article is to present a multidisciplinary and comprehensive overview of the disease. We will begin by analyzing cancer as a process, focusing on the current state of our knowledge on 4 specific aspects of its biology. Then, we will look at cancer as a global health problem, considering some epidemiological aspects, and discussing treatment, with a special focus on novel therapies. Finally, we present our vision on some of the challenges and perspectives of cancer in the 21st century.
The Biology of Cancer
Cancer is a disease that begins with genetic and epigenetic alterations occurring in specific cells, some of which can spread and migrate to other tissues.4 Although the biological processes affected in carcinogenesis and the evolution of neoplasms are many and widely different, we will focus on 4 aspects that are particularly relevant in tumor biology: genomic and epigenomic alterations that lead to cell transformation, the cells where these changes occur, and the processes of invasion and metastasis that, to an important degree, determine tumor aggressiveness.
Cancer Genomics
The genomics of cancer can be defined as the study of the complete sequence of DNA and its expression in tumor cells. Evidently, this study only becomes meaningful when compared to normal cells. The sequencing of the human genome, completed in 2003, was not only groundbreaking with respect to the knowledge of our gene pool, but also changed the way we study cancer. In the post-genomic era, various worldwide endeavors, such as the Human Cancer Genome Project, the Cancer Genome ATLAS (TCGA), the International Cancer Genome Consortium, and the Pan-Cancer Analysis Working Group (PCAWG), have contributed to the characterization of thousands of primary tumors from different neoplasias, generating more than 2.5 petabytes (1015) of genomic, epigenomic, and proteomic information. This has led to the building of databases and analytical tools that are available for the study of cancer from an “omic” perspective,7,8 and it has helped to modify classification and treatment of various neoplasms.
Studies in the past decade, including the work by the PCAWG, have shown that cancer generally begins with a small number of driving mutations (4 or 5 mutations) in particular genes, including oncogenes and tumor-suppressor genes. Mutations in TP53, a tumor-suppressor gene, for example, are found in more than half of all cancer types as an early event, and they are a hallmark of precancerous lesions.9-12 From that point on, the evolution of tumors may take decades, throughout which the mutational spectrum of tumor cells changes significantly. Mutational analysis of more than 19 000 exomes revealed a collection of genomic signatures, some associated with defects in the mechanism of DNA repair. These studies also revealed the importance of alterations in non-coding regions of DNA. Thus, for example, it has been observed that various pathways of cell proliferation and chromatin remodeling are altered by mutations in coding regions, while pathways, such as WNT and NOTCH, can be disrupted by coding and non-coding mutations. To the present date, 19 955 genes that codify for proteins and 25 511 genes for non-coding RNAs have been identified (https://www.gencodegenes.org/human/stats.html). Based on this genomic catalogue, the COSMIC (Catalogue Of Somatic Mutations In Cancer) repository, the most robust database to date, has registered 37 288 077 coding mutations, 19 396 fusions, 1 207 190 copy number variants, and 15 642 672 non-coding variants reported up to August 2020 (v92) (https://cosmic-blog.sanger.ac.uk/cosmic-release-v92/).
The genomic approach has accelerated the development of new cancer drugs. Indeed, two of the most relevant initiatives in recent years are ATOM (Accelerating Therapeutics for Opportunities in Medicine), which groups industry, government and academia, with the objective of accelerating the identification of drugs,13 and the Connectivity Map (CMAP), a collection of transcriptional data obtained from cell lines treated with drugs for the discovery of functional connections between genes, diseases, and drugs. The CMAP 1.0 covered 1300 small molecules and more than 6000 signatures; meanwhile, the CMAP 2.0 with L1000 assay profiled more than 1.3 million samples and approximately 400 000 signatures.14
The genomic study of tumors has had 2 fundamental contributions. On the one hand, it has allowed the confirmation and expansion of the concept of intratumor heterogeneity15,16; and on the other, it has given rise to new classification systems for cancer. Based on the molecular classification developed by expression profiles, together with mutational and epigenomic profiles, a variety of molecular signatures have been identified, leading to the production of various commercial multigene panels. In breast cancer, for example, different panels have been developed, such as Pam50/Prosigna, Blue Print, OncotypeDX, MammaPrint, Prosigna, Endopredict, Breast Cancer Index, Mammostrat, and IHC4.17
Currently, the genomic/molecular study of cancer is more closely integrated with clinical practice, from the classification of neoplasms, as in tumors of the nervous system,18 to its use in prediction, as in breast cancer.17 Improvement in molecular methods and techniques has allowed the use of smaller amounts of biological material, as well as paraffin-embedded samples for genomic studies, both of which provide a wealth of information.19 In addition, non-invasive methods, such as liquid biopsies, represent a great opportunity not only for the diagnosis of cancer, but also for follow-up, especially for unresectable tumors.20
Research for the production of genomic information on cancer is presently dominated by several consortia, which has allowed the generation of a great quantity of data. However, most of these consortia and studies are performed in countries with a high human development index (HDI), and countries with a low HDI are not well represented in these large genomic studies. This is why initiatives such as Human Heredity and Health in Africa (H3Africa) for genomic research in Africa are essential.21 Generation of new information and technological developments, such as third-generation sequencing, will undoubtedly continue to move forward in a multidisciplinary and complex systems context. However, the existing disparities in access to genomic tools for diagnosis, prognosis, and treatment of cancer will continue to be a pressing challenge at regional and social levels.
Cancer Epigenetics
Epigenetics studies the molecular mechanisms that produce hereditable changes in gene expression, without causing alterations in the DNA sequence. Epigenetic events are of 3 types: methylation of DNA and RNA, histone modification (acetylation, methylation, and phosphorylation), and the expression of non-coding RNA. Epigenetic aberrations can drive carcinogenesis when they alter chromosome conformation and the access to transcriptional machinery and to various regulatory elements (promoters, enhancers, and anchors for interaction with chromatin, for example). These changes may activate oncogenesis and silence tumor-suppressor mechanisms when they modulate coding and non-coding sequences (such as micro-RNAs and long-RNAs). This can then lead to uncontrolled growth, as well as the invasion and metastasis of cancer cells.
While genetic mutations are stable and irreversible, epigenetic alterations are dynamic and reversible; that is, there are several epigenomes, determined by space and time, which cause heterogeneity of the “epigenetic status” of tumors during their development and make them susceptible to environmental stimuli or chemotherapeutic treatment.22 Epigenomic variability creates differences between cells, and this creates the need to analyze cells at the individual level. In the past, epigenetic analyses measured “average states” of cell populations. These studies revealed general mechanisms, such as the role of epigenetic marks on active or repressed transcriptional states, and established maps of epigenetic composition in a variety of cell types in normal and cancerous tissue. However, these approaches are difficult to use to examine events occurring in heterogeneous cell populations or in uncommon cell types. This has led to the development of new techniques that permit marking of a sequence on the epigenome and improvement in the recovery yield of epigenetic material from individual cells. This has helped to determine changes in DNA, RNA, and histones, chromatin accessibility, and chromosome conformation in a variety of neoplasms.23,24
In cancer, DNA hypomethylation occurs on a global scale, while hypermethylation occurs in specific genomic loci, associated with abnormal nucleosome positioning and chromatin modifications. This information has allowed epigenomic profiles to be established in different types of neoplasms. In turn, these profiles have served as the basis to identify new neoplasm subgroups. For example, in triple negative breast cancer (TNBC),25 and in hepatocellular carcinoma,26 DNA methylation profiles have helped to the identification of distinct subgroups with clinical relevance. Epigenetic approaches have also helped to the development of prognostic tests to assess the sensitivity of cancer cells to specific drugs.27
Epigenetic traits could be used to characterize intratumoral heterogeneity and determine the relevance of such a heterogeneity in clonal evolution and sensitivity to drugs. However, it is clear that heterogeneity is not only determined by genetic and epigenetic diversity resulting from clonal evolution of tumor cells, but also by the various cell populations that form the tumor microenvironment (TME).28 Consequently, the epigenome of cancer cells is continually remodeled throughout tumorigenesis, during resistance to the activity of drugs, and in metastasis.29 This makes therapeutic action based on epigenomic profiles difficult, although significant advances in this area have been reported.30
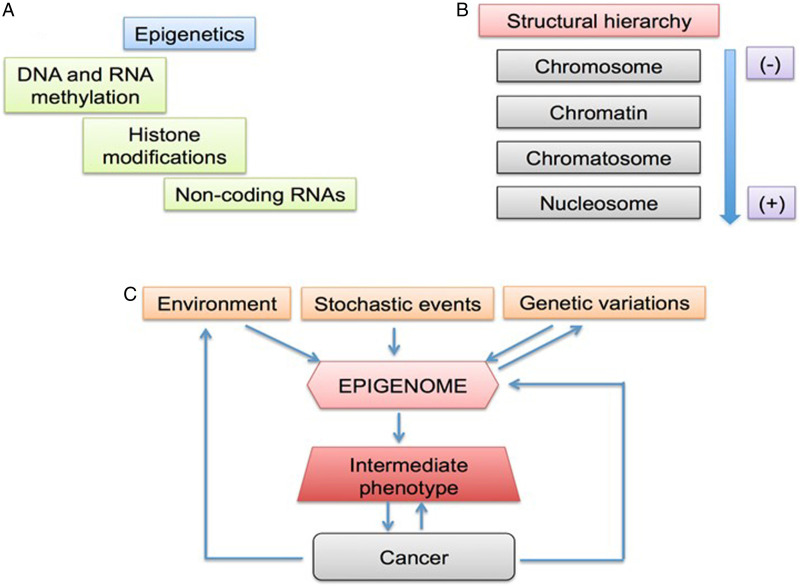
During carcinogenesis and tumor progression, epigenetic modifications are categorized by their mechanisms of regulation (Figure 1A) and the various levels of structural complexity (Figure 1B). In addition, the epigenome can be modified by environmental stimuli, stochastic events, and genetic variations that impact the phenotype (Figure 1C).31,32 The molecules that take part in these mechanisms/events/variations are therapeutic targets of interest with potential impact on clinical practice. There are studies on a wide variety of epidrugs, either alone or in combination, which improve antitumor efficacy.33 However, the problems with these drugs must not be underestimated. For a considerable number of epigenetic compounds still being under study, the main challenge is to translate in vitro efficacy of nanomolar (nM) concentrations into well-tolerated and efficient clinical use.34 The mechanisms of action of epidrugs may not be sufficiently controlled and could lead to diversion of the therapeutic target.35 It is known that certain epidrugs, such as valproic acid, produce unwanted epigenetic changes36; thus the need for a well-established safety profile before these drugs can be used in clinical therapy. Finally, resistance to certain epidrugs is another relevant problem.37,38
Figure 1.
Epigenetics of cancer. (A) Molecular mechanisms. (B) Structural hierarchy of epigenomics. (C) Factors affecting the epigenome. Modified from Refs. 31 and 32.
As we learn about the epigenome of specific cell populations in cancer patients, a door opens to the evaluation of sensitivity tests and the search for new molecular markers for detection, prognosis, follow-up, and/or response to treatment at various levels of molecular regulation. Likewise, the horizon expands for therapeutic alternatives in oncology with the use of epidrugs, such as pharmacoepigenomic modulators for genes and key pathways, including methylation of promoters and regulation of micro-RNAs involved in chemoresponse and immune response in cancer.39 There is no doubt that integrated approaches identifying stable pharmagenomic and epigenomic patterns and their relation with expression profiles and genetic functions will be more and more valuable in our fight against cancer.
Cancer Stem Cells
Tumors consist of different populations of neoplastic cells and a variety of elements that form part of the TME, including stromal cells and molecules of the extracellular matrix.40 Such intratumoral heterogeneity becomes even more complex during clonal variation of transformed cells, as well as influence the elements of the TME have on these cells throughout specific times and places.41 To explain the origin of cancer cell heterogeneity, 2 models have been put forward. The first proposes that mutations occur at random during development of the tumor in individual neoplastic cells, and this promotes the production of various tumor populations, which acquire specific growth and survival traits that lead them to evolve according to intratumor mechanisms of natural selection.42 The second model proposes that each tumor begins as a single cell that possess 2 functional properties: it can self-renew and it can produce several types of terminal cells. As these 2 properties are characteristics of somatic stem cells,43 the cells have been called cancer stem cells (CSCs).44 According to this model, tumors must have a hierarchical organization, where self-renewing stem cells produce highly proliferating progenitor cells, unable to self-renew but with a high proliferation potential. The latter, in turn, give rise to terminal cells.45 Current evidence indicates that both models may coexist in tumor progression. In agreement with this idea, new subclones could be produced as a result of a lack of genetic stability and mutational changes, in addition to the heterogeneity derived from the initial CSC and its descendants. Thus, in each tumor, a set of neoplastic cells with different genetic and epigenetic traits may be found, which would provide different phenotypic properties.46
The CSC concept was originally presented in a model of acute myeloid leukemia.47 The presence of CSCs was later proved in chronic myeloid leukemia, breast cancer, tumors of the central nervous system, lung cancer, colon cancer, liver cancer, prostate cancer, pancreatic cancer, melanoma, and cancer of the head and neck, amongst others. In all of these cases, detection of CSCs was based on separation of several cell populations according to expression of specific surface markers, such as CD133, CD44, CD24, CD117, and CD15.48 It is noteworthy that in some solid tumors, and even in some hematopoietic ones, a combination of specific markers that allow the isolation of CSCs has not been found. Interestingly, in such tumors, a high percentage of cells with the capacity to start secondary tumors has been observed; thus, the terms Tumor Initiating Cells (TIC) or Leukemia Initiating Cells (LIC) have been adopted.46
A relevant aspect of the biology of CSCs is that, just like normal stem cells, they can self-renew. Such self-renewal guarantees the maintenance or expansion of the tumor stem cell population. Another trait CSCs share with normal stem cells is their quiescence, first described in chronic myeloid leukemia.49 The persistence of quiescent CSCs in solid tumors has been recently described in colorectal cancer, where quiescent clones can become dominant after therapy with oxaliplatin.50 In non-hierarchical tumors, such as melanoma, the existence of slow-cycling cells that are resistant to antimitogenic agents has also been proved.51 Such experimental evidence supports the idea that quiescent CSCs or TICs are responsible for both tumor resistance to antineoplastic drugs and clinical relapse after initial therapeutic success.
In addition to quiescence, CSCs use other mechanisms to resist the action of chemotherapeutic drugs. One of these is their increased numbers: upon diagnosis, a high number of CSCs are observed in most analyzed tumors, making treatment unable to destroy all of them. On the other hand, CSCs have a high number of molecular pumps that expulse drugs, as well as high numbers of antiapoptotic molecules. In addition, they have very efficient mechanisms to repair DNA damage. In general, these cells show changes in a variety of signaling pathways involved in proliferation, survival, differentiation, and self-renewal. It is worth highlighting that in recent years, many of these pathways have become potential therapeutic targets in the elimination of CSCs.52 Another aspect that is highly relevant in understanding the biological behavior of CSCs is that they require a specific site for their development within the tissue where they are found that can provide whatever is needed for their survival and growth. These sites, known as niches, are made of various cells, both tumor and non-tumor, as well as a variety of non-cellular elements (extracellular matrix [ECM], soluble cytokines, ion concentration gradients, etc.), capable of regulating the physiology of CSCs in order to promote their expansion, the invasion of adjacent tissues, and metastasis.53
It is important to consider that although a large number of surface markers have been identified that allow us to enrich and prospectively follow tumor stem cell populations, to this day there is no combination of markers that allows us to find these populations in all tumors, and it is yet unclear if all tumors present them. In this regard, it is necessary to develop new purification strategies based on the gene expression profiles of these cells, so that tumor heterogeneity is taken into account, as it is evident that a tumor can include multiple clones of CSCs that, in spite of being functional, are genetically different, and that these clones can vary throughout space (occupying different microenvironments and niches) and time (during the progression of a range of tumor stages). Such strategies, in addition to new in vitro and in vivo assays, will allow the development of new and improved CSC elimination strategies. This will certainly have an impact on the development of more efficient therapeutic alternatives.
Invasion and Metastasis
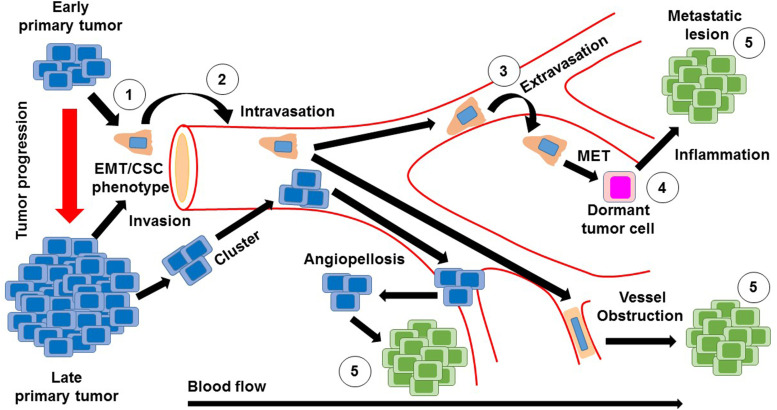
Nearly 90% of the mortality associated with cancer is related to metastasis.54 This consists of a cascade of events (Figure 2) that begins with the local invasion of a tumor into surrounding tissues, followed by intravasation of tumor cells into the blood stream or lymphatic circulation. Extravasation of neoplastic cells in areas distant from the primary tumor then leads to the formation of one or more micrometastatic lesions which subsequently proliferate to form clinically detectable lesions.4 The cells that are able to produce metastasis must acquire migratory characteristics, which occur by a process known as epithelial–mesenchymal transition (EMT), that is, the partial loss of epithelial characteristics and the acquirement of mesenchymal traits.55
Figure 2.
Invasion and metastasis cascade. Invasion and metastasis can occur early or late during tumor progression. In either case, invasion to adjacent tissues is driven by stem-like cells (cancer stem cells) that acquire the epithelial–mesenchymal transition (EMT) (1). Once they reach sites adjacent to blood vessels, tumor cells (individually or in clusters) enter the blood (2). Tumor cells in circulation can adhere to endothelium and extravasation takes place (3). Other mechanisms alternative to extravasation can exist, such as angiopelosis, in which clusters of tumor cells are internalized by the endothelium. Furthermore, at certain sites, tumor cells can obstruct microvasculature and initiate a metastatic lesion right there. Sometimes, a tumor cells that has just exit circulation goes into an MET in order to become quiescent (4). Inflammatory signals can activate quiescent metastatic cells that will proliferate and generate a clinically detectable lesion (5).
Although several of the factors involved in this process are currently known, many issues are still unsolved. For instance, it has not yet been possible to monitor in vivo the specific moment when it occurs54; the microenvironmental factors of the primary tumor that promote such a transition are not known with precision; and the exact moment during tumor evolution in which one cell or a cluster of cells begin to migrate to distant areas, is also unknown. The wide range of possibilities offered by intra- and inter-tumoral heterogeneity56 stands in the way of suggesting a generalized strategy that could resolve this complication.
It was previously believed that metastasis was only produced in late stages of tumor progression; however, recent studies indicate that EMT and metastasis can occur during the early course of the disease. In pancreatic cancer, for example, cells going through EMT are able to colonize and form metastatic lesions in the liver in the first stages of the disease.52,57 Metastatic cell clusters circulating in peripheral blood (PB) are prone to generate a metastatic site, compared to individual tumor cells.58,59 In this regard, novel strategies, such as the use of micro-RNAs, are being assessed in order to diminish induction of EMT.60 It must be mentioned, however, that the metastatic process seems to be even more complex, with alternative pathways that do not involve EMT.61,62
A crucial stage in the process of metastasis is the intravasation of tumor cells (alone or in clusters) towards the blood stream and/or lymphatic circulation.63 These mechanisms are also under intensive research because blocking them could allow the control of spreading of the primary tumor. In PB or lymphatic circulation, tumor cells travel to distant parts for the potential formation of a metastatic lesion. During their journey, these cells must stand the pressure of blood flow and escape interaction with natural killer (NK) cells .64 To avoid them, tumor cells often cover themselves with thrombocytes and also produce factors such as VEGF, angiopoietin-2, angiopoietin-4, and CCL2 that are involved in the induction of vascular permeability.54,65 Neutrophils also contribute to lung metastasis in the bloodstream by secreting IL-1β and metalloproteases to facilitate extravasation of tumor cells.64
The next step in the process of metastasis is extravasation, for which tumor cells, alone or in clusters, can use various mechanisms, including a recently described process known as angiopellosis that involves restructuring the endothelial barrier to internalize one or several cells into a tissue.66 The study of leukocyte extravasation has contributed to a more detailed knowledge of this process, in such a way that some of the proposed strategies to avoid extravasation include the use of integrin inhibitors, molecules that are vital for rolling, adhesion, and extravasation of tumor cells.67,68 Another strategy that has therapeutic potential is the use of antibodies that strengthen vascular integrity to obstruct transendothelial migration of tumor cells and aid in their destruction in PB.69
Following extravasation, tumor cells can return to an epithelial phenotype, a process known as mesenchymal–epithelial transition and may remain inactive for several years. They do this by competing for specialized niches, like those in the bone marrow, brain, and intestinal mucosa, which provide signals through the Notch and Wnt pathways.70 Through the action of the Wnt pathway, tumor cells enter a slow state of the cell cycle and induce the expression of molecules that inhibit the cytotoxic function of NK cells.71 The extravasated tumor cell that is in a quiescent state must comply with 2 traits typical of stem cells: they must have the capacity to self-renew and to generate all of the cells that form the secondary tumor.
There are still several questions regarding the metastatic process. One of the persisting debates at present is if EMT is essential for metastasis or if it plays a more important role in chemoresistance.61,62 It is equally important to know if there is a pattern in each tumor for the production of cells with the capacity to carry out EMT. In order to control metastasis, it is fundamental to know what triggers acquisition of the migratory phenotype and the intrinsic factors determining this transition. Furthermore, it is essential to know if mutations associated with the primary tumor or the variety of epigenetic changes are involved in this process.55 It is clear that metastatic cells have affinity for certain tissues, depending on the nature of the primary tumor (seed and soil hypothesis). This may be caused by factors such as the location and the direction of the bloodstream or lymphatic fluid, but also by conditioning of premetastatic niches at a distance (due to the large number of soluble factors secreted by the tumor and the recruitment of cells of the immune system to those sites).72 We have yet to identify and characterize all of the elements that participate in this process. Deciphering them will be of upmost importance from a therapeutic point of view.
Epidemiology of Cancer
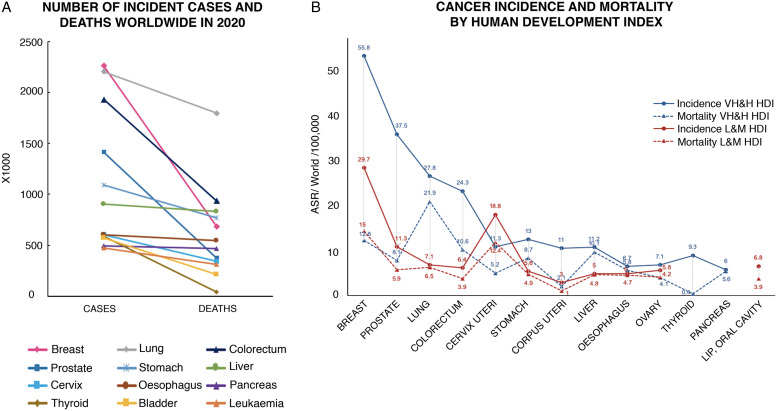
Cancer is the second cause of death worldwide; today one of every 6 deaths is due to a type of cancer. According to the International Agency for Research on Cancer (IARC), in 2020 there were approximately 19.3 million new cases of cancer, and 10 million deaths by this disease,6 while 23.8 million cases and 13.0 million deaths are projected to occur by 2030.73 In this regard, it is clear the increasing role that environmental factors—including environmental pollutants and processed food—play as cancer inducers and promoters.74 The types of cancer that produce the greatest numbers of cases and deaths worldwide are indicated in Table 1.6
Table 1.
Total Numbers of Cancer Cases and Deaths Worldwide in 2020 by Cancer Type (According to the Global Cancer Observatory, IARC).
| Cases | ||
|---|---|---|
| Both sexes | Women | Men |
| Breast (2.26 million) | Breast (2.26 million) | Lung (1.43 million) |
| Lung (2.20 million) | Colorectal (865 000) | Prostate (1.41 million) |
| Colorectal (1.93 million) | Lung (770 000) | Colorectal (1.06 million) |
| Prostate (1.41 million) | Cervical (604 000) | Stomach (719 000) |
| Stomach (1.08 million) | Thyroid (448 000) | Liver (632 000) |
Data presented on this table were obtained from Ref. 6.
As shown in Figure 3, lung, breast, prostate, and colorectal cancer are the most common throughout the world, and they are mostly concentrated in countries of high to very high human development index (HDI). Although breast, prostate, and colorectal cancer have a high incidence, the number of deaths they cause is proportionally low, mostly reflecting the great progress made in their control. However, these data also reveal the types of cancer that require further effort in prevention, precise early detection avoiding overdiagnosis, and efficient treatment. This is the case of liver, lung, esophageal, and pancreatic cancer, where the difference between the number of cases and deaths is smaller (Figure 3B). Social and economic transition in several countries has had an impact on reducing the incidence of neoplasms associated with infection and simultaneously produced an increase in the types related to reproductive, dietary, and hormonal factors.75
Figure 3.
Incidence and mortality for some types of cancer in the world. (A) Estimated number of cases and deaths in 2020 for the most frequent cancer types worldwide. (B) Incidence and mortality rates, normalized according to age, for the most frequent cancer types in countries with very high/& high (VH&H; blue) and/low and middle (L&M; red) Human Development Index (HDI). Data include both genders and all ages. Data according to https://gco.iarc.fr/today, as of June 10, 2021.
In the past 3 decades, cancer mortality rates have fallen in high HDI countries, with the exception of pancreatic cancer, and lung cancer in women. Nevertheless, changes in the incidence of cancer do not show the same consistency, possibly due to variables such as the possibility of early detection, exposure to risk factors, or genetic predisposition.76,77 Countries such as Australia, Canada, Denmark, Ireland, New Zealand, Norway, and the United Kingdom have reported a reduction in incidence and mortality in cancer of the stomach, colon, lung, and ovary, as well as an increase in survival.78 Changes in modifiable risk factors, such as the use of tobacco, have played an important role in prevention. In this respect, it has been estimated that decline in tobacco use can explain between 35% and 45% of the reduction in cancer mortality rates,79 while the fall in incidence and mortality due to stomach cancer can be attributed partly to the control of Helicobacter pylori infection.80 Another key factor in the fall of mortality rates in developed countries has been an increase in early detection as a result of screening programs, as in breast and prostate cancer, which have had their mortality rates decreased dramatically in spite of an increase in their incidence.76
Another important improvement observed in recent decades is the increase in survival rates, particularly in high HDI countries. In the USA, for example, survival rates for patients with prostate cancer at 5 years after initial diagnosis was 28% during 1947–1951; 69% during 1975–1977, and 100% during 2003–2009. Something similar occurred with breast cancer, with a 5-year survival rate of 54% in 1947–1951, 75% in 1975–1977, and 90% in 2003–2009.81 In the CONCORD 3 version, age-standardize 5-year survival for patients with breast cancer in the USA during 2010–2014 was 90%, and 97% for prostate cancer patients.82 Importantly, even among high HDI countries, significant differences have been identified in survival rates, being stage of disease at diagnosis, time for access to effective treatment, and comorbidities, the main factors influencing survival in these nations.78 Unfortunately, survival rates in low HDI countries are significantly lower due to several factors, including lack of information, deficient screening and early detection programs, limited access to treatment, and suboptimal cancer registration.82 It should be noted that in countries with low to middle HDI, neoplasms with the greatest incidence are those affecting women (breast and cervical cancer), which reflects not only a problem with access to health services, but also a serious inequality issue that involves social, cultural, and even religious obstacles.83
Up to 42% of incident cases and 47% of deaths by cancer in the USA are due to potentially modifiable risk factors such as use of tobacco, physical activity, diet, and infection.84 It has been calculated that 2.4 million deaths by cancer, mostly of the lung, can be attributed to tobacco.73 In 2020, the incidence rate of lung cancer in Western Africa was 2.2, whereas in Polynesia and Eastern Asia was 37.3 and 34.4, respectively.6 In contrast, the global burden of cancer associated with infection was 15.4%, but in Sub-Saharan Africa it was 30%.85 Likewise, the incidence of cervical cancer in Eastern Africa was 40.1, in contrast with the USA and Canada that have a rate of 6.2. This makes it clear that one of the challenges we face is the reduction of the risk factors that are potentially modifiable and associated with specific types of cancer.
Improvement of survival rates and its disparities worldwide are also important challenges. Five-year survival for breast cancer—diagnosed during 2010-2014— in the USA, for example, was 90%, whereas in countries like South Africa it was 40%.82 Childhood leukemia in the USA and several European countries shows a 5-year survival of 90%, while in Latin-American countries it is 50–76%.86 Interestingly, there are neoplasms, such as pancreatic cancer, for which there has been no significant increase in survival, which remains low (5–15%) both in developed and developing countries.82
Although data reported on global incidence and mortality gives a general overview on the epidemiology of cancer, it is important to note that there are great differences in coverage of cancer registries worldwide. To date, only 1 out of every 3 countries reports high quality data on the incidence of cancer.87 For the past 50 years, the IARC has supported population-based cancer registries; however, more than one-third of the countries belonging to the WHO, mainly countries of low and middle income (LMIC), have no data on more than half of the 18 indicators of sustainable development goals.88 High quality cancer registries only cover 4% of the population in Africa, 8% in Asia, and 7% in Latin America, contrasting with 83% in the USA and Canada, and 33% in Europe.89 In response to this situation, the Global Initiative for Cancer Registry Development was created in 2012 to generate improved infrastructure to permit greater coverage and better quality registries, especially in countries with low and middle HDI.88 It is expected that initiatives of this sort in the coming years will allow more and better information to guide strategies for the control of cancer worldwide, especially in developing regions. This will enable survival to be measured over longer periods of time (10, 15, or 20 years), as an effective measure in the control of cancer. The WHO has established as a target for 2025 to reduce deaths by cancer and other non-transmissible diseases by 25% in the population between the ages of 30–69; such an effort requires not only effective prevention measures to reduce incidence, but also more efficient health systems to diminish mortality and increase survival. At the moment, it is an even greater challenge because of the effects of the COVID-19 pandemic which has negatively impacted cancer prevention and health services.90
Oncologic Treatments
A General Perspective
At the beginning of the 20th century, cancer treatment, specifically treatment of solid tumors, was based fundamentally on surgical resection of tumors, which together with other methods for local control, such as cauterization, had been used since ancient times.91 At that time, there was an ongoing burst of clinical observations along with interventions sustained on fundamental knowledge about physics, chemistry, and biology. In the final years of the 19th century and the first half of the 20th, these technological developments gave rise to radiotherapy, hormone therapy, and chemotherapy.92-94 Simultaneously, immunotherapy was also developed, although usually on a smaller scale, in light of the overwhelming progress of chemotherapy and radiotherapy.95
Thus began the development and expansion of disciplines based on these approaches (surgery, radiotherapy, chemotherapy, hormone therapy, and immunotherapy), with their application evolving ever more rapidly up to their current uses. Today, there is a wide range of therapeutic tools for the care of cancer patients. These include elements that emerged empirically, arising from observations of their effects in various medical fields, as well as drugs that were designed to block processes and pathways that form part of the physiopathology of one or more neoplasms according to knowledge of specific molecular alterations. A classic example of the first sort of tool is mustard gas, originally used as a weapon in war,96 but when applied for medical purposes, marked the beginning of the use of chemicals in the treatment of malignant neoplasms, that is, chemotherapy.94 A clear example of the second case is imatinib, designed specifically to selectively inhibit a molecular alteration in chronic myeloid leukemia: the Bcr-Abl oncoprotein.97
It is on this foundation that today the 5 areas mentioned previously coexist and complement one another. The general framework that motivates this amalgam and guides its development is precision medicine, founded on the interaction of basic and clinical science. In the forecasts for development in each of these fields, surgery is expected to continue to be the fundamental approach for primary tumors in the foreseeable future, as well as when neoplastic disease in the patient is limited, or can be limited by applying systemic or regional elements, before and/or after surgical resection, and it can be reasonably anticipated for the patient to have a significant period free from disease or even to be cured. With regards to technology, intensive exploration of robotic surgery is contemplated.98
The technological possibilities for radiotherapy have progressed in such a way that it is now possible to radiate neoplastic tissue with an extraordinary level of precision, and therefore avoid damage to healthy tissue.99 This allows administration of large doses of ionizing radiation in one or a few fractions, what is known as “radiosurgery.” The greatest challenges to the efficacy of this approach are related to radio-resistance in certain neoplasms. Most efforts regarding research in this field are concentrated on understanding the underlying biological mechanisms of the phenomenon and their potential control through radiosensitizers.100
“Traditional” chemotherapy, based on the use of compounds obtained from plants and other natural products, acting in a non-specific manner on both neoplastic and healthy tissues with a high proliferation rate, continues to prevail.101 The family of chemotherapeutic drugs currently includes alkylating agents, antimetabolites, anti-topoisomerase agents, and anti-microtubules. Within the pharmacologic perspective, the objective is to attain a high concentration or activity of such molecules in specific tissues while avoiding their accumulation in others, in order to achieve an increase in effectiveness and a reduction in toxicity. This has been possible with the use of viral vectors, for example, that are able to limit their replication in neoplastic tissues, and activate prodrugs of normally nonspecific agents, like cyclophosphamide, exclusively in those specific areas.102 More broadly, chemotherapy also includes a subgroup of substances, known as molecular targeted therapy, that affect processes in a more direct and specific manner, which will be mentioned later.
There is no doubt that immunotherapy—to be explored next—is one of the therapeutic fields where development has been greatest in recent decades and one that has produced enormous expectation in cancer treatment.103 Likewise, cell therapy, based on the use of immune cells or stem cells, has come to complement the oncologic therapeutic arsenal.43 Each and every one of the therapeutic fields that have arisen in oncology to this day continue to prevail and evolve. Interestingly, the foreseeable future for the development of cancer treatment contemplates these approaches in a joint and complementary manner, within the general framework of precision medicine,104 and sustained by knowledge of the biological mechanisms involved in the appearance and progression of neoplasms.105,106
Immunotherapy
Stimulating the immune system to treat cancer patients has been a historical objective in the field of oncology. Since the early work of William Coley107 to the achievements reached at the end of the 20th century, scientific findings and technological developments paved the way to searching for new immunotherapeutic strategies. Recombinant DNA technology allowed the synthesis of cytokines, such as interferon-alpha (IFN-α) and interleukin 2 (IL-2), which were authorized by the US Food and Drug Administration (FDA) for the treatment of hairy cell leukemia in 1986,108 as well as kidney cancer and metastatic melanoma in 1992 and 1998, respectively.109
The first therapeutic vaccine against cancer, based on the use of autologous dendritic cells (DCs), was approved by the FDA against prostate cancer in 2010. However, progress in the field of immunotherapy against cancer was stalled in the first decade of the present century, mostly due to failure of several vaccines in clinical trials. In many cases, application of these vaccines was detained by the complexity and cost involved in their production. Nevertheless, with the coming of the concept of immune checkpoint control, and the demonstration of the relevance of molecules such as cytotoxic T-lymphocyte antigen 4 (CTLA-4), and programmed cell death molecule-1 (PD-1), immunotherapy against cancer recovered its global relevance. In 2011, the monoclonal antibody (mAb) ipilimumab, specific to the CTLA-4 molecule, was the first checkpoint inhibitor (CPI) approved for the treatment of advanced melanoma.110 Later, inhibitory mAbs for PD-1, or for the PD-1 ligand (PD-L1),111 as well as the production of T cells with chimeric receptors for antigen recognition (CAR-T),112 which have been approved to treat various types of cancer, including melanoma, non-small cell lung cancer (NSCLC), head and neck cancer, bladder cancer, renal cell carcinoma (RCC), and hepatocellular carcinoma, among others, have changed the paradigm of cancer treatment.
In spite of the current use of anti-CTLA-4 and anti-PD-L1 mAbs, only a subgroup of patients has responded favorably to these CPIs, and the number of patients achieving clinical benefit is still small. It has been estimated that more than 70% of patients with solid tumors do not respond to CPI immunotherapy because either they show primary resistance, or after responding favorably, develop resistance to treatment.113 In this regard, it is important to mention that in recent years very important steps have been taken to identify the intrinsic and extrinsic mechanisms that mediate resistance to CPI immunotherapy.114 Intrinsic mechanisms include changes in the antitumor immune response pathways, such as faulty processing and presentation of antigens by APCs, activation of T cells for tumor cell destruction, and changes in tumor cells that lead to an immunosuppressive TME. Extrinsic factors include the presence of immunosuppressive cells in the local TME, such as regulatory T cells, myeloid-derived suppressor cells (MDSC), mesenchymal stem/stromal cells (MSCs), and type 2 macrophages (M2), in addition to immunosuppressive cytokines.
On the other hand, classification of solid tumors as “hot,” “cold,” or “excluded,” depending on T cell infiltrates and the contact of such infiltrates with tumor cells, as well as those that present high tumor mutation burden (TMB), have redirected immunotherapy towards 3 main strategies115 (Table 2): (1) Making T-cell antitumor response more effective, using checkpoint inhibitors complementary to anti-CTLA-4 and anti-PD-L1, such as LAG3, Tim-3, and TIGT, as well as using CAR-T cells against tumor antigens. (2) Activating tumor-associated myeloid cells including monocytes, granulocytes, macrophages, and DC lineages, found at several frequencies within human solid tumors. (3) Regulating the biochemical pathways in TME that produce high concentrations of immunosuppressive molecules, such as kynurenine, a product of tryptophan metabolism, through the activity of indoleamine 2,3 dioxygenase; or adenosine, a product of ATP hydrolysis by the activity of the enzyme 5’nucleotidase (CD73).116
Table 2.
Current Strategies to Stimulate the Immune Response for Antitumor Immunotherapy.
| Strategies | T cells | Myeloid cells | TME |
|---|---|---|---|
| Lymph node | Anti-CTLA4 | TNF-α | |
| To improve tumor antigen presentation by APCs | Anti-CD137 | IFN-α | |
| To optimize effector T-cell activation | Anti-OX40 | IL-1 | |
| Anti-CD27/CD70 | GM-CSF | ||
| HVEM | CD40L/CD40 | ||
| GITR | CDN | ||
| L-2 | ATP | ||
| IL-12 | HMGB1 | ||
| TLR | |||
| STING | |||
| RIG-1/MDA-5 | |||
| Blood vessel | CX3CL1 | ||
| To improve T-cell traffic to tumors | CXCL9 | ||
| To favor T-cell infiltration into tumors | CXCL10 | ||
| Transference of T cells bearing antigen-specific receptor | CCL5 | ||
| LFA1/ICAM1 | |||
| Selectins | |||
| CAR-T cell | |||
| TCR-T cell | |||
| Tumor | Anti-PD-L1 | Anti-CSF1/CSF1R | Anti-VEGF |
| To improve tumor antigen uptake by APCs | Anti-CTLA-4 | Anti-CCR2 | Inhibitors of IDO anti-CD73 |
| To improve recognition and killing of tumor cells by T cells | Anti-LAG-3 | PI3Kγ | ARs antagonists |
| Anti-TIM-3 | |||
| Anti-TIGIT | |||
| TNFR-agonists | |||
| IL-2 | |||
| IL-10 |
Abbreviations: TME, tumor microenvironment; IL, interleukin; TNF, Tumor Necrosis Factor; TNFR, TNF-receptor; CD137, receptor–co-stimulator of the TNFR family; OX40, member number 4 of the TNFR superfamily; CD27/CD70, member of the TNFR superfamily; CD40/CD40L, antigen-presenting cells (APC) co-stimulator and its ligand; GM-CSF, granulocyte-macrophage colony-stimulating factor; IFN, interferon; STING, IFN genes-stimulator; RIG-I, retinoic acid inducible gene-I; MDA5, melanoma differentiation-associated protein 5; CDN, cyclic dinucleotide; ATP, adenosine triphosphate; HMGB1, high mobility group B1 protein; TLR, Toll-like receptor; HVEM, Herpes virus entry mediator; GITR, glucocorticoid-induced TNFR family-related gene; CTLA4, cytotoxic T lymphocyte antigen 4; PD-L1, programmed death ligand-1; TIGIT, T-cell immunoreceptor with immunoglobulin and tyrosine-based inhibition motives; CSF1/CSF1R, colony-stimulating factor-1 and its receptor; CCR2, Type 2 chemokine receptor; PI3Kγ, Phosphoinositide 3-Kinase γ; CXCL/CCL, chemokine ligands; LFA1, lymphocyte function-associated antigen 1; ICAM1, intercellular adhesion molecule 1; VEGF, vascular endothelial growth factor; IDO, indolamine 2,3-dioxigenase; TGF, transforming growth factor; LAG-3, lymphocyte-activation gene 3 protein; TIM-3, T-cell immunoglobulin and mucin-domain containing-3; CD73, 5´nucleotidase; ARs, adenosine receptors; Selectins, cell adhesion molecules; CAR-T, chimeric antigen receptor T cell; TCR-T, T-cell receptor engineered T cell.
Apart from the problems associated with its efficacy (only a small group of patients respond to it), immunotherapy faces several challenges related to its safety. In other words, immunotherapy can induce adverse events in patients, such as autoimmunity, where healthy tissues are attacked, or cytokine release syndrome and vascular leak syndrome, as observed with the use of IL-2, both of which lead to serious hypotension, fever, renal failure, and other adverse events that are potentially lethal. The main challenges to be faced by immunotherapy in the future will require the combined efforts of basic and clinical scientists, with the objective of accelerating the understanding of the complex interactions between cancer and the immune system, and improve treatment options for patients. Better comprehension of immune phenotypes in tumors, beyond the state of PD-L1 and TME, will be relevant to increase immunotherapy efficacy. In this context, the identification of precise tumor antigenicity biomarkers by means of new technologies, such as complete genome sequencing, single cell sequencing, and epigenetic analysis to identify sites or subclones typical in drug resistance, as well as activation, traffic and infiltration of effector cells of the immune response, and regulation of TME mechanisms, may help define patient populations that are good candidates for specific therapies and therapeutic combinations.117,118 Likewise, the use of agents that can induce specific activation and modulation of the response of T cells in tumor tissue, will help improve efficacy and safety profiles that can lead to better clinical results.
Molecular Targeted Therapy
For over 30 years, and based on the progress in our knowledge of tumor biology and its mechanisms, there has been a search for therapeutic alternatives that would allow spread and growth of tumors to be slowed down by blocking specific molecules. This approach is known as molecular targeted therapy.119 Among the elements generally used as molecular targets there are transcription factors, cytokines, membrane receptors, molecules involved in a variety of signaling pathways, apoptosis modulators, promoters of angiogenesis, and cell cycle regulators.120
Imatinib, a tyrosine kinase inhibitor for the treatment of chronic myeloid leukemia, became the first targeted therapy in the final years of the 1990s.97 From then on, new drugs have been developed by design, and today more than 60 targeted therapies have been approved by the FDA for the treatment of a variety of cancers (Table 3).121 This has had a significant impact on progression-free survival and global survival in neoplasms such as non-small cell lung cancer, breast cancer, renal cancer, and melanoma.
Table 3.
FDA Approved Molecular Targeted Therapies for the Treatment of Solid Tumors.
| Drug | Therapeutic target | Indications | Biomarkers |
|---|---|---|---|
| Abemaciclib | CDK4/6 inhibitor | Breast cancer | ER+/PR+ |
| Abiraterone | Anti-androgen | Prostate cancer | AR+ |
| Afatinib | TKI anti-ErbB, EGFR (ErbB1), HER2 (ErbB2), ErbB3, ErbB4 | NSCLC | EGFR mutated |
| Deletion of exon 19 | |||
| Substitution in exon 21 (L858R) | |||
| Aflibercept | Anti-VEGF fusion protein | Colorectal cancer | |
| Alectinib | Anti-ALK TKI | NSCLC | ALK+ |
| Alpelisib | PI3K inhibitor | Breast cancer | PI3K mutated |
| Apalutamide | Anti-androgen | Prostate cancer | AR+ |
| Atezolizumab | Anti-PD-L1 mAb | Breast cancer | PD-L1 |
| Hepatocellular carcinoma | |||
| NSCLC | |||
| Bladder cancer | |||
| Avapritinib | Kinase inhibitor | GIST | PDGFRA mutated in exon 18 (D842V) |
| Avelumab | Anti-PD-L1 mAb | Renal cancer | PD-L1 |
| Bladder cancer | |||
| Neuroendocrine tumors | |||
| Axitinib | Anti-VEGF TKI | Renal cancer | |
| Bevacizumab | Anti-VEGF mAb | CNS tumors | |
| Ovarian cancer | |||
| Cervical cancer | |||
| Colorectal cancer | |||
| Hepatocellular carcinoma | |||
| NSCLC | |||
| Renal cancer | |||
| Brigatinib | Anti-ALK TKI | NSCLC | ALK+ |
| Cabozantinib | TKR inhibitor: anti-MET, anti-VEGF, anti-RET, ROS1, MER, KIT | Renal cancer | |
| Hepatocellular carcinoma | |||
| Thyroid cancer | |||
| Ceritinib | Anti-ALK TKI | NSCLC | ALK+ |
| Cetuximab | Anti-EGFR mAb | Colorectal cancer | KRAS |
| Head and Neck cancer | EGFR+ | ||
| Crizotinib | Anti-ALK TKI | NSCLC | ALK+, ROS1+ |
| Dabrafenib | BRAF inhibitor | NSCLC | BRAF-V600E, V600K |
| Thyroid cancer | |||
| Melanoma | |||
| Dacomitinib | Anti-EGFR TKI | NSCLC | EGFR+ |
| Darolutamide | Anti-androgen | Prostate cancer | AR+ |
| Durvalumab | Anti-PD-L1 mAb | NSCLC | PD-L1 |
| Bladder cancer | |||
| Encorafenib | BRAF inhibitor | Colorectal cancer | BRAF-V600E |
| Melanoma | |||
| Entrectinib | Anti-ROS1 TKI | NSCLC | ROS1+ |
| Enzalutamide | Anti-androgen | Prostate cancer | AR+ |
| Erdafitinib | Anti-FGFR-1 TKI | Bladder cancer | |
| Erlotinib | Anti-EGFR TKI | NSCLC | EGFR mutated |
| Pancreatic caner | Deletion of exon 19 | ||
| Substitution in exon 21 (L858R) | |||
| Everolimus | mTOR inhibitor | CNS tumors | |
| Pancreatic cancer | |||
| Breast cancer | |||
| Renal cancer | |||
| Fulvestrant | ER antagonist | Breast cancer | ER+/PR+ |
| Gefitinib | Anti-EGFR TKI | NSCLC | EGFR mutated |
| Deletion of exon 19 | |||
| Substitution in exon 21 (L858R) | |||
| Imatinib | Anti-KIT TKI | GIST | KIT+ |
| Dermatofibroma protuberans | |||
| Ipilimumab | Anti-CTLA-4 mAb | Colorectal cancer | |
| Hepatocellular carcinoma | |||
| NSCLC | |||
| Melanoma | |||
| Renal cancer | |||
| Lapatinib | TKI: anti-EGFR, anti-HER2 | Breast cancer | ERBB2 over-expression or amplification |
| Lenvatinib | TKR: anti-VEGF, VEGFR1 (FLT1), VEGFR2 (KDR) y VEGFR3 (FLT4); (FGF) FGFR1, 2, 3 y 4, PDGF, PDGFRA, KIT, RET | Endometrial cancer | |
| Hepatocellular carcinoma | |||
| Renal cancer | |||
| Thyroid cancer | |||
| Lorlatinib | TKI: anti-ALK, anti-ROS2 | NSCLC | ALK+, ROS1+ |
| Necitumumab | Anti-EGFR mAb | NSCLC | EGFR+ |
| Neratinib | Anti-HER2 TKI | ||
| Anti-EGFR | Breast cancer | ERBB2 over-expression or amplification | |
| Niraparib | PARP inhibitor | Ovarian cancer | BRCA1/2 mutations |
| Fallopian tube cancer | Homologous recombination deficiency | ||
| Peritoneal cancer | |||
| Nivolumab | Anti-PD-1 mAb | Colorectal cancer | PD-1 |
| Esophageal cancer | |||
| Hepatocellular carcinoma | |||
| NSCLC | |||
| Melanoma | |||
| Renal cancer | |||
| Bladder cancer | |||
| Head and Neck cancer | |||
| Olparib | PARP inhibitor | Breast cancer | BRCA1/2 mutations |
| Ovarian cancer | |||
| Pancreatic cancer | |||
| Prostate cancer | |||
| Osimertinib | Anti-EGFR TKI | NSCLC | EGFR-T790M |
| Palbociclib | CDK4/6 inhibitor | Breast cancer | RE+/RP+ |
| Pantitumumab | Anti-EGFR mAb | Colorectal cancer | KRAS |
| EGFR+ | |||
| Pazopanib | TKI: Anti-VEGF, anti-PDGFR, anti-FGFR, anti-cKIT | Renal cancer | |
| Soft tissues sarcoma | |||
| Pembrolizumab | PD-1 inhibitor | Cervical cancer | PD-1 |
| Endometrial cancer | |||
| Esophageal cancer | |||
| Gastric cancer | |||
| Hepatocellular carcinoma | |||
| NSCLC | |||
| Bladder cancer | |||
| Head and Neck cancer | |||
| Pertuzumab | Anti-HER2 mAb | Breast cancer | ERBB2 over-expression or amplification |
| Ramucirumab | Anti-VEGF mAb | Colorectal cancer | |
| Esophageal cancer | |||
| Gastric cancer | |||
| Hepatocellular carcinoma | |||
| NSCLC | |||
| Regorafenib | Anti-cKIT TKI | Colorectal cancer | KIT+ |
| Hepatocellular carcinoma | |||
| GIST | |||
| Ribociclib | CDK4/6 inhibitor | Breast cancer | ER+/PR+ |
| Ripretinib | TKI: anti-KIT, anti-PDGFR | GIST | KIT+ |
| Rucaparib | PARP inhibitor | Prostate cancer | BRCA1/2 mutations |
| Ovarian cancer | |||
| Fallopian tube cancer | |||
| Peritoneal cancer | |||
| Sacituzumab-Govitecan | Conjugated Ab anti-trop-2 | Breast cancer | RE- RP- HER2- |
| Selpercatinib | Kinase inhibitor | NSCLC | RET+ |
| Thyroid cancer | |||
| Sorafenib | Multi-kinase inhibitor: anti-PDGFR, VEGFR, cKIT, TKR | Renal cancer | |
| Hepatocellular carcinoma | |||
| Thyroid cancer | |||
| Sunitinib | Multi-kinase inhibitor: anti-PDGFR, VEGFR, cKIT, TKR | Renal cancer | |
| Pancreatic cancer | |||
| GIST | |||
| Tamoxifeno | SERM | Breast cancer | ER+/PR+ |
| Talazoparib | PARP inhibitor | Breast cancer | BRCA1/2 mutations |
| Temsirolimus | mTOR inhibitor | Renal cancer | |
| Trametinib | BRAF inhibitor | NSCLC | BRAF-V600E, V600K |
| Thyroid cancer | |||
| Melanoma | |||
| Trastuzumab | Anti-HER2 mAb | Gastric cancer | ERBB2 over-expression of amplification |
| Gastro-esophageal junction cancer | |||
| Breast cancer | |||
| Trastuzumab-Deruxtecan | Anti-HER2 conjugated Ab | Breast cancer | ERBB2 over-expression of amplification |
| Trastuzumab-Emtansine | Anti-HER2 conjugated Ab | Breast cancer | ERBB2 over-expression of amplification |
| Tucatinib | Anti-HER2 TKI | Breast cancer | ERBB2 over-expression of amplification |
| Vandetanib | TKI: anti-VEGF, anti-EGFR | Thyroid cancer | EGFR+ |
| Vemurafenib | BRAF inhibitor | Melanoma | BRAF-V600E |
Abbreviations: mAb, monoclonal antibody; ALK, anaplastic lymphoma kinase; CDK, cyclin-dependent kinase; CTLA-4, cytotoxic lymphocyte antigen-4; EGFR, epidermal growth factor receptor; FGFR, fibroblast growth factor receptor; GIST, gastrointestinal stroma tumor; mTOR, target of rapamycine in mammal cells; NSCLC, non-small cell lung carcinoma; PARP, poli (ADP-ribose) polimerase; PD-1, programmed death protein-1; PDGFR, platelet-derived growth factor receptor; PD-L1, programmed death ligand-1; ER, estrogen receptor; PR, progesterone receptor; TKR, tyrosine kinase receptors; SERM, selective estrogen receptor modulator; TKI, tyrosine kinase inhibitor; VEGFR, vascular endothelial growth factor receptor. Modified from Ref. [127].
Most drugs classified as targeted therapies form part of 2 large groups: small molecules and mAbs. The former are defined as compounds of low molecular weight (<900 Daltons) that act upon entering the cell.120 Targets of these compounds are cell cycle regulatory proteins, proapoptotic proteins, or DNA repair proteins. These drugs are indicated based on histological diagnosis, as well as molecular tests. In this group there are multi-kinase inhibitors (RTKs) and tyrosine kinase inhibitors (TKIs), like sunitinib, sorafenib, and imatinib; cyclin-dependent kinase (CDK) inhibitors, such as palbociclib, ribociclib and abemaciclib; poli (ADP-ribose) polimerase inhibitors (PARPs), like olaparib and talazoparib; and selective small-molecule inhibitors, like ALK and ROS1.122
As for mAbs, they are protein molecules that act on membrane receptors or extracellular proteins by interrupting the interaction between ligands and receptors, in such a way that they reduce cell replication and induce cytostasis. Among the most widely used mAbs in oncology we have: trastuzumab, a drug directed against the receptor for human epidermal growth factor-2 (HER2), which is overexpressed in a subgroup of patients with breast and gastric cancer; and bevacizumab, that blocks vascular endothelial growth factor and is used in patients with colorectal cancer, cervical cancer, and ovarian cancer. Other mAbs approved by the FDA include pembolizumab, atezolizumab, nivolumab, avelumab, ipilimumab, durvalumab, and cemiplimab. These drugs require expression of response biomarkers, such as PD-1 and PD-L1, and must also have several resistance biomarkers, such as the expression of EGFR, the loss of PTEN, and alterations in beta-catenin.123
Because cancer is such a diverse disease, it is fundamental to have precise diagnostic methods that allow us to identify the most adequate therapy. Currently, basic immunohistochemistry is complemented with neoplastic molecular profiles to determine a more accurate diagnosis, and it is probable that in the near future cancer treatments will be based exclusively on molecular profiles. In this regard, it is worth mentioning that the use of targeted therapy depends on the existence of specific biomarkers that indicate if the patient will be susceptible to the effects of the drug or not. Thus, the importance of underlining that not all patients are susceptible to receive targeted therapy. In certain neoplasms, therapeutic targets are expressed in less than 5% of the diagnosed population, hindering a more extended use of certain drugs.
The identification of biomarkers and the use of new generation sequencing on tumor cells has shown predictive and prognostic relevance. Likewise, mutation analysis has allowed monitoring of tumor clone evolution, providing information on changes in canonic gene sequences, such as TP53, GATA3, PIK3CA, AKT1, and ERBB2; infrequent somatic mutations developed after primary treatments, like SWI-SNF and JAK2-STAT3; or acquired drug resistance mutations such as ESR1.124 The study of mutations is vital; in fact, many of them already have specific therapeutic indications, which have helped select adequate treatments.125
There is no doubt that molecular targeted therapy is one of the main pillars of precision medicine. However, it faces significant problems that often hinder obtaining better results. Among these, there is intratumor heterogeneity and differences between the primary tumor and metastatic sites, as well as intrinsic and acquired resistance to these therapies, the mechanisms of which include the presence of heterogeneous subclones, DNA hypermethylation, histone acetylation, and interruption of mRNA degradation and translation processes.126 Nonetheless, beyond the obstacles facing molecular targeted therapy from a biological and methodological point of view, in the real world, access to genomic testing and specific drugs continues to be an enormous limitation, in such a way that strategies must be designed in the future for precision medicine to be possible on a global scale.
Cell Therapy
Another improvement in cancer treatment is the use of cell therapy, that is, the use of specific cells as therapeutic agents. This clinical procedure has 2 modalities: the first consists of replacing and regenerating functional cells in a specific tissue by means of stem/progenitor cells of a certain kind,43 while the second uses immune cells as effectors to eliminate malignant cells.127
Regarding the first type, we must emphasize the development of cell therapy based on hematopoietic stem and progenitor cells.128 For over 50 years, hematopoietic cell transplants have been used to treat a variety of hematologic neoplasms (different forms of leukemia and lymphoma). Today, it is one of the most successful examples of cell therapy, including innovative modalities, such as haploidentical transplants,129 as well as application of stem cells expanded ex vivo.130 There are also therapies that have used immature cells that form part of the TME, such as MSCs. The replication potential and cytokine secretion capacity of these cells make them an excellent option for this type of treatment.131 Neural stem cells can also be manipulated to produce and secrete apoptotic factors, and when these cells are incorporated into primary neural tumors, they cause a certain degree of regression. They can even be transfected with genes that encode for oncolytic enzymes capable of inducing regression of glioblastomas.132
With respect to cell therapy using immune cells, several research groups have manipulated cells associated with tumors to make them effector cells and thus improve the efficacy and specificity of the antitumor treatment. PB leckocytes cultured in the presence of IL-2 to obtain activated lymphocytes, in combination with IL-2 administration, have been used in antitumor clinical protocols. Similarly, infiltrating lymphocytes from tumors with antitumor activity have been used and can be expanded ex vivo with IL-2. These lymphocyte populations have been used in immunomodulatory therapies in melanoma, and pancreatic and kidney tumors, producing a favorable response in treated patients.133 NK cells and macrophages have also been used in immunotherapy, although with limited results.134,135
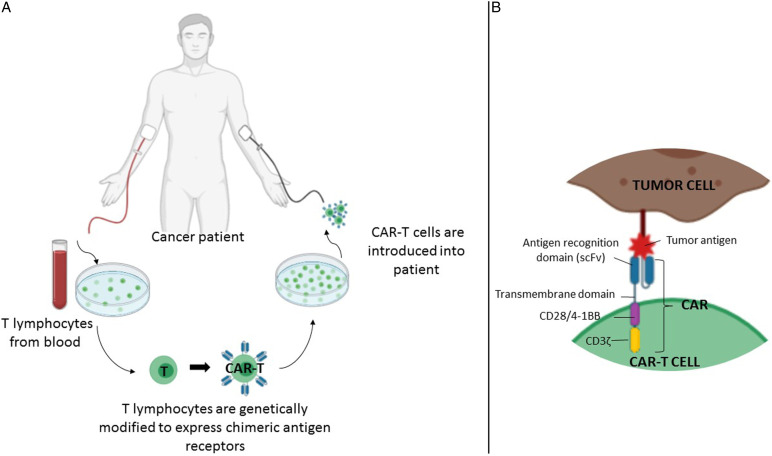
One of the cell therapies with better projection today is the use of CAR-T cells. This strategy combines 2 forms of advanced therapy: cell therapy and gene therapy. It involves the extraction of T cells from the cancer patient, which are genetically modified in vitro to express cell surface receptors that will recognize antigens on the surface of tumor cells. The modified T cells are then reintroduced in the patient to aid in an exacerbated immune response that leads to eradication of the tumor cells (Figure 4). Therapy with CAR-T cells has been used successfully in the treatment of some types of leukemia, lymphoma, and myeloma, producing complete responses in patients.136
Figure 4.
CAR-T cell therapy. (A) T lymphocytes obtained from cancer patients are genetically manipulated to produce CAR-T cells that recognize tumor cells in a very specific manner. (B) Interaction between CAR molecule and tumor antigen. CAR molecule is a receptor that results from the fusion between single-chain variable fragments (scFv) from a monoclonal antibody and one or more intracellular signaling domains from the T-cell receptor. CD3ζ, CD28 and 4-1BB correspond to signaling domains on the CAR molecule.
Undoubtedly, CAR-T cell therapy has been truly efficient in the treatment of various types of neoplasms. However, this therapeutic strategy can also have serious side effects, such as release of cytokines into the bloodstream, which can cause different symptoms, from high fever to multiorgan failure, and even neurotoxicity, leading to cerebral edema in many cases.137 Adequate control of these side effects is an important medical challenge. Several research groups are trying to improve CAR-T cell therapy through various approaches, including production of CAR-T cells directed against a wider variety of tumor cell-specific antigens that are able to attack different types of tumors, and the identification of more efficient types of T lymphocytes. Furthermore, producing CAR-T cells from a single donor that may be used in the treatment of several patients would reduce the cost of this sort of personalized cell therapy.136
Achieving wider use of cell therapy in oncologic diseases is an important challenge that requires solving various issues.138 One is intratumor cell heterogeneity, including malignant subclones and the various components of the TME, which results in a wide profile of membrane protein expression that complicates finding an ideal tumor antigen that allows specific identification (and elimination) of malignant cells. Likewise, structural organization of the TME challenges the use of cell therapy, as administration of cell vehicles capable of recognizing malignant cells might not be able to infiltrate the tumor. This results from low expression of chemokines in tumors and the presence of a dense fibrotic matrix that compacts the inner tumor mass and avoids antitumor cells from infiltrating and finding malignant target cells.
Further Challenges in the 21st Century
Beyond the challenges regarding oncologic biomedical research, the 21st century is facing important issues that must be solved as soon as possible if we truly wish to gain significant ground in our fight against cancer. Three of the most important have to do with prevention, early diagnosis, and access to oncologic medication and treatment.
Prevention and Early Diagnosis
Prevention is the most cost-effective strategy in the long term, both in low and high HDI nations. Data from countries like the USA indicate that between 40-50% of all types of cancer are preventable through potentially modifiable factors (primary prevention), such as use of tobacco and alcohol, diet, physical activity, exposure to ionizing radiation, as well as prevention of infection through access to vaccination, and by reducing exposure to environmental pollutants, such as pesticides, diesel exhaust particles, solvents, etc.74,84 Screening, on the other hand, has shown great effectiveness as secondary prevention. Once population-based screening programs are implemented, there is generally an initial increase in incidence; however, in the long term, a significant reduction occurs not only in incidence rates, but also in mortality rates due to detection of early lesions and timely and adequate treatment.
A good example is colon cancer. There are several options for colon cancer screening, such as detection of fecal occult blood, fecal immunohistochemistry, flexible sigmoidoscopy, and colonoscopy,139,140 which identify precursor lesions (polyp adenomas) and allow their removal. Such screening has allowed us to observe 3 patterns of incidence and mortality for colon cancer between the years 2000 and 2010: on one hand, an increase in incidence and mortality in countries with low to middle HDI, mainly countries in Asia, South America, and Eastern Europe; on the other hand, an increase in incidence and a fall in mortality in countries with very high HDI, such as Canada, the United Kingdom, Denmark, and Singapore; and finally a fall in incidence and mortality in countries like the USA, Japan, and France. The situation in South America and Asia seems to reflect limitations in medical infrastructure and a lack of access to early detection,141 while the patterns observed in developed countries reveal the success, even if it may be partial, of that which can be achieved by well-structured prevention programs.
Another example of success, but also of strong contrast, is cervical cancer. The discovery of the human papilloma virus (HPV) as the causal agent of cervical cancer brought about the development of vaccines and tests to detect oncogenic genotypes, which modified screening recommendations and guidelines, and allowed several developed countries to include the HPV vaccine in their national vaccination programs. Nevertheless, the outlook is quite different in other areas of the world. Eighty percent of the deaths by cervical cancer reported in 2018 occurred in low-income nations. This reveals the urgency of guaranteeing access to primary and secondary prevention (vaccination and screening, respectively) in these countries, or else it will continue to be a serious public health problem in spite of its preventability.
Screening programs for other neoplasms, such as breast, prostate, lung, and thyroid cancer have shown outlooks that differ from those just described, because, among other reasons, these neoplasms are highly diverse both biologically and clinically. Another relevant issue is the overdiagnosis of these neoplasms, that is, the diagnosis of disease that would not cause symptoms or death in the patient.142 It has been calculated that 25% of breast cancer (determined by mammogram), 50–60% of prostate cancer (determined by PSA), and 13–25% of lung cancer (determined by CT) are overdiagnosed.142 Thus, it is necessary to improve the sensitivity and specificity of screening tests. In this respect, knowledge provided by the biology of cancer and “omic” sciences offers a great opportunity to improve screening and prevention strategies. All of the above shows that prevention and early diagnosis are the foundations in the fight against cancer, and it is essential to continue to implement broader screening programs and better detection methods.
Global Equity in Oncologic Treatment
Progress in cancer treatment has considerably increased the number of cancer survivors. Nevertheless, this tendency is evident only in countries with a very solid economy. Indeed, during the past 30 years, cancer mortality rates have increased 30% worldwide.143 Global studies indicate that close to 70% of cancer deaths in the world occur in nations of low to middle income. But even in high-income countries, there are sectors of society that are more vulnerable and have less access to cancer treatments.144 Cancer continues to be a disease of great social inequality.
In Europe, the differences in access to cancer treatment are highly marked. These treatments are more accessible in Western Europe than in its Eastern counterpart.145 Furthermore, highly noticeable differences between high-income countries have been detected in the cost of cancer drugs.146 It is interesting to note that in many of these cases, treatment is too costly and the clinical benefit only marginal. Thus, the importance of these problems being approached by competent national, regional, and global authorities, because if these new drugs and therapeutic programs are not accessible to the majority, progress in biomedical, clinical and epidemiological research will have a limited impact in our fight against cancer. We must not forget that health is a universal right, from which low HDI countries must not be excluded, nor vulnerable populations in nations with high HDI. The participation of a well-informed society will also be fundamental to achieve a global impact, as today we must fight not only against the disease, but also against movements and ideas (such as the anti-vaccine movement and the so-called miracle therapies) that can block the medical battle against cancer.
Final Comments
From the second half of the 20th century to the present day, progress in our knowledge about the origin and development of cancer has been extraordinary. We now understand cancer in detail in genomic, molecular, cellular, and physiological terms, and this knowledge has had a significant impact in the clinic. There is no doubt that a patient who is diagnosed today with a type of cancer has a better prospect than a patient diagnosed 20 or 50 years ago. However, we are still far from winning the war against cancer. The challenges are still numerous. For this reason, oncologic biomedical research must be a worldwide priority. Likewise, one of the fundamental challenges for the coming decades must be to reduce unequal access to health services in areas of low- to middle income, and in populations that are especially vulnerable, as well as continue improving prevention programs, including public health programs to reduce exposure to environmental chemicals and improve diet and physical activity in the general population.74,84 Fostering research and incorporation of new technological resources, particularly in less privileged nations, will play a key role in our global fight against cancer.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Hector Mayani https://orcid.org/0000-0002-2483-3782
References
- 1.Hickey R, Vouche M, Sze DY, et al. Cancer concepts and principles: Primer for the interventional oncologist-Part II. J Vasc Intervent Radiol. 2013;24(8):1167-1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Preston-Martin S, Pike MC, Ross RK, Jones PA, Henderson BE. Increased cell division as a cause of human cancer. Canc Res 1990;50(23):7415-7421. [PubMed] [Google Scholar]
- 3.Weinberg RA. The Biology of Cancer. 2nd edition. New York: Garland Science, 2013. [Google Scholar]
- 4.Hanahan D, Weinberg RA. Hallmarks of cancer: The next generation. Cell. 2011;144(5):646-674. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization . WHO Report on Cancer: Setting Priorities, Investing Wisely and Providing Care for All. 2020. Licence: CC BY-NC-SA 3.0 IGO. https://apps.who.int/iris/handle/10665/330745. [Google Scholar]
- 6.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2021;71(3):209-249. [DOI] [PubMed] [Google Scholar]
- 7.Creighton CJ. Making use of cancer genomic databases. Curr Protoc Mol Biol. 2018;121:13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang Y, Dong X, Xie B, et al. Databases and web tools for cancer genomics study. Dev Reprod Biol. 2015;13(1):46-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The ICGC/TCGA Pan-Cancer Analysis of Whole Genomes Consortium . Pan-cancer analysis of whole genomes. Nature. 2020; 578(7793): 82-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexandrov LB, Kim J, Kim J, et al. The repertoire of mutational signatures in human cancer. Nature. 2020;578(7793):94-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rheinbay E, Nielsen MM, Abascal F, et al. Analyses of non-coding somatic drivers in 2,658 cancer whole genomes. Nature. 2020;578(7793):102-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerstung M, Jolly C, Jolly C, et al. The evolutionary history of 2,658 cancers. Nature. 2020;578(7793):122-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hinkson IV, Madej B, Stahlberg EA. Accelerating therapeutics for opportunities in medicine: A paradigm shift in drug discovery. Front Pharmacol. 2020;11:770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keenan AB, Wojciechowicz ML, Wang Z, et al. Connectivity mapping: methods and applications. Annual Review of Biomedical Data Science. 2019;2:69-92. [Google Scholar]
- 15.Gerlinger M, Rowan AJ, Horswell S, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med. 2012;366(10):883-892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li M, Zhang Z, Li L, Wang X.An algorithm to quantify intratumor heterogeneity based on alterations of gene expression profiles. Communications Biology. 2020;3(1):505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vieira AF, Schmitt F. An Update on Breast Cancer Multigene Prognostic Tests-Emergent Clinical Biomarkers. Front Med. 2018;5:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016;131(6):803-820. [DOI] [PubMed] [Google Scholar]
- 19.Turnbull AK, Selli C, Martinez-Perez C, et al.Unlocking the transcriptomic potential of formalin-fixed paraffin embedded clinical tissues: Comparison of gene expression profiling approaches. BMC Bioinf. 2020;21(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mattox AK, Bettegowda C, Zhou S, Papadopoulos N, Kinzler KW, Vogelstein B. Applications of liquid biopsies for cancer. Sci Transl Med. 2019;11(507):1984. [DOI] [PubMed] [Google Scholar]
- 21.Mulder NJ, Adebiyi E, Adebiyi M, et al. Development of bioinformatics infrastructure for genomics research. Global Heart. 2017;12(2):91-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Friedmann-Morvinski D, Verma IM. Dedifferentiation and reprogramming: Origins of cancer stem cells. EMBO Rep. 2014;15(3):244-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartzman O, Tanay A. Single-cell epigenomics: techniques and emerging applications. Nat Rev Genet. 2015;16(12):716-726. [DOI] [PubMed] [Google Scholar]
- 24.Kelsey G, Stegle O, Reik W. Single-cell epigenomics: Recording the past and predicting the future. Science. 2017;358(6359):69-75. [DOI] [PubMed] [Google Scholar]
- 25.Stirzaker C, Zotenko E, Song JZ, et al. Methylome sequencing in triple-negative breast cancer reveals distinct methylation clusters with prognostic value. Nat Commun. 2015;6:5899. [DOI] [PubMed] [Google Scholar]
- 26.Hou Y, Guo H, Cao C, et al. Single-cell triple omics sequencing reveals genetic, epigenetic, and transcriptomic heterogeneity in hepatocellular carcinomas. Cell Res. 2016;26(3):304-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Litzenburger UM, Buenrostro JD, Wu B, et al. Single-cell epigenomic variability reveals functional cancer heterogeneity. Genome Biol. 2017;18(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alizadeh AA, Aranda V, Bardelli A, et al. Toward understanding and exploiting tumor heterogeneity. Nat Med. 2015;21(8):846–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lo PK, Zhou Q. Emerging techniques in single-cell epigenomics and their applications to cancer research. J Clin Genom. 2018;1(1):10.4172/JCG.1000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baylin SB, Jones PA. A decade of exploring the cancer epigenome - biological and translational implications. Nat Rev Canc. 2011;11(10):726-734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marcum J. The cancer epigenome: A review. J Biotechnol Biomed. 2019; 2(3): 67-83. [Google Scholar]
- 32.Verma M. Genome-wide association studies and epigenome-wide association studies go together in cancer control. Future Oncol. 2016;12(13):1645-1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lu Y, Chan YT, Tan HY, Li S, Wang N, Feng Y. Epigenetic regulation in human cancer: The potential role of epi-drug in cancer therapy. Mol Canc. 2020;19(1):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amato RJ. Inhibition of DNA methylation by antisense oligonucleotide MG98 as cancer therapy. Clin Genitourin Canc. 2007;5(7):422-426. [DOI] [PubMed] [Google Scholar]
- 35.Finsterer J, Zarrouk Mahjoub S. Mitochondrial toxicity of antiepileptic drugs and their tolerability in mitochondrial disorders. Expet Opin Drug Metabol Toxicol. 2012;8(1):71-79. [DOI] [PubMed] [Google Scholar]
- 36.Chen H, Dzitoyeva S, Manev H. Effect of valproic acid on mitochondrial epigenetics. Eur J Pharmacol 2012;690(1-3):51-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rathert P, Roth M, Neumann T, et al. Transcriptional plasticity promotes primary and acquired resistance to BET inhibition. Nature. 2015;525(7570):543-547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alqahtani A, Choucair K, Ashraf M, et al. Bromodomain and extra-terminal motif inhibitors: A review of preclinical and clinical advances in cancer therapy. Future Science OA. 2019;5(3):FSO372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Piña-Sánchez P, Valdez-Salazar HA, Ruiz-Tachiquín ME. Circulating microRNAs and their role in the immune response in triple-negative breast cancer. Oncology Letters. 2020;20(5):224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schiavoni G, Gabriele L, Mattei F. The tumor microenvironment: A pitch for multiple players. Frontiers Oncol. 2013;3:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prasetyanti PR, Medema JP. Intra-tumor heterogeneity from a cancer stem cell perspective. Mol Canc. 2017;16(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meacham CE, Morrison SJ. Tumour heterogeneity and cancer cell plasticity. Nature. 2013;501(7467):328-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mayani H. A glance into somatic stem cell biology. Arch Med Res. 2003;34(1):3-15. [DOI] [PubMed] [Google Scholar]
- 44.Zhu P, Fan Z. Cancer stem cells and tumorigenesis. Biophys Rep. 2018;4(4):178-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chavez-Gonzalez A, Bakhshinejad B, Pakravan K, Guzman ML, Babashah S. Novel strategies for targeting leukemia stem cells: Sounding the death knell for blood cancer. Cell Oncol. 2017;40(1):1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kreso A, Dick JE.Evolution of the cancer stem cell model. Cell Stem Cell. 2014;14(3):275-291. [DOI] [PubMed] [Google Scholar]
- 47.Lapidot T, Sirard C, Vormoor J, et al. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature. 1994;367(6464):645-648. [DOI] [PubMed] [Google Scholar]
- 48.Pan Y, Ma S, Cao K, et al. Therapeutic approaches targeting cancer stem cells. J Canc Res Therapeut. 2018;14(7):1469-1475. [DOI] [PubMed] [Google Scholar]
- 49.Holyoake T, Jiang X, Eaves C, Eaves A. Isolation of a highly quiescent subpopulation of primitive leukemic cells in chronic myeloid leukemia. Blood. 1999;94(6):2056-2064. [PubMed] [Google Scholar]
- 50.Kreso A, O'Brien CA, Van Galen P, et al. Variable clonal repopulation dynamics influence chemotherapy response in colorectal cancer. Science. 2013;339(6119):543-548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roesch A, Fukunaga-Kalabis M, Schmidt EC, et al. A temporarily distinct subpopulation of slow-cycling melanoma cells is required for continuous tumor growth. Cell. 2010;141(4):583-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou B-BS, Zhang H, Damelin M, Geles KG, Grindley JC, Dirks PB.Tumour-initiating cells: Challenges and opportunities for anticancer drug discovery. Nat Rev Drug Discov. 2009;8(10):806-823. [DOI] [PubMed] [Google Scholar]
- 53.Plaks V, Kong N, Werb Z. The cancer stem cell Niche: How essential is the Niche in regulating stemness of tumor cells? Cell Stem Cell. 2015;16(3):225-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lambert AW, Pattabiraman DR, Weinberg RA. Emerging biological principles of metastasis. Cell. 2017;168(4):670-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pastushenko I, Blanpain C. EMT transition states during tumor progression and metastasis. Trends Cell Biol. 2019;29(3):212-226. [DOI] [PubMed] [Google Scholar]
- 56.Espinoza-Sánchez NA, Vadillo E, Balandrán JC, Monroy-García A, Pelayo R, Fuentes-Pananá EM. Evidence of lateral transmission of aggressive features between different types of breast cancer cells. Int J Oncol. 2017;51(5):1482-1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rhim AD, Mirek ET, Aiello NM, et al. EMT and dissemination precede pancreatic tumor formation. Cell. 2012;148(1-2):349-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aceto N, Bardia A, Miyamoto DT, et al. Circulating tumor cell clusters are oligoclonal precursors of breast cancer metastasis. Cell. 2014;158(5):1110-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chung Y-C, Wei W-C, Hung C-N, et al. Rab11 collaborates E-cadherin to promote collective cell migration and indicates a poor prognosis in colorectal carcinoma. Eur J Clin Invest. 2016;46(12):1002-1011. [DOI] [PubMed] [Google Scholar]
- 60.Tanabe S, Quader S, Cabral H, Ono R. Interplay of EMT and CSC in cancer and the potential therapeutic strategies. Front Pharmacol. 2020;11:904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fischer KR, Durrans A, Lee S, et al. Epithelial-to-mesenchymal transition is not required for lung metastasis but contributes to chemoresistance. Nature. 2015;527(7579):472-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zheng X, Carstens JL, Kim J, et al. Epithelial-to-mesenchymal transition is dispensable for metastasis but induces chemoresistance in pancreatic cancer. Nature. 2015;527(7579):525-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zavyalova MV, Denisov EV, Tashireva LA, et al. Intravasation as a key step in cancer metastasis. Biochemistry (Mosc). 2019;84(7):762-772. [DOI] [PubMed] [Google Scholar]
- 64.Spiegel A, Brooks MW, Houshyar S, et al. Neutrophils suppress intraluminal NK Cell-mediated tumor cell clearance and enhance extravasation of disseminated carcinoma cells. Canc Discov. 2016;6(6):630-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Foss A, Muñoz-Sagredo L, Sleeman J, Thiele W. The contribution of platelets to intravascular arrest, extravasation, and outgrowth of disseminated tumor cells. Clin Exp Metastasis. 2020;37(1):47-67. [DOI] [PubMed] [Google Scholar]
- 66.Allen TA, Asad D, Amu E, et al. Circulating tumor cells exit circulation while maintaining multicellularity, augmenting metastatic potential. J Cell Sci. 2019;132(17):231516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vadillo E, Dorantes-Acosta E, Pelayo R, Schnoor M.T cell acute lymphoblastic leukemia (T-ALL): New insights into the cellular origins and infiltration mechanisms common and unique among hematologic malignancies. Blood Rev. 2018;32(1):36-51. [DOI] [PubMed] [Google Scholar]
- 68.Sökeland G, Schumacher U. The functional role of integrins during intra- and extravasation within the metastatic cascade. Mol Canc. 2019;18(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Khan KA, Kerbel RS. A new Tie1 targeted antibody blocks tumor cell extravasation and metastasis. EMBO Mol Med. 2020;12(6):e12355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Oskarsson T, Batlle E, Massagué J. Metastatic stem cells: sources, niches, and vital pathways. Cell Stem Cell. 2014;14(3):306-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Malladi S, Macalinao DG, Jin X, et al. Metastatic latency and immune evasion through autocrine inhibition of WNT. Cell. 2016;165(1):45-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Massagué J, Obenauf AC. Metastatic colonization by circulating tumour cells. Nature. 2016;529(7586):298-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ferlay J, Laversanne M, Ervik M, et al. Global Cancer Observatory: Cancer Tomorrow. International Agency for Research on Cancer, 2020. Accessed on June 13, 2021. https://gco.iarc.fr/tomorrow. [Google Scholar]
- 74.Turner MC, Andersen ZJ, Baccarelli A, et al. Air pollutants and cancer: an overview of current evidence and public health recommendations. CA Cancer J Clin. 2020; 0: 1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Freddie B, Ahmedin J, Nathan G, et al. Global cancer transitions according to the Human Development Index (2008–2030): A population-based study. Lancet Oncol. 2012;13(8):790-801. [DOI] [PubMed] [Google Scholar]
- 76.Santucci C, Carioli G, Bertuccio P, et al. Progress in cancer mortality, incidence, and survival: a global overview. Eur J Canc Prev. 2020;29(5):367-381. [DOI] [PubMed] [Google Scholar]
- 77.Frank SA. Genetic predisposition to cancer - insights from population genetics. Nat Rev Genet. 2004;5(10):764-772. [DOI] [PubMed] [Google Scholar]
- 78.Arnold M, Rutherford MJ, Bardot A, et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995-2014 (ICBP SURVMARK-2): A population-based study. Lancet Oncol. 2019;20(11):1493-1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Reitsma MB, Fullman N, Ng M, et al. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: A systematic analysis from the Global Burden of Disease Study 2015. Lancet (London, England). 2017;389(10082):1885-1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee Y-C, Chiang T-H, Chou C-K, et al. Association between helicobacter pylori eradication and gastric cancer incidence: A systematic review and meta-analysis. Gastroenterology. 2016;150(5):1113-1124. [DOI] [PubMed] [Google Scholar]
- 81.Richiardi L, Terracini B. International agency for research on cancer. The first 50 years, 2016. [Google Scholar]
- 82.Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet (London, England). 2018;391(10125):1023-1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ginsburg O, Badwe R, Boyle P, et al. Changing global policy to deliver safe, equitable, and affordable care for women’s cancers. Lancet. 2017;389(10071):871-880. [DOI] [PubMed] [Google Scholar]
- 84.Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA A Cancer J Clin. 2018;68(1):31-54. [DOI] [PubMed] [Google Scholar]
- 85.Parkin DM, Hämmerl L, Ferlay J, Kantelhardt EJ. Cancer in Africa 2018: The role of infections. Int J Canc. 2020;146(8):2089-2103. [DOI] [PubMed] [Google Scholar]
- 86.Kehm RD, Spector LG, Poynter JN, Vock DM, Altekruse SF, Osypuk TL. Does socioeconomic status account for racial and ethnic disparities in childhood cancer survival? Cancer. 2018;124(20):4090-4097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.IARC . The value of cancer data. https://gicr.iarc.fr/about-the-gicr/value-of-cancer-data/16 June 2021.
- 88.Mery L, Bray F. Population-based cancer registries: A gateway to improved surveillance of non-communicable diseases. Ecancermedicalscience. 2020;14:ed95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Piñeros M, Abriata MG, Mery L, Bray F.Cancer registration for cancer control in Latin America: a status and progress report. Revista Panamericana de salud publica = Pan American Journal of Public Health. 2017;41:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Raymond E, Thieblemont C, Alran S, Faivre S. Impact of the COVID-19 outbreak on the management of patients with cancer. Targeted Oncol. 2020;15(3):249-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lawrence WJ. History of surgical oncology. In: Norton J, (ed). Surgery: Basic Science and Clinical Evidence. USA: Springer Verlag; 2001. [Google Scholar]
- 92.Beatson GT. On the treatment of inoperable cases of carcinoma of the mamma: Suggestions for a new method of treatment, with illustrative cases. Transactions. Medico-Chirurgical Society of Edinburgh. 1896;15:153-179. [PMC free article] [PubMed] [Google Scholar]
- 93.Leake R.100 years of the endocrine battle against breast cancer. Lancet. 1996;347(9018):1780-1781. [DOI] [PubMed] [Google Scholar]
- 94.DeVita VT, Chu E. A history of cancer chemotherapy. Canc Res. 2008;68(21):8643-8653. [DOI] [PubMed] [Google Scholar]
- 95.Decker WK, Safdar A. Bioimmunoadjuvants for the treatment of neoplastic and infectious disease: Coley’s legacy revisited. Cytokine Growth Factor Rev. 2009;20(4):271-281. [DOI] [PubMed] [Google Scholar]
- 96.Adair FE, Bagg HJ. Experimental and clinical studies on the treatment of cancer by dichlorethylsulphide (mustard gas). Ann Surg. 1931;93(1):190-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Druker BJ, Talpaz M, Resta DJ, et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med. 2001;344(14):1031-1037. [DOI] [PubMed] [Google Scholar]
- 98.Abitbol J, Gotlieb W, Zeng Z, et al. Incorporating robotic surgery into the management of ovarian cancer after neoadjuvant chemotherapy. International Journal of Gynecologic Cancer. 2019;29(9):1341, 1347. [DOI] [PubMed] [Google Scholar]
- 99.Meredith A, Morgan RKTH, Lawrence TS. Essentials of Radiation Therapy. In: De Vita VT, Jr., Lawrence TS, Rosenberg SA, (ed). Cancer: Principles and Practice of Oncology. USA: Wolters Kluwer; 2019. [Google Scholar]
- 100.Liauw SL, Connell PP, Weichselbaum RR. New paradigms and future challenges in radiation oncology: an update of biological targets and technology. Sci Transl Med. 2013;5(173):173sr2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dew KD. Cancer Therapeutics. In: Vincent T De Vita TSL, Jr., Rosenberg SA, (eds). Cancer: Principles and Practice of Oncology. USA: Wolters Kluwer; 2019. [Google Scholar]
- 102.Chase M, Chung RY, Chiocca EA. An oncolytic viral mutant that delivers the CYP2B1 transgene and augments cyclophosphamide chemotherapy. Nat Biotechnol. 1998;16(5):444-448. [DOI] [PubMed] [Google Scholar]
- 103.JWaJ G. Cancer Immunotherapy. In: Vincent T De Vita TSL, Jr., Rosenberg SA, (ed). Cancer: Principles and Practice of Oncology. USA: Wolters Kluwer; 2019. [Google Scholar]
- 104.Friedman AA, Letai A, Fisher DE, Flaherty KT.Precision medicine for cancer with next-generation functional diagnostics. Nat Rev Canc. 2015; 15(12): 747-756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Slamon DJ, Leyland-Jones B, Shak S, et al. Use of Chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783-792. [DOI] [PubMed] [Google Scholar]
- 106.Gustavsson B, Carlsson G, Machover D, et al. A review of the evolution of systemic chemotherapy in the management of colorectal cancer. Clin Colorectal Canc. 2015;14(1):1-10. [DOI] [PubMed] [Google Scholar]
- 107.Coley WB. The treatment of inoperable sarcoma by bacterial toxins (the mixed toxins of the Streptococcus erysipelas and the Bacillus prodigiosus). Proc Roy Soc Med. 1910; 3:1-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Quesada J, Hersh E, Manning J, et al. Treatment of hairy cell leukemia with recombinant alpha-interferon. Blood. 1986;68(2):493-497. [PubMed] [Google Scholar]
- 109.Rosenberg SA. IL-2: the first effective immunotherapy for human cancer. J Immunol. 2014;192(12):5451-5458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010; 363(8):711-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science. 2018; 359(6382):1350-1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fesnak AD, June CH, Levine BL. Engineered T cells: The promise and challenges of cancer immunotherapy. Nat Rev Canc. 2016; 16(9):566-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Das S, Johnson DB. Immune-related adverse events and anti-tumor efficacy of immune checkpoint inhibitors. Journal for ImmunoTherapy of Cancer. 2019; 7(1):306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bai R, Chen N, Li L, et al. Mechanisms of cancer resistance to immunotherapy. Frontiers Oncol. 2020;10:1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Egen JG, Ouyang W, Wu LC. Human anti-tumor immunity: Insights from immunotherapy clinical trials. Immunity 2020;52(1):36-54. [DOI] [PubMed] [Google Scholar]
- 116.Mora-García ML, Ávila-Ibarra LR, García-Rocha R, et al. Cervical cancer cells suppress effector functions of cytotoxic T cells through the adenosinergic pathway. Cell Immunol. 2017;320:46-55. [DOI] [PubMed] [Google Scholar]
- 117.Galon J, Bruni D. Tumor immunology and tumor evolution: Intertwined histories. Immunity .2020;52:55-81. [DOI] [PubMed] [Google Scholar]
- 118.Riley RS, June CH, Langer R, Mitchell MJ. Delivery technologies for cancer immunotherapy. Nat Rev Drug Discov. 2019;18(3):175-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Millner LM, Strotman LN.The future of precision medicine in oncology. Clin Lab Med. 2016;36(3):557-573. [DOI] [PubMed] [Google Scholar]
- 120.Lee YT, Tan YJ, Oon CE. Molecular targeted therapy: Treating cancer with specificity. Eur J Pharmacol. 2018;834:188-196. [DOI] [PubMed] [Google Scholar]
- 121.Sánchez NS, Mills GB, Mills Shaw KR.Precision oncology: Neither a silver bullet nor a dream. Pharmacogenomics. 2017;18(16):1525-1539. [DOI] [PubMed] [Google Scholar]
- 122.Bedard PL, Hyman DM, Davids MS, Siu LL.Small molecules, big impact: 20 years of targeted therapy in oncology. Lancet (London, England). 2020;395(102299):1078-1088. [DOI] [PubMed] [Google Scholar]
- 123.Tsimberidou AM, Fountzilas E, Nikanjam M, Kurzrock R.Review of precision cancer medicine: Evolution of the treatment paradigm. Canc Treat Rev. 2020;86:102019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yates LR, Knappskog S, Wedge D, et al. Genomic evolution of breast cancer metastasis and relapse. Canc Cell. 2017;32(2):169-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tsimberidou A-M. Targeted therapy in cancer. Canc Chemother Pharmacol. 2015;76(6):1113-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Boumahdi S, de Sauvage FJ.The great escape: Tumour cell plasticity in resistance to targeted therapy. Nat Rev Drug Discov 2019;19(1):39-56. [DOI] [PubMed] [Google Scholar]
- 127.Yang Y. Cancer immunotherapy: Harnessing the immune system to battle cancer. J Clin Invest. 2015;125(9):3335-3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mayani H. Human hematopoietic stem cells: Concepts and perspectives on the biology and use of fresh versus in vitro-generated cells for therapeutic applications. Curr Stem Cell Rep. 2019;5:115-124. [Google Scholar]
- 129.Gokgoz Z, Arslan O. Haploidentical stem cell transplantation: T cell depleted and repleted. Transfus Apher Sci. 2018;57(2):171-173. [DOI] [PubMed] [Google Scholar]
- 130.Mayani H, Wagner JE, Broxmeyer HE. Cord blood research, banking, and transplantation: Achievements, challenges, and perspectives. Bone Marrow Transplant. 2020;55(1):48-61. [DOI] [PubMed] [Google Scholar]
- 131.Castro-Manrreza ME, Montesinos JJ. Immunoregulation by mesenchymal stem cells: Biological aspects and clinical applications. J Immunol Res. 2015;2015:394917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bagó JR, Okolie O, Dumitru R, et al. Tumor-homing cytotoxic human induced neural stem cells for cancer therapy. Sci Transl Med. 2017;9(375):eaah6510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Skrombolas D, Frelinger JG. Challenges and developing solutions for increasing the benefits of IL-2 treatment in tumor therapy. Expet Rev Clin Immunol. 2014;10(2);207-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Veluchamy JP, Kok N, van der Vliet HJ, et al. The rise of allogeneic natural killer cells as a platform for cancer immunotherapy: Recent innovations and future developments. Front Immunol. 2017;8:1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Li X, Liu R, Su X, et al. Harnessing tumor-associated macrophages as aids for cancer immunotherapy. Mol Canc 2019;18(1):177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mohanty R, Chowdhury CR, Arega S, Sen P, Ganguly P, Ganguly N. CAR T cell therapy: A new era for cancer treatment (Review). Oncol Rep. 2019;42(6):2183-2195. [DOI] [PubMed] [Google Scholar]
- 137.Brudno JN, Kochenderfer JN. Recent advances in CAR T-cell toxicity: Mechanisms, manifestations and management. Blood Rev. 2019;34:45-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zhang Q, Ping J, Huang Z, et al. CAR-T cell therapy in cancer: Tribulations and road ahead. J Immunol Res. 2020;2020:1924379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Atkin WS, Edwards R, Kralj-Hans I, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: A multicentre randomised controlled trial. Lancet. 2010;375(9726):1624-1633. [DOI] [PubMed] [Google Scholar]
- 140.Doubeni CA, Corley DA, Quinn VP, et al. Effectiveness of screening colonoscopy in reducing the risk of death from right and left colon cancer: A large community-based study. Gut. 2018;67(2):291-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683-691. [DOI] [PubMed] [Google Scholar]
- 142.Srivastava S, Koay EJ, Borowsky AD, et al. Cancer overdiagnosis: A biological challenge and clinical dilemma. Nat Rev Canc. 2019;19(6):349-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA A Cancer J Clin. 2018;68(1):7-30. [DOI] [PubMed] [Google Scholar]
- 144.McCormick PJ. Cancer tsunami: Emerging trends, economic burden, and perioperative implications. Curr Anesthesiol Rep. 2018;8(4):348-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Wilking N, Bucsics A, Kandolf Sekulovic L, et al. Achieving equal and timely access to innovative anticancer drugs in the European Union (EU): summary of a multidisciplinary CECOG-driven roundtable discussion with a focus on Eastern and South-Eastern EU countries. ESMO Open. 2019;4:e000550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Salas-Vega S, Shearer E, Mossialos E. Relationship between costs and clinical benefits of new cancer medicines in Australia, France, the UK, and the US. Soc Sci Med 2020; 258: 113042. [DOI] [PubMed] [Google Scholar]